History of Respiratory Care
After reading this chapter you will be able to:
 Summarize some of the major events in the history of science and medicine.
Summarize some of the major events in the history of science and medicine.
 Explain how the respiratory care profession got started.
Explain how the respiratory care profession got started.
 Describe the historical development of the major clinical areas of respiratory care.
Describe the historical development of the major clinical areas of respiratory care.
 Name some of the important historical figures in respiratory care.
Name some of the important historical figures in respiratory care.
 Describe the major respiratory care educational, credentialing, and professional associations.
Describe the major respiratory care educational, credentialing, and professional associations.
 Explain how the important respiratory care organizations got started.
Explain how the important respiratory care organizations got started.
The history of science and medicine is a fascinating topic, which begins in ancient times and progresses to the twenty-first century. Although respiratory care is a newer discipline, its roots go back to the dawn of civilization. The first written account of positive pressure ventilation using mouth-to-mouth resuscitation is thought to have been recorded more than 28 centuries ago.1 Air was thought to be one of the four basic elements by the ancients, and the practice of medicine dates back to ancient Babylonia and Egypt. The progression of science and medicine continued through the centuries, and development of the modern disciplines of anesthesiology, pulmonary medicine, and respiratory care during the twentieth century was dependent on the work of many earlier scientists and physicians. This chapter describes the history and development of the field of respiratory care and possible future directions for the profession.
Definitions
Respiratory care, also known as respiratory therapy, has been defined as the health care discipline that specializes in the promotion of optimal cardiopulmonary function and health.2 Respiratory therapists (RTs) apply scientific principles to prevent, identify, and treat acute or chronic dysfunction of the cardiopulmonary system.2 Respiratory care includes the assessment, treatment, management, control, diagnostic evaluation, education, and care of patients with deficiencies and abnormalities of the cardiopulmonary system.2 Respiratory care is increasingly involved in the prevention of respiratory disease, the management of patients with chronic respiratory disease, and the promotion of health and wellness.2
Respiratory therapists, also known as respiratory care practitioners, are health care professionals who are educated and trained to provide respiratory care to patients. About 75% of all respiratory therapists work in hospitals or other acute care settings.3 However, many respiratory therapists are employed in clinics, physicians’ offices, skilled nursing facilities, cardiopulmonary diagnostic laboratories, and public schools. Others work in research, disease management programs, home care, and industry. Some respiratory therapists work in colleges and universities, teaching students the skills they need to become respiratory therapists. Regardless of practice setting, all direct patient care services provided by respiratory therapists must be done under the direction of a qualified physician. Medical directors are usually physicians who are specialists in pulmonary or critical care medicine.
A human resources survey conducted in 2009 revealed that there were approximately 145,000 respiratory therapists practicing in the United States3; this represented a 9.3% increase over a similar study conducted 4 years earlier in 2005. As the incidence of chronic respiratory diseases continues to increase, the demand for respiratory therapists is expected to be even greater in the years ahead. Although the respiratory therapist as a distinct health care provider was originally a uniquely North American phenomenon, since the 1990s there has been a steady increase in interest of other countries in having specially trained professionals provide respiratory care. This trend is referred to as the “globalization of respiratory care.”
History of Respiratory Medicine and Science
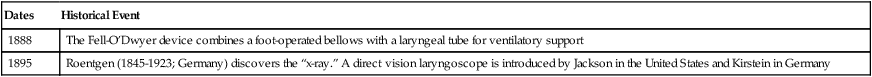
Several excellent reviews of the history of respiratory care have been written, and the reader is encouraged to review these publications.1,4–6 Summaries of notable historical events in science, medicine, and respiratory care are provided in Tables 1-1 and 1-2. A brief description of the history of science and medicine follows.
TABLE 1-1
| Dates | Historical Event |
| Ancient Period | |
| 1550 bc | What may be the world’s oldest medical document, known as Ebers Papyrus, describes an ancient Egyptian inhalational treatment for asthma |
| 800 bc | Biblical reference to what may be the first recorded episode of mouth-to-mouth resuscitation |
| 500-300 bc | Hippocrates (460-370 bc; Greece) describes diseases as “humoral disorders” and speculates that an essential substance in air enters the heart and is distributed throughout the body |
