Immediate Allergic Reactions
Learning Objectives
• Summarize the immunologic abnormalities associated with atopy
• List preformed mediators released during the early phase of an allergic response
• Compare and contrast the roles of preformed mediators in skin and lung allergic reactions
• Identify the late-phase mediators and their physiologic roles in allergic reactions
• Identify the two common complications of allergic rhinitis
• Design a treatment regimen for allergic rhinitis
• Design a treatment regimen for urticaria
• Explain the wheal-and-flare reaction in a skin test
• Compare and contrast urticaria and atopic dermatitis
• Identify the chemical characteristics of food allergens
• List foods that contain high histamine levels
• Explain the relationship between pollens, fruits, and oral allergy syndrome
• Identify the three physiologic and immunologic components in asthma
• Identify the drugs used to control acute and chronic asthma
• List the three types of asthma that are not immunologically mediated
• Compare and contrast anaphylaxis and anaphylactoid reactions
• Identify antibiotics and therapeutic agents that cause anaphylactoid reactions
• Relate the theory behind the use of hyposensitization therapy
• Identify the major allergens in latex
• List the populations at risk for latex sensitization
Key Terms
Allergic rhinitis
Anaphylaxis
Anaphylactoid
Aspirin-induced asthma
Asthma
Atopic dermatitis
Atopy
Early-phase IgE response
Hyposensitization therapy
Infectious asthma
Late-phase IgE response
Leukotrienes
Prostaglandins
Radioallergosorbent test (RAST)
Skin test
Urticaria
Introduction
Immediate allergic reactions are mediated by the immunoglobulin E (IgE) class of antibodies, and reactions typically occur 15 to 20 minutes after exposure to an allergen. The prevalence of allergies in the United States is estimated to be between 9% and 16% of the population, or 50 million people. Over the last three decades, the incidence and severity of allergic reactions have increased substantially, and allergic diseases are now among the top three causes of illness and disability.
Allergic reactions occur in the skin (urticaria and atopic dermatitis), nose and eyes (rhinitis and conjunctivitis), lungs (asthma), and the intestine (food allergies). Clinical signs and symptoms are related to the time course, the target organ, and the nature of the pharmacologic mediators released from mast cells and basophils.
Atopy
There is often a familial genetic tendency to develop rhinitis, urticaria, and asthma. This condition, called atopy, is characterized by elevated IgE levels directed at common aero-allergens or food allergens. Atopic individuals have increased numbers of CD4Th2 (T helper) cells and elevated interleukin 4 (IL-4) in peripheral blood. These abnormalities skew the immune response to IgE production. In addition, mast cells and basophils from atopic individuals have double the number of Fc receptors for IgE compared with nonatopic individuals. Atopic individuals also have hyperreactive airways that respond to low levels of cholinergic agonists that bind and activate acetylcholine receptors in the lung.
Although atopy is associated with genes on seven different chromosomes, single nucleotide polymorphisms in genes on chromosomes 5, 7, and 11 play a critical role in the frequency and evolution of allergic reactions (Table 15-1). These mutations increase cytokine production, expression of Fc receptors, IgE synthesis, and bronchial hyperreactivity.
Table 15-1
Examples of Chromosomal Locations and Genes Associated with Atopy and Asthma
| Chromosomal Location | Candidate Genes | Putative Role of Gene Products in Disease |
| 5q | Cytokine gene cluster (IL-4, IL-5, IL-13), CD14, β2-adrenergic receptor | Interleukin 4 (IL-4) and IL-13 promote immunoglobulin E (IgE) switching; IL-5 promotes eosinophil growth and activation; CD14 is a component of the lipopolysaccharide (LPS) receptor, which, via interaction with Toll receptor 4 (TLR4), may influence the balance between TH1 and TH2 responses to antigens; β2-adrenergic receptor regulates bronchial smooth muscle contraction |
| 6p | Class II major histocompatibility complex (MHC) | Some alleles may regulate T cell responses to allergens |
| 11a | FcεRI β-chain | Mediates mast cell activation |
| 12q | Stem cell factor, interferon-gamma (IFN-γ), STAT6 | Stem cell factor regulates mast cell growth and differentiation; IFN-γ opposes actions of IL-4; STAT6 mediates IL-4 signal transduction |
| 16 | IL-4 receptor α-chain | Subunit of both IL-4 and IL-13 receptors |
| 20p | ADAM33 | Metalloproteinase involved in airway remodeling |
| 2q | DPP10 | Peptidase that may regulate chemokine and cytokine activity |
| 13q | PHF11 | Transcriptional regulator involved in B cell clonal expansion and immunoglobulin expression |
Chromosome 5q genes regulate the production of cytokines (e.g., IL-4, IL-5, and IL-13). IL-4 and IL-13 drive isotypic switching to IgE production, and IL-5 promotes the growth and activation of eosinophils. IL-13 also increases bronchial mucus secretion. Tandem repeats in chromosome 11q13 are associated with polymorphisms in the FcεRI–beta chain and the number of Fc receptors expressed by mast cells and basophils. The FcεRI receptor acts as a trigger for immediate allergic reactions by stabilizing the receptor and amplifying intracellular signals. Bronchial hyperreactivity is controlled by the genes on chromosome 7.
