Knee and Lower Leg
Knee
More than 1 million knee injuries are treated annually in North American emergency departments (EDs).1 These injuries range in severity from minor contusions to limb-threatening injuries to the popliteal artery. The knee joins the longest mechanical levers in the body, the femur and tibia, and is therefore subject to high forces. It is the largest and most complex joint in the body and functions through a complicated interaction of flexion, extension, rotation, gliding, and rolling. Its large synovial space frequently is involved in infections and other inflammatory conditions.
Principles of Disease: Anatomy and Pathophysiology
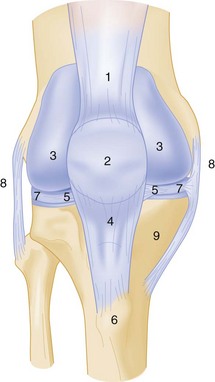
The knee is a modified-hinge diarthrodial synovial joint that consists of the tibiofemoral and patellofemoral joints.2 The head of the fibula, although not part of this articulation, is closely approximated laterally and provides a site for the attachment of muscles and ligaments. Joint stability is provided by ligaments, although surrounding muscles and the joint capsule contribute as well (Fig. 57-1).
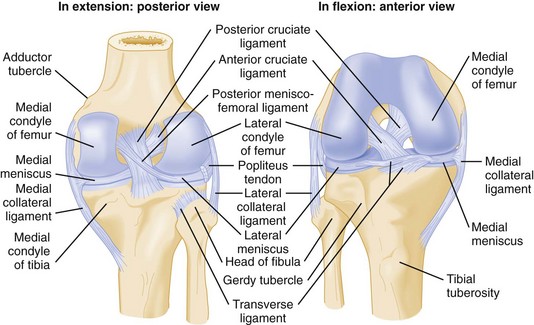
Figure 57-1 Posterior and anterior views of the right knee.
Depending on the population studied, management of knee and leg fractures commonly requires immobilization, which can result in deep vein thrombosis in up to 19% of patients. Prophylactic treatment with low-molecular-weight heparin reduces this risk.3
Clinical Features
Dislocation is among the most serious of knee injuries, because the popliteal artery is commonly injured. Because many knee dislocations reduce spontaneously before the patient arrives at the ED, normal findings on physical examination and radiographs do not rule out a recent dislocation.4 If a history of knee dislocation is suspected or when a trauma patient has unexplained vascular insufficiency of the foot, thorough evaluation of the neurovascular status of the feet is an integral part of the secondary trauma survey.
Physical Examination
Proper examination of the knee requires the patient to be supine with both legs exposed. The question of whether knee pain may be the result of hip or spine pathology should be raised early, and the neurovascular integrity of the foot should be assessed. Examination of the knee begins with visual inspection (Box 57-1), followed by palpation (Fig. 57-2). Any obvious deformity, swelling, effusion, or ecchymosis is noted. Localized swelling should be distinguished from the presence of a joint effusion, which may obliterate the normal contour of the knee. If a large effusion is present, the patella is elevated from the femur by fluid, and the patella can be “ballotted” against the femur. Loss of the medial peripatellar concavity may be the only sign of a small knee effusion. A small knee effusion may be accentuated by milking the suprapatellar pouch inferiorly to force fluid into the knee joint. An effusion in the prepatellar bursa is found just beneath the skin anterior to the patella; this should not be confused with a knee effusion.
Tests for Specific Injuries and Disturbances
Stability Testing: Although range of motion is important for documentation of disability, it is stability testing that provides the most specific diagnostic information. Stability testing seeks to identify tears of the four major ligaments of the knee—the ACL, PCL, MCL, and LCL. Stability testing in the acute phase is often misleading owing to splinting and effusion and is often not clinically useful in the ED. When the acute phase has passed, the goal of stability testing is to determine whether a patient may benefit from orthopedic referral for evaluation and repair.
Anterior Drawer Test: The anterior drawer test seeks to identify tears of the ACL. A positive test result is defined as greater anterior movement of the tibia as compared with the other knee. The test is performed with the patient in a supine position, the hip flexed at 45 degrees, and the knee flexed at 90 degrees. The examiner may stabilize the patient’s tibia by sitting on the patient’s foot. The examiner then determines the amount of step-off between the femoral condyle and the tibial plateau by placing the thumbs over the joint line while exerting a smooth, gentle pull anteriorly on the tibia. The amount of forward displacement is compared with that on the normal side. Significant laxity relative to the contralateral knee is fairly specific for ACL disruption, although a false-positive result can be caused by PCL insufficiency, which allows the tibia to slip back on the femur, with anterior movement as the slack in the PCL is taken up. Sensitivity of the anterior drawer test is poor—10% acutely and only 50% with general anesthesia.5 False-negative findings may result from an effusion preventing knee flexion to 90 degrees, insufficient force applied during the test, or simply the strength of the knee flexors and extensors preventing abnormal movement.
Lachman’s Test: Lachman’s test is the most accurate physical test for anterior cruciate ligament damage, with a sensitivity of 80% when performed acutely and 100% when performed with the patient under general anesthesia.5 Lachman’s test is done with the knee flexed 20 to 30 degrees while the examiner uses one hand to grasp the thigh and stabilize it. The tibia is pulled anteriorly, and the examiner notes tibial excursion. The examiner records “firmness” or a “soft endpoint.” The endpoint can be graded as 1+ (0-5 mm more displacement than on the normal side), 2+ (5-10 mm), or 3+ (more than 10 mm). The knee should be in a neutral position before manipulation, and the PCL must be intact for the test results to be valid. In an acute injury, any difference in translation or the feeling of a soft or indistinct endpoint may indicate a ligament tear. A PCL injury results in a false-positive test result as the knee is pulled forward. Potential causes of false-negative test results include hamstrings that are very strong or in spasm, meniscal tears, and third-degree MCL tears with posterior medial extension. Partial tears are not detected reliably. Lachman’s test is difficult if the examiner’s hands are small relative to the patient’s thigh.
Pivot Shift Test: The pivot shift test, also called subluxation provocation or the jerk test, is performed to detect anterolateral rotatory instability associated with an injury to the ACL or lateral capsular structure. This test should be done carefully, if at all, in the acutely injured knee because the test maneuvers can exacerbate the initial injury. Sensitivity in the acute phase is only 27%, but the test is highly specific for ACL tear.6
Posterior Drawer Test: The posterior drawer test assesses for PCL injury.5 The posterior drawer test can be accomplished with the patient’s knee flexed at 90 degrees and the foot stabilized by the examiner’s thigh. A smooth backward force is applied to the tibia. Posterior displacement of the tibia more than 5 mm, or a “soft endpoint,” indicates injury to the PCL. A normal knee should exhibit no significant posterior excursion. The posterior drawer test result may be positive in only 85% of patients with PCL insufficiency documented operatively.
Posterior Sag Sign Test: The posterior sag sign test is a second method of determining PCL integrity. Sensitivity in the acute phase is 79%.5 The test is done as follows. The patient is placed in a supine position, and a pillow is placed under the distal thigh for support while the heel rests on the stretcher. The knee is flexed to either 45 or 90 degrees, depending on which position provides the greater muscle relaxation. If the tibia sags backward, the test result is considered to be positive, indicating PCL insufficiency. If the posterior sag sign is not appreciated before the different drawer tests are performed, a false-positive result on the anterior drawer test is misinterpreted as an ACL injury. Posterior sag also may be shown by passive elevation of the leg in a fully extended position, with the examiner applying the elevating force at the ankle. As the leg is elevated, the tibia may fall back on the femur if the PCL is ruptured.
Instrument Testing: Arthrometers are devices that quantitate anterior displacement of the tibia relative to the femur and are far more accurate in diagnosing ACL tears than the anterior drawer and Lachman’s tests, although these devices are rarely used in the ED setting. Studies in which commercially available arthrometers were used indicate that a side-to-side difference exceeding 3 mm of anterior displacement at 20 pounds is predictive of ACL injury with high accuracy.7
Collateral Ligament Stress Test: The collateral ligament stress test is used to test the integrity of the MCL and LCL. With the patient lying supine, the examiner applies varus and valgus stress with the knee at 0 and 30 degrees of flexion. Joint line opening is the amount of movement (i.e., hinging) produced between the tibia and the femur; this can be palpated and estimated in millimeters. The normal knee should be subjected to the same amount of valgus and varus stress, and the joint line opening is then compared with that in the injured knee. Isolated collateral ligament tears are detected only with the knee in slight flexion, because in extension the cruciate ligaments, capsule, and lesser ligaments of the knee provide significant lateral stability. Laxity in full extension implies complete collateral ligament tear and also injury to the cruciate ligaments or other structures. Laxity may be graded as follows: grade I, some laxity; grade II, marked laxity; and grade III, total laxity.
Assessing for Meniscal Tears: Meniscal tears are difficult to diagnose in the acute setting, and these assessments are best reserved for the convalescent phase. Even then, small meniscal tears can cause significant symptoms but may not be detected on physical examination, and arthroscopic evaluation may be required for diagnosis. However, meniscal tears are likely to limit activity, rather than leading to further damage, so there is less urgency. By contrast, failure to diagnose a nondisplaced fracture can lead to displacement and severe consequences.
McMurray’s Test.: McMurray’s test is used to help identify meniscal tears. The patient is placed in supine position with the knee hyperflexed. The examiner grasps the foot with one hand and the knee with the other. The examiner flexes and extends the knee while simultaneously internally and externally rotating the tibia on the femur and providing slight varus and valgus stress. A positive test result is the occurrence of clicking palpable along the joint line, or locking of the knee. Internal rotation of the leg tests the posterior segment of the lateral meniscus. External rotation tests the posterior segment of the medial meniscus. In the acute setting, limitation of range of motion may not allow sufficient hyperflexion to perform McMurray’s test, and the test result may be falsely negative.
Apley’s Test.: Apley‘s test also aids in diagnosing meniscal tears. With the patient prone, the knee is flexed 90 degrees, and the leg is internally and externally rotated with pressure applied to the heel. Pain elicited by downward pressure suggests meniscal pathology. The pain should be relieved with distraction of the knee and rotation of the leg back to a neutral position. Although relatively specific, Apley’s test is not sensitive.6
Diagnostic Strategies
Plain Radiographs: In acute knee trauma, the goal of radiography is to rule out fracture. Because radiographs are not 100% sensitive, knee immobilization and orthopedic referral for reevaluation are options. When suspicion for a fracture is extremely high, computed tomography (CT) can be used; it is more sensitive than plain films. One study found a negative predictive value of only 49% for plain films in diagnosing knee fracture, with CT as the gold standard.8 Magnetic resonance imaging (MRI) is even more sensitive but is not customarily used in the ED evaluation of knee and leg trauma.
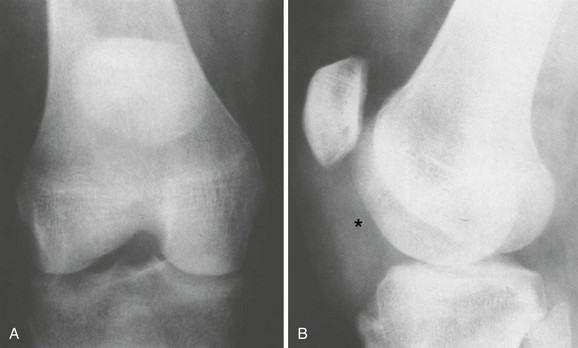
Plain films are useful for diagnosing fracture, effusion, foreign bodies, joint space narrowing, and lipohemarthrosis. Evaluating plain films begins with an assessment of bone anatomy and alignment. Nonobvious fractures are best detected by careful inspection of the cortex of all visualized bones. Any disruption of the continuous line of the cortex should raise suspicion for fracture. Subtle cortical disruptions indicate either nondisplaced fractures or draining cortical veins. The next step is to evaluate for the presence of an effusion, seen as a radiolucent area (of density similar to that of fat) distending the joint capsule. Presence of a linear interface between two different densities within an effusion suggests lipohemarthrosis (see Fig. 57-3), in which the effusion contains not only blood but also fat. This feature results from entry of marrow fat into the joint cavity and is diagnostic of fracture.
