Hip
The hip joint is one of the largest and most stable joints in the body. If it is injured or exhibits pathology, the lesion is usually immediately perceptible during walking. Because pain from the hip can be referred to the sacroiliac joints or the lumbar spine, it is imperative—unless there is evidence of direct trauma to the hip—that these joints be examined along with the hip.
Applied Anatomy
The hip joint is a multiaxial ball-and-socket joint that has maximum stability because of the deep insertion of the head of the femur into the acetabulum (Figure 11-1). The femoral head is much more stable in the acetabulum for the hip than the humerus is in the glenoid for the shoulder. To allow sufficient movement and proper alignment to occur at the hip joint, the femur has a longer neck than the humerus and is anteverted (Figure 11-2).
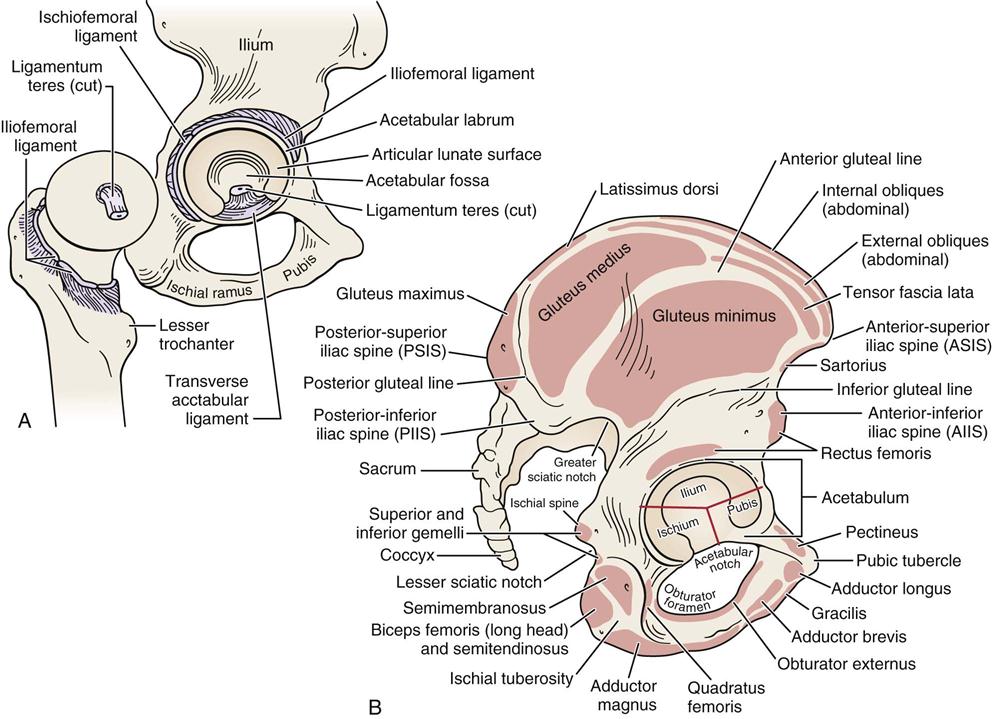
A, The right hip opened to show its internal components. B, Side view of right innominate bone (pelvis) showing muscle attachments. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, CV Mosby, pp. 388, 397.)
In addition, the hip, like the shoulder, has a labrum, which helps to deepen and stabilize the joint.1,2 The acetabular labrum increases the articular surface area of the acetabulum and volume, and it creates a seal for the central compartment, which is part of the intra-articular hip joint. The seal resists distraction of the femoral head from the socket by maintaining a negative pressure and resists fluid flow that enhances nutrition of the hip articular cartilage, which in turn provides a smooth gliding surface.3,4 The joint has a strong capsule and very strong muscles that control its actions (Figure 11-3). The acetabulum is formed by fusion of part of the ilium, ischium, and pubis, which taken as a group are sometimes called the innominate bone or pelvis. The acetabulum opens outward, forward, and downward. It is half of a sphere, and the femoral head is two thirds of a sphere. The hip, already a stable joint because of its bony configuration, is supported by three strong ligaments: the iliofemoral, the ischiofemoral, and the pubofemoral ligaments (Figure 11-4). The iliofemoral ligament (Y ligament of Bigelow) is considered to be the strongest ligament in the body. It is positioned to prevent excessive extension and plays a significant role in stabilizing and in maintaining upright posture at the hip while limiting anterior translation. The acetabular labrum plays a secondary role in stabilizing the hip during lateral rotation while preventing anterior translation.5 The ischiofemoral ligament, the weakest of these three strong ligaments, winds tightly on extension, helping to stabilize the hip in extension. The pubofemoral ligament prevents excessive abduction of the femur and limits extension. All three ligaments also limit medial rotation of the femur. A fourth ligament of the hip that sometimes is injured is the ligamentum teres or “ligament of the head,” which provides a physical attachment of the head of the femur to the acetabulum.6
Under low loads, the joint surfaces are incongruous; under heavy loads, they become congruous, providing maximum surface contact. The maximum contact brings the load per unit area down to a tolerable level. Depending on the activity, the forces exerted on the hip will vary.7
When considering movement or kinematics at the hip joint, one must consider whether the pelvis is moving on stationary femur (weight-bearing) or the femur (non–weight-bearing) is moving on the pelvis (Figure 11-5).