Evolution of an Immediate Allergic Reaction
Initial Exposure to an Allergen
During initial exposure, allergens are processed by macrophages and allergenic epitopes presented to CD4Th2 cells in the context of class II molecules. In allergic or atopic individuals, T cells secrete IL-4, IL-5, and IL-13, which promote the rapid isotypic switching and IgE production by plasma cells. Secreted IgE binds specifically to Fc receptors on tissue mast cells and circulating basophils.
Second Exposure to an Allergen
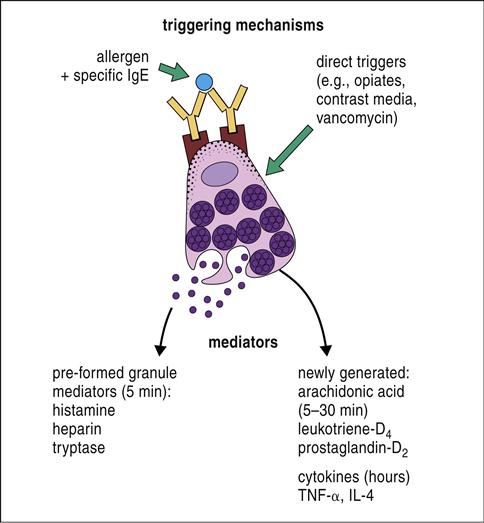
Upon second exposure, the allergen cross-links two cell-bound IgEs, which initiates an energy-dependent mechanism that culminates in a biphasic immune response. The early-phase response, which occurs within 20 minutes of exposure, involves IgE–antigen interactions and is mediated by preformed pharmacologic mediators. A late-phase response, which occurs 4 to 8 hours following exposure, does not involve antibodies and is facilitated by the newly synthesized products of the arachidonic acid pathway.
Early-Phase Reactions and Preformed Mediators
In the early-phase reaction, granules containing preformed pharmacologic mediators are extruded from mast cells and basophils. The major preformed mediators include histamine, heparin, eosinophil chemotactic factor (ECF), and neutrophil chemotactic factor (NCF). Histamine is a vasoactive amine that has tissue-dependent, physiologic effects. In the skin, histamine interacts with receptors (H1 receptor) on vascular endothelial cells to create gaps between adjacent cells and increase vascular permeability (H2 receptor). Fluid from blood escapes through the gaps, causing swelling or edema in the tissue. Histamine also irritates peripheral nerve endings, causing itching and pain (pruritus). Heparin, which is also released from mast cells and basophils, potentiates the tissue edema by binding to antithrombin and preventing the activation of the normal coagulation pathway.
In the lung, histamine reacts with H1 receptors on smooth muscle in the bronchioles. Muscular contraction of the airways reduces the airway diameter, impeding the flow of air. The chemotactic factors ECF and NCF act on circulating cells and cause an influx of eosinophils and granulocytes at the site of the allergic reaction. Although the role of eosinophils in allergic reactions has not been fully delineated, enzymes released from eosinophils are known to inactivate histamine.
Late-Phase Reactions and Synthesized Mediators
Mast cells and basophils synthesize and release late-phase mediators over the course of 4 to 8 hours. These mediators include prostaglandins, leukotrienes, and platelet activating factor (PAF) (Figure 15-1).