The traditional practice was to obtain anteroposterior (AP) and lateral radiographic views of the knee in all cases of acute knee trauma. More recent work has led to validation of clinical decision rules that help decrease unnecessary radiography.9–11 The Ottawa Knee Rule states that radiography is necessary only if any one of five conditions is present: (1) age older than 55 years, (2) inability to transfer weight from one foot to the next four times at the time of injury and in the ED, (3) inability to flex the knee to 90 degrees, (4) patellar tenderness with no other bone tenderness, or (5) tenderness of the fibular head. Initial tests found that this rule detected 100% of fractures while allowing significantly fewer radiographs to be done.10,11 The Pittsburgh Knee Rule similarly was found to be 100% sensitive.12 This decision rule states that radiography is necessary only if the patient fell or sustained blunt trauma to the knee and if either of two conditions is present: (1) age younger than 12 or older than 50 years or (2) inability to walk four full weight-bearing steps in the ED.
In a study comparing these two decision rules, both had good sensitivity, but the Pittsburgh rule was more specific, allowing fewer radiographs to be done without sacrificing sensitivity; in this study, the sensitivity of the Ottawa rule was 97% (95% confidence interval, 90 to 99%) and the sensitivity of the Pittsburgh rule was 99% (95% confidence interval, 94 to 100%).13 Either rule may be used, but patients should be told that this approach is associated with an approximately 1% chance of a missed fracture and that they should seek reevaluation in the event of persistent or progressive symptoms.
One study validated the Ottawa Knee Rule in children older than 5 years, finding a sensitivity of 100%. The Ottawa Knee Rule permitted a 31% reduction in the number of radiographic evaluations.14 In another pediatric study of the Ottawa Knee Rule, 1 of 13 fractures was missed, implying a sensitivity of only 92%, so application of the rule in children still requires clinical judgment.15
In another approach, investigators asked whether a single lateral radiograph could replace the traditional three-view “knee series” (AP, lateral, and tunnel views). These investigators found that a single lateral view could detect 100% of fractures identifiable on the full series.16 This innovative approach merits further study.
Computed Tomography: CT is most useful in detecting and classifying tibial plateau fractures and usually is done when the diagnosis is unclear or if operative intervention is being considered. CT angiography is an excellent tool for detecting injury to the popliteal artery, although its sensitivity relative to traditional angiography has not been quantified in large high-quality studies.17
Angiography
In the ED evaluation of trauma to the knee and leg, angiography is used to seek popliteal artery injury after knee dislocation. To obtain an angiogram, a catheter is placed in the femoral artery and contrast is injected while fluoroscopy (video x-ray examination) is performed. Complications occur in about 1.7% of these procedures, and include vascular injury and contrast nephropathy. False-positive results can lead to unnecessary surgical exploration. From a practical standpoint, the patient must be removed from the ED to a radiology suite, where other injuries cannot be addressed, and the angiography team must be mobilized, often resulting in delays in care.4 Because of these limitations, relatively accurate alternatives, including CT angiography and duplex ultrasound, have been adopted.17
Magnetic Resonance Imaging
MRI is highly accurate for diagnosis of fractures and ligamentous injuries, although it often misses small meniscal tears. It has proved to be superior to other imaging modalities in the evaluation of osteonecrosis, osteochondritis dissecans, occult fractures, and bone contusion.18 Its advantages are that it is noninvasive and painless and does not involve exposure to ionizing radiation. MRI of the knee is rarely performed on an emergency basis, because immobilization and non–weight-bearing status are the usual procedure, pending outpatient orthopedic evaluation.
Arthroscopy
Arthroscopy of the knee is the most commonly performed orthopedic surgical procedure in the United States. This nonemergent procedure is useful in diagnosis and treatment of knee injuries, including injuries of the meniscus, cruciate ligaments, articular cartilage, capsule, and synovium. The superior diagnostic accuracy of arthroscopy compared with the clinical knee examination has been well documented. In particular, arthroscopy has increased the accuracy of diagnosis of ACL injuries and small capsular tears. It is especially helpful in children, in whom diagnosis can be difficult because developing skeletal changes can obscure pathology. Difficulties in visualization arise when the capsular structures are tight and when meniscal tears are situated posteriorly. Arthroscopy is superior to MRI for diagnosis of meniscal tears and other soft tissue injuries, and the diagnosed problem can be repaired immediately. The need for arthroscopy is established in the convalescent phase of injury and need not be determined in the emergent setting, so long as appropriate referral to an orthopedist is made.19
Joint Injection
An open joint is considered a surgical emergency. When violation of the joint capsule is suspected but not obvious, the traditional approach was to inject methylene blue into the joint to see if it emerged from the laceration. Normal saline is now preferred over methylene blue, as the latter can interfere with arthroscopy and cause an inflammatory reaction. The technique is simple. With sterile technique, sterile saline is injected into the knee joint at a location distant from the laceration. If saline emerges from the laceration, an open joint is diagnosed. Historically, 50 mL was the recommended volume, but nearly 200 mL is needed to achieve a sensitivity of 95%.20 This can be accomplished with intravenous fluid and tubing; maintenance of sterility is crucial.
Knee Injuries
Anatomy and Pathophysiology: Knee dislocation refers to tibiofemoral dislocation and should not be confused with patellofemoral dislocation, a relatively minor injury. Knee dislocation is a limb-threatening emergency, because popliteal artery injury occurs frequently. Knee dislocation is uncommon but should be considered in the setting of an appropriate injury mechanism, because one half of all knee dislocations are reduced before the patient arrives at the ED.21 Reduction before ED arrival does not lessen the likelihood of vascular injury, and vascular injury should be considered in patients with severe ligamentous injuries and high-energy mechanisms.
Knee dislocations are always associated with significant ligamentous injury. The joint capsule is disrupted, with accompanying trauma to the muscles and tendons. Injury to the popliteal artery is the most severe complication and is the primary cause of morbidity and limb loss.22,23
Anatomically, dislocations are described according to the displacement of the tibia relative to the femur. They are classified into five types: anterior, posterior, medial, lateral, and rotary. More than half of all dislocations are anterior and result from hyperextension. Posterior dislocations are the second most common type and usually result from high-velocity direct trauma to the flexed knee, often in association with vehicular trauma (dashboard impact).22
Clinical Features: The diagnosis of knee dislocation is based on the mechanism of injury and clinical and radiographic findings. When a dislocation is present, it is usually obvious. There may be no effusion after reduction, because the ruptured capsule allows blood and joint fluid to escape into the thigh and leg. Some experts have advocated expanding the definition of knee dislocation to include bicruciate ligament (i.e., ACL and PCL) injuries, even when the knee is reduced on initial presentation.21 For this reason, patients with grossly unstable knees but no proven dislocation and patients who have a bicruciate ligament injury should be evaluated for concomitant injuries, as with patients with known dislocation.4
Vascular injury is a catastrophic complication of knee dislocation, and popliteal artery injury is reported in 4.8 to 65% of these patients, depending on the mechanisms of injury in the population studied.4,22 The collateral geniculate arteries around the knee also may be damaged directly or secondarily compressed by hematoma formation after the dislocation. Direct arterial injury, decreased collateral circulation, and elevated compartment pressures all may compromise limb perfusion. In addition to being clinically occult, vascular injury in blunt trauma is more difficult to manage because of associated soft tissue injury and edema.
“Hard” signs of vascular injury are absence of pulse, limb ischemia, rapidly expanding hematoma, pulsatile bleeding, and bruit or thrill over the wound, especially in penetrating injuries.24 Paresthesias in the leg should also lead to suspicion of injury to popliteal structures. When repair of a disrupted popliteal artery is delayed, the amputation rate increases with time, nearing 90% after 8 hours.23 The posterior tibial and dorsal pedal pulses should be evaluated but will be normal in 5 to 15% of popliteal artery injuries.25
Isolated intimal tears are usually managed without surgery, but a vascular surgeon should be consulted when such a tear is identified. Isolated intimal tears are not detectable on physical examination and are seen only angiographically or with duplex ultrasound. These injuries are treated with observation or anticoagulation alone but can result in popliteal artery occlusion during surgery. Injuries to small branches of the popliteal artery can be managed by observation and serial examinations, but vigilance for compartment syndrome is necessary.21
Neurologic integrity in the limb also should be assessed. Peroneal nerve injury is the most common major neurologic problem associated with knee dislocation; some degree of dysfunction occurs in 20 to 40% of patients and is permanent in approximately 80% of these.1,21,26 The peroneal nerve should be evaluated by determining sensation of the dorsum of the foot and by having the patient dorsiflex the ankle. Less commonly, the posterior tibial nerve may be injured, manifesting as diminished plantar sensation and plantar flexion of the foot. Complete nerve palsy in the acute setting is associated with a poor prognosis for recovery.26,27
Diagnostic Strategies: The diagnostic workup begins with an understanding of two crucial facts: half of all tibiofemoral dislocations are reduced before presentation, and injury to the popliteal artery is common with tibiofemoral dislocation regardless of whether there is spontaneous reduction or not. Therefore the diagnostic strategy is not applied only to the patient with known knee dislocation, but to any patient with a multiligament knee injury or with known or possible high-force trauma to the knee. The intubated multitrauma patient with ecchymosis around the knee may harbor an occult popliteal injury. The athlete with isolated knee trauma and no dislocation on presentation may end up an amputee.28
Serial physical examinations—meaning palpation of the pedal pulses—can detect most popliteal artery injuries, with a sensitivity of 79%, specificity of 91%, positive predictive value of 75%, and negative predictive value of 93%.24 This has led some authors to suggest physical examination alone as a screening tool. However, a miss rate of 7% is too high for such a devastating injury. Adding measurement of the ABI is thought to improve the sensitivity enough for safe clinical practice.
The ABI is traditional in primary care and vascular surgery clinics, where it is used to monitor arterial narrowing caused by peripheral vascular disease. The index is simply the ratio of the systolic blood pressure measured in the standard humeral location to the systolic pressure measured at the ankle. An ABI of greater than 0.9 has been found to have a negative predictive value for popliteal artery injury of 100% in knee dislocation.24
Duplex ultrasonography is thought to be equivalent to angiography as a sensitive tool for detection of traumatic occlusion or disruption of the popliteal artery, though the sensitivity has not been quantified in the setting of knee dislocation.29 CT angiography is promising, but its sensitivity has not been quantified in this setting.17,30,31
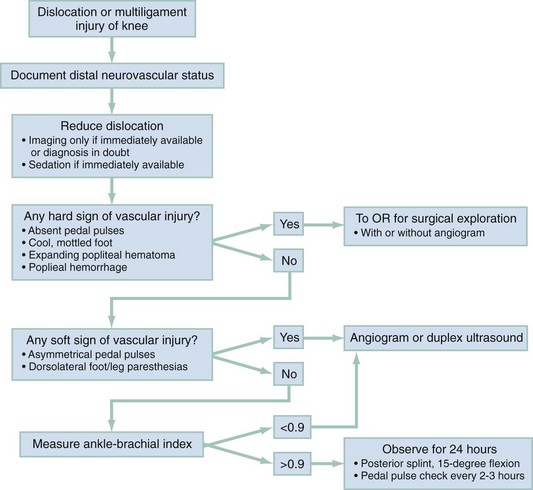
The choice of diagnostic strategy depends on the patient’s presentation. At one extreme is the patient with obviously impaired leg perfusion. In this case, emergency angiography or surgical exploration are indicated. At the other extreme is the patient with knee trauma but no clear indication that a dislocation even occurred. Figure 57-4 depicts a safe and efficient algorithm.28 During the secondary survey, the dislocation is reduced, if present on presentation. The feet are examined, and if both are warm and well perfused, dorsalis pedis and posterior tibial pulses are palpable and symmetrical, and, in the awake patient, sensation is subjectively and objectively intact, the ABI is measured. If the ABI is above 0.9, the physical examination is repeated every 3 to 4 hours for 24 hours. If no abnormalities attributable to popliteal artery disruption are detected, no further emergent workup is indicated. Before surgery to repair associated injuries, the surgeon may choose to perform duplex ultrasonography to rule out an isolated intimal tear, which, though not important to detect in the ED setting, can lead to complications during surgery. If the pedal pulses are asymmetrical or the ABI is below 0.9, immediate angiography is indicated. If pedal pulses are absent, the foot is cool or otherwise appears poorly perfused, or there is an expansile popliteal hematoma, immediate surgical exploration is indicated, with or without an arteriogram.