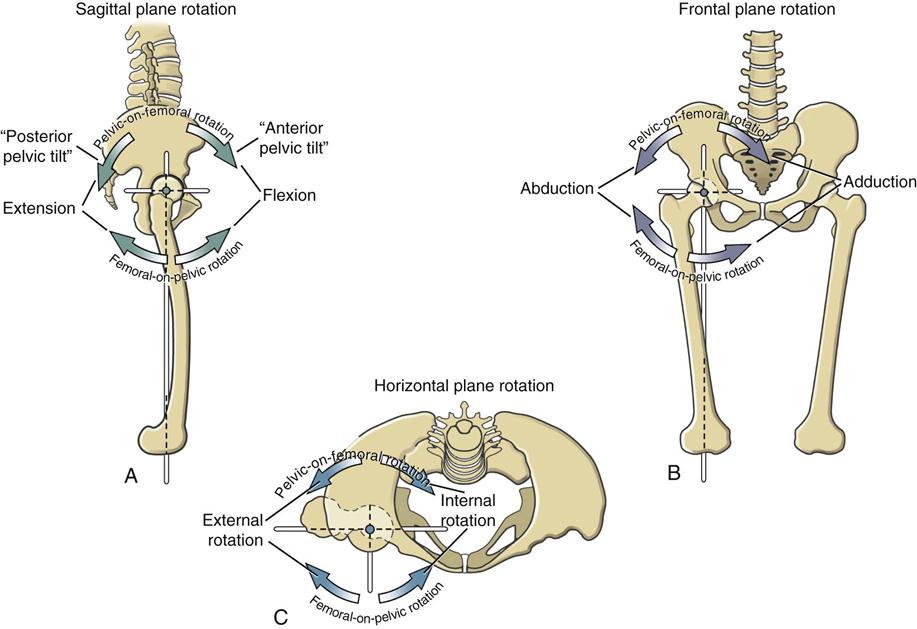
Femoral-on-pelvic and pelvic-on-femoral rotations occur in three planes. The axis of rotation for each plane of movement is shown as a colored dot, located at the center of the femoral head. A, Side view shows sagittal plane rotations around a medial-lateral axis of rotation. B, Front view shows frontal plane rotations around an anterior-posterior axis of rotation. C, Top view shows horizontal plane rotations around a longitudinal, or vertical, axis of rotation. (From Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2010, Mosby, p. 477.)
Patient History
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
2. If trauma was involved, what was the mechanism of injury? Did the patient land on the outside of the hip (e.g., trochanteric bursitis) or land on or hit the knee, thus jarring the hip (e.g., subluxation, acetabular labral tear)? Was the patient involved in repetitive loading activity (e.g., femoral stress fracture) or osteoporotic (insufficiency injury)?8 A careful determination of the mechanism of injury often leads to a diagnosis of the problem. Mechanical hip problems are reported as symptoms getting worse with activity, twisting movements are painful, sitting is uncomfortable (hip flexion), getting up from sitting may cause catching, ascending and descending stairs are difficult as is getting in and out of an automobile, and the patient may have difficulty putting on shoes and/or socks.9,10
3. What are the details of the present pain and other symptoms (Table 11-1)?11 Hip intra-articular pain, including labral tears and anterior impingement, is felt mainly in the groin and along the front or medial side of the thigh to the knee,1,12 whereas buttock pain is associated with posterior labral tears and lumbar spine problems.1,13 Adductor pain may be the result of overactive adductors caused by pelvic instability.14 Pain may also be referred to the hip area from several structures (Figure 11-6). Pain from the lumbar spine may commonly be referred to the back or lateral aspect of the hip.
