Chapter 5 Intradural Extramedullary Cystic Lesions
INTRADURAL ARACHNOID CYST
EPIDEMIOLOGY
• They are divided into acquired cyst and congenital cyst. Acquired arachnoid cysts are more common and can be the result of spinal cord trauma, postsurgical arachnoiditis, meningeal infection, and other insults that cause inflammation and subarachnoid adhesions.1
• Congenital or idiopathic spinal arachnoid cysts are diagnosed when there is no antecedent history of trauma or other etiologic factors and the intraoperative macroscopic and microscopic findings show a cyst wall composed of normal or slightly thickened arachnoid tissue.
• Various theories have been proposed to explain the formation of arachnoid cysts.2 Perret et al3 proposed that they arise from diverticula in the septum posticum. However, reports of cysts ventral to the spinal cord suggest that there must be another origin.4 Incarceration of arachnoid granulations may produce CSF that becomes entrapped in arachnoid diverticula. These sequestered pockets of fluid lead to further disruption of normal pulsatile CSF flow and thus are capable of expanding or producing associated syringomyelia.5,6
DISTRIBUTION
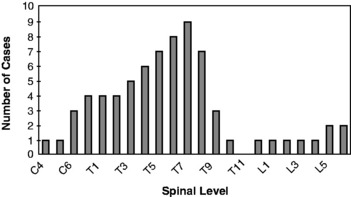
• The regional distribution of the spinal arachnoid cyst is presented in Fig. 5-1.2 Most of them are located in the thoracic region (80%), as compared with 15% in the cervical spine and 5% in the lumbar spine.
• Most of the arachnoid cyst is located dorsal to the spinal cord. In a review of the six published series that specified the arachnoid cysts’ location, 12 of 69 (17%) of the cysts were anterior to the spinal cord.5,7
RADIOLOGY
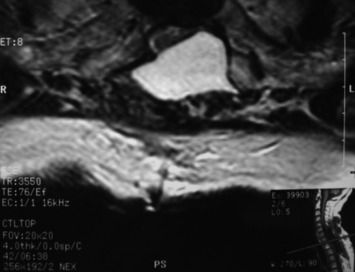
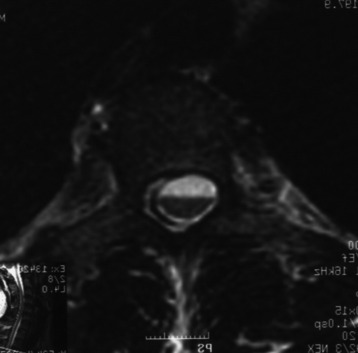
• The primary magnetic resonance imaging (MRI) finding is a spinal space–occupying mass, nonenhancing extramedullary loculated CSF collection.
• T1- and T2-weighted signals of arachnoid cyst are identical to those of CSF. There is no enhancement with gadolinium use.
• Intradural arachnoid cysts are poorly delineated on MRI because the signal intensities of both the cysts and the surrounding CSF space are more or less the same.
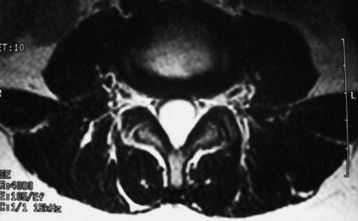
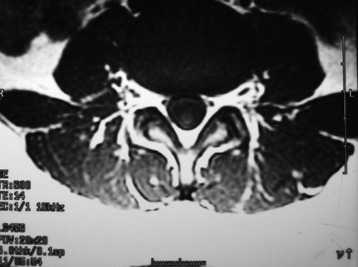
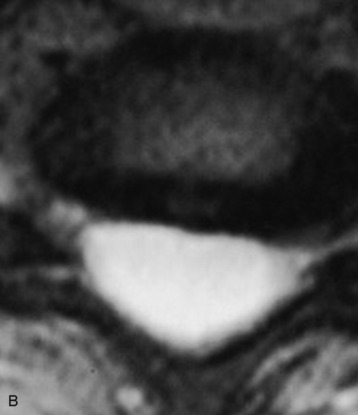
• Widening of the posterior CSF space on MRI, with anterior displacement and thinning of the spinal cord, may be the only sign of intradural arachnoid cyst (Figs. 5-4 and 5-5).8
• MRI results have been reported showing segmental clear-cut dilatation of the posterior CSF space, at one or two vertebral levels, with focal thinning of the neural structure, thus providing a definite diagnosis of intradural cysts.8
• However, because of the chronicity of this disorder, intradural arachnoid cysts may distend very slowly and elongate over multiple vertebral levels.
