Infection and Disease
After reading this chapter, the student will be able to:
• Name and differentiate between the different types of symbiotic relationships, and explain how microbes of the normal flora can become opportunistic pathogens
• Identify and describe the portals by which pathogens gain excess to the body and how pathogens exit the body
• Explain the difference between contamination and infection, as well as the stages and nature of infections, and discuss virulence, virulence factors, and pathogenicity
• Define etiology; and explain Koch’s postulates including its limitations
• Name and explain the terms used to describe the different patterns of infection in a population
• Explain the different approaches used in epidemiology to study the diseases in a population
• Describe the different reservoirs of infectious agents
• Explain the different ways of disease transmission and describe the classification of infectious diseases
• Describe the nature and types of healthcare-associated (nosocomial) infections, and discuss the monitoring and information systems initiated and administered by the Centers for Disease Control and Prevention (CDC) to help in the control of these infections
• Discuss the transmission and prevention of healthcare-associated infectious diseases
Host–Microbe Relationship
Symbiosis
Symbiosis is the term that describes a close relationship between two different types of organisms in a community. Depending on the outcome of this relationship, symbiosis can be classified as mutualism, commensalism, parasitism, or amensalism (Table 9.1):
TABLE 9.1
| Symbiosis Type | Organism 1 | Organism 2 | Example |
| Mutualism | Benefits | Benefits | Escherichia coli in human large intestine |
| Commensalism | Benefits | Neither harmed, nor helped | Many microbes that make up the normal flora of the human skin and mucous membranes |
| Parasitism | Benefits | Harmed | Tuberculosis bacterium in the human lung; certain protozoans, fungi, and helminths |
| Amensalism | Not affected | Impedes or restricts | Penicillium (mold) secretes penicillin, which kills certain bacteria |
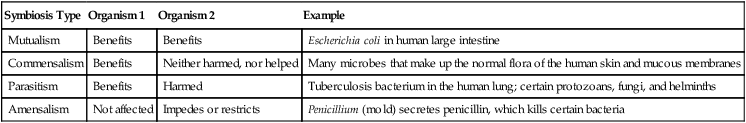
• Mutualism: Mutualism is a relationship between two organisms in which both members benefit from the interaction. For example, in the large intestine of humans, Escherichia coli releases vitamins during the breakdown of nutrients that are not digestible by the human gastrointestinal (GI) tract, but necessary for the survival of the bacteria. The vitamins released by E. coli can easily be absorbed by the intestinal epithelium of the human large intestine. As shown in the Life Application, probiotics are also examples of mutualism between specific bacterial species and the human gastrointestinal tract.
• Commensalism: Commensalism is a term used for a symbiotic relationship in which one of the organisms benefits and the other is neither harmed nor helped. Many microorganisms in the normal flora of the human skin and mucous membranes are commensals. Examples include certain saprophytic mycobacteria that inhabit the ear and external genitals, living on secretions and removed cells. These organisms do not appear to bring benefit or harm to the host.
• Parasitism: In parasitism one organism benefits, while the other is harmed, either slightly or to such an extreme that the host will be killed. A parasite that is capable of causing disease is called a pathogen. Species of bacteria, protozoans, algae, and fungi all can be microscopic human pathogens. Larger pathogens include the parasitic worms and biting arthropods.
• Amensalism: Amensalism is an interaction between two species in which one organism can hamper or prevent the growth and/or survival of another, without being positively or negatively affected by the other organism. A familiar example is Penicillium, a mold that secretes penicillin, a chemical capable of killing a wide range of bacteria (see Chapter 22, Antimicrobial Drugs).
Normal Flora (Microbiota)
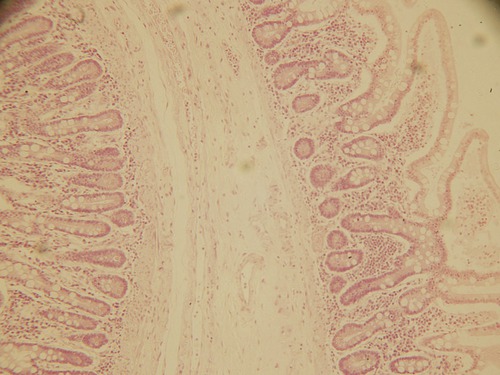
A newborn’s first contact with microorganisms occurs while traveling through the birth canal, where lactobacilli residing in the mother’s vagina will become the predominant organisms in the newborn’s intestine. The next exposure of the newborn to microorganisms occurs with the beginning of breathing, and this is soon followed by feeding. From then on, other orally acquired bacteria such as E. coli will begin to colonize the large intestine and will remain there throughout life. In other words, starting at birth the human body enters a state of dynamic equilibrium with microorganisms. In addition, throughout a person’s life, other microorganisms will establish residency in mucous membranes that are open to the external environment, on the skin and its derivatives (Figure 9.1). Mucous membranes open to the external environment include those of the respiratory tract (Figure 9.2), gastrointestinal tract (Figure 9.3), and urogenital tract (Figure 9.4). The microbes that establish themselves on the skin and mucous membranes usually do not cause disease and constitute the normal flora (microbiota) of the human body. This normal flora consists of resident or transient microbes:
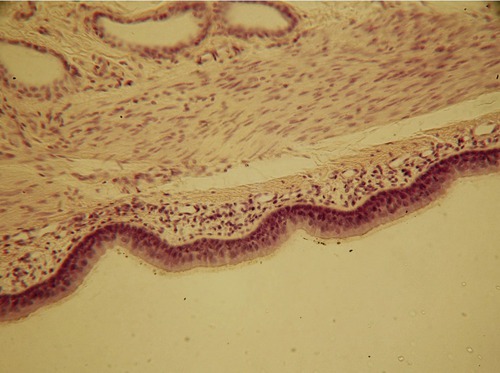
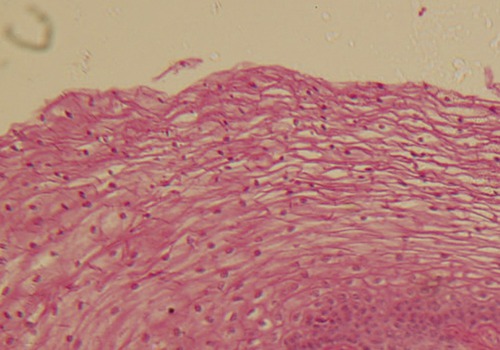
Micrograph of the skin, showing the protective layer of epidermis with the underlying connective tissue of the dermis.