Management: The dislocated knee should be reduced immediately and before radiographic confirmation unless the diagnosis is in doubt. Neurovascular status should be documented before and after reduction. For patients being transferred from nontrauma centers to trauma centers, reduction should be attempted before transfer. Reduction usually can be accomplished with simple traction-countertraction, ideally with sedation. Lateral pressure may be required—for example, for an anterior dislocation, the femur can be pushed posteriorly while the tibia is pulled anteriorly—but care should be taken not to apply undue pressure to the popliteal fossa. Posterolateral dislocations may not be reducible because the medial femoral condyle and MCL secure the dislocated joint in place, in which case, emergent open reduction in the operating room is indicated.27 Because many reductions are unstable, the limb should be immobilized in a long leg posterior splint with the knee in 15 to 20 degrees of flexion, and popliteal artery injury sought, according to the algorithm shown in Figure 57-4.
Loss and disability are minimized by expedient revascularization and primary arterial repair, heparinization when not contraindicated, repair of popliteal venous injury, and aggressive wound débridement. Open joints require prophylactic antibiotics. If the neurovascular structures remain intact after dislocation, the knee joint is reduced and allowed to rest for 2 to 3 days before reconstruction of the torn ligaments is considered.27,32
Delayed complications associated with traumatic knee dislocations include deep vein thrombosis, compartment syndrome, pseudoaneurysm, and arterial thrombosis. Compartment syndromes generally develop within 24 to 48 hours of the initial injury. Pseudoaneurysms are rare but may form several hours to months after popliteal artery injury.32 Heterotopic ossification is a poorly understood syndrome of calcification of the soft tissues of the knee.33 It has been observed in uninjured knees of patients who have sustained major trauma. In its most severe form, heterotopic ossification can cause dramatic decrease in knee mobility. Almost one half of dislocated knees are found to have subsequent heterotopic ossification, although the most function-limiting form may be limited to patients with a history of severe trauma.33
Distal Femur Fractures
Anatomy and Pathophysiology: Distal femur fractures are uncommon, constituting approximately 4% of femur fractures.32 A high-energy mechanism of injury is required. An isolated fracture of the femoral condyle may occur, or the fracture may extend in a T or Y pattern to include the intercondylar or supracondylar region of the femur. Condylar fractures are intra-articular and may result in disruption of the articular surface with subsequent arthritis.
Clinical Features: Patients with condylar or intercondylar fractures have pain and swelling in the distal femur and suprapatellar region and often are unable to bear weight. Examination may reveal shortening, rotation, and angulation of the extremity and tenderness to palpation along the medial or lateral joint line. Acute hemarthrosis is common and may be caused by intra-articular extension of the fracture or associated ligamentous injury. Distal neurovascular status should be documented. Any laceration in the region of the fracture represents an open fracture until proven otherwise.
Diagnostic Strategies: Routine AP and lateral views should be obtained and usually show the fracture pattern and any significant displacement of fragments. In high-energy injuries, radiographs of the ipsilateral hip and tibia are required to exclude associated fractures. Occasionally, CT or MRI may be required to diagnose a nondisplaced fracture. MRI is more sensitive, although CT is more readily available. If signs of vascular impairment are present, consultation for angiography or surgical exploration should be obtained emergently.
Management: After the initial examination, the leg should be splinted to prevent excessive motion of the fracture site. Early orthopedic consultation is advised. In a stable patient with an uncomplicated fracture, reduction may be done with skeletal traction, followed by immobilization. Intra-articular fractures generally are treated with open reduction and internal fixation. Distal femur fractures may be associated with thrombophlebitis, fat embolus syndrome, delayed union or malunion if reduction is incomplete or not maintained, intra-articular or quadriceps adhesions if the fracture is intra-articular, angulation deformities, and osteoarthritis, particularly affecting the patellofemoral articulation.
Tibial Plateau Fractures
Anatomy and Pathophysiology: The proximal end of the tibia is expanded into the medial and lateral condyles, the former having the greater surface of the two. Together they make up approximately three quarters of the proximal tibial surface, and their integrity is important for normal knee alignment, stability, and motion. The plateau normally slopes 10 degrees from anterior to posterior; on a straight AP view, the anterior and posterior portions of the plateau may not appear to be at the same level. In addition, the lateral plateau is slightly convex upward, whereas the medial is slightly concave upward.
Tibial plateau fractures encompass many differing degrees of articular depression and displacement. Because the initial injury mechanism usually is a valgus stress with an abduction force on the leg, 55 to 70% of condylar fractures involve the lateral plateau. Medial plateau fractures typically result from adduction forces on the distal leg and account for 10 to 23% of these fractures; both plateaus are involved in 11 to 31% of cases.32 If the knee is extended at the time of injury, the fracture tends to be anterior. Posterior condylar fractures usually occur when the knee is flexed at the time of impact.
The Segond fracture represents a bone avulsion of the lateral tibial plateau (Fig. 57-5). The avulsion occurs at the site of attachment of the lateral capsular ligament. On radiographs, an oval-shaped fragment can be seen adjacent to the lateral tibial plateau, which can be confused with an avulsion from the adjacent fibular styloid. Segond fractures are usually accompanied by ACL disruption and anterolateral rotatory instability. Most Segond fractures are caused by sports injuries, and the mechanism is almost always knee flexion with excessive internal rotation and varus stress.
Clinical Features: Knee fractures cause pain, tenderness, ecchymosis, soft tissue swelling, and hemarthrosis when intra-articular. A valgus or varus limb deformity may be present and usually indicates a depressed fracture or concomitant leg fracture. The most important aspect of the initial examination is assessment of neurovascular status. Many tibial plateau fractures cause vascular complications. The popliteal artery is immobile in this region and branches into the anterior and posterior tibial arteries at the upper edge of the interosseous membrane. The popliteal artery may be injured by fragments from bicondylar or comminuted fractures involving the subcondylar area. Vascular impairment may result in distal circulatory compromise. Displaced fractures of the lateral condyle may produce peroneal nerve paralysis in addition to injury to the anterior tibial artery. Stretch of the peroneal nerve is the usual cause of injury.
Soft tissue injuries also may involve the capsuloligamentous structures of the knee. Ligamentous injuries accompany tibial plateau fractures in up to 66% of cases, most often involving the ACL and MCL.34
Cruciate ligament injuries associated with tibial plateau fractures are associated with an increased incidence of late traumatic arthritis and a poor prognosis. Regardless of the type of treatment, operative or nonoperative, tibial plateau fractures with significant residual laxity fare poorly in comparison with stable fractures.35
Fractures of the tibial plateau generally carry a good prognosis, with good to excellent results reported in 90% of patients more than 20 years after injury; however, high-energy tibial plateau fractures generally are associated with a more guarded prognosis.36 In high-energy fractures, a large degree of articular depression, multiple displaced condylar fracture lines, and diaphyseal-metaphyseal extension and comminution in association with open injuries or an extensive internal degloving injury are poor prognostic signs.37
Diagnostic Strategies: Lipohemarthrosis, seen as a fat-fluid level on a plain film, suggests an occult fracture and is caused by entry of marrow fat into the joint space (see Fig. 57-3).38 Lipohemarthrosis also is detected when fat globules are found on aspiration of a hemarthrosis. All knee radiographs should be examined closely for bone avulsion fragments from the fibular head, femoral condyles, and intercondylar eminence, because these may indicate ligamentous injury. Widened joint spaces associated with a fracture of the opposite condyle also may indicate concomitant ligamentous injury.
CT and particularly MRI are more sensitive than plain radiography, help localize occult lesions, and help quantify the amount of depression in displaced fractures and the extent of articular surface involvement in comminuted fractures.34 These studies need not be undertaken emergently, because the knee can be immobilized pending orthopedic consultation.
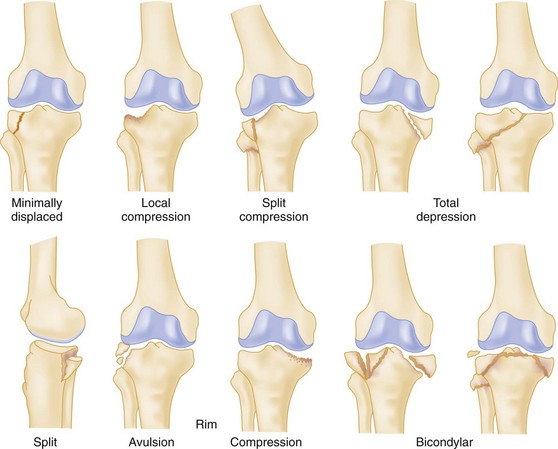
Several classification systems have been proposed. Most such systems depend on the mechanism of injury (i.e., the location and force with which the femoral condyle is driven into the plateau). The revised Hohl classification is in common although not universal use.32 As shown in Figure 57-6, this system divides the plateau fractures into two categories: minimally displaced (less than 4 mm of depression or displacement) and displaced. Displaced fractures are subdivided into six distinct types: local compression, split compression, total depression, splint, rim, and bicondylar.
Management: All patients with a tibial plateau fracture should be referred for evaluation by an orthopedist. In the acute phase, the fracture should be immobilized in a noncircumferential splint and the patient should not bear weight on the limb until seen by an orthopedist. The therapeutic goals include precise reconstruction of the articular surfaces, stable fragment fixation, and early knee motion to prevent stiffness. Weightbearing generally is delayed until healing is complete, usually 6 to 8 weeks. Stable nondisplaced fractures may be treated with immobilization alone, but instability or significant depression or disruption of the joint surface will necessitate surgical management.32
Fractures of the Intercondylar Eminence (Tibial Spine)
Anatomy and Pathophysiology: The intercondylar eminence, or tibial spine, is the central portion of the proximal tibial surface. The spine has two prominences: the medial and the lateral tubercle. The medial tubercle is larger and located more anteriorly than the lateral tubercle. Two intercondylar fossae are present on the proximal tibial surface, one anterior to the intercondylar eminence and one posterior to it. The ACL and the anterior horns of the medial and the lateral menisci attach in the anterior intercondylar fossa. The PCL and the posterior horns of the menisci attach in the posterior intercondylar fossa.
Tibial spine fractures are commonly seen in children and adolescents, but a study suggests that these fractures occur more frequently in adults than was previously thought.39 The injury is more common in children than in adults because the ligaments are stronger than the adjacent physeal plates in the immature skeleton. A fracture of the anterior tibial spine in children usually is associated with an ACL rupture, as is the case in adults.
Clinical Features: After tibial spine fracture the patient reports pain and swelling of the knee and may be unable to bear weight on the affected extremity. Examination confirms acute hemarthrosis and may reveal a block to full knee extension. Tense effusion may limit range of motion, hinder physical examination, and mask ligament disruption. Definite ACL laxity is associated with this injury, and patients may exhibit an anterior drawer sign, a positive result on Lachman’s test, or other signs of ligamentous laxity. In the presence of open physes, tibial spine fractures usually are isolated injuries. Adults are more likely to have an associated tear of the MCL, or intra-articular fracture, which portends a worse prognosis.39
Diagnostic Strategies: Radiographic evaluation should include standard AP and lateral views, and a tunnel view provides a clearer look at the intercondylar area and may reveal the diagnosis. Joint margins should be examined closely for evidence of collateral ligament or capsular bone avulsions. CT sometimes is required to show the location and displacement of the fracture. The fabella, present in some patients, is a sesamoid bone located in the lateral head of the gastrocnemius muscle and should not be mistaken for an intra-articular loose body or fracture fragment.
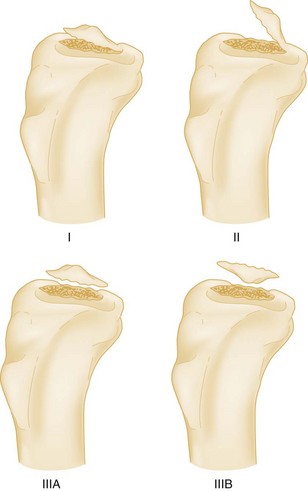
The classification of tibial spine fractures is based on the degree of displacement (Fig. 57-7). Type I involves incomplete avulsion of the tibial spine without displacement. In type II, an incomplete avulsion is associated with minimal displacement of the anterior third of the fracture fragment, but the posterior portion remains adherent. Type III is characterized by complete separation of the fragment from its fracture bed and has a higher associated rate of collateral ligament injuries and peripheral meniscal tears. Type III may be subdivided into type IIIA, fractures with complete displacement, and type IIIB, fractures with displacement and rotation (see Fig. 57-7).
