Chapter 21 Intubating Introducers, Stylets, and Lighted Stylets (Lightwands)
I Introduction
The procedure of placing an endotracheal tube (ETT) in the trachea for ventilation and oxygenation is more than a thousand years old. It was first performed on pigs by the Persian physician, Avicenna, between 980 and 1037 AD.1,2 Blind digital intubation in humans was first described in 1796 by Herholdt and Rafn in a resuscitation protocol for drowning victims.3 In 1880, Macewen described blind digital intubation in awake patients using a curved metal tube.4 However, modern methods of laryngoscopic endotracheal intubation did not emerge until early in the 20th century, after the introduction of a flexible metal tube by Kuhn5 and of the laryngoscope by Jackson.6
Over the years, direct laryngoscopic intubation has been shown to be an effective, safe, and relatively easy technique. In fact, using a laryngoscope to obtain line of sight to the laryngeal inlet has become the standard method of endotracheal intubation in the operating room, the intensive care unit, and the emergency department. However, even in the hands of experienced laryngoscopists, accurate and prompt placement of the ETT remains a significant challenge in some patients. This is particularly true in “unprepared” patients and in patients requiring emergency intubation. With any standard laryngoscope, obtaining line of sight to the patient’s larynx can prove difficult in the presence of specific anatomic variations such as a receding mandible, prominent upper incisors, a restricted mouth opening, or limited movement of the cervical spine. It has been estimated that 1% to 3% of surgical patients have a so-called difficult airway (DA), making laryngoscopic intubation problematic and sometimes impossible.7 In the obstetric population, the incidence of failed laryngoscopic intubation has been reported to be 0.05% to 0.35%.8 Many predictors of difficult laryngoscopy (DL) have been suggested in the literature,9,10 but the sensitivity and specificity of these tests remain relatively low.11–13 Therefore, all clinicians must be prepared to deal with the prospect of both anticipated and unanticipated DLs.
II Intubating Introducers and Stylets
A History
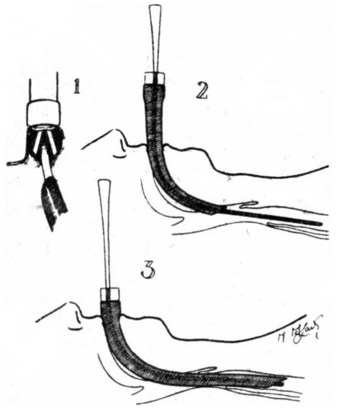
Intubating guides or introducers were first reported in the late 1940s. In 1949, Macintosh described “the use of a gum elastic introducer as an aid to passing endotracheal tubes” (Fig. 21-1) as follows14:
B The Eschmann Introducer
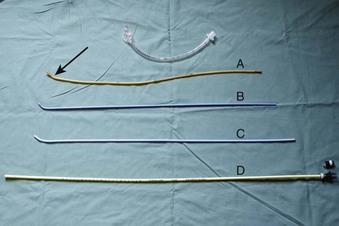
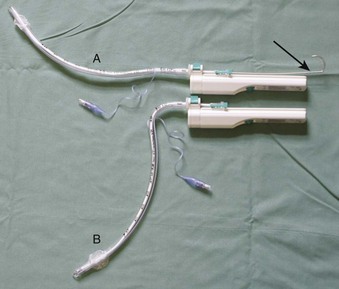
Use of an introducer in this fashion did not become widespread until the development of the Eschmann Introducer (EI) by Venn in 1973. Venn’s design has several key features. First, it is relatively long at 60 cm (Fig. 21-2), allowing one to place the introducer between the cords before “railroading” the ETT over its distal end. It has been suggested that a naked introducer affords better dexterity and tactile sensation to the user compared with an introducer on which an ETT has been preloaded.15 Second, the EI has a coudé tip (a 40-degree bend) for “hooking” under the epiglottis. The material from which the EI is made—a combination of a polyester core and resin covering—no doubt has contributed to its success.15 The EI is malleable, firm enough to direct, yet flexible enough to yield on contact. Furthermore, it is a multiuse device that can be sterilized between uses. The EI is commonly referred to as a “gum elastic bougie” despite not being made of gum, having no elastic properties, and not being a “bougie” at all (a bougie being a dilating device).16,17 The EI is currently sold under the name “Portex Venn Introducer” (Smiths Medical, UK.)
Although an EI can be used to direct the ETT toward an “anterior” or narrow larynx, its real strength lies as a tool to facilitate intubation when the laryngeal aperture cannot be seen during laryngoscopy (e.g., Cormack-Lehane grade 3 view).18 If the epiglottis cannot be visualized at all (i.e., Cormack-Lehane grade 4 view), we do not recommend use of the EI, because the likelihood of successful intubation with the EI is unacceptably low. In cases in which the epiglottis can be seen, the coudé tip can be hooked under the epiglottis and the EI advanced blindly through the glottis. The success of this maneuver is improved if the EI has been preshaped into a curve.19 As the introducer is advanced further, the tracheal “clicks” are felt approximately 90% of the time if the EI is correctly placed,20 whereas no “clicks” will be observed if the EI has been advanced into the esophagus. We believe that “clicks” are more likely to be perceived if, once the tip of the EI is through the cords, the introducer is advanced at a shallow angle relative to the patient. This maneuver is intended to ensure that the tip of the introducer will contact the cartilaginous rings on the anterior tracheal wall as it advances, producing the “clicking” sensation. One can imagine that “clicks” are less likely to be felt if the only contact between the trachea and the EI is the coudé bend in the introducer that is sliding along the posterior tracheal wall, or even along the trachealis muscle.
Additional clues to confirm correct tracheal placement include the perception that the EI slightly deviates to the right as it advances into the right main bronchus and a “hold up” felt at the 30- to 35-cm mark as the EI becomes lodged in a distal airway (reportedly a 100% reliable sign).20 In contrast, if the EI is placed in the esophagus, the entire EI could be advanced without encountering any resistance, although theoretically it would be possible for a pharyngeal pouch to hold up the introducer if one were present.21 Some authors have cautioned against the use of the hold-up sign, believing that it increases the risk of airway trauma. If clicks are felt, then the hold-up test is not required.20
After tracheal placement, the ETT is advanced distally over the EI into the trachea. A jaw lift-jaw thrust by the nondominant hand of the clinician or by a laryngoscope will facilitate the advancement of the ETT over the EI by elevating the tongue and epiglottis. If difficulty persists while the ETT is being advanced, rotating the ETT 90 degrees counterclockwise will turn its bevel posteriorly and minimize the risk of catching on the structures of the glottic opening.22 After intubation, the position of the ETT is confirmed by conventional methods such as measurement of the end-tidal carbon dioxide concentration (EtCO2) and auscultation.
The EI is long enough to be useful for nasal intubations and can also be used to place supralaryngeal airways (SLAs) or double-lumen tubes.23 The long length of the EI enables it to be used as an airway exchange device; it can be placed down the lumen of a correctly placed ETT or SLA, which can then be removed over the introducer and discarded before a new airway is “railroaded” in its place. During the whole maneuver, the EI remains within the trachea, thereby guiding correct placement of the new airway. After the EI is removed, as always, the position of the new airway should be confirmed with the use of standard methods.