A sports hernia, which is commonly caused by a deficient inguinal canal posterior wall, nerve entrapment or adductor tendonopathies, may have an insidious onset of unilateral dull, aching pain in the groin that may be sharp or burning and may radiate into the proximal thigh, low back, lower abdominal muscles, perineum and/or scrotum. The symptoms are aggravated by sudden acceleration, cutting, or kicking.15–18
Lateral hip pain may be due to a trochanteric bursitis or tear of the gluteus medius tendon, most commonly in older patients.19 Lateral hip pain may also simulate L4 nerve root pain; therefore, assessment of the back should also be considered for lateral or posterior symptoms. Hip pain may also be referred to the knee or back and may increase on walking. Clicking is common with labral tears.20,21 Snapping in and around the hip (coxa saltans) has many causes (Table 11-2). First and most commonly, it may be caused by slipping of the iliopsoas tendon over the osseous ridge of the lesser trochanter or anterior acetabulum, or the iliofemoral ligament may be riding over the femoral head.22–24 Some call this internal snapping. If due to the iliopsoas tendon or iliofemoral ligament, the snapping often occurs at approximately 45° of flexion when the hip is moving from flexion to extension, especially with the hip abducted and laterally rotated (snapping hip sign or extension test).25 The snap, which may be accompanied by pain or a jerk, is palpated anteriorly in the inguinal region.25,26 Second, the snapping may be caused by a tight iliotibial band or gluteus maximus tendon riding over the greater trochanter of the femur.22,23 This is sometimes called external snapping. This snapping or popping, which tends to be felt more lateral, occurs during hip flexion and extension, especially if the hip is held in medial rotation, and may be made worse if the trochanteric bursa is inflamed.26 The third cause of a snapping hip is acetabular labral tears or loose bodies, which may be the result of trauma or degeneration.23,27–29 This is sometimes referred to as intra-articular snapping. In this case, the patient (commonly between 20 to 40 years) complains of a sharp pain into the groin and anterior thigh, especially on pivoting movements. Passively, clicking may be felt and heard when the extended hip is adducted and laterally rotated.23,26 Each of these conditions may be referred to as snapping hip syndrome.
4. Is the condition improving? Worsening? Staying the same? Such a question gives the examiner some idea of the present state of the joint and pathology. Table 11-3 outlines criteria for osteoarthritis in patients with hip pain.30
5. Does any type of activity ease the pain or make it worse? For example, trochanteric bursitis often results from abnormal running mechanics with the feet crossing midline (increased adduction), wide pelvis and genu valgum, or running on tracks with no banking.26
8. Is there any past medical and/or surgical history, such as developmental disorders (e.g., hip dysplasia, Legg-Calvé-Perthes disease), systemic illnesses, metabolic, or inflammatory disorders?12 A history of alcohol, steroid or tobacco use can increase the risk of osteonecrosis.12
TABLE 11-1
| Type of Pain | Possible Causes |
| Dull, deep, aching | Arthritis, Paget disease |
| Sharp, intense, sudden, associated with weight bearing | Fracture |
| Tingling that radiates | Radiculopathy, spinal stenosis, meralgia paresthetica |
| Increased pain while sitting with the affected leg crossed | Trochanteric bursitis |
| Pain at sitting, legs not crossed | Ischiogluteal bursitis |
| Pain after standing, walking | Hip arthrosis |
| Pain on attempted weight bearing | Occult fracture, severe arthrosis |
| Unremitting, long duration | Paget disease, metastatic carcinoma, severe arthrosis (occasionally) |
From Schon L, Zuckerman JD: Hip pain in the elderly: evaluation and diagnosis. Geriatrics 43:58, 1988.
TABLE 11-2
Causes of Snapping Hip (Coxa Saltans) Symptoms
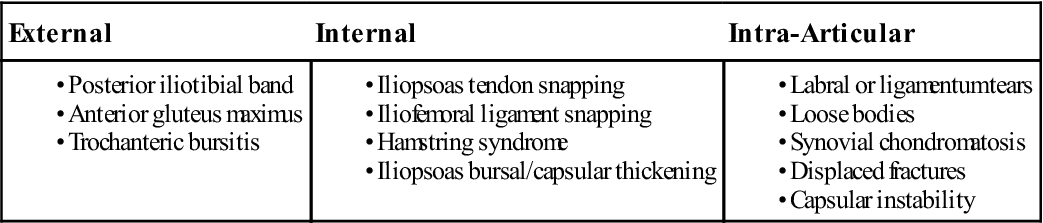
From Wahl CJ, Warren RF, Adler RS, et al: Internal coxa saltans (snapping hip) as a result of overtraining. Am J Sports Med 32:1303, 2004.