Management: Conservative treatment is effective for all type I injuries. Nondisplaced or incomplete tibial spine fractures generally heal well when treated with cast immobilization in full extension for approximately 6 weeks. Type I and II fractures may require arthroscopy for lavage and accurate classification. If satisfactory closed reduction cannot be obtained or there is associated ligamentous injury, open or arthroscopic reduction and internal fixation should be performed. For restoration of normal function of the ACL, displaced or rotated fragments must be reduced. Type III fractures usually require arthroscopic or open reduction; screws and tension band wiring techniques have yielded excellent results.32 With most uncomplicated fractures of the tibial spine, a good result can be expected when the fracture heals and restores function to the avulsed ACL. A poor outcome, with residual pain and instability, may be associated with additional intra-articular fractures and damage to the MCL.
Epiphyseal Fractures
Anatomy and Pathophysiology: The physes, which are present at the end of the long bones, are primarily responsible for longitudinal growth through the process of endochondral ossification. From birth to skeletal maturity, the distal femoral growth plate contributes 70% of the growth of the femur and 37% of the growth of the lower extremity.40 Likewise, the upper tibial epiphysis accounts for most of the long growth of the tibia.
Biomechanical data and clinical studies in children and adolescents have confirmed that the ligaments and articular capsule are stronger than the bone and epiphyseal plate.41 As a result, trauma to this region of the maturing skeleton usually injures the cartilaginous epiphyseal plate. In this way, the physis protects the joint surface from the grossly comminuted fractures seen in adults.
Despite data showing that the physis is the weakest link in the immature skeletal unit, only 15 to 20% of all fractures in children occur through the growth plate.42
The proximal tibial physis is far more resistant than other physes as a result of the unique anatomic features of this site.40 The proximal tibial physis has no significant attachments to the collateral ligaments of the knee. The LCL inserts into the head of the fibula and has no tibial attachment, and the MCL has only a minor attachment to the epiphysis. The major portion of this ligament is attached to the tibial shaft well below the epiphysis. Varus or valgus stress is more likely to injure the distal femoral physis or the tibial metaphysis. Fracture-separation of the distal femoral growth plate and proximal tibial epiphysis most often is caused by an indirect mechanism, commonly related to sports injuries.40 The Salter-Harris classification of epiphyseal injuries is described in Chapter 49.
Clinical Features: Epiphyseal injuries should be suspected in a child or adolescent who has juxta-articular (growth plate) tenderness, limps, or refuses to or cannot bear weight. The degree of discomfort varies, but the pain often is severe. Depending on the mechanism of injury, the overlying soft tissue may be abraded or lacerated. Swelling is usual in the overlying soft tissue, and an effusion may be present. If the separation is displaced, an angular deformity may be noted.
Epiphyseal growth plate fractures in the lower extremity carry a high incidence of associated injury. Physeal fractures in the region of the knee may be associated with ligament injuries, especially to the ACL and MCL, in one half of the patients. The most serious injury associated with a proximal tibial physis fracture is neurovascular trauma. In particular, popliteal artery injuries have been associated with these fractures, especially when posterolateral or posteromedial displacement is a feature. Peroneal nerve injury also has been reported and may range in severity from neurapraxia to complete disruption.40
Diagnostic Strategies: Plain radiography remains the primary means for evaluating epiphyseal injuries. Diagnosis is based on epiphyseal displacement, widening of the physis, and obliteration or haziness of the normal sharply defined, fine, sclerotic opposing margins of the metaphysis and epiphysis. The latter may result from angulation at one or both sites. Oblique views may be required to show nondisplaced fractures of the epiphysis. CT or MRI can evaluate more fully or classify injuries that already are established on the basis of plain radiography; in the acute setting, CT is more readily available.
Management: The most common complication of fractures through the proximal tibial physis is growth disturbance.41 When growth arrest occurs (approximately 1% of cases), it usually is partial and results from formation of a bridge of bone from the metaphysis to the epiphysis, crossing the growth plate. Although shortening or deformity is less well tolerated in the lower extremity because of weightbearing, many of the growth disturbances do not prove to be clinically significant because of the ability of the immature skeleton to remodel; few such cases are reported to be of sufficient severity to interfere with function.
If a child has juxta-articular tenderness with negative radiographic findings, a growth plate injury (Salter-Harris type I) should be assumed. If it is difficult to determine whether a line on the radiograph is an epiphyseal line or fracture, a comparison view of the contralateral limb should be obtained. Because growth centers ossify at different times, this technique of comparing the uninvolved limb is often of great assistance in confirming a suspected physeal injury. In such cases, when a physeal injury is suspected, the extremity should be immobilized for approximately 2 weeks and reevaluated with at least a plain film, looking for periosteal new bone or physeal thickening. In general, emergency management of most epiphyseal fractures of the distal femur or proximal tibia includes ice, elevation, and immobilization with a long leg posterior splint, with early orthopedic consultation. Anatomic reduction is desirable for displaced fractures of the distal femur and proximal tibial epiphysis. Open reduction usually is required only for patients in whom closed reduction fails.43
Late complications include angular deformity, leg length discrepancy, stiffness, quadriceps atrophy, and persistent instability of the knee. Delayed union or nonunion is almost never a problem except in patients with an underlying neuropathy.32 Because growth inhibition may follow even nondisplaced physeal fractures, long-term orthopedic follow-up care is advisable.
Bone Bruise
Bone bruise is a radiographic diagnosis, involving areas of cancellous bone with high signal intensity on MRI fat suppression sequences. Bone bruise may be present in approximately one half of acutely injured knees.44 A high proportion of patients with a bone bruise have significant soft tissue injury. Nearly all bone bruises resolve after 1 year.44
Osteochondritis Dissecans
Osteochondritis dissecans is a rare orthopedic disorder of unknown cause (Fig. 57-8). The disorder is found mainly in adolescents and results in partial or total separation of a segment of articular cartilage and subchondral bone from the underlying bone. It is commonly unilateral, involving the non–weight-bearing lateral aspect of the medial femoral condyle, and is thought to be related to acute or chronic trauma. Occasionally the lateral femoral condyle or inferior patella pole is involved. Patients often have pain, swelling, and giving-way episodes without a history of trauma. Localized tenderness of the condyle often is the only physical finding. Routine radiographic views usually are diagnostic; a subcortical lucency (see Fig. 57-8) can be appreciated, and an osteochondral fragment may be seen separated from the underlying bone. MRI or CT may aid in determining the exact location and extent of the osteochondrotic lesion. ED patients with suspected osteochondritis dissecans should not bear weight until seen by an orthopedist.
The management of these patients is based on the stability of the osteochondral fragment and the maturity of the skeleton.45 If the epiphyses are open, conservative treatment with protective weightbearing usually results in healing of the lesion. When the epiphyses are closed, the prognosis for healing is guarded. If the fragments are detached, the loose fragments require surgery for removal or fixation. Protected range of motion with non–weight-bearing activity for 6 to 10 weeks generally is advised.
Osteonecrosis
Osteonecrosis occurs when disruption of the blood supply to the bone causes infarction. The knee is a common site of involvement, particularly the weight-bearing surface of the medial femoral condyle.46 Spontaneous osteonecrosis usually affects middle-aged and elderly patients, whereas secondary osteonecrosis may occur in younger patients related to corticosteroid therapy or in association with sickle cell disease, lupus, or renal transplantation, among many other risk factors.46 The exact cause is unknown. A common clinical presentation is spontaneous onset of severe localized knee pain that may be accompanied by an effusion and loss of joint motion. The physical examination reveals point tenderness over the involved femoral condyle or tibial compartment. Radiographs obtained at the onset of symptoms usually are normal in appearance, and the diagnosis is confirmed with technetium bone scanning, which shows increased activity. MRI also is diagnostic of acute osteonecrosis. Subchondral marrow signal abnormality is the earliest change noted; subchondral collapse and fracture may be seen in more advanced cases.47
Initially, most patients can be managed with conservative treatment consisting of rest, protected weightbearing, and nonsteroidal anti-inflammatory drugs (NSAIDs). The outcome depends on the percentage of the weight-bearing surface involved with the process. If the lesion is small, no surgical treatment is required. Over the long term, degenerative changes will develop in most patients, but initially the changes are not severe. For more advanced stages of femoral osteonecrosis, various surgical treatments have been proposed, including arthroscopic débridement, proximal tibial osteotomy, prosthetic replacement, and allografting.46
Extensor Mechanism Injuries
Anatomy and Pathophysiology: The extensor mechanism consists of the quadriceps muscles, quadriceps tendon, medial and lateral retinacula, patella, patellar tendon, and tibial tubercle (Fig. 57-9). Passive and dynamic stabilization of the patella are aided by the surrounding soft tissue. Although this anatomic complex encompasses the most superficial aspect of the knee, ruptures of the extensor mechanism are infrequent injuries relative to other types of injuries of the knee joint. Disruptions of the extensor mechanism may occur at any level from the quadriceps muscle to the insertion on the tibial tubercle. Injury generally occurs as a result of sudden vigorous contraction of the quadriceps muscle with the knee in a flexed position, laceration, or a direct blow. Rupture of the quadriceps tendon usually occurs at or just proximal to the patellar insertion. Occasionally the rupture may extend into the vastus intermedius tendon or transversely into the retinaculum. Most patellar tendon ruptures occur at the site of origin on the inferior pole of the patella.
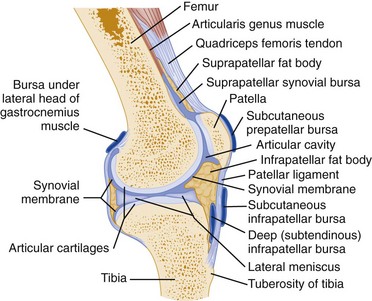
Figure 57-9 Parasagittal section (lateral to midline) of the knee showing extensor mechanisms and relevant structures.
Chronic systemic conditions, including rheumatoid arthritis, gout, systemic lupus erythematosus, hyperparathyroidism, and iatrogenic immunosuppression in organ transplant recipients, may render the tendon vulnerable to rupture.48 Several studies have implicated use of steroids or fluoroquinolones in tendon rupture.49 In children, quadriceps and patellar tendon ruptures are rare, and muscle tears seem to predominate. In adolescents, patellofemoral dysplasia, chronic tendinitis, and the use of steroids are predisposing factors. Dysplasia may cause extensor mechanism injury by repetitive tensile overloading, and corticosteroids seem to weaken collagen ultrastructure and impair the reparative process.
Clinical Features: Clinical evaluation can elicit the correct diagnosis in most cases of complete disruption of the extensor mechanism.50 Patients with extensor disruption may have the following signs and symptoms: (1) acute onset of pain, swelling, and ecchymoses over the anterior aspect of the knee and a palpable defect in the patella, quadriceps tendon, or patella tendon; (2) loss or limitation of ability for active leg extension (extension lag usually is seen when extension for the last 10 degrees is performed haltingly or with difficulty); (3) high-riding patella (patella alta) with patellar tendon rupture and superior retraction; and (4) low-riding patella (patella baja) with quadriceps tendon rupture and inferior retraction. Partial disruptions may be difficult to diagnose on clinical examination and may require MRI for confirmation.
Diagnostic Strategies: Standard AP and lateral radiographs should be obtained and may reveal characteristic findings, possibly including obliteration of the quadriceps or patella tendon, a poorly defined suprapatellar or infrapatellar soft tissue mass, soft tissue calcific densities, or a displaced patella (Fig. 57-10). Patella alta may be sought on the lateral radiograph with use of a ratio of patellar length to patellar tendon length (the Insall-Salvati ratio). If this ratio is less than 0.8, patella alta is present.51,52 The degree of flexion should not affect this ratio, which relies on the inelasticity of the patellar tendon. In patients with quadriceps rupture, degenerative spurring of the patella (tooth sign) commonly is seen on tangential views. Obliteration of the extensor tendons may be caused by a frayed tendon and surrounding hematoma. A soft tissue mass represents proximal or distal retraction of the torn tendon. Calcific densities may represent avulsed bone fragments of the patella or tibial tubercle or dystrophic calcifications in the substance of the tendons. Despite these multiple radiographic signs, the correct diagnosis is infrequently made by plain radiography in cases of incomplete quadriceps tendon rupture. MRI shows the entire extensor mechanism and is the best imaging modality for diagnosing pathology in this system, even in the acute phase. MRI usually is reserved for patients with possible incomplete disruption or for those with a complication of intra-articular derangements.