Prostaglandins and leukotrienes are the products of the arachidonic acid pathway. Two prostaglandins (PGD2 and PGE2) play critical roles in late-phase reactions by increasing vascular permeability, contracting smooth muscle, and acting as an NCF. Leukotrienes are 20 carbon unsaturated fatty acids (LTA4, LTB4, LTC4, LTD4, and LTE4) that cause bronchoconstriction, increased mucus production, and sustained inflammation. PAF released from polymorphonuclear cells, endothelial cells, and monocytes causes bronchoconstriction, retraction of endothelial cells, and vasodilation. Late-phase reactions occur in some, but not all, individuals.
Types of Immunoglobulin E–Mediated Allergic Reactions
Asthma
Asthma is a disease characterized by partial airway obstruction that is partially reversible either spontaneously or with treatment. The hallmark of allergic asthma is an early-phase allergic response. Approximately half of the patients with asthma also have late-phase responses. Chronic airway inflammation, airway injury, and airway repair (airway remodeling) also contribute to the pathogenesis of asthma and permanent abnormalities in lung function.
Chronic asthma has an inflammatory component. Cells involved in the inflammatory response include T cells, eosinophils, and mast cells. Cytokines released from activated macrophages mediate the inflammatory process. Tumor necrosis factor alpha (TNF-α) upregulates endothelial cell adhesion factors that bind neutrophils, monocytes, and eosinophils. The accumulation of cells forms the asthma inflammatory nidus.
If the airway inflammation is not resolved, reactive oxygen species produced by inflammatory cells injure the airways, and the tissue must be repaired and restructured. The interaction between lymphocyte CD28 and dendritic cell B7 activates dendritic cells and promotes the synthesis of proinflammatory cytokines. In tissue, L-arginine is converted to L-ornithine, which initiates cell proliferation, collagen synthesis, smooth muscle hypertrophy, and goblet cell hyperplasia. These changes culminate in the thickening of the sub-basement membrane, subepithelial fibrosis, and permanent damage to the bronchioles.
Treatment of Asthma
The clinician uses different medications to control the immediate reactions, the late-phase reaction, and chronic airway inflammation. Slow-acting β2-agonists and oral corticosteroids are used to relieve the acute exacerbations of asthma. Therapeutics used to control long-term and chronic pulmonary symptoms are mast cells stabilizers, leukotriene antagonists, long-acting β2-agonists, inhaled corticosteroids, and methylxanthines.
A new therapy uses a humanized monoclonal antibody, known as omalizumab, which is directed at IgE. It binds to soluble IgE and prevents binding to Fc receptors on mast cells and basophils. Omalizumab is usually prescribed to patients with moderate to severe asthma triggered by ubiquitous year-round allergens.
Allergic Rhinitis
Allergic rhinitis (AR) is the result of early-phase and late-phase IgE-mediated reactions and subsequent inflammation of the nasal passages, mucus membranes, nose, eyes, sinuses, and eustachian tubes. Early-phase mediators cause nasal edema, mucus secretion, itching, sneezing, and rhinorrhea. In the late phase, lymphocytes, basophils, and eosinophils accumulate in the area of an allergic reaction. Mediators released from the cellular infiltrate potentiate the inflammatory response.
AR is often complicated by sinusitis, which is infection or inflammation in any four sinus cavities in the skull. Inflammation causes the sinus lining to thicken, which impedes the flow of air or fluid. The chronic inflammation also results in the formation of nasal polyps. Usually, polyps are found in the ethmoidal sinuses located on either side of the nose between the eyes and the bridge of the nose. When the sinuses swell or the polyps impede the flow of air and fluid, bacteria begin to multiply and infect the cells lining the sinus. Acute sinusitis is usually caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Infections with Staphylococcus aureus and anaerobic bacteria are common in individuals with chronic sinusitis.
Treatment of Allergic Rhinitis
Individuals with acute or intermittent AR are treated with second-generation oral antihistamines, decongestants, nasal steroids, and leukotriene antagonists such as montelukast sodium. Intranasal antihistamines, sodium cromolyn, and anticholinergic agents are also effective in treating AR. Chronic rhinitis is treated with a short course of nasal steroids.