C Other Types of Intubating Guides
Many intubating guides of different sizes, shapes, lengths, and materials have been developed. All of the designs serve a function similar to that of the EI, but many have some additional features. Some are single-use devices that were designed after concern was raised regarding the possibility of prion transfer between patients with multiuse airway equipment. However, there is growing skepticism about whether disease transfer from reused but sterilized medical instruments poses any tangible risk to patients, whereas the risk to patients from the use of suboptimal airway equipment with limited clinical evaluation is very real. Clinicians should be wary of new equipment and always insist on using only instruments that have proved to be effective and safe.24
1 Frova Intubation Introducer
The Frova Intubation Introducer (Cook Inc., Bloomington, IN) is a single-use introducer, firmer than the EI, that has a 35-degree coudé tip, two side ports, and a hollow lumen (see Fig. 21-2). It comes with a Rapi-Fit connector that connects directly to standard ventilatory equipment, such as the bag of an air-mask-bag unit (AMBU) or an anesthetic circuit, enabling the Frova to also serve as a conduit for O2 delivery or ventilation. This requires extreme caution however, because high-pressure source ventilation via the narrow lumen may result in severe barotrauma. The Frova may be connected to an esophageal detection device so that one can confirm correct placement before “railroading” the ETT.25 The rigid, removable internal cannula is designed to increase the stiffness of the Frova; it has limited clinical indication and may increase the risk of trauma. The Frova introducer has two sizes: a 65-cm-long blue adult version for ETTs with greater than 5.5 mm inner diameter (ID) and a 33-cm-long yellow pediatric version for ETTs with 3.0 to 5.0 mm ID. First-pass success rates with the Frova introducer are similar to those with the EI and are substantially better than those of the similarly shaped Portex introducer.26 It is presumed that this success is due to the increased malleability of the EI and the Frova, which enables preshaping of the device, compared with the Portex introducer.26
2 Endotracheal Tube Introducer
The Endotracheal Tube Introducer (Sun Med, Largo, FL) is an example of a single-use version of the EI (see Fig. 21-2). It is similar to the EI in size and shape but 10 cm longer (i.e., 70 cm long). Like the Frova, it is stiffer than the EI. There are 10-cm markings on the top of the Sun Med introducer to indicate the depth of insertion. Although it is marketed as a single-use, disposable device, resterilization is possible.
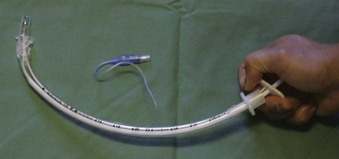
3 Parker Flex-It Directional Stylet
The Schroeder Oral/Nasal Directional Stylet, also known as the Parker Flex-It Directional Stylet (Parker Medical, Englewood, CO), is a disposable articulating stylet that requires no bending before intubation. Inserting the stylet into an ETT allows the clinician to elevate the tip of the ETT by wrapping all four fingers around the proximal ETT and using the base of thumb to depress the proximal end of the stylet (Fig. 21-3). Although the stylet is suitable for both oral and nasal intubation, it has been reported to be somewhat awkward to use, and the curvature created is not at the tip but rather over the distal half of the tube.27 However, it has been reported to be effective for difficult intubations (DIs) as well as for blind intubations.28
The effectiveness of intubating guides in patients with a DA has been well established.29–31 Most of these studies used the EI. With only a few exceptions, there are currently few data to support the use of the newer introducers for endotracheal intubation, particularly in patients with a history of DA. It should be emphasized that most of these new intubating guides and stylets are disposable and designed for single-use. In contrast, the EI is more cost-effective because it is reusable.
D Tube Exchangers
1 Cook Airway Exchange Catheter
The Cook Airway Exchange Catheter (CAEC; Cook Critical Care, division of Cook Inc.) is a hollow, flexible, straight tube that is designed as a tube exchanger for patients with a DA. The CAEC can be used to ventilate patients under difficult circumstances through the inner lumen and the distal ports after fitting the provided adaptor at the proximal end (see Fig. 21-2).
E Stylets
A stylet is a plastic-coated metal rod that can be placed inside the lumen of an ETT before intubation to stiffen or preshape the ETT. Unlike the EI and other introducers, the stylet should not protrude past the tip of the ETT, so as to avoid unnecessary trauma. Water-based lubricant should be used, and easy passage of the stylet in and out of the ETT should be demonstrated before use. The “best” shape for a stylet-shaped ETT depends on the clinician’s preference and the patient’s position and anatomy. However, Levitan and colleagues showed that the line of sight to the larynx can be improved if the stylet remains “straight to cuff,”32 at which point the ETT can then be bent to the desired angle (i.e., shaped like a hockey stick) (Fig. 21-4). An angle of 35 degrees or less reduces the risk of traumatic injury.32 Once the ETT has passed through the vocal cords, the stylet should be withdrawn as the ETT is advanced into the trachea.
In a randomized trial, Gataure and associates compared the efficacy of the EI with that of the malleable stylet in 100 patients with simulated DL (Cormack-Lehane grade 3 view) under general anesthesia. The EI group had a success rate of 96% after two attempts, compared with 66% in the stylet group.33
F Complications
Despite long-standing and widespread use, complications caused by ETT introducers, tube exchangers, and stylets are rare. To date, there have been only half a dozen case reports of pharyngeal, laryngeal, or tracheal perforation during airway manipulation that may have been caused by introducers or stylets.34,35 Reports of trauma during airway management frequently come from cases in which multiple attempts at securing the airway occurred and multiple devices were used, making it difficult to attribute damage to a single device. Because of their firmer material, single-use ETT introducers exert more pressure at the tip compared with the multiuse EI.26 Whether this corresponds to greater risk of airway trauma remains unknown.25 However, as with all airway devices, undue force should always be avoided. Holding an ETT introducer close to the coudé tip (i.e., with Magill’s forceps) increases the pressure exerted at the tip and therefore is not recommended.
After endotracheal intubation, all introducers and stylets should be inspected to ensure that no part of the device has been left behind. One report described a case in which the tip of an EI became detached and lodged in a patient’s airway,36 and in a similar case, plastic coating peeled off a stylet, blocking the ETT.37 An unusual case report described the involution of an ETT at its tip while the EI was being withdrawn, which caused the EI to lodge firmly within the ETT and necessitated removal of both instruments.38 Routine generous lubrication of intubating guides should reduce the likelihood of such events.
G Clinical Utility
Intubating introducers, stylets, and tube exchangers have been used successfully to facilitate endotracheal intubation for many decades. In particular, the EI is a cheap, reliable, and familiar tool in the hands of anesthesia practitioners and, more recently, those of emergency physicians and in the prehospital setting.39–42 Although the popularity of these nonvisual intubating techniques may decrease because of the improved glottic view afforded by the new video laryngoscopes, studies report the efficacy and usefulness of stylets and introducers to assist videoscopic intubation,43–48 suggesting that these instruments will remain a mainstay of intubating adjuncts.
III Lighted Stylets
A History
Macintosh and Richards are frequently credited with being the first to use a lighted stylet for orotracheal intubation. In 1957, they reported the use of a lighted introducer to assist the placement of an ETT in the trachea under direct vision using a laryngoscope.49 However, they did not describe the technique whereby transillumination of the soft tissues of the neck is used to guide the placement of the ETT. This transillumination technique was likely first described by Yamamura and colleagues, who reported the use of a lighted stylet for nasotracheal intubation in 1959.50
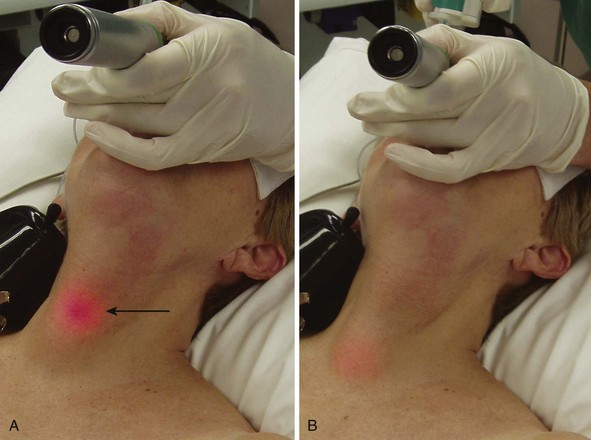
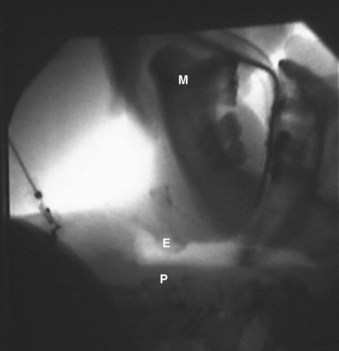
Modern lighted stylets use the principle of transillumination of the soft tissues of the anterior neck to guide the tip of the ETT into the trachea. This method takes advantage of the anterior (superficial) location of the trachea relative to the esophagus. When the tip of the ETT with the lighted stylet enters the glottic opening, a well-defined, circumscribed glow can be readily seen slightly below the thyroid prominence (Fig. 21-5A). However, if the tip of the ETT is in the esophagus, the transmitted glow is diffuse and cannot be readily detected under ambient lighting conditions (see Fig. 21-5B). If the tip of the ETT is placed in the vallecula, the light glow is diffuse and appears slightly above the thyroid prominence. Using these landmarks and principles, the clinician can guide the tip of the ETT easily and safely into the trachea without the use of a laryngoscope.
