Intraaortic balloon pump
Equipment
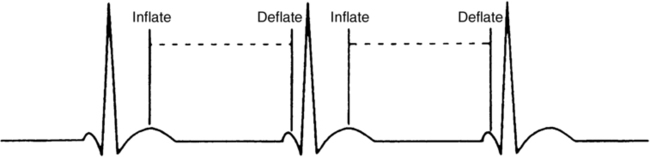
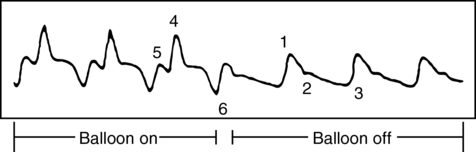
The catheter is connected to a drive console that has a pneumatic pump that uses helium to rapidly inflate the balloon and, just as quickly, deflate the balloon after a brief period of time. Balloon cycling is triggered either from the electrocardiogram R wave, inflating with diastole and deflating with onset of systole (Figure 153-1), or from the aortic pressure waveform. It should be adjusted to inflate when the dicrotic notch occurs in the pressure cycle (Figure 153-2). The balloon can be set to trigger with every beat, every other beat, or some other pattern.