Management: Treatment of acute extensor mechanism injuries produces a much better clinical outcome if instituted early, within 2 to 6 weeks of the initial injury. Accurate diagnosis at the time of injury is essential. Patients with delayed diagnosis of patellar tendon rupture may experience significant retraction of the patella proximally and subsequent development of quadriceps contractures or adhesions. If the tear is only partial, immobilization with the knee in full extension for 4 to 6 weeks is the treatment of choice.53 Surgical intervention is required for reattachment of complete tendon ruptures, and repair should be performed as soon as possible after injury for the best results to be achieved. Numerous techniques have been described for early and late repairs, and the choice of procedure depends on several factors, including location of the tear, lag time between injury and repair, and presence or absence of adhesions. After primary repair, the knee is immobilized in full extension with a long leg cast until healing is complete. Gradually progressive active and passive range-of-motion exercises are indicated for optimal results.
Patellar Fractures
Anatomy and Pathophysiology: The patella is the largest sesamoid bone in the body. It is held in place by the quadriceps tendon, the patellar ligament, and the medial and lateral retinacula. As an integral part of the extensor mechanism, the patella increases the effective lever arm of the quadriceps by providing anterior displacement of the quadriceps tendon.2 All fractures of the patella, except for small avulsion fractures of the rim, are intra-articular.
Patellar fractures constitute approximately 1% of all skeletal injuries and occur in all age groups.54 Patellar fractures are classified as transverse, stellate, or comminuted; longitudinal or marginal; proximal pole or distal pole; and rarely osteochondral. They may be either displaced or nondisplaced and occur either from direct or indirect forces or from dislocation. The most common fracture pattern is the transverse fracture (accounting for 50-80% of cases).54 This type often is seen in young adults and usually results from a powerful contractile force transmitted from the quadriceps tendon. This force may pull the superior portion of the patella upward, leading to wide displacement. In such cases the medial and lateral retinacula are usually disrupted, resulting in significant functional disability; active extension is impossible. Nondisplaced transverse patellar fractures usually are caused by a direct blow to the anterior aspect of the patella (e.g., a fall on the knee or a direct blow sustained in vehicular trauma). The retinaculum and extensor mechanism usually remain intact, and the patient retains limited functional ability for active extension. Stellate and comminuted fractures account for 30 to 35% of all patellar fractures and commonly result from a direct impact.54 The fracture elements often appear as separated fragments on plain radiographs, but they are held in place and supported by the medial and lateral retinacula and the overlying soft tissues. Small proximal fragments are at risk for avascular necrosis because the patellar blood supply is central and inferior. Longitudinal or marginal vertical patellar fractures are less common, usually are the result of direct injury, and involve the lateral facet.
Clinical Features: On physical examination, tenderness, swelling, and ecchymosis over the patella and prepatellar bursa are noted. Active extension may be limited or absent, depending on the fracture pattern and amount of fragment displacement. Associated injuries may include fractures of the femoral neck, dislocation of the hip, and acetabulum fractures.
Diagnostic Strategies: Radiologic evaluation of patellar fractures should include standard AP, lateral, and sunrise views. Most patellar fractures are obvious on plain radiographs, but vertical marginal fractures may be difficult to identify; they are obscured by the femur on the AP view and not seen at all on the lateral view.53,54 Close examination of sunrise (or equivalent) views may reveal an osteochondral avulsion fragment or marginal fracture (Fig. 57-11). Bipartite and multipartite patellae are common normal variants and should not be confused with fractures. Ossification centers are found at the upper outer quadrant of the patella and have smooth cortical margins, but differentiating physeal lines from fractures can be difficult. Comparison radiographs may be helpful because these anatomic anomalies often are bilateral. In some cases, MRI or arthroscopy may be needed to identify occult marginal fractures or free osteochondral fragments.
Management: If the patient can actively extend the knee without displacing the fracture, the retinaculum is intact, and the fracture may be treated nonoperatively. Nondisplaced patellar fractures usually are treated with a long leg cast for 4 to 6 weeks, with uniformly good results. Casting the knee in full extension relieves the patella of almost all stress during the healing period. For initial management, a knee immobilizer may be used. Patients should be instructed to use crutches, with partial weightbearing as tolerated, and should be referred for orthopedic or primary care follow-up.
Fracture fragment separation and dehiscence of the fracture repair are uncommon. They generally result from inadequate internal fixation or, in some cases, an inadequate period of immobilization. Avascular necrosis is rare. Range of motion generally is good after all procedures. Persistent patellofemoral pain and osteoarthritic symptoms are reported as late sequelae of patellar fractures in 56% of patients.54
Patellar Dislocation
Anatomy and Pathophysiology: Traumatic patellar dislocation is a relatively common knee injury and can lead to recurrent patellar subluxation and dislocation. It is more common in children than in adults. Most cases are lateral, and the mechanism of injury usually is a direct blow to the anterior or medial surface of the patella. It may occur from an athletic injury caused by a valgus stress combined with flexion and external rotation. In nearly all cases, disruption or sprain in the medial patellar retinaculum results from stretching of this structure as the patella subluxates laterally; subluxation usually indicates a stretched medial retinaculum, and dislocation suggests a tear. Although extra-articular patella dislocations are common, intra-articular dislocations are rare occurrences that are considered in any patient with a locked knee.
The quadriceps angle (Q angle) is measured with the quadriceps contracted. The angle is formed by lines drawn on an AP radiograph from the tibial tubercle to the center of the patella and from the center of the patella to the anterior superior iliac spine. Normally, this angle is 10 degrees or less in men; it may be 15 degrees in women. A Q angle exceeding these dimensions may predispose the patient to patellofemoral problems.55
Clinical Features: Patients with lateral patellar dislocation may complain of the knee giving out, accompanied by pain and swelling. Inability to bear weight and inability to flex the knee are common complaints. There may be a history of previous dislocation. Examination reveals a defect anteriorly with the patella deviated laterally. Tenderness along the medial joint line usually can be elicited by palpation, and an effusion may be present. Acute hemarthrosis is seen most commonly if there is an associated osteochondral fracture. Osteochondral fractures typically occur on the articular surface of the patella and may involve only cartilage (chondral fractures) or include a piece of underlying cortical bone. Patellar dislocations may reduce spontaneously, or the patient may self-reduce the dislocation, usually followed by formation of a large effusion.
Diagnostic Strategies: Standard AP and lateral radiographic views generally are adequate for diagnosis. Obtaining a sunrise (skyline) view usually is not possible because of pain and inability to flex the knee. Radiographic findings include lateral deviation of the patella out of the trochlear groove, usually with an effusion. Radiographs should be examined for evidence of avulsion fractures.
Management: After dislocation is diagnosed, closed reduction should be attempted. Force or pressure should be directed anteromedially on the lateral patellar margin while gentle extension of the leg is attempted simultaneously. Uncommonly, patellar reduction may be difficult. Closed reduction can be achieved by applying downward pressure to the lateral aspect of the patella, creating an external rotational force that unlocks the medial patellar facet.56 Postreduction radiographs are recommended and should reveal the patella in the trochlear grove. Osteochondral avulsion fragments may be visualized radiographically, and postreduction radiographs should be examined carefully for their presence. Radiologically evident intra-articular loose bodies may require arthroscopic removal.
After successful reduction, the knee should be immobilized in full extension for 3 to 6 weeks to allow adequate time for the medial retinaculum to heal. Ice, elevation, non–weight-bearing status, and analgesia provide additional benefit in the acute setting. The patient can be discharged with referral for orthopedic or primary care follow-up within 2 weeks. Although the incidence of recurrence may be decreased with appropriate therapy and proper patient selection, up to 44% will experience a recurrent dislocation, and more than one half of all patients with a primary patellar dislocation will continue to have symptoms of instability or anterior knee pain.57 Patellar dislocations often recur and sometimes require surgery, involving arthroscopic release of the lateral retinaculum.
Soft Tissue Injuries
Cruciate Ligament Injuries: The cruciate ligaments are the primary stabilizers for anterior and posterior displacement of the tibia on the femur. They are so named (Latin crus means “cross”) because they cross each other between their attachments. The ACL extends obliquely upward, medially, and backward from the anterior intercondylar area of the tibia to the medial aspect of the lateral femoral condyle. The ACL prevents excessive anterior displacement of the tibia on the femur and helps control rotation and hyperextension of the knee during cutting, twisting, and turning activities. It is the most commonly injured major ligament of the knee, with more than 100,000 new ACL tears occurring in the United States annually.58 The PCL passes upward, laterally, and forward medial to the ACL from the posterior intercondylar area of the tibia to the lateral aspect of the medial condyle of the femur. The PCL prevents excessive posterior displacement of the tibia on the femur, especially during flexion. The PCL is extremely strong, and injuries are relatively uncommon. Cruciate ligament injury is uncommon in children with open physes.
PCL injuries are comparatively rare. Mechanisms include a fall onto the ground with the foot plantar-flexed (striking the tibial tubercle), a direct posterior blow to a flexed knee (e.g., a dashboard injury), hyperflexion, hyperextension, severe varus or valgus loads after failure of the collaterals, and knee dislocations. Nearly all PCL injuries are associated with other ligament injuries, including concurrent injuries of the MCL, ACL, or posterolateral complex.58,59 PCL injuries are classified as partial (grade I or II) or complete (grade III) tears. Pain and swelling are common complaints with isolated PCL tears and with PCL tears having combined capsuloligamentous disruption. Popping or tearing sensations are infrequently noted, and instability usually is not immediately appreciated. Later, the patient may complain of feeling the femur “fall off” the tibia. The posterior drawer test (see earlier) is commonly done to assess the integrity of the PCL.
Clinical evaluation is moderately sensitive for ACL tears and other intra-articular injuries, with sensitivity for ACL injury ranging from 62 to 100% and 64 to 82% for meniscus injury.60 The lesions most difficult to diagnose are chondral fractures, tears in the ACL, loose bodies, and fibrotic fat pads.
Collateral Ligament Injuries: The medial stabilizers of the knee are the joint capsule and the MCL. The semimembranosus and pes anserinus are medial dynamic stabilizers. These structures resist valgus laxity and medial rotary instability. The MCL is a two-part structure with both a long superficial and a deep capsular component; the latter attaches to the medial meniscus and acts as a stabilizer for this structure. The MCL usually is injured by a direct blow or impact to the lateral aspect of the knee, which imposes a valgus stress. MCL injury is the most common isolated knee ligament injury, and it is the injury most commonly associated with ACL injury. MCL injury usually does not require surgical treatment.
Diagnostic Strategies.: Plain radiography may be used before stress testing in cases of suspected ligamentous injury to rule out the possibility of an associated fracture. Although patients with isolated collateral ligament strain rarely show acute osseous pathology, the yield increases in cases with radiographic evidence of traumatic effusion and in cases in which cruciate ligament injury is suspected. The initial radiographic evaluation should include AP, lateral, intercondylar notch, and sunrise views. Each radiograph should be evaluated for possible osteochondral injuries, loose bodies, or avulsion injuries at the attachment sites of ligaments. The lateral capsular sign, associated with the Segond fracture (see Fig. 57-5) and fracture of the posterior aspect of the lateral tibial plateau, commonly is associated with ACL tear.
Management.: Isolated collateral ligament injuries of all grades usually are managed nonoperatively, provided that the ACL is intact. The nonoperative approach should focus on controlling pain, restoring range of motion, regaining muscle strength, and protecting the knee from further injury. Appropriate initial therapy includes ice, NSAIDs, and immobilization if needed to control pain. Patients may be placed on a regimen of partial weight-bearing or non–weight-bearing status with use of crutches. Orthopedic or primary care follow-up is advised, and a rehabilitative exercise program for quadriceps and hamstring strengthening may be instituted when the acute injury has resolved.
Anatomy and Pathophysiology.: The medial and lateral menisci are crescent-shaped fibrocartilaginous cushions that sit on the superior articular surface of the tibia and provide a gliding surface for the femoral condyles. They function as shock absorbers and aid in the distribution of stress across the joint surface by providing a larger area of contact. They also act as secondary stabilizers by deepening the tibial plateau. Normal tibiofemoral articulation and function depend on meniscal integrity; damage or loss leads to osteoarthritis. The medial meniscus is firmly attached anteriorly and posteriorly to the joint capsule. The lateral meniscus is less firmly attached to the capsule and more mobile. The menisci move slightly forward with extension and backward with flexion. Because of its greater mobility, the lateral meniscus is less vulnerable to injury. The meniscus is avascular except at the peripheral third, which has the greatest potential to heal after injury.