• Inhomogeneous areas of hypointense T2-weighted signal with respect to the surrounding CSF may be seen. This phenomenon is consistently interpreted as artifacts from aortic pulsations into CSF (see Figs. 5-4 and 5-5).9
• Anterior cysts are more likely to cause weakness and myelopathy, whereas dorsal cysts present more commonly with neuropathic pain and numbness (Figs. 5-6 and 5-7).
DERMOID CYST
EPIDEMIOLOGY
• They arise from inclusion of ectodermal elements at the time of neural groove closure, which normally occurs between the third and fifth weeks of embryonic life.
• They might also occur after the introduction of dermal elements into the spinal subarachnoid space as a result of lumbar puncture, surgery, or trauma.10
• Combined malformation is often observed when the lesion involves the vertebrae (e.g., hemivertebrae, absent vertebrae, fused vertebrae, butterfly vertebrae, or midline bony spurs) and is associated with dermal sinuses, myelomeningocele, syringomyelia, and repeated lumbar punctures.11
DISTRIBUTION
• Dermoid cysts represent less than 1% of intraspinal tumors and might be intramedullary, intradural-extramedullary, or extradural.11 The extradural location is the most common site (75%).
HISTOLOGY
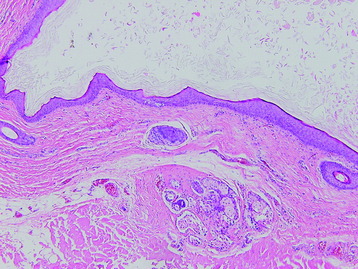
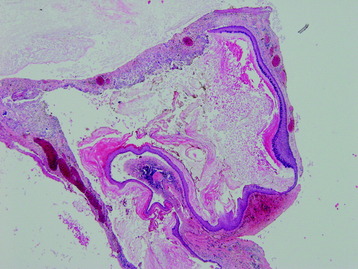
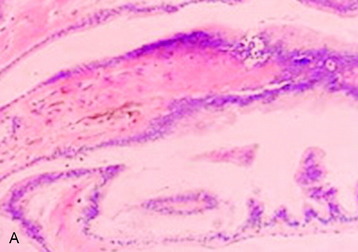
• Microscopic examination shows stratified squamous epithelium with hair follicles, sebaceous glands, and sweat glands (Fig. 5-9).
RADIOLOGY
• MR findings of dermoid tumors show a varied appearance depending on the fat content of the tumor. They are commonly visualized as heterogeneous lesions with very high signal intensity on T1-weighted images (T1WI) and low signal intensity on T2-weighted images (T2WI).10
EPIDERMOID CYST
EPIDEMIOLOGY
• The more common is an anomalous implantation of ectodermal cells during closure of the neural tube between the third and fifth week of embryonic life.14
• Another cause is the displacement of epithelial tissue secondary to previous lumbar puncture. The incidence of this phenomenon has decreased significantly in the last 25 years, but sporadic case reports still exist.15
DISTRIBUTION
HISTOLOGY
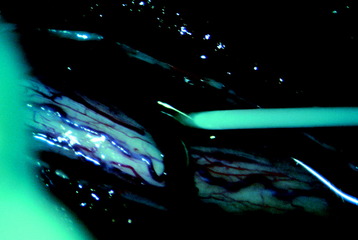
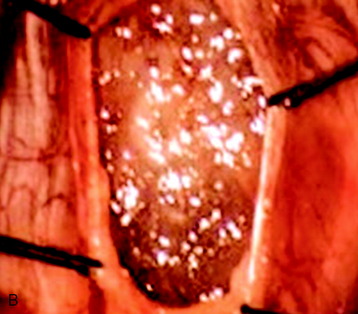
• A well-demarcated plane is noted between the tumor and the spinal cord. Grossly, the lesion is flaky and pearly white.
