Intensive Care Management of Individuals with Secondary Cardiovascular and Pulmonary Dysfunction
This chapter describes the principles and practice of cardiovascular and pulmonary physical therapy in the management of cardiovascular and pulmonary dysfunction secondary to other conditions that can lead to cardiovascular and pulmonary failure. Some common categories of conditions described include neuromuscular disease, morbid obesity, musculoskeletal trauma, head injury, spinal cord injury, and burns. Each category of condition is presented in two parts. The related pathophysiology and pertinent aspects of the medical management of the condition are presented in relation to the principles of physical therapy management. Invasive care and noninvasive care have common goals and thus are complementary. The principles presented are not treatment prescriptions. Each patient must be assessed and treated individually, taking into consideration the contribution of recumbency, restricted mobility, extrinsic factors related to the patient’s care, and intrinsic factors related to the individual patient (see Chapter 17) in addition to the underlying pathophysiology. Special considerations related to physical therapy intervention such as body positioning and mobilization for cardiovascular and pulmonary failure secondary to other conditions are emphasized.
Neuromuscular Conditions
Pathophysiology and Medical Management
Cardiovascular and pulmonary physical therapy has a central role in minimizing the need for mechanical ventilation in these patients because their prognosis for weaning is poor. Progressive respiratory insufficiency is best addressed early with the institution of nighttime ventilation at home before the development of failure and necessity for hospitalization. Patients with progressive neuromuscular conditions (e.g., muscular dystrophy) are living longer; thus cardiovascular and pulmonary insufficiency will be compounded by age-related changes of the cardiovascular and pulmonary system.1,2
Neuromuscular conditions contribute to cardiovascular and pulmonary dysfunction in numerous ways (see Chapters 6, 22, and 23).3 With progressive deterioration of inspiratory and expiratory muscle strength and endurance, respiratory insufficiency and failure can ensue. Depending on the specific pathology, such deficits include reduced lung volumes and flow rates, reduced alveolar ventilation, increased airway resistance, ventilation and perfusion mismatch, impaired mucociliary transport, accumulation of mucus, reduced cough and gag reflexes, relatively unprotected airway secondary to impaired glottic closure and weakness of the pharyngeal and laryngeal structures, and increased work of breathing.
Iatrogenic effects of medications can confound muscle weakness. Muscle relaxants and corticosteroids are used commonly in the intensive care unit (ICU) and can lead to muscle weakness. The clinical diagnosis of ICU-acquired weakness is achieved by clinical assessment, electrophysiological studies, and morphologic analysis of muscle and nerve tissue.4
Principles of Physical Therapy Management
A patient with restrictive pulmonary disease secondary to neuromuscular conditions is at considerable risk of succumbing to the negative cardiovascular and pulmonary sequelae of reduced mobility and recumbency, in addition to the pathophysiological consequences of respiratory failure. Provided the patient has some residual muscle power, the balance between oxygen demand and supply will determine the degree to which mobilization can be exploited to maximize oxygen transport.5 The treatment goals for these patients are to maximize oxygen delivery, enhance the efficiency of oxygen uptake and usage, and thereby reduce the work of breathing. In these patients, minimizing oxygen demand overall (i.e., during mobilization as well as at rest) is a priority. Mobilization needs to be prescribed in body positions that enhance oxygen transport and its efficiency so that the benefits of mobilization can be exploited more fully without worsening arterial oxygenation. The patient requires continuous monitoring of oxygen transport and hemodynamic monitoring to ensure the exercise stimulus is optimally therapeutic and not excessive.
Patients who are hypotonic and generally weak and debilitated fail to adapt normally to position-dependent fluid shifts and thus are more prone to orthostatic intolerance.6 Gravitational stimulation is essential to maintain the volume-regulating mechanisms. Tilt tables should be used judiciously given the potential risks in these patients, which are compounded by the loss of the lower-extremity muscle pump mechanism. Stretcher chairs may be preferable. Because of potential adverse reactions to fluid shifts and the potential for desaturation, falling PaO2 levels, and dysrhythmias, the patient’s hemodynamic status must be monitored closely during gravitational challenges.
