Hip
The hip is the articulation between the large spherical head of the femur and the deep socket provided by the acetabulum of the pelvis (Figure 12-1). Because of the joints’ central location within the body, the logical question arises: do the hips serve as “base” joints for the lower extremities, or basilar joints for the entire superimposed pelvis and trunk? As this chapter unfolds, it will become clear that the hips serve both roles. For this reason the hips play a dominant kinesiologic role in movements across a large part of the body. Pathology or trauma affecting the hips typically causes a wide range of functional limitations, including difficulty in walking, dressing, driving a car, lifting and carrying loads, and climbing stairs.
OSTEOLOGY
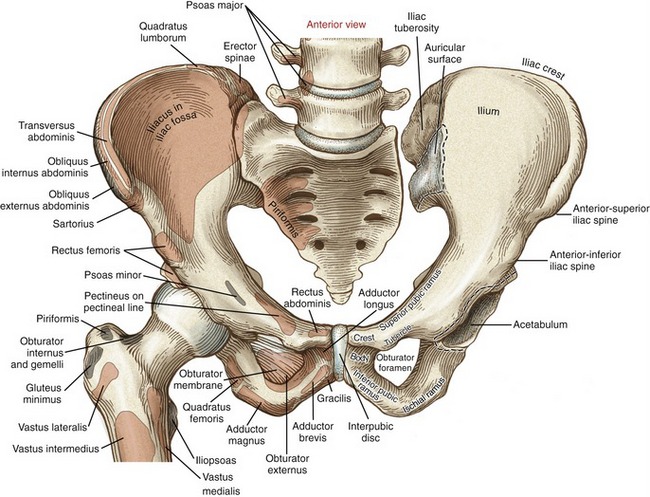
Each innominate (from the Latin innominatum, meaning nameless) is the union of three bones: the ilium, pubis, and ischium (see Figures 12-1 and 12-2). The right and left innominates connect with each other anteriorly at the pubic symphysis and posteriorly at the sacrum. These connections form a complete osteoligamentous ring, referred to as the pelvis (from the Latin, meaning basin or bowl). The pelvis is associated with three important and very different functions. First, the pelvis serves as a common attachment point for many large muscles of the lower extremity and the trunk. The pelvis also transmits the weight of the upper body and trunk either to the ischial tuberosities during sitting or to the lower extremities during standing and walking. Last, with the aid of the muscles and connective tissues of the pelvic floor, the pelvis supports the organs involved with bowel, bladder, and reproductive functions.
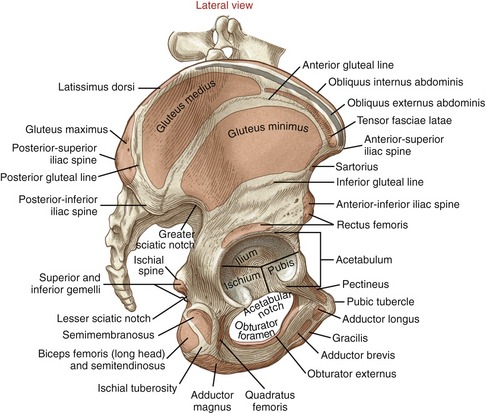
The external surface of the pelvis has three striking features. The large fan-shaped wing (or ala) of the ilium forms the superior half of the innominate. Just below the wing is the deep, cup-shaped acetabulum. Just inferior and slightly medial to the acetabulum is the obturator foramen—the largest foramen in the body. This foramen is covered by an obturator membrane (see Figure 12-1).
While a person stands, the pelvis is normally oriented so that when viewed laterally a vertical line passes between the anterior-superior iliac spine and the pubic tubercle (see Figure 12-2).
ILIUM
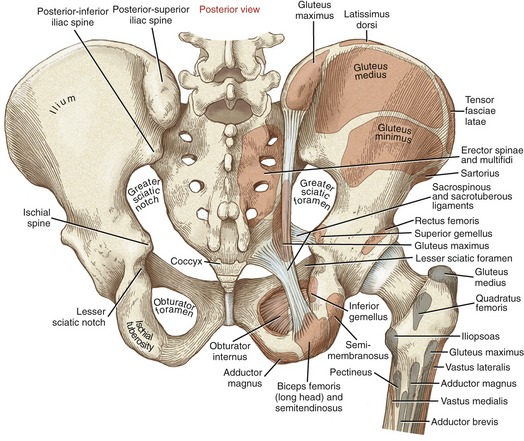
The external surface of the ilium is marked by rather faint posterior, anterior, and inferior gluteal lines (see Figure 12-2). These lines help to identify attachment sites of the gluteal muscles. At the most anterior extent of the ilium is the easily palpable anterior-superior iliac spine (see Figures 12-1 and 12-2). Below this spine is the anterior-inferior iliac spine. The prominent iliac crest, the most superior rim of the ilium, continues posteriorly and ends at the posterior-superior iliac spine (Figure 12-3). The soft tissue superficial to the posterior-superior iliac spine is often marked by a dimple in the skin. The less prominent posterior-inferior iliac spine marks the superior rim of the greater sciatic notch. The opening of this notch is converted to the greater sciatic foramen by the sacrotuberous and sacrospinous ligaments.
The internal aspect of the ilium has three notable features (see Figure 12-1). Anteriorly, the smooth concave iliac fossa is filled by the iliacus muscle. Posteriorly, the auricular surface articulates with the sacrum at the sacroiliac joint. Just posterior to the auricular surface is the large, rough iliac tuberosity, which marks the attachments of sacroiliac ligaments.
PUBIS
The superior pubic ramus extends anteriorly from the anterior wall of the acetabulum to the large flattened body of the pubis (see Figure 12-1). The upper border of the body of the pubis is the pubic crest, serving as an attachment for the rectus abdominus muscle. On the upper surface of the superior ramus is the pectineal line, marking the attachment of the pectineus muscle. The pubic tubercle projects anteriorly from the superior pubic ramus, serving as an attachment for the inguinal ligament. The inferior pubic ramus extends from the body of the pubis posteriorly to the junction of the ischium.
The two pubic bones articulate in the midline by way of the pubic symphysis joint (see Figure 12-1). This relatively immobile joint is typically classified as a synarthrosis. Hyaline cartilage lines the opposing surfaces of the articulation; the surfaces are not completely flat but possess small raised ridges, likely designed to resist shear.160 The joint is firmly bound by a fibrocartilaginous interpubic disc and ligaments. The interpubic disc is strengthened by an interlacing of collagen fibers, combined with distal attachments made by the rectus abdominis muscles.160 Up to 2 mm of translation and very slight rotation occur at the pubic symphysis joint.168 The pubic symphysis provides stress relief throughout the anterior ring of the pelvis during walking and, in women, during childbirth.
Symphysis pubis dysfunction can occur in some women during pregnancy or just after birth. This painful condition is associated with increased instability in the symphysis pubis caused by the physiologic relaxation of the joint’s supporting ligaments.89
ISCHIUM
The sharp ischial spine projects from the posterior side of the ischium, just inferior to the greater sciatic notch (see Figure 12-3). The lesser sciatic notch is located just inferior to the spine. The sacrotuberous and sacrospinous ligaments convert the lesser sciatic notch into a lesser sciatic foramen.
Projecting posteriorly and inferiorly from the acetabulum is the large, stout ischial tuberosity (see Figure 12-3). This palpable structure serves as the proximal attachment for many muscles of the lower extremity, most notably the hamstrings and part of the adductor magnus. The ischial ramus extends anteriorly from the ischial tuberosity, ending at the junction with the inferior pubic ramus (see Figure 12-1).
ACETABULUM
Located just above the obturator foramen is the large cup-shaped acetabulum (see Figure 12-2). The acetabulum forms the socket of the hip. All three bones of the pelvis contribute to the formation of the acetabulum: the ilium and ischium contribute about 75%, and the pubis contributes the remaining approximately 25%. The specific features of the acetabulum are discussed in the section on arthrology.
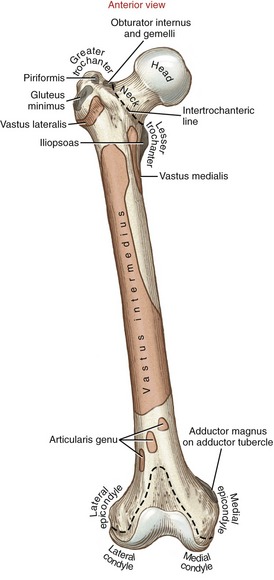
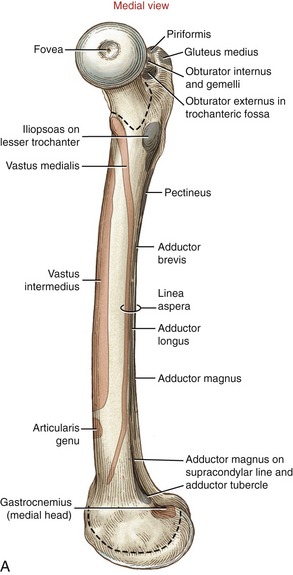
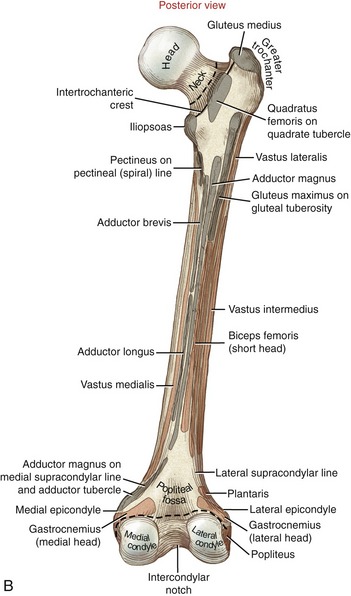
Femur
The femur is the longest and strongest bone of the human body (Figure 12-4). Its shape and robust stature reflect the powerful action of muscles and contribute to the long stride length during walking. At its proximal end, the femoral head projects medially and slightly anteriorly for an articulation with the acetabulum. The femoral neck connects the femoral head to the shaft. The neck serves to displace the proximal shaft of the femur laterally away from the joint, thereby reducing the likelihood of bony impingement against the pelvis. Distal to the neck, the shaft of the femur courses slightly medially, effectively placing the knees and feet closer to the midline of the body.
The shaft of the femur displays a slight anterior convexity (Figure 12-5, A). As a long, eccentrically loaded column, the femur bows very slightly when subjected to the weight of the body. Consequently, stress along the bone is dissipated through compression along its posterior shaft and through tension along its anterior shaft. Ultimately this bowing allows the femur to bear a greater load than if the femur were perfectly straight.
Anteriorly, the intertrochanteric line marks the distal attachment of the capsular ligaments (see Figure 12-4). The greater trochanter extends laterally and posteriorly from the junction of the femoral neck and shaft (see Figure 12-5, B). This prominent and easily palpable structure serves as the distal attachment for many muscles. On the medial surface of the greater trochanter is a small pit called the trochanteric fossa (see Figures 12-5, A and 12-6). This fossa marks the distal attachment of the obturator externus muscle.
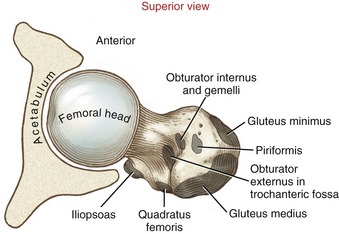
FIGURE 12-6. The superior aspect of the right femur. Distal attachments of muscles are shown in gray.
Posteriorly, the femoral neck joins the femoral shaft at the raised intertrochanteric crest (see Figure 12-5, B). The quadrate tubercle, the distal attachment of the quadratus femoris muscle, is a slightly raised area on the crest just inferior to the trochanteric fossa. The lesser trochanter projects sharply from the inferior end of the crest in a posterior-medial direction. The lesser trochanter serves as the distal attachment for the iliopsoas muscle, an important hip flexor and vertical stabilizer of the lumbar spine.
The middle third of the posterior side of the femoral shaft is clearly marked by a vertical ridge called the linea aspera (Latin words linea, line + aspera, rough). This raised line serves as an attachment site for the vasti muscles of the quadriceps group, many of the adductor muscles, and the intermuscular fascia of the thigh. Proximally, the linea aspera splits into the pectineal (spiral) line medially and the gluteal tuberosity laterally (see Figure 12-5, B). At the distal end of the femur, the linea aspera divides into the lateral and medial supracondylar lines. The adductor tubercle is located at the extreme distal end of the medial supracondylar line.
SHAPE OF THE PROXIMAL FEMUR
The ultimate shape and configuration of the developing proximal femur are determined by several factors, including differential growth of the bone’s ossification centers, the force of muscle activation and weight bearing, and circulation.171 Abnormal growth and development resulting in a misshaped proximal femur is referred to generically as femoral dysplasia (from the Greek dys, ill or bad, + plasia, growth). Trauma or other acquired factors can also affect the shape of the proximal femur. The shape and configuration of the proximal femur have important implications on the congruity and stability of the joint, as well as the stress placed on the joint structures. This topic will be revisited throughout this chapter.
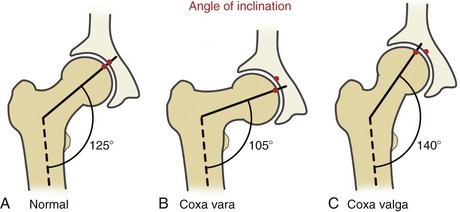
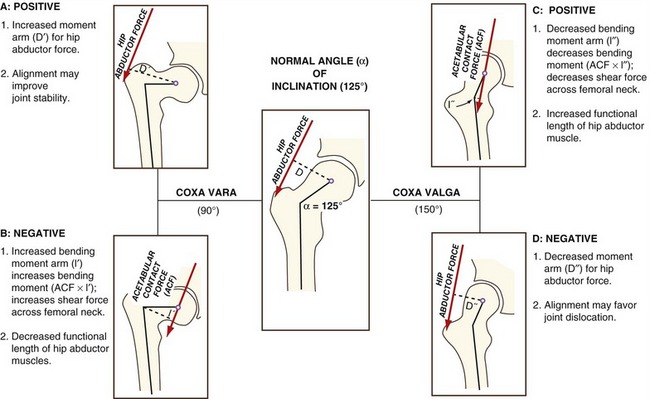
Angle of Inclination: The angle of inclination of the proximal femur describes the angle within the frontal plane between the femoral neck and the medial side of the femoral shaft (Figure 12-7). At birth this angle measures about 140 to 150 degrees. Primarily because of the loading across the femoral neck during walking, this angle usually reduces to its normal adulthood value of about 125 degrees.16,132 As depicted by the pair of red dots in Figure 12-7, this angle optimizes the alignment of the joint surfaces.
A change in the normal angle of inclination is referred to as either coxa vara or coxa valga. Coxa vara (Latin coxa, hip, + vara, to bend inward) describes an angle of inclination markedly less than 125 degrees; coxa valga (Latin valga, to bend outward) describes an angle of inclination markedly greater than 125 degrees (see Figure 12-7, B and C). These abnormal angles can significantly alter the articulation between the femoral head and the acetabulum, thereby affecting hip biomechanics. Severe malalignment may lead to dislocation or stress-induced degeneration of the joint.
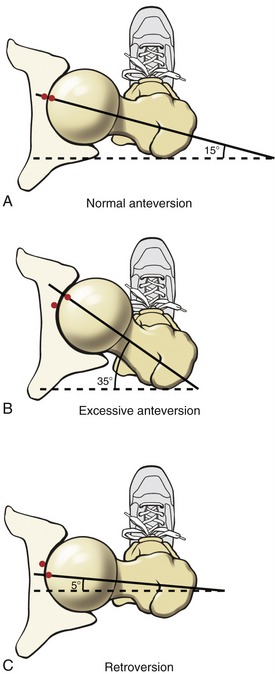
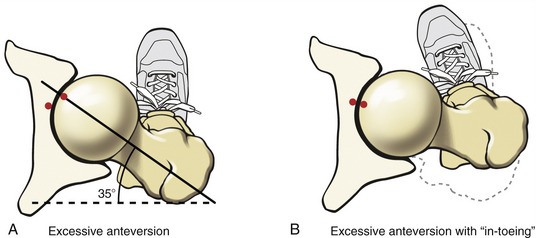
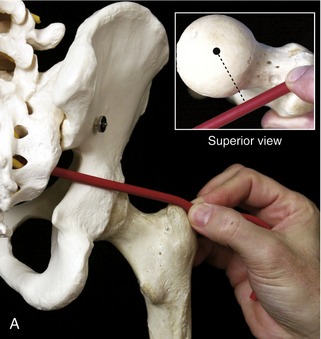
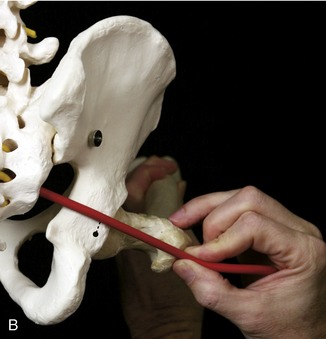
Femoral Torsion: Femoral torsion describes the relative rotation (twist) between the bone’s shaft and neck. Normally, as viewed from above, the femoral neck projects about 15 degrees anterior to a medial-lateral axis through the femoral condyles.43 This degree of torsion is called normal anteversion (Figure 12-8, A). In conjunction with the normal angle of inclination, an approximate 15-degree angle of anteversion affords optimal alignment and joint congruence (see alignment of red dots in Figure 12-8, A).
Femoral torsion that is markedly different from 15 degrees is considered abnormal. Torsion significantly greater than 15 degrees is called excessive anteversion (see Figure 12-8, B). In contrast, torsion significantly less than 15 degrees (i.e., approaching 0 degrees) is called retroversion (see Figure 12-8, C).
Typically a healthy infant is born with about 40 degrees of femoral anteversion.43 With continued bone growth, increased weight bearing, and muscle activity, this angle usually decreases to about 15 degrees by 16 years of age. Excessive anteversion that persists into adulthood can increase the likelihood of hip dislocation, articular incongruence, increased joint contact force, and increased wear on the articular cartilage.57 These factors may lead to secondary osteoarthritis of the hip.147
Excessive anteversion in children may be associated with an abnormal gait pattern called “in-toeing.” In-toeing is a walking pattern with exaggerated posturing of hip internal rotation. The amount of in-toeing is generally related to the amount of femoral anteversion. This gait pattern apparently is a compensatory mechanism used to guide the excessively anteverted femoral head more directly into the acetabulum (Figure 12-9). In addition, Arnold and colleagues have shown that the exaggerated internally rotated position during walking serves to increase the moment arm of the important hip abductor muscles—leverage that is substantially reduced with excessive femoral anteversion.9 Regardless of the reason for the internal rotated position, children may, over time, develop shortening of the internal rotator muscles and various ligaments, thereby reducing external rotation range of motion. Fortunately, most children with in-toeing eventually walk normally.163 The gait pattern typically improves with time because of a natural normalization of the anteversion or a combined structural compensation in other parts of the lower extremity, most commonly the tibia.60 There is no evidence that nonoperative treatment can reduce excessive femoral anteversion.
