Knee
General Anatomic and Alignment Considerations
Capsule and Reinforcing Ligaments
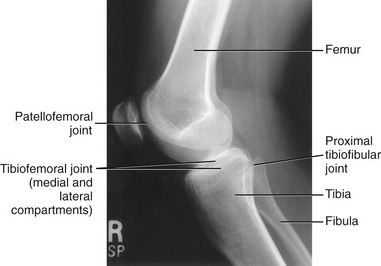
The knee consists of the lateral and medial compartments of the tibiofemoral joint and the patellofemoral joint (Figure 13-1). Motion at the knee occurs in two planes, allowing flexion and extension, and internal and external rotation. Functionally, however, these movements rarely occur independent of movement at other joints within the lower limb. Consider, for example, the interaction among the hip, knee, and ankle during running, climbing, or standing from a seated position. The strong functional association within the joints of the lower limb is reflected by the fact that about two thirds of the muscles that cross the knee also cross either the hip or the ankle.
OSTEOLOGY
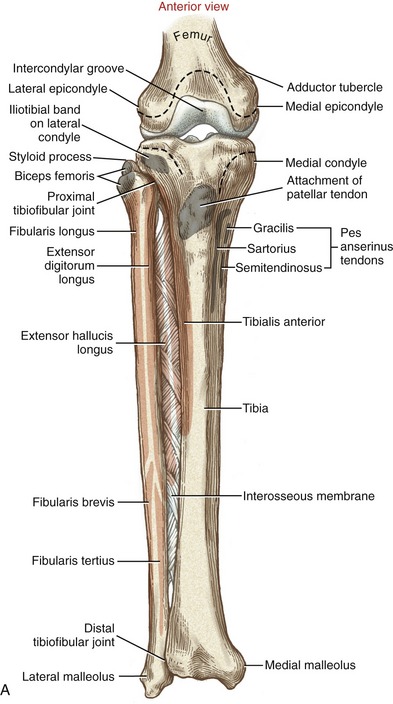
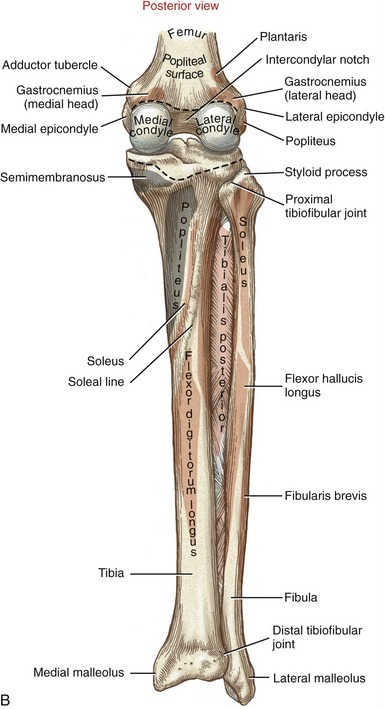
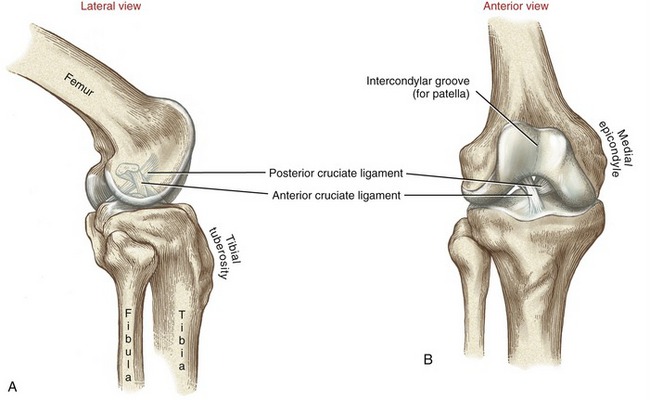
At the distal end of the femur are the large lateral and medial condyles (from the Greek kondylos, knuckle) (Figure 13-2). Lateral and medial epicondyles project from each condyle, providing elevated attachment sites for the collateral ligaments. A large intercondylar notch separates the lateral and medial condyles, forming a passageway for the cruciate ligaments. A narrower than average notch may increase the likelihood of injury to the anterior cruciate ligament.267
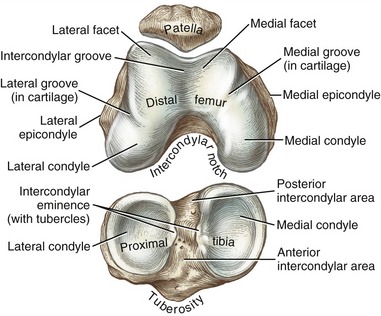
FIGURE 13-2. Osteology of the right patella, articular surfaces of the distal femur, and proximal tibia.
The femoral condyles fuse anteriorly to form the intercondylar (trochlear) groove (see Figure 13-2). This groove articulates with the posterior side of the patella, forming the patellofemoral joint. The intercondylar groove is concave from side to side and slightly convex from front to back. The sloping sides of the intercondylar groove form lateral and medial facets. The more pronounced lateral facet extends more proximally and anteriorly than the medial facet. The steeper slope of the lateral facet helps to stabilize the patella within the groove during knee movement.
Lateral and medial grooves are etched faintly in the cartilage that covers much of the articular surface of the femoral condyles (see Figure 13-2). When the knee is fully extended, the anterior edge of the tibia is aligned with these grooves. The position of the grooves highlights the asymmetry in the shape of the medial and lateral articular surfaces of the distal femur. As explained later in this chapter, the asymmetry in the shape of the condyles affects the sagittal plane kinematics.
The articular capsule of the knee extends across all sides of the tibiofemoral joint and the patellofemoral joint (see dotted lines in Figure 13-3). Posteriorly, the capsule attaches just proximal to the femoral condyles, immediately distal to the popliteal surface of the femur.
Proximal Tibia and Fibula
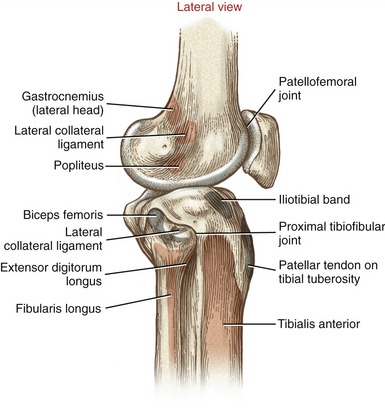
Although the fibula has no direct function at the knee, the slender bone splints the lateral side of the tibia and helps maintain its alignment. The head of the fibula serves as an attachment for the biceps femoris and the lateral collateral ligament. The fibula is attached to the lateral side of the tibia by proximal and distal tibiofibular joints (see Figure 13-3). The structure and function of these joints are discussed in Chapter 14.
The primary function of the tibia is to transfer weight across the knee and to the ankle. The proximal end of the tibia flares into medial and lateral condyles, which form articular surfaces with the distal femur (see Figure 13-3). The superior surfaces of the condyles form a broad region, often referred to as the tibial plateau. The plateau supports two smooth articular surfaces that accept the large femoral condyles, forming medial and lateral compartments of the tibiofemoral joint. The larger, medial articular surface is slightly concave, whereas the lateral articular surface is flat to slightly convex. The articular surfaces are separated down the midline by an intercondylar eminence, formed by irregularly shaped medial and lateral tubercles (see Figure 13-2). Shallow anterior and posterior intercondylar areas flank both ends of the eminence. The cruciate ligaments and menisci attach along the intercondylar region of the tibia.
The prominent tibial tuberosity is located on the anterior surface of the proximal shaft of the tibia (see Figure 13-3, A). The tibial tuberosity serves as the distal attachment for the quadriceps femoris muscle, via the patellar tendon. On the posterior side of the proximal tibia is a roughened soleal line, coursing diagonally in a distal-to-medial direction (see Figure 13-3, B).
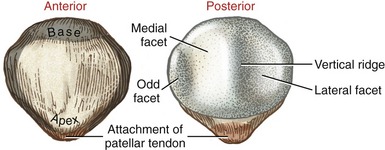
Patella
The patella (from the Latin, “small plate”) is a nearly triangular bone embedded within the quadriceps tendon. It is the largest sesamoid bone in the body. The patella has a curved base superiorly and a pointed apex inferiorly (Figures 13-4 and 13-5). The thick patellar tendon attaches to and between the apex of the patella and the tibial tuberosity. In a relaxed standing position, the apex of the patella lies just proximal to the knee joint line. The subcutaneous anterior surface of the patella is convex in all directions.
The posterior articular surface of the patella is covered with articular cartilage up to 4 to 5 mm thick (see Figure 13-5).65 Part of this surface articulates with the intercondylar groove of the femur, forming the patellofemoral joint. The thick cartilage helps to disperse the large compression forces that cross the joint. A rounded vertical ridge runs longitudinally from top to bottom across the posterior surface of the patella. On either side of this ridge is a lateral or a medial facet. The larger and slightly concave lateral facet matches the general contour of the lateral facet on the intercondylar groove of the femur (see Figure 13-2). The medial facet shows significant anatomic variation. A third “odd” facet exists along the extreme medial border of the medial facet.
ARTHROLOGY
General Anatomic and Alignment Considerations
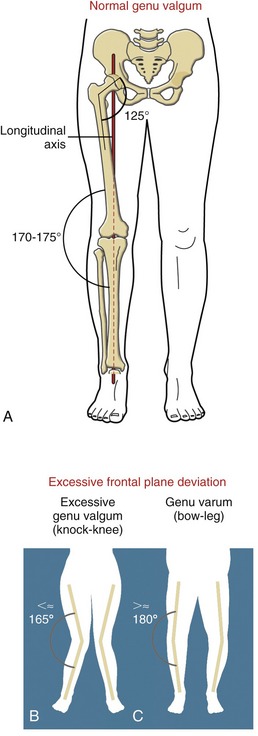
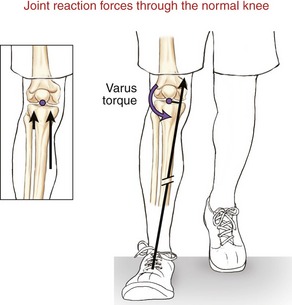
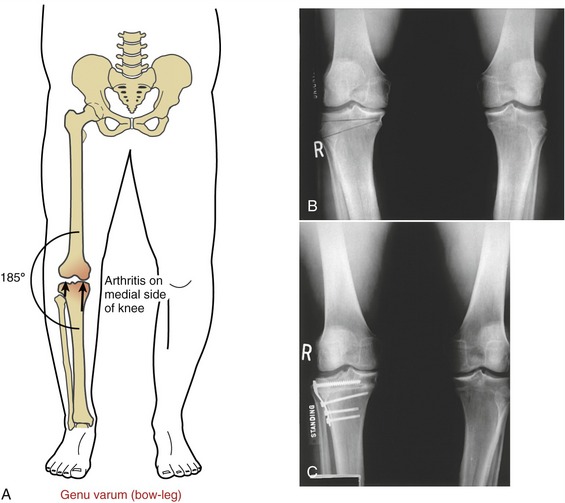
The shaft of the femur angles slightly medially as it descends toward the knee. This oblique orientation is a result of the natural 125-degree angle of inclination of the proximal femur (Figure 13-6, A). Because the articular surface of the proximal tibia is oriented nearly horizontally, the knee forms an angle on its lateral side of about 170 to 175 degrees. This normal alignment of the knee within the frontal plane is referred to as genu valgum.
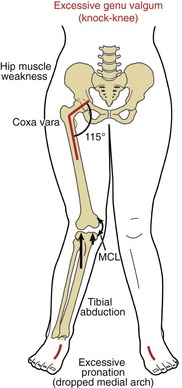
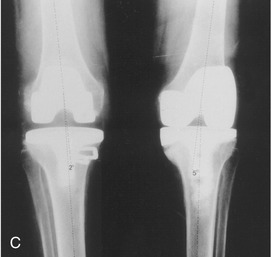
Variation in normal frontal plane alignment at the knee is not uncommon. A lateral angle less than 170 degrees is called excessive genu valgum, or “knock-knee” (see Figure 13-6, B). In contrast, a lateral angle that exceeds about 180 degrees is called genu varum, or “bow-leg” (Figure 13-6, C).
The longitudinal or vertical axis of rotation at the hip is defined in Chapter 12 as a line connecting the femoral head with the center of the knee joint. As depicted in Figure 13-6, A, this longitudinal axis can be extended inferiorly through the knee to the ankle and foot. The axis mechanically links the horizontal plane movements of the major joints of the entire lower limb. Horizontal plane rotations that occur in the hip, for example, affect the posture of the joints throughout the lower limb as far distal as those in the foot, and vice versa.
Capsule and Reinforcing Ligaments
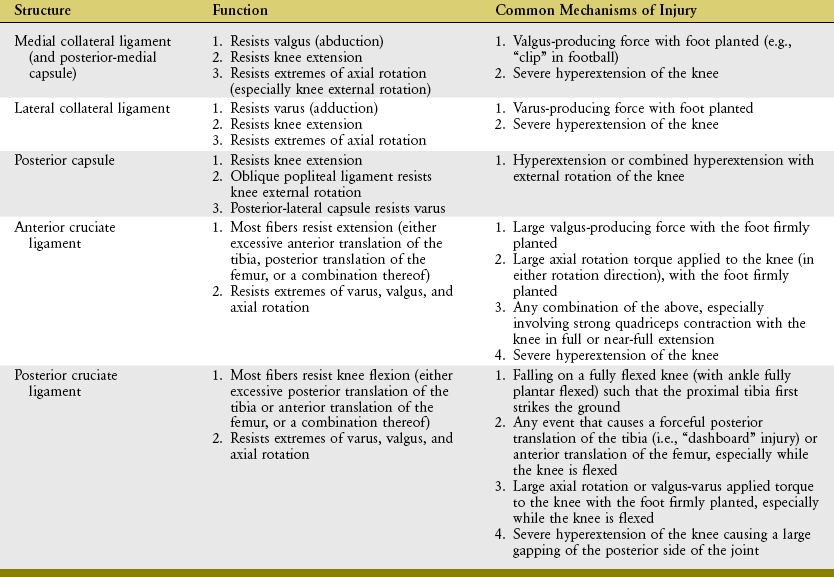
The fibrous capsule of the knee encloses the medial and lateral compartments of the tibiofemoral joint and the patellofemoral joint. The proximal and distal attachments of the capsule to bone are indicated by the dotted lines in Figure 13-3, A and B. The capsule of the knee receives significant reinforcement from muscles, ligaments, and fascia. Five reinforced regions of the capsule are described next and are summarized in Table 13-1.