| 304 bc | Erasistratus of Alexandria describes the pneumatic theory of respiration, in which air travels through the lungs to the heart and then through the air-filled arteries to the tissues of the body |
| 100-200 ad | Galen (130-199 ad) in Asia Minor identifies “pneuma” as the vital substance in inspired air that enters the heart and then the blood |
| Middle Ages (500-1500 ad) and Renaissance (1450-1600) | |
| 500-1500 ad | The Middle Ages brings a period of little scientific progress in the West; however, this period coincides with the Golden Age of Arabian medicine (850-1050 ad) |
| 1400s-1500s | da Vinci (1452-1519; Italy) performs human dissections and physiologic experiments on animals, learning that subatmospheric intrapleural pressures inflate the lungs and that there is a vital substance in air that supports combustion |
| 1542 | Vesalius (1514-1564; Belgium), one of the great early pioneers in human anatomy, performs a thoracotomy on a pig, placing a reed tracheotomy tube for ventilation of the animal, and resuscitates an apparently dead person |
| Seventeenth Century (1600s) | |
| 1628 | Harvey (1578-1657; England) describes the arterial and venous circulatory systems |
| 1643 | Torricelli (1608-1647; Italy) builds the world’s first barometer for measurement of atmospheric pressure |
| 1648 | Pascal (1623-1662) describes the relationship between altitude and barometric pressure |
| 1662; 1666 | Boyle (1627-1691; England) explains the inverse relationship between gas pressure and volume (Boyle’s law: pressure [P] × volume [V] = k or [P1V1] = [P2V2]). Boyle also describes a mysterious substance in air that supports combustion |
| 1683 | van Leewenhoek (1632-1723; Holland) improves the microscope and begins the science of microbiology |
| Eighteenth Century (1700s) | |
| 1738 | Bernoulli (1700-1782; Switzerland) determines that as the velocity of a liquid or gas increases, the pressure decreases (Bernoulli principle). Bernoulli also proposed that gases are composed of tiny particles in rapid, random motion. This idea became the basis of the modern kinetic theory of gases, which was developed further by Maxwell (1831-1879; Scotland) in 1860 |
| 1744 | Fothergill (1712-1780; England) reports successful resuscitation methods |
| 1754 | Black (1728-1799; Scotland) rediscovers carbon dioxide, which he calls “fixed air” (prior work had been done by van Helmot in the 1600s) |
| 1771 | Scheele (1742-1786; Sweden) makes “fire air” (oxygen) by heating magnesium oxide; Scheele’s findings are published in June 1774 |
| 1774 | Priestley (1733-1804; England), usually credited with the discovery of oxygen, publishes his work on “dephlogisticated air” (oxygen) 3 months after Scheele’s report |
| 1775 | Lavosier (1743-1794; France) renames “dephlogisticated air” “oxygen,” or “acid maker” and shows that oxygen is absorbed by the lungs and consumed by the body, producing carbon dioxide and water vapor, which are exhaled |
| 1776 | Hunter (1728-1793; England) recommends use of a fireplace bellows for artificial ventilation |
| 1787 | Charles (1746-1823; France) describes the relationship between gas temperature and volume; Charles’ law: volume (V)/temperature (T) = constant; or (V1/T1) = (V2/T2) |
| 1794 | Lavosier (1743-1794; France) describes oxygen absorption by the lungs and carbon dioxide production |
| 1798 | Beddoes (1760-1808; England) establishes the Pneumatic Institute in Bristol and uses oxygen to treat various disorders |
| Nineteenth Century (1800s) | |
| 1800 | Henry (1774-1836; England) determines that the amount of gas dissolved in a liquid is directly proportioned to its partial pressure (Henry’s law) |
| 1800s | Fick (1829-1911) describes a method to calculate cardiac output based on oxygen consumption and arterial and venous oxygen content: 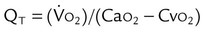 |
| 1801-1808 | Dalton (1766-1844; England) describes his atomic theory and the relationship between the partial pressures and total pressure of a gas mixture; Dalton’s law: P1 + P2 + P3 … PN = PTotal, where P = pressure |
| 1806 | de LaPlace (1749-1827; France) describes the relationship between pressure and surface tension in fluid droplets |
| 1808 | Gay-Lussac (1778-1850; France) describes the relationship between gas pressure and temperature; Gay-Lussac’s law: pressure (P)/temperature (T) = constant; or (P1/T1) = (P2/T2) |
| 1811 | Avogadro (1776-1856; Italy) describes “Avogadro principle,” where equal volumes of all gases (at the same temperature and pressure) contain the same number of molecules |
| 1816 | Laennec (1781-1826; France) invents the stethoscope for chest auscultation and lays the foundation for modern pulmonology with his book Diseases of the Chest |
| 1831 | Graham (1805-1869; Scotland) describes diffusion of gases (Graham’s law) |
| 1837 | Magnus (1802-1870; Germany) measures arterial and venous blood oxygen and carbon dioxide content |
| 1846 | Hutchinson (1811-1861; England) develops the spirometer and measures the vital capacity of more than 2000 human subjects |
| 1864 | Jones (United States) patents a negative pressure device to support ventilation |