Excessive femoral anteversion of 25 to 45 degrees is common in persons with cerebral palsy, and even anteversion as high as 60 to 80 degrees has been reported.8,16 In-toeing typically persists in children with cerebral palsy who are ambulatory and usually does not resolve.149
INTERNAL STRUCTURE OF THE PROXIMAL FEMUR
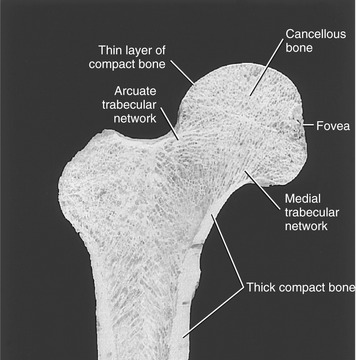
Compact and Cancellous Bone: Walking produces tension, compression, bending, shear, and torsion on the proximal femur. Many of these forces are large, exceeding one’s body weight. Throughout a lifetime, the proximal femur typically resists and absorbs these repetitive forces without incurring injury. This is accomplished by two strikingly different compositions of bone. Compact bone is very dense and unyielding, with an ability to withstand large loads. This type of bone is particularly thick in the cortex, or outer shell, of the lower femoral neck and entire shaft (Figure 12-10). These regions are subjected to large shear and torsion forces. Cancellous bone, in contrast, is relatively porous, consisting of a spongy, three-dimensional trabecular lattice, as shown in Figure 12-10. The relative elasticity of cancellous bone is ideal for repeatedly absorbing external forces. Cancellous bone tends to concentrate along lines of stress, forming trabecular networks. A medial trabecular and an arcuate trabecular network are visible within the femur shown in Figure 12-10. The overall pattern of the trabecular network changes when the proximal femur is subjected to abnormal forces over an extended time.
ARTHROLOGY
Functional Anatomy of the Hip Joint
FEMORAL HEAD
The femoral head is located just inferior to the middle one third of the inguinal ligament. On average, the centers of the two adult femoral heads are 17.5 cm (6.9 inches) apart from each other.127 The head of the femur forms about two thirds of a nearly perfect sphere (Figure 12-11). Located slightly posterior to the center of the head is a prominent pit, or fovea (see Figure 12-5, A). The entire surface of the femoral head is covered by articular cartilage, except for the region of the fovea. The cartilage is thickest (about 3.5 mm) in a broad region above and slightly anterior to the fovea (see highlighted region in Figure 12-11).86
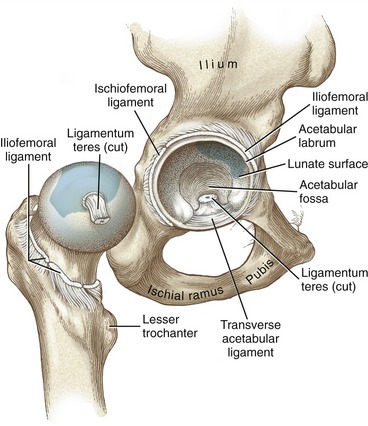
The ligamentum teres (also known as the ligament to the head of the femur) is a tubular sheath of synovial-lined connective tissue that runs between the transverse acetabular ligament and the fovea of the femoral head (see Figure 12-11). Although the ligament is stretched during flexion and adduction, it likely contributes only a small amount of stability to the articulation.160 Interestingly, the ligament functions primarily as a protective conduit, or sheath, for the passage of the small acetabular artery (a branch from the obturator artery) to the femoral head. The small and inconstant acetabular artery provides only a minor source of blood to the femur.28,160 The primary blood supply to the head and neck of the femur is through the medial and lateral circumflex arteries, which pierce the capsule of the joint adjacent to the femoral neck.
ACETABULUM
The acetabulum (from Latin, meaning “vinegar cup”) is a deep, hemispheric cuplike socket that accepts the femoral head. About 60 to 70 degrees of the rim of the acetabulum are incomplete near its inferior pole, creating the acetabular notch (see Figure 12-2).
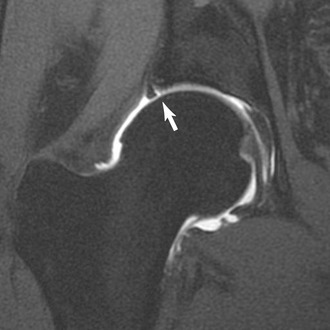
The femoral head contacts the acetabulum only along its horseshoe-shaped lunate surface (see Figure 12-11). This surface is covered with articular cartilage, thickest along the superior-anterior region of its dome.38,86 The region of thickest cartilage (about 3.5 mm) corresponds to approximately the same region of highest joint force during walking.31 During walking, hip forces fluctuate from 13% of body weight during mid-swing phase to over 300% of body weight during the mid-stance phase. During the stance phase—when forces are the greatest—the lunate surface flattens slightly as the acetabular notch widens slightly, thereby increasing contact area as a means to reduce peak pressure (Figure 12-12).38,101 This natural dampening mechanism represents yet another design that strives to keep the stress on the subchondral bone within physiologic tolerable levels.
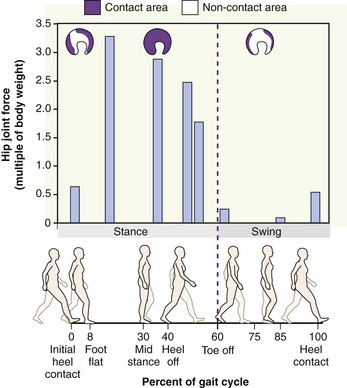
FIGURE 12-12. Graph shows a computer model’s estimate of the hip joint compression force as a multiple of body weight during the gait cycle. The stance phase is between 0% and 60% of the gait cycle, and the swing phase is between 60% and 100% of the gait cycle (vertical stippled line separates these major divisions of the gait cycle). The images above the graph indicate the approximate area of acetabular contact at three selected magnitudes of hip joint force, estimated by data published in the literature.38 The area of joint contact increases from about 20% of the lunate surface during the swing phase to about 98% during mid stance phase.
ACETABULAR LABRUM
The acetabular labrum is a flexible ring of primary fibrocartilage that surrounds the outer circumference (rim) of the acetabulum (see Figure 12-11).142 Adjacent to the acetabular notch, the labrum widens as it is transformed into the transverse acetabular ligament.160
The acetabular labrum is nearly triangular in cross-section, with its apex projecting outward about 5 mm toward the femoral head.164 The base of the labrum attaches along the internal and external surfaces of the acetabulum rim. The part of the labrum that attaches to the internal surface gradually fuses with the articular cartilage within the acetabulum.
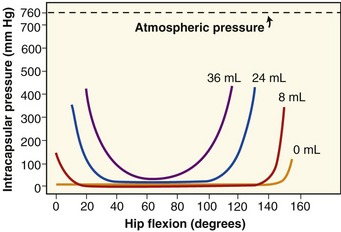
The acetabular labrum provides significant stability to the hip by “gripping” the femoral head and by deepening the volume of the socket by approximately 30%.164 The seal formed around the joint by the labrum helps maintain a negative intra-articular pressure, thereby creating a modest suction that resists distraction of the joint surfaces. The circumferential seal also holds the synovial fluid within the joint; therefore the labrum indirectly enhances the lubrication and load dissipation functions of the articular cartilage.44 The labrum directly protects the articular cartilage by reducing contact stress (force/area) by increasing the surface area of the acetabulum.164
Consisting primarily of fibrocartilage, the labrum is poorly vascularized, receiving only modest blood supply to its outer one third.109,142 For this reason, a torn labrum has a very limited ability to heal. In contrast to its poor vascularization, the labrum is well supplied by afferent nerves capable of providing proprioceptive feedback and, when the labrum is acutely injured, the sensation of pain.82
ACETABULAR ALIGNMENT
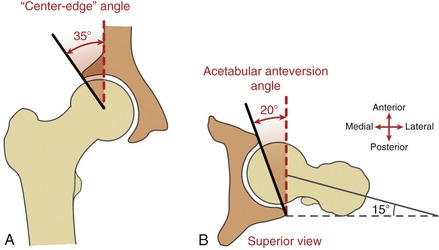
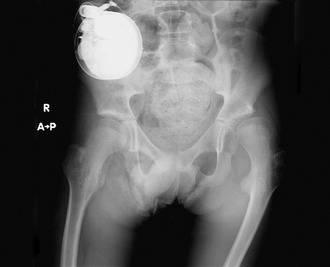
Center-Edge Angle: The center-edge angle is highly variable but on average measures about 35 degrees in radiographs from adults (Figure 12-13, A).4,50 As described in the legend of Figure 12-13, a significantly lower central-edge angle reduces the acetabular coverage of the femoral head. This reduced coverage increases the risk of dislocation and, equally important, reduces the contact area within the joint.108 A central-edge angle of only 15 degrees, for example, reduces normal contact area by as much as 35%.50 During the single-limb–support phase of walking, for instance, this reduced surface area would theoretically increase joint pressure (force/area) by about 50%. Over many years of walking, this scenario may lead to premature hip osteoarthritis, often starting with degeneration of the acetabular labrum.26,94,111
Acetabular Anteversion Angle: The acetabular anteversion angle measures the extent to which the acetabulum projects anteriorly within the horizontal plane, relative to the pelvis. Such a perspective can be measured through computed tomography. Observed from above, the acetabular anteversion angle is normally about 20 degrees (Figure 12-13, B).4,148 Even when normal, this orientation exposes part of the anterior side of the femoral head. The thick anterior capsular ligament of the hip and the iliopsoas tendon naturally cover and support this vulnerable side of the joint. A hip demonstrating excessive acetabular anteversion is more exposed anteriorly: when anteversion is severe, the hip is more prone to anterior dislocation and associated lesions of the anterior labrum, especially at the extremes of external rotation. The likelihood of these associated pathologies increases when acetabular anteversion is combined with excessive femoral anteversion.95
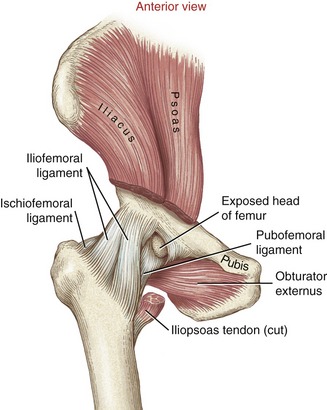
CAPSULE AND LIGAMENTS OF THE HIP
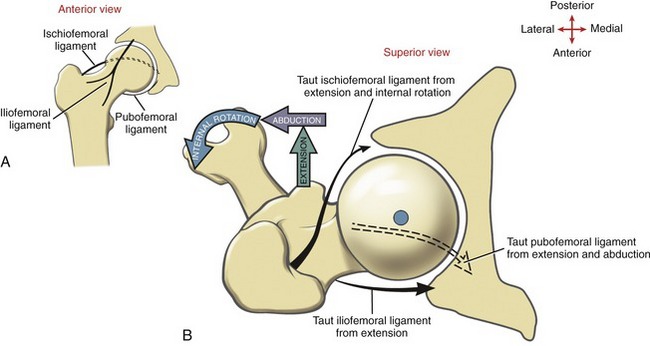
A synovial membrane lines the internal surface of the hip joint capsule. The iliofemoral, pubofemoral, and ischiofemoral ligaments reinforce the external surface of the capsule (Figures 12-14 and 12-15). Passive tension in stretched ligaments, the adjacent capsule, and the surrounding muscles help define the end-range of movements of the hip (Table 12-1).47 Increasing the flexibility in various parts of the capsule is an important component of manual physical therapy for restricted motion of the hip.66,103
TABLE 12-1.
Connective Tissues and Selected Muscles That Become Taut at the End-Ranges of Passive Hip Motion
| End-Range Position | Taut Tissue |
| Hip flexion (knee extended) | Hamstrings |
| Hip flexion (knee flexed) | Inferior and posterior capsule; gluteus maximus |
| Hip extension (knee extended) | Primarily iliofemoral ligament, some fibers of the pubofemoral and ischiofemoral ligaments; psoas major |
| Hip extension (knee flexed) | Rectus femoris |
| Abduction | Pubofemoral ligament; adductor muscles |
| Adduction | Superior fibers of ischiofemoral ligament; iliotibial band; and abductor muscles such as the tensor fasciae latae and gluteus medius |
| Internal rotation | Ischiofemoral ligament; external rotator muscles, such as the piriformis or gluteus maximus |
| External rotation | Iliofemoral and pubofemoral ligaments; internal rotator muscles, such as the tensor fasciae latae or gluteus minimus |
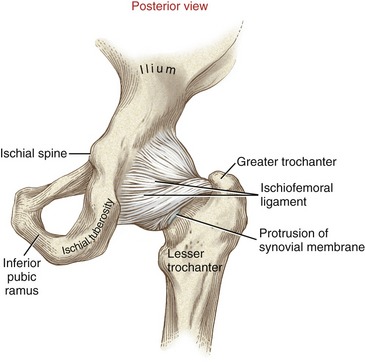
FIGURE 12-15. The posterior capsule and ligaments of the right hip.
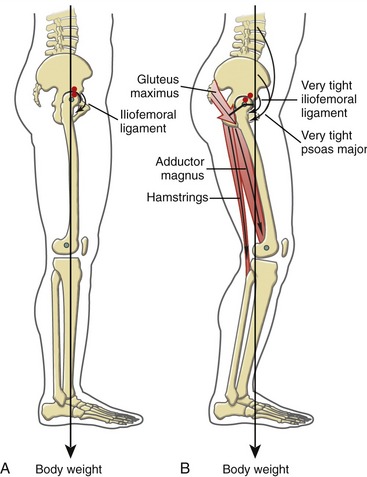
The iliofemoral ligament (or Y-ligament) is a thick and strong sheet of connective tissue, resembling an inverted Y. Proximally, the iliofemoral ligament attaches near the anterior-inferior iliac spine and along the adjacent margin of the acetabulum. Fibers form distinct medial and lateral fasciculi, each attaching to either end of the intertrochanteric line of the femur (see Figure 12-14). Full hip extension stretches the iliofemoral ligament and anterior capsule. Full external rotation also elongates fibers of the iliofemoral ligament, especially those within the lateral fasciculus.47,106
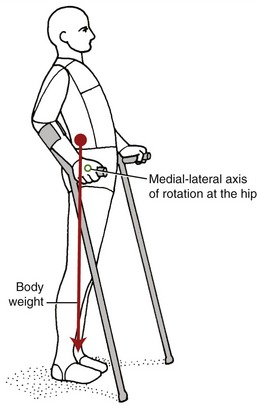
The iliofemoral ligament is the strongest and stiffest ligament of the hip.61,162 The mean maximal force required to disrupt either fasciculus is approximately 330 N (75 lb).61 When a person stands with the hip fully extended, the anterior surface of the femoral head presses firmly against the iliofemoral ligament and superimposed iliopsoas muscle.181 From a position of standing, passive tension in these structures forms an important stabilizing force that resists further hip extension. Persons with paraplegia often rely on the passive tension in an elongated and taut iliofemoral ligament to assist with standing (Figure 12-16).
Although thinner and more circular than the fibers of the iliofemoral ligament, the pubofemoral and ischiofemoral ligaments blend with and strengthen adjacent aspects of the capsule. The pubofemoral ligament attaches along the anterior and inferior rim of the acetabulum and adjacent parts of the superior pubic ramus and obturator membrane (see Figure 12-14). The fibers blend with the medial fasciculus of the iliofemoral ligament, becoming taut in hip abduction and extension and, to a lesser degree, external rotation.106
The ischiofemoral ligament attaches from the posterior and inferior aspects of the acetabulum, primarily from the adjacent ischium (see Figure 12-15). Fibers from this ligament join circular fibers located deeper within the posterior and inferior capsule. Other more superficial fibers spiral superiorly and laterally across the posterior neck of the femur to attach near the apex of the greater trochanter (see Figure 12-14). These superficial fibers become taut in full internal rotation and extension106; other more superior fibers become taut in full adduction.
Close-Packed Position of the Hip: Full extension of the hip (i.e., about 20 degrees beyond the neutral position) in conjunction with slight internal rotation and slight abduction twists or “spirals” most of the fibers within the capsular ligaments to their most taut position (Figure 12-17). This position is useful therapeutically during attempts to stretch the entirety of the hip’s capsular ligaments. Because the position of full extension, slight internal rotation and abduction elongates most of the capsule, it is considered the close-packed position at the hip.160 The passive tension generated especially by full extension lends stability to the joint and reduces passive accessory movement or “joint play.” The hip is one of a very few joints in the body in which the close-packed position is not also associated with the position of maximal joint congruency. The hip joint surfaces fit most congruently in about 90 degrees of flexion with moderate abduction and external rotation. In this position, most of the capsule and associated ligaments have “unraveled” to a more slackened state, adding only little passive tension to the joint.
Osteokinematics
This section describes the range of motion allowed by the adult hip, including the factors that permit and restrict this motion. Reduced hip motion may be an early indicator of disease or trauma, either at the hip or elsewhere in the body.41 Limited hip motion can impose significant functional limitations in activities such as walking, standing upright comfortably, or picking up objects off the floor.
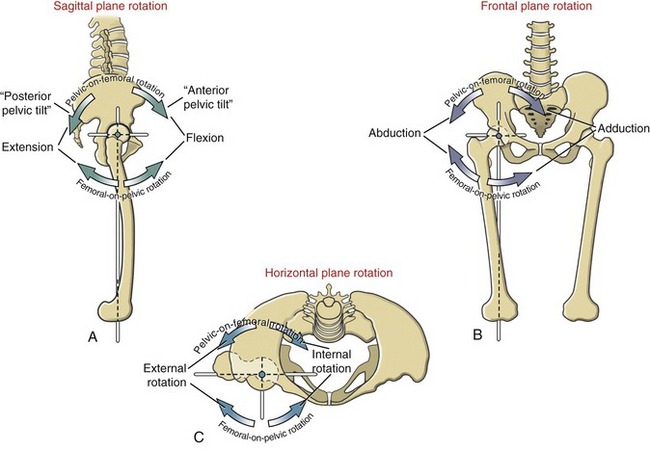
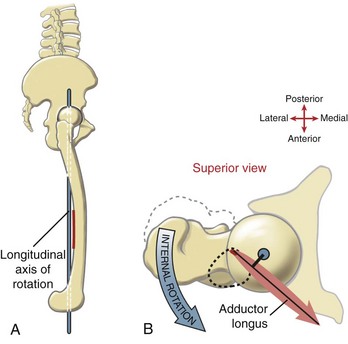
Two terms are used to describe the kinematics at the hip. Femoral-on-pelvic hip osteokinematics describes the rotation of the femur about a relatively fixed pelvis. Pelvic-on-femoral hip osteokinematics, in contrast, describes the rotation of the pelvis, and often the superimposed trunk, over relatively fixed femurs. Regardless of whether the femur or the pelvis is the moving segment, the osteokinematics are described from the anatomic position. The names of the movements are as follows: flexion and extension in the sagittal plane, abduction and adduction in the frontal plane, and internal and external rotation in the horizontal plane (Figure 12-19).
