Humidification and filtration
Heat and moisture exchanger (HME) humidifiers
These are compact, inexpensive, passive and effective humidifiers for most clinical situations (Figs 9.1 and 9.2). The British Standard describes them as ‘devices intended to retain a portion of the patient’s expired moisture and heat, and return it to the respiratory tract during inspiration’.
Components
1. Two ports, designed to accept 15- and 22-mm size tubings and connections. Some designs have provision for connection of a sampling tube for gas and vapour concentration monitoring.
2. The head which contains a medium with hygrophobic properties in the form of a mesh with a large surface area (Fig. 9.3). It can be made of ceramic fibre, corrugated aluminium or paper, cellulose, metalized polyurethane foam or stainless-steel fibres.
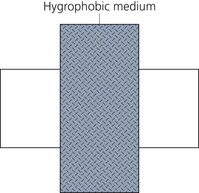
Fig. 9.3 Heat and moisture exchanger.
Mechanism of action
1. Warm humidified exhaled gases pass through the humidifier, causing water vapour to condense on the cooler HME medium. The condensed water is evaporated and returned to the patient with the next inspiration of dry and cold gases, humidifying them. There is no addition of water over and above that previously exhaled.
2. The greater the temperature difference between each side of the HME, the greater the potential for heat and moisture to be transferred during exhalation and inspiration.
3. The HME humidifier requires about 5–20 min before it reaches its optimal ability to humidify dry gases.
4. Some designs with a pore size of about 0.2 µm can filter out bacteria, viruses and particles from the gas flow in either direction, as discussed later. They are called heat and moisture exchanging filters (HMEF).
5. Their volumes range from 7.8 mL (paediatric practice) to 100 mL. This increases the apparatus dead space.
6. The performance of the HME is affected by:
a) water vapour content and temperature of the inspired and exhaled gases
b) inspiratory and expiratory flow rates affecting the time the gas is in contact with the HME medium hence the heat and moisture exchange
c) the volume and efficiency of the HME medium – the larger the medium, the greater the performance. Low thermal conductivity, i.e. poor heat conduction, helps to maintain a greater temperature difference across the HME increasing the potential performance.
Problems in practice and safety features
1. The estimated increase in resistance to flow due to these humidifiers ranges from 0.1 to 2.0 cm H2O depending on the flow rate and the device used. Obstruction of the HME with mucus or because of the expansion of saturated heat exchanging material may occur and can result in dangerous increases in resistance.
2. It is recommended that they are used for a maximum of 24 h and for single patient use only. There is a risk of increased airway resistance because of the accumulation of water in the filter housing if used for longer periods.
3. The humidifying efficiency decreases when large tidal volumes are used.
4. For the HME to function adequately, a two-way gas flow is required.
5. For optimal function, HME must be placed in the breathing system close to the patient.
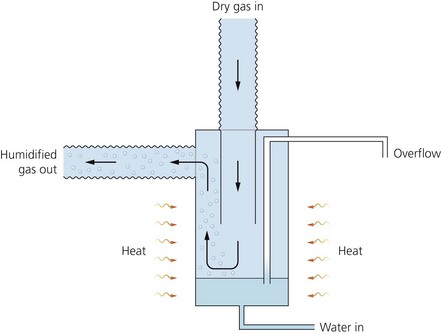
Hot water bath humidifier
This humidifier is used to deliver relative humidities higher than the heat moisture exchange humidifier. It is usually used in intensive care units (Fig. 9.4).
Components
1. A disposable reservoir of water with an inlet and outlet for inspired gases. Heated sterile water partly fills the container.
2. A thermostatically controlled heating element with temperature sensors, both in the reservoir and in the breathing system close to the patient.
3. Tubing is used to deliver the humidified and warm gases to the patient. It should be as short as possible. A water trap is positioned between the patient and the humidifier along the tubing. The trap is positioned lower than the level of the patient.
Mechanism of action
1. Powered by electricity, the water is heated to between 45°C and 60°C (Fig. 9.5).
2. Dry cold gas enters the container where some passes close to the water surface, gaining maximum saturation. Some gas passes far from the water surface, gaining minimal saturation and heat.
3. The container has a large surface area for vaporization. This is to ensure that the gas is fully saturated at the temperature of the water bath. The amount of gas effectively bypassing the water surface should be minimal.
4. The tubing has poor thermal insulation properties causing a decrease in the temperature of inspired gases. This is partly compensated for by the release of the heat of condensation.