The importance of chest wall mobility to optimize three-dimensional chest wall excursion in individuals with chronic neurological conditions is emphasized in Chapters 22 and 23. This goal is particularly challenging if complicated by acute respiratory insufficiency. The goal is to promote alveolar ventilation, reduce areas of atelectasis, and optimize ventilation and perfusion matching and breathing efficiency to augment and minimize reliance on respiratory support (i.e., supplemental oxygen and mechanical ventilation) while minimizing respiratory distress. This is especially important because patients with neuromuscular conditions are poor candidates for being weaned off mechanical ventilation. In addition, these patients are prone to microaspiration. Promotion of mucociliary transport is therefore essential to facilitate clearing of aspirate and minimize bacterial colonization and risk of infection.
Another major problem for patients with restrictive lung disease secondary to generalized weakness and neuromuscular disease is an ineffective cough. Cough facilitation techniques (e.g., body positioning, abdominal counter pressure, and tracheal tickle; see Chapters 22 and 23) can be used to increase intraabdominal and intrathoracic pressures and cough effectiveness. A natural cough, even when facilitated, is preferable and more effective in dislodging mucus from the sixth or seventh generation of bronchi than repeated suctioning. Even a weak, facilitated cough may be effective in dislodging secretions to the central airways for removal by suctioning or for redistribution of peripheral secretions.7 Huffing, a modified cough performed with the glottis open and with abdominal support, may help mobilize secretions in patients with generalized weakness. In some cases suctioning may be the only means of eliciting a cough and clearing secretions simultaneously. Coughing attempts are usually exhausting for these patients. Thus ample rest periods must be interspersed during treatment, particularly for the ventilated patient. Coughing maneuvers must be strategically planned. Even though the patient may be able to effect only a series of a few weak coughs, it is essential that these attempts be maximized (i.e., the patient, optimally rested and medicated [e.g., bronchodilators, analgesia, reduced sedation and narcotics], is physically positioned to optimize length-tension relationship of the diaphragm and abdominal muscles; is positioned vertically to optimize inspiratory lung volumes and expiratory flows and avoid aspiration; and is provided thoracic and abdominal support during expiration to maximize intrathoracic and intraabdominal pressures) (see Chapter 22). These supportive measures will ensure that the benefits of the normal physiological cough mechanism, which is the single best secretion clearance technique, are maximized (i.e., the most productive cough with the least energy expenditure).8 Forced chest wall compression or forced expiratory maneuvers are contraindicated because of airway closure and impairment of gas exchange.9
Obesity
Pathophysiology and Medical Management
Principles of Physical Therapy Management
Although patients who are obese do not tolerate the prone position well, the semiprone position can be beneficial by simulating the benefits of the upright lean-forward position on the displacement of the abdominal viscera.10 This position also simulates the prone abdomen-free position, which is associated with even greater benefit than the prone abdomen-restricted position. The benefits of the prone position for the obese individual include increased lung compliance and enhanced gas exchange and oxygenation. The full prone abdomen-restricted position is contraindicated in the obese individual with cardiovascular and pulmonary failure, however, because this position can compromise diaphragmatic descent and contribute to further cardiovascular and pulmonary distress and failure and possibly cardiac arrest.
Musculoskeletal Trauma
Pathophysiology and Medical Management
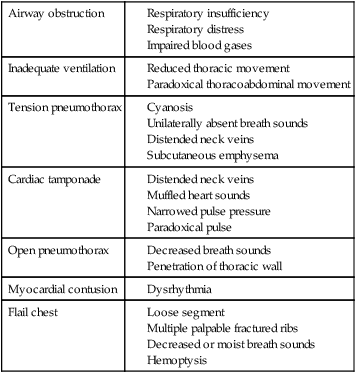
Crush and penetrating injuries of the chest are commonly seen in the ICU. Damage to the chest wall, lung parenchyma, and heart contributes to the risk of cardiovascular and pulmonary failure (Table 35-1). Associated injuries of the head, spinal cord, and abdomen may also contribute. Fractures of long bones and the pelvis are associated with fat emboli, which pose the threat of pulmonary embolism. In addition, fluid loss in multiple trauma contributes to loss of blood volume, hypovolemia, and hemodynamic instability. The more extensive the injuries, the greater the pain and requirement for analgesia. Pain contributes significantly to reduced alveolar ventilation, airway closure, and inefficient breathing patterns.