Despite its potential clinical advantages, intubation using a lighted stylet (lightwand) did not receive widespread popularity until a commercial intubating device became available. During the past 30 years, several versions of a lighted stylet have been introduced, including the Fiberoptic Lighted-Intubation Stilette (Benson Medical Industries Inc., Markham, Ont., Canada), the Flexilum (Concept Corporation, Clearwater, FL), the Tubestat (Concept Corporation), and the Fiberoptic Lighted Stylet (Fiberoptic Medical Products, Inc., Allentown, PA) (Fig. 21-6). Over the years, these devices have proved to be effective and safe in placing the ETT both orally and nasally.51–53 Despite favorable results and growing experience with the technique of light-guided intubation,51–54 early commercial lighted stylets had some limitations. These included: (1) poor light intensity; (2) short length, which limited the use of the lighted stylet device to short or cut ETTs; (3) absence of a connector to secure the ETT to the lighted-stylet device; (4) rigidity of the lighted stylet, which hampered use of the devices for other intubating techniques, including light-guided nasal intubation; and (5) single-use design in most lighted stylets, which increased the cost of intubation.
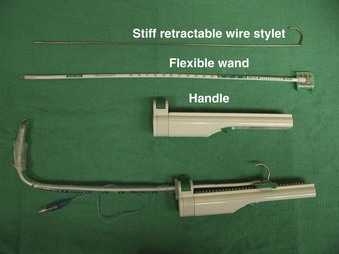
B Trachlight
The Trachlight consists of three parts: a reusable handle, a flexible wand, and a retractable metal wire stylet (Fig. 21-7). The power control circuitry and 3 AAA batteries are encased within the handle. The stylet or “wand” consists of a durable, flexible plastic shaft with a bright light bulb affixed at the distal end. Enclosed within the wand is a stiff but malleable, retractable wire stylet. This stylet may well be the most important feature of this device, because it significantly improves its ease of use.
A major feature of the Trachlight is its improved light source, which in most cases permits intubation under ambient lighting conditions. After 30 seconds of illumination, the light bulb blinks to minimize heat production and provide a convenient reminder of elapsed time. Because the tip of the stylet is encased within the ETT, and because of the efficient heat-exchange capacity of the upper airway mucosa, it is extremely unlikely that heat from the bulb would cause any thermal injury during intubation. An animal study confirmed that there were no histopathologic changes after use of the Trachlight.55
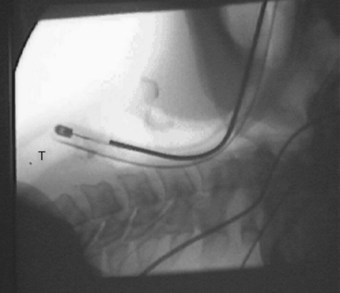
For standard orotracheal intubation, the retractable wire stylet is best used to shape the ETT into the form of a field-hockey stick (see Fig. 21-7). This configuration directs the bright light of the bulb against the anterior wall of the larynx and trachea. In addition, the hockey-stick configuration enhances maneuverability during intubation and facilitates placement of the ETT through the glottic opening. However, this is an awkwardly shaped object to advance into the trachea. Therefore, once the tip of the ETT-Trachlight (ETT-TL) unit has passed through the glottic opening, the wire stylet should be retracted by approximately 10 cm. This makes the distal end of the ETT-TL unit pliable and enables advancement into the trachea safely and without difficulty.
The glow emitted from the Trachlight can be seen to migrate down the patient’s neck and may be used to confirm correct placement of the ETT. When the glow reaches the sternal notch, the tip of the ETT is located about halfway between the vocal cords and the carina.56 The clamp securing the ETT to the Trachlight is released, and the Trachlight is removed, leaving the ETT in place.
C Lighted-Stylet Intubation: Detailed Technique
1 Preparation
With the Trachlight in place, the ETT-Trachlight (ETT-TL) unit is bent at a 90-degree angle just proximal to the cuff of the tube, similar to a field-hockey stick. The degree of bend should be individualized to the patient, but the 90-degree bend usually makes the intubation considerably easier and is our preference for most orotracheal intubations. When the tip of the ETT is in the glottic opening, the 90-degree bend projects the maximum light intensity toward the surface of the skin, producing a well-defined, circumscribed exterior glow through the soft tissues of the neck. In contrast, if the Trachlight is bent to 45 degrees, the maximum light intensity will be directed down the trachea, and the glow will not be so readily seen. For obese patients and patients with short necks, a more acute bend (>90 degrees) provides better transillumination. The exact point at which to make the bend in the Trachlight has been debated, although it is our experience that 6.5 to 8.5 cm is suitable for most patients. A study by Chen and colleagues suggested that the bent length of the Trachlight should be adjusted according to the patient’s thyroid prominence-to-mandibular angle distance (TMD) after demonstrating that a shorter bent length (6.5 cm) was more suitable for patients with a shorter TMD (<5.5 cm).57 It stands to reason that the shape of the Trachlight should be individualized to the patient’s anatomy.
3 Control of Ambient Light
Compared with its predecessors, the light emitted by the Trachlight is extremely bright, with a directed beam that enhances soft tissue transillumination of the neck. In most cases, endotracheal intubation can be performed easily under ambient lighting conditions. In a large clinical study, endotracheal intubation using the Trachlight was successfully performed under ambient light in 85% of the cases.58 In very thin patients and in children, it is possible to mistakenly interpret an esophageal intubation as an intratracheal placement, although the glow generated from inside the esophagus is more diffuse in character. Dimming of the room lights should be done only when absolutely necessary, such as in the case of an obese patient or a patient with a thick neck. In the emergency department or prehospital setting where control of the ambient lighting is not possible, it may be helpful to shade the neck with a towel or hand.
4 Technique of Intubation
a Orotracheal Intubation
As with other intubation techniques, proper denitrogenation should precede airway manipulation. Full muscle relaxation is recommended, if clinically appropriate. In a study of 176 patients, Masso and colleagues showed that muscle relaxation is associated with a lower failure rate, decreased intubation time, and fewer attempts when performing lighted-stylet orotracheal intubation.59 When the patient is under anesthesia and lying supine, the tongue falls posteriorly, pushing the epiglottis against the posterior pharyngeal wall (Fig. 21-8). In order to have a clear passage to the glottic opening during intubation, it is necessary for the clinician to grasp the jaw or mandible and lift it upward using the thumb and index finger of the nondominant hand (Fig. 21-9). This lifts the tongue and epiglottis away from the posterior pharyngeal wall to facilitate placement of the tip of the ETT posterior to the epiglottis and into the glottic opening. The nondominant hand must be kept close to the corner of the mouth to ensure an unobstructed path in the midline for the lighted stylet.