Allergic Conjunctivitis
Atopic patients often develop conjunctivitis, called allergic conjunctivitis, which is characterized by redness, itching, and excessive tearing of the eyes. Conjunctivitis follows the same seasonal patterns of AR. Vernal conjunctivitis is a more serious, persistent form of conjunctivitis. It is characterized by redness and itching of the eyes, mucus production, and photophobia. In some cases, hypertrophy and edema of the upper eyelid form papillae. This form of conjunctivitis is called giant papillary conjunctivitis.
Treatment of Conjunctivitis
Various therapies are used to reduce the physiologic effects at different stages of AR. Artificial tear preparations are used to dilute the allergens and inflammatory mediators. Systemic or topical antihistamines reduce some symptoms.
Urticaria
Urticaria is a rash characterized by raised, flat-topped areas with associated red edematous welts (Figure 15-2).
Urticaria may be acute (6 or less weeks in duration) or chronic (6 or more weeks in duration). Acute urticaria is usually caused by food allergens such as eggs, nuts, shellfish, chocolate, tomatoes, berries, and milk. In rare instances, acute urticaria has been associated with the use of aspirin, angiotensin-converting enzyme (ACE) inhibitors, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Urticaria is subdivided into types I and II on the basis of the nature of the immune response. Type I urticaria is a true IgE allergic reaction with both early and late phases. Type II urticaria is an aberrant reaction mediated by cytotoxic T cells, antibodies, complement activation, and the deposition of fibrin.
Treatment of Urticaria
Second-generation oral antihistamines, which have a minimal sedating effect, are commonly used for the treatment of IgE-mediated urticaria. Topical therapy with doxepin or capsaicin provides relief from refractory urticaria. Glucocorticosteroids are also indicated for the treatment of refractory urticaria, but their efficacy is controversial.
Atopic Dermatitis
Atopic dermatitis is a chronic, eczematous skin disease that is characterized by itching, swelling, cracking, and weeping skin lesions (Figure 15-3). Atopic dermatitis should not be confused with contact dermatitis. The former is an IgE-mediated allergic reaction, and the latter is a T cell–mediated delayed hypersensitivity reaction.
Of the two prevalent theories concerning the pathogenesis of atopic dermatitis, one postulates that allergen-stimulated Langerhans cells produce large amounts of IL-4, which causes rapid isotypic switching and the production of the IgE isotype. The second theory postulates that a topical S. aureus infection is the cause of atopic dermatitis. Staphylococcal superantigens stimulate Langerhans cells to produce high concentrations of IL-4 and isotypic switching.
Treatment of Atopic Dermatitis
Low- to medium-potency topical steroids are usually prescribed for the treatment of atopic dermatitis. However, calcineurin inhibitors are replacing corticosteroids because they have fewer adverse effects and can be used on all skin surfaces, including the skin on the face and neck.
Oral Allergy Syndrome
Over 25% of pollen-sensitive individuals develop burning or pruritus of the lips and tongue and edema of the buccal mucosa after ingestion of certain raw fruits and vegetables. The syndrome is an IgE-mediated early-phase reaction caused by exposure to antigens shared between pollens and fruits or vegetables. A list of pollens and their cross-reactive antigens is provided in Table 15-2.
