76
Histiocytoses
Langerhans Cell Histiocytoses
• Langerhans cells have Birbeck granules by electron microscopy.
• Common in children ages 1–3 years, but can occur at any age.
• Traditionally classified into the following categories but they exist along a clinical spectrum.
Letterer–Siwe Disease (Multifocal, Multisystem)
• Multisystem involvement (skin, lung, liver, lymph nodes, bone, bone marrow).
• Classically in those <1–2 year(s) of age.
• Favors scalp, flexural neck, axilla, perineum, trunk (Fig. 76.1).
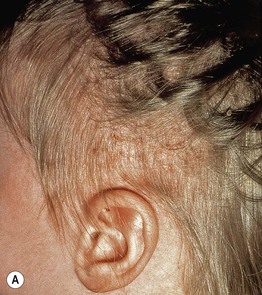





Fig. 76.1 Langerhans cell histiocytosis – clinical spectrum. A Scalp involvement may initially be diagnosed as seborrheic dermatitis; however, there are usually more discrete papules and crusting. B Pink, thin plaques with fissuring along the inguinal crease can also resemble seborrheic dermatitis. C Advanced disease with coalescence of papules into large plaques and prominent inguinal lymphadenopathy. D The presence of petechiae and purpuric papules is a clue to the diagnosis. E In an adult, the clinical presentation of inguinal involvement is similar to that of infants. F In patients with darkly pigmented skin, the papules can be hypopigmented. B, Courtesy, Richard Antaya, MD; D, F, Courtesy, Julie V. Schaffer, MD.
• Secondary changes include scale, crusts, petechiae/purpura.
Hand–Schüller–Christian Disease
Eosinophilic Granuloma (Unifocal)
• Localized variant (Fig. 76.2).

Fig. 76.2 Langerhans cell histiocytosis (eosinophilic granuloma of the bone). Radiography of the femur shows a large well-circumscribed osteolytic lesion. Courtesy, Edward McCarthy, MD.
• Classically in children, ages 7–12 years.
Hashimoto–Pritzker Disease (Congenital Self-Healing Reticulohistiocytosis)
• Limited to skin, rapidly self-healing.
• At birth or during first few days of life.
• Variable presentation from a single nodule to widespread red-brown papules/nodules that crust and involute after several weeks (Fig. 76.3).
Non-Langerhans Cell Histiocytoses
Juvenile Xanthogranuloma
• Most common of the non-Langerhans cell histiocytoses.
• Appears primarily in infants and children (75% present during the first year of life).
• Usually a single papule or nodule (Fig. 76.4).


Fig. 76.4 Juvenile xanthogranuloma. A Pink nodule with a few telangiectasias representing an early lesion. B Well-developed yellow-brown papulonodule on the chin, with the color reflecting the accumulation of lipid within histiocytes. Courtesy, Julie V. Schaffer, MD.
• Head/neck > trunk > upper extremities > lower extremities.
• Self-limiting; no treatment necessary.
• If multiple lesions, consider ophthalmologic examination for ocular involvement.
Benign Cephalic Histiocytosis
Generalized Eruptive Histiocytoma
Indeterminate Cell Histiocytosis
Necrobiotic Xanthogranuloma
• Rare, generally in adults >50 years of age.
• Firm, yellowish plaques or papulonodules; sometimes ulcerated.
• Classically periorbital (Fig. 76.8).

Fig. 76.8 Necrobiotic xanthogranuloma. Yellow-brown papules and plaques in a periorbital distribution in a patient with chronic lymphocytic leukemia. Such lesions may initially be mistaken for xanthelasma. Courtesy, Kalman Watsky, MD.
• Underlying plasma cell dyscrasia common; also increased risk of lymphoproliferative disorders.
Multicentric Reticulohistiocytosis/Giant Cell Reticulohistiocytoma
– A skin-colored to pink papulonodule often on the head.
– 50% with mucous membrane involvement.
– Up to one third of affected patients can have an associated malignancy.



Fig. 76.9 Multicentric reticulohistiocytosis. A Grouped firm pink papules on the dorsal surface of the fingers, hand, and wrist of a 73-year-old African-American woman. B Grouped pink papulonodules on the elbow in a second patient. C A more subtle presentation in a third patient, with small pink papules and thin plaques that favor the skin overlying the small joints of the hands; this is the form that can initially be confused with dermatomyositis. A, Courtesy, Susan D. Laman, MD; B, Courtesy, Jean L. Bolognia, MD; C, Courtesy, Kalman Watsky, MD.
Rosai–Dorfman Disease (Sinus Histiocytosis with Massive Lymphadenopathy)
Xanthoma Disseminatum
• Rare, generally before age 25 years.
• Symmetric eruption of tens to hundreds of yellow, red, or brown papules and plaques.
• Favors face and flexural areas, including major folds (Fig. 76.11).

Fig. 76.11 Xanthoma disseminatum. Symmetric involvement of the major flexures is a characteristic finding. Note the yellow discoloration of some of the coalescing papulonodules. Courtesy, David Wetter, MD.
• Rarely sclerosis (Fig. 76.12).

Fig. 76.12 Xanthoma disseminatum. Sclerotic form of xanthoma disseminatum in a patient who developed multiple myeloma.
• Mucous membrane involvement: oral, upper airway, ocular (may threaten vision).
Progressive Nodular Histiocytoma
Although we have made all these distinctions in the non-Langerhans cell histiocytoses, patients may have overlapping clinical and histopathologic features (including immunohistochemical staining). As a result, the evaluation of a patient with a non-Langerhans cell histiocytosis should include a total body skin examination and general physical examination, inclusive of eyes, mucosae, and lymph nodes. In addition, laboratory testing should include serum protein electrophoresis, immunofixation electrophoresis, and evaluation for diabetes insipidus.
For further information see Ch. 91. From Dermatology, Third Edition.












