Chapter 7 Intramedullary Tumors
ASTROCYTOMA
EPIDEMIOLOGY
DISTRIBUTION
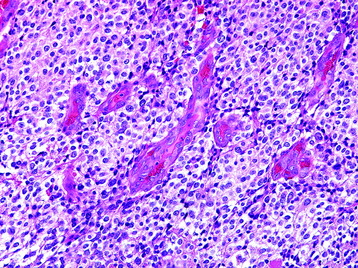
HISTOLOGY/GRADING
General
Pilocytic Astrocytoma (Grade I)
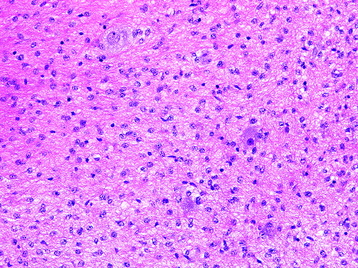
Diffuse Astrocytoma (Grade II)
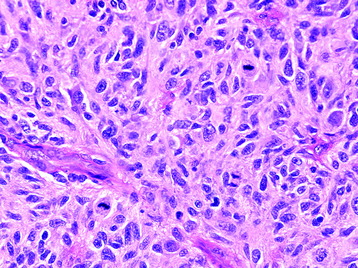
Anaplastic Astrocytoma (Grade III)
Glioblastoma (Grade IV)
RADIOLOGY
EPENDYMOMA
EPIDEMIOLOGY
DISTRIBUTION
HISTOLOGY/GRADING
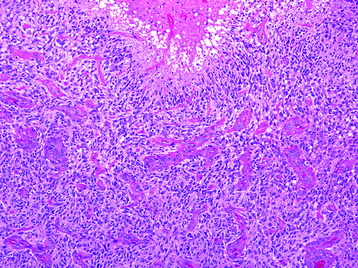
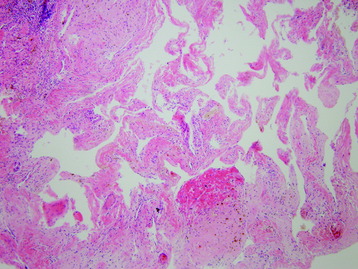
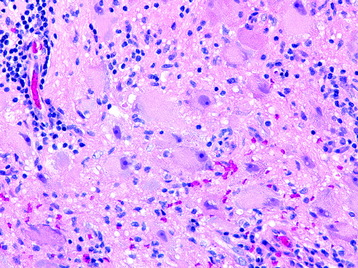
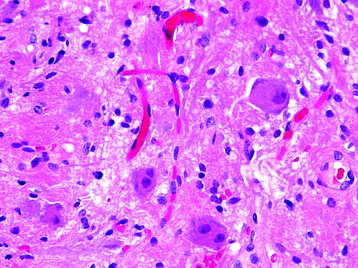
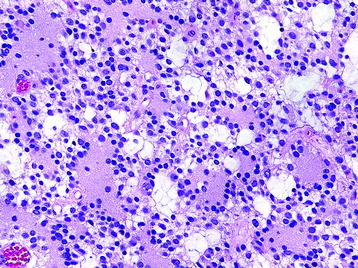
Most spinal ependymomas are histologically benign and rarely show infiltrative growth. Though they do not form tumor capsules, the interface between the tumor mass and the surrounding normal cord tissue is relatively well defined.4
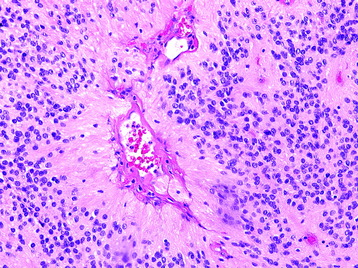
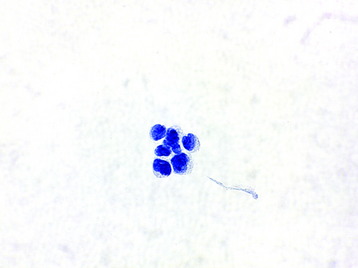
General
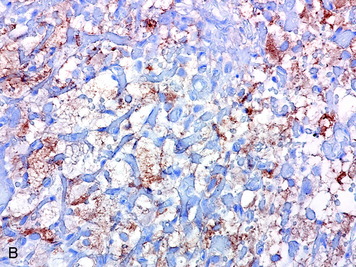
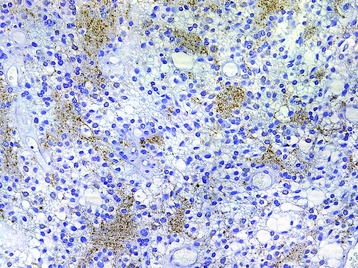