TABLE 13-1.
Ligaments, Fascia, and Muscles That Reinforce the Capsule of the Knee
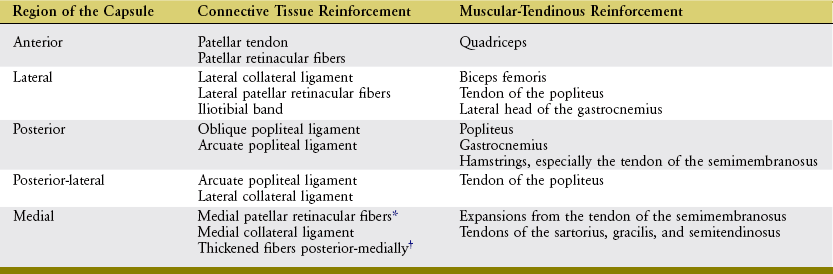
*Often referred to as the medial patellofemoral ligament.
†Often referred to as the posterior-medial capsule or the posterior oblique ligament.
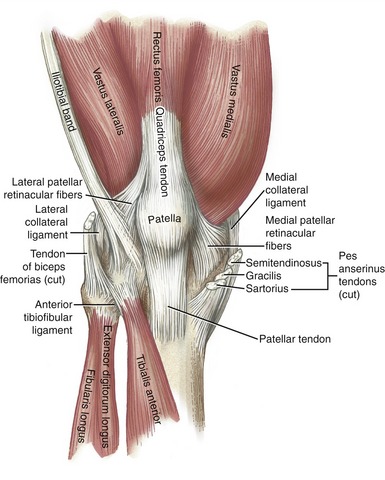
The anterior capsule of the knee attaches to the margins of the patella and the patellar tendon, being reinforced by the quadriceps muscle and medial and lateral patellar retinacular fibers (Figure 13-7). The retinacular fibers are extensions of the connective tissue covering the vastus lateralis, vastus medialis, and iliotibial band. The extensive set of netlike fibers has connection to and among the femur, tibia, patella, quadriceps and patellar tendon, collateral ligaments, and menisci.
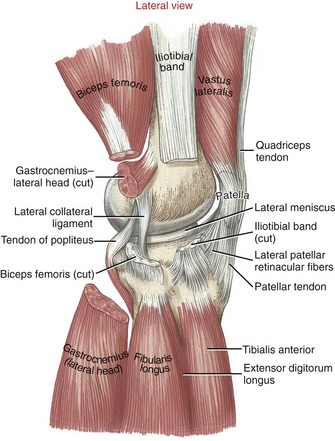
The lateral capsule of the knee is reinforced by the lateral (fibular) collateral ligament, lateral patellar retinacular fibers, and iliotibial band (Figure 13-8).232 Muscular stability is provided by the biceps femoris, the tendon of the popliteus, and the lateral head of the gastrocnemius.
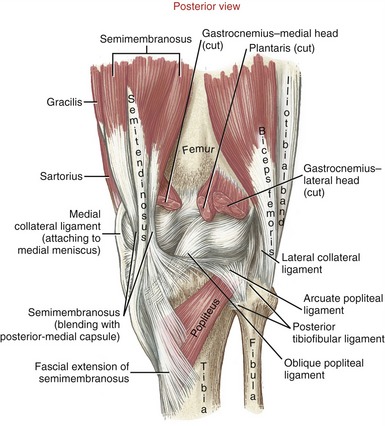
The posterior capsule is reinforced by the oblique popliteal ligament and the arcuate popliteal ligament (Figure 13-9). The oblique popliteal ligament originates medially from the posterior-medial capsule and the semimembranosus tendon. Laterally and superiorly, the fibers blend with the capsule adjacent to the lateral femoral condyle. This ligament is pulled taut in full knee extension, a position that naturally includes slight external rotation of the tibia relative to the femur. The arcuate popliteal ligament originates from the fibular head and then divides into two limbs. The larger and more prominent limb arches (hence the term “arcuate”) across the tendon of the popliteus muscle to attach to the posterior intercondylar area of the tibia. An inconsistent and smaller limb attaches to the posterior side of the lateral femoral condyle, and often to a sesamoid bone (or fabella, meaning “little bean”) embedded within the lateral head of the gastrocnemius. The posterior capsule is further reinforced by the popliteus, gastrocnemius, and hamstring muscles, especially by the fibrous extensions of the semimembranosus tendon. Unlike the elbow, the knee has no bony block against hyperextension. The muscles and posterior capsule limit hyperextension.
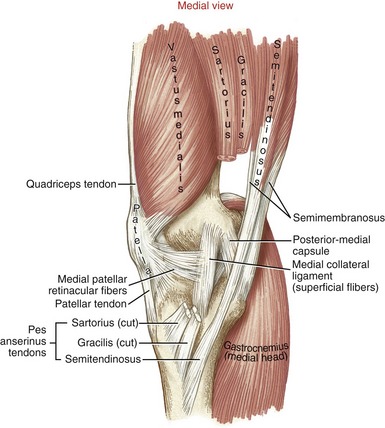
The medial capsule of the knee extends in varying thickness from the patellar tendon to the posterior capsule.226,258 Its anterior one third consists of a thin layer of fascia reinforced by the medial patellar retinacular fibers (Figure 13-10). The middle one third of the capsule is reinforced by a continuation of the medial patellar retinacular fibers and, more substantially, by the superficial and deep fibers of the medial collateral ligament (the deep fibers are not exposed in Figure 13-10). The posterior one third of the capsule is relatively thick, originating near the adductor tubercle and blending with tendinous expansions of the semimembranosis and to the adjacent posterior capsule.226 The posterior one third of the medial capsule is relatively well defined and is frequently described as a discrete structure, often under the name of the posterior-medial capsule or, less frequently, the posterior oblique ligament.203,226 The posterior-medial capsule is reinforced by the flat conjoined tendons of the sartorius, gracilis, and semitendinosus—collectively referred to as the pes anserinus (from the Latin, “goose’s foot”) tendons. The posterior two thirds of the medial capsule and its associated structures provide an important source of stabilization to the knee.225
Synovial Membrane, Bursae, and Fat Pads
The internal surface of the capsule of the knee is lined with a synovial membrane. The anatomic organization of this membrane is complicated, in part, by the knee’s convoluted embryonic development.258
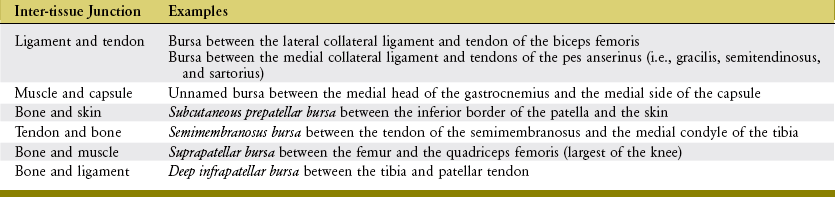
The knee has as many as 14 bursae, which form at inter-tissue junctions that encounter high friction during movement.258 These inter-tissue junctions involve tendon, ligament, skin, bone, capsule, and muscle (Table 13-2). Although some bursae are simply extensions of the synovial membrane, others are formed external to the capsule. Activities that involve excessive and repetitive forces at these inter-tissue junctions potentially lead to bursitis, an inflammation of the bursa.
Tibiofemoral Joint
The tibiofemoral joint consists of the articulations between the large, convex femoral condyles and the nearly flat and smaller tibial condyles (see Figure 13-4). The large articular surface area of the femoral condyles permits extensive knee motion in the sagittal plane for activities such as running, squatting, and climbing. Joint stability is provided not by a tight bony fit, but by forces and physical containment provided by muscles, ligaments, capsule, menisci, and body weight.
MENISCI
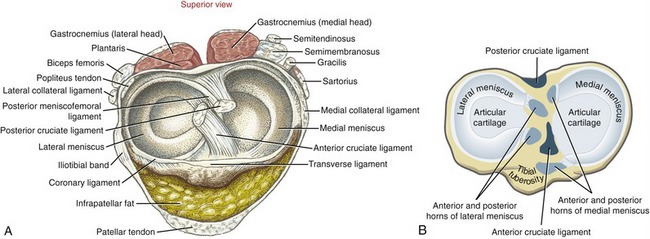
Anatomic Considerations: The medial and lateral menisci are crescent-shaped, fibrocartilaginous structures located within the knee joint (Figure 13-11). The menisci transform the articular surfaces of the tibia into shallow seats for the larger convex femoral condyles. This transformation is most important laterally because of the flat to slightly convex shape of the tibia’s lateral articular surface.
The menisci are anchored to the intercondylar region of the tibia by their free ends, known as anterior and posterior horns. The external edge of each meniscus is attached to the tibia and the adjacent capsule by coronary (or meniscotibial) ligaments (see Figure 13-11, A). The coronary ligaments are relatively loose, thereby allowing the menisci, especially the lateral meniscus, to pivot freely during movement.232 A slender transverse ligament connects the two menisci anteriorly.
Several muscles have secondary attachments into the menisci. The quadriceps and semimembranosus attach to both menisci,124 whereas the popliteus attaches to the lateral meniscus.54,232 Through these attachments, the muscles help stabilize the position of the menisci.
Blood supply to the menisci is greatest near the peripheral (external) border. Blood comes from capillaries located within the adjacent synovial membrane and capsule.258 The internal border of the menisci, in contrast, is essentially avascular.
The two menisci have different shapes and methods of attaching to the tibia. The medial meniscus has an oval shape, with its external border attaching to the deep surface of the medial collateral ligament and adjacent capsule; the lateral meniscus has more of a circular shape, with its external border attaching only to the lateral capsule. The tendon of the popliteus passes between the lateral collateral ligament and the external border of the lateral meniscus (Figure 13-12).
Functional Considerations: The primary function of the menisci is to reduce the compressive stress* across the tibiofemoral joint.123,137 Other functions of the menisci include stabilizing the joint during motion, lubricating the articular cartilage, providing proprioception,284 and helping to guide the knee’s arthrokinematics.
Compression forces at the knee joint routinely reach 2.5 to 3 times body weight while one is walking, and over 4 times body weight while one ascends stairs.176,283 By nearly tripling the area of joint contact, the menisci significantly reduce pressure (i.e., force per unit area) on the articular cartilage. This method of attenuating peak pressure is essential to the health and protection of the knee joint.51 A complete lateral meniscectomy has been shown to increase peak contact pressures at the knee by 230%, which increases the risk of development of stress-related arthritis.52,163,192 Even a tear or a partial meniscectomy significantly increases local stress, which is strongly believed to cause excessive wear on the articular cartilage.137 When possible, surgically repairing a meniscus instead of removing the damaged regions is clearly the treatment of choice.163,216 In certain cases, after a complete meniscectomy a meniscal allograft transplantation may be indicated, with goals of limiting the degeneration of the articular cartilage.35,229
At every step, the menisci deform peripherally as they are compressed.123,248 This mechanism allows part of the compression force at the knee to be absorbed as a circumferential tension (known as hoop stress) throughout each meniscus. Studies indicate that a torn medial meniscus, most notably with an avulsion tear of its posterior horn, loses its ability to optimally resist hoop stress, thereby reducing the capacity for protecting the underlying articular cartilage and bone.161
Common Mechanisms of Injury: Tears of the meniscus are the most common injury of the knee, occurring relatively frequently in both the athletic and the general population.145,187 According to research cited by Lohmander and colleagues, 50% of all acute injuries of the anterior cruciate ligaments are associated with a concurrent injury to a meniscus.145 In general, meniscal tears are often associated with a forceful, axial rotation of the femoral condyles over a partially flexed and weight-bearing knee. The axial torsion within the compressed knee can pinch and dislodge the meniscus. A dislodged or folded flap of meniscus (often referred to as a “bucket-handle tear”) can mechanically block knee movement.
The medial meniscus is injured twice as frequently as the lateral meniscus.29 The mechanism of injury for a medial meniscus tear often involves axial rotation, and also may involve an external force applied to the lateral aspect of the knee. This force—typically described as a “valgus force”—can cause an excessive valgus position of the knee and subsequent large stress on the medial collateral ligament and posterior-medial capsule. Because of the anatomic connections between the medial meniscus and these connective tissues, a significant valgus force delivered to the knee can indirectly strain and thereby injure the medial meniscus.