• A resident flora remains part of the normal flora throughout the life of a person. An example would be Staphylococcus epidermidis, a resident of the skin, or E. coli, which is part of the intestinal flora. A detailed listing of the various organisms that reside in/on the human body is provided in Table 9.2.
TABLE 9.2
Normal Flora in Selected Regions of the Human Body
| Region | Genera | Observation |
| Skin | Staphylococcus, Propionibacterium, Corynebacterium, Micrococcus, Acinetobacter, Candida (fungus), Malassezia (fungus) | The varied environment of the skin results in locally dense or sparse populations, depending on moisture, temperature, and exposure to the environment. In general, the microbes live on the outer layer of the skin, in hair follicles, and in pores of glands |
| Eyes (conjunctiva) | Staphylococcus, Propionibacterium, Micrococcus, Corynebacterium | Although the microbiota is similar to that of the skin, tears reduce the normal flora and prevent others from colonizing |
| Upper respiratory tract | Fusobacterium, Haemophilus, Lactobacillus, Moraxella, Staphylococcus, Streptococcus | Microbes that are part of the normal flora are potential pathogens, but are generally kept at bay by an intact immune system, by nasal secretions, and by the ciliary escalator of the trachea |
| Mouth (upper digestive tract) | Fusobacterium, Haemophilus, Lactobacillus, Staphylococcus, Streptococcus, Actinomyces, Treponema, Corynebacterium, Candida (fungus) | Although saliva does contain antimicrobial substances, the moisture, warmth, and continuous supply of food support many microorganisms. Normally these microbes do not cause infections, but some of them are potential pathogens |
| Lower digestive tract | Escherichia coli, Bacteroides, Fusobacterium, Lactobacillus, Enterococcus, Enterobacter, Bifidobacterium, Citrobacter, Proteus, Klebsiella, Candida (fungus) | The large intestine contains the largest amount of resident microbes. Bacteria are mostly anaerobes but some facultative anaerobes also present |
| Female urogenital tract | Lactobacillus, Bacteroides, Clostridium, Staphylococcus, Streptococcus, Candida (fungus), Trichomonas (protozoan) | As the pH of the vagina changes so does the microbial flora. Flow of urine prevents extensive colonization of the urethra and urinary bladder |
| Male urogenital tract | Lactobacillus, Bacteroides, Fusobacterium, Mycobacterium, Peptostreptococcus, Staphylococcus, Streptococcus | Flow of urine prevents excessive colonization of microbes in the urethra or urinary bladder |
• A transient flora can be found in the same locations as the resident flora, but remains in the body for only a few hours, days, or months before it vanishes. These organisms cannot survive for reasons such as competition with other microorganisms for nutrients, elimination by the host’s immune system, or chemical and physical changes in the body of the host. An example would be Bacillus laterosporus, sometimes found in the intestines; when present the organism helps to keep fungal populations such as Candida in check.
Opportunistic Pathogens
• Compromised immune system immune suppression (see Chapter 20, The Immune System): Any factors that suppress or weaken the immune system can enable opportunistic pathogens to cause infections and disease. These factors include acute and chronic diseases, especially those involving the immune system directly (e.g., AIDS); malnutrition, stress (emotional and physical), age (very young or very old), the use of radiation and chemotherapy in the treatment of cancer, or the use of immunosuppressive drugs in transplant patients.
• Changes in the normal flora: The normal flora plays a somewhat protective role regarding pathogens, because it takes up space, uses available nutrients, and releases toxic waste products, all of which present a problem for arriving pathogens, which must compete well enough to become established to infect and cause disease in the desired host. This condition is acknowledged as microbial competition or antagonism. When the normal flora changes for any reason it may allow one of the members to become an opportunistic pathogen and thrive. Examples include vaginal yeast infections by Candida albicans in women after prolonged antibiotic therapy, or oral thrush also caused by Candida spp. in cancer patients after chemotherapy. Other conditions that change the normal flora include hormonal changes, stress, changes in the diet, or exposure to an excessive number of pathogenic organisms.
• Entrance of a member of the normal flora into areas of the body where it is not present under normal conditions: This can occur after injury, in burn victims, or even when an intestinal organism such as E. coli enters the urethra, where it then becomes opportunistic.
Stages of Infection
Portal of Entry
Portals of entry are generally the same areas that support normal flora: the skin and the mucous membranes of the gastrointestinal, respiratory, and urogenital tracts (Figure 9.5). The majority of pathogens have their preferred portal of entry, which provides the necessary habitat for further growth and eventual spreading. Most often, if a pathogen enters the wrong portal, infection will not occur. For example, influenza virus uses the respiratory mucosa as its portal of entry, where it may successfully infect its host, but when limited to contact with the skin only, influenza virus will not cause an infection. Some infectious agents can enter via more than one portal of entry, such as the skin and mucous membranes, where the infection then can lead to various diseases. For example, Streptococcus and Staphylococcus have adapted to several portals of entry such as the skin and the urogenital and respiratory tracts.
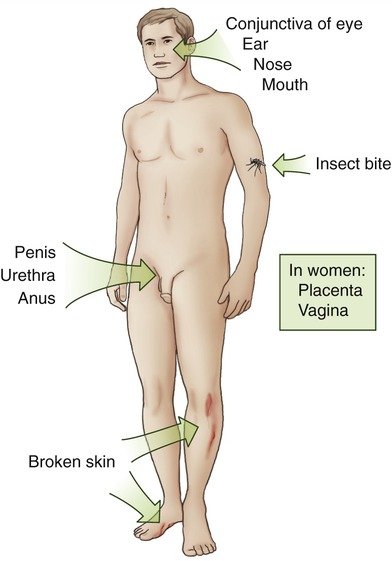
The portals of entry for microbes include the skin (broken skin, insect bites); the mucous membranes of the gastrointestinal, respiratory, and urogenital tracts; as well as the conjunctiva and the placenta.
Mucous Membranes
• The gastrointestinal (GI) tract serves as the portal of entry for pathogens present in food, liquid, and other ingested substances. Microorganisms that can survive in the GI tract are adapted to survive the action of digestive enzymes and environments that undergo drastic changes in the pH. Enteric bacterial pathogens include Salmonella, Shigella, Vibrio, and certain strains of E. coli. Viruses using the GI tract as a portal of entry include poliovirus, hepatitis A virus, echovirus, and rotavirus. The most common enteric protozoans are Entamoeba histolytica and Giardia lamblia. Helminths, although not considered microbes, are infectious agents entering through the GI tract and include trematodes, cestodes, and nematodes (see Chapter 8, Eukaryotic Microorganisms).