Once satisfied that the tip of the ETT-TL is close to the larynx, the clinician looks to see a glow in the anterior neck. The dominant hand can then be used to slowly rotate the Trachlight slightly to the right or left. These movements are exaggerated at the tip of the ETT-TL. By watching the transillumination in the patient’s neck moving from side to side, the degree of rotation required to ensure that the tip of the Trachlight is exactly midline can be established. Once it is in the midline, a faint glow seen above the laryngeal prominence indicates that the tip of the ETT-TL is located in the vallecula. A jaw lift or a retraction of the tongue60 helps to elevate the epiglottis and enhance passage of the ETT-TL under the epiglottis, and “rocking” the handle backward advances the tip of the lighted stylet toward the vocal cords. When the tip of the ETT-TL enters the glottic opening, a well-defined, circumscribed glow can be seen in the anterior neck slightly below the laryngeal prominence (see Fig. 21-5A). However, the ETT-TL cannot be readily advanced into the trachea because of the preshaped hockey stick configuration of the Trachlight (Fig. 21-10).
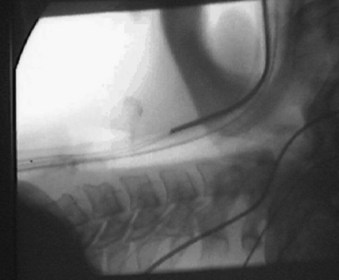
Retraction of the stiff internal wire stylet approximately 10 cm makes the distal portion of the ETT-TL unit more pliable, allowing advancement into the trachea with reduced risk of trauma (Fig. 21-11). Advancement of the pliable ETT-TL unit into the trachea before removal of the Trachlight improves the success rate of intubation. This is analogous to the successful placement of an intravenous cannula by advancing the angiocath together with the needle a few millimeters into the vein after the needle tip has entered the vein. This ensures that the catheter is inside the vein before the needle is removed from the angiocath. The glow from the ETT-TL can be seen migrating down the neck. When the glow begins to disappear at the sternal notch (Fig. 21-12), the tip of the ETT is approximately 5 cm above the carina in the average adult.61
Occasionally, the circumscribed glow cannot be readily seen in the anterior neck due to anatomic features such as morbid obesity or a short neck. Neck extension, as described earlier, may be helpful. Placement of a support under the shoulders may further assist neck extension.62 Retraction of the breast or chest wall tissues caudally together with indentation of the tissues around the trachea by an assistant enhances transillumination of the soft tissues in the anterior neck. Dimming of the ambient light is required only in some occasions.
b Nasotracheal Intubation
Complete removal of the internal stiff wire stylet from Trachlight makes the ETT-TL unit pliable enough for atraumatic nasotracheal intubation. If a nasal Ring-Adair-Elwyn (RAE) ETT is used, the internal stiff wire stylet of the Trachlight can be retracted halfway (about 15 cm). This “unbends” the proximal curvature of the nasal RAE ETT (Fig. 21-13), making lighted-stylet nasal intubation with a RAE ETT easier.
As with oral Trachlight intubation, the head is placed in a neutral or extended position, not the sniffing position. The Trachlight is switched on once the tip of the ETT-TL has been advanced into the oropharynx, positioned in the midline, and advanced gently using the light glow as a guide. A jaw-lift maneuver is necessary to lift the epiglottis from the posterior pharyngeal wall (Fig. 21-14). However, without the stiff internal wire stylet in situ, difficulty may be encountered controlling the tip of the ETT during blind nasal intubation. In particular, because of the natural curvature of the ETT, the tip commonly goes posteriorly into the esophagus. Various maneuvers may help. To bring the tip of the ETT anteriorly during intubation, it is sometimes necessary to flex the neck of the patient while advancing the ETT-TL slowly. If flexing of the neck is contraindicated, inflating the ETT cuff completely with 20 cc of air will help to elevate the ETT tip and align it with the glottis during intubation.63 Alternatively, an ETT with a controllable tip (the Endotrol tube by Mallinckrodt Critical Care, Inc., St. Louis) can be used for nasotracheal intubations and directed toward the glottis.64 In some difficult circumstances, nasotracheal intubation can be performed effectively and safely with the internal stiff wire stylet in place.65,66 Although there can be an increased risk of nasal trauma with the wire stylet in place, this technique may be associated with fewer head-neck manipulations and perhaps better control of the tip of the ETT.
D Clinical Utility of Lighted Stylets
1 Routine Use
Endotracheal intubation using a lighted stylet is easy to learn. The Trachlight has a learning curve of 10 to 30 intubations.67,68 Once mastered, the Trachlight is quick to use. A large study involving 950 elective surgical patients demonstrated Trachlight intubation to be statistically significantly faster than direct laryngoscopic intubation (15.7 ± 10.8 versus 19.6 ± 23.7 seconds, respectively),58 although such a small time difference is unlikely to be clinically significant. In the same study, the Trachlight appeared to compare favorably with the conventional laryngoscopic technique with regard to effectiveness and failure rate. There was a 1% failure rate with the Trachlight, and 92% of intubations were successful on the first attempt, compared with a 3% failure rate and an 89% success rate on first attempt using a standard laryngoscope. There were significantly fewer traumatic events and sore throats in the Trachlight group compared with laryngoscopy patients. Tsutsui and Setoyama reported similar findings in a study with 511 patients.69 Trachlight intubation appeared to be highly effective (99%), with successful intubation after one attempt in most cases (93%). Unsuccessful intubation, even after three attempts, occurred in 3 patients (1%).
Other lighted stylets have been less well studied. However, in 1991, a letter to the editor reported on 1200 TubeStat intubations in one institution over a 2-year period. In that series, the TubeStat was used without laryngoscopic assistance. Although most intubations were undertaken with the patient under general anesthesia, some were performed with topical anesthesia in anticipation of a probable DA. The authors reported that the TubeStat had a high success rate after failed laryngoscopic intubation and a low failure rate when used as a first-choice device. They concluded that “in the majority of elective cases, TubeStat intubation is our method of choice.”70
2 Difficult Airway
The Trachlight has also proved to be useful for nasal or oral intubation in patients with anticipated or unanticipated DAs.71 During the development of the Trachlight, a study reported on its clinical utility in 265 patients with DAs. Group 1 (n = 206) had a documented history of DA or anticipated DA, whereas group 2 (n = 59) were anesthetized patients with an unanticipated failed laryngoscopic intubation. In group 1, intubation was successful in all but 2 of the patients, with a mean (±SD) time to intubation of 25.7 ± 20.1 seconds. The tracheas of these 2 patients (1 morbidly obese patient weighing 220 kg and 1 patient with severe flexion deformity of the cervical spine) were intubated successfully using a flexible fiberoptic bronchoscope (FFB). Orotracheal intubation with the Trachlight was successful in all patients in group 2, with a mean time to intubation of 19.7 ± 13.5 seconds. Apart from minor mucosal bleeding (mostly from nasal intubation), no serious complications were observed in any of the study patients.