As depicted in Figure 12-19, each plane of motion is associated with a unique axis of rotation. The axis of rotation for internal and external rotation is often referred to as a “longitudinal” or vertical axis. (The vertical description assumes the subject is standing with the hip in the anatomic position.) This longitudinal axis of rotation extends as a straight line between the center of the femoral head and the center of the knee joint. Because of the angle of inclination of the proximal femur and the anterior bowing of the femoral shaft, most of the longitudinal axis of rotation lies outside the femur itself (see Figure 12-19, A and B). The extramedullary axis has implications on some of the actions of hip muscles, a point discussed later in this chapter.
Unless otherwise specified, the following discussions include passive ranges of motion. The connective tissues and selected muscles that limit motion are also described and are summarized in Table 12-1. The muscles used to produce and control hip motion are discussed later in this chapter. Although femoral-on-pelvic and pelvic-on-femoral movements often occur simultaneously, they are presented here separately.
FEMORAL-ON-PELVIC OSTEOKINEMATICS
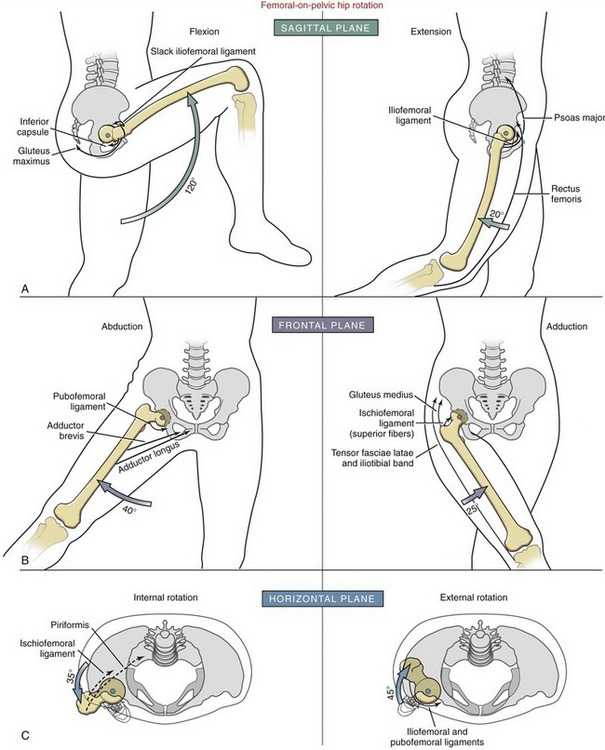
Rotation of the Femur in the Sagittal Plane: On average, with the knee flexed, the hip flexes to about 120 degrees (Figure 12-20, A).41,150 Tasks such as comfortably squatting or tying a shoelace typically require this amount of hip flexion.77 Full hip flexion slackens the three primary capsular ligaments but stretches the inferior capsule and muscles such as the gluteus maximus. With the knee fully extended, hip flexion is typically limited to 70 to 80 degrees by increased tension in the hamstring muscles. Considerable variability can be expected in this movement because of high inter-subject variability in hamstring muscle flexibility.
The hip normally extends about 20 degrees beyond the neutral position.150 Full hip extension increases the passive tension throughout the capsular ligaments—especially the iliofemoral ligament and the hip flexor muscles. When the knee is fully flexed during hip extension, passive tension in the stretched rectus femoris, which crosses both the hip and the knee, reduces hip extension to about the neutral position.
Rotation of the Femur in the Frontal Plane: The hip abducts on average about 40 degrees, limited primarily by the pubofemoral ligament and the adductor muscles (see Figure 12-20, B).150 The hip adducts about 25 degrees beyond the neutral position.17 In addition to interference with the contralateral limb, passive tension in stretched hip abductor muscles, iliotibial band, and superior fibers of the ischiofemoral ligament limits full adduction.
Rotation of the Femur in the Horizontal Plane: The magnitude of internal and external rotation of the hip is particularly variable among subjects. On average, the hip internally rotates about 35 degrees from the neutral position (see Figure 12-20, C).150,156 With the hip in extension, maximal internal rotation elongates the external rotator muscles, such as the piriformis, and parts of the ischiofemoral ligament.
PELVIC-ON-FEMORAL OSTEOKINEMATICS
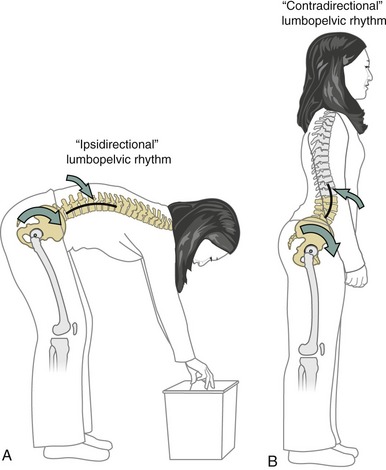
Lumbopelvic Rhythm: The caudal end of the axial skeleton is firmly attached to the pelvis by way of the sacroiliac joints. As a consequence, rotation of the pelvis over the femoral heads typically changes the configuration of the lumbar spine. This important kinematic relationship is known as lumbopelvic rhythm, introduced in Chapter 9. This concept is revisited in this chapter with a focus on the kinesiology at the hip.
Figure 12-21 shows two contrasting types of lumbopelvic rhythms frequently used during pelvic-on-femoral (hip) flexion. Although the kinematics depicted are limited to the sagittal plane, the concepts can also be applied to pelvic rotations in frontal and horizontal planes. Figure 12-21, A shows an example of an ipsidirectional lumbopelvic rhythm, in which the pelvis and lumbar spine rotate in the same direction.90 The effect of this movement is to maximize the angular displacement of the entire trunk relative to the lower extremities—an effective strategy for increasing reach of the upper extremities. The kinematics of the ipsidirectional lumbopelvic rhythm are discussed in detail in Chapter 9. In contrast, during contradirectional lumbopelvic rhythm, the pelvis rotates in one direction while the lumbar spine simultaneously rotates in the opposite direction (see Figure 12-21, B). The important consequence of this movement is that the supralumbar trunk (i.e., that part of the body located above the first lumbar vertebra) can remain nearly stationary as the pelvis rotates over the femurs. This type of rhythm is used during walking, for example, when the position of the supralumbar trunk—including the head and eyes—needs to be held relatively fixed in space, independent of the rotation of the pelvis. In this manner the lumbar spine functions as a mechanical “decoupler,” allowing the pelvis and the supralumbar trunk to move independently.152 A person with a fused lumbar spine, therefore, is unable to rotate the pelvis about the hips without a similar rotation of parts of the supralumbar trunk. This abnormal situation is readily apparent when the individual walks.
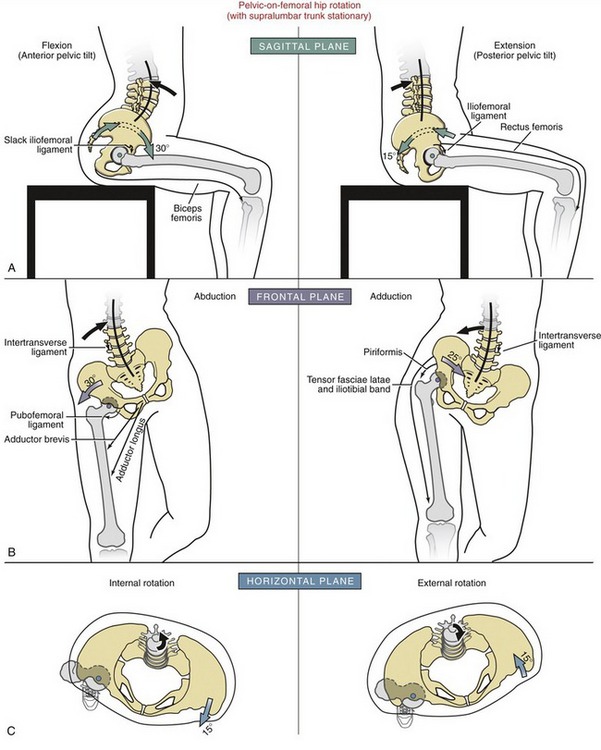
Figure 12-22 shows pelvic-on-femoral osteokinematics at the hip, organized by plane of motion. These kinematics are all based on the contradirectional lumbopelvic rhythm. In many cases the amount of pelvic-on-femoral rotation is restricted by natural limitations of movement within the lumbar spine.
Pelvic Rotation in the Sagittal Plane: Anterior and Posterior Pelvic Tilting: Hip flexion can occur through an anterior pelvic tilt (see Figure 12-22, A). As defined in Chapter 9, a “pelvic tilt” is a short-arc, sagittal plane rotation of the pelvis relative to stationary femurs. The direction of the tilt—either anterior or posterior—is based on the direction of rotation of a point on the iliac crest. The anterior tilt of the pelvis occurs about a medial-lateral axis of rotation through both femoral heads. The associated increased lumbar lordosis offsets most of the tendency of the supralumbar trunk to follow the forward rotation of the pelvis. While sitting with 90 degrees of hip flexion, the normal adult can perform about 30 degrees of additional pelvic-on-femoral hip flexion before being restricted by a completely extended lumbar spine. Full anterior tilt of the pelvis slackens most of the ligaments of the hip, most notably the iliofemoral ligament. Marked tightness in any hip extensor muscle—such as the hamstrings—could theoretically limit the extremes of an anterior pelvic tilt. As depicted in Figure 12-22, A, however, because the knees are flexed, the partially slackened hamstring muscles would not normally produce any noticeable resistance to an anterior pelvic rotation. During standing (and with knees fully extended), however, the more elongated hamstrings are more likely to resist an anterior pelvic tilt, but the amount of resistance is usually insignificant unless the muscle is physiologically impaired and generating extreme resistance to elongation.97
As depicted in Figure 12-22, A, the hips can be extended about 10 to 20 degrees from the 90-degree sitting posture via a posterior tilt of the pelvis. During sitting, this short-arc pelvic rotation would increase the length (and therefore tension) only minimally in the iliofemoral ligament and rectus femoris muscle. As depicted in the figure, the lumbar spine flexes, or flattens, as the pelvis posteriorly tilts.
Pelvic Rotation in the Frontal Plane: Pelvic-on-femoral rotation in the frontal and horizontal planes is best described assuming a person is standing on one limb. The weight-bearing extremity is referred to as the support hip.
Abduction of the support hip occurs by raising or “hiking” the iliac crest on the side of the nonsupport hip (see Figure 12-22, B). Assuming that the supralumbar trunk remains nearly stationary, the lumbar spine must bend in the direction opposite the rotating pelvis. A slight lateral convexity occurs within the lumbar region toward the side of the abducting hip.
Pelvic Rotation in the Horizontal Plane: Pelvic-on-femoral rotation occurs in the horizontal plane about a longitudinal axis of rotation (see green circle at femoral head in Figure 12-22, C). Internal rotation of the support hip occurs as the iliac crest on the side of the nonsupport hip rotates forward in the horizontal plane. During external rotation, in contrast, the iliac crest on the side of the nonsupport hip rotates backward in the horizontal plane. If the pelvis is rotating beneath a relatively stationary trunk, the lumbar spine must rotate (or twist) in the opposite direction as the rotating pelvis. The small amount of axial rotation normally permitted in the lumbar spine significantly limits the full expression of horizontal plane rotation of the support hip. The full potential of pelvic-on-femoral rotation requires that the lumbar spine and trunk follow the rotation of the pelvis—a movement strategy more consistent with an ipsidirectional lumbopelvic rhythm.
Arthrokinematics
During hip motion, the nearly spherical femoral head normally remains snugly seated within the confines of the acetabulum. The steep walls of the acetabulum, in conjunction with the tightly fitting acetabular labrum, limit significant translation between the joint surfaces. Hip arthrokinematics are based on the traditional convex-on-concave or concave-on-convex principles (see Chapter 1).
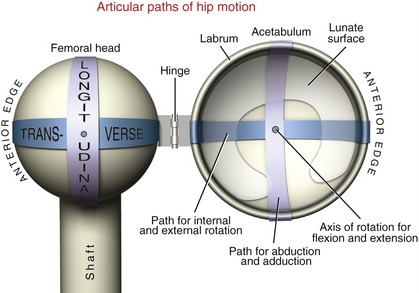
Figure 12-23 shows a highly mechanical illustration of a hip opened to enable visualization of the paths of articular motion. Abduction and adduction occur across the longitudinal diameter of the joint surfaces. With the hip extended, internal and external rotation occur across the transverse diameter of the joint surfaces. Flexion and extension occur as a spin between the femoral head and the lunate surfaces of the acetabulum. The axis of rotation for this spin passes through the femoral head.
MUSCLE AND JOINT INTERACTION
Innervation of the Muscles and Joint
INNERVATION OF MUSCLES
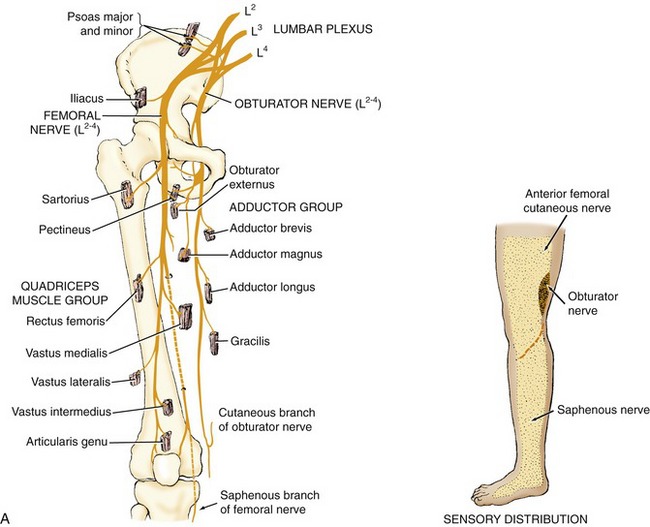
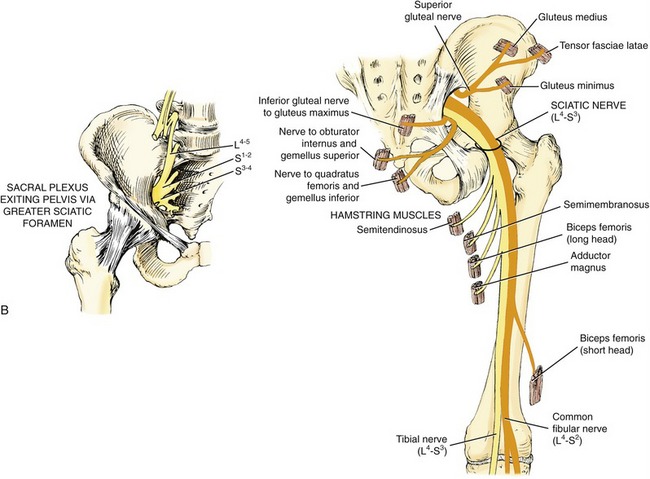
Lumbar Plexus: The lumbar plexus is formed from the ventral rami of spinal nerve roots T12-L4. This plexus gives rise to the femoral and obturator nerves (Figure 12-24, A). The femoral nerve, the largest branch of the lumbar plexus, is formed by L2-L4 nerve roots. Motor branches innervate most hip flexors and all knee extensors. Within the pelvis, proximal to the inguinal ligament, the femoral nerve innervates the psoas major and iliacus. Distal to the inguinal ligament, the femoral nerve innervates the sartorius, part of the pectineus, and the quadriceps muscle group. The femoral nerve has an extensive sensory distribution covering much of the skin of the anterior-medial aspect of the thigh. The sensory branches of the femoral nerve innervate the skin of the anterior-medial aspect of the lower leg, via the saphenous cutaneous nerve.
Sacral Plexus: The sacral plexus, located on the posterior wall of the pelvis, is formed from the ventral rami of L4-S4 spinal nerve roots. Most nerves from the sacral plexus exit the pelvis via the greater sciatic foramen to innervate the posterior hip muscles (see Figure 12-24, B).
As a reference, the primary spinal nerve roots that supply the muscles of the lower extremity are listed in Appendix IV, Part A. In addition, Appendix IV, Parts B and C include additional reference items to help guide the clinical assessment of the functional status of the L2-S3 nerve roots.
SENSORY INNERVATION OF THE HIP
As a general rule, the hip capsule, ligaments, and parts of the labrum receive sensory innervation through the same nerve roots that supply the overlying muscles. The anterior part of the capsule of the hip receives sensory fibers from the femoral nerve. The posterior capsule receives sensory fibers from all nerve roots originating from the sacral plexus.74,160 The connective tissues of the medial aspects of the hip and knee joints receive sensory fibers from the obturator nerve; this may explain why inflammation of the hip may be perceived as pain in the medial knee region.
Muscular Function at the Hip
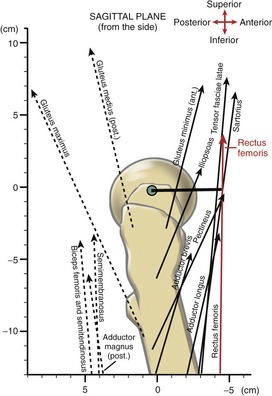
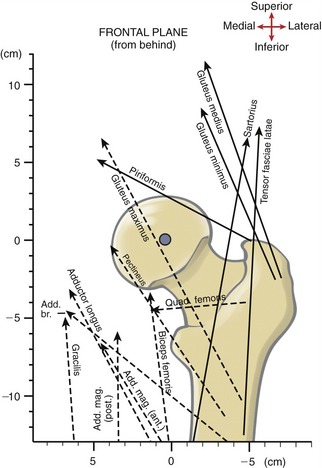
Throughout this chapter, the line of force of several muscles is illustrated relative to the axes of rotation at the hip. Figure 12-25, for example, shows a sagittal plane representation of the significant flexor and extensor muscles of the hip.35,36 Although Figure 12-25 provides useful insight into the potential function of several muscles of the hip, two limitations must be considered. First, the line of force of each muscle does not represent a force vector, but the overall direction of the muscle’s force within the sagittal plane. The figure therefore does not provide the information needed to compare the “strength”—or torque—potential between the muscles. This comparison requires additional information, such as the muscle’s three-dimensional orientation to the hip and its cross-sectional area. Second, the lines of force and subsequent lengths of the moment arms depicted in Figure 12-25 apply only when the hip is in the anatomic position. Once the hip moves out of this position, the potential action and torque potential of each muscle change.15 This partially explains why the maximal-effort internal torque of a muscle group varies throughout the range of motion.