• The respiratory tract is the most frequently used portal of entry. Pathogens are able to enter the mouth and nose by air, via dust particles, moisture, and respiratory droplets from an infected person. Mucous membranes that line the upper respiratory tract are continuous with the membranes of the sinuses and of the auditory tubes, and pathogens can be transferred from one site to the other. Examples of bacteria using this portal of entry include the causative agents of sore throat, meningitis, diphtheria, and whooping cough. Examples of viral agents include those causing the common cold, influenza, measles, meningitis, mumps, rubella, and chickenpox (see Chapter 11, Infections of the Respiratory System).
• The urogenital tract is a portal of entry for pathogens that are generally contracted by sexual contact (see Chapter 17, Sexually Transmitted Infections/Diseases). However, girls and women who are not sexually active are also susceptible to lower urinary tract infections because of the close proximity of the anus to the female urethra. Therefore urinary tract infections caused by E. coli, as opportunistic organisms, are more common in women than men. Vaginal yeast infections are common in women who are under stress; taking birth control pills, antibiotics, and/or steroids; who are pregnant; or because of other factors. Vaginal yeast infections are usually due to an overgrowth of Candida albicans.
• The conjunctiva is generally a good barrier against infectious agents, but some bacteria such as Haemophilus aegyptius (pinkeye), Chlamydia trachomatis, and Neisseria gonorrhoeae can easily attach to this membrane.
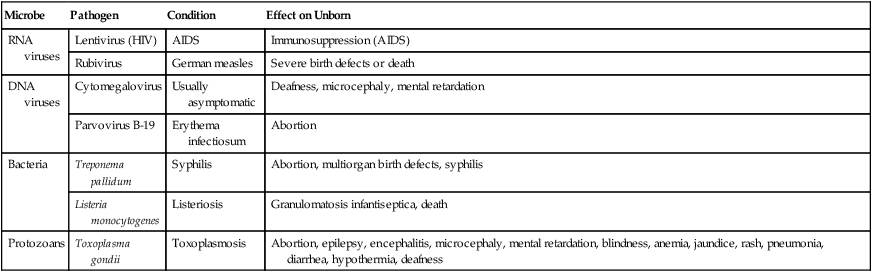
Placenta
HEALTHCARE APPLICATION
Pathogens That Cross the Placenta
| Microbe | Pathogen | Condition | Effect on Unborn |
| RNA viruses | Lentivirus (HIV) | AIDS | Immunosuppression (AIDS) |
| Rubivirus | German measles | Severe birth defects or death | |
| DNA viruses | Cytomegalovirus | Usually asymptomatic | Deafness, microcephaly, mental retardation |
| Parvovirus B-19 | Erythema infectiosum | Abortion | |
| Bacteria | Treponema pallidum | Syphilis | Abortion, multiorgan birth defects, syphilis |
| Listeria monocytogenes | Listeriosis | Granulomatosis infantiseptica, death | |
| Protozoans | Toxoplasma gondii | Toxoplasmosis | Abortion, epilepsy, encephalitis, microcephaly, mental retardation, blindness, anemia, jaundice, rash, pneumonia, diarrhea, hypothermia, deafness |
Virulence and Pathogenicity
Virulence refers to the degree of pathogenicity or disease-evoking power of a specific microbe. Virulence therefore is the degree of pathogenicity of a microbe and is based on virulence factors. A pathogen is a microorganism that is capable of causing disease. The ability of a microorganism to cause disease is directly related to the number of infecting organisms, the portal of entry, the host defense mechanisms (see Chapter 20, The Immune System), and the intrinsic characteristics of the bacteria and their virulence factors. These include the following:
• Adhesion: Adhesion is the first and probably the most crucial step in infection, because without adhesion to the host cells or tissue, the microbes will be removed by ciliary motion (see Chapter 3, Cell Structure and Function), sneezing, coughing, swallowing, urine flow, flow of tears, or intestinal peristalsis. Bacteria must first bind to the host cell, via pili, fimbriae, or specific membrane receptor sites. Viral adhesion occurs by capsid or envelope proteins. The mechanism of the adhesion process can be nonspecific or specific:
• Nonspecific adhesion involves nonspecific attractive forces or interactions the microorganism uses to move toward the eukaryotic host. These interactions and forces can include the following:
• Atomic and molecular vibrations
• Recruitment and trapping by biofilms (see Chapter 6, Bacteria and Archaea)
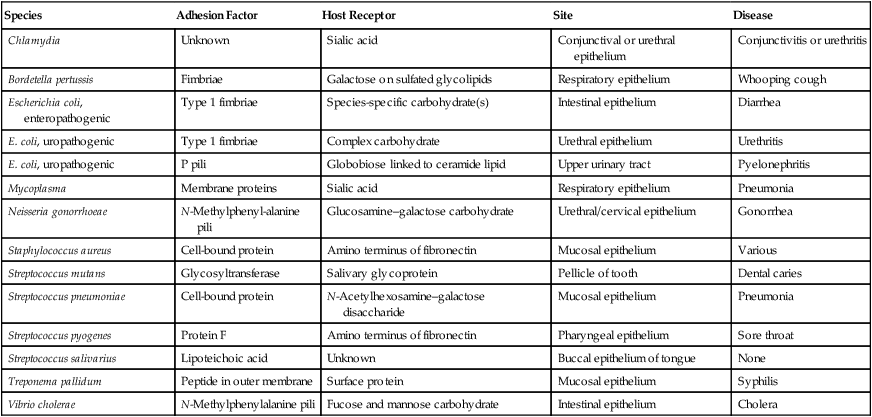
• Specific adhesion involves a permanent lock-and-key interaction between complementary molecules on each cell surface and under normal physiological conditions this attachment becomes irreversible. Examples of such specific attachments/adhesions are illustrated in Table 9.3.