Table 35-1
Factors Contributing to Cardiovascular and Pulmonary Failure after Trauma and Their Diagnostic Signs
| Airway obstruction | |
| Inadequate ventilation | |
| Tension pneumothorax | |
| Cardiac tamponade | |
| Open pneumothorax | |
| Myocardial contusion | |
| Flail chest |
Analysis of blood gases in the patient who has sustained traumatic injuries to the chest often shows severe hypoxemia and moderate elevations of arterial PCO2. The presence of acidemia is common, which may have both respiratory and metabolic components. Patients with severe injuries have improved outcomes if hemodynamic status can be optimized.11 Being less than 40 years of age is the best predictor of achieving optimal levels. Increasing DO2 and maintaining normal SVO2 are particularly relevant goals.12
Principles of Physical Therapy Management
Multiple Trauma
The management of multiple trauma is a major challenge for the ICU team. Multisystem involvement and complications often present a precarious situation in which priorities have to be defined for each individual situation. Multiple trauma can include head injury, chest wall injuries, fractures, lung contusions, diaphragm injury, pleural space disorders, internal injuries, thromboemboli, fat emboli, and cardiac contusions. Deep vein thrombosis occurs in 20% to 40% of patients in the absence of prophylaxis.13 Shock and acute respiratory distress syndrome (ARDS) may ensue (see Chapter 36). Early intervention with body positioning significantly lowers the incidence of ARDS compared with later intervention in patients with multiple trauma.14 The clinical picture of the patient with multiple trauma is compounded by the mobilization and positioning restrictions imposed.15 Positive end-expiratory pressure (PEEP) is frequently used to reduce the effects of lung congestion secondary to shock or ARDS. Arterial blood gases are assessed to evaluate the effectiveness of PEEP in effecting improved oxygen transfer.
Multiple Fractures
Relaxation interventions, both active and passive, should be integrated into the treatment regimen for the trauma patient to reduce excessive oxygen consumption and promote comfort.16 Active relaxation refers to relaxing the patient through participation of the patient in relaxation procedures. Passive relaxation refers to relaxing the patient using passive procedures (e.g., body positioning, physical supports, talking slowly and calmly, and taking adequate time for conducting treatments). Taking time to implement mobilization is essential. First, mechanically moving and having patients who have multiple injuries move, requires a prolonged period of time. In addition, the cardiovascular and pulmonary systems of patients who are critically ill need time to adapt to new positions physiologically and to control discomfort. Prolonged periods of time may be required to turn a patient, dangle him or her over the bed, or transfer him or her to a chair with continuous monitoring. Every effort is made to maintain the patient’s spirits, reduce stress, and encourage a positive attitude toward active participation early in the rehabilitation program that begins in the ICU.
Head Injury
Pathophysiology and Medical Management
The head of the bed is usually maintained at 30 to 40 degrees to promote venous drainage and thereby reduce ICP. The patient’s head and neck can be fixed in a neutral position by halo traction or by sandbags positioned on either side (Figure 35-1). Mechanical hyperventilation is used to maintain PCO2 below normal limits but above 20 mm Hg. Arterial blood gases are checked during or immediately after hyperventilation. Prolonged hyperventilation is avoided.
A complication of head injuries is acute lung injury, specifically neurogenic pulmonary edema (see Chapter 36). Autonomical nervous system dysfunction contributes to hypertension and neurogenic pulmonary edema. The endothelial tight junctions in the pulmonary capillaries leak protein into the interstitium along with fluid. Constriction of the lymphatic vessels may also contribute to fluid accumulation by impeding the removal of lung water. Increased fluid accumulation in the interstitium may progress to the alveoli, contributing further to impaired gas exchange and reduced lung compliance.