This risk of developing tears in the meniscus of the knee increases if the knee is malaligned or has a history of ligamentous instability, most notably in the anterior cruciate.145,163
OSTEOKINEMATICS AT THE TIBIOFEMORAL JOINT
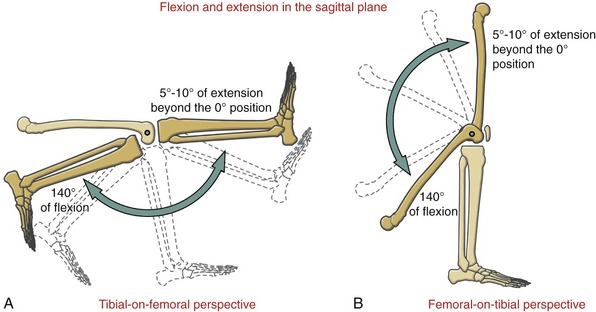
The tibiofemoral joint possesses two degrees of freedom: flexion and extension in the sagittal plane and, provided the knee is at least slightly flexed, internal and external rotation. These motions are shown for tibial-on-femoral and femoral-on-tibial situations in Figures 13-13 and 13-14. Frontal plane motion at the knee occurs passively only, limited to about 6 to 7 degrees.159
Flexion and Extension: Flexion and extension at the knee occur about a medial-lateral axis of rotation. Range of motion varies with age and gender, but in general the healthy knee moves from 130 to 150 degrees of flexion to about 5 to 10 degrees beyond the 0-degree (straight) position.83,224
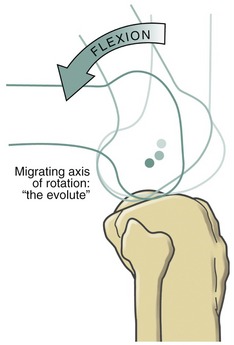
The medial-lateral axis of rotation for flexion and extension is not fixed, but migrates within the femoral condyles.251 The curved path of the axis is known as an “evolute” (Figure 13-15). The path of the axis is influenced by the eccentric curvature of the femoral condyles.97,251
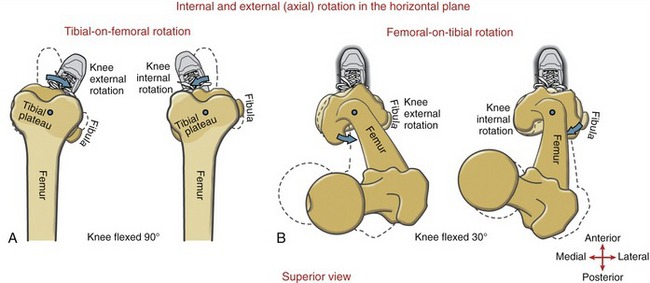
Internal and External (Axial) Rotation: Internal and external rotation of the knee occurs about a vertical or longitudinal axis of rotation. This motion is also called “axial” rotation. In general, the freedom of axial rotation increases with greater knee flexion. A knee flexed to 90 degrees can perform about 40 to 45 degrees of total axial rotation.178,190 External rotation range of motion generally exceeds internal rotation by a ratio of nearly 2 : 1.178 Once the knee is in full extension, however, axial rotation is maximally restricted. Rotation of the knee is significantly blocked by passive tension in the stretched ligaments, parts of the capsule, and increased bony congruity within the joint.
As depicted in Figure 13-14, axial rotation of the knee occurs by either tibial-on-femoral or femoral-on-tibial rotation. (Although not depicted, axial rotation can also occur as a result of both rotational perspectives occuring simultaneously.) Axial rotation of the knee provides an important functional element of mobility to the lower extremity as a whole. The terminology used to describe axial rotation of the knee is important to understand. As a rule, the naming of axial rotation of the knee is based on the position of the tibial tuberosity relative to the anterior distal femur. External rotation of the knee, for example, occurs when the tibial tuberosity is located lateral to the distal anterior femur. This rule, however, does not stipulate whether the femur or tibia is the moving bone; it only stipulates the relative articular orientation of the rotated knee. To demonstrate, compare external rotation of the knee in Figures 13-14, A and B. Tibial-on-femoral external rotation of the knee occurs as the tibia rotates externally relative to a stationary femur. On the other hand, femoral-on-tibial external rotation of the knee occurs as the femur rotates internally relative to a stationary tibia (and foot). Both examples fit the definition of external rotation of the knee because both motions end up with a similar articular orientation: the tibial tuberosity is located lateral to the anterior distal femur. The distinction between bony rotation (tibial or femoral) and knee joint rotation must always be clear to avoid misinterpretation. This point is particularly important in describing femoral-on-tibial osteokinematics.
ARTHROKINEMATICS AT THE TIBIOFEMORAL JOINT
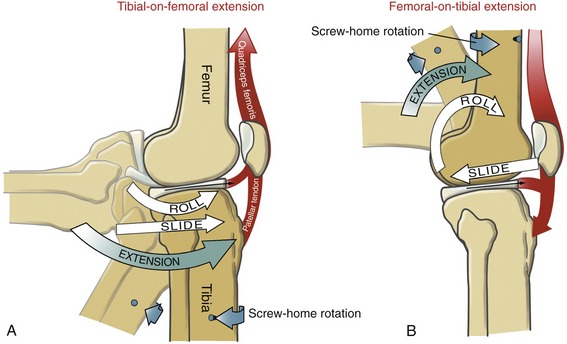
Extension of the Knee: Figure 13-16 depicts the arthrokinematics of the last 90 degrees of active knee extension. During tibial-on-femoral extension, the articular surface of the tibia rolls and slides anteriorly on the femoral condyles (see Figure 13-16, A). The menisci are shown pulled anteriorly by the contracting quadriceps muscle.
During femoral-on-tibial extension, as in standing up from a deep squat position, the femoral condyles simultaneously roll anteriorly and slide posteriorly on the articular surface of the tibia (see Figure 13-16, B). These “offsetting” arthrokinematics limit the magnitude of anterior translation of the femur on the tibia. The quadriceps muscle directs the roll of the femoral condyles and stabilizes the menisci against the horizontal shear caused by the sliding femur.
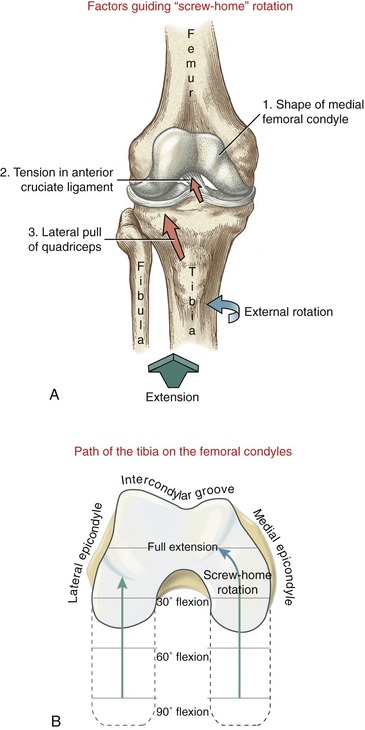
“Screw-Home” Rotation of the Knee: Locking the knee in full extension requires about 10 degrees of external rotation.109 The rotary locking action has historically been referred to as the “screw-home” rotation, based on the observable twisting of the knee during the last 30 or so degrees of extension. The external rotation described here is fundamentally different from the axial rotation illustrated in Figure 13-14. Screw-home (external) rotation has been described as a conjunct rotation, emphasizing the fact that it is mechanically linked (or coupled) to the flexion and extension kinematics and cannot be performed independently.200,258 The combined external rotation and knee extension maximizes the overall contact area of the adult knee: 375 mm2 in the medial tibiofemoral joint and about 275 mm2 in the lateral tibiofemoral joint.200 This final position of extension increases joint congruence and favors stability.
To observe the screw-home rotation at the knee, have a partner sit with the knee flexed to about 90 degrees. Draw a line on the skin between the tibial tuberosity and the apex of the patella. After the partner completes full tibial-on-femoral extension, redraw this line between the same landmarks and note the change in position of the externally rotated tibia. A similar but less obvious locking mechanism also functions during femoral-on-tibial extension (compare Figure 13-16, A with B). When one rises up from a squat position, for example, the knee locks into extension as the femur internally rotates relative to the fixed tibia. Regardless of whether the thigh or leg is the moving segment, both knee extension movements depicted in Figure 13-16, A and B show a knee joint that is relatively externally rotated when fully extended.
The screw-home rotation mechanics are driven by at least three factors: the shape of the medial femoral condyle, the passive tension in the anterior cruciate ligament, and the slight lateral pull of the quadriceps muscle (Figure 13-17). The most important (or at least obvious) factor is the shape of the medial femoral condyle. As depicted in Figure 13-17, B, the articular surface of the medial femoral condyle curves about 30 degrees laterally, as it approaches the intercondylar groove. Because the articular surface of the medial condyle extends farther anteriorly than the lateral condyle, the tibia is obliged to “follow” the laterally curved path into full tibial-on-femoral extension. During femoral-on-tibial extension, the femur follows a medially curved path on the tibia. In either case, the result is external rotation of the knee at full extension.
Flexion of the Knee: The arthrokinematics of knee flexion occur by a reverse fashion as that depicted in Figure 13-16. For a knee that is fully extended to be unlocked, the joint must first internally rotate slightly.200,206,225 This action is driven primarily by the popliteus muscle. The muscle can rotate the femur externally to initiate femoral-on-tibial flexion or can rotate the tibia internally to initiate tibial-on-femoral flexion.
Internal and External (Axial) Rotation of the Knee: As described earlier, the knee must be flexed to maximize independent axial rotation between the tibia and femur. Once the knee is flexed, the arthrokinematics of internal and external rotation involve primarily a spin between the menisci and the articular surfaces of the tibia and femur. Axial rotation of the femur over the tibia causes the menisci to deform slightly, as they are compressed between the spinning femoral condyles. The menisci are stabilized by connections from active musculature such as the popliteus and semimembranosus.
MEDIAL AND LATERAL COLLATERAL LIGAMENTS
Anatomic Considerations: The medial (tibial) collateral ligament (MCL) is a flat, broad structure that crosses the medial side of the joint.258 Although different terminology exists, this chapter describes the MCL as having superficial and deep parts.225,226 The larger superficial part consists of a relatively well-defined set of parallel running fibers about 10 cm in length (see Figure 13-10).226 After arising from the medial epicondyle of the femur, the superficial fibers course distally to blend with medial patellar retinacular fibers before attaching to the medial-proximal aspect of the tibia. The fibers attach just posterior to the distal attachments of the closely aligned tendons of the sartorius and the gracilis.
The deep part of the MCL consists of a shorter and more oblique set of fibers, lying immediately deep and slightly posterior and distal to the proximal attachment of the superficial fibers. Although not visible on Figure 13-10, the deep fibers attach distally to the posterior-medial joint capsule, medial meniscus, and tendon of the semimembranosus muscle.226,258
The lateral (fibular) collateral ligament consists of a round, strong cord that runs nearly vertically between the lateral epicondyle of the femur and the head of the fibula (see Figure 13-8).135,232 Distally, the lateral collateral ligament blends with the tendon of the biceps femoris muscle. Unlike its medial counterpart, the MCL, the lateral collateral ligament does not attach to the adjacent lateral meniscus (see Figure 13-12). As described later in this chapter, the tendon of the popliteus courses between these two structures.
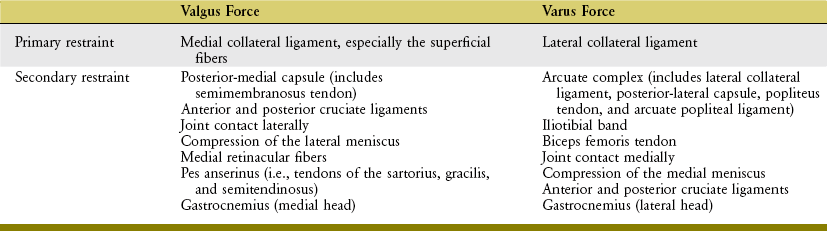
Functional Considerations: The primary function of the collateral ligaments is to limit excessive knee motion within the frontal plane. With the knee extended, the superficial part of the MCL provides the primary resistance against a valgus (abduction) force.74,225 The lateral collateral ligament, in comparison, provides the primary resistance against a varus (adduction) force.95,237 Table 13-3 lists several other tissues that provide restraint against valgus and varus applied forces to the knee.
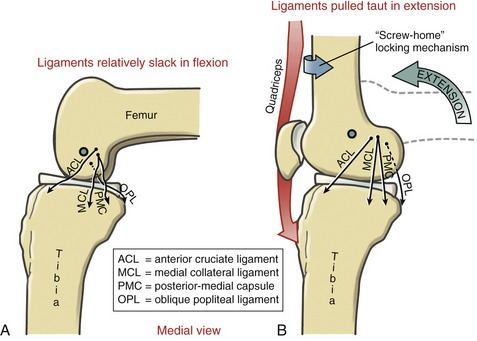
A secondary function of the collateral ligaments is to produce a generalized stabilizing tension at the knee throughout the sagittal plane range of motion. Although some of the fibers that constitute the collateral ligaments are taut throughout the full range of knee flexion and extension, most are positioned slightly posterior to the medial-lateral axis of rotation of the knee and therefore are pulled relatively taut in full extension.197,225,268 Other structures that become more taut in full extension are the posterior-medial capsule, the oblique popliteal ligament (representative of the posterior capsule), the knee flexor muscles, and the components of the anterior cruciate ligament.197,203,225 Figure 13-18 demonstrates these tissues as being relatively slack in flexion (A) and more taut as the knee assumes the locked position of full femoral-on-tibial extension (B). Full extension—which includes the kinematics of the screw-home rotation—elongates the collateral ligaments roughly 20% beyond their length at full flexion.270 Although a valuable stabilizer in full extension, a taut MCL and posterior-medial capsule are especially vulnerable to injury from a valgus (i.e., an abduction) load delivered over a planted foot. Because the deeper fibers of the MCL are shorter than the superficial, the deeper fibers experience a greater percentage of stretch when subjected to similar valgus (abduction) strain.225 Primarily for this reason, the deeper fibers of the MCL are more frequently injured than the superficial fibers during an excessive valgus-related trauma, such as what typically occurs in the “clip” injury in American football.250
The collateral ligaments and adjacent capsule also provide resistance to the extremes of internal and external rotation.232,270 Most notable in this regard are the elongation and subsequent increased passive tension in the superficial fibers of the MCL at the extremes of external rotation of the knee.74,225 Planting the right foot securely on the ground and vigorously rotating the superimposed femur (and body) to the left, for example, may damage the superficial fibers of the right MCL. This potential for injury increases if the externally rotating knee (i.e., internally rotating femur) is simultaneously experiencing a substantial valgus load.