| 1865 | Pasteur (1822-1895; France) describes his “germ theory” of disease |
| 1876 | Woillez develops the spirophore negative pressure ventilator |
| 1878 | Bert (1833-1886; France) shows that low inspired oxygen levels cause hyperventilation |
| 1880 | MacEwen reports success with oral endotracheal intubation |
| 1885 | Miescher-Rusch demonstrates that carbon dioxide is the major stimulus for breathing |
| 1886; 1904 | Bohr (1855-1911; Danish) describes the oxyhemoglobin dissociation curve |
| 1888 | The Fell-O’Dwyer device combines a foot-operated bellows with a laryngeal tube for ventilatory support |
| 1895 | Roentgen (1845-1923; Germany) discovers the “x-ray.” A direct vision laryngoscope is introduced by Jackson in the United States and Kirstein in Germany |
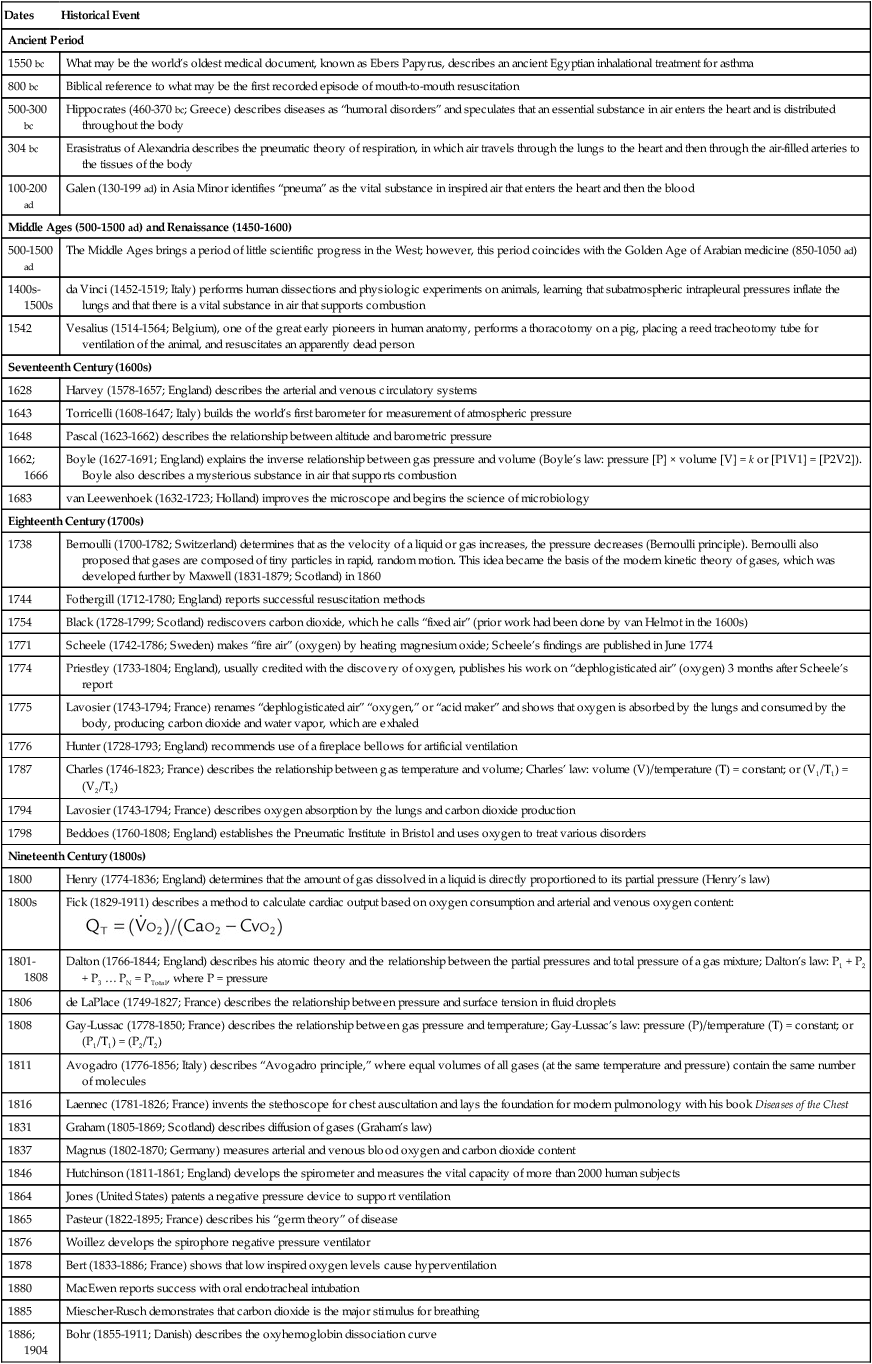
Data from references 1, 3–13, and 16.
TABLE 1-2
| Twentieth Century | |
| Early 1900s | Bohr (1855-1911; Denmark), Hasselbach (1874-1962; Denmark), Krogh (1874-1940; Denmark), Haldane (1860-1936; Scotland), Barcroft (1872-1947; Ireland), Priestly (1880-1941; Britain), Y. Henderson (1873-1944; United States), L.J. Henderson (1878-1942; United States), Fenn (1893-1971; United States), Rahn (1912-1990; United States), and others make great strides in respiratory physiology and the understanding of oxygenation, ventilation, and acid-base balance |
| 1904 | Bohr, Hasselbach, and Krogh (1874-1940) describe the relationships between oxygen and carbon dioxide transport. Sauerbruch (1875-1951; Germany) uses a negative pressure operating chamber for surgery in Europe |
| 1907 | von Linde (1842-1934; Germany) begins large-scale commercial preparation of oxygen |
| 1909 | Melltzer (1851-1920; United States) introduces oral endotracheal intubation |
| 1910 | Oxygen tents are in use, and the clinical use of aerosolized epinephrine is introduced |
| 1911 | Drager (1847-1917; Germany) develops the Pulmotor ventilator for use in resuscitation |
| 1913 | Jackson develops a laryngoscope to insert endotracheal tubes |
| 1918 | Oxygen mask is used to treat combat-induced pulmonary edema |
| 1919 | Strohl (1887-1977; France) suggests the use of FVC as a measure of pulmonary function |
| 1920 | Hill develops an oxygen tent to treat leg ulcers |
| 1926 | Barach develops an oxygen tent with cooling and carbon dioxide removal |
| 1928 | Drinker develops his “iron lung” negative pressure ventilator |
| 1938 | Barach develops the meter mask for administering dilute oxygen. Boothby, Lovelace, and Bulbulian devise the BLB mask at the Mayo Clinic for delivering high concentrations of oxygen |
| 1940 | Isoproterenol, a potent beta-1 and beta-2 bronchodilator administered via aerosol, is introduced. Most common side effects are cardiac (beta-1) |
| 1945 | Motley, Cournand, and Werko use IPPB to treat various respiratory disorders |
| 1947 | The ITA is formed in Chicago, Illinois. The ITA later becomes the AARC |
| 1948 | Bennett introduces the TV-2P positive pressure ventilator |
| 1948 | FEV1 is introduced as a pulmonary function measure of obstructive lung disease |
| 1951 | Isoetherine (Bronkosol), a preferential beta-2 aerosol bronchodilator with fewer cardiac side effects, is introduced |
| 1952 | Mørch introduces the piston ventilator |
| 1954 | The ITA becomes the AAIT |
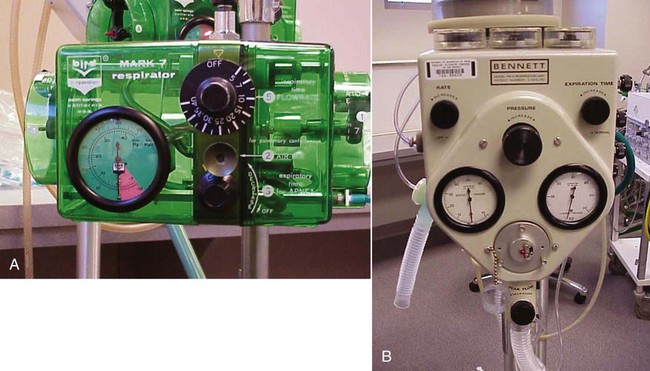
| 1958 | Bird introduces the Bird Mark 7 positive pressure ventilator |
| 1960 | The Campbell Ventimask for delivering dilute concentrations of oxygen is introduced |
| 1961 | Jenn becomes the first registered respiratory therapist. Also, metaproterenol, a preferential beta-2 bronchodilator, is introduced |
| 1963 | Board of Schools is formed to accredit inhalation therapy educational programs |
| 1964 | The Emerson Postoperative Ventilator (3-PV) positive pressure volume ventilator is introduced |
| 1967 | The Bennett MA-1 volume ventilator is introduced, ushering in the modern age of mechanical ventilatory support for routine use in critical care units |
| 1967 | Combined pH-Clark-Severinghaus electrode is developed for rapid blood gas analysis |
| 1968 | Fiberoptic bronchoscope becomes available for clinical use. The Engström 300 and Ohio 560 positive pressure volume ventilators are introduced |
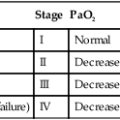
| 1969 | ARDS and PEEP are described by Petty, Ashblaugh, and Bigelow |
| 1970 | Swan-Ganz catheter developed for measurement of pulmonary artery pressures. The ARCF is incorporated. The JRCITE is incorporated to accredit respiratory therapy educational programs |
| 1971 | Continuous positive airway pressure is introduced by Gregory. Respiratory Care journal is named |
| 1972 | Siemens Servo 900 ventilator is introduced |
| 1973 | IMV is described by Kirby and Downs. The AAIT becomes the AART |
| 1974 | IMV Emerson ventilator is introduced |
| 1974 | NBRT is formed |
| 1975 | Bourns Bear I ventilator is introduced |
| 1977 | The JRCITE becomes the JRCRTE |
| 1978 | Puritan Bennett introduces the MA-2 volume ventilator. The AAR Times magazine is introduced |
| 1979 | AIDS is recognized by the Centers for Disease Control (CDC [later, Centers for Disease Control and Prevention]) |
| 1982 | Siemens Servo 900C and Bourns Bear II ventilators are introduced |