• Intraoperative spillage of the cyst content (e.g., keratin debris) during removal may lead to a prolonged chemical meningitis and subsequent arachnoiditis. Great concern should be taken not to contaminate the intradural space with cyst content.
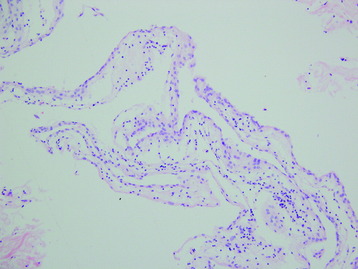
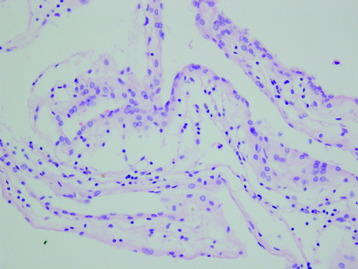
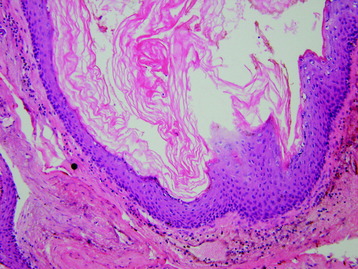
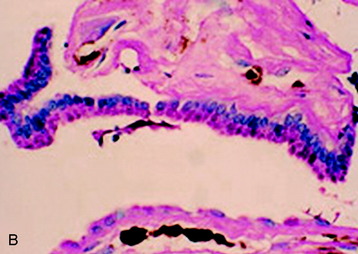
• The histologic examination reveals multiple layers of stratified squamous epithelium and anucleated squames in the cyst (Fig. 5-11). Rupture of cyst evolves foreign body type granulomatous inflammation (Fig. 5-12).
RADIOLOGY
• Radiographic characteristics of epidermoids typically show a displacement of nerve roots and the spinal cord in the subdural space.
• T1- and T2-weighted signal on MRI usually varies from hypointense to isointense but may occasionally have increased intensity on T2WI (Figs. 5-13 to 5-18).16
• This variation in signal characteristics, which might be related to the chemical state of cholesterol or the relative composition of cholesterol and keratin, makes the preoperative diagnosis in the spinal lesions difficult.
• Differential diagnosis is considered with nerve sheath tumor, meningioma, ependymoma, paraganglioma, and intradural lipoma.
NEURENTERIC CYST
EPIDEMIOLOGY
• Neurenteric (NE) cyst is an uncommon developmental lesion lined with epithelium of endodermal origin. This malformation is the result of ectoderm–endoderm adhesion.17
• Approximately one-half of the patients with NE cyst are known to have spinal anomalies, including anterior spina bifida, Klippel–Feil anomaly, other segmentation and fusion anomalies, spinal canal enlargement, diastematomyelia, and posterior spina bifida.18,19
• Their occurrences have been reported by other authors but are rare, comprising 0.7–1.3% of all spinal cord tumors and 16% of cysts.16 About 150 cases with histologic verification have been reported in the literature.17
DISTRIBUTION
Intradural NE cysts are usually located ventral to the spinal cord and are extramedullary lesions.18,19 It also is well known that they are commonly located in cervical, cervicothoracic, and thoracic spine regions.19
RADIOLOGY
• Most intraspinal NE cysts are intradural, extramedullary cystic lesions. Rarely, extraspinal extension through the dural defect has been reported. Intramedullary location also has been reported.
• MR findings are low signal intensity on T1WI and high signal intensity on T2WI. They look like cerebrospinal fluid. NE cysts do not show gadolinium enhancement (Fig. 5-21).
• Differential diagnosis should be considered for cystic intradural extramedullary tumors such as neurilemmoma, epidermoid, or dermoid cysts.
• It is an important differential point that NE cysts have the tendency of ventral location compared with the other cystic tumors.