Table 13-4 provides a summary of the functions and common mechanisms of injury for the major ligaments of the knee, including the posterior-medial and posterior capsule.
ANTERIOR AND POSTERIOR CRUCIATE LIGAMENTS
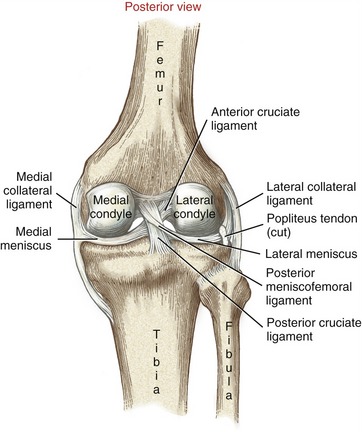
General Considerations: Cruciate, meaning cross-shaped, describes the spatial relation of the anterior and posterior cruciate ligaments as they cross within the intercondylar notch of the femur (Figure 13-19). The cruciate ligaments are intracapsular and covered by an extensive synovial lining. The ligaments are supplied with blood from small vessels located in the synovial membrane and nearby tissues.
The cruciate ligaments are named according to their attachment to the tibia (see Figure 13-11). Both ligaments are thick and strong, reflecting their important role in providing multiplanar stability to the knee. Acting together, the anterior and posterior cruciate ligaments resist the extremes of all knee movements (review Table 13-4).* Most important, however, the cruciate ligaments provide most of the resistance to anterior-posterior shear forces created between the tibia and femur. These forces reflect the natural sagittal plane kinematics associated with walking, running, squatting, and jumping.
In addition to stabilizing the knee, tension in the anterior and posterior cruciate ligaments helps guide the knee’s arthrokinematics. Furthermore, because the cruciates contain mechanoreceptors, they indirectly provide the nervous systems with proprioceptive feedback.234,236 In addition to helping control movement, these sensory receptors may also play a protective role by reflexively limiting muscle activation that could create large and potentially damaging strain on the anterior cruciate ligament.253,266
ANTERIOR CRUCIATE LIGAMENT
Anatomy and Function: The anterior cruciate ligament (ACL) attaches along an impression on the anterior intercondylar area of the tibial plateau. From this attachment, the ligament runs obliquely in a posterior, superior, and lateral direction to attach on the medial side of the lateral femoral condyle (see Figure 13-19). The collagen fibers within the ACL twist on one another, forming two often indistinct spiraling bundles.14 The bundles are often referred to as anterior-medial and posterior-lateral, named according to their relative attachments to the tibia.48,49,56
The tension and orientation of the ACL change as the knee flexes and extends.48,114,181 Although some fibers of the ACL remain relatively taut throughout the full range of sagittal plane motion, most fibers, especially those within the posterior-lateral bundle, become increasingly taut as the knee approaches and reaches full extension.13,32,114,166 In addition to most fibers of the ACL, the posterior capsule, parts of the collateral ligaments, and all knee flexor muscles also become relatively taut in extension, which helps stabilize the knee, especially during weight-bearing activities (review Figure 13-18, B).
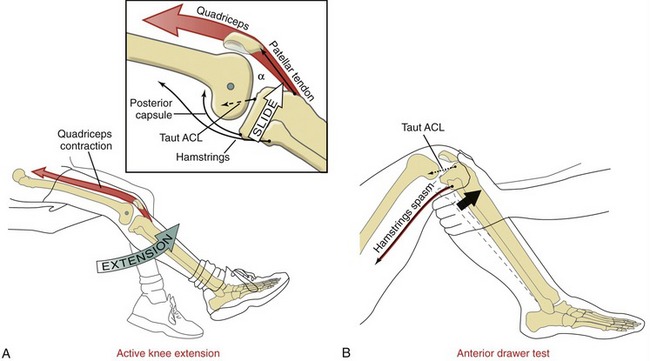
During the last approximately 50 to 60 degrees of complete knee extension, the active force generated by the contracting quadriceps pulls the tibia anteriorly, thereby powering the anterior slide arthrokinematics (Figure 13-20, A).14,142,143,157,160 The resulting tension in the stretched fibers of the ACL helps limit the extent of this anterior slide. Clinically, it is useful to appreciate the general similarity between the anterior force placed on the ACL by quadriceps contraction and the anterior-directed pull applied to the tibia as a clinician performs an anterior drawer test (see Figure 13-20, B). This test is one of several used by clinicians to assess the relative amount of laxity in a knee with a suspected injured ACL. The basic component of this test involves pulling the proximal end of the tibia (leg) forward with the knee flexed to about 90 degrees. In the normal knee the ACL provides about 85% of the total passive resistance to the anterior translation of the tibia.26 An anterior translation of 8 mm ( inch) greater than the contralateral knee suggests a possible tear of the ACL. As illustrated in Figure 13-20, B, protective spasm in the hamstring muscles may limit anterior translation of the tibia, thereby masking a torn ACL.
inch) greater than the contralateral knee suggests a possible tear of the ACL. As illustrated in Figure 13-20, B, protective spasm in the hamstring muscles may limit anterior translation of the tibia, thereby masking a torn ACL.
Clinically, the quadriceps muscle is often referred to as an “ACL antagonist.” This naming reflects the fact that the contraction force from the quadriceps at relatively low flexion angles stretches (or antagonizes) most fibers of the ACL.108,166,194,241 Studies have reported a 4.4% strain on the ACL after a maximal-effort, isometric activation of the quadriceps at 15 degrees of flexion.12 This level of strain would increase as a result of a forceful contraction of the quadriceps that abruptly brings the tibia into full knee extension. The ability of the quadriceps to strain the ACL is greatest at full extension because this position maximizes the angle-of-insertion of the patellar tendon relative to the tibia (see α in Figure 13-20, A).168 The greater this angle-of-insertion, the greater the proportion of quadriceps force is available to slide the tibia anteriorly relative to the femur. The angle-of-insertion is progressively reduced with greater knee flexion, thereby reducing the muscle’s ability to slide the tibia anteriorly and stretch the ACL.13,16,120,157,167 Understanding factors that naturally strain the ACL becomes important when considering mechanisms that cause ACL injury or ways to protect an ACL graft early after surgery.45 These issues will be revisited later in this chapter.
Common Mechanisms of Injury: The oblique manner by which the ACL courses through the knee allows for at least a part of its structure to resist the extremes of essentially all movements of the knee.14,59 Although this spatial orientation is ideal for providing a wide range of stability, it also renders the ligament vulnerable to injury from many combinations of extreme movements. One variable that is common to essentially all ACL injuries is the presence of a high-velocity stretch to a ligament that is already under tension; the ligament ruptures when the tensile stress exceeds its physiologic strength.14 Biomechanical factors associated with the amount of tension in the ACL at any given instant are interrelated and complex. These factors include the direction and magnitude of the ground reaction force; the amount, control, and precise sequencing of protective muscular forces; the integrity and strength of the surrounding tissues; and the alignment and position of the knee.92
The ACL is the most frequently totally ruptured ligament of the knee. Approximately half of all ACL injuries occur in persons between 15 and 25 years of age, often during high-velocity sporting activities such as American football, downhill skiing, lacrosse, basketball, and soccer.99 Most ACL tears involve a transient subluxation of the knee, causing secondary trauma to other tissues, including bone, articular cartilage, menisci, or the MCL.152,188,256
Injury to the ACL can lead to marked instability of the knee and potentially stressful kinematics.269 An ACL-deficient knee is also more vulnerable to injury or deterioration of other structures.185,268 Furthermore, because the ligament does not spontaneously heal on its own, surgical reconstruction is often recommended, requiring an autograft (using the person’s own patellar tendon or hamstring-adductor tendon) or an allograft.9,14,207 Although these reconstructions are reasonably successful at restoring basic stability and function to the knee, the natural kinematics and in some cases the preinjury muscle strength are not fully restored.14,136,262,274 Even after surgical reconstruction, persons who have had an ACL rupture are at an elevated risk for developing stress-related osteoarthritis of the knee at some point in their lives.145,183
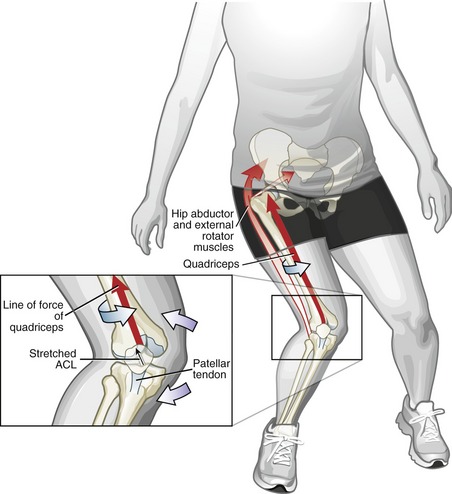
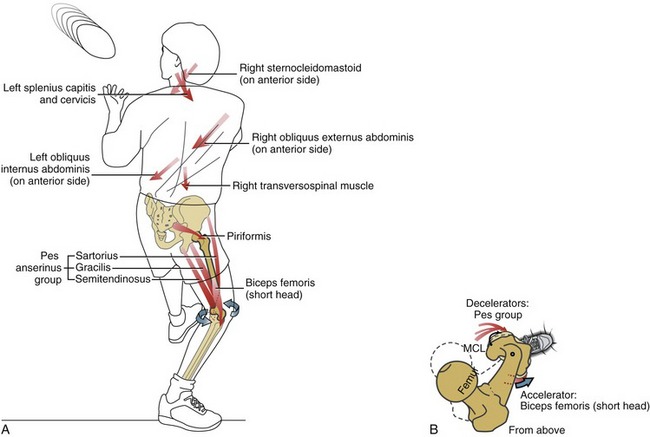
Approximately 70% of ACL sporting-related injuries occur through noncontact, or at least minimal contact, situations.128,171 Many noncontact injuries occur while landing from a jump, or while quickly and forcefully decelerating, cutting, or pivoting over a single planted lower limb.67 The mechanisms causing the injury are often unpredictable and occur very rapidly; therefore the precise position and prevailing direction of the forces applied to the knee at the time of injury are not always certain. Much of what is known about the mechanisms associated with noncontact ACL injury are from reports from the injured players; careful video analysis of the injury; and simulated injury and stress-strain relationships using ligaments of cadavers, implanted strain gauges in the ACL in live persons and cadavers, and computer-based biomechanical models.* As stated earlier, one movement situation that is frequently associated with a noncontact injury of the ACL involves landing from a jump.246,278 Self-reports, video analysis, and other study methods frequently confirm at least three factors associated with this potentially harmful event: (1) strong activation of the quadriceps muscle over a slightly flexed or fully extended knee, (2) a marked “valgus collapse” of the knee, and (3) excessive external rotation of the knee (i.e., the femur excessively rotated internally at the hip relative to a fixed tibia).** All three of these elements are present in Figure 13-21. Research has indeed confirmed that the kinetic and kinematic situations described relative to Figure 13-21 can, when combined or extreme, overload the tensile strength of the ACL.† Although not depicted in Figure 13-21, excessive internal rotation of the knee (when combined with extension and extreme valgus) has also been shown to be a predisposing factor to ACL injury.‡59,160,246
Another common mechanism for injuring the ACL involves excessive hyperextension of the knee while the foot is firmly planted on the ground.19 Normal extension kinematics would, in theory, involve an excessive posterior slide of the femur relative to the tibia (review Figure 13-16, B). During hyperextension, however, the posterior femoral slide relative to the fixed tibia may overstretch and rupture the ACL. A large concurrent activation of the quadriceps muscle may pull the tibia forward relative to the posterior sliding femur, thereby adding to the likelihood of injury.45 Often, hyperextension-related ACL injuries are associated with large axial rotation or valgus-producing forces, thereby further increasing the tension on the ACL.160,246 In addition to injuring the ACL, marked hyperextension frequently causes injury to the posterior capsule and MCL. Table 13-4 summarizes many of the common mechanisms of injury that may be associated with the ACL.