Throughout this chapter, a muscle’s action is considered as either primary or secondary (Table 12-2). The designation of muscle action is based on data such as moment arm length, muscle size and overall fiber direction, and, when available, reports from electromyography (EMG)-based and anatomic studies. Unless otherwise specified, muscle actions are based on a concentric contraction, originating from the anatomic position. A muscle with a relatively insignificant action, or an action that is more substantial in a hip position other than the anatomic position, is not included in Table 12-2. Consult Appendix IV, Part D for a listing of detailed attachments and innervation of all muscles of the hip.
TABLE 12-2.
Muscles of the Hip, Organized According to Primary or Secondary Actions*
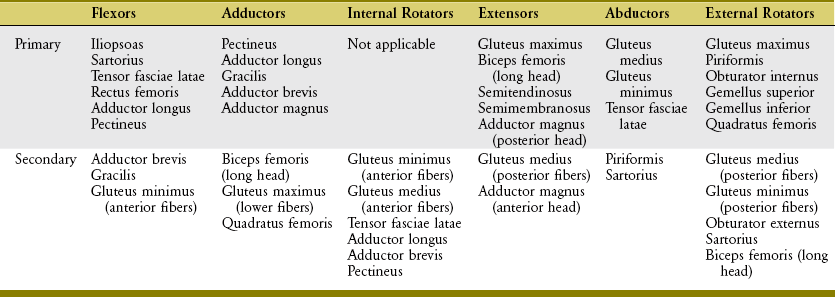
*Each action assumes a muscle contraction that originates from the anatomic position. Several of these muscles may have a different action when they contract from a position other than the anatomic position.
HIP FLEXOR MUSCLES
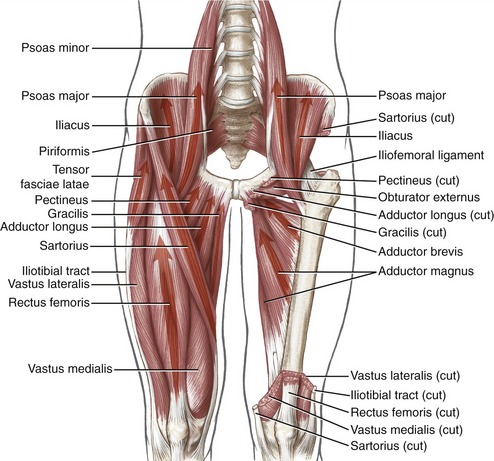
The primary hip flexors are the iliopsoas, sartorius, tensor fasciae latae, rectus femoris, adductor longus, and pectineus (Figure 12-26).36 Figure 12-25 shows the excellent flexion leverage of many of these muscles. Secondary hip flexors are the adductor brevis, gracilis, and anterior fibers of the gluteus minimus.
Anatomy and Individual Action: The iliopsoas is large and long, spanning the area between the last thoracic vertebra and the proximal femur (see Figure 12-26). Anatomically, the iliopsoas consists of two muscles: the iliacus and the psoas major. The iliacus attaches on the iliac fossa and extreme lateral edge of sacrum, just over the sacroiliac joint. The psoas major attaches along the transverse processes of the last thoracic and all lumbar vertebrae, including the intervertebral discs.53 The fibers of the iliacus and the psoas major usually fuse just anterior to the femoral head (see Figure 12-26, left hip). A tendon forms that anchors the muscle to the femur, on the lesser trochanter. En route to its distal insertion, the broad tendon of the iliopsoas is deflected posteriorly about 35 to 45 degrees, immediately after it crosses the superior pubic ramus. With the hip in full extension, this deflection raises the tendon’s angle-of-insertion to the femur, thereby increasing the muscle’s leverage for hip flexion.
The iliopsoas is a potent hip flexor from both a femoral-on-pelvic and pelvic-on-femoral perspective. From the anatomic position, the iliopsoas is not an effective rotator, although with the hip abducted the iliopsoas assists with external rotation.157
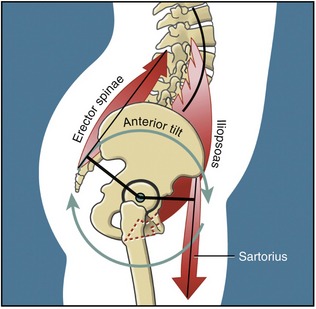
The iliopsoas muscle produces force that crosses the lumbar and lumbosacral regions as well as the hip.5,78,154 Because of its strong anterior tilting action on the pelvis, the iliopsoas can accentuate the lumbar lordosis if the pelvis is not well stabilized by an abdominal muscle such as the rectus abdominis. The psoas major provides excellent vertical stability to the lumbar spine, especially in near full hip extension, where the passive tension in the muscle is greatest (see Chapter 10).181
The psoas minor lies anterior to the muscle belly of the psoas major, although it may be absent in about 40% of people.160 This slender muscle attaches proximally between the twelfth thoracic and first lumbar vertebra and distally to the pelvis near the pectineal line. The psoas minor has no ability to flex the hip; isolated bilteral contraction of the psoas minor may have the ability to posteriorly tilt the pelvis.
The sartorius, the longest muscle in the body, originates at the anterior-superior iliac spine (see Figure 12-26). This thin, fusiform muscle courses distally and medially across the thigh to attach on the medial surface of the proximal tibia (see Figure 13-7). The name sartorius is based on the Latin root sartor, referring to a tailor’s position of cross-legged sitting. This name describes the muscle’s combined action of hip flexion, external rotation, and abduction.
The tensor fasciae latae attaches to the ilium just lateral to the sartorius (see Figure 12-26). This relatively short muscle attaches distally to the proximal part of the iliotibial band. The band extends distally across the knee to attach to the lateral tubercle of the tibia.
The iliotibial band is a component of a more extensive connective tissue known as the fascia lata of the thigh.160 Laterally, the fascia lata is thickened by attachments from the tensor fasciae latae and the gluteus maximus. At multiple locations the fascia lata turns inward between muscles, forming distinct fascial sheets known as intermuscular septa. These septa partition each of the main muscle groups of the thigh according to innervation. The intermuscular septa of the thigh ultimately attach to the linea aspera on the posterior surface of the femur, along with attachments of most of the adductor muscles and several of the vasti muscles (components of the quadriceps).
From the anatomic position, the tensor fasciae latae is a primary flexor and abductor of the hip. The muscle is also a secondary internal rotator.136 As indicated by its name, the tensor fasciae latae increases tension throughout the fascia lata. Tension passed inferiorly through the iliotibial band may help stabilize the extended knee. Repetitive tension within the iliotibial band may cause inflammation at its insertion site near the lateral tubercle of the tibia. Stretching a tightened iliotibial band with the knee extended often incorporates various combinations of hip adduction and extension.48
The proximal part of the rectus femoris emerges between the limbs of an inverted V formed by the sartorius and tensor fasciae latae (see Figure 12-26). This large bipennate-shaped muscle has its proximal attachment on the anterior-inferior iliac spine and along the superior rim of the acetabulum and in the joint capsule.160 Along with the other members of the quadriceps, the rectus femoris attaches to the tibia via the patellar tendon. The rectus femoris is responsible for about one third of the total isometric, flexion torque at the hip.105 In addition, the rectus femoris is a primary knee extensor. The combined two-joint actions of this important muscle are considered in Chapter 13. The anatomy and function of the pectineus and adductor longus are described in the section on the adductors of the hip.
Pelvic-on-Femoral Hip Flexion: Anterior Pelvic Tilt: The anterior pelvic tilt is performed by a force-couple between the hip flexors and low-back extensor muscles (Figure 12-27). With fixed femurs, contraction of the hip flexors rotates the pelvis about the medial-lateral axis through both hips. Although Figure 12-27 illustrates the iliopsoas and sartorius, any muscle capable of femoral-on-pelvic flexion is equally capable of tilting the pelvis anteriorly. Clinically, an important aspect of the anterior tilt is related to the increase in lordosis at the lumbar spine. Greater lordosis increases the compressive loads on the lumbar apophyseal joints and increases anterior shear force at the lumbosacral junction.
A lumbopelvic posture with normal lumbar lordosis optimizes the alignment of the entire spine (see Chapter 9). Some persons, however, have difficulty maintaining lumbar lordosis and therefore have a relatively flat (i.e., slightly flexed) lumbar spine. This abnormal posture may be caused by a combination of factors, including habit, pain avoidance, compensation from another poorly aligned region of the body, increased stiffness in connective tissue around the lumbar spine, and, in extreme cases, tension emanating from hip extensor muscles. The quantitative relationship between tightness in the hamstring muscles and the posture of the pelvis-and-lumbar region during standing remains controversial.97
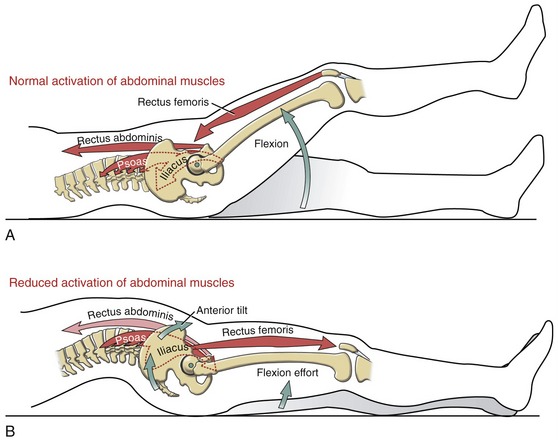
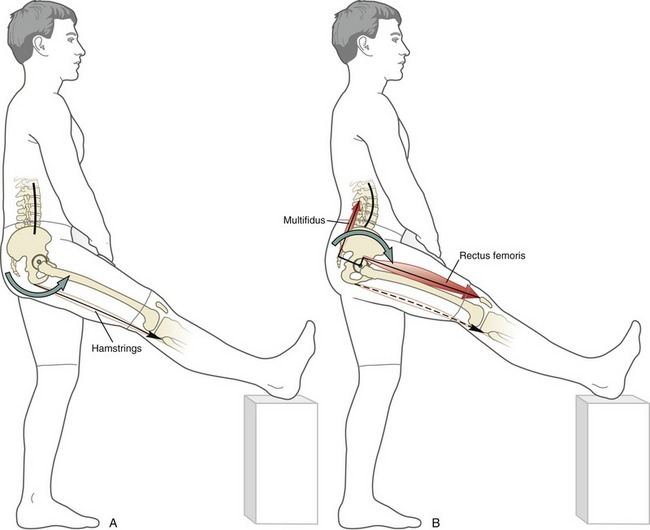
Femoral-on-Pelvic Hip Flexion: Femoral-on-pelvic hip flexion often occurs simultaneously with knee flexion as a means to shorten the functional length of the lower extremity during the swing phase of walking or running. The action of moderate- to high-power hip flexion requires coactivation of the hip flexor and abdominal muscles. This intermuscular cooperation is apparent when the leg is lifted while the knee is held in extension (i.e., a “straight-leg-raise” movement). This action requires that the rectus abdominis (a representative “abdominal” muscle) generate a potent posterior pelvic tilt effort that is strong enough to neutralize the strong anterior pelvic tilt potential of the hip flexor muscles (Figure 12-28, A).65 The degree to which the abdominal muscles actually neutralize the anterior pelvic tilt depends on the demands of the activity and the relative forces produced by the contributing muscle groups.34 Without sufficient stabilization from the abdominal muscles, however, contraction of the hip flexor muscles is inefficiently spent tilting the pelvis anteriorly (see Figure 12-28, B). As stated, the excessive anterior tilt of the pelvis accentuates the lumbar lordosis.
The pathomechanics depicted in Figure 12-28, B are most severe in situations in which the abdominal muscles are markedly weakened but the hip flexors remain relatively strong. With the exception of pathology such as poliomyelitis or muscular dystrophy, this pattern of weakness is relatively rare. More commonly, the abdominal muscles are only moderately weak, secondary to disuse or abdominal surgery. In this case, persons may develop low-back pain because of the increased compression on the apophyseal joints of the chronically, fully extended lumbar vertebrae.
HIP ADDUCTOR MUSCLES
The primary adductors of the hip are the pectineus, adductor longus, gracilis, adductor brevis, and adductor magnus (see Figure 12-26). Secondary adductors are the biceps femoris (long head), the gluteus maximus, especially the lower fibers, and the quadratus femoris. The line of force of many of these muscles is shown in Figure 12-29.
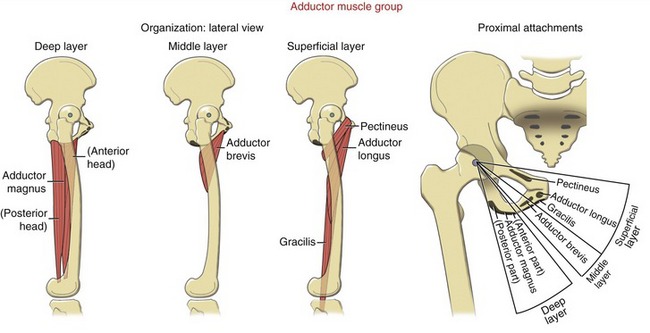
Functional Anatomy: The adductor muscle group occupies the medial quadrant of the thigh. Topographically, the adductor muscles are organized into three layers (Figure 12-31). The pectineus, adductor longus, and gracilis occupy the superficial layer. Proximally, these muscles attach along the superior and inferior pubic ramus and adjacent body of the pubis. Distally, the pectineus and the adductor longus attach to the posterior surface of the femur—near and along varying regions of the linea aspera. The long and slender gracilis attaches distally to the medial side of the proximal tibia (see Figure 13-7). The middle layer of the adductor group is occupied by the triangular-shaped adductor brevis. The adductor brevis attaches to the pelvis on the inferior pubic ramus and to the femur along the proximal one third of the linea aspera.
The deep layer of the adductor group is occupied by the massive, triangular adductor magnus (see Figure 12-26, left side, and Figure 12-37, right side). This large muscle attaches primarily from the ischial ramus and part of the ischial tuberosity. From its proximal attachment the adductor magnus forms anterior and posterior heads.
Overall Function: The line of force of the adductors approaches the hip from many different orientations. Functionally, therefore, the adductor muscles produce torques in all three planes at the hip.36,119 The following section considers the primary actions of the adductors in the frontal and sagittal planes. The action of these muscles as secondary internal rotators is discussed later in this chapter.
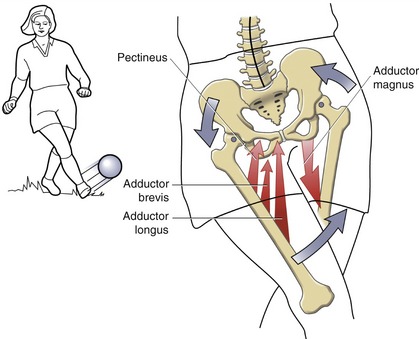
Frontal Plane Function: The most obvious function of the adductor muscles is production of adduction torque. The torque controls the kinematics of both femoral-on-pelvic and pelvic-on-femoral hip adduction. Figure 12-32 shows an example of selected adductor muscles contracting bilaterally to control both forms of motion. On the right side, several adductors are shown accelerating the femur toward the ball. Adding to the forcefulness of this action is the downward rotation or lowering of the right iliac crest—a motion occurring by pelvic-on-femoral adduction of the left hip. Although only the adductor magnus is shown on the left side, other adductor muscles assist in this action. Such an adduction action of the planted left hip likely also requires eccentric activation of the left hip abductors (such as the gluteus medius), which are well suited to decelerate the pelvic-on-femoral hip adduction.
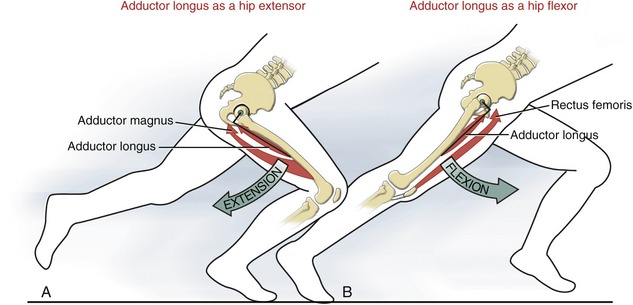
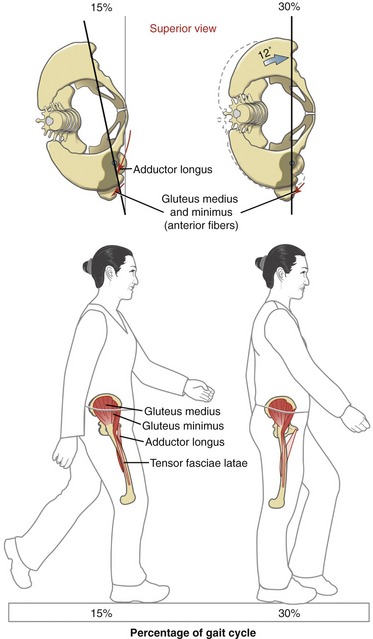
Sagittal Plane Function: Regardless of hip position, the posterior fibers of the adductor magnus are powerful extensors of the hip, similar to the hamstring muscles. Of interest, however, is that within an arc of about 40 to 70 degrees of hip flexion, the line of force of most of the other adductor muscles runs directly through or close to the medial-lateral axis of rotation of the hip. At this point, the adductor muscles lose their potential to produce any torque in the sagittal plane.67 When outside the 40- to 70-degree flexed position, however, the individual adductor muscles regain leverage as significant flexors or extensors of the hip.36,67 Consider, for example, the adductor longus as a representative adductor muscle during a fast sprint (Figure 12-33, A). From a position of about 100 degrees of hip flexion, the line of force of the adductor longus is well posterior to the medial-lateral axis of the joint. At this position the adductor longus has an extensor moment arm and is capable of generating an extension torque—similar to the posterior head of the adductor magnus. From a hip position of near extension, however, the line of force of the adductor longus is well anterior to the medial-lateral axis of rotation (see Figure 12-33, B). The adductor longus now has a flexor moment arm and generates a flexion torque similar to that of the rectus femoris, for example. The adductor muscles therefore provide a useful source of flexion and extension torque at the hip. The bidirectional torques are useful during high-power, cyclic motions such as sprinting, cycling, running up a steep hill, and descending and rising from a deep squat. When the hip is near full flexion, the adductors are most mechanically prepared to augment the extensors. In contrast, when the hip is near full extension, they are most mechanically prepared to augment the flexors. This utilitarian function of the adductors may partially explain their relatively high susceptibility to strain injury during running and jumping, especially while quickly changing directions.