TABLE 11-3
Classification Criteria for Osteoarthritis of the Hip
| Clinical (history, physical examination, laboratory) classification criteria for osteoarthritis of the hip, classification tree format* | |
| Combined clinical (history, physical examination, laboratory) and radiographic classification criteria for osteoarthritis of the hip, traditional format** | Hip pain, and at least two of the following three features: |
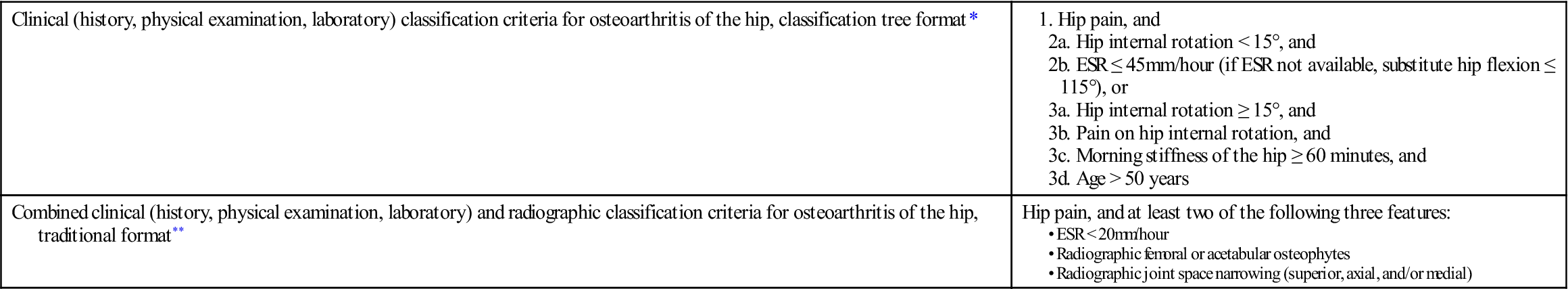
ESR, Erythrocyte sedimentation rate (Westergren).
*This classification method yields a sensitivity of 86% and a specificity of 75%.
**This classification method yields a sensitivity of 89% and a specificity of 91%.
Modified from Altman R, Alarcon G, Appelrouth D, et al.: The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arth Rheum 34:511–512, 1991.
Observation
As the patient comes into the assessment area, the gait should be observed. If the hip is affected, the weight is lowered carefully on the affected side and the knee bends slightly to absorb the shock. The length of the step on the affected side is shorter so that weight can be taken off the leg quickly. If the hip is stiff, the entire trunk and affected leg swing forward together. It is also important to watch for “balance” of the pelvis on the hip. In standing, the patient commonly has the hip slightly flexed if there is pain in the hip.
Pathology in the hip region can lead to tight adductors, iliopsoas, piriformis, tensor fasciae latae, rectus femoris, and hamstrings while, at the same time, the gluteus maximus, medius, and minimus become weak.31,32 Weak abductors can lead to a Trendelenburg gait or an “abductor lurch.” Internal hip pathology or a flexion contracture may lead to a “pelvic wink.” This is excessive rotation in the axial plane (more than 40°) toward the affected hip in an attempt by the patient to obtain terminal hip extension.33 If there is an imbalance of the flexors or extensors in the sagittal plane, the forward–backward motion of the trunk is altered to help maintain balance. For example, a bilateral hip flexion contracture causes the lumbar spine to extend to a greater degree (increased lordosis) as a compensating mechanism. Weak extensors cause the patient to move the trunk backward to maintain balance and avoid falling as a result of the unopposed action of the flexors. If the lateral rotators are significantly stronger than the medial rotators, as is normally the case, excessive toe-out can result. In addition, the patellae may have a “frog eyes” appearance (turn-out). Contracture of either of the rotators may lead to a pivoting at the hip during gait.34 The different types of gait are discussed in greater detail in Chapter 14.
If the patient uses a cane, it should be held in the hand opposite the affected side to negate some of the force of gravity on the affected hip.35 The use of a cane can decrease the load on the hip by as much as 40%.35,36
The patient should be standing and suitably undressed for the examiner to perform a proper observation. The following aspects are noted from the front, side, and behind:
1. Posture: The examiner should watch for pelvic obliquity caused by, for example, unequal leg length, muscle contractures, or scoliosis (see Chapter 15 for more details). It must be remembered that injury to iliopsoas may also affect the spine. Therefore, when asking patients to do movements involving these muscles, the examiner must watch the effect on the spine and spinal movement (see the “Thomas Test” section later in this chapter). Tightness of the iliopsoas can cause deviation of the spine to the same side.37
3. Balance: It is important to check the patient’s proprioceptive control in the joints being assessed. This control may be evaluated by asking the patient to balance first on one leg (the good one) and then the other leg—first with the eyes open, and then with the eyes closed. Differences should be noted through comparison. Loss of proprioceptive control is especially obvious when the patient’s eyes are closed. The use of the stork standing test34 (Figure 11-7) has also been advocated for testing proprioception. This test may also test stability at the sacroiliac joints, the knee, and the ankle and foot. With both methods, the examiner should watch for a positive Trendelenburg sign, which would negate the proprioceptive tests.