Principles of Physical Therapy Management
Physical therapy priorities in the management of the patient with cardiovascular and pulmonary dysfunction secondary to head injury are shown in Box 35-1. Body positioning, a mainstay of treatment for the patient with reduced consciousness, is based on a detailed assessment, consideration of multisystem status, and serial monitoring of the patient’s response.17
If the ICP is unstable and a risk of brain damage exists, physical therapy should follow sedation. Ideally treatments should be performed when the ICP is low and intracranial compliance is satisfactory. Patients whose cerebral compliance is compromised need monitoring during position changes.18 The head-down position is contraindicated. Noise and noxious stimulation that increases ICP should be kept to a minimum.
Spinal Cord Injury
Pathophysiology and Medical Management
Spinal cord injuries above C3 result in loss of phrenic nerve innervation, necessitating a tracheostomy and mechanical ventilation. The lower the level of the spinal cord lesion, the lower the cardiovascular and pulmonary risk. All patients with spinal cord injuries are at risk for developing atelectasis and pneumonia. The coughing mechanics of patients with quadriplegia are abnormal and contribute to ineffective airway clearance.19 In addition, the quadriplegic patient is at risk for developing pulmonary emboli. Prophylactic low-dose heparin is used routinely unless the presence of pulmonary emboli is suspected and higher doses are indicated.
Principles of Physical Therapy Management
Because of the need to maintain relative immobility in the acute stabilization period of suspected spinal cord injury, therapeutic body positioning rather than mobilization is a primary intervention for optimizing oxygen transport. Although modified body positioning can be achieved, the provision of optimal care under these restricted conditions is a singularly important challenge to the physical therapist, particularly with respect to the management of adequate oxygen transport while the patient is in the ICU. Patients with high spinal cord lesions can be positioned in all positions within the limits of the cervical traction device being used, barring head injury. Both head- and foot-tipped positions, however, are introduced cautiously and with hemodynamic monitoring because both positions can have significant cardiovascular and pulmonary and hemodynamic consequences secondary to spinal nerve loss and hence sympathetic nerve loss to the peripheral blood vessels. Turning frames such as the Stryker frame facilitate turning and tipping of these hemodynamically labile patients in the supine and prone positions.20
Effective body positioning, despite the need in some cases for extensive modification, may be sufficient to optimize oxygen transport secondary to improved regional ventilation and perfusion to all lung fields. In the spontaneously breathing patient, deep breathing and coughing maneuvers need to be coupled with position changes to optimize mucociliary transport. Some patients may not tolerate numerous positions and position changes and thus have impaired mucociliary transport. If secretion accumulation and stasis develop, postural drainage can be instituted; however, tipping must be attempted very cautiously. Patients should be monitored closely during and after treatment. Because of the hemodynamic lability of acute quadriplegic patients and the well-documented side effects of percussion and vibration,8 these procedures must be applied cautiously, should they be indicated, depending on the severity of any complicating fracture-dislocation(s), the stability of fixation, the condition of the lungs, the presence of chest wall injuries, and hemodynamic lability.
Respiratory muscle weakness and fatigue, two physiologically distinct entities, are probably much more common in patients in the ICU than appreciated. These states need to be recognized and detected early because both are well known to cause respiratory muscle failure.21 The distinction between the two conditions is that weakened muscles respond to resistive muscle training, whereas fatigued muscles do not. Exposing fatigued respiratory muscles to resistive loads can accentuate respiratory failure. The indication for respiratory muscle training, therefore, is weak rather than fatigued respiratory muscles. Rest is indicated for fatigued respiratory muscles. Whether the respiratory muscles are weak or fatigued must be established before respiratory muscle training is prescribed. Patients with quadriplegia with weak respiratory muscles, even if ventilated for a prolonged period, potentially may be weaned (low-level injury) or minimally may breathe independently for brief periods after a course of inspiratory muscle training.22 For further detail on respiratory muscle training refer to Chapter 26.