Clinical Features.: Meniscal injuries are unusual in children but become increasingly more common in adolescents and adults. An isolated meniscal tear should be suspected in a patient with a history of intermittent locking, effusion, giving way, and pain and physical examination findings of joint line tenderness and a positive result on McMurray’s test. Cruciate tears invariably result in immediate hemarthrosis; meniscal tears usually result in development of an effusion over 12 to 24 hours. A second, more common presentation is that of a patient with an unstable knee who has chronic ACL insufficiency and similar history and physical examination findings.
Diagnostic Strategies.: Diagnosis of acute meniscal injury is difficult, and more so in the presence of any acute knee injury, especially ACL tear.60 Meniscal injury cannot be diagnosed by plain radiography or CT scanning. Arthroscopy is the gold standard for diagnosis, and MRI is an alternative but may miss some meniscal tears.
Management.: Definitive treatment of a meniscal injury is not urgent. Unless the knee is locked and cannot be extended or flexed, a patient with a meniscal tear should be managed with analgesics, immobilization, ice, non–weight-bearing status, and referral for orthopedic or primary care follow-up. The locked knee requires acute orthopedic consultation if a knee immobilizer cannot be applied. Surgery is reserved for cases with persistent symptoms that limit activity. Surgery involves arthroscopic exploration. The torn meniscal fragment is reattached if it is well vascularized; otherwise, it is resected.
Overuse Syndromes
Anatomy and Pathophysiology.: The patellofemoral pain syndrome refers to the clinical presentation of anterior knee pain related to changes in the patellofemoral articulation. Chondromalacia patellae describes softening of the articular cartilage. Correlating pathologic changes on the surface of the patella and clinical symptoms has been difficult, and the pain mechanism has not been precisely defined.
Clinical Features.: As noted, the patellofemoral pain syndrome is the most common cause of knee pain. Affected patients generally are 10 to 20 years of age and often have difficulty describing their symptoms clearly. The pain usually begins gradually and commonly is not related to trauma. One knee usually is more affected than the other. The knee is more painful with prolonged flexion (e.g., from sitting in a movie theater), and the discomfort typically is accentuated by stair climbing and kneeling. The patient may have instability related to patellar subluxation or dislocation. The syndrome occurs both in athletes and in elderly patients who have arthritis affecting the patellofemoral joint. Considerations in the differential diagnosis include tears of the menisci, plica syndrome, inflammatory or degenerative arthritis, ligament injuries, and overuse syndromes (e.g., prepatellar bursitis, patella tendinitis).
Diagnostic Strategies.: Plain films are typically normal, and more advanced studies should be undertaken only if other diagnoses are being considered.
Management.: Most patients, regardless of the cause of their condition, respond to a rehabilitation program. Conservative treatment for patellofemoral pain usually is effective, with most patients responding to one or more of four types of treatment: (1) exercises to strengthen the quadriceps, (2) brace support of the patellofemoral mechanism, (3) activity modification limiting flexion, and (4) medications such as NSAIDs for pain. The initial goal is to reduce pain and improve function, with emphasis placed on strengthening the vastus medialis oblique muscle. The patient should receive appropriate referral to ensure that an optimal rehabilitative scheme is designed.
Iliotibial Band Syndrome: The IT band is a strip of fascia lata that extends from the iliac crest to the lateral tibial tubercle. It connects the lateral femoral condyle and the lateral tibia and stabilizes the knee joint in extension. Irritation from overuse can cause inflammation of a bursa underlying the IT band at the lateral femoral epicondyle, resulting in lateral knee pain. The syndrome is most common in distance runners and is more likely in hyperpronators. Physical findings include localized tenderness of the lateral femoral epicondyle and IT tightness or pain, elicited by Ober’s or a related test.61 In Ober’s test the patient lies on the side with the unaffected leg down, flexed to 90 degrees at the hip and knee. The affected hip is abducted, the knee is extended, then the hip is allowed to return to neutral adduction with gravity. Failure of the hip to adduct fully with gravity or reproduction of pain at the lateral knee indicates IT tightness or inflammation, respectively. Radiographs are normal in appearance. Considerations in the differential diagnosis include early degenerative joint disease, cystic or torn lateral meniscus, lateral capsular strain, lateral tibial or femoral condyle osteonecrosis, stress reactions, chondromalacia, and popliteus tendinitis. Treatment involves rest, ice, and NSAIDs during the acute phase, followed by an IT band stretching regimen, improved footwear and orthotics when indicated, and gradual return to previous levels of activity. Steroid injections are helpful for refractory cases, and surgical release is uncommonly required.
Peripatellar Tendinitis: Peripatellar tendinitis, or jumper’s knee, refers to a spectrum of patellar tendon and extensor mechanism abnormalities that result from chronic repetitive stress from jumping, running, or cutting. Microscopic tears occur in the tendon. Treatment involves NSAIDs, rest, and activity modification. Local steroid injections are not recommended. For highly competitive athletes and patients in whom conservative treatment fails to effect improvement, surgery with débridement of abnormal tissue may be performed.
Plica Syndrome: Plicae, or redundant folds of synovium, are normal embryologic structures that persist in the adult knee. Repetitive bouts of synovitis within the plica may result in a tight inelastic band that interferes with knee motion. Patients typically complain of pain over the region of the medial femoral condyle brought on by activity but also occurring after sitting for prolonged periods. A snapping sensation is another commonly reported symptom as the plica sweeps across the femoral condyle. Other nonspecific symptoms include intermittent swelling, locking, weakness, and stiffness. The physical examination often elicits tenderness over the medial femoral condyle but not the medial joint line; the latter finding would be more typical of a medial meniscal lesion. An effusion, crepitus, loss of motion, quadriceps atrophy, and a positive result on McMurray’s test may be noted as well.62
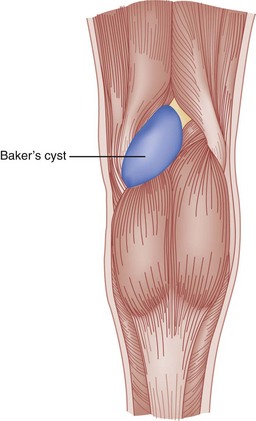
Popliteus Tendinitis: The popliteus is a small, flat muscle that originates on the lateral femoral condyle and inserts on the posteromedial tibia, capsule, and lateral meniscus. It passes beneath the lateral head of the gastrocnemius. Its tendon is surrounded by a bursa that separates it from the fibular collateral ligament, femoral condyle, and capsule. Functionally, it prevents external rotation of the tibia and withdraws the lateral meniscus during flexion to prevent impingement between the femur and the tibia. A third function, along with the quadriceps and PCL, is to stabilize the knee by preventing forward displacement of the femur on the tibia. Popliteal tendinitis usually occurs in athletes and often causes localized pain over the posterior or posterolateral aspect of the knee. Running and walking downhill exacerbate symptoms. Usually there is no history of effusion, locking, or giving way.63
Bursitis: The knee has several bursae, which decrease friction between moving structures. They usually are thin but with repeated stress may become thickened and fluid-filled. The prepatellar bursa is located between the patella and the skin. The superficial infrapatellar bursa is located between the tibial tubercle and the skin. The deep infrapatellar bursa is located between the posterior margin of the distal part of the patellar tendon and the anterior aspect of the tibia. The suprapatellar bursa is not a true bursa but rather is an extension of the tibiofemoral joint capsule. The anserine bursa separates the pes anserinus from the distal portion of the MCL and the medial tibial condyle. As noted previously, pes anserinus means “goose foot” and anserine means “related to the pes anserinus.” The term derives from the fact that the bursa underlies the anserine tendon, a three-forked structure constituting the insertion of the gracilis, sartorius, and semitendinosus muscles.
Baker’s Cyst
Baker’s cyst (popliteal cyst) is a herniation of the synovial membrane through the posterior aspect of the capsule of the knee (Fig. 57-12). It results from an enlarging knee effusion of any cause. A mass is palpable in the posteromedial corner of the knee and often produces pressure, pain, and limitation of range of motion. Rupture of the bursa with resultant escape of fluid into the calf may produce a clinical picture similar to that of deep vein thrombosis or compartment syndrome.64 In this circumstance, ruptured Baker’s cyst is a diagnosis of exclusion (i.e., thrombosis should be ruled out). Treatment is directed at the underlying intra-articular pathology.
Leg
Mechanisms of Injury and Management
Proximal Extra-articular Tibial Fractures
Subcondylar Tibial Fractures: Subcondylar tibial fractures usually are associated with tibial plateau fractures, especially bicondylar fractures. Subcondylar fractures involve the proximal tibial metaphysis and typically are transverse or oblique. The mechanism of injury involves a rotational or angular stress accompanied by vertical compression. Examination reveals tenderness and swelling of the involved area. A hemarthrosis may indicate extension of the fracture into the joint or associated ligamentous injury. Routine radiographic views usually are adequate in showing the fracture line. ED management includes ice and immobilization with a long leg posterior splint. Stable extra-articular nondisplaced transverse fractures usually are treated conservatively with a long leg splint, followed by delayed casting on an outpatient basis (because of the risk of swelling and compartment syndrome). In children, casting (with adequate padding) is sometimes performed acutely. Comminuted fractures or fractures associated with an intra-articular component require open reduction and internal fixation and may be treated in the acute setting.
Anatomy and Pathophysiology.: The tibial tubercle is located at the proximal anterior border of the tibial shaft and is the insertion point of the patellar ligament. The proximal tibial epiphysis and the tibial tuberosity develop from two separate ossification centers that coalesce during adolescence. Epiphyseal ossification terminates in late adolescence.
Avulsion fractures of the tibial tubercle are uncommon. They occur predominantly in adolescent boys.65 The injury typically occurs near the end of growth, when endochondral ossification of the physeal cartilage of the tibial tubercle occurs. Avulsion fractures mainly occur as an indirect injury during activity. The mechanism of injury has been described as a violent flexion of the knee against a tightly contracted quadriceps muscle, which also can cause patellar tendon rupture. The Watson-Jones classification describes three grades of injury depending on the extent of displacement (Fig. 57-13). In type I injuries, the tubercle is hinged upward without displacement from the proximal base. The type II injury has a small portion of the tubercle avulsed, but it is retracted proximally; the articular surface is not involved. Type III fractures are more severe and extend across the articular surface; displacement of the fragment and often comminution are features.
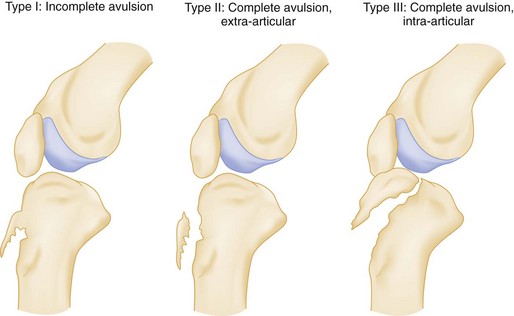
Figure 57-13 Tibial tuberosity fractures.
Clinical Features.: Physical examination reveals acute tenderness and swelling at the anterior aspect of the knee and proximal tibia. Depending on the type of injury, functional disability may range in severity from extensor lag to complete loss of active extension. Hemarthrosis is evident with type III injury because of intra-articular fracture extension across the proximal epiphysis.
Diagnostic Strategies.: Plain radiographs usually are adequate for diagnosis. The lateral view shows the avulsion fracture, number of fragments, and amount of displacement. Swelling of the overlying soft tissue is evident. Comparison views may be necessary when a type I injury is suspected.
Management.: Treatment depends on the degree of displacement and the presence of joint involvement. Nondisplaced type I avulsions are treated with cast immobilization with the knee in extension until healing results. Minimally displaced type II avulsions may be treated similarly if the displacement can be reduced by external manual maneuvers. Displaced type III fractures are treated by open reduction and internal fixation to restore proper biomechanics and joint congruity. Fixation screw and tension band wiring techniques have yielded excellent results. After a period of immobilization and progressive rehabilitation, most patients are able to return to full activity.
Complications of tibial tubercle fractures are rare and include genu recurvatum (backward curvature of the knee), patella alta, meniscal tears, failure of surgical fixation, and subsequent heterotopic ossification and osteonecrosis of the tubercle.66 If the involved growth plates are closing at the time of injury, premature physeal closure can rarely result in a significant recurvatum deformity.
Osgood-Schlatter Disease
Anatomy and Pathophysiology: Adolescents are susceptible to the development of Osgood-Schlatter disease, also known as osteochondritis of the tibial tuberosity or apophysitis of the tibial tuberosity. This common condition results from traction of the distal patellar tendon on the tibial tubercle, causing repetitive microtrauma with subsequent healing of the physis of the tibial tuberosity. This traction apophysitis occurs during the adolescent growth spurt, usually in athletically active children.