Table 15-2
Pollens and Their Cross-Reactive Antigens
| Pollen | Cross-Reacting Antigens |
| Alder | Almond, apple, celery, chery, hazelnut, peach, pear, parsley, strawberry, raspberry |
| Birch | Apple, carrot, cherry, pear, peach, plum, fennel, walnut, potato, wheat |
| Grass | Melon, tomato, watermelon, orange, wheat |
| Ragweed | Banana, cantaloupe, cucumber, honeydew, watermelon, zucchini, echinacea, artichoke, dandelion, hibiscus or chamomile tea |
| Pine | Pine nuts |
Food Allergies
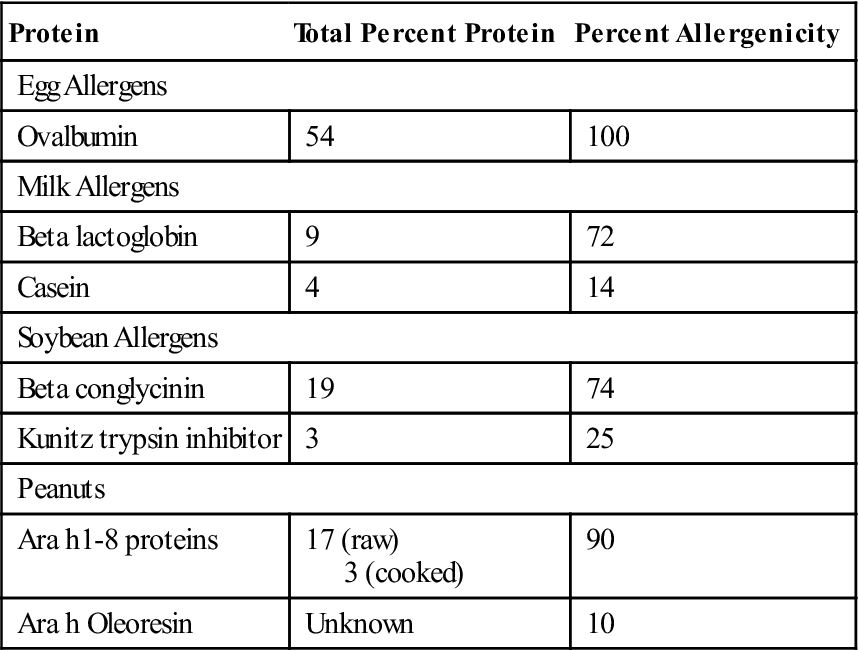
Food allergens usually are large, water-soluble glycoproteins that are resistant to heating at 212°F and gastric proteolysis at pH 2 to pH 3. These large molecules are absorbed from the intestine and stimulate the synthesis of allergen-specific IgE. Major food allergens are peanuts, soybeans, tree nuts, milk, eggs, crustaceans, fish, and wheat (Table 15-3).
Table 15-3
Allergens in Common Food Products
< ?comst?>
| Protein | Total Percent Protein | Percent Allergenicity |
| Egg Allergens | ||
| Ovalbumin | 54 | 100 |
| Milk Allergens | ||
| Beta lactoglobin | 9 | 72 |
| Casein | 4 | 14 |
| Soybean Allergens | ||
| Beta conglycinin | 19 | 74 |
| Kunitz trypsin inhibitor | 3 | 25 |
| Peanuts | ||
| Ara h1-8 proteins | 17 (raw) 3 (cooked) |
90 |
| Ara h Oleoresin | Unknown | 10 |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Modified from Metcalfe DD, Astwood JD, Townsend R, et al: Assessment of the allergenic potential of foods derived from genetically engineered crop plants, Crit Rev Food Sci Nutr, 36:S177, 1996.
These allergens induce an early-phase response mediated by heparin and histamine, which cause vomiting, diarrhea, malabsorption, blood loss, and protein loss through the intestine. Acute urticaria, angioedema, and atopic dermatitis are also common in individuals with food allergies.
Treatment of Food Allergies
Elimination of the allergenic food from the diet is the only treatment for food allergies and other adverse food reactions.
Anaphylaxis
Anaphylaxis is the most severe and often fatal allergic reaction, which involves total cardiovascular and respiratory collapse. This IgE-mediated reaction results in the massive release of histamine, LTC4, and PGD2. Increased vascular permeability causes a massive shift of fluids from blood into tissue within 10 minutes of exposure. The combination of vasodilation and increased vascular permeability causes hypovolemic shock and death within 15 to 60 minutes. Penicillin, bee stings, and peanuts are the most common causes of anaphylaxis.
Prevention of Anaphylaxis
Highly sensitized individuals at risk of anaphylaxis carry a self-injectable epinephrine delivery device. Epinephrine is a catecholamine that binds to α-adrenergic and β-adrenergic receptors to relax smooth muscles, decrease vascular permeability, and reduce vasodilation.
