Infections of the Eyes, Ears, and Sinuses
1. Describe the anatomy of the eye, including naming the external and internal structures.
2. Name the three tissues, outer to inner, of the eyeball.
3. Differentiate normal flora of the eye and potential pathogens.
4. Describe the defense mechanisms of the eye for the protection from infective agents.
5. Define the following diseases of the eye: blepharitis, conjunctivitis, keratitis, and endophthalmitis.
6. List the common types of eye infections, the associated etiologic agents, and the at-risk patient population for each.
7. Define keratitis, and identify the organisms associated with the infection, the virulence factors, and the antimicrobial-resistant properties for each.
8. Define endophthalmitis, explain how it is contracted, and identify the etiologic agents.
9. Explain mycotic endophthalmitis, and list the risk factors that may predispose an individual to this type of infection.
10. Define a periocular infection, and list some of the associated infectious agents and the different types of clinical presentations of the infection.
11. Identify the anatomic parts of the ear, and list the structures associated with each region within the ear.
12. Define the following external ear infections: acute externa otitis and chronic externa otitis; list the potential pathogens.
13. Define otitis media; differentiate acute and chronic otitis media, and name the most frequently encountered pathogens and the age group most often affected by this disease.
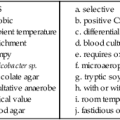
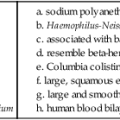
14. Explain the laboratory method used to culture the eye and the ear, including appropriate media; describe collection and transportation requirements.
15. Differentiate acute and chronic sinusitis.
16. Explain why the organisms causing otitis media are often the same ones responsible for sinusitis.
17. List the collection methods and culture media used for cases of sinusitis.
18. Correlate signs and symptoms of infection with the results of laboratory diagnostic procedures for the identification of the etiologic agent associated with infections of the eye, ear, and sinuses.
Eyes
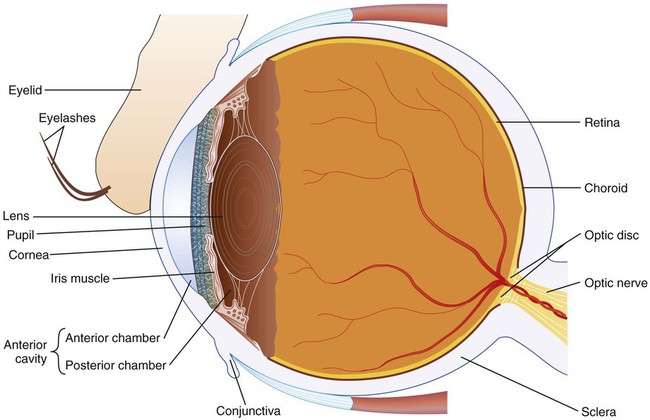
Anatomy
The external structures of the eye—eyelids, conjunctiva, sclera, and cornea—are depicted in Figure 72-1. The eyeball comprises three layers. From the outside in, these tissues are the sclera, choroid, and retina. The sclera is a tough, white, fibrous tissue (i.e., “white” of the eye). The anterior (toward the front) portion of the sclera is the cornea, which is transparent and has no blood vessels. A mucous membrane, called the conjunctiva, lines each eyelid and extends onto the surface of the eye itself.
Only a small portion of the eye is exposed to the environment; about five sixths of the eyeball is enclosed within bony orbits shaped like four-sided pyramids. The large interior space of the eyeball is divided into two sections: the anterior and posterior cavities (see Figure 72-1). The anterior cavity is filled with a clear and watery substance called aqueous humor; the posterior cavity is filled with a soft, gelatin-like substance called vitreous humor.