| 1983 | The NBRT becomes the NBRC |
| 1983 | President Reagan signs proclamation declaring National Respiratory Care Week |
| 1984 | Bennett 7200 microprocessor controlled ventilator is introduced |
| 1984 | The AART is renamed the AARC |
| 1991 | Servo 300 ventilator is introduced |
| 1992, 1993 | The AARC holds national respiratory care education consensus conferences |
| 1994 | The CDC publishes the first guidelines for the prevention of VAP |
| 1998 | The CoARC is formed, replacing the JRCRTE |
| Twenty-First Century | |
| 2002 | The NBRC adopts a continuing competency program for respiratory therapists to maintain their credentials |
| 2002 | The Tripartite Statements of Support are adopted by the AARC, NBRC, and CoARC to advance respiratory care education and credentialing |
| 2003 | The AARC publishes its white paper on the development of baccalaureate and graduate education in respiratory care. Asian bird flu appears in South Korea |
| 2004 | The Fiftieth AARC International Congress is held in New Orleans |
| 2005 | Number of working respiratory therapists in the United States reaches 132,651 |
| 2006 | The National Heart, Lung and Blood Institute (NHLBI) of the U.S. Department of Health and Human Services begins national awareness and education campaign for COPD. The AARC works with government officials to recruit and train respiratory therapists for disaster response |
| 2007 | The first AARC president to serve a 2-year term begins term of office |
| 2008 | First of three conferences held for 2015 and Beyond strategic initiative of the AARC |
Data from references 1, 3–13, and 16.
Ancient Times
Humans have been concerned about the common problems of sickness, disease, old age, and death since primitive times. Early cultures developed herbal treatments for many diseases, and surgery may have been performed in Neolithic times. Physicians practiced medicine in ancient Mesopotamia, Egypt, India, and China.1,4,7 However, the foundation of modern Western medicine was laid in ancient Greece with the development of the Hippocratic Corpus.1,4,7,8 This ancient collection of medical treatises is attributed to the “father of medicine,” Hippocrates, a Greek physician who lived during the fifth and fourth centuries bc.1,7,8 Hippocratic medicine was based on four essential fluids, or “humors”—phlegm, blood, yellow bile, and black bile—and the four elements—earth (cold, dry), fire (hot, dry), water (cold, moist), and air (hot, moist). Diseases were thought to be humoral disorders caused by imbalances in these essential substances. Hippocrates believed there was an essential substance in air that was distributed to the body by the heart.1 The Hippocratic Oath, which admonishes physicians to follow certain ethical principles, is given in a modern form to many medical students at graduation.1,8
Aristotle (384-322 bc), a Greek philosopher and perhaps the first great biologist, believed that knowledge could be gained through careful observation.1,8 Aristotle made many scientific observations, including observations obtained by performing experiments on animals. Erasistratus (about 330-240 bc), regarded by some as the founder of the science of physiology, developed a pneumatic theory of respiration in Alexandria, Egypt, in which air (“pneuma”) entered the lungs and was transferred to the heart.1,7 Galen (130-199 ad) was an anatomist in Asia Minor whose comprehensive work dominated medical thinking for centuries.1,6,7 Galen also believed that inspired air contained a vital substance that somehow charged the blood through the heart.1
Middle Ages, the Renaissance, and the Enlightenment Period
The Romans carried on the Greek traditions in philosophy, science, and medicine. With the fall of the Western Roman Empire in 476 ad, many Greek and Roman texts were lost and Europe entered a period during which there were few advances in science or medicine. In the seventh century ad, the Arabians conquered Persia, where they found and preserved many of the works of the ancient Greeks, including the works of Hippocrates, Aristotle, and Galen.1,7 A Golden Age of Arabian medicine (850-1050 ad) followed.
An intellectual rebirth in Europe began in the twelfth century.1,7 Medieval universities were formed, and contact with the Arabs in Spain and Sicily reintroduced ancient Greek and Roman texts. Magnus (1192-1280) studied the works of Aristotle and made many observations related to astronomy, botany, chemistry, zoology, and physiology. The Renaissance (1450-1600) ushered in a period of scientific, artistic, and medical advances. da Vinci (1452-1519) studied human anatomy, determined that subatmospheric interpleural pressures inflated the lungs, and observed that fire consumed a vital substance in air without which animals could not live.1,4 Vesalius (1514-1564), considered to be the founder of the modern field of human anatomy, performed human dissections and experimented with resuscitation.1 In 1543, the date commonly given as the start of the modern Scientific Revolution, Copernicus observed that the Earth orbited the sun.8 Before this time, it had been accepted that the Earth was the center of the universe.