Identification of Agents Causing Allergic Reactions
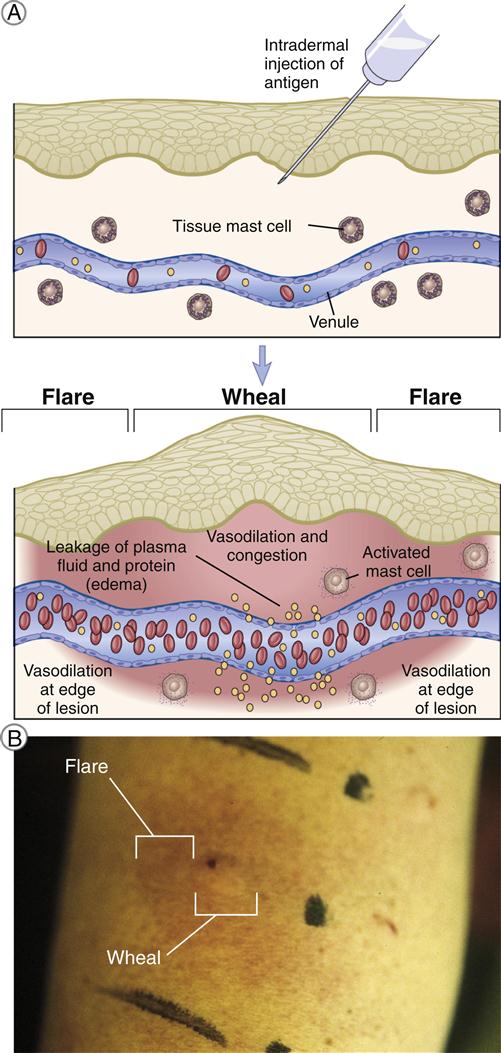
If an allergic reaction is suspected, the clinician assesses the clinical symptoms and obtains skin test data to determine the source of the allergic reaction. Prick and intradermal tests are used in the diagnosis of allergies. When the prick test is used, the allergen is placed on the skin, and the skin is gently scratched or pricked. In the intradermal test, small amounts of allergen are injected subcutaneously under the skin.
If the patient is sensitive to a specific allergen, a wheal-and-flare reaction occurs at the skin test site within 15 to 20 minutes (Figure 15-4). Plasma leaking from the vessel into the skin induces edema, or swelling in the skin (wheal). Blood vessels at the periphery of the wheal then dilate, and red blood cells accumulate in the area, causing redness (flare) in the skin.
Some individuals who are at a high risk for anaphylaxis cannot have a skin test. In these cases, an in vitro radioallergosorbent test (RAST) is used to determine the presence of allergen-specific IgE. The classic RAST is actually an indirect ELISA, in which the secondary antibody is labeled with a radioisotope such as iodine-125. Because of the issues related to the handling and disposal of radioisotopes, secondary antibodies are now labeled with enzymes or fluorochromes.
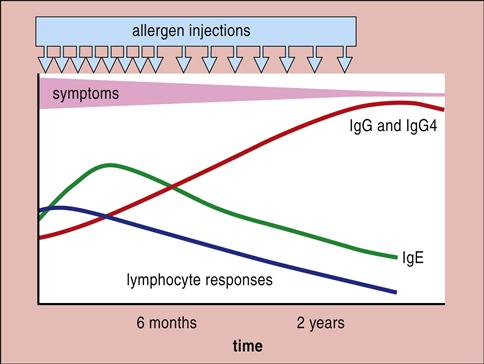
Hyposensitization Therapy
Clinicians often implement hyposensitization therapy when allergic reactions cannot be effectively controlled with pharmacologic agents. During therapy, patients are given small amounts of allergens orally or subcutaneously. Over a period of months, the amount of allergen is increased to a maximum tolerated dose, which is called the maintenance dose. Hyposensitization therapy induces the synthesis of IgG antibodies, which are called blocking antibodies (Figure 15-5).
The IgG binds the allergen, thus preventing interaction with mast cell–bound IgE. Evidence has shown that hyposensitization therapy also increases the number of T regulatory cells that inhibit the production of allergen-specific IgE. Hyposensitization results in the reduction, but not elimination, of clinical symptoms in 60% to 90% of patients.
Pseudoallergic Reactions not Mediated by Immunoglobulin E
Symptoms similar to allergic asthma, food allergies, and anaphylaxis can be elicited by nonimmunologic reactions. Respiratory infections, exercise, and aspirin ingestion can cause asthma in some patients. High histamine levels in foods can cause symptoms consistent with a food allergy. Finally, some chemicals can induce anaphylactoid reactions that are similar to life-threatening anaphylaxis.