Clinical Features: The disease is characterized by painful swelling over the tibial tubercle, which is exacerbated by activity, is relieved by rest, and is usually of several months’ duration. The tubercle may appear abnormally prominent, often on both sides. Pain is elicited on resisted extension of the flexed knee, and occasionally an extensor lag may be noted. Tenderness is most pronounced at the insertion of the patellar tendon. Bilateral involvement is noted in 20 to 30% of patients.67
Diagnostic Strategies: The diagnosis of Osgood-Schlatter disease is based on clinical signs and symptoms. Plain radiography of the knee may be useful to exclude other pathologic entities (e.g., tumors, infection, avulsion fractures) but generally is not required. Radiographs are normal in appearance or reveal pretibial soft tissue edema or prominence of the tubercle, with no other bone abnormalities.
Management: Treatment varies according to the acuteness of the symptoms and the skeletal age of the patient. Initially, rest, ice, and analgesics are the mainstays of therapy. As symptoms subside, a rehabilitation program that stretches and strengthens the quadriceps should be instituted. Knee orthoses are used to damp the pull of the extensor mechanism on the weakened tibial apophysis. Immobilization is reserved for the unreliable patient who will not or cannot comply with the program of relative rest in which aggravating activities are avoided. For children with severe symptoms, immobilization for 2 to 3 weeks may be used. Surgical repair may be required if the conservative treatment fails, but it cannot be implemented until the epiphysis is closed, at which time the problem usually is resolved.
Tibial Shaft Fractures
Anatomy and Pathophysiology: The tibia and fibula are tightly bound to each other by the syndesmotic ligament. This strong band of tissue can transmit energy such that the tibia and fibula may be fractured at nonadjacent sites. The fibula remains intact in only 15 to 25% of tibial shaft fractures. Tibial shaft factures are associated with a high incidence of infection, delayed union, nonunion, and malunion, in part because of the poor soft tissue coverage of the anterior tibia.
Clinical Features: Tibial shaft fractures cause pain, swelling, and localized deformity, usually angulation or rotation of the foot. Determination of vascular integrity is the priority. Distal dorsalis pedis and posterior tibial pulses should be assessed; however, vascular injury is a rare complication of these fractures. Neurologic injury, by contrast, is common, particularly injury of the peroneal nerve. Motor function of the peroneal nerve is checked by testing active ankle and toe dorsiflexion (deep peroneal nerve) and active foot eversion (superficial peroneal nerve). Sensory function of the peroneal nerve is documented by testing sensation in the first dorsal web space in the foot (deep peroneal nerve distribution) and sensation of the dorsal lateral foot (superficial peroneal nerve distribution). Integrity of the posterior tibial nerve is assessed by checking for the presence or absence of plantar sensation. Significant soft tissue damage also may accompany tibial shaft fractures. Compartment syndrome may be a complication of tibial fractures and usually develops within the first 24 to 48 hours.
Diagnostic Strategies: AP and lateral radiographic studies document the fracture, define the fracture pattern, and identify any associated bone loss (Fig. 57-14). The knee and ankle should be included in both views, and radiographs of the pelvis and ipsilateral femur may be required to assess for associated injuries. Postreduction views should be taken after any manipulation of the extremity and should include the knee and ankle joints so that alignment of the proximal and distal joint surfaces can be determined.
Management: The initial management of closed tibial shaft fractures consists of immobilization in a long leg posterior splint applied with the knee in 10 to 20 degrees of flexion. The splinting procedure may require analgesia and sedation. In general, after fractures have been immobilized, pain decreases. If the patient reports continued severe pain after immobilization, a complication such as compartment syndrome, nerve root compression, or limb ischemia should be considered. Circumferential casts generally are avoided in the acute setting because of the risk of compartment syndrome, although some orthopedists will cast pediatric fractures in the acute phase. Initial hospitalization is indicated for most patients with significant tibial shaft fractures to allow adequate pain control and observation for compartment syndrome.
Open fractures should be covered by a sterile dressing. Antistaphylococcal antibiotics (typically cefazolin) should be given, with consideration of agents active against methicillin-resistant S. aureus (MRSA). Gentamicin is added for severely contaminated wounds.68 Tetanus vaccination status should be updated as indicated. A long leg posterior splint should be applied. (This applies to all open fractures.)
In general, tibial fractures are slow to heal. The average time to union is approximately 20 weeks for stable tibial shaft fractures caused by a low-energy mechanism and more than 30 weeks for unstable fractures caused by a high-energy mechanism.69 Delayed union describes fracture segments that have not united after 24 weeks or that show no radiographic evidence of callus formation for 3 consecutive months. Nonunion is a radiographic diagnosis, with a finding of rounded, well-corticated edges of the major fracture fragments. It is much more common in adult long bone fractures than in childhood fractures, which generally heal rapidly. Delayed vascular injuries, including pseudoaneurysm, arteriovenous fistula, and deep vein thrombosis, also may occur as a complication of tibial shaft fractures. Fat embolism also may occur acutely, especially after reamed nailing. Additional late complications include malrotation of the leg, refracture, and reflex sympathetic dystrophy.
Proximal Fibula Fractures
Anatomy and Pathophysiology: Isolated fibular fractures are relatively unimportant because the fibula is a non–weight-bearing bone. The mechanism of injury usually is a direct blow to the lateral aspect of the leg or an indirect varus stress to the knee. An important exception is the Maisonneuve fracture (Fig. 57-15). This injury involves a medial ankle disruption (deltoid ligament tear or medial malleolar fracture), with complete tearing of the syndesmotic ligament joining the tibia and fibula, and fracture of the proximal fibula. Consequently, the fibula floats free relative to the tibia, resulting in an unstable ankle mortise, for which surgical fixation is required. The possibility of this injury indicates the need for examination of the proximal fibula in all medial ankle injuries.
Clinical Features: Isolated fibular shaft fractures cause lateral leg pain that is exacerbated by walking. Local pain, swelling, and tenderness at the fracture site may be elicited, although signs and symptoms can be subtle. A thorough evaluation should be done to exclude serious associated occult neurovascular or ligamentous injuries. The common peroneal nerve courses around the neck of the fibula and may be contused or lacerated at the time of injury. The LCL of the knee may be ruptured or strained in association with the fracture, and anterior tibial artery injury with thrombosis may occur.
Management: Isolated fibular shaft fractures are treated symptomatically with ice, analgesia, and non–weight-bearing status. Immobilization in a long leg cast is rarely done but may provide symptomatic relief beginning 2 days after the acute injury. Weightbearing may be advanced progressively as tolerated; pain should be avoided. Patients with nondisplaced or minimally displaced fractures may have little pain and tolerate crutch walking without casting. In general, isolated fibula shaft fractures can be managed on an outpatient basis and heal without complication.
Proximal Tibiofibular Joint Dislocations
Anatomy and Pathophysiology: The proximal tibiofibular joint is a small synovial joint between a circular or oval facet on the head of the fibula and a similar facet on the inferior aspect of the lateral tibial condyle. The proximal tibiofibular joint is stabilized by the joint capsule and the anterior and posterior tibiofibular ligaments. Dislocation of the proximal tibiofibular joint is rare, occurring most commonly in adolescents and young adults because of its association with motor vehicle collisions and sports injuries.70 Several types of dislocations of the joint have been described; anterolateral dislocation is the most common and usually is caused by a fall on a flexed, abducted leg. Posterior medial dislocation generally is caused by a direct blow to the flexed knee and is more often associated with peroneal nerve injury. Superior dislocation is associated with ankle diastasis and typically occurs simultaneously with an ankle fracture.
Clinical Features: The patient may complain that the knee feels “out of joint,” or if the problem is intermittent, the knee may lock or give way periodically. Physical examination reveals tenderness and swelling over the proximal fibula and tibiofibular joint. In the absence of associated injury, findings on knee examination are otherwise normal, with full range of motion and no joint line tenderness or effusion.
Diagnostic Strategies: Plain radiography may confirm the diagnosis, although CT may be required. On the AP view, the fibular head is displaced laterally, and the interosseous space is widened. Comparison views of the uninjured knee may be necessary to appreciate these findings.
Management: Traumatic proximal tibiofibular dislocation is treated initially with closed reduction. If the patient seeks treatment within a few days of injury, reduction of an anterolateral dislocation can be accomplished in the ED by flexing the knee to 90 degrees, everting the ankle, and applying direct pressure to the head of the fibula.70 Orthopedic referral and immobilization of the knee for a minimum of 3 to 6 weeks are necessary after reduction. If closed reduction fails, the patient may require open reduction, with repair of the torn capsule ligaments and pinning. For recurrent dislocations or injuries that do not respond to initial treatment, resection of the proximal fibula or arthrodesis may be effective.
Stress Fractures
Anatomy and Pathophysiology: The tibia is a common site of stress fracture. Usually the stress fracture occurs on the tibial shaft. Fractures typically are horizontal or oblique and uncommonly longitudinal.71 Other sites of stress fracture include the femur, fibula, tarsals (especially navicular), and metatarsals. Stress fractures result from overuse. Stress fractures, which occur as a result of excessive repetitive force to normal bone, are distinguished from pathologic fractures, which occur as a result of normal forces acting on abnormal bone (because of osteoporosis or tumor, for example).
Clinical Features: Bone pain and tenderness without a history of direct trauma are characteristic. The most important historical information includes a recent increase in physical activity, training on hard surfaces, and inadequate footwear. The pain usually is insidious in onset and progressive but may be sudden. Pain is usually relieved with rest. The differential diagnosis for lower leg pain also includes shin splints (see later), exercise-induced compartment syndrome, contusion, muscle strains, tendinitis, periostitis, and interosseous membrane strains. The physical examination may reveal localized bone tenderness and swelling of the overlying soft tissues. Usually there is no muscle atrophy, weakness, or restriction of joint range of motion.
Diagnostic Strategies: The radiographic findings vary depending on the location of the fracture and stage of healing. Approximately one third of stress fractures are evident radiographically at the time of initial diagnosis, compared with one half after 2 to 6 weeks. The radiographic findings often are subtle and may include periosteal new bone, sclerosis, and a lucent line perpendicular to the cortex. MRI can diagnose the condition earlier and more accurately than plain films.71
Management: Most tibial and fibula stress fractures can be treated nonoperatively. Activity should be decreased for 3 to 6 weeks to allow for healing, and serial radiographs should be obtained. In those rare instances in which walking causes pain, a cast and non–weight-bearing status may be required. Serial radiographs are used to evaluate healing. Rare cases of nonunion require surgery.
Compartment Syndrome
Compartment syndrome is caused by increased pressure within a fascial compartment, leading to necrosis of muscle and nerve, and is discussed in Chapter 49.
Soft Tissue Injuries Involving the Lower Leg
Gastrocnemius Strain.: The medial head of the gastrocnemius muscle often is strained in athletics and sometimes ruptures. On physical examination, a palpable gap may be identified in the substance of the muscle, and point tenderness may be elicited in the medial and inferior borders of the muscle belly. Any attempted active or passive ankle dorsiflexion elicits pain.
Plantaris Strain and Rupture.: The plantaris is a small, variable muscle that originates at the lateral condyle of the femur and passes beneath the soleus to insert on the Achilles tendon. It is a feeble flexor of the knee and plantar flexor of the ankle joint with little functional significance. Rupture may occur at the myotendinous junction with or without an associated partial tear of the medial head of the gastrocnemius muscle. A strain of the more proximal plantaris muscle also may occur as an isolated injury or in conjunction with injury to the ACL of the knee. The patient may describe a sudden sharp snap in the posterior calf, followed by a duller deep ache, which may be disabling. Tenderness is greatest just lateral to the midline of the posterior calf. Treatment is symptomatic.
Shin Splints: Shin splints refers to anterior tibial pain occurring during or after exercise. The most common causes are a tibial stress reaction or periostitis. Tibial stress reactions are microfractures caused by stress placed on the tibia and are distinct from gross stress fractures, which predispose the affected bone to complete fracture.
Foreign Bodies: Foreign bodies such as plant matter (e.g., thorns) are commonly encountered in the leg. Missed retained foreign bodies in the lower leg can be the cause of cellulitis, abscess, necrotizing fasciitis, and gangrene. Plain films are a necessary part of evaluation but will be unhelpful when the foreign body is radiolucent. Ultrasound imaging is superior for diagnosis and localization, and fluoroscopy and MRI are alternatives.72 Surgical exploration is sometimes necessary. Extraction is difficult, and deep foreign bodies should be removed by a surgeon, often in the operating room.