5. Any obvious shortening of a leg: Shortening of the leg may be demonstrated by a spinal scoliosis if the shortening is present in only one lower limb. Shortening may be structural or functional. Structural changes at the hip that may lead to altered limb length include hip angulation deformity, congenital hypoplasia, femoral growth plate problems and developmental disorders.12 If the hips are unstable (e.g., bilateral unreduced congenital dislocation of the hip [CDH]), an increased lumbar lordosis may be evident because the head of the femur usually rests above and behind the acetabulum, causing the patient to have an increased lordosis to maintain the center of gravity.
6. Color and texture of the skin
8. The patient’s willingness to move: If the hip is painful, the patient has an antalgic gait (see Chapter 14) and does not want to move the hip. If the hip is unstable, the patient has more difficulty controlling its movement.

Anterior View
The examiner should note any abnormality of the bony and soft-tissue contours. With many patients, differences in these contours are difficult to detect because of muscle bulk and other soft-tissue deposition around the hips. The examiner must, therefore, look closely. The same is true for swelling. Swelling in the hip joint itself is virtually impossible to detect by observation, and swelling resulting from a psoas or trochanteric bursitis can easily be missed if the examiner is not carefully observant.
Lateral View
While the patient is viewed from the side, the contour of the buttock should be observed for any abnormality (gluteus maximus atrophy or atonia). In addition, a hip flexion deformity is best observed from this position. The examiner should take the time to compare the two sides and note any subtle differences.
Posterior View
The position of the hip and the effect, if any, of this position on the spine should be noted. For example, a hip flexion contracture may lead to an increased lumbar lordosis. Any differences in bony and soft-tissue contours should again be noted.
Examination