HIP INTERNAL ROTATOR MUSCLES
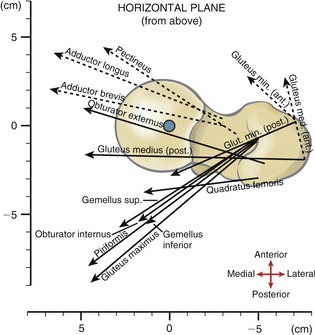
Overall Function: An “ideal” primary internal rotator muscle of the hip would theoretically be oriented in the horizontal plane during standing, at some linear distance from the longitudinal or vertical axis of rotation at the hip. From the anatomic position, however, there are no primary internal rotators because no muscle is oriented even close to the horizontal plane. Several secondary internal rotators exist, however, including the anterior fibers of the gluteus minimus and the gluteus medius, tensor fasciae latae, adductor longus, adductor brevis, and pectineus. The horizontal line of force of many of these muscles is depicted in Figure 12-34.36,91,104 The anatomy of each of the internal rotators is described in other sections (see Figures 12-26 and 12-41).
With the hip approaching 90 degrees of flexion, the internal rotation torque potential of the internal rotator muscles dramatically increases.33,36,104 This becomes clear with the help of a skeleton model and piece of string to mimic the line of force of muscles, such as the anterior fibers of the gluteus minimus or gluteus medius. Flexing the hip close to 90 degrees reorients the line of force of these muscles from nearly parallel to nearly perpendicular to the longitudinal axis of rotation at the hip. This occurs because the longitudinal axis of rotation remains parallel with the shaft of the repositioned femur. Delp and co-workers have reported that the internal rotation moment arm of the anterior part of the gluteus medius, for example, increases eightfold between 0 and 90 degrees of flexion.33 Even some external rotator muscles (such as the piriformis, anterior fibers of the gluteus maximus, and posterior fibers of the gluteus minimus) switch actions and become internal rotators beyond about 90 degrees of flexion.33 These changes in muscle action help explain why maximal-effort internal rotation torque in healthy persons has been shown to be about 50% greater with the hip flexed rather than extended.99
The kinesiologic phenomenon just described also helps explain the excessively internally rotated and flexed (“crouched”) gait pattern often observed in persons with cerebral palsy.62,166 With poor active control of hip extension (especially combined with contracture of the hip flexor muscles), the flexed posture of the hip exaggerates the internal rotation torque potential of many muscles of the hip.6,7,33 This gait pattern may be better controlled by enhanced activation of the gluteus maximus, a potent extensor and external rotator.6
Biomechanics of the Adductor Muscles as Internal Rotators of the Hip: In general, most of the adductor muscles are capable of producing a modest internal rotation torque at the hip when the body is in or near the anatomic position.36,91,104 This action, however, may be difficult to reconcile considering that most adductors attach to the posterior side of the femur along the linea aspera. With normal anatomy of the hip, a shortening of these muscles would appear to rotate the femur externally instead of internally. What must be considered, however, is the effect that the natural anterior bowing of the femoral shaft has on the line of force of the muscles. Bowing places much of the linea aspera anterior to the longitudinal axis of rotation at the hip (Figure 12-35, A). As depicted in Figure 12-35, B, the horizontal force component of an adductor muscle, such as the adductor longus, lies anterior to the axis of rotation. Force from this muscle therefore acts with a moment arm to produce internal rotation.
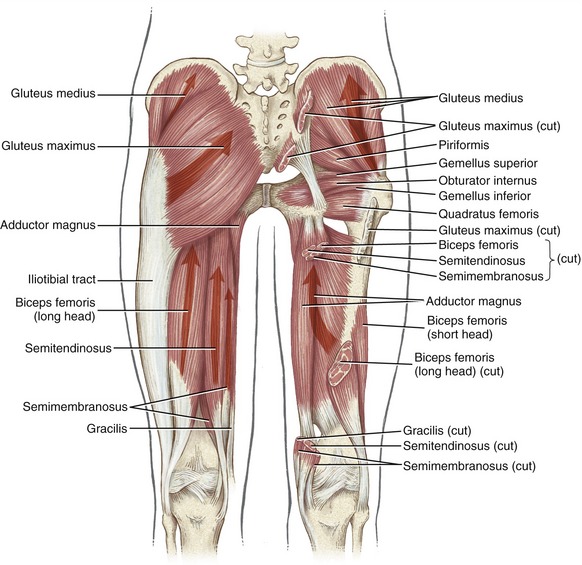
HIP EXTENSOR MUSCLES
Anatomy and Individual Action: The primary hip extensors are the gluteus maximus, the hamstrings (i.e., the long head of the biceps femoris, the semitendinosus, and the semimembranosus), and the posterior head of the adductor magnus (Figure 12-37).36 The posterior fibers of the gluteus medius and anterior fibers of the adductor magnus are secondary extensors. With the hip flexed to at least about 70 degrees and beyond, most adductors muscles (with the possible exception of the pectineus) are capable of assisting with hip extension.
Figure 12-25 depicts the line of force of the primary hip extensors. In the extended position the posterior head of the adductor magnus has the greatest moment arm for extension. The adductor magnus and the gluteus maximus have the greatest cross-sectional areas of all the extensors.176
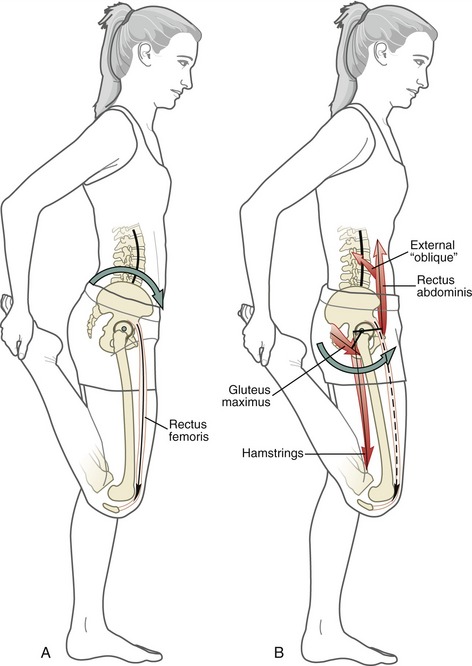
Pelvic-on-Femoral Hip Extension: The following sections describe two different situations in which the hip extensor muscles control pelvic-on-femoral extension.
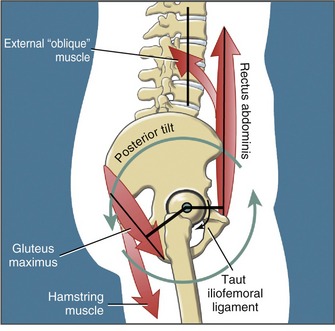
Hip Extensors Performing a Posterior Pelvic Tilt: With the supralumbar trunk held relatively stationary, the hip extensor and abdominal muscles act as a force-couple to posteriorly tilt the pelvis (Figure 12-38). The posterior tilt extends the hip joints slightly and reduces the lumbar lordosis.
The muscular mechanics involved with posterior tilting of the pelvis are generally similar to those described for the anterior tilting of the pelvis (compare Figures 12-27 and 12-38). In both tilting actions, a force-couple exists between the hip and trunk muscles. Consequently the pelvis rotates through a relatively short arc, using the femoral heads as a pivot point. During standing, a combination of tension in the hip’s capsular ligaments and hip flexor muscles normally determines the end-range of the posterior pelvic movement. Interestingly, unlike the end-range of an anterior pelvic tilt, the lumbar spine does not normally restrict the end-range of the posterior pelvic tilt.
Hip Extensors Controlling a Forward Lean of the Body: Leaning forward while standing is a very common activity. Consider, for example, the forward lean used to brush your teeth over a sink. The muscular support at the hip for this near static posture is primarily the responsibility of the hamstring muscles. Consider two phases of a forward lean shown in Figure 12-39. During a slight forward lean (see Figure 12-39, A), body weight is displaced just anterior to the medial-lateral axis of rotation at the hips. This slightly flexed posture is restrained by minimal activation from the gluteus maximus and hamstring muscles. A more significant forward lean, however, displaces body weight farther in front of the hips (see Figure 12-39, B). Supporting this markedly flexed posture requires greater muscle activation from the hamstring muscles. The gluteus maximus, however, remains relatively inactive in this position—a point verifiable by palpation and inferred from electromyographic data.45 The apparent increased responsibility of the hamstrings (in contrast to the gluteus maximus) can be explained biomechanically and physiologically. Forward leaning increases the hip extension moment arm of the hamstring muscles while it decreases the hip extensor moment arm of the gluteus maximus.145 (Compare the 15-degree and 30-degree points in the graph in Figure 12-39.) Leaning forward, therefore, mechanically optimizes the extension torque potential of the hamstrings.67 A significant forward lean also elongates the hamstring muscles across both the hip and the knee joints. The resulting increased passive tension in these elongated biarticular muscles helps support the partially flexed position of the hips. For these reasons the hamstrings appear uniquely equipped to support the hip during a forward lean. Apparently the nervous system holds the gluteus maximus partially in reserve for more powerful hip extension activities, such as rapidly climbing a flight of stairs.
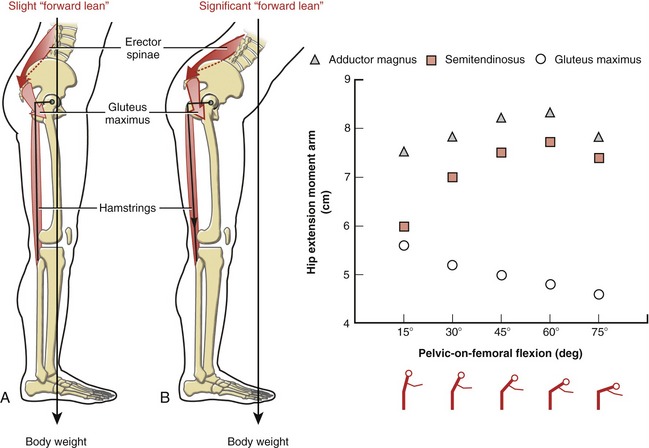
FIGURE 12-39. The hip extensor muscles are shown controlling a forward lean of the pelvis over the thighs. A, Slight forward lean of the upper body displaces the body weight force slightly anterior to the medial-lateral axis of rotation at the hip. B, A more significant forward lean displaces the body weight force even farther anteriorly. The greater flexion of the hips rotates the ischial tuberosities posteriorly, thereby increasing the hip extension moment arm of the hamstrings. The taut line (with arrow head within the stretched hamstring muscles) indicates the increased passive tension. In both A and B, the relative demands placed on the muscles are shown by relative shades of red. At right is a graph showing the length of hip extension moment arms of selected hip extensors as a function of forward lean.145
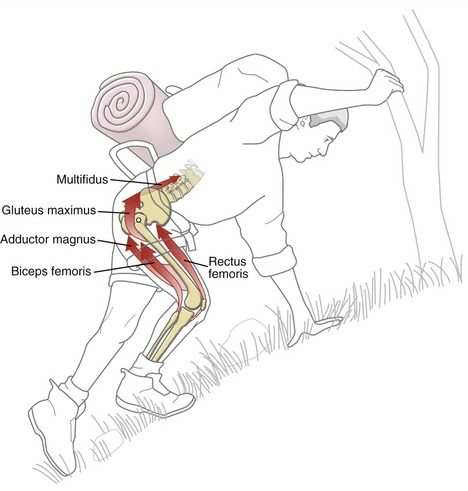
Femoral-on-Pelvic Hip Extension: As a group, the hip extensor muscles are frequently required to produce large and powerful femoral-on-pelvic hip extension torque to accelerate the body forward and upward. Consider, for example, the demands placed on the right hip extensors while one climbs a steep hill (Figure 12-40). The flexed position of the right hip while the climber is carrying a heavy pack imposes a large external (flexion) torque at the hip. The flexed position, however, favors greater extension torque generation from the hip extensor muscles. Furthermore, with the hip markedly flexed, many of the adductor muscles can produce an extension torque, thereby assisting the primary hip extensors. Activation of the low-back extensor muscles helps support the flexed trunk, as well as stabilizing the pelvis for the strongly activated hip extensor muscles.
HIP ABDUCTOR MUSCLES
Anatomy and Individual Action: The primary hip abductor muscles are the gluteus medius, gluteus minimus, and tensor fasciae latae.23 The piriformis and sartorius are considered secondary hip abductors.
The gluteus medius attaches on the external surface of the ilium above the anterior gluteal line. The muscle attaches distally on the lateral aspect of the greater trochanter (see Figure 12-37). The distal attachment provides the gluteus medius with the greatest abductor moment arm of all the abductor muscles (see Figure 12-29). The gluteus medius is also the largest of the hip abductor muscles, occupying about 60% of the total abductor cross-sectional area.23 The broad and fan-shaped gluteus medius has been considered as having three functional sets of fibers: anterior, middle, and posterior.23,159 All fibers contribute to abduction of the hip; however, from the anatomic position the anterior fibers also produce internal rotation, and the posterior fibers also produce extension and external rotation. These actions may change considerably when muscle activation is initiated from outside the anatomic position.8
The gluteus minimus lies deep and slightly anterior to the gluteus medius. This muscle attaches proximally on the ilium—between the anterior and inferior gluteal lines—and distally on the anterior-lateral aspect of the greater trochanter (Figure 12-41). The muscle also attaches into the superior capsule of the joint.169 These attachments may retract this part of the capsule away from the joint during motion—a mechanism that may prevent capsular impingement.
All the fibers of the gluteus minimus contribute to abduction; the more anterior fibers also contribute to internal rotation and flexion.23,85 The gluteus minimus is smaller than the gluteus medius, occupying about 20% of the total abductor cross-sectional area.23
The tensor fasciae latae is the smallest of the three primary hip abductors, occupying about 11% of the total abductor cross-sectional area.23 The anatomy of the tensor fasciae latae is discussed elsewhere in this text.
Hip Abductor Mechanism: Control of Frontal Plane Stability of the Pelvis during Walking: The abduction torque produced by the hip abductor muscles is essential to the control of the frontal plane pelvic-on-femoral kinematics during walking. During most of the stance phase, the hip abductors stabilize the pelvis over the relatively fixed femur (see Figure 12-36).71,72 During the stance phase, therefore, the hip abductor muscles have a role in controlling the pelvis in the frontal plane and, as discussed earlier, the horizontal plane.
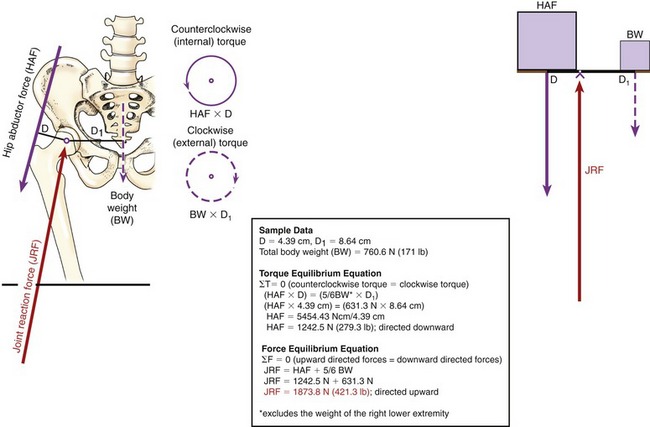
Hip Abductor Mechanism: Role in the Production of Compression Force at the Hip: Figure 12-42 shows the major factors involved with maintaining frontal plane stability of the right hip during single-limb-support, similar to that required during the mid-stance phase of walking. The forces created by active hip abductors and body weight create opposing torques that control the position and stability of the pelvis (within the frontal plane) over the femoral head. During single-limb support, the pelvis is comparable to a seesaw, with its fulcrum represented by the femoral head. When the seesaw is balanced, the counterclockwise (internal) torque produced by the right hip abductor force (HAF) equals the clockwise (external) torque caused by body weight (BW). Balance of opposing torques is called static rotary equilibrium.
During single-limb support, the hip abductor muscles—in particular the gluteus medius—produce most of the compression force across the hip.31 This important point is demonstrated by the model in Figure 12-42.121,123 Note that the internal moment arm (D) used by the hip abductor muscles is about half the length of the external moment arm (D1) used by body weight.127 Given this length disparity, the hip abductor muscles must produce a force twice that of body weight in order to achieve stability during single-limb support. On every step, therefore, the acetabulum is pulled against the femoral head by the combined forces produced by the hip abductor muscles and the pull of body weight. To achieve static linear equilibrium, this downward force is counteracted by a joint reaction force (JRF) of equal magnitude but oriented in nearly the opposite direction (see Figure 12-42). The joint reaction force is directed 10 to 15 degrees off vertical—an angle that is strongly influenced by the orientation of the hip abductor muscle force vector.72
The sample data supplied in Figure 12-42 show how to estimate the approximate magnitude of the hip abductor force and hip joint reaction force. (For simplicity, it is assumed that all forces act vertically, as shown in the seesaw model.) As shown in the calculations, an upward-directed joint reaction force (JRF) of 1873.8 N (421.3 lb) occurs when a person weighing 760.6 N (171 lb) is in single-limb support over the right limb. This reaction force is about 2.5 times body weight, 66% of which comes from the hip abductor muscles. During walking, the joint reaction force is even greater because of the acceleration of the pelvis over the femoral head. Data based on computer modeling or direct measurements from strain gauges implanted into a hip prosthesis show that joint compression forces reach three times body weight during walking.71,161 These forces can increase to at least 5 or 6 times body weight while running or ascending and descending stairs or ramps.12,153 Even ordinary daily functional activities can generate surprisingly large hip joint forces.64 In general, these forces serve important physiologic functions, such as stabilizing the femoral head within the acetabulum, assisting in the nutrition of the articular cartilage, and providing the stimulus for normal development and shape of joint structure in the growing child. The articular cartilage and trabecular bone normally protect the joint by safely dispersing large forces. A hip with arthritis, however, may no longer be able to provide this protection.
