47
Keratodermas
• Three major types of involvement.
– Diffuse PPK: confluent over the entire palmoplantar surface; onset by early childhood in hereditary forms, with initial erythema evolving into thick, yellow hyperkeratosis that may be waxy or verrucous (Fig. 47.1).

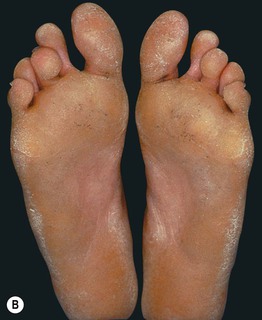

Fig. 47.1 Diffuse palmoplantar keratoderma. A Non-epidermolytic keratoderma with sharp demarcation at the wrist and side of the thumb. B Non-epidermolytic keratoderma with greater thickness in sites of pressure. C Epidermolytic keratoderma with prominent erythema at the border. In general, epidermolytic and non-epidermolytic forms cannot be distinguished clinically. A, Courtesy, Julie V. Schaffer, MD; B, C, Courtesy, Alfons L. Krol, MD, and Dawn Siegel, MD.
– Focal PPK: primarily in areas of friction or pressure; the areata/nummular (oval) pattern affects the soles (Fig. 47.2A) > palms; the striate (linear) pattern extends from the palms to the volar fingers (Fig. 47.2B).


Fig. 47.2 Focal palmoplantar keratoderma. A Areata type on the soles. B Striate type on the palm. A, Courtesy, Alfons L. Krol, MD, and Dawn Siegel, MD.
– Punctate PPK: small (≤1 cm) keratotic papules on the palms and soles; onset is usually in adolescence or early adulthood, with initial pinhead-sized translucent papules that may become larger and callus-like (Fig. 47.3).


Fig. 47.3 Punctate palmoplantar keratoderma. Keratotic papules, some coalescing to form plaques, on the palm (A) and sole (B). A, Courtesy, Kalman Watsky, MD.
• Other possible features include hyperhidrosis, an erythematous border (see Fig. 47.1C), extension beyond the palmoplantar skin (e.g. onto dorsal hands/feet; ‘transgrediens’), digital constriction bands (pseudoainhum; see Fig. 47.4B), and the histologic finding of epidermolytic hyperkeratosis (‘epidermolytic PPK’).

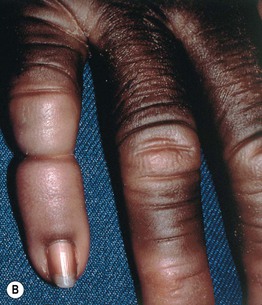

Fig. 47.4 Palmoplantar keratoderma associated with deafness due to connexin 26 mutations. A Diffuse ‘honeycombed’ keratoderma on the sole. B Pseudoainhum formation in Vohwinkel syndrome, which can also feature ‘starfish’ keratoses on the knuckles. C Leukonychia and knuckle pads in Bart–Pumphrey syndrome. A, C, Courtesy, Alfons L. Krol, MD, and Dawn Siegel, MD.
• Table 47.1 outlines major forms of PPK, either isolated or associated with additional cutaneous and extracutaneous manifestations (Figs. 47.4–47.11; Table 47.2).
Table 47.1
Major forms of palmoplantar keratoderma (PPK).
The most common types in children and adults are shaded pink and blue, respectively. Selected genetic etiologies are in parentheses.
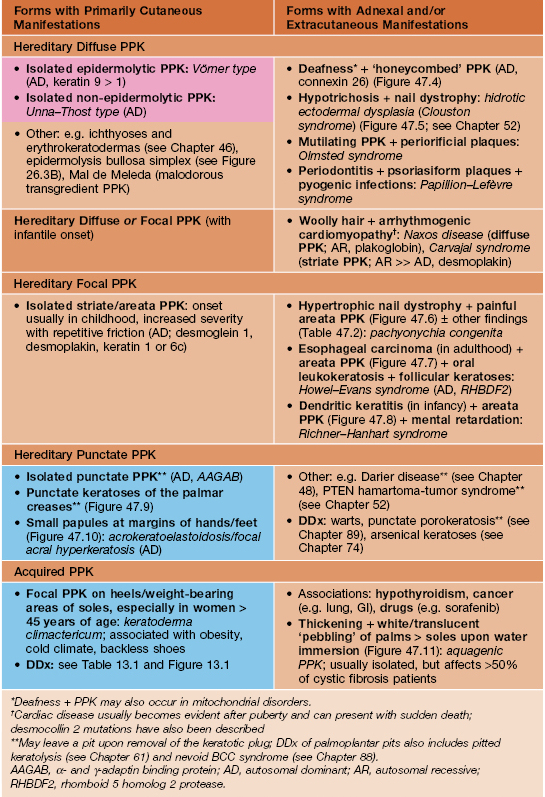

Fig. 47.5 Hidrotic ectodermal dysplasia (Clouston syndrome). Note the ‘pebbled’ skin on the dorsal aspect of the toes as well as the dystrophic nail plates. Courtesy, D. Sasseville, MD, and R. Wilkinson, MD.


Fig. 47.6 Pachyonychia congenita. A Painful focal plantar keratoderma with associated erythema and blistering. B Thickening of palmar skin and hypertrophic nail dystrophy with wedge-shaped subungual hyperkeratosis. A, Courtesy, Alfons L. Krol, MD, and Dawn Siegel, MD.

Fig. 47.7 Howel–Evans syndrome. Focal palmoplantar keratoderma, usually with onset at 5–15 years of age, associated with development of carcinoma of the esophagus in adulthood. Courtesy, Alfons L. Krol, MD, and Dawn Siegel, MD.

Fig. 47.8 Richner–Hanhart syndrome (tyrosinemia II). Focal painful keratoses on the plantar surface in a patient with corneal ulcers and mental retardation. In this disorder, the onset of keratoderma ranges from early childhood to adolescence. Courtesy, Jean L. Bolognia, MD.

Fig. 47.10 Focal acrokeratoelastoidosis. Multiple skin-colored papules at the margin of the palmar skin.

Fig. 47.11 Aquagenic keratoderma. White ‘pebbly’ changes on the palm following immersion in water for a few minutes in a healthy teenage girl. Courtesy, Julie V. Schaffer, MD.
Table 47.2
Clinical features of pachyonychia congenita (PC).
++, present in majority of patients; + present in minority of patients. PC-6a/16 and PC-6b/17 are caused by mutations in the genes encoding keratin 6a or 16 and keratin 6b or 17, respectively.
| Feature | PC-6a/16 (Formerly PC-1) | PC-6b/17 (Formerly PC-2) |
| Painful focal palmoplantar keratoderma* (Fig. 47.6A) | ++ | ++ |
| Hypertrophic nail dystrophy† (Fig. 47.6B) | ++ | ++ |
| Oral leukokeratosis | ++ | + |
| Follicular keratoses | ++ | ++ |
| Steatocystoma multiplex and vellus hair cysts | + (uncommon) | ++ |
| Natal/prenatal teeth | – | + (primarily in PC-17) |
| Pili torti/other hair abnormalities** | + (uncommon) | + |
* Soles (median onset at age 2 years) > palms; hyperhidrosis is common, and acral blistering may occur.
† Wedge-shaped subungual hyperkeratosis as well as thickened, omega-shaped nail plates.
** For example, coarse, brittle, and/or curly hair.
For further information see Ch. 58. From Dermatology, Third Edition.