POSTERIOR CRUCIATE LIGAMENT
Anatomy and Function: Slightly thicker than the ACL, the posterior cruciate ligament (PCL) attaches from the posterior intercondylar area of the tibia to the lateral side of the medial femoral condyle (see Figures 13-11, 13-12, and 13-19). The specific anatomy of the PCL is usually described as having two primary bundles: a larger anterior set (anterior-lateral), forming the bulk of the ligament, and a smaller posterior set (posterior-medial).2,158,196 Some authors have proposed four distinct fiber bundles within the PCL.37,158
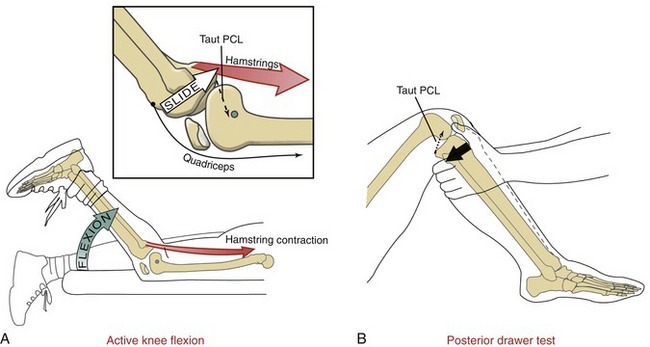
As the knee flexes, the PCL undergoes a complex twisting and changing in its length and orientation.43,196 The precise mechanical effect of this dynamic deformation is not completely understood. Because of the relative low incidence of PCL injury, research regarding its specific function has lagged behind that of the ACL. What is known, however, is that some fibers within the PCL remain taut throughout most of flexion and extension, although the majority of the ligament becomes increasingly taut with greater flexion.131,196,217 Between full extension and approximately 30 to 40 degrees of flexion, most of the PCL is relatively slackened; tension peaks between 90 and 120 degrees of flexion.37,141,196 In vivo analysis through magnetic resonance imaging (MRI) shows that, on average, the bulk of the PCL elongates approximately 30% of its length between full extension and 90 degrees of flexion; this correlates to an approximate 3% increase in length per 10 degrees of flexion.196 This relative sharp increase in tension explains, in part, why many PCL injuries involve significant knee flexion. In addition to becoming taut in flexion, the PCL provides a secondary restraint to varus-and-valgus loads, as well as excessive axial rotation.37
While a person actively flexes the knee against gravity, such as when lying prone, the knee flexor muscles (such as the hamstrings) actively slide the tibia (along with the fibula) posteriorly relative to the femur. The extent of the posterior slide arthrokinematics is limited, in part, by passive tension in the PCL (Figure 13-22, A).141 For this reason, the hamstrings are often referred to as a “PCL antagonist,” especially at flexion angles closer to a 90-degree position, which aligns the hamstrings nearly perpendicular to the long axis of the tibia. Adding a forceful contraction of the quadriceps to an existing hamstring contraction reduces the strain on the PCL.69,96
One of the most commonly performed tests to evaluate the integrity of the PCL is the “posterior drawer” test. This test involves pushing the proximal end of the tibia (leg) posteriorly with the knee flexed to about 90 degrees (see Figure 13-22, B). In this position the PCL provides about 95% of the total passive resistance to the posterior translation of the tibia.6 With the knee held between 0 and about 30 degrees flexion, the PCL provides only negligible passive resistance to posterior translation of the tibia; most of the resistance is furnished by the posterior capsule and the majority of the fibers within the collateral ligaments—tissues that are naturally stretched in near extension.37
Another function of the PCL is to limit the extent of anterior translation of the femur relative to the fixed lower leg. Activities such as rapid descent into a deep squat can create a potential anterior translation of the femur relative to the tibia. The femur is prevented from sliding off the anterior edge of the tibia by tension in the PCL as well as the surrounding capsule and compression forces within the tibiofemoral joint caused by gravity and muscular coactivation. As apparent in Figure 13-8, the stout tendon of the popliteus, by crossing obliquely across the posterior-lateral side of the knee, can resist anterior translation of the femur relative to the tibia (or posterior translation of the tibia relative to the femur).232 The importance of the restraining function of the popliteus is more evident in persons with a PCL-deficient knee.232
Common Mechanisms of Injury: Most PCL injuries are associated with high-energy trauma, such as being in an automobile accident or playing contact sports like American football.198,235 It is generally reported that isolated sports-related PCL injuries are rare.156 The cited percentage of sports-related injuries involving isolated PCL tears is generally within the 2% to 10% range.33,156,204 Approximately half of all PCL injuries also involve other knee structures, including the meniscus, ACL, and posterior-lateral capsule.235
Several mechanisms have been described for injury to the PCL.110,204,235 One relatively frequent mechanism involves falling over a fully flexed knee (with the ankle plantar flexed) such that the proximal tibia first strikes the ground.156,235 One of the most common high-energy injuries to the PCL is the “dashboard” injury, in which the knee of a passenger in an automobile strikes the dashboard subsequent to a front-end collision, driving the tibia posteriorly relative to the femur. Other mechanisms of injury are listed in Table 13-4.
Often after a PCL injury the proximal tibia sags posteriorly relative to the femur when the lower leg is subjected to the pull of gravity. This observation, in conjunction with a positive posterior drawer sign, suggests a ruptured PCL. Often, isolated PCL injuries can be managed conservatively without tendon graft reconstructive surgery. Surgery is often recommended, however, if marked posterior instability or subluxation is evident and (as frequently is the case) the PCL is injured along with other ligaments. Data on long-term function of the knee after PCL injury are lacking. Most studies suggest that the PCL-deficient knee is more likely to develop posttraumatic knee osteoarthritis.22,223,240 Whether PCL reconstruction following injury prevents the knee from significant instability and degeneration later in life is a controversial topic.156
Patellofemoral Joint
PATELLOFEMORAL JOINT KINEMATICS
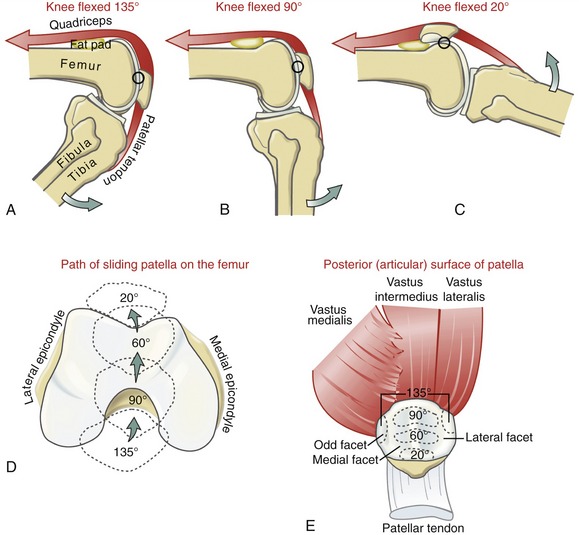
Path and Area of Patellar Contact on the Femur: Data from in vivo and in vitro studies have provided detailed descriptions of the kinematics and contact areas within the patellofemoral joint during flexion and extension.* Most in vivo measurements are made using MRI scanners or fluoroscopy or by inserting metallic pins into bone. Data primarily from the work of Goodfellow and Hungerford were used to help construct the model illustrated in Figure 13-23.70 At 135 degrees of flexion, the patella contacts the femur primarily near its superior pole (see Figure 13-23, A). At this near fully flexed position, the patella rests below the intercondylar groove, bridging the intercondylar notch of the femur (see Figure 13-23, D). In this position, the lateral edge of the lateral facet and the “odd” facet of the patella share articular contact with the femur (see Figure 13-23, E). As the knee extends toward 90 degrees of flexion, the primary contact region on the patella starts to migrate toward its inferior pole (see Figure 13-23, B).220,231 Between 90 and 60 degrees of flexion, the patella is usually engaged within the intercondylar groove of the femur. Within this arc of motion, the contact area between the patella and femur is therefore greatest (see Figure 13-23, D and E).41,102 Even at its maximum, however, the contact area is only about one third of the total surface area of the posterior side of the patella. Joint pressure (i.e., compression force per unit area), therefore, can rise to very large levels within the patellofemoral joint, given strong activation of the quadriceps muscle.
As the knee extends through the last 20 to 30 degrees of flexion, the primary contact point on the patella migrates to its inferior pole (see Figure 13-23, C). Within this arc the patella loses much of its mechanical engagement with the intercondylar groove. Once in full extension, the patella rests completely proximal to the groove and against the suprapatellar fat pad. In this position, with the quadriceps relaxed, the patella can be moved freely relative to the femur. The overall reduced fit of the patella within the intercondylar groove in the first 20 or 30 degrees of flexion explains, in part, why most chronic lateral dislocations of the patella occur near this position.1 The reason why the patella typically dislocates laterally is based primarily on the overall lateral line of force of the quadriceps muscle relative to the long axis of the patellar tendon—a topic that is covered in the upcoming sections that describe the structure and function of the quadriceps muscles.
MUSCLE AND JOINT INTERACTION
The quadriceps femoris is innervated by the femoral nerve (see Figure 12-24, A). Like the triceps at the elbow, the knee’s sole extensor group is innervated by just one peripheral nerve. A complete femoral nerve lesion, therefore, can cause total paralysis of the knee extensors. The flexors and rotators of the knee are innervated by several nerves from both the lumbar and sacral plexus, but primarily by the tibial portion of the sciatic nerve (see Figure 12-24, B). Table 13-5 lists the motor innervation of all muscles that cross the knee.
TABLE 13-5.
Actions and Innervation of Muscles that Cross the Knee*
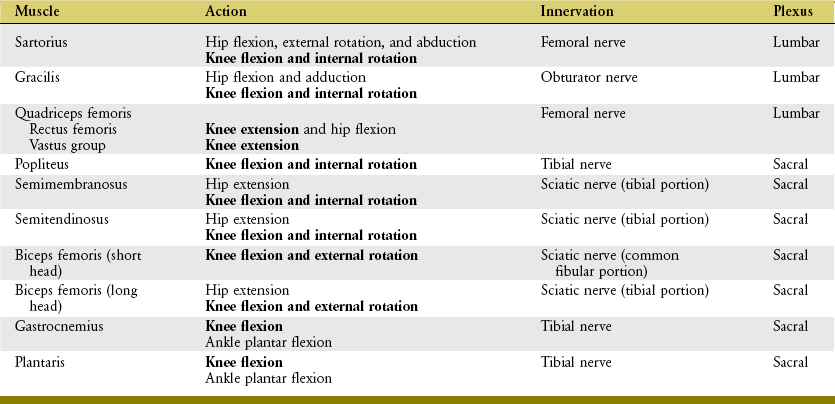
*The actions involving the knee are shown in bold. Muscles are listed in descending order of nerve root innervations.
As an additional reference, the primary spinal nerve roots that supply the muscles of the lower extremity are listed in Appendix IV, Part A. In addition, Appendix IV, Parts B and C include additional reference items to help guide the clinical assessment of the functional status of the L2-S3 spinal nerve roots.
Sensory Innervation of the Knee Joint
Sensory innervation of the knee and associated ligaments is supplied primarily from L3 through L5 spinal nerve roots, which travel to the spinal cord primarily in the posterior tibial, obturator, and femoral nerves.106,119 The posterior tibial nerve (a branch of the tibial portion of the sciatic) is the largest afferent supply to the knee joint. It supplies sensation to the posterior capsule and associated ligaments and most of the internal structures of the knee as far anterior as the infrapatellar fat pad. Afferent fibers within the obturator nerve carry sensation from the skin over the medial aspect of the knee and parts of the posterior and posterior-medial capsule. Afferent fibers from the femoral nerve supply most of the anterior-medial and anterior-lateral capsule.
Muscular Function at the Knee
Muscles of the knee are described as two groups: the knee extensors (i.e., quadriceps femoris) and the knee flexor-rotators. The anatomy of many of these muscles is presented in Chapter 12. Consult Appendix IV, Part D for a summary of the attachments and nerve supply to the muscles of the knee.
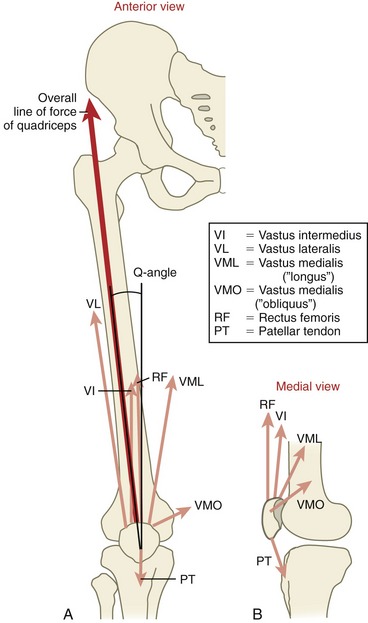
EXTENSORS OF THE KNEE: QUADRICEPS FEMORIS MUSCLE
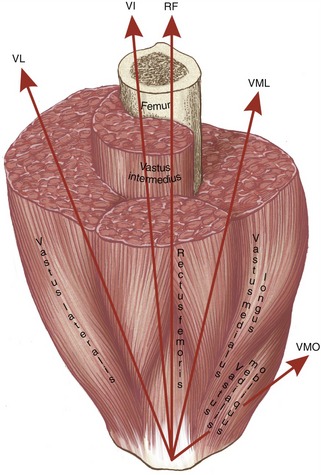
Anatomic Considerations: The quadriceps femoris is a large and powerful extensor muscle, consisting of the rectus femoris, vastus lateralis, vastus medialis, and deeper vastus intermedius (see Figures 13-7 and 13-24). The large vastus group of muscles produces about 80% of the total extension torque at the knee, and the rectus femoris produces about 20%.101 Contraction of the vastus muscles extends the knee only. Contraction of the rectus femoris, however, causes hip flexion and knee extension.
All heads of the quadriceps unite to form a strong quadriceps tendon that attaches to the base and sides of the patella. The patellar tendon connects the apex of the patella to the tibial tuberosity. The vastus lateralis and vastus medialis muscles attach into the capsule and menisci via patellar retinacular fibers (see Figure 13-7). Together, the quadriceps muscle and tendon, patella, and patellar tendon are referred to as the knee extensor mechanism.
The rectus femoris attaches to the pelvis near the anterior-inferior iliac spine. The vastus muscles, however, attach to an extensive part of the femur, particularly the anterior-lateral shaft and the linea aspera (Figure 12-5). Although the vastus lateralis has the largest cross-sectional area of the quadriceps muscles, the vastus medialis extends farther distally toward the knee.277
The vastus medialis consists of fibers that form two distinct fiber directions. The more distal oblique fibers (the vastus medialis “obliquus”) approach the patella at 50 to 55 degrees medial to the quadriceps tendon (see Figure 13-24). The remaining more longitudinal fibers (the vastus medialis “longus”) approach the patella at 15 to 18 degrees medial to the quadriceps tendon.144 The oblique fibers of the vastus medialis extend further distally than other muscular components of the quadriceps. Although the oblique fibers account for only 30% of the cross-sectional area of the entire vastus medialis muscle,218 the oblique pull on the patella has important implications for the stabilization and orientation of the patella as it slides (tracks) through the intercondylar groove of the femur.
The deepest quadriceps muscle, the vastus intermedius, is located under the rectus femoris. Deep to the vastus intermedius is the poorly defined articularis genu. This muscle contains a few slips of fibers that attach proximally to the anterior side of the distal femur, and then distally into the anterior capsule. This muscle pulls the capsule and synovial membrane proximally during active knee extension.258 The articularis genu is analogous to the poorly defined articularis cubiti at the elbow.