5. By raising the temperature in the humidifier above body temperature, it is possible to deliver gases at 37°C and fully saturated. The temperature of gases at the patient’s end is measured by a thermistor. Via a feedback mechanism, the thermistor controls the temperature of water in the container.
6. The temperature of gases at the patient’s end depends on the surface area available for vaporization, the flow rate and the amount of cooling and condensation taking place in the inspiratory tubing.
7. Some designs have heated elements placed in the inspiratory and expiratory limb of the breathing system to maintain the temperature and prevent rain out (condensation) within the tube.
Problems in practice and safety features
1. The humidifier, which is electrically powered, should be safe to use with no risk of scalding, overhydration and electric shock. A second backup thermostat cuts in should there be malfunction of the first thermostat.
2. The humidifier and water trap(s) should be positioned below the level of the tracheal tube to prevent flooding of the airway by condensed water.
3. Colonization of the water by bacteria can be prevented by increasing the temperature to 60°C. This poses greater risk of scalding.
4. The humidifier is large, expensive and can be awkward to use.
5. There are more connections in a ventilator set up and so the risk of disconnections or leaks increases.
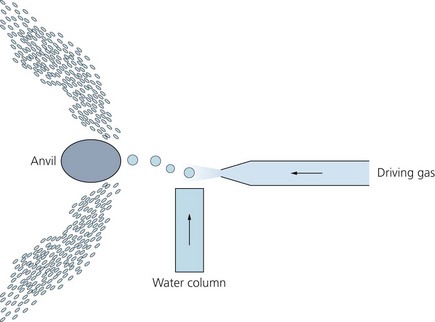
Nebulizers (Fig. 9.6)
There are three types: gas driven, spinning disc and ultrasonic.
Gas-driven (jet) nebulizer
Mechanism of action
1. A high-pressure gas flows through the Venturi, creating a negative pressure.
2. Water is drawn up through the capillary tube and broken into a fine spray. Even smaller droplets can be achieved as the spray hits an anvil or a baffle.
3. The majority of the droplets are in the range of 2–4 µm. These droplets tend to deposit on the pharynx and upper airway with a small amount reaching the bronchial level. This nebulizer is also capable of producing larger droplets of up to 20 µm in size. Droplets with diameters of 5 µm or more fall back into the container leaving droplets of 4 µm or less to float out with the fresh gas flow.
4. The device is compact, making it easy to place close to the patient.
Bacterial and viral filters
These minimize the risk of cross-transmission of bacteria and/or viruses between patients using the same anaesthetic breathing systems. The British Standard defines them as ‘devices intended to reduce transmission of particulates, including micro-organisms, in breathing systems’. It is thought that the incidence of bleeding after orotracheal intubation is 86%. The filter should be positioned as close to the patient as possible, e.g. on the disposable catheter mount, to protect the rest of the breathing system, ventilator and anaesthetic machine. It is recommended that a new filter should be used for each patient. A humidification element can be added producing a heat and moisture exchanging filter (HMEF) (see Fig. 9.1).
Components
1. Two ports designed to accept 15- and 22-mm size tubings and connections.
2. A sampling port to measure the gases’/agents’ concentrations positioned on the anaesthetic breathing system side.
3. The filtration element can either be a felt-like electrostatic material or a pleated hydrophobic material.
Mechanism of action
There are five main mechanisms by which filtration can be achieved on a fibre:
1. Direct interception: large particles (=1 µm), such as dust and large bacteria, are physically prevented from passing through the pores of the filter because of their large size.
2. Inertial impaction: smaller particles (0.5–1 µm) collide with the filter medium because of their inertia. They tend to continue in straight lines, carried along by their own momentum rather than following the path of least resistance taken by the gas. The particles are held by Van der Waal’s electrostatic forces.
3. Diffusional interception: very small particles (<0.5 µm), such as viruses, are captured because they undergo considerable Brownian motion (i.e. random movement) because of their very small mass. This movement increases their apparent diameter so that they are more likely to be captured by the filter element.
4. Electrostatic attraction: this can be very important but it is difficult to measure as it requires knowing the charge on the particles and on the fibres. Increasing the charge on either the particles or the fibres increases the filtration efficiency. Charged particles are attracted to oppositely charged fibres by coulombic attraction.
5. Gravitational settling: this affects large particles (>5 µm). The rate of settling depends on the balance between the effect of gravity on the particle and the buoyancy of the particle. In filters used in anaesthesia, it has minimal effect as most of the settling occurs before the particles reach the filter.