When doing an examination of the hip, the examiner must keep in mind that pain may be referred to the hip from the sacroiliac joints or the lumbar spine, and vice versa. Therefore, the examination may be an extensive one. If there is any doubt as to the location of the lesion, an assessment of the lumbar spine and sacroiliac joints should be performed along with the hip. It is only through a careful examination of the three areas, especially if there has been no history of trauma, that the examiner can discern the location of the lesion.
As with any examination, the examiner should compare one side of the body with the other, noting any differences. This comparison is necessary because of the individual differences among normal people.
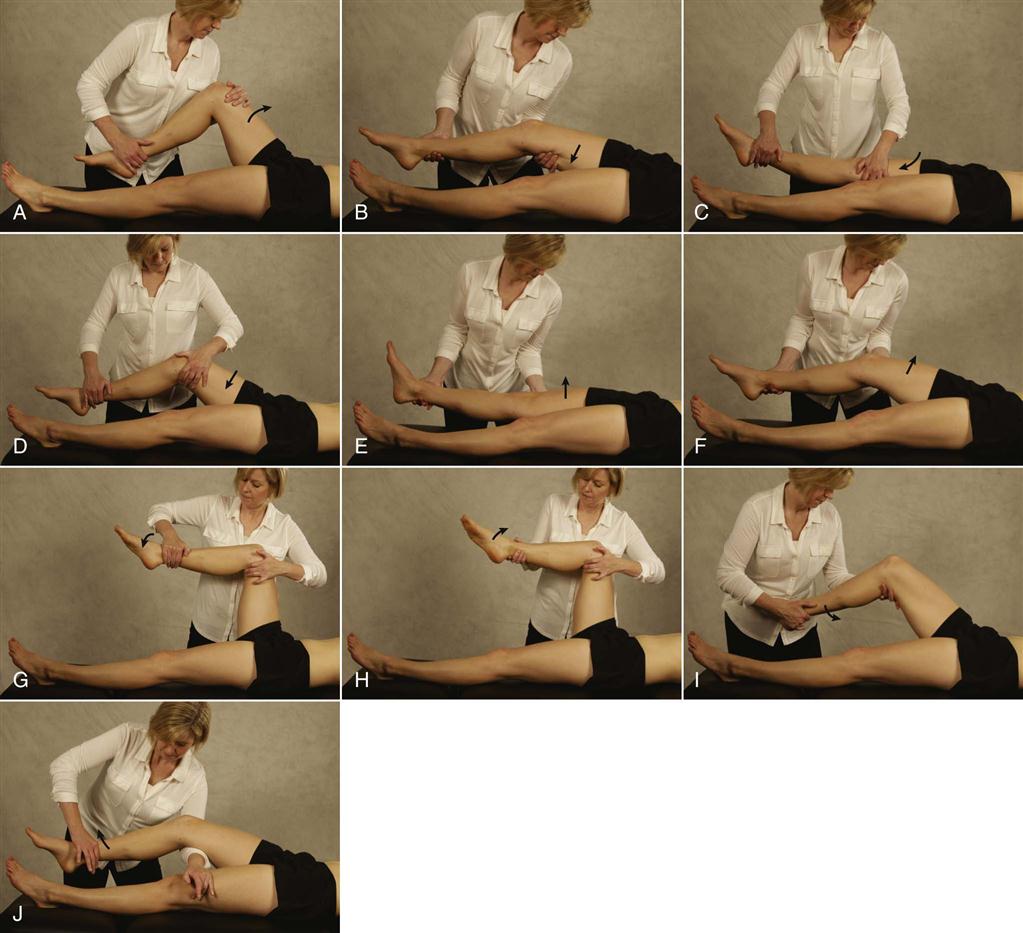
Active Movements
The active movements (Figure 11-8) are done in such a way that the most painful ones are done last. To keep movement of the patient to a minimum, some movements are tested with the patient in the supine position, and others are tested in the prone position. For ease of description, the movements are described together. The examiner should follow the order as stated in the précis at the end of the chapter when examining the patient. If the history has indicated that repetitive movements, sustained postures, or combined movements have caused symptoms, the examiner should ensure that these movements are tested as well. For example, sustained extension of the hip may provoke gluteal pain in the presence of claudication in the common or internal iliac artery.38 During the active movements, the examiner should always watch for the possibility of muscle or force-couple imbalances that lead to abnormal muscle recruitment patterns. For example, during extension, the normal pattern is contraction of the gluteus maximus followed by the erector spinae on the opposite side and the hamstrings (depending on the load being extended). If the erector spinae contract first, the pelvis rotates anteriorly and hyperextension of the lumbar spine occurs. When doing the active movements, the examiner should watch the pelvis and the anterior superior (supine) and posterior superior (prone) iliac spines. During hip movement, if the pelvic force-couples are normal, the pelvis and anterior superior iliac spine (ASIS)/posterior superior iliac spine (PSIS) will not move. If they do, it may be an indication of muscle imbalance (Figure 11-9).
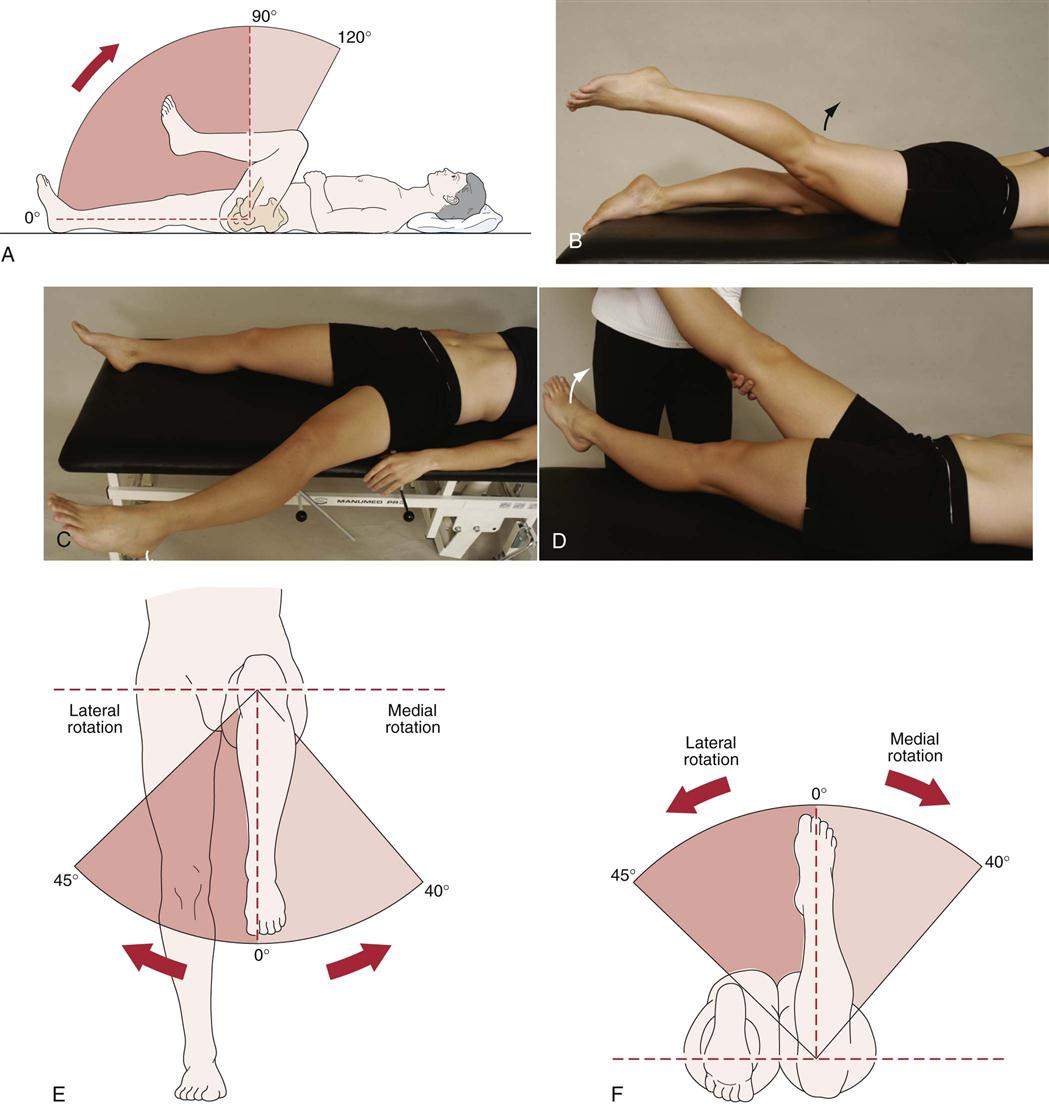
 Figure 11-8 Active movements of the hip.