TABLE 9.3
Examples of Specific Adhesions of Bacteria to the Host
| Species | Adhesion Factor | Host Receptor | Site | Disease |
| Chlamydia | Unknown | Sialic acid | Conjunctival or urethral epithelium | Conjunctivitis or urethritis |
| Bordetella pertussis | Fimbriae | Galactose on sulfated glycolipids | Respiratory epithelium | Whooping cough |
| Escherichia coli, enteropathogenic | Type 1 fimbriae | Species-specific carbohydrate(s) | Intestinal epithelium | Diarrhea |
| E. coli, uropathogenic | Type 1 fimbriae | Complex carbohydrate | Urethral epithelium | Urethritis |
| E. coli, uropathogenic | P pili | Globobiose linked to ceramide lipid | Upper urinary tract | Pyelonephritis |
| Mycoplasma | Membrane proteins | Sialic acid | Respiratory epithelium | Pneumonia |
| Neisseria gonorrhoeae | N-Methylphenyl-alanine pili | Glucosamine–galactose carbohydrate | Urethral/cervical epithelium | Gonorrhea |
| Staphylococcus aureus | Cell-bound protein | Amino terminus of fibronectin | Mucosal epithelium | Various |
| Streptococcus mutans | Glycosyltransferase | Salivary glycoprotein | Pellicle of tooth | Dental caries |
| Streptococcus pneumoniae | Cell-bound protein | N-Acetylhexosamine–galactose disaccharide | Mucosal epithelium | Pneumonia |
| Streptococcus pyogenes | Protein F | Amino terminus of fibronectin | Pharyngeal epithelium | Sore throat |
| Streptococcus salivarius | Lipoteichoic acid | Unknown | Buccal epithelium of tongue | None |
| Treponema pallidum | Peptide in outer membrane | Surface protein | Mucosal epithelium | Syphilis |
| Vibrio cholerae | N-Methylphenylalanine pili | Fucose and mannose carbohydrate | Intestinal epithelium | Cholera |
• Colonization: Another essential step in the development of an infection is the establishment of the pathogen at the portal of entry once adhesion of the pathogen has occurred. Human pathogens usually colonize tissues that are in contact with the external environment, such as the urogenital tract, the digestive tract, the respiratory tract, and the conjunctiva of the eye. Some virulent bacteria may produce special proteins that allow them to colonize these parts to cause disease.
• Invasion: The invasive qualities of a pathogen may be aided by the production of extracellular substances, allowing it to disrupt host cell membranes, breaking down the primary and secondary defensive barriers of the host. These substances are referred to as invasins (Table 9.4) and their activity then facilitates the growth and spread of the pathogen.
TABLE 9.4
| Invasin | Organism(s) Producing Invasin | Mechanism |
| Hyaluronidase | Streptococci, staphylococci, clostridia | Assaults the matrix of connective tissue by depolymerizing hyaluronic acid |
| Collagenase | Clostridium histolyticum, Clostridium perfringens | Breaks down collagen |
| Neuraminidase | Vibrio cholerae, Shigella dysenteriae | Degrades neuraminic acid of the intestinal mucosa |
| Kinases | Streptococci and staphylococci | Converts plasminogen to plasmin, which digests fibrin |
| Leukocidin | Staphylococcus aureus | Disrupts neutrophil membranes and causes discharge of lysosomal granules |
| Streptolysin | Streptococcus pyogenes | Repels phagocytes and disrupts phagocyte membrane, causing discharge of lysosomal granules |
| Hemolysins | Streptococci, staphylococci, clostridia | Phospholipases or lecithinases that destroy erythrocytes and other cells by lysis |
| Phospholipases | Clostridium perfringens | Destroys phospholipids of the plasma membrane |
| Lecithinases | Clostridium perfringens | Destroys lecithin in cell membranes |
| Anthrax EF | Bacillus anthracis | An adenylate cyclase that causes increased levels of intracellular cAMP |
| Pertussis AC | Bordetella pertussis | An adenylate cyclase that causes increased levels of intracellular cAMP and subsequent increase in respiratory secretions |
• Evasion of host defenses: The ability to avoid the host response can be due to the presence of a capsule, the production of proteins that bind to the host cell antibodies, or mutation of the organism to alter its antigenicity. Various strategies are used by microbes to avoid being eliminated by the host phagocytes, but usually they involve blocking one or more steps of phagocytosis (see Chapter 20, The Immune System). Some of these strategies include but are not limited to the following:
• Avoidance of contact with phagocytes by invading or remaining in regions that are inaccessible to phagocytes or are not patrolled by them. Some pathogens induce minimal or no inflammation to avoid provoking an intense immune response. Other organisms inhibit phagocyte chemotaxis; for example, Clostridium produces a toxin that inhibits neutrophil chemotaxis. In addition, some bacteria hide their antigenic surface so that phagocytes do not recognize the organism as non-self.
• Inhibition of phagocytic engulfment is used by some bacteria that have substances on their surfaces that inhibit phagocytic activity or engulfment.
• Survival inside phagocytes, either neutrophils or macrophages, is another way by which some microbes can resist killing. These organisms are considered intracellular parasites.
• Yet another, aggressive strategy used by some organisms is to produce products that kill or damage phagocytes either before ingestion or after ingestion.
• Toxins: Another virulence factor is determined by the ability of the organism to produce enzymes, exotoxins, and endotoxins that will damage the host cells or interfere with a vital host cell function. Toxins constitute a major virulence factor.
Toxins
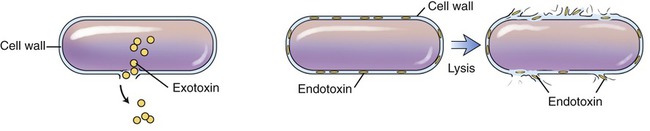
Chemically, bacterial toxins are either lipopolysaccharides associated with the cell wall of gram-negative bacteria, or proteins released from the bacterial cell. Toxins associated with the cell wall are called endotoxins, and proteins released from a bacterium are referred to as exotoxins (Figure 9.6). Bacterial toxins are among the most powerful toxins known to humankind.
Exotoxins
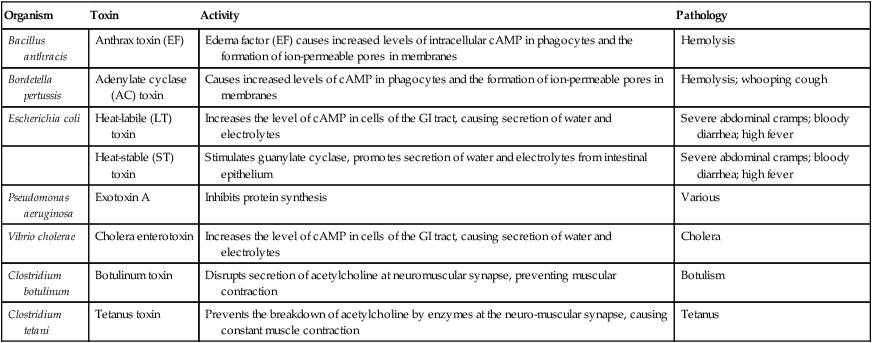
Exotoxins are typically soluble proteins secreted by bacterial cells during their exponential growth phase. They can act at sites other than the location of the infection and bacterial growth. Often the toxins produced are species specific and associated with a particular disease (Table 9.5). For example, Clostridium tetani is the only organism to produce the tetanus toxin, and Corynebacterium diphtheriae makes diphtheria toxin. As with other proteins, these enzymes can be denatured by heat, acid, and proteolytic enzymes (enzymes that break down proteins).