Functional Considerations: In general, the knee extensor muscles produce a torque about two thirds greater than that produced by the knee flexor muscles.28,71 Through their isometric, eccentric, and concentric activations, this extensor torque is used to perform multiple functions at the knee. Through isometric activation, the quadriceps stabilizes and helps to protect the knee; through eccentric activation, the quadriceps controls the rate of descent of the body’s center of mass, such as during sitting or squatting. Eccentric activation of these muscles also provides shock absorption to the knee. At the heel contact phase of walking, the knee flexes slightly in response to the ground reaction force. Eccentrically active quadriceps controls the extent of the knee flexion. Acting as a spring, the muscle helps dampen the impact of loading on the joint. This protection is especially useful during high-impact loading, such as during landing from a jump, the initial foot contact phase of running, or descending from a high step. A person whose knee is braced or fused in extension lacks this natural shock absorption mechanism.
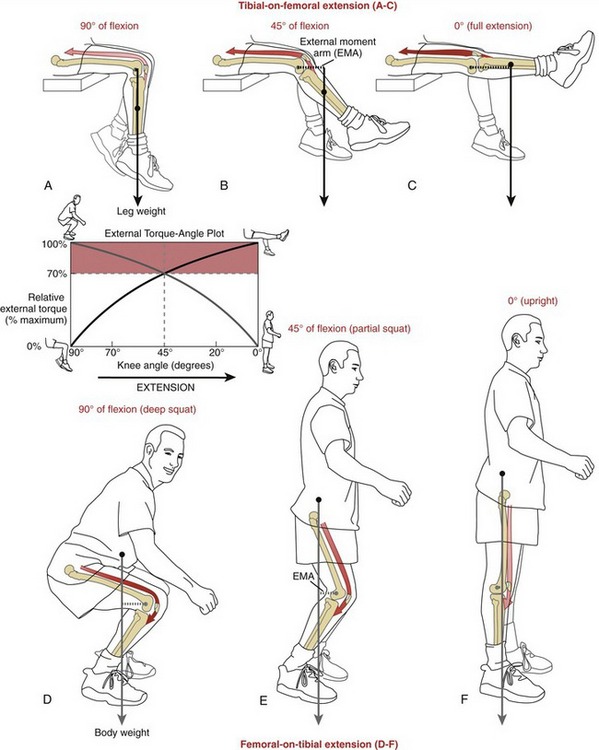
Quadriceps Action at the Knee: Understanding the Biomechanical Interactions between External and Internal Torques: In many upright activities, an external (flexor) torque is acting on the knee. This external torque is equal to the external load being moved or supported, multiplied by its external moment arm. The external flexor torque must often be met or exceeded by an opposing internal (extensor) torque, which is the product of quadriceps force multiplied by its internal moment arm. An understanding of how these opposing torques are produced and functionally interact is the focus of this section. This topic is an important component of many aspects of strengthening the quadriceps as part of a rehabilitation program.279
External Torque Demands Placed against the Quadriceps: Contrasting “Tibial-on-Femoral” with “Femoral-on-Tibial” Methods of Knee Extension: Many strengthening exercises designed to challenge the quadriceps muscle rely on resistive, external torques generated by gravity acting on the body. The magnitude of the external torque is highly dependent on the specific manner in which the knee is being extended. These differences are illustrated in Figure 13-25. During tibial-on-femoral knee extension, the external moment arm of the weight of the lower leg increases from 90 to 0 degrees of knee flexion (see Figure 13-25, A to C). In contrast, during femoral-on-tibial knee extension (as in rising from a squat position), the external moment arm of the upper body weight decreases from 90 to 0 degrees of knee flexion (see Figure 13-25, D to F). The graph included in Figure 13-25 contrasts the external torque–knee angle relationships for the two methods of extending the knee between 90 degrees of flexion and full extension.
Information contained in the graph in Figure 13-25 is useful for designing quadriceps strengthening exercises. By necessity, exercises that significantly challenge the quadriceps also stress the knee joint and its associated periarticular connective tissues. Clinically, this stress may be considered potentially damaging or therapeutic, depending on the medical history of the person performing the exercise. A person with marked patellofemoral joint pain or painful knee arthritis, for example, is typically advised against producing large muscular-based stresses on the knee. A completely healthy person or a high-level athelete in the later phases of postsurgical ACL rehabilitation, in contrast, may actually benefit from such judiciously applied muscular stresses to the knee.
External torques applied to the knee by a constant load vary in a predictable fashion, based on knee angle and orientation of the limb segments. As depicted by the red shading in the graph in Figure 13-25, external torques are relatively large from 90 to 45 degrees of flexion via femoral-on-tibial extension, and from 45 to 0 degrees of flexion via tibial-on-femoral extension. Reducing these external torques can be accomplished by several strategies. An external load, for example, can be applied at the ankle during tibial-on-femoral knee extension between 90 and 45 degrees of flexion. This activity can be followed by an exercise that involves rising from a partial squat position, a motion that incorporates femoral-on-tibial extension between 45 and 0 degrees of flexion. Combining both exercises in the manner described provides only moderate to minimal external torques against the quadriceps, throughout a continuous range of motion.
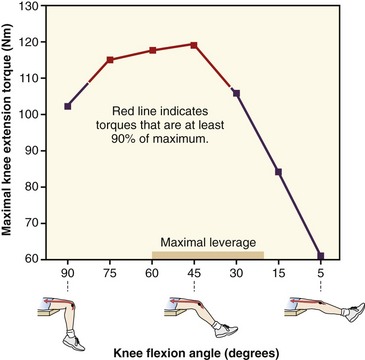
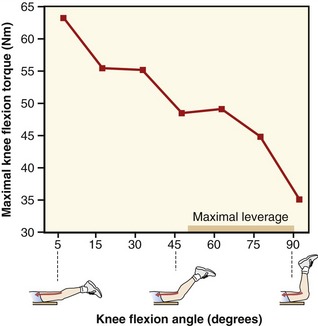
Internal Torque–Joint Angle Relationship of the Quadriceps Muscle: Maximal knee extension (internal) torque typically occurs between 45 and 70 degrees of knee flexion, with less torque produced at the near extremes of flexion and extension.129,130,205,219,251 The specific shape of this torque-angle curve varies, however, based on the type and speed of activation and position of the hip.130,205 A representative maximal-effort torque versus joint angle curve obtained from healthy male subjects is displayed in Figure 13-26. In this study, subjects produced maximal-effort (isometric) knee extension torque with hips held fixed in extension.251 As depicted by the red line in Figure 13-26, maximal-effort knee extension torque remains at least 90% of maximum between 80 and 30 degrees of flexion. This high-torque potential of the quadriceps within this arc of motion is used during many functional activities that incorporate femoral-on-tibial kinematics, such as ascending a high step, rising from a chair, or holding a partial squat position while participating in sports, such as basketball or speed skating. Note the rapid decline in internal torque potential as the knee angle approaches full extension. Most studies report a 50% to 70% reduction in maximal internal torque as the knee approaches full extension.130,205,251 Of interest, the external torque applied against the knee during femoral-on-tibial extension also declines rapidly during this same range of motion (see Figure 13-25, graph). There appears to be a general biomechanical match in the internal torque potential of the quadriceps and the external torques applied against the quadriceps during the last approximately 45 to 70 degrees of complete femoral-on-tibial knee extension. This match accounts, in part, for the popularity of “closed-kinematic chain” exercises that focus on applying resistance to the quadriceps while the upright person moves the body through this arc of femoral-on-tibial knee extension.279
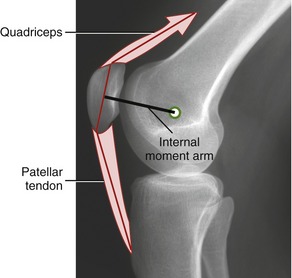
Functional Role of the Patella: The patella acts as a “spacer” between the femur and quadriceps muscle, which increases the internal moment arm of the knee extensor mechanism (Figure 13-27). By definition, the knee extensor internal moment arm is the perpendicular distance between the medial-lateral axis of rotation and the line of force of the muscle. Because torque is the product of force and its moment arm, the presence of the patella augments the extension torque at the knee.
Researchers have shown that the knee extensor internal moment arm changes considerably across the full arc of knee flexion and extension.127,251,257 Although the data published on this topic differ considerably based on methodology and natural variability, most studies report that the knee extensor moment arm is greatest between about 20 and 60 degrees of knee flexion (see bar on horizontal axis in graph of Figure 13-26).24,127,251 This range of relatively high leverage partially explains why knee extension torques are typically highest across a significant part of this same range of motion. Maximal-effort knee extension torque typically falls off dramatically in the last 30 degrees of extension, likely because of a combination of reduced extension leverage and shortened muscle length.
At least three factors affect the length of the knee extension moment arm across the sagittal plane range of motion. These include (1) the shape and position of the patella, (2) the shape of the distal femur (including the depth of the intercondylar groove), and (3) the migrating medial-lateral axis of rotation at the knee (referred to as the evolute earlier in this chapter). Exactly how the changing length of the internal moment arm influences the shape of the extensor torque–joint angle curve, such as that depicted in Figure 13-26 is uncertain. It is technically difficult to isolate the effects of leverage from those of changing muscle length: both factors simultaneously change throughout the range of motion, and both directly or indirectly affect knee extension torque.
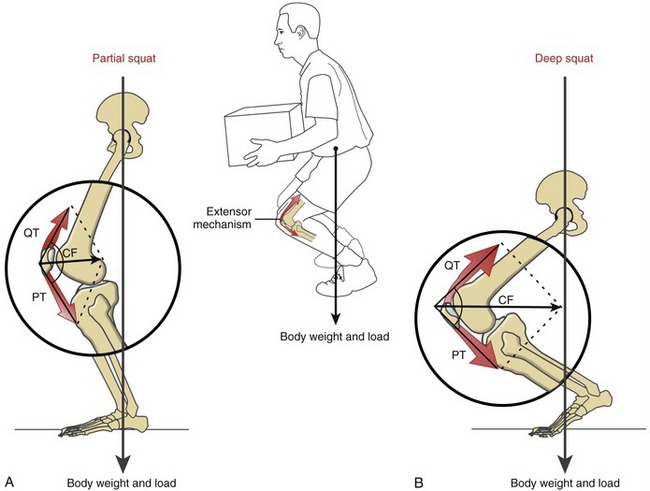
PATELLOFEMORAL JOINT KINETICS
The patellofemoral joint is routinely exposed to high magnitudes of compression force. A sampling of these forces include 1.3 times body weight during walking on level surfaces, 2.6 times body weight during performance of a straight leg raise, 3.3 times body weight during climbing of stairs, and up to 7.8 times body weight during performance of deep knee bends.55,139,221,242 Although these compression forces originate primarily from active forces produced from the overlying quadriceps, their magnitude is strongly influenced by the amount of knee flexion at the time of muscle activation. To illustrate this important interaction, consider the compression force on the patellofemoral joint in a partial squat position (Figure 13-28, A). Forces within the extensor mechanism are transmitted proximally and distally through the quadriceps tendon (QT) and patellar tendon (PT), much like a cable crossing a pulley. The resultant, or combined, effect of these forces is directed toward the intercondylar groove of the femur as a joint compression force (CF). Increasing knee flexion by descending into a deeper squat significantly raises the force demands throughout the extensor mechanism, and ultimately on the patellofemoral joint (see Figure 13-28, B). The increased knee flexion associated with the deeper squat also reduces the angle formed by the intersection of force vectors QT and PT. As shown by vector addition, reducing the angle of these force increases the magnitude of the CF directed between the patella and the femur. In theory, if the QT and PT vectors were collinear and oriented in opposite directions, the muscular-based compression force on the patellofemoral joint would be zero.
Both the compression force and area of articular contact on the patellofemoral joint increase with knee flexion, reaching a maximum between 60 and 90 degrees of knee flexion.102,148,167,231 As described earlier, the compression force can rise to very high levels during descent into a squat position. Because increased flexion is associated with a greater relative increase in compression force than relative increase in articular contact area, the stress (force/area) is also greatest in the patellofemoral joint in the position of 60 to 90 degrees of knee flexion. Without the relatively large contact area to disperse the large compression force produced by the quadriceps, the stress within the joint would rise to intolerable physiologic levels.11,55,148 Having the area of joint contact greatest at positions that are generally associated with the largest muscular-based compression force naturally protects the joint against stress-induced cartilage degeneration. This mechanism allows most healthy and normally aligned patellofemoral joints to tolerate large compression forces over a lifetime, often with little or no appreciable discomfort or degeneration of the articular cartilage or subchondral bone. As will be explained, for many persons, however, the natural high force environment within the patellofemoral joint is a contributing factor to the development of patellofemoral pain syndrome.
FACTORS AFFECTING THE TRACKING OF THE PATELLA ACROSS THE PATELLOFEMORAL JOINT
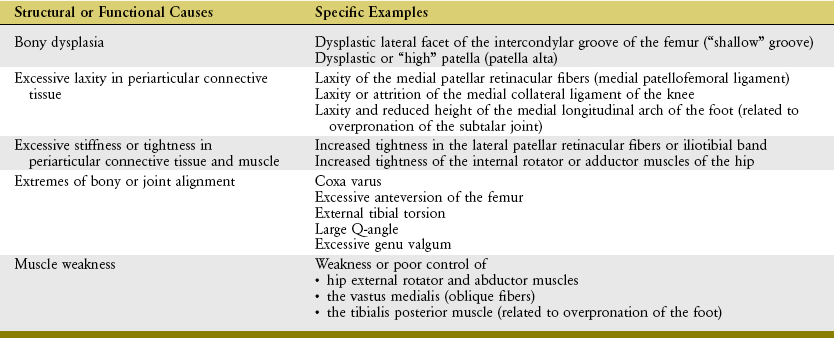
The large compression forces that naturally occur at the patellofemoral joint are typically well tolerated, provided that the forces are evenly dispersed across the largest possible area of articular surface. A joint with less than optimal congruity, or one with subtle structural anomalies, will likely experience abnormal “tracking” of the patella. As a consequence, the patellofemoral joint is exposed to higher joint contact stress, thereby increasing its risk for developing degenerative lesions and pain.53,132,220 Such a scenario may ultimately lead to patellofemoral pain syndrome or potentially trigger osteoarthritis.
