71
Infestations
Scabies
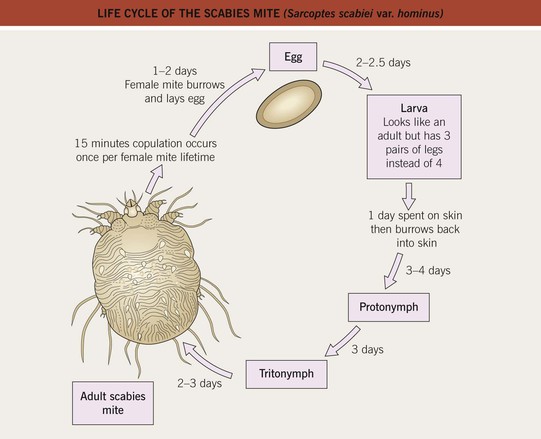
• Infestation by Sarcoptes scabiei var. hominis, a mite that lives within the stratum corneum of human skin (Fig. 71.1).

Fig. 71.1 Female scabies mite with egg. The female scabies mite in a potassium hydroxide wet mount obtained from skin scrapings, revealing a flattened, oval body with wrinkle-like corrugations, eight short legs, and an egg ready for deposition (40×). With permission from Taplin D, Meinking TL. Infestations. In: Schachner LA, Hansen RC (Eds.), Pediatric Dermatology, 4th edn. Edinburgh, UK: Mosby, 2011:1141–1180.
• Asymptomatic infestation by scabies is not uncommon (‘carriers’ of scabies).
• Skin lesions are variable and include erythematous papules with scale-crust, small patches of eczema, excoriations, vesicles (especially acrally in infants), and nodules; the classic burrow – a thread-like, grayish-white, wavy, 1- to 10-mm linear structure – favors acral sites (Figs. 71.2 and 71.3).



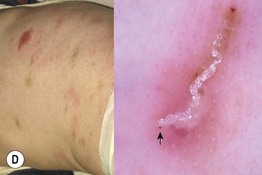



Fig. 71.2 Scabies. A, B Erythematous papules, linear burrows, areas of crusting and acral vesiculopustules in two infants with scabies. C Close-up of a linear burrow post scraping for examination under mineral oil. D By dermoscopy, a characteristic ‘jet with contrail’ structure can be identified corresponding to the anterior part of the mite (arrow) and the burrow behind it. E, F Penile involvement with erythematous papules and nodules.G Nodular scabies in an infant. D, Courtesy, Iris Zalaudek, MD; F, Courtesy, Robert Hartman, MD. G, Courtesy, Kalman Watsky, MD.
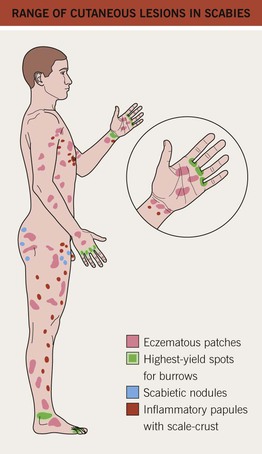
Fig. 71.3 Range of cutaneous lesions in scabies. Typical sites affected by scabies are highlighted. In infants and the elderly or immunocompromised, all surfaces can be involved, including the scalp and face.
• Clinical confirmation is by mineral oil examination of skin scrapings (see Chapter 2) or dermoscopy (see Fig. 71.2D).
• Usually <100 mites, but often no more than 10–15, living on an infested individual (Fig. 71.4); there may be thousands of mites in crusted scabies (thick scale, especially acrally, with minimal inflammation), which affects immunocompromised hosts, those with altered skin sensation, and sometimes the elderly (Fig. 71.5).