Maximal Abduction Torque Varies According to Hip Joint Angle: The unique relationship between a muscle group’s internal torque and joint angle provides insight into the functional demands naturally placed on the muscles. The shape of the plot depicted in Figure 12-43, for example, clearly shows that the abductor muscles produce their peak torque (greatest strength) when elongated.127 The maximal torque is produced when the hip is slightly adducted or in a neutral (0-degree) hip position. This frontal plane hip angle naturally occurs when the body is in or close to the single-limb support phase of walking: precisely when these muscles are needed to provide frontal plane stability to the hip. In essence, the abductor muscles have their greatest torque reserve at muscle lengths that correspond to their greatest functional demands.
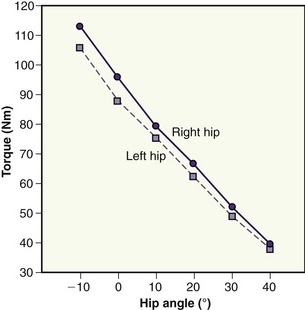
FIGURE 12-43. This plot shows the effect of frontal plane range of hip motion on the maximal-effort, isometric hip abduction torque in 30 healthy persons.127 The −10-degree hip angle represents the adducted position at which the muscles are at their longest. Data are shown for both right and left sides.
The adducted position of the hip also increases the passive tension in the naturally stiff iliotibial band. This passive tension, although likely relatively small, can nevertheless augment the abduction torque required during the single-limb support phase of walking.128
In contrast, hip abduction torque potential is least at the near–fully shortened muscle length that corresponds to 40 degrees of abduction (see Figure 12-43). Ironically, the near–maximally abducted hip is in the position traditionally suggested for manually testing the strength of the hip abductors.80
HIP EXTERNAL ROTATOR MUSCLES
The primary external rotator muscles of the hip are the gluteus maximus and five of the six “short external rotators.” In the anatomic position, muscles considered as secondary external rotators are the posterior fibers of the gluteus medius and minimus, obturator externus, sartorius, and long head of the biceps femoris. The obturator externus is considered a secondary rotator because in the anatomic position its line of force lies only a few millimeters posterior to the longitudinal axis of rotation (see Figure 12-34).
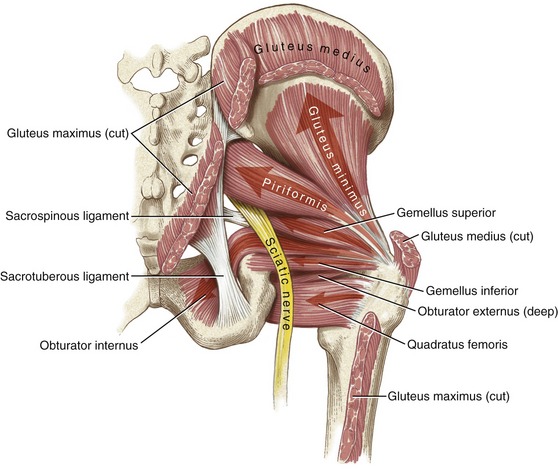
Functional Anatomy of the “Short External Rotators”: The six “short external rotators” of the hip are the piriformis, obturator internus, gemellus superior, gemellus inferior, quadratus femoris, and obturator externus (see Figures 12-14, 12-37, and 12-41). The line of force of these muscles is oriented primarily in the horizontal plane. This orientation is optimal for the production of external rotation torque, as most of the force component of each muscle has a perpendicular intersection with the vertical axis of rotation. In a manner similar to the infraspinatus and teres minor at the shoulder, the short external rotators also provide stability to the posterior side of the joint.
The piriformis attaches proximally on the anterior surface of the sacrum, among the ventral sacral foramina (see Figure 12-26). Exiting the pelvis posteriorly through the greater sciatic foramen, the piriformis attaches to the superior aspect of the greater trochanter (see Figure 12-41).
In addition to the action of external rotation, the piriformis is a secondary hip abductor. Both actions are apparent in the muscle’s line of force relative to the axis of rotation at the hip (see Figures 12-29 and 12-34).
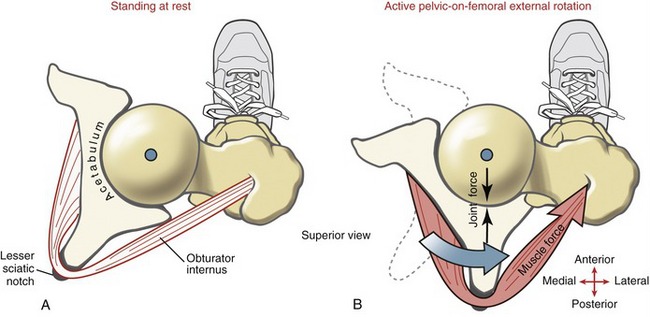
The obturator internus muscle arises from the internal side of the obturator membrane and from the adjacent ilium (see Figure 12-41). From this origin, the fibers converge to a central tendon after exiting the pelvis through lesser sciatic foramen. This notch, which is lined with hyaline cartilage, functions as a pulley by deflecting the tendon of the obturator internus by about 130 degrees on its approach to the trochanteric fossa of the femur (Figure 12-44, A).160 With the femur firmly fixed during standing, strong contraction of this muscle rotates the pelvis (and superimposed trunk) relative to the femoral head (see Figure 12-44, B). In addition to rotating the pelvis, the force produced by the obturator internus compresses the surfaces of the joint, thereby providing an element of dynamic stability to the hip.
The gemellus superior and inferior (from the Latin root geminus, meaning twins) are two, small, nearly identically sized muscles with proximal attachments on either side of the lesser sciatic notch (see Figure 12-41). Each muscle blends in with the central tendon of the obturator internus for a common attachment to the femur. Immediately below the gemellus inferior is the quadratus femoris muscle. This flat muscle arises from the external side of the ischial tuberosity and inserts on the posterior side of the proximal femur.
The obturator externus muscle arises from the external side of the obturator membrane and adjacent ilium (see Figure 12-14). The belly of this muscle is visible from the anterior side of the pelvis after removal of the adductor longus and pectineus muscles (see Figure 12-26, left side). The muscle attaches posteriorly on the femur at the trochanteric fossa (see Figure 12-6). (Based on its location and innervation, the obturator externus is more anatomically associated with the adductor group of muscles, rather than the other five short external rotators. The obturator externus is innervated by nerve roots that originate from the lumbar plexus [via the obturator nerve], as are most of the other adductor muscles. The other small external rotators, in contrast, are innervated through the sacral plexus, with nerve roots as low as S2.)
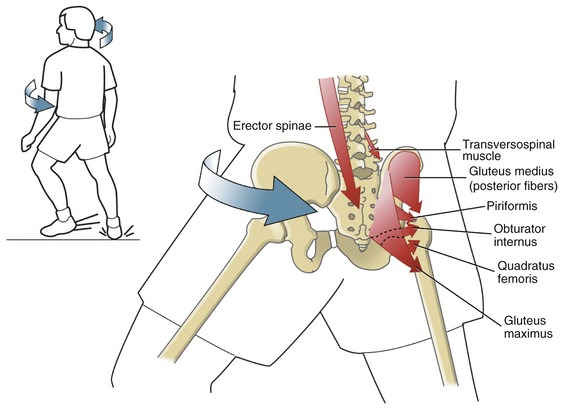
Overall Function: The functional potential of the external rotators is most evident during pelvic-on-femoral rotation. Consider, for example, the external rotator muscles contracting to rotate the pelvis over the femur (Figure 12-45). With the right lower extremity firmly in contact with the ground, contraction of the right external rotators accelerates the anterior side of the pelvis and attached trunk to the left—contralateral to the fixed femur. This action of planting a foot and “cutting” to the opposite side is the natural way to abruptly change direction while running. As indicated in Figure 12-45, activation of the right gluteus maximus, for instance, is very capable of imparting both the extension and external rotation thrust to the hip during this action. If needed, the external rotation torque can be decelerated by eccentric action of internal rotator muscles. Extremely rapid eccentric activation of the adductor longus or brevis, for example, may be used to decelerate the contralateral-directed pelvic rotation—an action that may cause “strain” injury to these muscles. The mechanism of injury may partially explain the relatively high incidence of adductor muscle strain during many sporting activities that involve rapid rotation of the pelvis and trunk while running.
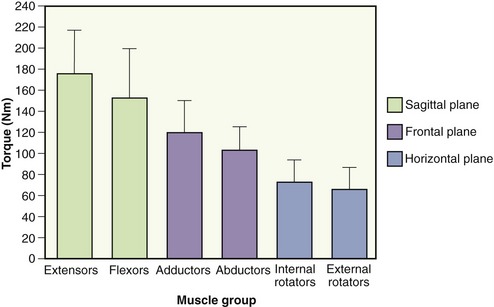
MAXIMAL TORQUE PRODUCED BY THE HIP MUSCLES
Normative data on the maximal-effort torque production of the hip muscles can serve as useful information in assessment of progress and setting of goals for persons involved in rehabilitation and training programs. Figure 12-46 depicts the average, maximal internal torque produced by a sample of healthy males.21 It is interesting to observe the ranking of the peak torques across the three planes of motion. The greatest torque is produced within the sagittal plane, with extension torque slightly exceeding flexion torque. The predominant strength of the hip extensors compared with all other muscle groups is not surprising: these muscles must lift or propel the body upward (and often forward) against gravity or control the descent of the body. The relatively high strength of the hip flexor muscles reflects the need to rapidly accelerate the lower limb during running, in addition to controlling the entire trunk and pelvis relative to fixed lower extremities. Consider in the latter case the physically powerful iliopsoas, for example—a muscle that likely accounts for a significant proportion of the flexion torque potential at the hip.
EXAMPLES OF HIP DISEASE: RATIONALE FOR SELECTED THERAPEUTIC AND SURGICAL INTERVENTIONS
Fracture of the Hip
Fracture of the hip (i.e., proximal femur) is a major health and economic problem in the United States.167,170 About 95% of all fractures of the hip are the result of falls.137 The incidence of hip fracture increases with advanced age, and hip fracture is the second leading cause of hospitalization in the elderly.174 Two primary factors often associated with the higher incidence of hip fracture in the elderly are age-related osteoporosis and the higher incidence of falling.30,170
The number of hip fractures in the United States is expected to triple by the year 2050 because of the rapidly increasing number of persons aged 85 years and older.170 Large increases in the number of hip fractures are also anticipated over the next several decades worldwide.51
Mortality is surprisingly high after hip fracture: studies report 12% to 25% of persons die within 1 year of fracturing a hip.68,134,170 Much of this mortality is associated with an underlying medical condition rather than the actual trauma of the fracture.140 Although nearly 80% of persons over 65 years of age who sustain hip fractures are women, the mortality rate in men is almost twice as high after a hip fracture.79,170
Hip fracture can result in significant loss of function.135 Research indicates that only about 40% of persons are able to independently perform their basic functional activities 6 to 12 months after hip fracture.37,68,179 About half these persons also continue to require an assistive device to aid their walking.
Osteoarthritis of the Hip
Hip osteoarthritis is a disease manifested primarily by deterioration of the joint’s articular cartilage, loss of joint space, sclerosis of subchondral bone, and the presence of osteophytes.3 Without an adequate dampening mechanism to dissipate joint forces, the hip can experience marked degeneration and change in shape. The American College of Rheumatology recommends the following criteria for diagnosing hip osteoarthritis without the use of radiography: hip pain, less than 115 degrees of hip flexion, and less than 15 degrees of internal rotation.2 The reduced range of motion may be caused by restrictions in soft tissue (such as posterior and inferior capsule or parts of the ischiofemoral ligament) and, in more severe cases, articular malalignment and osteophyte formation. Additional symptoms may include atrophy and weakness of hip muscles, morning stiffness, crepitus, inflammation of soft tissues, and abnormal gait pattern (such as a compensated Trendelenburg gait) or altered step length.103
Hip osteoarthritis can cause major disability and occurs in 10% to 20% of persons in the aging population.39,131 Impairments associated with hip osteoarthritis can cause significant loss in function, such as difficulty climbing stairs, bathing, dressing the lower extremities, and rising from a low chair.
The exact cause of primary hip osteoarthritis remains unclear. Although the frequency of osteoarthritis at any joint increases with age, the disease is not triggered solely by the aging process.102 If this were true, then all elderly persons would eventually develop this disease. The causes of osteoarthritis are complicated and not exclusively based on a simple wear-and-tear phenomenon. Although physical stress may increase the rate and amount of wear at the hip, this does not always lead to osteoarthritis.98,143,147 Other mechanisms that may be related to osteoarthritis are metabolism of the ground matrix of the cartilage, genetics, immune system factors, neuromuscular disorders, and biochemical factors.63,102
Therapeutic Intervention for a Painful or Mechanically Unstable Hip
USING A CANE AND PROPER METHODS FOR CARRYING EXTERNAL LOADS
Severe fracture or osteoarthritis of the hip can lead to chronic pain and mechanical instability. These potentially disabling impairments can also occur in a hip that is either acutely inflamed, brittle because of severe osteoporosis, or markedly dysplastic. Conservative treatment for such conditions may include instructions in assisted gait and functional activities,84,122,123 modalities for relieving pain, and, when appropriate, graded aerobic conditioning and exercise.151 In addition, clinicians frequently provide advice on how to limit the magnitude of potentially large forces that may exacerbate or further complicate the underlying pathology.123 Such advice on hip “joint protection” may include reducing body weight; walking with reduced speed, cadence, and stride length; using an assistance device such as a cane; and methods of carrying loads.13,120,121,161
One of the most practical and effective methods of reducing compression forces on the hip during walking is to use a cane held in the hand opposite the affected hip.1 Use of the cane in this fashion reduces joint reaction forces caused by activation of the hip abductor muscles.120 Figure 12-47 shows that applying a cane force (CF) by the left hand results in a joint reaction force at the right hip of 1195.4 N (268.8 lb).120 This correlates with a 36% reduction in joint reaction force compared with that produced when a cane is not used (see Figure 12-42 for comparison). In essence, the force applied to the cane (held in the left hand) produces a torque about the right hip that is in the same rotary direction as that produced by the overlying hip abductor muscles. Pushing on the cane, therefore, can substitute for part of the force that is naturally required by the hip abductor muscles: reduced demands placed on the hip abductor muscles during single-limb support equates to reduced compression force on the hip joint.112
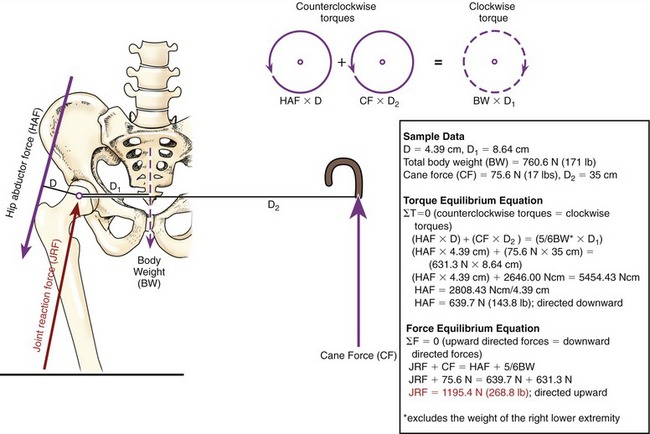
FIGURE 12-47. A frontal plane diagram shows how a cane force (CF) applied by the left hand produces a frontal plane torque about the right hip in single-limb support. The pelvis and trunk are assumed to be in static (linear and rotary) equilibrium about the right hip. The cane-produced torque minimizes the torque and force demands on the right hip abductor muscles. Note that the clockwise torque (dashed circle) resulting from body weight (BW × D1) is balanced by the counterclockwise torques (solid circles) resulting from the hip abductor force (HAF × D) and the cane force (CF × D2). The data shown in the box are used in the torque and force equilibrium equations to estimate the approximate magnitude of hip abductor force and joint reaction force (JRF). The moment arm used by cane force is represented by D2. (See Figure 12-42 for additional abbreviations and background.) (To simplify the mathematics, the calculations assume that all forces are acting in a vertical direction. This assumption introduces modest error in the results. All moment arm directions are assigned positive values.) (From Neumann DA: Hip abductor muscle activity as subjects with hip prosthesis walk with different methods of using a cane, Phys Ther 78:490, 1998. With permission of the American Physical Therapy Association.)
Methods of carrying external loads significantly influence the demands placed on the hip abductor muscles and therefore on the underlying hip joint. Persons with painful, unstable, or surgically replaced hips are to be cautioned about the consequences of carrying relatively large hand-held loads opposite, or contralateral to, the affected hip.13,121,124,126 As shown in Figure 12-48, the contralateral load has a very large external moment arm (D2), creating a substantial clockwise torque about the right hip.121 For frontal plane stability, the right hip abductors must create a counterclockwise torque large enough to balance the clockwise torques caused by the external load (CL × D2) and body weight (BW × D1). As a result of the relatively small moment arm available to the hip abductor muscles (D), the hip abductor force during single-limb support is very large. As shown by the calculations in Figure 12-48, carrying a contralaterally held load of 15% of body weight (114.1 N or 25.7 lb) produces a joint reaction force of 2897.6 N (651.1 lb). A healthy hip can usually tolerate this amount of force without difficulty. Caution must be exercised, however, if structural stability of the hip is compromised.
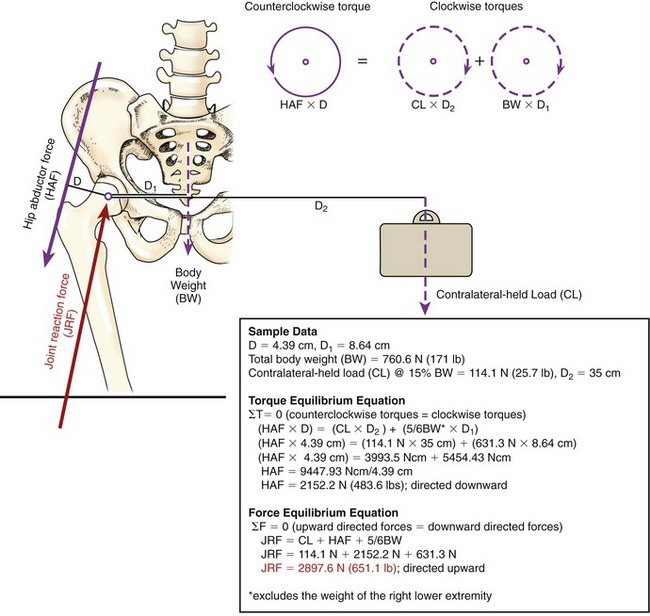
FIGURE 12-48. A frontal plane diagram shows how a load held in the left hand significantly increases the right hip abductor force (HAF) during single-limb support. Two clockwise torques (dashed circles) are produced about the right hip because of the contralateral-held load (CL × D2) and body weight (BW × D1). For equilibrium about the right hip, the clockwise torques must be balanced by a counterclockwise torque (solid circle) produced by the hip abductor force (HAF × D). The data shown in the box are used in the torque and force equilibrium equations to estimate the approximate magnitude of hip abductor force and joint reaction force (JRF). D2 designates the moment arm used by the contralateral-held load (CL). Refer to Figure 12-42 for background and other abbreviations. (To simplify the mathematics, the calculations assume that all force vectors are acting in a vertical direction. This assumption introduces modest error in the results. All moment arm directions are assigned positive values.) (From Neumann DA: Hip abductor muscle activity in persons with a hip prosthesis while carrying loads in one hand, Phys Ther 76:1320, 1996. With permission of the American Physical Therapy Association.)