The seventeenth century was a time of great advances in science. Accomplished scientists from this period include Kepler, Bacon, Galileo, Pascal, Hooke, and Newton. In 1628, Harvey fully described the circulatory system.4,8 In 1662, the chemist Boyle published what is now known as Boyle’s law, governing the relationship between gas volume and pressure.8 Torricelli invented the barometer in 1650, and Pascal showed that atmospheric pressure decreases with altitude.1,4 van Leeuwenhoek (1632-1723), known as the “father of microbiology,” improved the microscope and was the first to observe and describe single-celled organisms, which he called “animalcules.”7
The eighteenth-century Enlightenment Period brought further advances in the sciences. In 1754, Black described the properties of carbon dioxide, although the discovery of carbon dioxide should be credited to van Helmont, whose work occurred about 100 years earlier.1 In 1774, Priestley described his discovery of oxygen, which he called “dephlogisticated air.”1,4 Before 1773, Scheele performed the laboratory synthesis of oxygen, which he called “fire air”; a general description of his discovery appeared in 1774, and a more thorough description appeared in 1777.1,4 Shortly after the discovery of oxygen, Spallazani worked out the relationship between the consumption of oxygen and tissue respiration.1 In 1787, Charles described the relationship between gas temperature and volume now known as Charles’ law.8 In experiments performed between 1775 and 1794, Lavoisier showed that oxygen was absorbed by the lungs and that carbon dioxide and water were exhaled.1,4 In 1798, Beddoes began using oxygen to treat various conditions at his Pneumatic Institute in Bristol.1,4
Nineteenth and Early Twentieth Centuries
During the nineteenth century, important advances were made in physics and chemistry related to respiratory physiology. Dalton described his law of partial pressures for a gas mixture in 1801 and his atomic theory in 1808.8 Young in 1805 and de LaPlace in 1806 described the relationship between pressure and surface tension in fluid droplets.8 Gay-Lussac described the relationship between gas pressure and temperature in 1808, and in 1811, Avogadro stated that equal volumes of gases at the same temperature and pressure contain the same number of molecules.1,8 In 1831, Graham described his law of diffusion for gases (Graham’s law).8
In 1865, Pasteur advanced his “germ theory” of disease, which held that many diseases are caused by microorganisms.8 Medical advances during this time included the invention of the spirometer and ether anesthesia in 1846, antiseptic techniques in 1865, and vaccines in the 1880s.1,4,7 Koch, a pioneer in bacteriology, discovered the tubercle bacillus, which causes tuberculosis, in 1882 and the vibrio bacterium, which causes cholera, in 1883.7 Respiratory physiology also progressed with the measurement in 1837 of blood oxygen and carbon dioxide content, the description around 1880 of the respiratory quotient, demonstration in 1885 that carbon dioxide is the major stimulant for breathing, and demonstration in 1878 that oxygen partial pressure and blood oxygen content were related.1,4,9 In 1895, Roentgen discovered the x-ray, and the modern field of radiologic imaging sciences was born.8 Pioneering respiratory physiologists of the early twentieth century described oxygen diffusion, oxygen and carbon dioxide transport, the oxyhemoglobin dissociation curve, acid-base balance, and the mechanics of breathing and made other important advances in respiratory physiology (see Table 1-2).
Development of the Respiratory Care Profession
Clinical Advances in Respiratory Care
The first health care specialists in the field were oxygen technicians in the 1940s.1,4,5 The first inhalation therapists were oxygen technicians or oxygen orderlies who could haul cylinders of oxygen and related equipment around the hospital and set up oxygen tents, masks, and nasal catheters. The development of positive pressure breathing during World War II for breathing support of high-altitude pilots led to its use as a method to treat pulmonary patients and deliver aerosol medications during the 1950s, expanding the role of the inhalation therapist. Inhalation therapists began to be trained in the 1950s, and formal education programs began in the 1960s.1,4,5 The development of sophisticated mechanical ventilators in the 1960s naturally led to a further expansion in the role of respiratory therapists, who soon also found themselves responsible for arterial blood gas and pulmonary function laboratories. In 1974, the designation “respiratory therapist” became standard, and the respiratory therapist became the allied health professional primarily concerned with the assessment, diagnostic testing, treatment, education, and care of patients with deficiencies and abnormalities of the cardiopulmonary system. The historical development of several clinical areas of respiratory care is described next, followed by an overview of the establishment of the major professional organizations in the field. The evolution of respiratory care education is also described.
Oxygen Therapy
Although the therapeutic administration of oxygen first occurred in 1798, and Bert showed that lack of oxygen caused hyperventilation in 1878, the physiologic basis and indications for oxygen therapy were not well understood until the twentieth century.1,4 Large-scale production of oxygen was developed by von Linde in 1907. The use of a nasal catheter for oxygen administration was introduced by Lane in the same year.1,4 Oxygen tents were in use in 1910, and an oxygen mask was used to treat combat gas–induced pulmonary edema in 1918.1 In 1920, Hill developed an oxygen tent to treat leg ulcers, and in 1926, Barach introduced a sophisticated oxygen tent for clinical use. Oxygen chambers and whole oxygen rooms were designed.1,4 In 1938, a meter mask was developed by Barach to administer dilute oxygen.1,4 The BLB mask (named for Boothby, Lovelace, and Bulbulian) to administer 80% to 100% oxygen to pilots was introduced during World War II and later used on patients.1,4 By the 1940s, oxygen was widely prescribed in hospitals, although there was still no good way to measure blood oxygen levels routinely until the mid-1960s, with the introduction of the Clark electrode, followed by the clinical use of the ear oximeter in 1974 and the pulse oximeter in the 1980s.1,4,5 The Campbell Ventimask, which allowed the administration of 24%, 28%, 35%, or 40% oxygen, was introduced in 1960, and modern versions of the nasal cannula, simple oxygen mask, partial rebreathing mask, and nonrebreathing mask were available by the late 1960s. Portable liquid oxygen systems for long-term oxygen therapy in the home were introduced in the 1970s, and the oxygen concentrator soon followed. Oxygen-conserving devices, including reservoir cannulas, demand pulse oxygen systems, and transtracheal oxygen catheters, were introduced in the 1980s.