TABLE 9.5
Examples of Bacterial Exotoxins
| Organism | Toxin | Activity | Pathology |
| Bacillus anthracis | Anthrax toxin (EF) | Edema factor (EF) causes increased levels of intracellular cAMP in phagocytes and the formation of ion-permeable pores in membranes | Hemolysis |
| Bordetella pertussis | Adenylate cyclase (AC) toxin | Causes increased levels of cAMP in phagocytes and the formation of ion-permeable pores in membranes | Hemolysis; whooping cough |
| Escherichia coli | Heat-labile (LT) toxin | Increases the level of cAMP in cells of the GI tract, causing secretion of water and electrolytes | Severe abdominal cramps; bloody diarrhea; high fever |
| Heat-stable (ST) toxin | Stimulates guanylate cyclase, promotes secretion of water and electrolytes from intestinal epithelium | Severe abdominal cramps; bloody diarrhea; high fever | |
| Pseudomonas aeruginosa | Exotoxin A | Inhibits protein synthesis | Various |
| Vibrio cholerae | Cholera enterotoxin | Increases the level of cAMP in cells of the GI tract, causing secretion of water and electrolytes | Cholera |
| Clostridium botulinum | Botulinum toxin | Disrupts secretion of acetylcholine at neuromuscular synapse, preventing muscular contraction | Botulism |
| Clostridium tetani | Tetanus toxin | Prevents the breakdown of acetylcholine by enzymes at the neuro-muscular synapse, causing constant muscle contraction | Tetanus |
Endotoxins
Endotoxins are lipopolysaccharides and structural components of gram-negative bacterial cell walls (e.g., Shiga toxin). Endotoxins are released from the cell walls during lysis initiated by an effective host defense or by the action of antibiotics. After release, these toxins can also act on sites remote from the original site of infection and growth. In contrast to exotoxins, endotoxins are less potent and less specific in their actions. Because these toxins are lipopolysaccharides and not proteins, they are heat stable and even boiling for 30 minutes does not destabilize them. However, certain oxidizing agents such as superoxide, peroxide, and hypochlorite have been reported to be effective in neutralizing them. A general comparison between bacterial exotoxins and endotoxins is presented in Table 9.6.
TABLE 9.6
Comparison of Bacterial Exotoxins and Endotoxins
| Feature | Exotoxin | Endotoxin |
| Chemical nature | Protein | Lipopolysaccharides |
| Location | Extracellular | Part of cell wall |
| Specificity | High degree | Low degree |
| Potency | Relatively high | Relatively low |
| Denatured by heat | Yes | No |
| Antigenic | Yes | Yes |
| Toxoid* | Yes | No |
*A toxoid is an endotoxin modified so that it is no longer toxic, but still causes the host to generate antitoxin.
Etiology of Infectious Diseases
Patterns of Infection
• Local infections are the simplest ones; the organism enters the body and remains confined to a specific tissue. This is the case with boils, fungal skin infections, and warts.
• Focal infections occur when the pathogen spreads from a local infection to other tissues.
• Systemic infections occur when an infection spreads to several sites and tissue fluids, usually by way of the circulatory system.
• Septicemia is a systemic infection caused by the multiplication of pathogens in the blood. This condition is a common example of sepsis, a toxic inflammatory condition arising from the spread of microbes.
• Bacteremia represents the presence of bacteria in the blood.
• Toxemia refers to the presence of toxins in the blood.
• Viremia is the term used to describe viruses in the blood.
• Mixed infections occur when several infectious agents concurrently establish themselves at the same site. Some mixed infections are synergistic infections in which microbes cooperate in breaking down the tissue.
• Acute infections are infections that appear rapidly, with pronounced (severe) symptoms, but then rapidly vanish.
• Chronic infections have usually less severe symptoms than acute infections, but they persist for long periods of time.
• A primary infection is an initial infection, which is followed by complications due to another microbe.
• A secondary infection follows a primary infection. In general, secondary infections are caused by a different microbe, which gains access to the body through a lesion of either the skin or the mucous membrane damaged by the first pathogen, or they can be microbes of the normal flora that become opportunistic because of a compromised immune system.
• A subclinical infection is one that does not cause any apparent symptoms, and can be carried over long periods of time without causing symptoms of illness in the individual.
Koch’s Postulates
The germ theory of disease was proposed by Louis Pasteur and Robert Koch (see Chapter 1, Scope of Microbiology). Although Louis Pasteur was convinced that microbes caused disease in humans he was not able to link a specific microbe with a particular disease. After many years of experimentation, Koch was able to establish that specific microorganisms cause specific diseases. Koch developed a series of conditions—postulates—that must be met to identify a particular microbe as pathogenic and the cause of a particular disease. Using his postulates he proved that Bacillus anthracis is the causative agent for anthrax and that Mycobacterium tuberculosis causes tuberculosis. This concept is now known as Koch’s postulates (Figure 9.7), and can be summarized as follows:
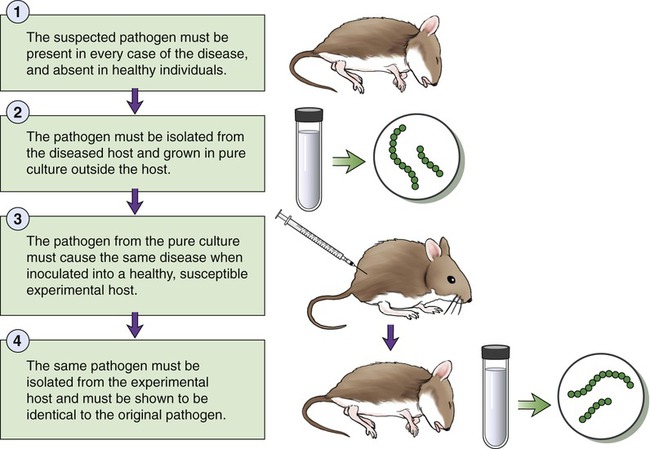
• The suspected pathogen must be present in every case of the disease, and absent in healthy individuals.