Burns
Pathophysiology and Medical Management
Cardiovascular and pulmonary complications are common in patients with smoke inhalation with or without severe burns and are a major cause of death. Smoke and chemical inhalation produce edema, bronchospasm, cough, mucosal sloughing, hemorrhage, hoarseness, stridor, and profuse carbonaceous secretions. Irritation of the alveoli and acute pulmonary edema can result in a condition resembling ARDS (see Chapter 36).
Treatment is directed at improving arterial saturation, maintaining fluid balance, and preventing infection. Hypoxemia is effectively treated with the administration of oxygen and maintenance of clear airways. If the patient is breathing spontaneously, oxygen is given via nasal cannulas or mask at flows of 1 to 5 L/min, depending on the arterial oxygen saturation. Moisture can be administered through a face tent with a heated nebulizer. Fluid balance is particularly challenging in the patient with burns because of the loss of skin, which is essential to the retention and compartmentalization of body fluids and in the regulation of fluid and electrolyte loss from the body. In addition, these patients may lose blood because of injury at the time of the accident. There is also a period without fluid replacement from before the injury to the time medical attention is available and intravenous fluid resuscitation commenced. Because of the nature of burns, even when fluid resuscitation has begun, fluid and electrolyte balance remains a challenge until considerable healing and repair have occurred. Fluid and electrolyte imbalances have considerable implications for hemodynamics and cardiovascular and pulmonary function (see Chapter 16) and contribute to hemodynamic instability, which necessitates modification of the physical therapy management.
Principles of Physical Therapy Management
Cardiovascular and pulmonary physical therapy often has to be modified in the patient with burns. Mobilization to enhance oxygen transport is exploited as much as possible; however, because of blood volume and hemodynamic problems, orthostatic intolerance may limit mobilization and positioning alternatives. With more severe burns and more extensive burn distribution, body positioning is the primary intervention. Positioning for an optimal therapeutic effect on oxygen transport is challenging because of the significant physical limitations that may exist. Given that body positioning profoundly influences ventilation and perfusion matching,23 the reduced number of positioning alternatives will contribute to shunt, ventilation and perfusion mismatch, and hypoxemia. This effect will be accentuated if the patient is mechanically ventilated (see Chapter 33).
Patients who have skin grafts require particular care during moving or positioning because of the danger of shearing forces on the graft, which can disrupt the circulation, nutrition, and healing of the new skin. Sterile procedures must be observed at all times. The physical therapist is usually required to cap, gown, mask, and glove before treating the patient with extensive exposed areas and to cover the chest with a sterile drape. Facilitating mucociliary transport is a priority if the patient has significant mobility and positioning restrictions because of the burn severity. Wherever possible, mobilization in conjunction with multiple body positions and position changes is attempted to maximize mucociliary clearance.24 If secretions have accumulated, positioning for postural drainage requires the same consideration as positioning for improved alveolar ventilation and ventilation and perfusion matching. In the spontaneously breathing patient, postural drainage positions can be used selectively to increase alveolar volume in the superior lung fields and alveolar ventilation to inferior lung fields, in addition to facilitating drainage of the superior bronchopulmonary segments. If the patient is mechanically ventilated, however, the superior lung fields are preferentially ventilated (see Chapter 33). Should the addition of manual techniques be indicated, percussion may not be comfortably tolerated in the presence of first- and second-degree burns. Manual vibration may be substituted. Manual techniques are contraindicated over freshly grafted skin; however, manual vibration may be transmitted from a more distal site to a lung field that cannot be vibrated directly.
Organ Transplantation
Optimal nutrition and exercise have been advocated as means of improving outcomes before and after transplantation.25 The benefits of regular physical exercise have been well documented for patients who have had transplants. The benefits, however, begin in the ICU, where mobilization is prescribed to reap similar benefits including improved oxygen transport and physical conditioning and to potentially reduce or attenuate the side effects of immunosuppression.26,27 In addition, the progression from mobilization in the ICU and hospital to the community can also help to address conditions that are often seen in these patients, including hypertension, type 2 diabetes mellitus, hyperlipidemia, and other cardiovascular risks. Once discharged, patients may attain a similar or even higher level of health and conditioning than their peers who have not undergone transplantation surgery.