Ependymomas demonstrate cytoplasmic GFAP immunoreactivity. Both punctate intracytoplasmic and ring-like epithelial membrane antigen (EMA) immunoreactivity have been reported in ependymomas.5,6
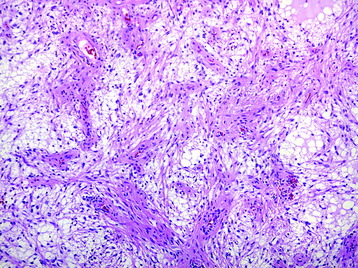
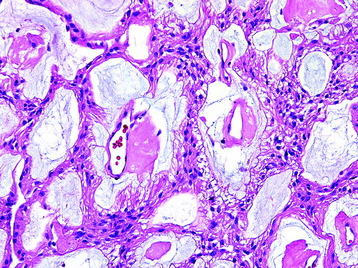
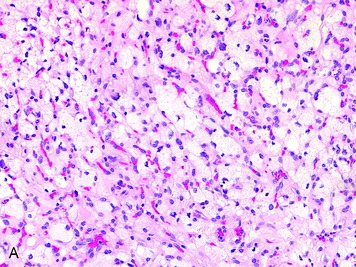
Myxopapillary Ependymoma (Grade I) (Fig. 7-9)
Ependymoma (WHO Grade II)
RADIOLOGY

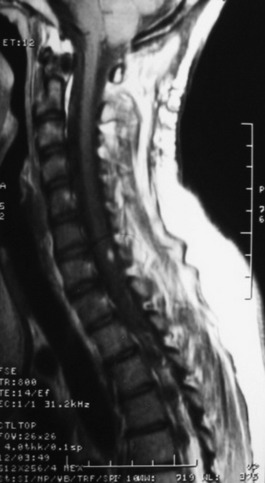
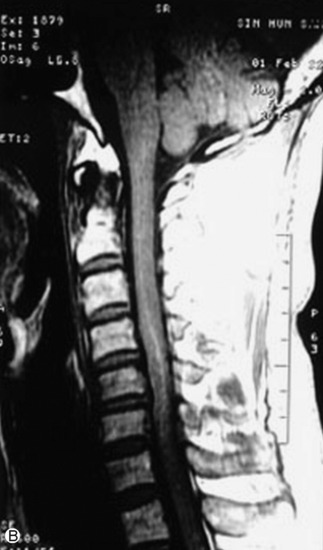
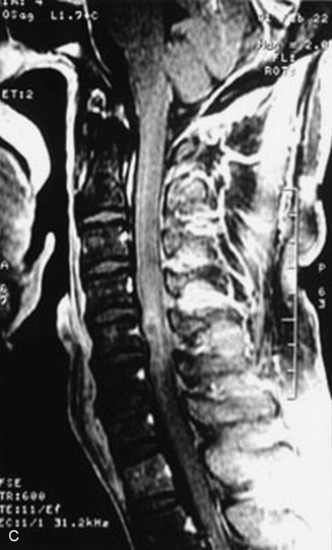
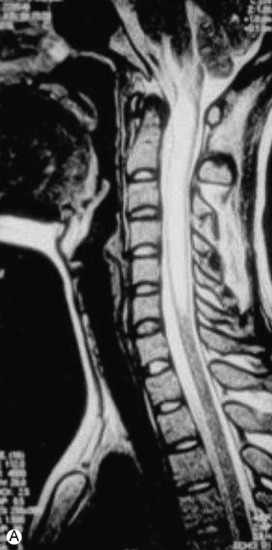
Fig. 7-12 T1 sagittal MR of myxopapillary ependymoma. The mass signal is isointense to the spinal cord.
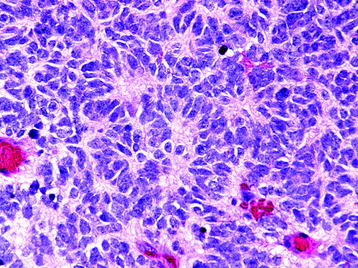
CAPILLARY HEMANGIOBLASTOMA
EPIDEMIOLOGY
DISTRIBUTION
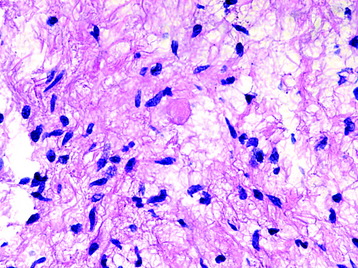
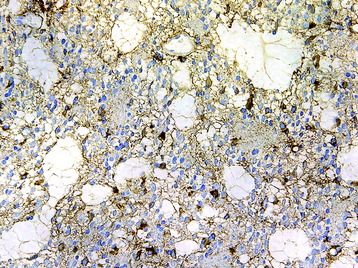
HISTOLOGY/GRADING
RADIOLOGY
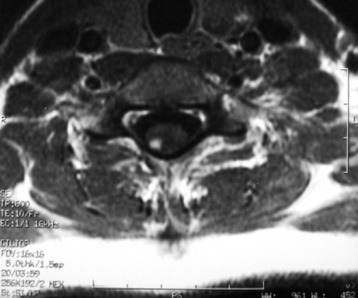
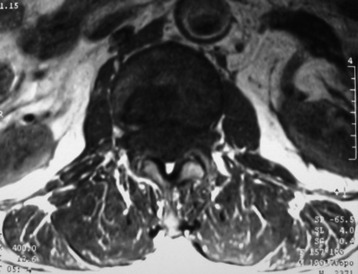
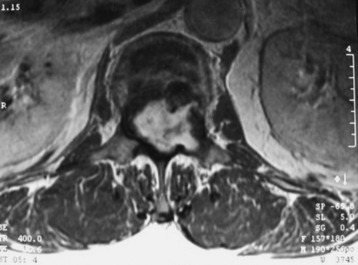
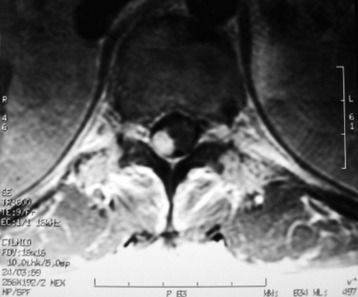
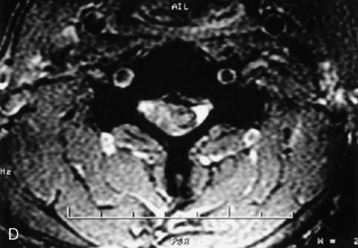
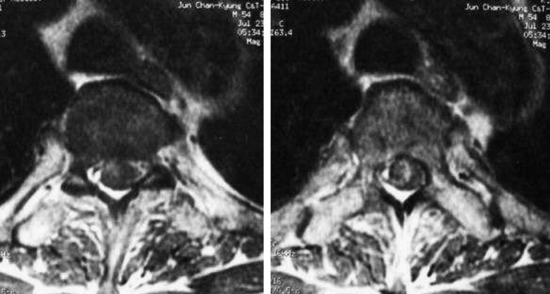
Fig. 7-20 On axial view, the enhanced nodule is located on the right posterior surface of the spinal cord.