• The pathogen must be isolated from the diseased host and grown in pure culture outside the host.
• The pathogen from the pure culture must cause the same disease when inoculated into a healthy, susceptible experimental host.
• The same pathogen must be isolated from the experimental host and must be shown to be identical to the original pathogen.
Exceptions to Koch’s Postulates
• Some pathogens cannot be cultured in the laboratory.
• Many infectious diseases can be caused by several different pathogens.
• A particular pathogen can cause different diseases, depending on the portal of entry.
• Some diseases are caused by a combination of pathogens, such as liver infections caused by both the hepatitis B virus and the hepatitis D virusoid. The latter cannot cause infection without the hepatitis B virus. Other exceptions are polymicrobial diseases caused by biofilms.
• Some pathogens are exclusively human pathogens and ethical considerations prevent human inoculation to prove Koch’s postulates. These exceptions include diseases caused by viruses or animal parasites. Also, Rickettsia and Chlamydia are obligate intracellular parasites without an animal model.
Epidemiology and Public Health
• Descriptive epidemiology is the collecting and tabulating of data concerning the disease. These data generally include information about the affected individuals and the location and period of time of disease occurrence. Information about patients may include age, gender, occupation, health history, sexual behavior, eating habits, travel history, and socioeconomic status. Seasonal variations in the climate may also be a consideration. The time course and chain of transmission are important in descriptive epidemiology and investigators make every effort to identify the index case, the first case, of the disease. This might be difficult because the victim of the disease may have recovered, moved, or died.
• Analytical epidemiology attempts to demonstrate a probable cause-and-effect relationship, using analysis of the data collected by descriptive epidemiology. Analytical studies may be retrospective if the data are analyzed after an epidemic has subsided, or prospective if the data collection is done during an ongoing epidemic. Analytical epidemiology is often applied when it is unethical to apply Koch’s postulates, because the disease is a human disease only and does not have an animal model.
• Experimental epidemiology starts with a hypothesis about a particular disease, followed by the design of experiments and studies to test the hypothesis. The application of Koch’s postulates is a perfect example of experimental epidemiology.
Epidemiology is a subject of major importance to state and federal public health departments. The Centers for Disease Control and Prevention (CDC) is the central source of epidemiological information in the United States. The CDC publishes the Morbidity and Mortality Weekly Report (MMWR), which can be viewed at the CDC website (www.cdc.gov). This publication contains data on morbidity (the incidence of specific notifiable diseases), and mortality (the number of deaths associated with a particular disease). The morbidity rate reflects the number of people affected by a particular disease during a given time in relation to the total population. The mortality rate shows the number of deaths resulting from a disease in a population during a given period of time in relation to the total population. The Morbidity and Mortality Weekly Report is of interest to microbiologists, physicians, and other healthcare and public health professionals. Nationally notifiable infectious diseases are diseases that must be reported by physicians to the U.S. Public Health Service and are shown in Box 9.1. A well-developed network of individuals and agencies keeps track of infectious diseases at the local, district, state, national, and international levels. The CDC shares its information and statistics with the World Health Organization (WHO) for the purpose of worldwide tabulation and control.
Diseases in the Population
• Endemic disease is a disease that is repeatedly present in a given population or geographical area. An example of an endemic disease is the common cold.
• Sporadic disease is a disease that breaks out only occasionally, such as typhoid fever in the United States.
• Epidemic disease is a disease that occurs with greater frequency than usual in a population of a given area. Influenza is an example of a disease that can occasionally reach epidemic proportions.
• Pandemic disease is a worldwide epidemic such as AIDS and the influenza of 1918.
Reservoirs
Animal Reservoirs
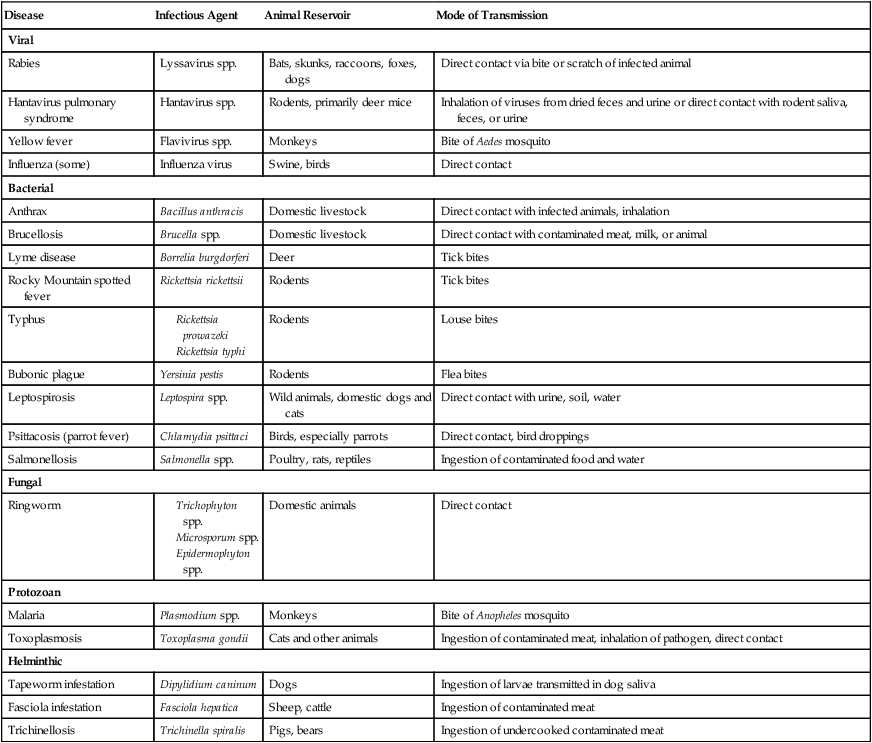
Many of the pathogens that normally infect animals, either domesticated or wild, also can affect humans. Diseases that occur primarily in animals and can be transmitted to humans are referred to as zoonoses (Table 9.7). Humans can be infected by zoonoses by several routes: direct contact with the infected animal; contact with animal waste, or with waste-contaminated food or water; contact with dust from contaminated hides, fur, or feathers; consumption of infected animal products; or through the medium of insect vectors. Humans often are the definitive (final) host for zoonotic pathogens and usually are not a significant reservoir for reinfection of animal hosts. However, zoonotic diseases transmitted by blood-sucking arthropods are likely to be transmitted back to the species of the animal host.