Other investigators have also reported successful use of the Trachlight for tracheal placement in patients with a DA. These reports have included patients with a history of limited mouth opening,72 severe burn contractures,73 pediatric tongue-flap surgery,74 Pierre-Robin syndrome,75 other pediatric craniofacial abnormalities,76 and patients with DA and cardiac conditions.77
The Trachlight can also be used for patients with cervical spine abnormalities. In a randomized crossover trial of 36 healthy patients, Turkstra and associates compared cervical spine motion produced by Macintosh laryngoscopy, the Glidescope video laryngoscope, and the Trachlight when manual in-line stabilization was applied.78 Using fluoroscopic video, these investigators showed that the Glidescope and Trachlight methods of intubation produced roughly half as much cervical spine motion as Macintosh laryngoscopy. This study, and another by Huang,79 found Trachlight intubation to be considerably faster than Glidescope intubation in healthy anesthetized patients with simulated in-line cervical spine stabilization. In Huang’s randomized study of 60 patients, time to intubate was 15 ± 5 seconds in the Trachlight group and 33 ± 9 seconds in the Glidescope group (P < 0.05).79 In a more recent prospective, randomized crossover trial of 20 patients, the Trachlight produced as little cervical spine motion as intubation using an FFB in anesthetized, paralyzed adults with a normal cervical spine.80 A prospective, randomized trial of 148 patients with cervical spine abnormalities compared airway management with the Trachlight versus the Fastrach laryngeal mask airway (LMA), an intubating LMA (iLMA). The Trachlight was found to be considerably quicker (23 ± 9 versus 71 ± 24 seconds) and more reliable (97.3% versus 73.0% successful intubations after a maximum of two attempts) than the iLMA in this patient population.81
The utility of lighted stylets for the management of predicted DA is not limited to the Trachlight. In 2009, Rhee and coworkers randomly assigned 60 patients with high Mallampati scores (class III or IV) to receive endotracheal intubation using either the standard laryngoscope or the Surch-Lite lighted stylet (Aaron Medical Industries, St. Petersburg, FL). The rate of successful endotracheal intubation was significantly higher in the Surch-Lite group after one attempt (97%, versus 80% in the direct laryngoscopy group), and Surch-Lite intubation was also significantly quicker (12 ± 6 versus 17 ± 12 seconds, respectively).82
3 Hemodynamic Effects
Although many studies have reported on the comparative hemodynamic changes associated with Trachlight intubation and laryngoscopic intubation, the results have been inconsistent. Several studies involving only a small number of patients (26 to 60) showed that there were no statistical differences in the hemodynamic changes occurring after endotracheal intubation using either the lighted stylet or the laryngoscope.83–87 However, most of these studies did not perform a power analysis to determine the appropriate sample size for the study, thereby running the risk of having a type II error. Although the study by Siddiqui and colleagues comparing conventional laryngoscopy to the Trachlight and the Glidescope was properly powered to detect changes in blood pressure and heart rate, there was no significant difference in these parameters between the groups.86 One study did not include a standardized general anesthetic technique.83
These findings were not consistent with the results of other studies that showed lower hemodynamic responses after endotracheal intubation using a lighted stylet compared to a laryngoscope.69,88–90 In one large study (n = 511), Tsutsui and Setoyama reported that Trachlight intubation was associated with less elevation of the blood pressure during intubation, compared with laryngoscopic intubation.69 During the development of the Trachlight, a study involving 450 elective surgical patients showed that the increases in mean arterial pressure (MAP) and heart rate occurring after intubation were significantly less with the Trachlight than with laryngoscopy.88 However, the anesthetic technique used in this study was not standardized. In a study by Rhee and associates of 60 patients with high Mallampati scores (class III and IV), those patients who received direct laryngoscopy had significantly higher increases in MAP and heart rate after intubation than did those in the Surch-Lite lighted-stylet group.82
In a small study (n = 40), Nishikawa and coworkers showed that the lighted-stylet technique significantly attenuated hemodynamic changes after intubation in normotensive patients, compared with the laryngoscopic technique.89 However, they did not find any significant difference in hemodynamic changes between the two techniques in patients with hypertension. These results were in direct contrast to the findings of another comparative study of the hemodynamic changes using three intubating techniques: a Macintosh laryngoscope, a Trachlight, and an iLMA in 75 patients.90 The investigators in that study reported that both the iLMA and the Trachlight attenuated the hemodynamic stress response to endotracheal intubation, compared with the Macintosh laryngoscope, in hypertensive but not in normotensive patients.
In a randomized, controlled trial of 80 patients with coronary artery disease, Montes and colleagues compared hemodynamic responses to intubation with the Trachlight versus direct-vision laryngoscopy.91 Although the results were not significantly different, the Trachlight group tended to have lower blood pressure and heart rate during the intubation period.91 Clearly, future studies involving large numbers of patients are necessary to clarify these conflicting data regarding the hemodynamic stimulation associated with endotracheal intubation using a lighted stylet.
4 Pediatric Use
The pediatric Trachlight has been used both orally and nasally,92 including in patients with a DA.74,93 In 2008, Xue and coworkers published a case series of four children with craniofacial abnormalities who were unable to be intubated via direct laryngoscopy (all children had Cormack-Lehane grade 4 views) or with a FFB.76 The tracheas of these four children were intubated successfully within 30 seconds using the Trachlight. The small body of published pediatric Trachlight experience suggests that some adjustments to technique may be necessary. Suggestions include the following76:
1. The Trachlight should be bent to 60 to 80 degrees instead of the usual 90 degrees to better suit pediatric anatomy.
2. The distance before the bend in the Trachlight should reflect the short length of the pediatric airway.
3. Because of the small distances involved, transillumination must be expected soon after insertion of the Trachlight.
4. The Trachlight glow is so readily seen through the relatively small amount of tissue in a child that transilllumination from the esophagus can more easily be mistaken for that from the trachea, although experience will enable the clinician to tell the difference.
5 Synergy with Direct Laryngoscopy
Endotracheal intubation can fail with the Trachlight as well as with the laryngoscope. However, in an early study of 950 patients, all Trachlight failures were resolved with direct laryngoscopy.58 Similarly, all failures of direct laryngoscopy were resolved with Trachlight. These results suggest that a success rate approaching 100% can be achieved in endotracheal intubation by combining the two methods.
The techniques can even be used simultaneously, which may be particularly useful for unanticipated DL (e.g., patients with a Cormack-Lehane grade 3 laryngoscopic view).18 While maintaining the grade 3 view with a standard laryngoscope in situ, the clinician can use an ETT-TL with a 90-degree bend. Under direct laryngoscopy, the tip of the ETT-TL can be “hooked” under the epiglottis. If the tip of the ETT is placed at the glottic opening, a well-defined, circumscribed glow can be seen in the anterior neck slightly below the laryngeal prominence. If a glow is not seen, the ETT-TL should be repositioned until a glow can be seen in the anterior neck. Since the development of the Trachlight, we have recorded more than a dozen failed intubations using either the Trachlight or a laryngoscope, but in each of these failures, endotracheal intubation was successful using the laryngoscope together with the Trachlight. Others have also reported the successful use of this combined technique. In one study, the investigators successfully performed endotracheal intubation in all 350 study surgical patients with a simulated DA using the laryngoscope together with the Trachlight.94
6 Use with Other Airway Devices
In addition to its use with the laryngoscope, the Trachlight has been combined successfully with other intubating techniques. These include intubation through the LMA-Classic,95,96 through the iLMA,97 with the Bullard laryngoscope,98,99 and with a retrograde intubating technique.100
7 Percutaneous Tracheotomy
The Trachlight can be used to identify the intratracheal position of the tip of the ETT during percutaneous tracheostomy.101 This simple technique can help to avoid puncturing the ETT or the cuff, thus ensuring adequate ventilation and oxygenation during the percutaneous tracheotomy. This technique is also inexpensive and minimizes the risk of damaging equipment such as the FFB. If it is used properly, it is possible that this simple, light-guided technique can also be used to accurately determine when the tip of the ETT is above the surgical tracheotomy site as the tube is pulled back during surgical tracheotomy.