Aerosol Medications
Aerosol therapy is defined as the administration of liquid or powdered aerosol particles via inhalation to achieve a desired therapeutic effect. Bland aerosols (sterile water, saline solutions) or solutions containing pharmacologically active drugs may be administered. In 1802, the use of inhaled Datura leaf fumes, which contain atropine, to treat asthma was described.10 Early use of aerosol medications dates to 1910, when the first use of aerosolized epinephrine was reported. Later, other short-acting bronchodilators such as isoproterenol (1940), isoetharine (1951), metaproterenol (1961), albuterol sulfate (1980), and levalbuterol (2000) were introduced, primarily for the emergency treatment of acute asthma attacks.10 Oral and injectable steroids were first used in the treatment of asthma in the early 1950s, and the use of aerosolized steroids for the maintenance of patients with moderate to severe asthma began in the 1970s.10 Since that time, numerous medications have been designed for aerosol administration, including long-acting bronchodilators, mucolytics, antibiotics, and antiinflammatory agents. Along with newer respiratory drugs, newer delivery devices such as dry powder inhalers and innovative designs for small volume nebulizers have been introduced.
Mechanical Ventilation
Mechanical ventilation refers to the use of a mechanical device to provide ventilatory support for patients. In 1744, Fothergill advocated mouth-to-mouth resuscitation for drowning victims.1,6 During the mid to late 1700s, there was a great deal of interest in resuscitation, and additional procedures for cardiopulmonary resuscitation (CPR) were developed.1,4,6 Positive pressure ventilation using a bag-mask system or bellows was suggested. However, the observation that a fatal pneumothorax may result caused this technique to be rejected around 1827.1,4 Interest in negative pressure ventilation developed, and the first negative pressure tank ventilator was described in 1832.6 Other negative pressure ventilators began to appear in the mid-1800s; in 1928, the iron lung was developed by Drinker, an industrial hygienist and faculty member at Harvard University.1 Emerson developed a commercial version of the iron lung that was used extensively during the polio epidemics of the 1930s and 1950s (Figure 1-1).1,11 The chest cuirass negative pressure ventilator was introduced in the early 1900s, and a negative pressure “wrap” ventilator was introduced in the 1950s.12 Other early noninvasive techniques to augment ventilation included the rocking bed (1950) and the pneumobelt (1959).12

Originally, positive pressure ventilators were developed for use during anesthesia and later were altered for use on hospital wards.13 Early positive pressure ventilators included the Drager Pulmotor (1911), the Spiropulsator (1934), the Bennett TV-2P (1948), the Morch Piston Ventilator (1952), and the Bird Mark 7 (1958) (Figure 1-2).1,13 More sophisticated positive pressure volume ventilators were developed in the 1960s and included the Emerson Postoperative Ventilator, MA-1 (Figure 1-3), Engstrom 300, and Ohio 560.1,13 A new generation of volume ventilators appeared in the 1970s that included the Servo 900, Bourns Bear I and II, and MA-II. By the 1980s, microprocessor-controlled ventilators began to appear, led by the Bennett 7200 in 1984, and in 1988, the Respironics BiPAP (bilevel positive airway pressure) device was introduced for providing noninvasive positive pressure ventilation in a wide variety of settings.1 During the 1990s and early 2000s, new ventilators have continued to be developed, including the Hamilton Galileo, Servo-i, Bennett 840, and Drager Evita series (see Chapter 42). Since 1970, more than 50 new ventilators have been introduced with various characteristics for clinical use.14,15
Early mechanical ventilators provided only controlled ventilation. “Assist-control” as a mode of ventilation appeared with the early Bird and Bennett pressure-limited ventilators in the 1950s, which were often used for intermittent positive pressure breathing (IPPB). Positive end-expiratory pressure (PEEP) was introduced for use in patients with acute respiratory distress syndrome (ARDS) in 1967. The modern form of intermittent mandatory ventilation (IMV) was introduced in 1971, followed by synchronized intermittent mandatory ventilation in 1975 and mandatory minute volume ventilation in 1977.1,4 Pressure support ventilation and pressure control ventilation were introduced in the 1980s, followed by airway pressure release ventilation and inverse ratio ventilation. In the 1990s, volume support ventilation, pressure-regulated volume control, and adaptive support ventilation were introduced. The commercial implementation of proportional assist ventilation and other modes of ventilation occurred in the twenty-first century.
Airway Management
Airway management refers to the use of various techniques and devices to establish or maintain a functional air passageway. Tracheotomies may have been performed to relieve airway obstruction in 1500 bc.6 Galen, the Greek anatomist, described a tracheotomy and laryngeal intubation in 160 ad. Vesalius, the anatomist, described a tracheotomy in an animal in 1555.1,6 In 1667, Hooke described a tracheotomy and use of a bellows for ventilation.6 In 1776, tracheal intubation was suggested for resuscitation.6 In 1880, MacEwen reported success with oral endotracheal intubation in patients.6 O’Dwyer further described the technique for endotracheal tube placement. By 1887, Fell had developed a bellows-endotracheal tube system for mechanical ventilation, and this system was used in 1900 to deliver anesthesia.6
In 1913, the laryngoscope was introduced by Jackson. Additional early laryngoscopes were designed by Kirstein, Janeway, and others.1,6 Endotracheal intubation for anesthesia administration was firmly established by World War I. After the war, Magill introduced the use of soft rubber endotracheal tubes, and this made blind nasal intubation possible, as described by Magill in 1930.6 In 1938, Haight advocated nasotracheal suctioning for secretion removal, and in 1941, Murphy described the ideal suction catheter, which included side holes known as “Murphy eyes.”6 The double-lumen Carlen tube for independent lung ventilation was introduced in 1940, followed by a double-lumen tube developed by Robertshaw in 1962. Damage to the trachea by the tube cuff was reduced with the introduction of low-pressure cuffs in the 1970s.6
Cardiopulmonary Diagnostics and Pulmonary Function Testing
Pulmonary function testing refers to a wide range of diagnostic procedures to measure and evaluate lung function. The volume of air that can be inhaled in a single deep breath was first measured in 1679, and the measurement of the lung’s residual volume was first performed in 1800.9 In 1846, Hutchinson developed a water seal spirometer, with which he measured the vital capacity of more than 2000 subjects.9,16 Hutchinson observed the relationship between height and lung volume and that vital capacity decreases with age, obesity, and lung disease. Hering and Breuer described the effects of lung inflation and deflation on breathing—the “Hering-Breuer reflex”—in 1868.4 In 1919, Strohl suggested the use of forced vital capacity (FVC), and in 1948, forced expiratory volume in 1 second (FEV1) was suggested as a measure of obstructive lung disease by Tiffeneau.9
Arterial and venous oxygen and carbon dioxide contents were measured in 1837, and methods to measure blood oxygen and carbon dioxide levels were available in the 1920s. These early methods for measuring blood oxygen, carbon dioxide, and pH were slow and cumbersome. In 1967, the combined pH, Clark, and Severinghaus electrodes produced a rapid and practical blood gas analyzer for routine clinical use.1,4 The ear oximeter was introduced in 1974, and the pulse oximeter was introduced in the 1980s. Sleep medicine became well established in the 1980s, and polysomnography became a routine clinical test, often performed by respiratory therapists.