References
1. Roberts, DM, Stallard, TC. Emergency department evaluation and treatment of knee and leg injuries. Emerg Med Clin North Am. 2000;18:67.
2. Snell, RS. Clinical anatomy. In: Snell RS, ed. Clinical Anatomy. Philadelphia: Lippincott, Williams & Wilkins, 2004.
3. Lassen, MR, Borris, LC, Nakov, RL. Use of the low-molecular-weight heparin reviparin to prevent deep-vein thrombosis after leg injury requiring immobilization. N Engl J Med. 2002;347:726.
4. Stannard, JP, et al. Vascular injuries in knee dislocations: The role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86:910.
5. Lubovitz, JH, Bernardini, BJ, Reid, JB, 3rd. Current concepts review: Comprehensive physical examination for instability of the knee. Am J Sports Med. 2003;36:577.
6. Jackson, JL, O’Malley, PG, Kroenke, K. Evaluation of acute knee pain in primary care. Ann Intern Med. 2003;139:575.
7. Hurley, WL, Denegar, C, Buckley, WE. The relationship between grading and instrument measurements of anterior knee laxity. J Sport Rehabil. 2008;17:60.
8. Mustonen, AO, Koskinen, SK, Kiuru, MJ. Acute knee trauma: Analysis of multidetector computer tomography findings and comparison with conventional radiography. Acta Radiol. 2005;46:866–874.
9. Stiell, IG, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA. 1996;275:611.
10. Stiell, IG, et al. Implementation of the Ottawa Knee Rule for the use of radiography in acute knee injuries. JAMA. 1997;278:2075.
11. Ketelslegers, E, et al. Validation of the Ottawa knee rules in an emergency teaching centre. Eur Radiol. 2002;12:1218–1220.
12. Seaberg, DC, Jackson, R. Clinical decision rule for knee radiographs. Am J Emerg Med. 1994;12:541.
13. Seaberg, DC, Yealy, DM, Lukens, T, Auble, T, Mathias, S. Multicenter comparison of two clinical decision rules for the use of radiography in acute, high-risk knee injuries. Ann Emerg Med. 1998;32:8.
14. Bulloch, B, et al. Validation of the Ottawa Knee Rule in children: A multicenter study. Ann Emerg Med. 2003;42:48.
15. Khine, H, Dorfman, DH, Avner, JR. Applicability of Ottawa knee rule for knee injury in children. Pediatr Emerg Care. 2001;17:401.
16. Verma, A, Su, A, Golin, AM, O’Marrah, B, Amorosa, JK. A screening method for knee trauma. Acad Radiol. 2001;8:392.
17. Redmond, JM, Levy, BA, Dajani, KA, Cass, JR, Cole, PA. Detecting vascular injury in lower-extremity orthopedic trauma: The role of CT angiography. Orthopedics. 2008;31:761–767.
18. Beall, DP, et al. Magnetic resonance imaging of the collateral ligaments and anatomic quadrants of the knee. Radiol Clin North Am. 2007;45:983.
19. Vaz, CE, Camargo, OP, Santana, PJ, Valezi, AC. Accuracy of magnetic resonance imaging in identifying traumatic intra-articular knee lesions. Clinics (Sao Paulo). 2005;60:445.
20. Keese, GR, Boody, AR, Wongworawat, MD, Jobe, CM. The accuracy of the saline load test in the diagnosis of traumatic knee arthrotomies. J Orthop Trauma. 2007;21:442–443.
21. Wascher, DC, Dvirnak, PC, DeCoster, TA. Knee dislocation: Initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525.
22. Robertson, A, Nutton, RW, Keating, JF. Dislocation of the knee. J Bone Joint Surg Br. 2006;88:706.
23. Frykberg, ER. Popliteal vascular injury. Surg Clin North Am. 2002;82:67.
24. Barnes, CJ, Pietrobon, R, Higgins, LD. Does the pulse examination in patients with traumatic knee dislocation predict a surgical arterial injury? A meta-analysis. J Trauma. 2002;53:1109–1114.
25. Bandyk, DF. Vascular injury associated with extremity trauma. Clin Orthop Relat Res. 1995;318:117.
26. Niall, DM, Nutton, RW, Keatiing, JF. Palsy of the common peroneal nerve after traumatic dislocation of the knee. J Bone Joint Surg Br. 2005;87:664.
27. Ríos, A, Villa, A, Fahandezh, H, de José, C, Vaquero, J. Results after treatment of traumatic knee dislocations: A report of 26 cases. J Trauma. 2003;55:489.
28. Nicandri, GT, Dunbar, RP, Wahl, CJ. Are evidence-based protocols which identify vascular injury associated with knee dislocation underutilized? Knee Surg Sports Traumatol Arthrosc. 2010;18:1005–1012.
29. Nicandri, GT, Chamberlain, AM, Wahl, CJ. Practical management of knee dislocations: A selective angiography protocol to detect limb-threatening vascular injuries. Clin J Sport Med. 2009;19:125–129.
30. Peng, PD, et al. CT angiography effectively evaluates extremity vascular trauma. Am Surg. 2008;74:103.
31. Miller-Thomas, MM, West, OC, Cohen, AM. Diagnosing traumatic arterial injury in the extremities with CT angiography: Pearls and pitfalls. Radiographics. 2005;25(Suppl 1):S133.
32. Wiss, DA, Watson, JT, Johnson, EE. Fractures of the knee. In: Rockwood CA, Jr., Green DP, eds. Fractures in Adults. 4th ed. Philadelphia: Lippincott-Raven; 1996:1919.
33. Mills, WJ, Tejwani, N. Heterotopic ossification after knee dislocation: The predictive value of the injury severity score. J Orthop Trauma. 2003;17:338.
34. Mui, LW, Engelsohn, E, Umans, H. Comparison of CT and MRI in patients with tibial plateau fracture: Can CT findings predict ligament tear or meniscus injury? Skeletal Radiol. 2007;36:145.
35. Papagelopoulos, PJ, et al. Complications after tibia plateau fracture surgery. Injury. 2006;37:475.
36. Weigel, DP, Marsh, JL. High-energy fractures of the tibial plateau: Knee function after longer follow-up. J Bone Joint Surg Am. 2002;84:1541.
37. Watson, JT. High-energy fractures of the tibial plateau. Orthop Clin North Am. 1994;25:723.
38. Pallin, DJ. Images in emergency medicine: Lipohemarthrosis. Ann Emerg Med. 2007;50:120.
39. Aderinto, J, Walmsley, P, Keating, JF. Fractures of the tibial spine: Epidemiology and outcome. Knee. 2008;15:164.
40. Schenck, RC, Jr. Injuries of the knee. In: Rockwood CA, Jr., Green DP, eds. Fractures in Adults. 5th ed. Philadelphia: Lippincott-Raven; 2001:1843.
41. Sponseller, P, Beaty, JH. Fractures and dislocations about the knee. In: Rockwood CA, Jr., Green DP, eds. Fractures in Children. 4th ed. Philadelphia: Lippincott-Raven; 1996:1233–1329.
42. Ogden, JA. Skeletal Injury in the Child, 2nd ed. Philadelphia: Saunders; 1990.
43. Perron, AD, Miller, MD, Brady, WJ. Orthopedic pitfalls in the emergency department: Pediatric growth plate injuries. Am J Emerg Med. 2002;20:50.
44. Bretlau, T, et al. Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc. 2002;10:96.
45. Kocher, MS, Tucker, R, Ganley, TJ, Flynn, JM. Management of osteochondritis dissecans of the knee: Current concepts review. Am J Sports Med. 2006;34:1181.
46. Lotke, PA, Battish, R, Nelson, CL. Treatment of osteonecrosis of the knee. Instr Course Lect. 2001;50:483.
47. Gil, HC, Levine, SM, Zoga, AC. MRI findings in the subchondral bone marrow: A discussion including transient osteoporosis, transient bone marrow edema syndrome, SONK, and bone marrow edema of the knee. Semin Musculoskelet Radiol. 2006;10:177.
48. Kellersman, R, Blattert, TR, Weckbach, A. Bilateral patellar tendon rupture without predisposing systemic disease or steroid use: A case report and review of the literature. Arch Orthop Trauma Surg. 2005;125:127.
49. Maffuli, N, Wong, J. Rupture of the Achilles and patellar tendons. Clin Sports Med. 2003;22:761.
50. Scuderi, GR, Scott, WN, Insall, JN. Injuries of the knee. In: Rockwood CA, Jr., Green DP, Bucholz R, Heckman JD, eds. Rockwood and Green’s Fractures in Adults. 4th ed. Philadelphia: Lippincott-Raven; 1996:2001–2126.
51. Alemparte, J, et al. Patellofemoral evaluation with radiographs and computed tomography scans in 60 knees of asymptomatic subjects. Arthroscopy. 2007;23:170.
52. Merchant, AC. Patellofemoral imaging. Clin Orthop Relat Res. 2001;389:15.
53. Cooper, ME, Selesnick, FH. Partial rupture of the distal insertion of the patellar tendon: A report of two cases in professional athletes. Am J Sports Med. 2000;28:402.
54. Wiss, DA, Watson, JT, Johnson, EE. Fractures of the knee. In: Rockwood CA, Jr., Green DP, Bucholz R, Heckman JD, eds. Rockwood and Green’s Fractures in Adults. 4th ed. Philadelphia: Lippincott-Raven; 1996:1919–2001.
55. Fredericson, M, Yoon, K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil. 2006;85:234.
56. Ufberg, J, McNamara, R. Management of common dislocations. In Roberts JR, Hedges JR, eds.: Clinical Procedures in Emergency Medicine, 4th ed, Philadelphia: Saunders, 2004.
57. Stefancin, JJ, Parker, RD. First-time traumatic patellar dislocation. Clin Orthop Relat Res. 2007;455:93.
58. Prodromos, CC, Han, Y, Rogowski, J, Joyce, B, Shi, K. A meta-analysis of the incidence of anterior cruciate ligament injury as a function of gender, sport, and knee injury-reduction regimen. Arthroscopy. 2007;23:1320.
59. Harner, CD, Hoher, J. Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med. 1998;26:471.
60. Solomon, DH, Simel, DL, Bates, DW, Katz, JN, Schaffer, JL. The rational clinical examination. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA. 2001;286:1610–1620.
61. Herrington, L, Rivet, N, Munro, S. The relationship between patellar position and the length of the iliotibial band as assessed using Ober’s test. Man Ther. 2006;11:182.
62. Ieda, Y, Kotani, A, Ishii, Y. Bilateral plica synovialis mediopatellaris syndrome: A case report. J Orthop Sci. 2003;8:218.
63. Blake, SM, Treble, NJ. Popliteus tendon tenosynovitis. Br J Sports Med. 2005;39:e42.
64. Klovning, J, Beadle, T. Compartment syndrome secondary to spontaneous rupture of a Baker’s cyst. J La State Med Assoc. 2007;159:43.
65. Uppal, A, Lyne, ED. Tibial tubercle fracture with avulsion of the patellar ligament: A case report. Am J Orthop. 2007;36:273.
66. Mosier, SM, Sanitaki, CL. Acute tibial tubercle avulsion fractures. J Pediatr Orthop. 2004;24:181.
67. Gholve, PA, Scher, DM, Khakharia, S, Widmann, RF, Green, DW. Osgood-Schlatter syndrome. Curr Opin Pediatr. 2007;19:44.
68. Okike, K, Bhattacharya, T. Trends in the management of open fractures. J Bone Joint Surg Am. 2006;88:2739.
69. Mechrefe, AP, Koh, EY, Trafton, PG, DiGiovanni, CW. Tibial nonunion. Foot Ankle Clin. 2006;11:1.
70. Van Seymortier, P, Ryckaert, A, Verdonk, P, Almqvist, KF, Verdonk, R. Traumatic proximal tibiofibular dislocation. Am J Sports Med. 2008;36:793.
71. Ruohola, JP, Kiuru, MJ, Pihlajamaki, HK. Fatigue bone injuries causing anterior lower leg pain. Clin Orthop Relat Res. 2006;444:216.
72. Manthey, DE, Storrow, AB, Milbourn, JM, Wagner, BJ. Ultrasound versus radiography in the detection of soft-tissue foreign bodies. Ann Emerg Med. 1996;28:7.