F Complications
In 2001, Aoyama and colleagues reported that the epiglottis of a patient was partially pushed into the laryngeal inlet, along with the ETT, after Trachlight intubation.102 To investigate the potential risk of laryngeal damage during Trachlight intubation. Hung and colleagues placed an FFB in the nasopharynx. They reported that during orotracheal placement of the ETT using the Trachlight, structures around the glottic opening, including the epiglottis and the arytenoids, could be transiently displaced. In some instances, the epiglottis was pushed into the glottic opening. Usually, the epiglottis spontaneously returned to the correct position. The authors suggested that there are potential risks of laryngeal damage in addition to downfolding of the epiglottis during ETT placement using the Trachlight, but such occurrences have not been observed to cause permanent damage, and the reduction in the incidence of sore throat in patients undergoing Trachlight intubation compared to laryngoscopic intubation suggests that such occurrences are of little clinical significance.58
Subluxation of the cricoarytenoid cartilage occurs rarely but was reported in a study using an older version of a lighted stylet (Tubestat).103 However, with correct use of the retractable wire stylet, the risk of damaging the arytenoid cartilage during Trachlight intubation is low.
In 2008, Zhang and associates reported a case in which the part of the silicon sheath that protects the Trachlight wand and bulb broke from the Trachlight unit during intubation and was left behind within the lumen of the ETT.104 This is the only such published case involving the Trachlight, although there have been four similar case reports of instrument disarticulation with other lightwand devices.105–107 In Zhang’s case, “the wand was withdrawn from the ETT with some difficulty.”104 Softening the ETT before intubation by placing it in warm saline makes it more malleable, and lubricating the wand with a water-based lubricant makes disengaging the Trachlight from the ETT unit much easier. These steps, together with the mindset that undue force should always be avoided, will likely reduce any structural damage to the Trachlight. Nevertheless, it is good practice to always examine the Trachlight after intubation for structural integrity.
Noguchi and colleagues reported that application of 8% xylocaine in a pump spray as a lubricant for the Trachlight resulted in disappearance of the print markings of the wand.108 However, lidocaine jelly and glycerin showed no effect on the print marks. The investigators suggested that lidocaine pump spray should not be used as a lubricant on the Trachlight wand.
V Clinical Pearls
• The Eschmann Introducer (EI) is best used when the epiglottis can be seen under direct laryngoscopy (Cormack-Lehane grade 3 view); the coudé tip can be hooked under the epiglottis and the EI advanced blindly through the glottis. The success of this maneuver is improved if the EI has been preshaped into a curve.
• If “clicks” are felt on blind advancement of the EI into the trachea, the potentially more traumatic “hold-up sign,” though reliable, need not be sought.
• To facilitate the advancement of the ETT over the EI after tracheal placement, the tongue and epiglottis should be elevated by a jaw lift, or preferably by a laryngoscope.
• During blind nasotracheal intubation, inflating the ETT cuff completely with 20 cc of air can help to elevate the ETT tip and align it with the glottic opening, facilitating tracheal placement.
• In order to have a clear passage to the glottic opening during lightwand intubation, it is necessary for the clinician to perform a jaw lift, which will elevate the tongue and epiglottis away from the posterior pharyngeal wall to facilitate placement of the tip of the ETT posterior to the epiglottis and into the glottic opening.
• Although the lightwand has been demonstrated to be effective and safe for endotracheal intubation, the technique requires transillumination of the soft tissues of the anterior neck without visualization of the laryngeal structure. Therefore, a lightwand should not be used in patients with known abnormalities of the upper airway, such as tumors, polyps, infection, or trauma of the upper airway.
All references can be found online at expertconsult.com.
13 Karkouti K, Rose D, Wigglesworth D, Cohen M. Predicting difficult intubation: A multivariable analysis. Can J Anesth. 2000;47:730–739.
18 Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111.
27 Levitan R, Ochroch EA. Airway management and direct laryngoscopy: A review and update. Crit Care Clin. 2000;16:373–388. v
32 Levitan RM, Pisaturo JT, Kinkle WC, et al. Stylet bend angles and tracheal tube passage using a straight-to-cuff shape. Acad Emerg Med. 2006;13:1255–1258.
57 Chen TH, Tsai SK, Lin CJ, et al. Does the suggested lightwand bent length fit every patient? The relation between bent length and patient’s thyroid prominence–to–mandibular angle distance. Anesthesiology. 2003;98:1070–1076.
71 Hung OR, Pytka S, Morris I, et al. Lightwand intubation: II. Clinical trail of a new lightwand to intubate patients with difficult airways. Can J Anaesth. 1995;42:826–830.
78 Turkstra TP, Craen RA, Pelz DM, Gelb AW. Cervical spine motion: A fluoroscopic comparison during intubation with lighted stylet, GlideScope, and Macintosh laryngoscope. Anesth Analg. 2005;101:910–915. table of contents
86 Siddiqui N, Katznelson R, Friedman Z. Heart rate/blood pressure response and airway morbidity following tracheal intubation with direct laryngoscopy, GlideScope and Trachlight: A randomized control trial. Eur J Anaesthesiol. 2009;26:740–745.
100 Hung OR, al-Qatari M. Light-guided retrograde intubation. Can J Anaesth. 1997;44:877–882.
1 Mihic D, Binkert E, Novoselac M. The first endotracheal intubation. Anesthesiology. 1980;52:523.
2 Frostad AB, Ronning-Arnesen A. Tracheostomy in acute obstructive laryngitis. J Laryngol Otol. 1973;87:1101–1106.
3 Herholdt JR, Rafn CG. An attempt at an historical survey of life-saving measures for drowning persons and information of the best means by which they can again be brought back to life. Copenhagen: H Tikiob; 1796.
4 Macewen W. Clinical observations on the introduction of tracheal tubes by the mouth, instead of performing tracheotomy or laryngotomy. Br Med J. 1880;2:163–165.
5 Goerig M. Franz Kuhn (1866–1929) on the 125th anniversary of his birthday. Anasthesiol Intensivmed Notfallmed Schmerzther. 1991;26:416–424.
6 Jackson C. The technique of insertion of intratracheal insufflation tubes. Surg Gynecol Obstet. 1913;17:507.
7 Latto I. Management of difficult intubation. In: Latto I, Rosen M. Difficulties in tracheal intubation. London: Bailliere Tindall; 1987:99–141.
8 Davies JM, Weeks S, Crone LA, Pavlin E. Difficult intubation in the parturient. Can J Anaesth. 1989;36:668–674.
9 Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61:211–216.
10 Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: A prospective study. Can Anaesth Soc J. 1985;32:429–434.
11 el-Ganzouri AR, McCarthy RJ, Tuman KJ, et al. Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–1204.
12 Rose DK, Cohen MM. The airway: Problems and predictions in 18,500 patients. Can J Anaesth. 1994;41:372–383.
13 Karkouti K, Rose D, Wigglesworth D, Cohen M. Predicting difficult intubation: A multivariable analysis. Can J Anesth. 2000;47:730–739.
14 Macintosh RR. An aid to oral intubation. Br Med J. 1949;1:28.
15 Henderson JJ. Development of the “gum-elastic bougie.”. Anaesthesia. 2003;58:103–104.
16 El-Orbany MI, Salem MR, Joseph NJ. The Eschmann tracheal tube introducer is not gum, elastic, or a bougie. Anesthesiology. 2004;101:1240. author reply, 1242–1244
17 Viswanathan S, Campbell C, Wood DG, et al. The Eschmann Tracheal Tube Introducer (gum elastic bougie). Anesthesiol Rev. 1992;19:29–34.
18 Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111.
19 Hodzovic I, Wilkes AR, Latto IP. To shape or not to shape: Simulated bougie-assisted difficult intubation in a manikin. Anaesthesia. 2003;58:792–797.
20 Kidd JF, Dyson A, Latto IP. Successful difficult intubation: Use of the gum elastic bougie. Anaesthesia. 1988;43:437–438.
21 Dagg LE, Jefferson P, Ball DR. “Hold up” and the gum elastic bougie. Anaesthesia. 2003;58:103.
22 Hagberg CA. Special devices and techniques. Anesthesiol Clin North Am. 2002;20:907–932.
23 Arisaka H, Sakuraba S, Furuya M, et al. Application of gum elastic bougie to nasal intubation. Anesth Prog. 2010;57:112–113.