Professional Organizations and Events
American Association for Respiratory Care (AARC)
Founded in 1947 in Chicago, the Inhalational Therapy Association (ITA) was the first professional association for the field of respiratory care.1,4,5 The purpose of the ITA was to provide for professional advancement, foster cooperation with physicians, and advance the knowledge of inhalation therapy through educational activities.5 The ITA provided a forum to discuss the clinical application of oxygen therapy, improve patient care, and advance the art and science of the field.1 There were 59 charter members of the ITA.1 The ITA became the American Association for Inhalation Therapists (AAIT) in 1954, the American Association for Respiratory Therapy (ARRT) in 1973, and the American Association for Respiratory Care (AARC) in 1982.4,5 By early 2011, membership in the AARC had reached 52,000 respiratory therapists, respiratory therapy students, physicians, nurses, and others interested in respiratory care. The AARC also has a formal affiliation with all 50 state respiratory societies (known as Chartered Affiliates) as well as with similar organizations in several foreign countries.17
The stated mission of the AARC is to “encourage and promote professional excellence, advance the science and practice of respiratory care, and serve as an advocate for patients, their families, the public, the profession and the respiratory therapist.”18 The AARC serves as an advocate for the profession to legislative and regulatory bodies, the insurance industry, and the general public. To fulfill its mission, the AARC sponsors many continuing educational activities, including international meetings, conferences and seminars, publications, and a sophisticated website (see www.AARC.org). In addition to the monthly science journal Respiratory Care, the AARC publishes the monthly news magazine AARC Times and numerous electronic newsletters. In the fall of each year, the AARC also sponsors the International Respiratory Congress, the largest respiratory care scientific meeting in the world. Finally, in an effort to ensure that the unique practice interests of AARC members are addressed (e.g., neonatal/pediatrics, adult acute care, management, home care, diagnostics), members are invited to join one or more of 10 Specialty Sections (Box 1-1) within the AARC, designed to facilitate networking and the free exchange of ideas.
American Respiratory Care Foundation (ARCF)
Established in 1970 by the AARC, the American Respiratory Care Foundation (ARCF) is a not-for-profit charitable foundation that helps promote and further the mission of the AARC. Commonly known as the Foundation, the ARCF collects and manages contributions from individuals, corporations, and other foundations to recognize individual achievements of excellence in clinical practice, chronic disease management, public respiratory health, scientific research, and literary excellence. The ARCF also provides research grants to establish the scientific basis of respiratory care further. Lastly, the ARCF oversees and distributes numerous scholarships for respiratory therapy students who are student members of the AARC. The ARCF awards and scholarships are presented at the awards ceremony held in conjunction with the annual International Respiratory Congress of the AARC. Respiratory therapy students who are interested in applying for an ARCF scholarship should visit the ARCF website (see www.arcfoundation.org) to learn more about this great opportunity.
National Board for Respiratory Care (NBRC)
The credentialing body for registered respiratory therapists began in 1960 as the American Registry of Inhalation Therapists (to test and credential registered therapists), and a certification board was established in 1968 to certify technicians.1,4 These two groups merged in 1974 as the National Board for Respiratory Therapy, which became the National Board for Respiratory Care (NBRC) in 1983.1,4 Also in 1983, the National Board for Cardiopulmonary Technologists joined the NBRC, and the credentialing examinations for pulmonary function technology were brought in under the respiratory care umbrella.1,4 Since 1968, there have been two levels of clinical practice credentialing examinations in the United States: the certified technician and the registered therapist (see www.NBRC.org).
In 1998, the NBRC renamed the lower level certified respiratory therapist (CRT, or entry-level respiratory therapist); the advanced level remained registered respiratory therapist (RRT, or advanced-level respiratory therapist).19 The NBRC began offering specialty examinations for pulmonary function technology in 1984 and neonatal/pediatrics in 1991. The NBRC is considering new specialty credentialing examinations in the areas of polysomnography and critical care.
Committee on Accreditation for Respiratory Care (CoARC)
In 1956, the first guidelines for respiratory care educational programs were published, followed by the formation of the Board of Schools to accredit programs in 1963.1 The Board of Schools was replaced by the Joint Review Committee for Inhalation Therapy Education (JRCITE) in 1970, led by its first chairman, Helmholtz.1,4 The JRCITE became the Joint Review Committee for Respiratory Therapy Education (JRCRTE) in 1977 and then the Committee on Accreditation for Respiratory Care (CoARC) in 1996 (see www.COARC.com).4 Today, respiratory care educational programs in the United States are accredited by the CoARC in collaboration with the Association of Specialized and Professional Accreditors.20–22
Respiratory Care Education
The first formal educational course in inhalation therapy was offered in Chicago in 1950.1 In the 1960s, numerous schools were developed to prepare students to become respiratory therapists. Early programs concentrated on teaching students the proper application of oxygen therapy, oxygen delivery systems, humidifiers, and nebulizers and the use of various IPPB devices. The advent of sophisticated critical care ventilators, blood gas analyzers, and monitoring devices in the 1960s and 1970s helped propel the respiratory therapist into the role of cardiopulmonary technology expert.