Nonallergic Asthma
Infectious Asthma
Nonallergic asthma can be caused by influenza, respiratory syncytial virus (RSV), or parainfluenza viruses. The replication of viruses often destroys the epithelial layers of the respiratory tract and exposes the sensory nerve endings. Stimulation of nerve endings by cold air or irritants causes a reflex bronchoconstriction. Asthma symptoms abate when the respiratory epithelium regenerates.
Rhinovirus and enterovirus (common cold viruses) can disrupt the control mechanisms for smooth muscle contraction by inhibiting the synthesis of the M2 muscarinic receptors. M2 receptors act in a negative feedback loop that controls the release of acetylcholine. The lack of M2 receptors allows the release of acetylcholine and increases the contraction of smooth muscle, causing symptoms that mimic asthma.
Exercise-Induced Asthma
In individuals with underlying bronchial hyperreactivity, exercise triggers an acute bronchospasm and symptoms similar to those of asthma. At rest, most individuals breathe through the nose, which serves to humidify and control the temperature in the lungs. After vigorous exercising, individuals tend to become mouth breathers. Mouth breathing evaporates water from the bronchioles, which alters airway humidity and temperature. When combined with existing airway edema, these changes induce a reflex bronchoconstriction.
Aspirin-Induced Asthma
Aspirin-induced asthma attacks occur within 1 hour of aspirin ingestion and are often accompanied by rhinorrhea and conjunctival irritation. Sensitive individual have defects in the metabolism of aspirin and the control of leukotriene production. Aspirin-sensitive individuals are poor aspirin metabolizers, and large concentrations of parental acetylsalicylic acid accumulate in the blood. In lung tissue, acetylsalicylic acid stimulates mast cells to produce leukotrienes. Aspirin-sensitive patients have a single nucleotide polymorphism in the LTC4 synthetase gene that causes the overproduction of LTC4. The C4 leukotriene is converted to LTD4 that causes airway narrowing, mucus secretion, and increased vascular permeability.
Nonallergic Food Reactions
Histamine in Foods
In sensitive individuals, severe gastrointestinal reactions occur following the ingestion of foods containing high concentrations of histamine. Eggplant, spinach, cheese, sauerkraut, vinegar, strawberry, and red wine (Chianti) contain high levels of histamine. In certain circumstances, histamine is present in tuna and mackerel. If these fish are improperly refrigerated, Klebsiella species decarboxylate tissue histidine to histamine, which causes a clinical syndrome called scromboid fish poisoning. Symptoms include diarrhea, facial flushing, dizziness, and vomiting.
Anaphylactoid Reactions
Anaphylactoid reactions are not mediated by IgE, but the symptoms mimic severe anaphylaxis. Most anaphylactoid agents activate the complement cascade or react directly with mast cells or basophils. Opiates, vancomycin, polymyxins, and ciprofloxacin are associated with anaphylactoid reactions resulting from complement activation. Activation of the complement cascade produces C3a, C4a, and C5a anaphylatoxins, which release mediators from mast cells and basophils.
Hyperosmolar radiocontrast media used in angiography reacts directly with mast cells and basophils to release pharmacologically active mediators. In addition to rashes, urticaria, angioneurotic edema, and smooth muscle spasms, some individuals develop hypotension, pulmonary edema, and cardiac arrest. Mortality from radiocontrast media–related anaphylactoid reactions is 1 to 5 per 100,000.
New and Novel Allergens
Latex Allergens
Latex is a milky fluid produced by rubber trees (Hevea brasiliensis) in Southeast Asia and Malaysia. The major component of latex is C1-4 polyisoprene, which is not allergenic. However, latex preparations are often contaminated with allergenic plant defense proteins called hevein and hevein amine. These allergens are carried through the manufacturing process and are present in the finished products. Latex has multiple commercial uses and is commonly found in a number of products (Box 15-1).