24 Rowley E, Dingwall R. The use of single-use devices in anaesthesia: Balancing the risks to patient safety. Anaesthesia. 2007;62:569–574.
25 Frova G. Comparison of tracheal introducers. Anaesthesia. 2005;60:516–517. author reply, 517–518
26 Hodzovic I, Latto IP, Wilkes AR, et al. Evaluation of Frova, single-use intubation introducer, in a manikin: Comparison with Eschmann multiple-use introducer and Portex single-use introducer. Anaesthesia. 2004;59:811–816.
27 Levitan R, Ochroch EA. Airway management and direct laryngoscopy: A review and update. Crit Care Clin. 2000;6:373–388. v
28 Weiss M. Management of difficult tracheal intubation with a video-optically modified Schroeder intubation stylet. Anesth Analg. 1997;85:1181–1182.
29 Nolan JP, Wilson ME. An evaluation of the gum elastic bougie: Intubation times and incidence of sore throat. Anaesthesia. 1992;47:878–881.
30 Nolan JP, Wilson ME. Orotracheal intubation in patients with potential cervical spine injuries: An indication for the gum elastic bougie. Anaesthesia. 1993;48:630–633.
31 Rao TL, Mathru M, Gorski DW, Salem MR. Experience with a new intubation guide for difficult tracheal intubation. Crit Care Med. 1982;10:882–883.
32 Levitan RM, Pisaturo JT, Kinkle WC, et al. Stylet bend angles and tracheal tube passage using a straight-to-cuff shape. Acad Emerg Med. 2006;13:1255–1258.
33 Gataure PS, Vaughan RS, Latto IP. Simulated difficult intubation: Comparison of the gum elastic bougie and the stylet. Anaesthesia. 1996;51:935–938.
34 Hodzovic I, Latto IP, Henderson JJ. Bougie trauma: What trauma? Anaesthesia. 2003;58:192–193.
35 Arndt GA, Cambray AJ, Tomasson J. Intubation bougie dissection of tracheal mucosa and intratracheal airway obstruction. Anesth Analg. 2008;107:603–604.
36 Gardner M, Janokwski S. Detachment of the tip of a gum-elastic bougie. Anaesthesia. 2002;57:88–89.
37 Bhargava M, Pothula SN, Joshi S. The obstruction of an endotracheal tube by the plastic coating sheared from a stylet: A revisit. Anesthesiology. 1998;88:548–549.
38 Arya VK, Makker S, Bedi SP. Impacted gum-elastic bougie in an endotracheal tube after successful intubation of a difficult airway. J Clin Anesth. 2007;19:566.
39 Shah KH, Kwong BM, Hazan A, et al. Success of the gum elastic bougie as a rescue airway in the emergency department. J Emerg Med. 2011;40:1–6.
40 Heegaard WG, Black C, Pasquerella C, Miner J. Use of the endotracheal tube introducer as an adjunct for oral tracheal intubation in the prehospital setting. Air Med J. 2003;22:28–31.
41 Le DH, Reed DB, Weinstein G, et al. Paramedic use of endotracheal tube introducers for the difficult airway. Prehosp Emerg Care. 2001;5:155–158.
42 Combes X, Jabre P, Margenet A, et al. Unanticipated difficult airway management in the prehospital emergency setting: Prospective validation of an algorithm. Anesthesiology. 2011;114:105–110.
43 Anez Simon C, Montori Lacamara N, Santos Marques ML, et al. [McGrath video laryngoscope used with a Frova intubating introducer for management of the difficult airway]. Rev Esp Anestesiol Reanim. 2010;57:61–64.
44 Conklin LD, Cox WS, Blank RS. Endotracheal tube introducer-assisted intubation with the GlideScope video laryngoscope. J Clin Anesth. 2010;22:303–305.
45 Iizuka T, Shimoyama N, Notoya A. [Tube introducer catheter as an adjunct to the airway scope for tracheal intubation in a manikin model]. Masui. 2010;59:1534–1538.
46 Muallem M, Baraka A. Tracheal intubation using the GlideScope with a combined curved pipe stylet, and endotracheal tube introducer. Can J Anaesth. 2007;54:77–78.
47 Donat N, Villevieille T, Masson Y, et al. In case of difficult intubation with the Airtraq(®): The gum elastic bougie may assist. Ann Fr Anesth Reanim. 2011;30:87–88.
48 Heitz JW, Mastrando D. The use of a gum elastic bougie in combination with a videolaryngoscope. J Clin Anesth. 2005;17:408–409.
49 Macintosh R, Richards H. Illuminated introducer for endotracheal tubes. Anaesthesia. 1957;12:223–225.
50 Yamamura H, Yamamato T, Kamiyama M. Device for blind nasal intubation. Anesthesiology. 1959;20:221.
51 Vollmer TP, Stewart RD, Paris PM, et al. Use of a lighted stylet for guided orotracheal intubation in the prehospital setting. Ann Emerg Med. 1985;14:324–328.
52 Ellis DG, Stewart RD, Kaplan RM, et al. Success rates of blind orotracheal intubation using a transillumination technique with a lighted stylet. Ann Emerg Med. 1986;15:138–142.
53 Ainsworth QP, Howells TH. Transilluminated tracheal intubation. Br J Anaesth. 1989;62:494–497.
54 Weis FR, Hatton MN. Intubation by use of the light wand: Experience in 253 patients. J Oral Maxillofac Surg. 1989;47:577–580. discussion, 581
55 Nishiyama T, Matsukawa T, Hanaoka K. Safety of a new lightwand device (Trachlight): Temperature and histopathological study. Anesth Analg. 1998;87:717–718.
56 Stewart RD, LaRosee A, Kaplan RM, Ilkhanipour K. Correct positioning of an endotracheal tube using a flexible lighted stylet. Crit Care Med. 1990;18:97–99.
57 Chen TH, Tsai SK, Lin CJ, et al. Does the suggested lightwand bent length fit every patient? The relation between bent length and patient’s thyroid prominence–to–mandibular angle distance. Anesthesiology. 2003;98:1070–1076.
58 Hung OR, Pytka S, Morris I, et al. Clinical trial of a new lightwand (TrachlightTM) to intubate the trachea. Anesthesiology. 1995;83:509–514.
59 Masso E, Sabate S, Hinojosa M, Vila P, Canet J, Langeron O. Lightwand tracheal intubation with and without muscle relaxation. Anesthesiology. 2006;104:249–254.
60 Umesh G, George M, Venkateswaran R. Tongue traction is as effective as jaw lift maneuver for Trachlight-guided orotracheal intubation. Acta Anaesthesiol Taiwan. 2010;48:130–135.
61 Stewart RD, LaRosee A, Kaplan RM, Ilkhanipour K. Correct positioning of an endotracheal tube using a flexible lighted stylet. Crit Care Med. 1990;18:97–99.
62 Umesh G, Mathew G, Ramkumar V. Trachlight: More practical solutions to commonly encountered problems. Can J Anaesth. 2007;54:398–399.
63 Hung OR. Nasal intubation with the Trachlight. Can J Anaesth. 1999;46:907–908.
64 Asai T. Endotrol tube for blind nasotracheal intubation [letter]. Anaesthesia. 1996;50:507.
65 Agro F, Brimacombe J, Marchionni L, et al. Nasal intubation with the Trachlight. Can J Anaesth. 1999;46:907–908.
66 Favaro R, Tordiglione P, Di Lascio F, et al. Effective nasotracheal intubation using a modified transillumination technique. Can J Anaesth. 2002;49:91–95.
67 Langeron O, Lenfant F, Aubrun F, et al. Évaluation de l’apprentissage d’un nouveau guide lumineux (trachlight(TM)) pour l’intubation trachéale. Ann Fr Anesth Reanim. 1997;16:229–233.