Diseases
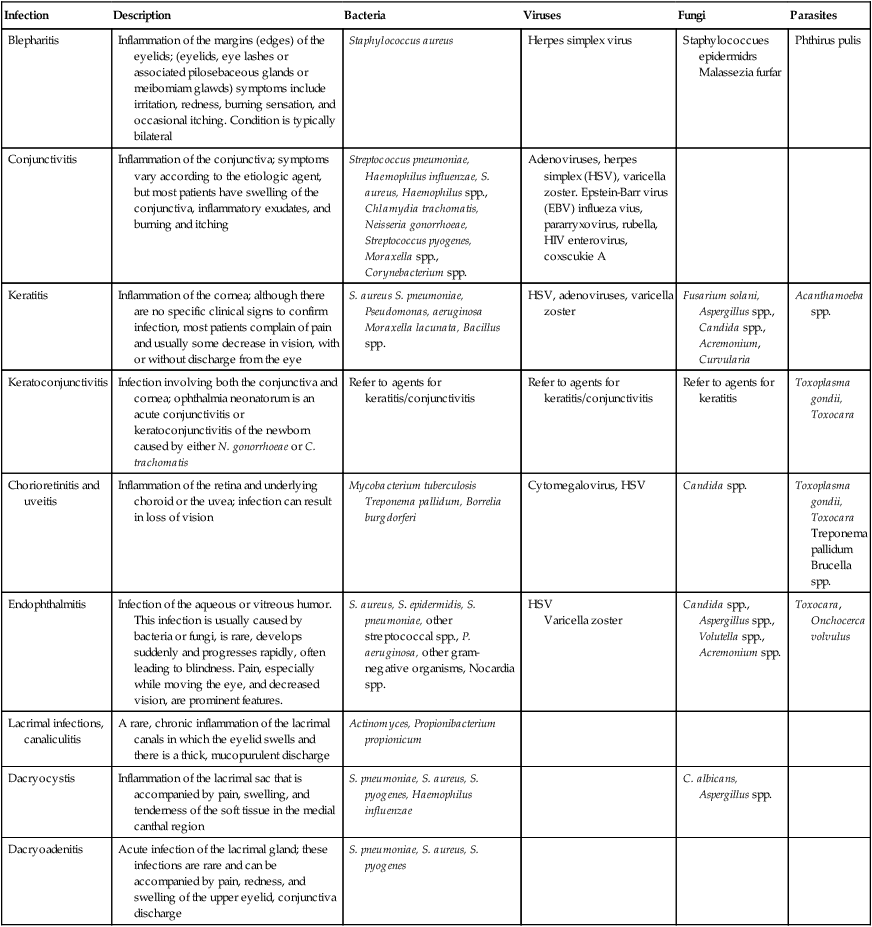
The eye and its associated structures are uniquely predisposed to infection by various microorganisms. The major infections of the eye are listed in Table 72-1 along with a brief description of the disease.
TABLE 72-1
| Infection | Description | Bacteria | Viruses | Fungi | Parasites |
| Blepharitis | Inflammation of the margins (edges) of the eyelids; (eyelids, eye lashes or associated pilosebaceous glands or meibomiam glawds) symptoms include irritation, redness, burning sensation, and occasional itching. Condition is typically bilateral | Staphylococcus aureus | Herpes simplex virus | Staphylococcues epidermidrs Malassezia furfar |
Phthirus pulis |
| Conjunctivitis | Inflammation of the conjunctiva; symptoms vary according to the etiologic agent, but most patients have swelling of the conjunctiva, inflammatory exudates, and burning and itching | Streptococcus pneumoniae, Haemophilus influenzae, S. aureus, Haemophilus spp., Chlamydia trachomatis, Neisseria gonorrhoeae, Streptococcus pyogenes, Moraxella spp., Corynebacterium spp. | Adenoviruses, herpes simplex (HSV), varicella zoster. Epstein-Barr virus (EBV) influeza vius, pararryxovirus, rubella, HIV enterovirus, coxscukie A | ||
| Keratitis | Inflammation of the cornea; although there are no specific clinical signs to confirm infection, most patients complain of pain and usually some decrease in vision, with or without discharge from the eye | S. aureus S. pneumoniae, Pseudomonas, aeruginosa Moraxella lacunata, Bacillus spp. | HSV, adenoviruses, varicella zoster | Fusarium solani, Aspergillus spp., Candida spp., Acremonium, Curvularia | Acanthamoeba spp. |
| Keratoconjunctivitis | Infection involving both the conjunctiva and cornea; ophthalmia neonatorum is an acute conjunctivitis or keratoconjunctivitis of the newborn caused by either N. gonorrhoeae or C. trachomatis | Refer to agents for keratitis/conjunctivitis | Refer to agents for keratitis/conjunctivitis | Refer to agents for keratitis | Toxoplasma gondii, Toxocara |
| Chorioretinitis and uveitis | Inflammation of the retina and underlying choroid or the uvea; infection can result in loss of vision | Mycobacterium tuberculosis Treponema pallidum, Borrelia burgdorferi |
Cytomegalovirus, HSV | Candida spp. | Toxoplasma gondii, Toxocara Treponema pallidum Brucella spp. |
| Endophthalmitis | Infection of the aqueous or vitreous humor. This infection is usually caused by bacteria or fungi, is rare, develops suddenly and progresses rapidly, often leading to blindness. Pain, especially while moving the eye, and decreased vision, are prominent features. | S. aureus, S. epidermidis, S. pneumoniae, other streptococcal spp., P. aeruginosa, other gram-negative organisms, Nocardia spp. | HSV Varicella zoster |
Candida spp., Aspergillus spp., Volutella spp., Acremonium spp. | Toxocara, Onchocerca volvulus |