Fig. 71.5 Crusted scabies. Asymptomatic hyperkeratosis of the hands, which may be misdiagnosed as hand dermatitis. This disorder was previously referred to as Norwegian scabies. Courtesy, Joyce Rico, MD.
• DDx: arthropod bites, including bites of animal mites (e.g. Cheyletiella); diseases associated with generalized pruritus (e.g. atopic dermatitis; see Table 4.1); in infants, infantile acropustulosis, which may also occur following successful treatment of scabies.
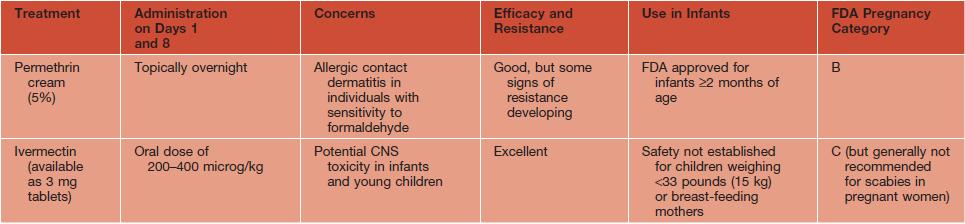
– Permethrin 5% cream is the preferred topical agent.
– All clothing and bedding should be washed in hot water and dried with high heat, or stored in a bag for 10 days (3 days after the second treatment).
– All family members and close contacts should be treated simultaneously, even if asymptomatic.
Table 71.1
Topical and oral treatments for scabies.
All treatments should be given on two separate occasions, 1 week apart. Other topical therapies are sometimes utilized, based on availability, but suffer from inferior efficacy and toxicities, e.g. lindane (CNS toxicity), sulfur 5–10%, and crotamiton.
Head Lice (Pediculosis Capitis)
• Secondary to Pediculus capitis, a bloodsucking, six-legged insect that lays its eggs near the base of the hairs on the scalp (Fig. 71.6); the casing remains after the egg hatches and migrates outward with growth of the hair shaft.

Fig. 71.6 Head louse family. From left to right: female, male, and nymph. With permission from Taplin D, Meinking TL. Infestations. In: Schachner LA, Hansen RC (Eds.), Pediatric Dermatology, 4th edn. Edinburgh, UK: Mosby, 2011:1141–1180.
• Transmission is by direct contact with an infested person or fomites (e.g. hats, brushes).
• Diagnosis is generally made by visual examination, followed by microscopic inspection and the detection of 0.8 mm eggs or their casings attached to scalp hairs (‘nits’); high-yield locations include hairs above the ears and the lower occipital scalp (Fig. 71.7).


Fig. 71.7 Head lice. A The head louse egg or nit is 0.8 mm in length. B Head lice nits on hair. With permission from Taplin D, Meinking TL. Infestations. In: Schachner LA, Hansen RC (Eds.), Pediatric Dermatology, 4th edn. Edinburgh, UK: Mosby, 2011:1141–1180.
• DDx of scalp pruritus: seborrheic dermatitis, psoriasis, atopic dermatitis.
• DDx of nits: hair casts, dandruff, hair gel, and other causes of hair shaft nodules (see Fig. 64.3).
Table 71.2
Topical and oral treatments for head lice.
All treatments should be given on two separate occasions, 1 week apart, with the exception of a single application for ivermectin lotion. Carbaryl shampoo (0.5%), lindane shampoo (1%), and permethrin cream (5%) are sometimes used, but generally have inferior efficacy.
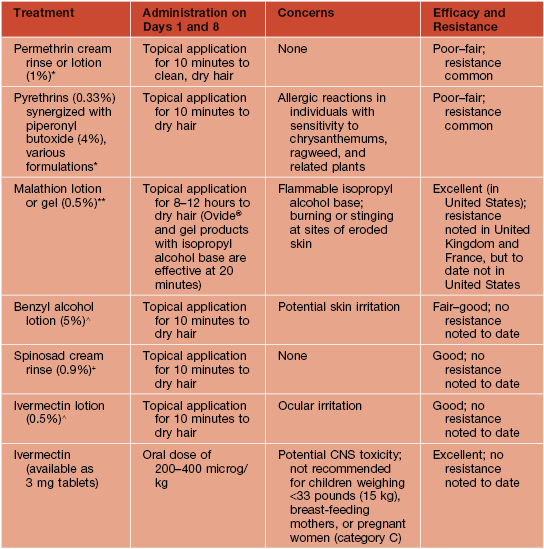
* Over-the-counter products.
** Approved for individuals ≥6 years of age; pregnancy category B.
+ Approved for individuals ≥4 years of age; avoid in infants <6 months of age; pregnancy category B.
∧ Approved for individuals ≥6 months of age; pregnancy category B.
Crab Lice (Pediculosis Pubis)
• While body and head lice are similar in appearance, crab lice are shorter and broader, thus actually resembling crabs (Fig. 71.8).