68 Yamamoto T, Aoyama K, Takenaka I, et al. Light-guided tracheal intubation using a Trachlight: Causes of difficulty and skill acquisition. Masui. 1999;48:672–677.
69 Tsutsui T, Setoyama K. [A clinical evaluation of blind orotracheal intubation using Trachlight in 511 patients]. Masui. 2001;50:854–858.
70 Graham DH, Doll WA, Robinson AD, Warriner CB. Intubation with lighted stylet. Can J Anaesth. 1991;38:261–262.
71 Hung OR, Pytka S, Morris I, et al. Lightwand intubation: II. Clinical trial of a new lightwand to intubate patients with difficult airways. Can J Anaesth. 1995;42:826–830.
72 Favaro R, Tordiglione P, Di Lascio F, et al. Effective nasotracheal intubation using a modified transillumination technique. Can J Anaesth. 2002;49:91–95.
73 Bhardwaj A, Kidwai SN, Verma V, et al. Continuous anesthetic insufflation and topical anesthesia of the airway using Trachlight in chronic facial burns. Anesth Analg. 2006;102:334.
74 Garg R. Trachlight for airway management in tongue flap division surgery. Paediatr Anaesth. 2009;19:279–280.
75 Iseki K, Watanabe K, Iwama H. Use of the Trachlight for intubation in the Pierre-Robin syndrome. Anaesthesia. 1997;52:801–802.
76 Xue FS, Yang QY, Lio X, et al. Lightwand guided intubation in paediatric patients with a known difficult airway: A report of four cases. Anaesthesia. 2008;63:520–525.
77 Gille A, Komar K, Schmidt E, Alexander T. [Transillumination technique in difficult intubations in heart surgery]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2002;37:604–608.
78 Turkstra TP, Craen RA, Pelz DM, Gelb AW. Cervical spine motion: A fluoroscopic comparison during intubation with lighted stylet, GlideScope, and Macintosh laryngoscope. Anesth Analg. 2005;101:910–915. table of contents
79 Huang WT, Huang CY, Chung YT. Clinical comparisons between GlideScope video laryngoscope and Trachlight in simulated cervical spine instability. J Clin Anesth. 2007;19:110–114.
80 Houde BJ, Williams SR, Cadrin-Chenevert A, et al. A comparison of cervical spine motion during orotracheal intubation with the Trachlight(r) or the flexible fiberoptic bronchoscope. Anesth Analg. 2009;108:1638–1643.
81 Inoue Y, Koga K, Shigematsu A. A comparison of two tracheal intubation techniques with Trachlight and Fastrach in patients with cervical spine disorders. Anesth Analg. 2002;94:667–671. table of contents
82 Rhee KY, Lee JR, Kim J, et al. A comparison of lighted stylet (Surch-Lite) and direct laryngoscopic intubation in patients with high Mallampati scores. Anesth Analg. 2009;108:1215–1219.
83 Friedman PG, Rosenberg MK, Lebenborm-Mansour M. A comparison of light wand and suspension laryngoscopic intubation techniques in outpatients. Anesth Analg. 1997;85:578–582.
84 Hirabayashi Y, Hiruta M, Kawakami T, et al. Effects of lightwand (Trachlight) compared with direct laryngoscopy on circulatory responses to tracheal intubation. Br J Anaesth. 1998;81:253–255.
85 Takahashi S, Mizutani T, Miyabe M, Toyooka H. Hemodynamic responses to tracheal intubation with laryngoscope versus lightwand intubating device (Trachlight) in adults with normal airway. Anesth Analg. 2002;95:480–484. table of contents
86 Siddiqui N, Katznelson R, Friedman Z. Heart rate/blood pressure response and airway morbidity following tracheal intubation with direct laryngoscopy, GlideScope and Trachlight: A randomized control trial. Eur J Anaesthesiol. 2009;26:740–745.
87 Kanaide M, Fukusaki M, Tamura S, et al. Hemodynamic and catecholamine responses during tracheal intubation using a lightwand device (Trachlight) in elderly patients with hypertension. J Anesth. 2003;17:161–165.
88 Hung OR, Pytka S, Murphy MF, et al. Comparative hemodynamic changes following laryngoscopic or lightwand intubation. Anesthesiology. 1993;79(3A):A497.
89 Nishikawa K, Omote K, Kawana S, Namiki A. A comparison of hemodynamic changes after endotracheal intubation by using the lightwand device and the laryngoscope in normotensive and hypertensive patients. Anesth Analg. 2000;90:1203–1207.
90 Kihara S, Brimacombe J, Yaguchi Y, et al. Hemodynamic responses among three tracheal intubation devices in normotensive and hypertensive patients. Anesth Analg. 2003;96:890–895. table of contents
91 Montes FR, Giraldo JC, Betancur LA, et al. Endotracheal intubation with a lightwand or a laryngoscope results in similar hemodynamic variations in patients with coronary artery disease. Can J Anaesth. 2003;50:824–828.
92 Xue FS, Luo MP, Liao X, Zhang YM. Lightwand guided nasotracheal intubation in children with difficult airways. Paediatr Anaesth. 2008;18:1276–1278.
93 Nishikawa M, Inomata S. Cautious use of Trachlight in infants. Anesth Analg. 2006;102:1298.
94 Agro F, Benumof JL, Carassiti M, et al. Efficacy of a combined technique using the Trachlight together with direct laryngoscopy under simulated difficult airway conditions in 350 anesthetized patients. Can J Anaesth. 2002;49:525–526.
95 Asai T, Latto IP. Use of the lighted stylet for tracheal intubation via the laryngeal mask airway. Br J Anaesth. 1995;75:503–504.
96 Asai T, Latto IP. Unexpected difficulty in the lighted stylet-aided tracheal intubation via the laryngeal mask. Br J Anaesth. 1996;76:111–112.
97 Fan KH, Hung OR, Agro F. A comparative study of tracheal intubation using a Fastrach alone or together with a lightwand. J Clin Anesth. 2000;12:581–585.
98 McGuire G, Krestow M. Bullard assisted trachlight technique. Can J Anaesth. 1999;46:907.
99 Gutstein HB. Use of the Bullard laryngoscope and lightwand in pediatric patients. Anesthesiol Clin North Am. 1998;16:795–812.
100 Hung OR, al-Qatari M. Light-guided retrograde intubation. Can J Anaesth. 1997;44:877–882.
101 Addas BM, Howes WJ, Hung OR. Light-guided tracheal puncture for percutaneous tracheostomy. Can J Anaesth. 2000;47:919–922.
102 Aoyama K, Takenaka I, Nagaoka E, et al. Potential damage to the larynx associated with light-guided intubation: A case and series of fiberoptic examinations. Anesthesiology. 2001;94:165–167.
103 Debo RF, Colonna D, Dewerd G, Gonzalez C. Cricoarytenoid subluxation: Complication of blind intubation with a lighted stylet. Ear Nose Throat J. 1989;68:517–520.
104 Zhang YM, Xue FS, Liao X. Foreign body from the lightbulb sheath of a Trachlight in the endotracheal tube. Can J Anaesth. 2008;55:789–790.
105 Stone DJ, Stirt JA, Kaplan MJ, McLean WC. A complication of lightwand-guided nasotracheal intubation. Anesthesiology. 1984;61:780–781.
106 Dowson S, Greenwald KM. A potential complication of lightwand-guided intubation. Anesth Analg. 1992;74:169.
107 Stalter BA, Currier DS. Endotracheal tube foreign body after intubation with a Vital Signs, Inc., lightwand. Anesthesiology. 2003;99:514–515.
108 Noguchi T, Koga K, Shiga Y, Shigematsu A. [Preliminary report: dissolving effect of 8% lidocaine pump spray on the print mark of the Trachlight wand]. Masui. 2002;51:503–504.