TABLE 9.7
| Disease | Infectious Agent | Animal Reservoir | Mode of Transmission |
| Viral | |||
| Rabies | Lyssavirus spp. | Bats, skunks, raccoons, foxes, dogs | Direct contact via bite or scratch of infected animal |
| Hantavirus pulmonary syndrome | Hantavirus spp. | Rodents, primarily deer mice | Inhalation of viruses from dried feces and urine or direct contact with rodent saliva, feces, or urine |
| Yellow fever | Flavivirus spp. | Monkeys | Bite of Aedes mosquito |
| Influenza (some) | Influenza virus | Swine, birds | Direct contact |
| Bacterial | |||
| Anthrax | Bacillus anthracis | Domestic livestock | Direct contact with infected animals, inhalation |
| Brucellosis | Brucella spp. | Domestic livestock | Direct contact with contaminated meat, milk, or animal |
| Lyme disease | Borrelia burgdorferi | Deer | Tick bites |
| Rocky Mountain spotted fever | Rickettsia rickettsii | Rodents | Tick bites |
| Typhus | |||
Modes of Transmission
Contact Transmission
• Direct contact transmission involves direct physical contact of the infectious agent between hosts, such as by person-to-person contact; no intermediate object is involved. Common forms of direct contact transmission are touching, kissing, and sexual intercourse. Examples of pathogens transmitted this way include agents causing respiratory tract infections, staphylococcal infections, measles, scarlet fever, and sexually transmitted diseases. Zoonoses can also be transmitted from an animal reservoir to a human by direct contact through touching, biting, or scratching. Furthermore, direct transmission is possible within a single individual with poor personal hygiene when putting fingers in the mouth that are contaminated with fecal material.
• Indirect contact transmission occurs when the pathogen is transmitted from the reservoir to the susceptible host by a fomite—a nonliving object. Fomites can be tissues, handkerchiefs, towels, bedding, toys, clothes, diapers, money, eating utensils, drinking cups/glasses, medical equipment and devices, contaminated needles, and any other items that can harbor or transmit pathogens. Contaminated needles are a common fomite for the transmission of HIV and hepatitis B and C.
• Droplet transmission occurs when infectious agents are transmitted through respiratory droplets that travel a distance less than 1 meter. These droplets are released into the environment by normal exhaling, laughing, coughing, or sneezing. Sneezing is the most effective form of droplet transmission. Examples include the transmission of the common cold, influenza, pneumonia, and pertussis.
Vehicle Transmission
Any transmission of pathogens that require some sort of medium is considered a vehicle transmission. Modes of transmission in this category include airborne, waterborne, and foodborne transmissions, as well as transmission through bodily fluids and intravenous fluids. Foodborne, waterborne, and airborne diseases are also shown in the Healthcare Applications tables of Chapter 1 (Scope of Microbiology).
• Airborne transmission refers to the spread of pathogens by droplet nuclei (droplets of mucus), other aerosols, and dust that travel more than 1 meter from the reservoir to the host. Aerosols may originate from coughing or sneezing and from air conditioning and other cooling systems. Pathogens can attach themselves to dust particles and be transmitted by air via sweeping, mopping, changing of bed linens, changing of clothes, or simple dusting.
• Waterborne transmission generally occurs through untreated or poorly treated sewage. Many gastrointestinal diseases including giardiasis, amebic dysentery, and cholera are transmitted by water. Waterborne shigellosis and leptospirosis can also be transmitted via this route. Fecal–oral infections are the major source of diseases in the world as pathogens such as Schistosoma worms and enteroviruses are shed in feces, get into the water supply, subsequently enter the gastrointestinal mucosa or skin, and then cause disease elsewhere in the body.
• Foodborne transmission generally involves pathogens in or on foods that are incompletely cooked, poorly processed under unsanitary conditions, not refrigerated, or poorly refrigerated. This type of contamination can be by normal microbial flora, with zoonotic pathogens, and with parasitic worms that alternate between human and animal hosts. Viruses such as the hepatitis A virus can also be transmitted this way.
• Bodily fluid transmission needs to be considered, especially in healthcare workers, who must take precautions when handling these fluids, which can potentially be contaminated with pathogens. Blood, urine, saliva, and other bodily fluids can be reservoirs for different pathogens. Examples of diseases that can be transmitted via this route include AIDS, hepatitis, and herpes.
Vector Transmission
Vectors are animals, usually arthropods, that carry pathogens from one host to another. Vectors can transmit the pathogens either biologically or mechanically (Box 9.2).
• Biological vectors transmit pathogens, but also serve as host for a part of the pathogen’s life cycle. Biological vectors important to human diseases are biting insects, including mosquitoes, ticks, lice, fleas, blood-sucking flies or bugs, and mites.
• Mechanical vectors, on the other hand, do not have to be a host for the pathogen, but passively carry the agents to a new host by their feet or other body parts, such as happens with flies.
Healthcare-associated (Nosocomial) Infections
Nosocomial infections are infections acquired in the course of treatment in a hospital or hospital-like setting, but secondary to the patient’s original conditions. Infections obtained by patients or healthcare providers while they are treated or working in a healthcare setting such as a hospital, clinic, nursing home, dental office, and other healthcare facility are referred to as healthcare-associated infections (HAIs). HAIs are among the top 10 leading causes of death in the United States. In the latest update (2009) by the CDC, it is estimated that in American hospitals alone HAIs account for an estimated 1.7 million infections and 99,000 associated deaths each year (Box 9.3).
Types of Nosocomial Infections
• Exogenous HAIs are caused by pathogens in the healthcare environment, shed from sick people.
• Endogenous infections are caused by microbes in the normal flora of a patient, which become pathogenic because of a variety of factors associated with the healthcare setting. These factors include the state of the patient’s immune system, immovability (bedridden), diet, and many others. Another factor is the use of antimicrobial drugs that may inhibit some of the normal flora, allowing the overgrowth of others, causing superinfections in the absence of the usual competition. Superinfections, however, are not limited to healthcare settings.
• Iatrogenic infections are a set of infections that may result from the use of medical procedures such as the use of catheters, invasive diagnostic procedures, and surgery.