Figure 11-8 Active movements of the hip.A, Flexion. B, Extension. C, Abduction. D, Adduction. E, Rotation in the supine position. F, Rotation in the prone position. (A, E, and F, Redrawn from Beetham WP, Polley HF, Slocumb CH, et al: Physical examination of the joints, Philadelphia, 1965, WB Saunders, pp. 134, 137, and 138, respectively.)
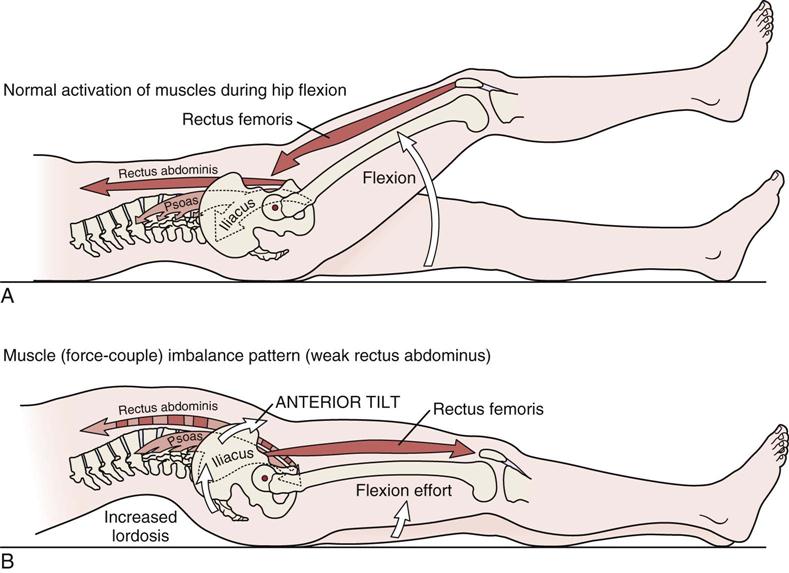
A, With normal activation of the rectus abdominis and the hip flexors (psoas and rectus femoris), the pelvis is stabilized and prevented from anterior tilting by the pull of the hip flexor muscles. B, With reduced activation of the rectus abdominis, contraction of the hip flexor muscles causes a marked anterior tilt of the pelvis. Note the increase in lumbar lordosis that accompanies the anterior tilt of the pelvis. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, CV Mosby, p. 413.)