As a general principle, persons with an unstable or painful hip should be advised to avoid or limit the carrying of any external loads. For most ambulatory persons, however, this advice is impractical. More practically, when loads must be carried, they should be as light as possible, carried in a backpack or by hand ipsilateral to the affected hip, or divided in half and carried bilaterally.13,124,125 Research has shown that a strategy of combining the use of a contralaterally held cane with an ipsilaterally held load (equal to or less than 15% of body weight) reduces the demands on the hip abductor muscles to a greater degree than either method implemented separately.122
The previous discussion focuses on methods that reduce the force demands on the hip abductor muscles as a means to reduce the force on a painful or an unstable hip. The same methods also apply to protecting an unstable hip associated with an arthroplasty (joint replacement). Although these methods may have their desired effect, the reduced functional demand placed on the hip may also perpetuate prolonged weakness in the hip abductor muscles, which in turn leads to deviations in gait.141 A study on a group of persons with hip osteoarthritis awaiting arthroplastic surgery reported a 31% average loss in hip abduction torque compared with aged-match controls.10 This loss in strength exceeded that of the hip flexors, extensors, and adductor muscles. Clinicians must meet the dual challenge of protecting a vulnerable hip from excessive and potentially damaging forces from the abductor muscles while simultaneously increasing the functional strength and endurance of these muscles. This requires knowledge of the normal and abnormal frontal plane mechanics of the hip, the pathology specific to the patient’s condition, and the symptoms that suggest the hip is being subjected to potentially damaging forces. These signs and symptoms include excessive pain, marked gait deviation, generalized hip instability, and abnormal positioning of the lower limb.
Surgical Intervention after Fracture or Osteoarthritis
A hip arthroplasty is often performed when a person with hip disease, most often osteoarthritis, has constant pain that significantly limits function and quality of life. This operation replaces the diseased or degenerated acetabulum and/or femoral head with biologically inert materials. The arthroplasty may totally replace or resurface the femoral head.133 A prosthetic hip may be secured by cement, or through biologic fixation provided by bone growth into the surface of the implanted components. Although the total hip arthroplasty is typically a successful procedure,114 premature loosening or dislocation of the femoral and/or acetabular component can be a postoperative problem.18,83,92,116 Large torsional loads between the prosthetic implant and the bony interface may contribute to the loss of fixation. Until sufficient long-term data emerge from clinical trials, debate regarding the most durable materials and effective methods of fixation and implantation continues.29,58,70,113
BIOMECHANICAL CONSEQUENCES OF COXA VARA AND COXA VALGA
As previously described in this chapter, the average angle of inclination of the femoral neck is approximately 125 degrees (see Figure 12-7, A). The angle may be changed as a result of a surgical repair of a fractured hip or the specific design of a prosthetic hip. In addition, a surgical operation known as a coxa vara (or valga) osteotomy intentionally alters a preexisting angle of inclination. This operation involves cutting a wedge of bone from the proximal femur, thereby changing the orientation of the femoral head to the acetabulum. A goal of this operation is often to improve the congruency of the weight-bearing surfaces of the hip (Figure 12-49).
Regardless of the type of and rationale for the hip surgery, changing the angle of inclination of the proximal femur alters the biomechanics of the joint. These alterations can have positive or negative biomechanical effects. Figure 12-50, A shows two potentially positive biomechanical effects of coxa vara. The varus position increases the moment arm of the hip abductor force (indicated by D′). The greater leverage increases the abduction torque produced per unit of hip abductor muscle force. This situation may benefit persons with hip abductor weakness. Also, increasing the leverage of the abductor muscles may allow a given level of abduction torque required during the stance phase of walking to be generated by less muscle force. Reducing the magnitude of muscular-based joint forces can help protect an arthritic or unstable prosthetic hip from excessive wear during walking. A varus osteotomy may in some patients improve the stability of the joint by aligning the femoral head more directly into the acetabulum.
A potentially negative effect of coxa vara is an increased bending moment (or torque) generated across the femoral neck (see Figure 12-50, B). The bending moment arm (dashed line indicated by I′) increases as the angle of inclination approaches 90 degrees. Increasing the bending moment raises the tension across the superior aspect of the femoral neck. This situation may cause a fracture of the femoral neck or a structural failure of a prosthesis. Marked coxa vara increases the vertical shear between the femoral head and the adjacent epiphysis. In children this situation may lead to a condition known as a slipped capital femoral epiphysis.100 Coxa vara may decrease the functional length of the hip abductor muscles, thereby reducing the force-generating capability of these muscles and increasing the likelihood of a “gluteus medius limp.” The loss in muscle force may offset the increased abduction torque potential gained by the increased hip abductor moment arm.
Coxa valga may result from a surgical intervention or from pathology such as hip dysplasia. A potentially positive effect of the valgus position is a decrease in bending moment arm across the femoral neck (see I″ in Figure 12-50, C). This situation also decreases the vertical shear across the femoral neck. The valgus position, however, may increase the functional length of the hip abductor muscles, thus improving their force-generating ability. In contrast, a potentially negative effect of coxa valga is the decreased moment arm available to the hip abductor force (indicated by D″ in Figure 12-50, D). In extreme coxa valga, the femoral head may be positioned more lateral to the acetabulum, possibly favoring dislocation.
REFERENCES
1. Ajemian, S, Thon, D, Clare, P, et al. Cane-assisted gait biomechanics and electromyography after total hip arthroplasty. Arch Phys Med Rehabil. 2004;85:1966–1971.
2. Altman, R, Alarcón, G, Appelrouth, D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–514.
3. Altman, RD, Bloch, DA, Dougados, M, et al. Measurement of structural progression in osteoarthritis of the hip: the Barcelona consensus group. Osteoarthritis Cartilage. 2004;12:515–524.
4. Anda, S, Svenningsen, S, Dale, LG, Benum, P. The acetabular sector angle of the adult hip determined by computed tomography. Acta Radiol Diagn (Stockh). 1986;27:443–447.
5. Andersson, E, Oddsson, L, Grundström, H, Thorstensson, A. The role of the psoas and iliacus muscles for stability and movement of the lumbar spine, pelvis and hip. Scand J Med Sci Sports. 1995;5:10–16.
6. Arnold, AS, Anderson, FC, Pandy, MG, Delp, SL. Muscular contributions to hip and knee extension during the single limb stance phase of normal gait: a framework for investigating the causes of crouch gait. J Biomech. 2005;38:2181–2189.
7. Arnold, AS, Asakawa, DJ, Delp, SL. Do the hamstrings and adductors contribute to excessive internal rotation of the hip in persons with cerebral palsy? Gait Posture. 2000;11:181–190.
8. Arnold, AS, Delp, SL. Rotational moment arms of the medial hamstrings and adductors vary with femoral geometry and limb position: implications for the treatment of internally rotated gait. J Biomech. 2001;34:437–447.
9. Arnold, AS, Komattu, AV, Delp, SL. Internal rotation gait: a compensatory mechanism to restore abduction capacity decreased by bone deformity. Dev Med Child Neurol. 1997;39:40–44.
10. Arokoski, MH, Arokoski, JP, Haara, M, et al. Hip muscle strength and muscle cross sectional area in men with and without hip osteoarthritis. J Rheumatol. 2002;29:2187–2195.
11. Beck, M, Kalhor, M, Leunig, M, Ganz, R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018.
12. Bergmann, G, Graichen, F, Rohlmann, A. Hip joint loading during walking and running, measured in two patients. J Biomech. 1993;26:969–990.
13. Bergmann, G, Graichen, F, Rohlmann, A, Linke, H. Hip joint forces during load carrying. Clin Orthop Relat Res. 1997;335:190–201.
14. Bizzini, M, Notzli, HP, Maffiuletti, NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35:1955–1959.
15. Blemker, SS, Delp, SL. Three-dimensional representation of complex muscle architectures and geometries. Ann Biomed Eng. 2005;33:661–673.
16. Bobroff, ED, Chambers, HG, Sartoris, DJ, et al. Femoral anteversion and neck-shaft angle in children with cerebral palsy. Clin Orthop Relat Res. 1999;364:194–204.
17. Boone, DC, Azen, SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61:756–759.
18. Bordini, B, Stea, S, De, CM, et al. Factors affecting aseptic loosening of 4750 total hip arthroplasties: multivariate survival analysis. BMC Musculoskelet Disord. 2007;8:69.
19. Broadhurst, NA, Simmons, DN, Bond, MJ. Piriformis syndrome: correlation of muscle morphology with symptoms and signs. Arch Phys Med Rehabil. 2004;85:2036–2039.
20. Burnett, RS, la Rocca, GJ, Prather, H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448–1457.
21. Cahalan, TD, Johnson, ME, Liu, S, Chao, EY. Quantitative measurements of hip strength in different age groups. Clin Orthop Relat Res. 1989;246:136–145.
22. Carey, TS, Crompton, RH. The metabolic costs of “bent-hip, bent-knee” walking in humans. J Hum Evol. 2005;48:25–44.
23. Clark, JM, Haynor, DR. Anatomy of the abductor muscles of the hip as studied by computed tomography. J Bone Joint Surg Am. 1987;69:1021–1031.
24. Coleman, SS. Congenital dysplasia of the hip in the Navajo infant. Clin Orthop Relat Res. 1968;56:179–193.
25. Congdon, R, Bohannon, R, Tiberio, D. Intrinsic and imposed hamstring length influence posterior pelvic rotation during hip flexion. Clin Biomech (Bristol, Avon). 2005;20:947–951.
26. Cooperman, DR, Wallensten, R, Stulberg, SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;175:79–85.
27. Crawford, JR, Villar, RN. Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br. 2005;87:1459–1462.
28. Crock, HV. An atlas of the arterial supply of the head and neck of the femur in man. Clin Orthop Relat Res. 1980;152:17–27.
29. Cuckler, JM. The rationale for metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2005;441:132–136.
30. Cummings, SR, Nevitt, MC. A hypothesis: the causes of hip fractures. J Gerontol. 1989;44:M107–M111.
31. Dalstra, M, Huiskes, R. Load transfer across the pelvic bone. J Biomech. 1995;28:715–724.
32. de Jong, PT, Haverkamp, D, van der Vis, HM, Marti, RK, et al. Total hip replacement with a superolateral bone graft for osteoarthritis secondary to dysplasia: a long-term follow-up. J Bone Joint Surg Br. 2006;88:173–178.
33. Delp, SL, Hess, WE, Hungerford, DS, Jones, LC. Variation of rotation moment arms with hip flexion. J Biomech. 1999;32:493–501.
34. Dewberry, MJ, Bohannon, RW, Tiberio, D, et al. Pelvic and femoral contributions to bilateral hip flexion by subjects suspended from a bar. Clin Biomech (Bristol, Avon). 2003;18:494–499.
35. Dostal, WF, Andrews, JG. A three-dimensional biomechanical model of hip musculature. J Biomech. 1981;14:803–812.
36. Dostal, WF, Soderberg, GL, Andrews, JG. Actions of hip muscles. Phys Ther. 1986;66:351–361.
37. Eastwood, EA, Magaziner, J, Wang, J, et al. Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc. 2002;50:1240–1249.
38. Eckstein, F, von Eisenhart-Rothe, R, Landgraf, J, et al. Quantitative analysis of incongruity, contact areas and cartilage thickness in the human hip joint. Acta Anat (Basel). 1997;158:192–204.
39. Elders, MJ. The increasing impact of arthritis on public health. J Rheumatol Suppl. 2000;60:6–8.
40. Enseki, KR, Martin, RL, Draovitch, P, et al. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36:516–525.
41. Escalante, A, Lichtenstein, MJ, Dhanda, R, et al. Determinants of hip and knee flexion range: results from the San Antonio Longitudinal Study of Aging. Arthritis Care Res. 1999;12:8–18.
42. Esola, MA, McClure, PW, Fitzgerald, GK, Siegler, S. Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine. 1996;21:71–78.
43. Fabry, G, MacEwen, GD, Shands, AR, Jr. Torsion of the femur. A follow-up study in normal and abnormal conditions. J Bone Joint Surg Am. 1973;55:1726–1738.
44. Ferguson, SJ, Bryant, JT, Ganz, R. An in vitro investigation of the acetabular labrum seal in hip joint mechanics. J Biomech. 2003;36:171–178.
45. Fischer, FJ, Houtz, SJ. Evaluation of the function of the gluteus maximus muscle. An electromyographic study. Am J Phys Med. 1968;47:182–191.
46. Freedman, BA, Potter, BK, Dinauer, PA, et al. Prognostic value of magnetic resonance arthrography for Czerny stage II and III acetabular labral tears. Arthroscopy. 2006;22:742–747.
47. Fuss, FK, Bacher, A. New aspects of the morphology and function of the human hip joint ligaments. Am J Anat. 1991;192:1–13.
48. Gajdosik, RL, Sandler, MM, Marr, HL. Influence of knee positions and gender on the Ober test for length of the iliotibial band. Clin Biomech (Bristol, Avon). 2003;18:77–79.
49. Ganz, R, Leunig, M, Leunig-Ganz, K, Harris, WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272.
50. Genda, E, Iwasaki, N, Li, G, et al. Normal hip joint contact pressure distribution in single-leg standing—effect of gender and anatomic parameters. J Biomech. 2001;34:895–905.
51. Gullberg, B, Johnell, O, Kanis, JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413.
52. Halbertsma, JP, Göeken, LN, Hof, AL, et al. Extensibility and stiffness of the hamstrings in patients with nonspecific low back pain. Arch Phys Med Rehabil. 2001;82:232–238.
53. Hansen, L, de Zee, M, Rasmussen, J, et al. Anatomy and biomechanics of the back muscles in the lumbar spine with reference to biomechanical modeling. Spine. 2006;31:1888–1899.
54. Hardcastle, P, Nade, S. The significance of the Trendelenburg test. J Bone Joint Surg Br. 1985;67:741–746.
55. Harris, WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33.
56. Hartig, DE, Henderson, JM. Increasing hamstring flexibility decreases lower extremity overuse injuries in military basic trainees. Am J Sports Med. 1999;27:173–176.
57. Heller, MO, Bergmann, G, Deuretzbacher, G, et al. Influence of femoral anteversion on proximal femoral loading: measurement and simulation in four patients. Clin Biomech (Bristol, Avon). 2001;16:644–649.
58. Helm, CS, Greenwald, AS. The rationale and performance of modularity in total hip arthroplasty. Orthopedics. 2005;28:S1113–S1115.
59. Herring, JA. Tachdjian’s pediatric orthopaedics, Vol 1. Philadelphia: Saunders, 2002.
60. Herring, JA. Tachdjian’s pediatric orthopaedics, Vol 3. Philadelphia: Saunders, 2002.
61. Hewitt, JD, Glisson, RR, Guilak, F, Vail, TP. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002;17:82–89.
62. Hicks, JL, Schwartz, MH, Arnold, AS, Delp, SL. Crouched postures reduce the capacity of muscles to extend the hip and knee during the single-limb stance phase of gait. J Biomech. 2008;41:960–967.
63. Hoaglund, FT, Steinbach, LS. Primary osteoarthritis of the hip: etiology and epidemiology. J Am Acad Orthop Surg. 2001;9:320–327.
64. Hodge, WA, Carlson, KL, Fijan, RS, et al. Contact pressures from an instrumented hip endoprosthesis. J Bone Joint Surg Am. 1989;71:1378–1386.
65. Hodges, PW, Richardson, CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997;77:132–142.
66. Hoeksma, HL, Dekker, J, Ronday, HK, et al. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip: a randomized clinical trial. Arthritis Rheum. 2004;51:722–729.
67. Hoy, MG, Zajac, FE, Gordon, ME. A musculoskeletal model of the human lower extremity: the effect of muscle, tendon, and moment arm on the moment-angle relationship of musculotendon actuators at the hip, knee, and ankle. J Biomech. 1990;23:157–169.
68. Huddleston, JM, Whitford, KJ. Medical care of elderly patients with hip fractures. Mayo Clin Proc. 2001;76:295–298.
69. Hummer, CD, MacEwen, GD. The coexistence of torticollis and congenital dysplasia of the hip. J Bone Joint Surg Am. 1972;54:1255–1256.
70. Huo, MH, Parvizi, J, Bal, BS, et al. What’s new in total hip arthroplasty. J Bone Joint Surg Am. 2008;90:2043–2055.
71. Hurwitz, DE, Foucher, KC, Andriacchi, TP. A new parametric approach for modeling hip forces during gait. J Biomech. 2003;36:113–119.
72. Inman, VT. Functional aspects of the abductor muscles of the hip. J Bone Joint Surg Am. 1947;29:607–619.
73. Inman, VT, Ralston, HJ, Todd, F. Human walking. Baltimore: Williams & Wilkins; 1981.
74. Inman, VT, Saunders, JB. Referred pain from skeletal structures. J Nerv Ment Dis. 1944;99:660–667.
75. Ito, K, Minka, MA, 2nd., Leunig, M, et al. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176.
76. Jette, AM, Delitto, A. Physical therapy treatment choices for musculoskeletal impairments. Phys Ther. 1997;77:145–154.
77. Johnston, RC, Smidt, GL. Hip motion measurements for selected activities of daily living. Clin Orthop Relat Res. 1970;72:205–215.
78. Keagy, RD, Brumlik, J, Bergan, JL. Direct electromyography of the psoas major muscle in man. J Bone Joint Surg Am. 1966;48:1377–1382.
79. Kelsey, JL. The epidemiology of diseases of the hip: a review of the literature. Int J Epidemiol. 1977;6:269–280.
80. Kendall, FP, McCreary, AK, Provance, PG. Muscles: testing and function, ed 4. Baltimore: Williams & Wilkins; 1993.
81. Kim, WY, Hutchinson, CE, Andrew, JG, Allen, PD. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. 2006;88:727–729.
82. Kim, YT, Azuma, H. The nerve endings of the acetabular labrum. Clin Orthop Relat Res. 1995;320:176–181.
83. Kinov, P, Leithner, A, Radl, R, et al. Role of free radicals in aseptic loosening of hip arthroplasty. J Orthop Res. 2006;24:55–62.