Nosocomial infections can be caused by a variety of organisms (Table 9.8), some of which cause specific infections and disease; others have the capacity to cause a variety of infections, depending on their portal of entry. Bacteria that gain entrance to the bloodstream have the chance to settle at a site different from the site of entry if not treated promptly. Septicemia is less common, but can occur when surgery is performed on an infected area or an area where bacteria normally grow (i.e., intestine).
TABLE 9.8
Infectious Diseases That May Be Acquired in Healthcare Facilities
| Pathogen | Disease |
| Acinetobacter | Variety, ranging from pneumonia to serious blood or wound infections |
| Blood-borne pathogens | |
| Hepatitis B | Hepatitis |
| Hepatitis C | Hepatitis |
| HIV/AIDS | HIV/AIDS |
| Burkholderia cepacia | Respiratory infections, pneumonia, especially in patients with cystic fibrosis |
| Clostridium difficile | Diarrhea, colitis |
| Clostridium sordellii | Pneumonia, endocarditis, arthritis, peritonitis, myonecrosis, toxic shock syndrome (gynecologic infections) |
| Creutzfeldt-Jakob prion | Creutzfeldt-Jakob disease |
| Ebola | Viral hemorrhagic fever |
| Enteric bacteria | Gastrointestinal infections |
| Hepatitis A | Hepatitis |
| Influenza viruses | Influenza |
| Methicillin-resistant Staphylococcus aureus (MRSA) | Potentially life-threatening infections such as pneumonia, surgical site infection, bloodstream infections |
| Mumps virus | Mumps |
| Norovirus | Gastroenteritis |
| Parvovirus | Erythema infectiosum (fifth disease) |
| Poliovirus | Poliomyelitis (rare) |
| Rubella virus | Rubella |
| Coronavirus | SARS |
| Pseudomonas aeruginosa | Infections in burn patients |
| Streptococcus pneumoniae (drug resistant) | Meningitis, bacteremia, pneumonia, otitis media |
| Mycobacterium tuberculosis | Tuberculosis |
| Varicella | Chicken pox |
| Vancomycin-intermediate Staphylococcus aureus (VISA) | Potentially life-threatening infections such as pneumonia, surgical site infection, bloodstream infections |
| Vancomycin-resistant enterococci (VRE) | Various infections |
Antimicrobial Resistance in Healthcare Settings
Drug-resistant pathogens are becoming an increasing threat to the population (see Chapter 18, Emerging Infectious Diseases), particularly in healthcare settings. Of all patients with nosocomial infections in the United States, 99,000 annually die as a result of their infection. More than 70% of the bacteria causing these infections are resistant to at least one of the drugs commonly used to treat them. Persons infected with drug-resistant organisms generally have longer hospital stays and require second- or third-choice drugs that may be less effective and more toxic.
Control and Prevention
Each healthcare facility has a safety program, policies, and procedures (see Chapter 5, Safety Issues) that will include procedures and precautions designed to reduce the incidence of HAIs. These procedures are aimed at preventing the transmission of pathogens to patients and healthcare personnel. In general, these measures include disinfection, medical asepsis (good housekeeping, hand washing, bathing, sanitary food handling, proper hygiene, measures to prevent the spread of pathogens between patients), surgical asepsis, and isolation of contagious and particularly susceptible patients.
Summary
• Under normal circumstances the newborn is initially exposed to microbes during birth, followed by many more exposures. This is the start of the development of a relationship between humans and microbes. The relationship between two different types of organisms is referred to as symbiosis, and, depending on the outcome of the relationship, symbiosis is classified as mutualism, commensalism, parasitism, or amensalism.
• Microorganisms that establish residency on the skin and in the mucous membranes that open to the external environment, and do not cause disease, represent the normal flora.
• Whenever the balance between the normal flora and the human host is interrupted, the microorganisms of the normal flora can cause infection and disease—they become opportunistic pathogens.
• Contamination is the presence of microbes in or on the body; it can result in infection and disease, and the microorganisms can enter the host via several possible portals of entry.
• After gaining entry into the host, the pathogen must undergo adhesion and several other steps to be able to cause an infection, but not all infections cause disease.
• Infections have varied patterns, and when an infectious agent causes pathological changes and interferes with the normal functioning of the body it is termed infectious disease; the study of the cause of the disease is called etiology.
• Robert Koch established a series of conditions—postulates—that must be met to identify a particular microbe as pathogenic and the cause of a particular disease. Although these postulates provide the basics of the etiology of an infectious disease, they are not always applicable.
• Epidemiology is the study of the distribution and causes of diseases in a population, and is the foundation for necessary interventions in the interest of public health. It is a subject of major importance for state and federal public health departments. Diseases in a population are reported as the prevalence of the disease, measured by incidence, which is the number of new cases over a certain period of time compared with the healthy population.
• For an infectious disease to continue to exist, its causative agent must have a permanent place to reside, a reservoir of infection. Infectious agents can be transmitted to a host by contact, vehicle, or vector transmission.
• Healthcare-associated (nosocomial) infections (HAIs) are infections acquired as a result of treatment or working in healthcare facilities. Healthcare facilities serve sick people, capable of shedding pathogens. Transmission of pathogens and the development of resistant strains in this setting are becoming an increasing problem to public health.
Review Questions
1. Which type of symbiosis benefits both members?
2. The mold that produces penicillin is an example of:
3. The presence of microbes in or on the body is a(n):
4. All of the following areas of the human body contain normal flora except the:
6. When a pathogen spreads from the original site to other tissues or organs it is called a(n) ___________ infection.
7. A disease that is generally present in a given population is:
8. Which of the following is not considered to be a vehicle transmission?
9. Which of the following is likely to be the most frequently used portal of entry?
10. Infections that may result from the use of catheters are classified as:
11. The symbiotic relationship in which one of the organisms benefits and the other is not harmed or helped is referred to as __________.
12. A flora found in the same location as the resident flora, but which remains only for a given amount of time, is called a(n) __________ flora.
13. A microorganism capable of causing disease is called a(n) __________.
14. A vector that transmits pathogens and also serves as host for a part of the pathogen’s life cycle is a(n) __________ vector.
15. A worldwide epidemic is considered a(n) __________ disease.
16. Describe how microbes of a normal flora in the human body can become opportunistic pathogens.
17. Describe the three basic approaches used by epidemiologists to study the dynamics of a disease in a population.
18. Discuss Koch’s postulates and its limitations.
19. Describe the necessary steps a microbe must take before it can cause infection and disease.
20. Discuss healthcare-associated (nosocomial) infections (HAIs).