Fig. 71.8 Adult crab louse. The shape is shorter and broader than that of head and body lice. Courtesy, Tony Burns, MD.
• May coexist with other STDs; pruritus is common.
• In addition to lice that are attached to hairs or moving about the surface of the skin (Fig. 71.9A), hemorrhagic crusts, perifollicular erythema, and macula caerulea (asymptomatic slate-gray to blue macules on the trunk and thighs) may be seen; secondary bacterial infection may also occur.


Fig. 71.9 Crab lice. A Both adult crab lice and nits are evident on pubic hairs. B Crab lice nits and feces on the eyelashes. A, Courtesy, Louis A. Fragola, Jr., MD; B, With permission from Taplin D, Meinking TL. Infestations. In: Schachner LA, Hansen RC (Eds.), Pediatric Dermatology, 4th edn. Edinburgh, UK: Mosby, 2011:1141–1180.
• If the infestation involves the eyelashes, feces can accumulate at the base of the hairs and at the inferior margin of the lower eyelid (Fig. 71.9B).
• DDx: other causes of genital pruritus; nits must be distinguished from other causes of hair nodules (see Fig. 64.3).
Table 71.3
Topical and oral treatments for crab lice.
All crab lice treatments should be given on two separate occasions, 1 week apart. Lindane shampoo (1%) is occasionally used but has inferior efficacy.
| Treatment | Administration on Days 1 and 8 | Efficacy |
| Permethrin (1%) cream rinse or synergized pyrethrin shampoo* | Topical application for 10 minutes to clean, dry hair | Fair |
| Permethrin cream (5%) | Topical application for 8–12 hours | Good |
| Ivermectin (available as 3 mg tablets) | Oral dose of 250 microg/kg | Excellent |
* Over-the-counter product.
Body Lice (Pediculosis Corporis)
• Associated with overcrowding, poor hygiene, poverty, wars, and natural disasters.
• Severe pruritus common, especially on the back, waist, shoulders, and neck.
• Body lice and nits are primarily found in clothing seams (Fig. 71.10).

Fig. 71.10 Body lice eggs in the seams of clothing.
• DDx: bites from other arthropods and other causes of generalized pruritus (see Table 4.1).
Tungiasis
• Secondary to the burrowing flea, Tunga penetrans.
• Endemic in Central and South America, Caribbean Islands, Africa, Pakistan, and India.
• Pregnant female flea burrows into the skin, especially on the feet of individuals who do not wear shoes or wear only flip-flops (Fig. 71.11).

Fig. 71.11 Tungiasis in a child. Courtesy, Terri L. Meinking, MD, Craig N. Burkhart, MD, and Craig G. Burkhart, MD.
• Commonly, a 1- or 2-cm nodule with surrounding erythema develops; there may be multiple lesions.
• Rarely, tetanus, gangrene, or autoamputation may result.
• Rx: removal of the flea; tetanus prophylaxis should be considered.
• Prevention: wear shoes and avoid sitting on sandy beaches in endemic areas.
Cutaneous Myiasis
• Infestation of skin by fly larvae; furuncular myiasis presents as a boil-like lesion, most commonly secondary to Dermatobia hominis (human botfly) and Cordylobia anthropophaga (tumbu fly); wound myiasis is most often due to Cochliomyia hominivorax or Chrysomya bezziana (Fig. 71.12).



Fig. 71.12 Cutaneous myiasis. A Furuncular myiasis presenting as a papulonodule with a central punctum on the leg. B Wound myiasis in an amputation stump. C Botfly larva. B, Courtesy, Louis A. Fragola, Jr., MD.
• Complications may occur, especially when the sinuses, nasal cavity, or scalp are involved.
• DDx for furuncular myiasis: ruptured cyst, abscess, furunculosis, and foreign body reaction.
For further information see Ch. 84. From Dermatology, Third Edition.