Persons sensitized to latex allergens develop IgE-mediated urticaria and rhinitis. Inhalation of latex allergens also causes asthma. Populations at risk for latex allergy are hospital workers and patients with spina bifida or congenital urogenital disease. An estimated 25% of the hospital workers are sensitized to latex. Because of the extensive use of urinary and intrathecal catheters, 28% to 68% of patients with spina bifida are sensitized to latex.
The diagnosis of latex allergy is confounded by the fact that many other chemicals are added to latex to accelerate curing (thiuram, mercaptobenzothiazoles, and carbamates) and vulcanization (sulfur). These compounds elicit an irritant dermatitis caused by disruption of the skin or a delayed hypersensitivity response resembling poison ivy. Clinicians must perform in vivo and in vitro testing to differentiate among allergic, irritant, or delayed hypersensitivity reactions.
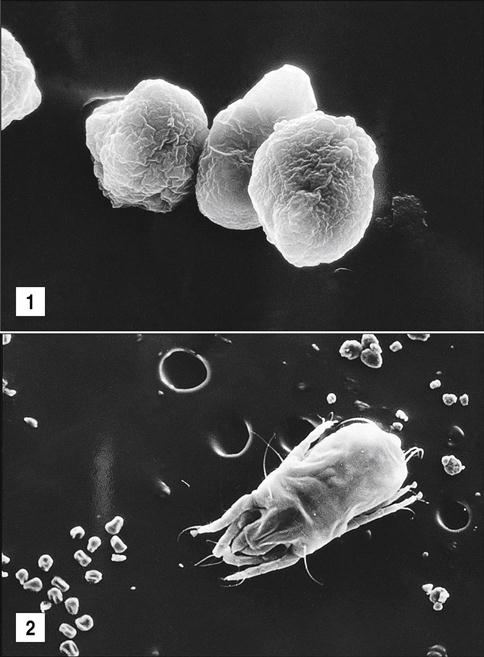
Mite Allergens
Mites are microscopic insects that inhabit bedding, upholstered furniture, draperies, and carpets. The two species of house dust mites are (1) Dermatophagoides pteronyssinus, which is found in Europe, and (2) Dermatophagoides farinae, which is the most commonly encountered species in the United States (Figure 15-6).
The major allergens are proteins found in fecal balls. A half teaspoon of house dust contains about 250,000 fecal pellets, which are of the same size as respirable pollens. The most significant allergens (Der p1 and Der p2) are cysteine proteases. In the lung, these proteases degrade the tight junctions in the vascular epithelium and allow the entry of allergens into the blood and the stimulation of an immune response. Der p1 also cleaves the low-affinity IgE receptor (CD23) on B cells, which normally acts as a control mechanism for IgE synthesis. Uncontrolled IgE synthesis and the release of proinflammatory cytokines and pharmacologically active mediators from basophils and mast cells cause contraction of smooth muscle and asthmatic symptoms.
Cockroach-Related Allergens
Between 23% and 60% of those living in crowded inner-city areas are sensitized to cockroaches. Allergens come from the saliva, fecal matter, secretions, cast skins, and dead bodies of cockroaches. The major cockroach-related allergens are Bla g1, 2, 4, and 5. However, Bla g1 is the major allergen that elicits IgE synthesis in 60% to 80% of sensitized individuals. The structure of Bla g1 is similar to that of an aspartic proteinase, but it has no enzymatic activity. The combination of sensitivity to cockroaches and repeated exposures to airborne allergens causes the increase in asthma reported in many inner-city areas.
Drugs and Immediate Allergic Reactions
With the exception of penicillins (see Chapter 3) and beta lactam antibiotics, pharmaceuticals are not usually involved in IgE-mediated immediate allergic reactions. Rather, drugs may evoke delayed hypersensitivity reactions. The major lesion in drug hypersensitivity is a morbilliform rash. By definition, a morbilliform rash consists of macules and papules of differing sizes that begin on the trunk and spread to the extremities. Rashes can occur during or after drug therapy.
Immunoglobulin E and Parasitic Infections
In certain regions of the world with endemic parasitic helminthic infections, most individuals have increased CD4Th2 lymphocytes and high levels of parasite-specific IgE in serum. In the intestine, the release of preformed mediators causes violent peristaltic contractions that expel the intestinal worms. In addition, IL-4, IL-5, and IL-13 cause the release of cytotoxic proteins from eosinophils.
Summary