Role of the Quadriceps Muscle in Patellar Tracking: Among the most important influences on patellofemoral joint biomechanics are the magnitude and direction of force produced by the overlying quadriceps muscle. As the knee is extending, the contracting quadriceps pulls the patella not only superiorly within the intercondylar groove, but also slightly laterally and posteriorly. The slight but omnipresent lateral line of force exerted by the quadriceps results, in part, from the larger cross-sectional area and force potential of the vastus lateralis. Because of the purported association between patellofemoral joint pain and excessive lateral tracking (and subluxation) of the patella, assessing the overall lateral line of pull of the quadriceps relative to the patella is a meaningful clinical measure. Such a measure is referred to as the quadriceps angle, or more commonly the Q-angle (Figure 13-29, A).62,195 The Q-angle is formed between (1) a line representing the resultant line of force of the quadriceps, made by connecting a point near the anterior-superior iliac spine to the midpoint of the patella, and (2) a line representing the long axis of the patellar tendon, made by connecting a point on the tibial tuberosity with the midpoint of the patella. Q-angles average about 13 to 15 degrees (± 4.5 degrees) when measured across a healthy adult population.195 The Q-angle assessment has been criticized for its low association with pathology at the patellofemoral joint, poorly standardized measurement protocol,87,211 and inability to measure dynamic alignment. Nevertheless, the Q-angle remains the most popular and simple clinical index for assessing the relative lateral pull of the quadriceps on the patella.62,102,195 Factors that naturally offset or limit the lateral pull of the patella are described in the next section. If these factors fail to operate in a coordinated fashion, the patella may track (shift and tilt) more laterally within the intercondylar groove—kinematics that reduce contact area, increase patellofemoral joint stress,64,82 and increase the likelihood of chronic lateral dislocation of the patella.1,220,231
Activation of the quadriceps as a whole also pulls and compresses the patella posteriorly, thereby stabilizing its path of movement relative to the distal femur. This stabilization effect increases with greater knee flexion (review Figure 13-28). Even in full knee extension, however, some fibers of the quadriceps are aligned to produce a posterior compression through the patellofemoral joint. This is particularly apparent by observing a side-view diagram of the line of force of the oblique fibers of the vastus medialis (see Figure 13-29, B). Although relatively small, this posterior stabilizing effect on the patella is especially useful in the last 20 degrees of extension, at a point when (1) the patella is no longer fully engaged within the intercondylar groove of the femur and (2) the resultant joint compression (stabilizing) force produced by the quadriceps as a whole is least.1
Factors that Naturally Oppose the Lateral Pull of the Quadriceps on the Patella: Several factors throughout the lower extremity oppose and thereby limit the lateral bias in pull of the quadriceps relative to the patellofemoral joint. These factors are important to optimal tracking. In this context, optimal tracking is defined as movement between the patella and femur across the greatest possible area of articular surface with the least possible stress. Understanding the factors that favor optimal tracking provides insight into most pathomechanics and many treatments for pain and other dysfunctions of the patellofemoral joint. Both local and global factors will be described. Local factors are those that act directly on the patellofemoral joint. Global factors, on the other hand, are those related to the alignment of the bones and joints of the lower limb. Although these factors are described as separate entities, in reality, their effectiveness in optimizing patellar tracking is based on the sum of their combined influences.
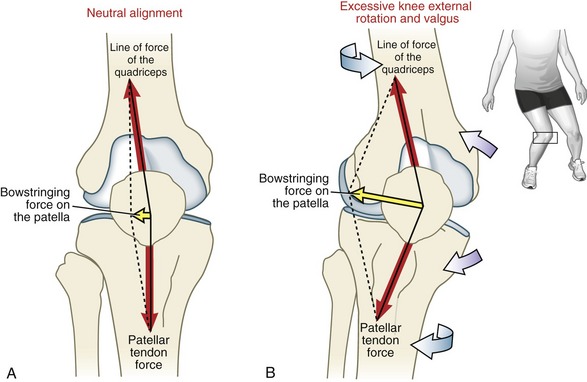
Local Factors: As previously introduced, the overall line of force of the quadriceps is indicated by the Q-angle (see Figure 13-29, A). Biomechanically, this net lateral pull of the quadriceps produces a lateral “bowstringing” force on the patella (Figure 13-30). As apparent by the vector addition in Figure 13-30, a larger Q-angle creates a larger lateral bowstringing force.102,220 A large lateral bowstringing force has the tendency to pull the patella laterally over a region of reduced contact area, thereby increasing the stress on its articular surfaces and potentially increasing the likelihood of dislocation.115
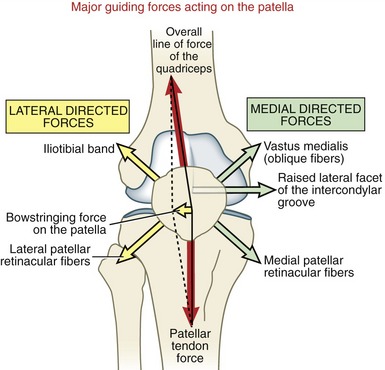
FIGURE 13-30. Highly diagrammatic and idealized illustration showing the interaction of locally produced forces acting on the patella as it moves through the intercondylar groove of the femur. Each force has a tendency to pull (or push in the case of the raised lateral facet of the intercondylar groove of the femur) the patella generally laterally or medially. Ideally, the opposing forces counteract one another so that the patella tracks optimally during flexion and extension of the knee. Note that the magnitude of the lateral bowstringing force is determined by the parallelogram method of vector addition (see Chapter 4). In theory, if the line of force of the quadriceps is collinear with the patellar tendon force, the lateral bowstringing force would be zero. Vectors are not drawn to scale.
As indicated in Figure 13-30, excessive tension in the iliotibial band or lateral patellar retinacular fibers can add to the natural lateral pull on the patella. Although the procedure is controversial, some surgeons perform a partial release of the lateral retinacular fibers in efforts to reduce excessive lateral tracking of the patella.55
Structures that oppose the lateral bowstringing force on the patella are shown on the right side of Figure 13-30. The lateral facet of the intercondylar groove is normally steeper than the medial facet (compare facets in Figure 13-23, D). This steeper slope naturally blocks, or at least resists, an approaching patella and thereby limits its excessive lateral shift.209 For a patella to laterally dislocate, it must traverse completely up and over this relatively steep slope. Researchers who experimentally flattened the lateral facet of the intercondylar groove on cadaver specimens report an average 55% loss in medial patellar stability across the tested knee range of motion; in other words, the patella could be shifted laterally with 55% less force than before the facet was flattened.238 The normally steep slope of the lateral facet of the intercondylar groove provides the single most important source of local resistance to excessive lateral translation of the patella. A dysplastic (or “shallow”) intercondylar groove may occur in otherwise healthy persons and is one of several recognized risk factors for excessive lateral tracking or chronic dislocation of the patella.153
The oblique fibers of the vastus medialis (frequently abbreviated as VMO) appear uniquely oriented to help balance the lateral pull exerted on the patella by the quadriceps muscle as a whole (review Figure 13-24). Selectively cutting fibers of the VMO in cadaver specimens produces an average 27% loss in medial patellar stability across the tested knee range of motion.4 This finding may be difficult to apply to clinical settings because it is extremely rare for a person to have isolated paralysis of the VMO. For decades, however, anecdotal evidence has suggested a preferential atrophy in the VMO in persons with chronic patellofemoral pain or history of chronic subluxation or dislocation, apparently from disuse or neurogenic inhibition.5 It is not certain, however, if the observed atrophy of the VMO is any more extreme than the atrophy often observed across the entire quadriceps muscle. Nevertheless, the suspicion of preferential atrophy or inhibition of the VMO has led to the development of multiple conservative treatments designed to selectively recruit, strengthen, or otherwise augment the action of this relatively small portion of the quadriceps. Although the biomechanical rationale for this approach is sound,50 the ability to selectively recruit and functionally strengthen one component of the quadriceps remains a controversial topic.*
Finally, the medial patellar retinacular fibers are oriented in medial-distal and medial directions (see Figure 13-7). The clinical and research literature often refers to these fibers as the medial patellofemoral ligament, which includes a broad but thin set of fibers interconnecting the medial patella, femur, tibia, medial meniscus, and undersurface of the VMO.3,17 This ligament is well known medically because it is usually ruptured after a complete lateral dislocation of the patella. Selectively cutting the medial patellofemoral ligament in cadaver specimens produces an average 27% loss in medial patellar stability across the tested knee range of motion.238 It is noteworthy that the loss in medial patellar stability increases sharply to 50% when the knee is in full extension.
The medial patellofemoral ligament is drawn most taut in the last 20 degrees of extension.3 Bicos and colleagues suggest that the ligament is pulled taut in extension with the aid of the activated VMO, to which the ligament partially attaches.17 These combined active and passive actions provide a useful source of medial stability to the patella at a point in the knee’s range of motion at which the patella is least stable because, in part, it is relatively disengaged from the bony “grip” of the intercondylar groove of the femur.
Global Factors: The magnitude of the lateral bowstringing force applied to the patella is strongly influenced by the frontal and horizontal plane alignment of the bones associated with the knee extensor mechanism. As a general principle, factors that resist excessive valgus or the extremes of axial rotation of the tibiofemoral joint favor optimal tracking of the patellofemoral joint. These factors are referred to as “global” in the sense that they are associated with joints distant to the patellofemoral joint, as far removed as the hip and the subtalar joint of the foot.
Excessive genu valgum can increase the Q-angle and thereby increase the lateral bowstringing force on the patella (compare Figure 13-31, A and B).173,211 If persistent, the lateral force on the patella can alter its alignment and thereby increase the stress at the patellofemoral joint. Increased valgus of the knee can occur from laxity of or injury to the MCL of the knee, but also indirectly from a chronic posture of the hip that involves increased adduction of the femur in an upright position.211 Weakness of the hip abductor muscles, tightness of the hip adductor muscles, or a condition of coxa vara (see Chapter 12) can allow the femur to slant excessively medially toward the midline during standing, thereby placing excessive tension on the medial structures of the knee—often a precursor to excessive valgus of the knee.107,162,255 Furthermore, excessive pronation (eversion) of the subtalar joint can, in some cases, create an excessive valgus load and posturing at the knee in a weight-bearing position. This issue is described in greater detail in Chapter 14.
As depicted in the drawing of the woman’s knee in Figure 13-31, B, excessive external rotation of the knee often occurs in conjunction with an excessive valgus load. External rotation of the knee places the tibial tuberosity and attached patellar tendon in a more lateral position relative to the distal femur.211 As shown by comparing Figure 13-31, A and B, excessive external rotation of the knee can also increase the Q-angle and thereby amplify the lateral bowstringing force on the patella.139,211 As indicated by the pair of blue arrows in Figure 13-31, external rotation of the knee can occur as a combination of femoral-on-tibial and tibial-on-femoral perspectives. Often, however, excessive external rotation of the knee is expressed in a weight-bearing position, as the femur is internally rotated relative to a fixed or nearly fixed lower leg. Persistent internal rotation posturing of the femur during weight-bearing activities may occur from reduced strength or neuromuscular control of the external rotator muscles of the hip,162,211,255 tightness of the hip internal rotator muscles, or as a compensation for excessive femoral anteversion (see Chapter 12)138 or excessive tibial (external) torsion. When weakness or poor control of the hip muscles is present, the posture of excessive hip internal rotation is often combined with varying amounts of hip adduction.107 Although this postural weakness can be subtle, it is often observed when a person is asked to slowly descend a step or assume a partial single-leg squat position. During this maneuver, the distal femur may be observed to “roll” inward slightly, despite conscious effort to resist this motion by activation of hip muscles.
Postural weakness of the hip external rotators and abductors is surprisingly common in otherwise normal and healthy females21,154,227 and is believed by many who study this phenomenon to be an important global factor that may increase the risk of developing patellofemoral joint pain and recurrent dislocation.98,107,125,275 Powers and colleagues used kinematic MRI to evaluate the patellofemoral kinematics in a group of young females with a history of patellofemoral joint pain.215 One component of the study instructed subjects to actively rise from a partial one-legged squat position, from 45 degrees of flexion to full knee extension. On average, the femurs of the extending hips rotated internally rather sharply throughout the last 20 degrees of full knee extension. On close individual analysis, images showed that the intercondylar groove of the femur rotated medially under the patella which was held fixed by the strong contraction of the quadriceps. Such femoral-on-patellar kinematics aligned the extensor mechanism and embedded patella more laterally and closer to the raised lateral facet of the intercondylar groove of the femur. This precarious alignment places the patella closer to a point of lateral subluxation or dislocation. These observations suggest that the pathomechanics of lateral patellofemoral dislocation can result from the femur dislocating medially under the patella, as well as the patella dislocating laterally over the femur, as is generally described.