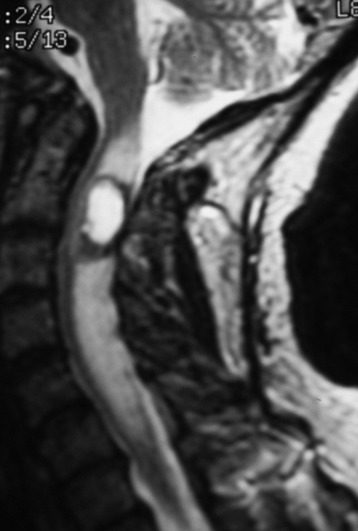
Fig. 7-21 Thorcolumbar spine MR of the same patient in Figure 7-20. At T11 level, another enhancing nodule is found. The enhancing pattern is similar. The patient is a 26-year-old female diagnosed with VHL disease.

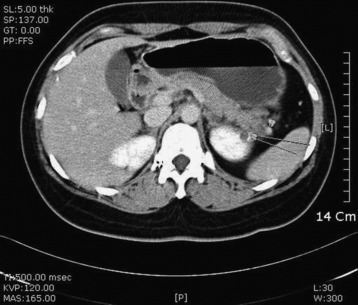
Fig. 7-24 Abdominal CT of the same patient in Fig. 7-23. A 17-mm highly enhancing solid mass, related to renal cell carcinoma, is found in the right kidney.
SPINAL CORD CAVERNOUS ANGIOMA
EPIDEMIOLOGY
DISTRIBUTION
HISTOLOGY
RADIOLOGY
GANGLIOGLIOMA
EPIDEMIOLOGY
DISTRIBUTION
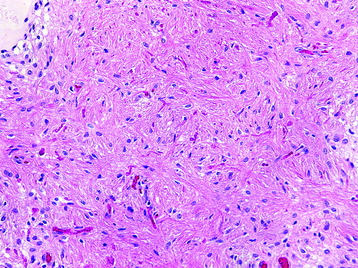
HISTOLOGY/GRADING
RADIOLOGY
NEUROCYTIC TUMORS
EPIDEMIOLOGY
DISTRIBUTION
The thoracic spine has been the predominant site of involvement by these tumors in case reports.
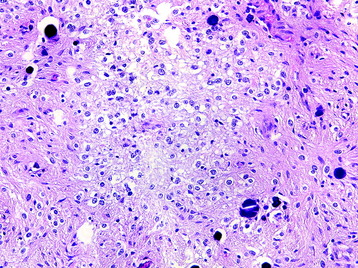
HISTOLOGY/GRADING
OLIGODENDROGLIOMA
EPIDEMIOLOGY
HISTOLOGY/GRADING
EMBRYONAL NEOPLASMS
EPIDEMIOLOGY
Primary primitive neuroectodermal tumors (PNETs) of the spinal cord are exceptionally rare, with approximately 20 reported cases.26