| Lacrimal infections, canaliculitis | A rare, chronic inflammation of the lacrimal canals in which the eyelid swells and there is a thick, mucopurulent discharge | Actinomyces, Propionibacterium propionicum | |||
| Dacryocystis | Inflammation of the lacrimal sac that is accompanied by pain, swelling, and tenderness of the soft tissue in the medial canthal region | S. pneumoniae, S. aureus, S. pyogenes, Haemophilus influenzae | C. albicans, Aspergillus spp. | ||
| Dacryoadenitis | Acute infection of the lacrimal gland; these infections are rare and can be accompanied by pain, redness, and swelling of the upper eyelid, conjunctiva discharge | S. pneumoniae, S. aureus, S. pyogenes |
Epidemiology and Etiology of Disease
Blepharitis
Conjunctivitis
Bacterial conjunctivitis, commonly referred to as “pink eye,” is the most common type of ocular infection and may be caused by allergies or bacterial or viral infection. The principal causes of acute conjunctivitis in the normal host are listed in Table 72-1. Age-related factors are key in the identification of the etiologic agent. In neonates, neisserial and chlamydial infections are frequent and are acquired during passage through an infected vaginal canal. With the common practice of instilling antibiotic drops into the eyes of newborns in the United States, the incidence of gonococcal and chlamydial conjunctivitis has dropped dramatically. However, Chlamydia trachomatis remains responsible for one of the most important types of conjunctivitis, trachoma, one of the leading causes of blindness in the world, primarily in underdeveloped countries.
Endophthalmitis
Mycotic infection of the eye has increased significantly since the 1980s because of the increased use of antibiotics, corticosteroids, antineoplastic chemotherapy, addictive drugs, and hyperalimentation (overeating). Fungi generally considered to be saprophytic are important causes of postoperative endophthalmitis (see Table 72-1). Endogenous mycotic endophthalmitis is most often caused by Candida albicans. High-risk patients include those with diabetes or some other chronic underlying disease. Other causes of hematogenous ocular infection include Aspergillus, Cryptococcus, Coccidioides, Sporothrix, and Blastomyces.
Periocular
Canaliculitis, one of three infections of the lacrimal apparatus (see Table 72-1), is an inflammation of the lacrimal canal and is usually caused by Actinomyces or Propionibacterium propionicum (formerly Arachnia). Infection of the lacrimal sac (dacryocystitis) may involve numerous bacterial and fungal agents; the major causes are listed in Table 72-1. Dacryoadenitis is an uncommon infection of the lacrimal gland characterized by pain of the upper eyelid with erythema and often involves pyogenic bacteria such as S. aureus and streptococci. Chronic infections of the lacrimal gland occur in tuberculosis, syphilis, leprosy, and schistosomiasis. Acute inflammation of the gland may occur during the course of the mumps and infectious mononucleosis.