Excessive internal rotation of the knee has also been suggested as a predisposing factor to patellofemoral joint pain.211 Although excessive internal rotation of the knee would theoretically decrease the Q-angle and associated lateral bowstringing force on the patella, it has been theorized that this posture could adversely alter the kinematics at the patellofemoral joint.139,231 Clinically, this issue is most often associated with the pathomechanics of excessive pronation of the subtalar joint in the early and mid-stance phase of walking.212 As will be described in Chapter 14, excessive pronation of the foot during this part of the gait cycle is usually mechanically coupled with excessive internal rotation of the leg.222 For this reason, the use of foot orthotics may be an appropriate treatment strategy for someone with patellofemoral pain syndrome.75,112
Evidence consistently suggests that females experience a greater incidence of abnormal kinematics and related pathology at the patellofemoral joint than males.57,263 Data collected at a large sports medicine clinic, for instance, showed that recurrent lateral dislocation of the patella accounted for 58.4% of all joint dislocations in women, compared with only 14% in men.44 It has been speculated that the gender bias in chronic patellar dislocation may in some persons be biomechanically associated with the 3 to 4 degrees of greater Q-angle often measured in females.100 A greater Q-angle may reflect a greater pelvic width–to–femoral length ratio in females.195 Whether the apparent greater Q-angle in females (and assumed greater lateral bowstringing force on the patella) alters patellar tracking and stress to a point of actually causing an increased incidence in dislocation and pain is difficult to prove, although this is an important and logical point to consider.84
Summary: Table 13-6 provides a list of potential indirect and direct causes of excessive lateral tracking of the patella. Although many of the causes listed in Table 13-6 are described as separate entities, in reality many occur in combinations. Clinical evaluation of persons with patellofemoral joint pathology must therefore consider several potential interrelated factors that can contribute to the problem. Much more clinical research is needed in this area to improve the conservative and surgical treatment of patellofemoral joint pain and chronic dislocation.
KNEE FLEXOR-ROTATOR MUSCLES
With the exception of the gastrocnemius, all muscles that cross posterior to the knee have the ability to flex and to internally or externally rotate the knee.25 The so-called flexor-rotator group of the knee includes the hamstrings, sartorius, gracilis, and popliteus. Unlike the knee extensor group, which is innervated by the femoral nerve, the flexor-rotator muscles have three sources of innervation: femoral, obturator, and sciatic.
Functional Anatomy: The hamstring muscles (i.e., semimembranosus, semitendinosus, and long head of the biceps femoris) have their proximal attachment on the ischial tuberosity. The short head of the biceps has its proximal attachment on the lateral lip of the linea aspera of the femur. Distally, the hamstrings cross the knee joint and attach to the tibia and fibula (see Figures 13-9 to 13-10).
The semimembranosus attaches distally to the posterior side of the medial condyle of the tibia. Additional distal attachments of this muscle include the MCL, both menisci, the oblique popliteal ligament, and the popliteus muscle. For most of its course, the sinewy semitendinosus tendon lies posterior to the semimembranosus muscle. Just proximal to the knee, however, the tendon of the semitendinosus courses anteriorly toward its distal attachment on the anterior-medial aspect of tibia. Both heads of the biceps femoris attach primarily to the head of the fibula, with lesser insertions to the lateral collateral ligament, lateral capsule of the knee, and lateral tubercle of the tibia.232,258
All hamstring muscles, except the short head of the biceps femoris, cross the hip and knee. As described in Chapter 12, the three biarticular hamstrings are very effective hip extensors, especially in the control of the position of the pelvis and trunk over the femur.
In addition to flexing the knee, the medial hamstrings (i.e., semimembranosus and semitendinosus) internally rotate the knee. The biceps femoris flexes and externally rotates the knee. Active axial rotation in either direction is freest with the knee partially flexed. This axial rotation action of the hamstrings can be appreciated by palpating the tendons of semitendinosus and biceps femoris behind the knee as the leg is actively internally and externally rotated repeatedly. This is performed while the subject sits with the knee flexed 70 to 90 degrees. As the knee is gradually extended, the pivot point of the rotating lower leg shifts from the knee to the hip. At full extension, active rotation at the knee is restricted because the knee is mechanically locked and most ligaments are pulled taut. Furthermore, the moment arm of the hamstrings for internal and external rotation of the knee is reduced significantly in full extension.25
The sartorius and gracilis have their proximal attachments on different parts of the pelvis (see Chapter 12). At the hip, both muscles are hip flexors, but they have opposite actions in the frontal and horizontal planes. Distally, the tendons of the sartorius and gracilis travel side by side across the medial side of the knee to attach to the proximal shaft of the tibia, near the semitendinosus (see Figure 13-10). The three juxtaposed tendons of the sartorius, gracilis, and semitendinosus attach to the tibia using a common, broad sheet of connective tissue known as the pes anserinus. As a group the “pes muscles” are effective internal rotators of the knee. Connective tissues hold the tendons of the pes group just posterior to the medial-lateral axis of rotation of the knee. The three pes muscles therefore flex and internally rotate the knee.
The pes anserinus group adds significant dynamic stability to the medial side of the knee.174 Along with the MCL and posterior-medial capsule, active tension in the pes muscles resists knee external rotation and valgus loads applied to the knee.
The popliteus is a triangular muscle located deep to the gastrocnemius within the popliteal fossa (see Figure 13-9). By a strong intracapsular tendon, the popliteus attaches proximally to the lateral condyle of the femur, between the lateral collateral ligament and the lateral meniscus (see Figures 13-8 and 13-11). The popliteus is the only muscle of the knee that attaches within the capsule of the knee joint. More distally, the popliteus has an extensive attachment to the posterior side of the tibia. Fibers from the popliteus attach to the lateral meniscus and blend with the arcuate popliteal ligament.
The anatomy and action of the gastrocnemius and plantaris are considered in Chapter 14.
Group Action of Flexor-Rotator Muscles: Many of the overall functions of the flexor-rotator muscles of the knee are expressed during walking and running activities. Examples of these functions are considered separately for tibial-on-femoral and femoral-on-tibial movements of the knee.
Control of Tibial-on-Femoral Osteokinematics: An important action of the flexor-rotator muscles is to accelerate or decelerate the lower leg during the swing phase of walking or running. Typically, these muscles produce relatively low-to-moderate forces but at relatively high shortening or lengthening velocities. One of the more important functions of the hamstring muscles, for example, is to decelerate the advancing lower leg at the late swing phase of walking. Through eccentric action, the muscles help dampen the impact of full knee extension. Consider also sprinting or rapidly walking. These same muscles rapidly contract to accelerate knee flexion in order to shorten the functional length of the lower limb during the swing phase.
Control of Femoral-on-Tibial Osteokinematics: The muscular demand needed to control femoral-on-tibial motions is generally larger and more complex than that needed to control most ordinary tibial-on-femoral knee motions. A muscle such as the sartorius, for example, may have to simultaneously control up to five degrees of freedom (i.e., two at the knee and three at the hip). Consider the action of several knee flexor-rotator muscles while one runs to catch a ball (Figure 13-32, A). While the right foot is firmly fixed to the ground, the right femur, pelvis, trunk, neck, head, and eyes all rotate to the left. Note the diagonal flow of activated muscles between the right fibula and left side of the neck. The muscle action epitomizes intermuscular synergy. In this case the short head of the biceps femoris anchors the bottom of the diagonal kinetic chain to the fibula. The fibula, in turn, is anchored to the tibia via the interosseous membrane and other muscles.
Stability and control at the knee require interaction of forces produced by surrounding muscles and ligaments. Interaction is especially important for control of high-velocity movements in the horizontal and frontal planes. To illustrate, refer to Figure 13-32, B. With the right foot planted, the short head of the biceps femoris accelerates the femur internally. By way of eccentric activation, the pes anserinus muscles help decelerate the internal rotation of the femur over the tibia. The pes anserinus group may be regarded as a “dynamic medial collateral ligament” by resisting not only the external rotation of the knee but also any valgus loads. The pes group of muscles may help compensate for a weak or lax MCL or posterior-medial capsule. Although not depicted in Figure 13-32, B, eccentric activation of the popliteus can assist the pes group with decelerating external rotation of the knee.135,232
Maximal Torque Production of the Knee Flexor-Rotator Muscles: Maximal-effort knee flexion torque is generally greatest with the knee in the last 20 degrees of full extension and then declines steadily as the knee is progressively flexed.130,251 A representative plot of published torque data from healthy males is shown in Figure 13-33.251 Subjects produced maximal-effort isometric knee flexion torque with hips held in extension. Although a wide range of values have been reported, in general the hamstrings have their greatest flexor moment arm (leverage) at 50 to 90 degrees of knee flexion (see bar on horizontal axis in graph of Figure 13-33).24,118,147,191,251 The torque-angle data depicted in Figure 13-33 clearly indicate that the hamstrings (and presumably other knee flexors) generate their greatest torque at knee angles that coincide with relative elongated muscle length, rather than high leverage. (As noted in Figure 13-26, this is in slight contrast to the quadriceps, where maximal-effort knee extensor torque partially overlaps the point in the range of motion where leverage is greatest.) Flexing the hip to elongate the hamstrings promotes even greater knee flexion torque.20 The length-tension relationship appears to be a very influential factor in determining the flexion torque potential of the hamstring muscles.118
Few data are available on the maximal torque potential of the internal and external rotator muscles of the knee. When tested isokinetically with the knee flexed to 90 degrees, the internal and external rotators at the knee have been shown to produce nearly equal peak torques.8 At first thought, these results may be surprising considering the far greater number of internal rotator muscles compared with just one external rotator muscle at the knee (i.e., the biceps femoris). The apparent conflict can be partially reconciled by the fact that, with the knee flexed to 90 degrees, the biceps femoris muscle has a threefold greater axial rotation moment arm than the average of all the internal rotators.25 The laterally displaced distal attachment of the biceps femoris to the head of the fibula apparently augments this muscle’s rotational leverage.
The average axial rotation leverage for virtually all rotators of the knee is greatest between 70 and 90 degrees of knee flexion, where the muscles’ line of force is nearly perpendicular to the longitudinal (vertical) axis of rotation through the tibia.25 The only exception to this design is the popliteus muscle, which has its greatest moment arm to internally rotate the knee at about 40 degrees of flexion.
Abnormal Alignment of the Knee
Genu Varum with Unicompartmental Osteoarthritis of the Knee: During walking at normal speeds across level terrain, the joint reaction force at the knee reaches about 2.5 to 3 times body weight.243,283 This force is created by the combined effect of muscle activation and the ground reaction force. During the loading (early) phase of the gait cycle, the ground reaction force normally passes just lateral to the heel, then upward and medial to the knee as it continues toward the center of gravity of the body as a whole.104 As depicted in Figure 13-34, by passing medial to an anterior-posterior axis at the knee, the ground reaction force produces a varus torque at the knee with every step.61,94 As a result, joint reaction force at the knee during walking is normally several times greater on the medial joint compartment than on the lateral joint compartment (see inset in Figure 13-34).244 Throughout one’s lifetime, this repetitive varus loading is partially absorbed by tension in lateral structures at the knee, such as the lateral collateral ligament and iliotibial band.
Most persons tolerate the asymmetrical dynamic loading of the knee with little or no difficulty. In some persons, however, the asymmetry may lead to excessive wear of the articular cartilage, ultimately leading to (medial) unicompartmental osteoarthritis.47,239 A 20% increase in peak varus torque at the knee during walking has been shown to be associated with a sixfold increase in the risk of developing medial compartment knee osteoarthritis.172 Thinning of the articular cartilage and meniscus on the medial side can tilt the knee into genu varum, or a bow-legged deformity (Figure 13-35, A). A vicious circle may develop: the varus deformity increases medial joint compartment loading, resulting in greater loss of medial joint space, causing greater varus deformity, and so on. Figure 13-35, B is an anterior view x-ray film showing bilateral genu varum. Both knees show signs of medial joint osteoarthritis (i.e., loss of medial joint space and hypertrophic reactive bone around the medial compartment). Management of severe genu varum often involves surgery, such as a high tibial (wedge) osteotomy. The goal of this surgery is to correct the varus deformity and reduce the stress over the medial joint compartment (Figure 13-35, C). In addition to surgery, foot orthoses, valgus knee bracing, reduced walking velocity, and the use of a cane held in the contralateral hand have all been shown to reduce stress on the medial side of the knee.180,244 A laterally wedged insole worn within the shoe typically produces a valgus torque on the knee during the stance phase. This, in turn, reduces the net varus torque at every step, which reduces the compression load on the medial joint compartment of the knee.94,122,244 This relatively simple orthotic approach has been shown to reduce pain and improve function in persons with medial compartment osteoarthritis.38,94
Excessive Genu Valgum: Several factors can lead to excessive genu valgum, or knock-knee (Figure 13-36). These include previous injury, genetic predisposition, high body mass index, and laxity of ligaments. Genu valgum may also result from or be exacerbated by abnormal alignment or muscle weakness at either end of the lower extremity. As indicated in Figure 13-36, coxa vara (i.e., a femoral neck-shaft angle less than 125 degrees) or weakened hip muscles (such as the gluteus medius) can, at least in theory, increase the valgus load on the knee. In some cases excessive foot pronation may increase the valgus load on the knee by allowing the distal end of the tibia to slant (“abduct”) farther away from the midline of the body. Over time, the tensional stress placed on the MCL and adjacent capsule may weaken the tissue. As described earlier in this chapter, excessive valgus of the knee may negatively affect patellofemoral joint tracking and create additional stress on the ACL.
Standing with a valgus deformity of approximately 10 degrees greater than normal directs most of the joint compression force to the lateral joint compartment.111 This increased regional stress may lead to lateral unicompartmental osteoarthritis.47,239 Knee replacement surgery may be indicated to correct a valgus deformity, especially if it is progressive, is painful, or causes loss of function. Figure 13-37, A and B show severe bilateral osteoarthritis of the knee, with severe genu valgum on the right and genu varum on the left. This “wind-swept” deformity was corrected surgically with bilateral knee replacements (see Figure 13-37, C).
SAGITTAL PLANE
Genu Recurvatum: Full extension with slight external rotation is the knee’s close-packed, most stable position. The knee may be extended beyond neutral an additional 5 to 10 degrees, although this is highly variable among persons. Standing with the knee in full extension usually directs the line of gravity from body weight slightly anterior to the medial-lateral axis of rotation at the knee. Gravity, therefore, produces a slight knee extension torque that can naturally assist with locking of the knee, allowing the quadriceps to relax intermittently during standing. Normally this gravity-assisted extension torque is resisted primarily by passive tension in the stretched posterior capsule and stretched flexor muscles of the knee, including the gastrocnemius.