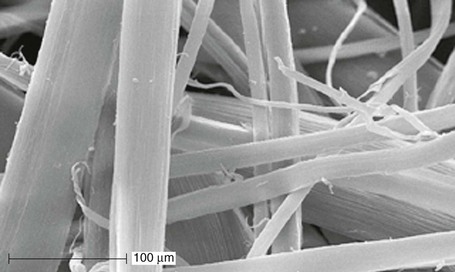
Electrostatic filters (Fig. 9.8)
1. The element used is subjected to an electric field producing a felt-like material with high polarity. One type of fibre becomes positively charged and the other type negatively charged. Usually two polymer fibres (modacrylic and polyprolyne) are used.
2. A flat layer of filter material can be used as the resistance to gas flow is lower per unit area.
3. These filters rely on the electrical charge to attract oppositely charged particles from the gas flow. They have a filtration efficiency of 99.99%.
4. The electrical charge increases the efficiency of the filter when the element is dry but can deteriorate rapidly when it is wet. The resistance to flow increases when the element is wet.
5. The electrical charge on the filter fibres decays with time so it has a limited life.
6. A hygroscopic layer can be added to the filter in order to provide humidification. In such an HMEF, the pressure drop across the element and thus the resistance to breathing will also increase with gradual absorption of water.
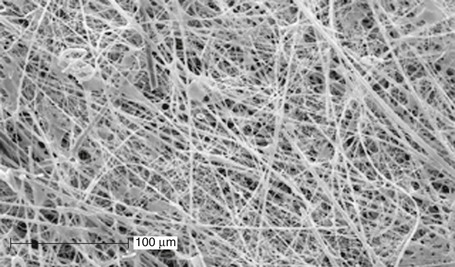
Pleated hydrophobic filters (Fig. 9.9)
1. The very small pore size filter membrane provides adequate filtration over longer periods of time. These filters rely on the naturally occurring electrostatic interactions to remove the particles. A filtration efficiency of 99.999% can be achieved.
2. To achieve minimal pressure drop across the device with such a small pore size, so allowing high gas flows while retaining low resistance, a large surface area is required. Pleated paper filters made of inorganic fibres are used to achieve this.
3. The forces between individual liquid water molecules are stronger than those between the water molecules and the hydrophobic membrane. This leads to the collection of water on the surface of the membrane with no absorption. Such a filter can successfully prevent the passage of water under pressures as high as 60 cm H2O.
4. Although hydrophobic filters provide some humidification, a hygroscopic element can be added to improve humidification.
5. Currently there is no evidence showing any type of filter is clinically superior to another.
Medical Devices Agency. Heat and moisture exchangers (HMEs) including those intended for use as breathing system filters. UK Market-Product review. London: Medical Devices Agency; 1998. No. 347
MHRA. Medical advice alert (MDA/2004/013). Online. Available at http://www.mhra.gov.uk/home/groups/dts-bs/documents/medicaldevicealert/con008574.pdf, 2004.
MHRA. Medical device alert (MDA/2004/037). Online. Available at http://www.mhra.gov.uk/home/groups/dts-bs/documents/medicaldevicealert/con008522.pdf, 2004.
Turnbull D., Fisher P.C., Mills G.H., et al. Performance of breathing filters under wet conditions: a laboratory evaluation. British Journal of Anaesthesia. 2005;94:675–682.
Wilkes A.R. Breathing system filters. British Journal of Anaesthesia CEPD Reviews. 2002;2:151–154.
Wilkes A.R., Malan C.A., Hall J.E. The effect of flow on the filtration performance of paediatric breathing system filters. Anaesthesia. 2008;63:71–76.
In the following lists, which of the statements (a) to (e) are true?
a) The gas-driven nebulizer can deliver much smaller droplets than the ultrasonic nebulizer.
b) There is a risk of drowning.
c) The temperature of the gas determines the amount of water delivered.
d) The smaller the droplets are, the more stable they are.
e) Droplets of 1 µm or less are deposited in the alveoli and lower airways.
a) Humidity is measured using a hair hygrometer.
b) Air fully saturated with water vapour has a relative humidity of about 44 mg/L at 37°C.
c) Using the circle breathing system, some humidification can be achieved despite using dry fresh gas flow.
d) Relative humidity is the ratio of the mass of water vapour in a given volume of air to the mass of water vapour required to saturate the same volume at the same temperature.
e) The ideal relative humidity in the operating theatre is about 45–55%.