Ears
Anatomy
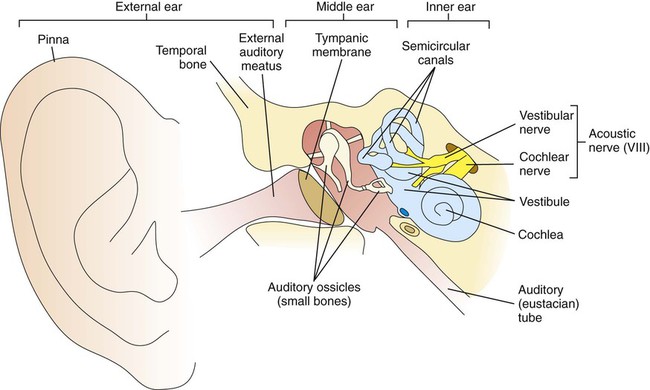
The ear is divided into three anatomic parts: the external, middle, and inner ear. Important anatomic structures are depicted in Figure 72-2.
Diseases, Epidemiology, and Etiology of Disease
Otitis Externa (External Ear Infections)
Otitis Media (Middle Ear Infections)
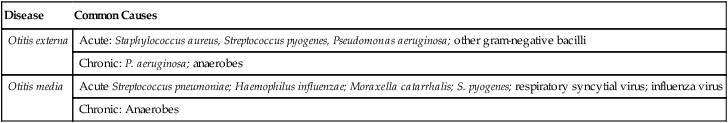
Chronic otitis media yields a predominantly anaerobic flora, with Peptostreptococcus spp., Bacteroides fragilis group, Prevotella melaninogenica (pigmented, anaerobic, gram-negative rods), Porphyromonas, other Prevotella spp., and Fusobacterium nucleatum as the principal pathogens; less frequently present are S. aureus, Pseudomonas aeruginosa, Proteus spp., and other gram-negative facultative bacilli. Table 72-2 summarizes the major causes of ear infections.
TABLE 72-2
Major Infectious Causes of Ear Disease
| Disease | Common Causes |
| Otitis externa | Acute: Staphylococcus aureus, Streptococcus pyogenes, Pseudomonas aeruginosa; other gram-negative bacilli |
| Chronic: P. aeruginosa; anaerobes | |
| Otitis media | Acute Streptococcus pneumoniae; Haemophilus influenzae; Moraxella catarrhalis; S. pyogenes; respiratory syncytial virus; influenza virus |
| Chronic: Anaerobes |
Sinuses
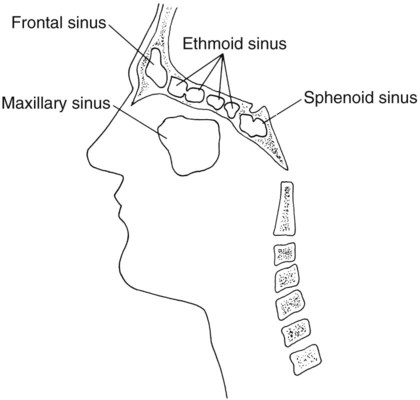
Anatomy
The sinuses, like the mastoids, are unique, air-filled cavities within the head (Figure 72-3). The sinuses are normally sterile. These structures, as well as the eustachian tube, the middle ear, and the respiratory portion of the pharynx, are lined by respiratory epithelium. The clearance of secretions and contaminants depends on normal ciliary activity and mucous flow.
Epidemiology and Etiology of Disease
Among children, S. pneumoniae, H. influenzae, and M. catarrhalis are most common. Rhinovirus is found in 15% of patients, influenza virus in 5%, parainfluenza virus in 3%, and adenovirus in less than 1%. The major causes of acute sinusitis are summarized in Table 72-3. M. catarrhalis has been isolated in chronic sinusitis in children.
TABLE 72-3
Major Infectious Causes of Acute Sinusitis
| Age Group | Common Causes |
| Young adults | Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus pyogenes, Moraxella catarrhalis |
| Children | S. pneumoniae, H. influenzae, M. catarrhalis, rhinovirus |