84. Krebs, DE, Elbaum, L, Riley, PO, et al. Exercise and gait effects on in vivo hip contact pressures. Phys Ther. 1991;71:301–309.
85. Kumagai, M, Shiba, N, Higuchi, F, et al. Functional evaluation of hip abductor muscles with use of magnetic resonance imaging. J Orthop Res. 1997;15:888–893.
86. Kurrat, HJ, Oberlander, W. The thickness of the cartilage in the hip joint. J Anat. 1978;126:145–155.
87. Lalonde, FD, Frick, SL, Wenger, DR. Surgical correction of residual hip dysplasia in two pediatric age-groups. J Bone Joint Surg Am. 2002;84:1148–1156.
88. Lavigne, M, Parvizi, J, Beck, M, et al. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66.
89. Leadbetter, RE, Mawer, D, Lindow, SW. Symphysis pubis dysfunction: a review of the literature. J Matern Fetal Neonatal Med. 2004;16:349–354.
90. Lee, RY, Wong, TK. Relationship between the movements of the lumbar spine and hip. Hum Mov Sci. 2002;21:481–494.
91. Lengsfeld, M, Pressel, T, Stammberger, U. Lengths and lever arms of hip joint muscles: geometrical analyses using a human multibody model. Gait Posture. 1997;6:18–26.
92. Lennon, AB, Britton, JR, MacNiocaill, RF, et al. Predicting revision risk for aseptic loosening of femoral components in total hip arthroplasty in individual patients—a finite element study. J Orthop Res. 2007;25:779–788.
93. Leunig, M, Beck, M, Woo, A, et al. Acetabular rim degeneration: a constant finding in the aged hip. Clin Orthop Relat Res. 2003;413:201–207.
94. Leunig, M, Podeszwa, D, Beck, M, et al. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74–80.
95. Lewis, CL, Sahrmann, SA. Acetabular labral tears. Phys Ther. 2006;86:110–121.
96. Lewis, CL, Sahrmann, SA, Moran, DW. Anterior hip joint force increases with hip extension, decreased gluteal force, or decreased iliopsoas force. J Biomech. 2007;40:3725–3731.
97. Li, Y, McClure, PW, Pratt, N. The effect of hamstring muscle stretching on standing posture and on lumbar and hip motions during forward bending. Phys Ther. 1996;76:836–845.
98. Lievense, AM, Bierma-Zeinstra, SM, Verhagen, AP, et al. Influence of sporting activities on the development of osteoarthritis of the hip: a systematic review. Arthritis Rheum. 2003;49:228–236.
99. Lindsay, DM, Maitland, ME, Lowe, RC. Comparison of isokinetic internal and external hip rotation torques using different testing positions. J Orthop Sports Phys Ther. 1992;16:43–50.
100. Loder, RT, Aronsson, DD, Dobbs, MB, et al. Slipped capital femoral epiphysis. Instr Course Lect. 2001;50:555–570.
101. Löhe, F, Eckstein, F, Sauer, T, Putz, R. Structure, strain and function of the transverse acetabular ligament. Acta Anat (Basel). 1996;157:315–323.
102. Lohmander, LS. Articular cartilage and osteoarthrosis. The role of molecular markers to monitor breakdown, repair and disease. J Anat. 1994;184:477–492.
103. MacDonald, CW, Whitman, JM, Cleland, JA, et al. Clinical outcomes following manual physical therapy and exercise for hip osteoarthritis: a case series. J Orthop Sports Phys Ther. 2006;36:588–599.
104. Mansour, JM, Pereira, JM. Quantitative functional anatomy of the lower limb with application to human gait. J Biomech. 1987;20:51–58.
105. Markhede, G, Stener, B. Function after removal of various hip and thigh muscles for extirpation of tumors. Acta Orthop Scand. 1981;52:373–395.
106. Martin, HD, Savage, A, Braly, BA, et al. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24:188–195.
107. Martin, RL, Enseki, KR, Draovitch, P, et al. Acetabular labral tears of the hip: examination and diagnostic challenges. J Orthop Sports Phys Ther. 2006;36:503–515.
108. Mavcic, B, Pompe, B, Antolic, V, et al. Mathematical estimation of stress distribution in normal and dysplastic human hips. J Orthop Res. 2002;20:1025–1030.
109. McCarthy, J, Noble, P, Aluisio, FV, et al. Anatomy, pathologic features, and treatment of acetabular labral tears. Clin Orthop Relat Res. 2003;406:38–47.
110. McCarthy, JC. The diagnosis and treatment of labral and chondral injuries. Instr Course Lect. 2004;53:573–577.
111. McCarthy, JC, Noble, PC, Schuck, MR, et al. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37.
112. McGibbon, CA, Krebs, DE, Mann, RW. In vivo hip pressures during cane and load-carrying gait. Arthritis Care Res. 1997;10:300–307.
113. Mehmood, S, Jinnah, RH, Pandit, H. Review on ceramic-on-ceramic total hip arthroplasty. J Surg Orthop Adv. 2008;17:45–50.
114. Montin, L, Leino-Kilpi, H, Suominen, T, Lepistö, J. A systematic review of empirical studies between 1966 and 2005 of patient outcomes of total hip arthroplasty and related factors. J Clin Nurs. 2008;17:40–45.
115. Moore, KL, Persaud, TVN. The developing human: clinically oriented embryology, ed 7. St Louis: Elsevier; 2003.
116. Münger, P, Röder, C, Ackermann-Liebrich, U, Busato, A. Patient-related risk factors leading to aseptic stem loosening in total hip arthroplasty: a case-control study of 5,035 patients. Acta Orthop. 2006;77:567–574.
117. Nakamura, J, Kamegaya, M, Saisu, T, et al. Treatment for developmental dysplasia of the hip using the Pavlik harness: long-term results. J Bone Joint Surg Br. 2007;89:230–235.
118. Narvani, AA, Tsiridis, E, Tai, CC, Thomas, P. Acetabular labrum and its tears. Br J Sports Med. 2003;37:207–211.
119. Nemeth, G, Ohlsen, H. Moment arms of the hip abductor and adductor muscles measured in vivo by computed tomography. Clin Biomech (Bristol, Avon). 1989;4:133–136.
120. Neumann, DA. Hip abductor muscle activity as subjects with hip prostheses walk with different methods of using a cane. Phys Ther. 1998;78:490–501.
121. Neumann, DA. Hip abductor muscle activity in persons with a hip prosthesis while carrying loads in one hand. Phys Ther. 1996;76:1320–1330.
122. Neumann, DA. An electromyographic study of the hip abductor muscles as subjects with a hip prosthesis walked with different methods of using a cane and carrying a load. Phys Ther. 1999;79:1163–1173.
123. Neumann, DA. Biomechanical analysis of selected principles of hip joint protection. Arthritis Care Res. 1989;2:146–155.
124. Neumann, DA, Cook, TM. Effect of load and carrying position on the electromyographic activity of the gluteus medius muscle during walking. Phys Ther. 1985;65:305–311.
125. Neumann, DA, Cook, TM, Sholty, RL, Sobush, DC. An electromyographic analysis of hip abductor muscle activity when subjects are carrying loads in one or both hands. Phys Ther. 1992;72:207–217.
126. Neumann, DA, Hase, AD. An electromyographic analysis of the hip abductors during load carriage: implications for hip joint protection. J Orthop Sports Phys Ther. 1994;19:296–304.
127. Neumann, DA, Soderberg, GL, Cook, TM. Comparison of maximal isometric hip abductor muscle torques between hip sides. Phys Ther. 1988;68:496–502.
128. Neumann, DA, Soderberg, GL, Cook, TM. Electromyographic analysis of hip abductor musculature in healthy right-handed persons. Phys Ther. 1989;69:431–440.
129. Noble, PC, Kamaric, E, Sugano, N, et al. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;417:27–40.
130. Notzli, HP, Wyss, TF, Stoecklin, CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560.
131. Odding, E, Valkenburg, HA, Stam, HJ, Hofman, A. Determinants of locomotor disability in people aged 55 years and over: the Rotterdam Study. Eur J Epidemiol. 2001;17:1033–1041.
132. Oguz, O. Measurement and relationship of the inclination angle, Alsberg angle and the angle between the anatomical and mechanical axes of the femur in males. Surg Radiol Anat. 1996;18:29–31.
133. Ong, KL, Kurtz, SM, Manley, MT, et al. Biomechanics of the Birmingham hip resurfacing arthroplasty. J Bone Joint Surg Br. 2006;88:1110–1115.
134. Paksima, N, Koval, KJ, Aharanoff, G, et al. Predictors of mortality after hip fracture: a 10-year prospective study. Bull NYU Hosp Jt Dis. 2008;66:111–117.
135. Palombaro, KM, Craik, RL, Mangione, KK, Tomlinson, JD. Determining meaningful changes in gait speed after hip fracture. Phys Ther. 2006;86:809–816.
136. Pare, EB, Stern, JT, Jr., Schwartz, JM. Functional differentiation within the tensor fasciae latae. A telemetered electromyographic analysis of its locomotor roles. J Bone Joint Surg Am. 1981;63:1457–1471.
137. Parkkari, J, Kannus, P, Palvanen, M, et al. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int. 1999;65:183–187.
138. Paton, RW, Hinduja, K, Thomas, CD. The significance of at-risk factors in ultrasound surveillance of developmental dysplasia of the hip. A ten-year prospective study. J Bone Joint Surg Br. 2005;87:1264–1266.
139. Peelle, MW, la Rocca, GJ, Maloney, WJ, et al. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333.
140. Penrod, JD, Litke, A, Hawkes, WG, et al. The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63:867–872.
141. Perron, M, Malouin, F, Moffet, H, McFadyen, BJ. Three-dimensional gait analysis in women with a total hip arthroplasty. Clin Biomech (Bristol, Avon). 2000;15:504–515.
142. Petersen, W, Petersen, F, Tillmann, B. Structure and vascularization of the acetabular labrum with regard to the pathogenesis and healing of labral lesions. Arch Orthop Trauma Surg. 2003;123:283–288.
143. Peyron, JG. Osteoarthritis. The epidemiologic viewpoint. Clin Orthop Relat Res. 1986;213:13–19.
144. Pfirrmann, CW, Chung, CB, Theumann, NH, et al. Greater trochanter of the hip: attachment of the abductor mechanism and a complex of three bursae—MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001;221:469–477.
145. Pohtilla, JF. Kinesiology of hip extension at selected angles of pelvifemoral extension. Arch Phys Med Rehabil. 1969;50:241–250.
146. Ralis, Z, McKibbin, B. Changes in shape of the human hip joint during its development and their relation to its stability. J Bone Joint Surg Br. 1973;55:780–785.
147. Recnik, G, Kralj-Iglic, V, Iglic, A, et al. Higher peak contact hip stress predetermines the side of hip involved in idiopathic osteoarthritis. Clin Biomech (Bristol, Avon). 2007;22:1119–1124.
148. Reikeras, O, Bjerkreim, I, Kolbenstvedt, A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54:18–23.
149. Rethlefsen, SA, Healy, BS, Wren, TA, et al. Causes of intoeing gait in children with cerebral palsy. J Bone Joint Surg Am. 2006;88:2175–2180.
150. Roach, KE, Miles, TP. Normal hip and knee active range of motion: the relationship to age. Phys Ther. 1991;71:656–665.
151. Roddy, E, Zhang, W, Doherty, M, et al. Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee—the MOVE consensus. Rheumatology (Oxford). 2005;44:67–73.
152. Rozumalski, A, Schwartz, MH, Wervey, R, et al. The in vivo three-dimensional motion of the human lumbar spine during gait. Gait Posture. 2008;28:378–384.
153. Rydell, N. Biomechanics of the hip-joint. Clin Orthop Relat Res. 1973;92:6–15.
154. Santaguida, PL, McGill, SM. The psoas major muscle: a three-dimensional geometric study. J Biomech. 1995;28:339–345.
155. Siebenrock, KA, Schoeniger, R, Ganz, R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A:278–286.
156. Simoneau, GG, Hoenig, KJ, Lepley, JE, Papanek, PE. Influence of hip position and gender on active hip internal and external rotation. J Orthop Sports Phys Ther. 1998;28:158–164.
157. Skyrme, AD, Cahill, DJ, Marsh, HP, Ellis, H. Psoas major and its controversial rotational action. Clin Anat. 1999;12:264–265.
158. Snijders, CJ, Hermans, PF, Kleinrensink, GJ. Functional aspects of cross-legged sitting with special attention to piriformis muscles and sacroiliac joints. Clin Biomech (Bristol, Avon). 2006;21:116–121.
159. Soderberg, GL, Dostal, WF. Electromyographic study of three parts of the gluteus medius muscle during functional activities. Phys Ther. 1978;58:691–696.
160. Standring, S. Gray’s anatomy: the anatomical basis of clinical practice, ed 40. St Louis: Elsevier; 2009.
161. Stansfield, BW, Nicol, AC. Hip joint contact forces in normal subjects and subjects with total hip prostheses: walking and stair and ramp negotiation. Clin Biomech (Bristol, Avon). 2002;17:130–139.
162. Stewart, K, Edmonds-Wilson, R, Brand, R, Brown, TD. Spatial distribution of hip capsule structural and material properties. J Biomech. 2002;35:1491–1498.
163. Svenningsen, S, Apalset, K, Terjesen, T, Anda, S. Regression of femoral anteversion. A prospective study of intoeing children. Acta Orthop Scand. 1989;60:170–173.
164. Tan, V, Seldes, RM, Katz, MA, et al. Contribution of acetabular labrum to articulating surface area and femoral head coverage in adult hip joints: an anatomic study in cadavera. Am J Orthop. 2001;30:809–812.
165. Tanzer, M, Noiseux, N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177.
166. Thelen, DD, Riewald, SA, Asakawa, DS, et al. Abnormal coupling of knee and hip moments during maximal exertions in persons with cerebral palsy. Muscle Nerve. 2003;27:486–493.
167. Toussant, EM, Kohia, M. A critical review of literature regarding the effectiveness of physical therapy management of hip fracture in elderly persons. J Gerontol A Biol Sci Med Sci. 2005;60:1285–1291.
168. Walheim, GG, Selvik, G. Mobility of the pubic symphysis. In vivo measurements with an electromechanic method and a roentgen stereophotogrammetric method. Clin Orthop Relat Res. 1984;191:129–135.
169. Walters, J, Solomons, M, Davies, J. Gluteus minimus: observations on its insertion. J Anat. 2001;198:239–242.
170. Wehren, LE, Magaziner, J. Hip fracture: risk factors and outcomes. Current Osteoporosis Reports. 2003;1:78–85.
171. Weinstein, SL, Mubarak, SJ, Wenger, DR. Developmental hip dysplasia and dislocation: Part I. Instr Course Lect. 2004;53:523–530.
172. Weinstein, SL, Mubarak, SJ, Wenger, DR. Developmental hip dysplasia and dislocation: Part II. Instr Course Lect. 2004;53:531–542.
173. Wenger, DE, Kendell, KR, Miner, MR, Trousdale, RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150.
174. Wilkins, K. Health care consequences of falls for seniors. Health Rep. 1999;10:47–55.
175. Wingstrand, H, Wingstrand, A, Krantz, P. Intracapsular and atmospheric pressure in the dynamics and stability of the hip. A biomechanical study. Acta Orthop Scand. 1990;61:231–235.
176. Winter, DA. Biomechanics and motor control of human movement. New Jersey: John Wiley & Sons; 2005.
177. Winters, MV, Blake, CG, Trost, JS, et al. Passive versus active stretching of hip flexor muscles in subjects with limited hip extension: a randomized clinical trial. Phys Ther. 2004;84:800–807.
178. Wisniewski, SJ, Grogg, B. Femoroacetabular impingement: an overlooked cause of hip pain. Am J Phys Med Rehabil. 2006;85:546–549.
179. Wolinsky, FD, Fitzgerald, JF, Stump, TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health. 1997;87:398–403.
180. Woodley, SJ, Nicholson, HD, Livingstone, V, et al. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. J Orthop Sports Phys Ther. 2008;38:313–328.
181. Yoshio, M, Murakami, G, Sato, T, et al. The function of the psoas major muscle: passive kinetics and morphological studies using donated cadavers. J Orthop Sci. 2002;7:199–207.
STUDY QUESTIONS
1. What structures convert the greater sciatic notch to a foramen? List three structures (nerves or muscles) that pass through this foramen.
2. A patient has excessive anteversion of the femur and acetabulum. Which extreme hip motion (in the horizontal plane) would most likely be associated with a spontaneous anterior dislocation?
3. What characteristics define the close-packed position of the hip? How do these characteristics differ from those of most other synovial joints of the body?
4. Explain why a patient with an inflamed capsule of the hip joint may be susceptible to a hip flexion contracture.
5. Describe how the ischiofemoral ligament becomes taut in full internal rotation and extension of the hip. Include both femoral-on-pelvic and pelvic-on-femoral perspectives in your description.
6. While standing, a person performs a full posterior pelvic tilt while keeping the trunk essentially stationary. Describe how this movement could indirectly alter the tension in the anterior longitudinal ligament and the ligamentum flavum in the lumbar region.
7. Using a ruler and Figure 12-29 as a reference, which muscle appears to have the greatest moment arm for hip abduction?
8. Based on Figure 12-34, which muscle has (a) the least leverage and (b) the greatest leverage for producing internal rotation torque?
9. A patient sustained a severe fracture of the femoral head and the acetabulum, with marked reduction in contact area between the articular surfaces of the joint. As part of the reconstructive surgery, the surgeon decides to slightly increase the internal moment arm of the hip abductor muscles. What is the likely rationale for this procedure?
10. Explain how a reduced center-edge angle of the acetabulum could favor a dislocation of the hip.
11. Contrast the arthrokinematics of (femoral-on-pelvic) hip flexion and extension with those of internal and external rotation.
12. As indicated in Figure 12-12, during the swing phase of walking the hip experiences (compression) forces of about 10% to 20% of body weight. What causes this force?
13. Figure 12-22, A shows a seated person performing a 30-degree anterior pelvic tilt. What structure(s) is (are) most likely responsible for determining the end-range of this motion?
14. A person sustained an injury of the cauda equina resulting in reduced function of spinal nerve roots L3 and below. What pattern of muscular tightness may develop without adequate physical therapy intervention? (Consult Appendix IV, Part A, for assistance in responding to this question.)
15. Justify how bilateral tightness in the adductor longus and brevis could contribute to excessive lumbar lordosis during standing.
 Answers to the study questions can be found on the Evolve website.
Answers to the study questions can be found on the Evolve website.