Respiratory care educational programs in the United States are offered at technical and community colleges, 4-year colleges, and universities. These programs are designed to prepare competent respiratory therapists to care for patients. The minimum degree required to become a respiratory therapist is an associate degree.20 There are approximately 300 associate, 50 baccalaureate, and 3 graduate-level degree programs in the United States; 19 programs in Canada; and a handful of respiratory care educational programs in Mexico, South America, Japan, India, Taiwan, and other countries.22–24
The AARC completed a Delphi study and held two important Education Consensus Conferences in the early 1990s to assess the status of respiratory care education and recommend future direction for the field.25–28 The first conference suggested that major trends affecting the field were advances in technology; demographic trends and the aging of the population; a need to provide better assessment, outcome evaluation, problem solving, and analytical skills; use of protocol-based care; and the need to increase the focus on patient education, prevention, and wellness, to include tobacco education and smoking cessation.26 The conference concluded that the curriculum should encompass a broad scope of clinical practice, a significant arts and science component, emphasis on communication skills, and a minimum of an associate degree to enter practice. The second Educational Consensus Conference, held in the fall of 1993, focused on strategies to implement the recommendations made at the first conference.28 Both conferences identified the need for more baccalaureate and graduate education in respiratory care. The view that programs should prepare students better in the areas of patient assessment, care plan development, protocols, disease management, pulmonary rehabilitation, research, and geriatrics/gerontology became well accepted.29,30
In 1997, Mishoe and MacIntyre31 described a profession as “a calling or vocation requiring specialized knowledge, methods, and skills as well as preparation, in an institution of higher learning, in the scholarly, scientific, and historical principles underlying such methods and skills.” These authors noted that professional roles are different and more complex than technical roles, which are oriented to performing specific tasks as ordered by the physician. Examples of professional roles in respiratory care include patient assessment and care plan development, ventilator management, disease management, pulmonary rehabilitation, and respiratory care consulting services. Technical roles may include basic task performance (e.g., oxygen, aerosol therapy, bronchial hygiene), routine diagnostic testing (e.g., electrocardiography, phlebotomy), and other routine tasks where little or no assessment is required and decisions are limited to device selection and fine-tuning therapy.31 In professional practice, the therapist may function as a physician extender who applies protocols or guidelines.31 Examples include making protocol-based ventilator adjustments, applying assessment-based care plans, and performance of advanced procedures such as arterial line insertion and management, intubation and extubation of patients, application of ventilator weaning protocols, and application of advanced cardiopulmonary technologies (e.g., extracorporeal membrane oxygenation, nitric oxide therapy, aortic balloon pumps).
According to Mishoe and MacIntyre, economic, educational, and institutional forces may limit respiratory care in certain settings to a task-oriented, technical role. There are many opportunities, however, for the respiratory therapist to function as a physician extender, in a role similar to the physician assistant. Working under the supervision of a physician, the physician assistant may perform many medical procedures that might otherwise be performed by a physician. In a similar way, the respiratory physician extender could improve the quality of care while controlling costs and minimizing unnecessary care. Many authorities believe that the critical thinking, assessment, problem-solving, and decision-making skills needed for advanced practice in the twenty-first century require advanced levels of education.31
In 1998, Hess32 observed that a task orientation has coincided with a pattern of overordering and misallocation of respiratory care services. Therapist-driven protocols and the increasing use of the respiratory therapist as a consultant may allow physicians to order protocols as opposed to specific therapies. The therapist assesses the patient, develops a care plan, implements the plan, and evaluates and modifies care as appropriate.32 Protocol-based care has been shown to be safe and effective, while reducing misallocation of care and helping to control costs.32,33 Acceptance by physicians of respiratory therapists as consultants depends on the professionalism, education, and skill of the therapists at the bedside.32
In 2001, a report of the Conference Proceedings on Evidence-Based Medicine in Respiratory Care was published.34 Evidence-based practice requires careful examination of the evidence for diagnosis, treatment, prognosis, and, in turn, practice using a formal set of rules.35 The best evidence is used for clinical decision making, which should lead to optimal respiratory care.35 Evidence-based practice has been advocated for all respiratory care delivered.
In 2002, the AARC, NBRC, and CoARC published their “Tripartite Statements of Support,” which suggested that all respiratory therapists seek and obtain the RRT credential.36 An AARC white paper followed in 2003, which encouraged the continuing development of baccalaureate and graduate education in respiratory care.37
Future of Respiratory Care
In 2001, Pierson, a prominent pulmonary physician and one of the many physician supporters of respiratory therapists, set out to describe the future of respiratory care.38 Among other responsibilities, Pierson predicted a much greater use of patient assessment and protocols in chronic disease state management in all clinical settings. He also envisioned a more active role for respiratory therapists in palliative and end-of-life care, increasing emphasis on smoking cessation and prevention, early detection, and intervention in chronic obstructive pulmonary disease (COPD). Pierson also predicted an increase in the use of respiratory therapists acting as coordinators and caregivers in home care.
2015 and Beyond
1. How will most patients receive health care services in the future?
2. How will respiratory care services be provided?
3. What new knowledge, skills, and attributes will respiratory therapists need to be able to provide care that is safe, efficacious, and cost-effective in 2015?
4. What education and credentialing systems will be needed to ensure respiratory therapists acquire the new knowledge, skills, and attributes?
5. How should the profession transition from traditional practice to the newer system without adversely impacting the existing workforce?39
• Eleven significant changes in how health care would be delivered (Box 1-2),
• Nine changes likely to occur in the U.S. health care workforce (Box 1-3), and
• Five expected changes in how respiratory care services would be provided (Box 1-4).40
In the words of one conference organizer, “the take home message was that indeed the scope and depth of respiratory care practice will increase by 2015.”39 The second conference was held in the spring of 2009 and built on the findings of the 2008 conference by identifying the competencies needed by graduate respiratory therapists and the educational content and curriculum that would be needed to practice in 2015 and beyond. Conference participants agreed that there would be seven major competencies (Box 1-5) that future respiratory therapists would need to practice effectively by 2015.40,41 The third conference was held in the summer of 2010 to determine how the educational programs for entry-level respiratory therapists would have to be structured to accomplish the seven major competencies identified during the 2009 conference. The recommendations of the third conference were published in 2011.42