3. Bacterial and viral filters:
a) Particles of less than 0.5 µm can be captured by direct interception.
b) They can achieve a filtration action of 99.999%.
c) They should be effective when either wet or dry.
d) The filtration element used can be either an electrostatic or a pleated hydrophobic material.
e) The hydrophobic filter has a more limited lifespan than the electrostatic filter.
4. Hot water bath humidifiers:
a) Heating the water improves the performance.
b) Because of its efficiency, the surface area for vaporization does not have to be large.
c) There is a risk of scalding to the patient.
d) Temperature in the humidifier is usually kept below body temperature.
e) The temperature of water in the container is controlled by a feedback mechanism using a thermistor which measures the temperature of the gases at the patient’s end.
a) Inspired gases are warmed to 29–34°C.
b) Performance is improved by increasing the volume of the medium.
c) An absolute humidity of 60–70% can be achieved.
d) At high flows, the performance is reduced.
e) Performance is affected by the temperature of the inspired and exhaled gases.
6. Which of the following statements are true:
a) Mucus can cause obstruction of the heat and moisture exchanger (HME).
b) 2–5-µm-sized nebulized droplets are deposited in the alveoli.
c) HMEs should deliver a minimum of 300 g water vapour at 30°C.
d) A relative humidity of 80% at the carina can be achieved during normal breathing.
e) HME requires some time before it reaches its optimal ability to humidify dry gases.
a) False. The ultrasonic nebulizer can deliver very much smaller droplets. 2–4-µm droplets can be delivered by the gas-driven nebulizer. Droplets of less than 1–2 µm in size can be delivered by the ultrasonic nebulizer.
b) True. This is especially so in children using the ultrasonic nebulizer.
c) False. The temperature of the gas has no effect on the quantity of water droplets delivered. The temperature of the gas is of more importance in the humidifier.
d) True. Very small droplets generated by the ultrasonic nebulizer are very stable and can be deposited in the alveoli and lower airways.
a) True. The hair hygrometer is used to measure relative humidity between 15% and 85%. It is commonly used in the operating theatre. The length of the hair increases with the increase in ambient humidity. This causes a pointer to move over a chart measuring the relative humidity.
b) False. It should be absolute humidity and not relative humidity. Relative humidity is measured as a percentage.
c) True. Water is produced as a product of the reaction between CO2 and NaOH. An absolute humidity of 29 mg/L at 37°C can be achieved.
e) True. A high relative humidity is uncomfortable for the staff in the operating theatre. Too low a relative humidity can lead to the build up of static electricity increasing the risk of ignition.
3. Bacterial and viral filters:
a) False. Such small particles are captured by diffusional interception. Direct interception can capture particles with sizes equal to or more than 1 µm.
b) True. Hydrophobic filters can achieve a filtration action of 99.999%. Electrostatic filters can achieve 99.99% which is thought to be adequate for routine use during anaesthesia.
c) True. Hydrophobic filters are effective both when dry and wet. Electrostatic filters become less effective when wet.
e) False. The electrostatic filter has a more limited lifespan than the hydrophobic filter. The efficacy of the electrostatic filter decreases as the electrical charge on the filter fibres decays.
4. Hot water bath humidifiers:
a) True. This is due to the loss of latent heat of vaporization as more water changes into vapour. The lower the water temperature, the less vapour is produced.
b) False. A large surface area is needed to improve efficiency.
c) True. A faulty thermostat can cause overheating of the water. There is usually a second thermostat to prevent this.
d) False. The temperature of the humidifier is usually kept above body temperature. A large amount of heat is lost as the vapour and gases pass through the plastic tubings.
b) True. The larger the volume of the medium, the better the performance of the HME. This is because of the larger surface area of contact between the gas and the medium.
c) False. A relative, not absolute, humidity of 60–70% can be achieved.
d) True. At high flows, the time the gas is in contact with the medium is reduced so decreasing the performance of the HME. The opposite is also correct.
e) True. The higher the temperature of the gases, the better the performance of the HME.
6. Which of the following statements are true:
a) True. Mucus can cause obstruction of the HME resulting in dangerous increases in resistance.
b) False. 2–5-µm nebulized droplets are deposited in the tracheobronchial tree. Smaller droplets of 0.5–1 µm are deposited in the alveoli.
c) False. HME should deliver a minimum of 30 g water vapour at 30°C.
e) True. HME requires 5–20 min before it reaches its optimal ability to humidify dry gases.