Flexion of the hip is tested in the supine position and normally ranges from 110° to 120° with the knee flexed. If the ASIS begins to move, the movement is stopped because pelvic rotation is occurring rather than hip flexion. The patient’s knee is flexed during the test to prevent limitation of movement caused by hamstring tightness. If sharp anterior groin pain that may refer to the gluteal or trochanteric region is elicited on full flexion, adduction and medial rotation, the pain may be the result of anterior impingement of the femoral neck against the acetabular rim.39–45 The pain is made worse by certain movements (e.g., pivoting, movement into extreme rotation) or long periods of sitting, standing or walking.46 This femoroacetabular impingement (FAI) (Figure 11-10) may be cam type or pincer type. Both types are usually associated with femoral head (e.g., Legg-Calvé-Perthes disease, slipped capital femoral epiphysis) or acetabular dysplasia.47–52 The cam type impingement (see Figure 11-10, B) is commonly due to impingement of a large aspherical femoral head in a tight acetabulum. The deformed (flattened) head (pistol grip deformity or head tilt deformity) leads to shearing of the labrum and acetabular cartilage.53 The cam type impingement may also lead to increased stress at the symphysis pubis and may be a precursor to athletic pubalgia.54 Pincer type impingement (see Figure 11-10, C) is due to over coverage of the humeral head by a prominent acetabular rim (i.e., the acetabulum overhangs the femoral head due to acetabular dysplasia, acetabular retroversion, or coxa profunda) leading to pinching of the femoral neck against the labrum with the same ultimate result as the cam type degeneration of the labrum and adjacent cartilage.55–57 In the presence of acetabular retroversion or decreased femoral anteversion, hip flexion in the neutral line is limited to as little as 90° but full range is accomplished if the hip is allowed to laterally rotate and abduct. Lateral rotation may exceed 60° with medial rotation limited.49,58 The examiner should palpate the ASIS when testing hip movements. In the presence of FSI, the ASIS moves early due to limited hip flexion as the lumbar spine flexes to allow more movement.59 If medial rotation is measured at 90° flexion, medial rotation in the FSI patient will be limited.59 During the movement, if the abdominals are weak, the pelvis rotates anteriorly (see Figure 11-8). If the hip flexors are weak, the pelvis rotates posteriorly.
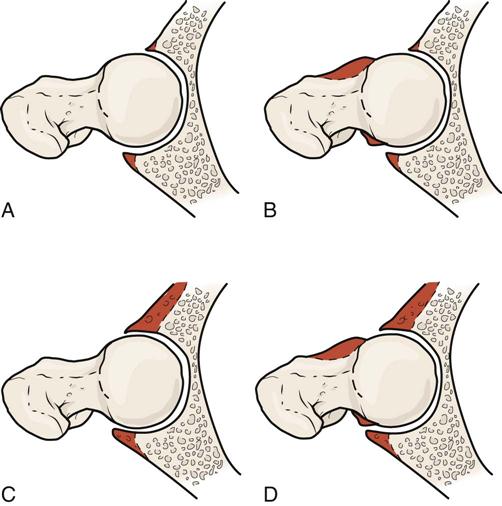
A, Normal hip. B, Reduced femoral head-neck offset (cam-type impingement). C, Excessive overcoverage of the femoral head (pincer-type impingement). D, Combination of cam and pincer types of impingement.
Extension of the hip normally ranges from 0° to 15°. The patient is in the prone position, and the examiner must differentiate between hip extension and spinal extension. Patients often have a tendency to extend the lumbar spine at the same time that they are extending the hip, giving the appearance of increased hip extension. Elevation of the pelvis or superior movement of the PSIS indicates the patient has passed the end of hip extension.
Hip abduction normally ranges from 30° to 50° and is tested with the patient in the supine position. Before asking the patient to do the abduction or adduction movement, the examiner should ensure that the patient’s pelvis is “balanced” or level, with the ASISs being level and the legs being perpendicular to a line joining the two ASISs. The patient is then asked to abduct one leg at a time. Abduction is stopped when the pelvis begins to move. Normally, the patient should be able to do hip abduction while the lower extremities, pelvis, trunk and shoulders remain aligned in the frontal plane.60 Pelvic motion is detected by palpation of the ASIS and by telling the patient to stop the movement as soon as the ASIS on either side starts to move. Normally, the ASIS on the movement side elevates while the opposite ASIS may drop or elevate. When the patient abducts the leg, the opposite ASIS tends to move first; with an adduction contracture, this occurs earlier in the range of movement.
If, during abduction, lateral rotation and slight flexion occurs early in the movement, the tensor fascia lata may be stronger and gluteus medius/minimus weak. If lateral rotation occurs later in the ROM, the iliopsoas or piriformis may be overactive. If the pelvis tilts up at the beginning of movement, the quadratus lumborum is overactive. All of these movements demonstrate imbalance patterns.
Hip adduction is normally 30° and is measured from the same starting position as abduction. The patient is asked to adduct one leg over the other while the examiner ensures that the pelvis does not move. An alternative method is for the patient to flex the opposite hip and knee and hold the limb in flexion with the arms; the patient then adducts the test leg under the other leg. This method is useful only for thin patients. When the patient adducts the leg, the ASIS on the same side moves first. This movement occurs earlier in the ROM if there is an abduction contracture. Adduction may also be measured by asking the patient to abduct one leg and leave it abducted; the other leg is then tested for the amount of adduction present. The advantage of this method is that the test leg does not have to be flexed to clear the other leg before doing the adduction movement.
Rotation movements may be performed with the patient supine, prone, or sitting. Medial rotation normally ranges from 30° to 40°, and lateral rotation from 40° to 60°. In the supine position, the patient simply rotates the straight leg on a balanced pelvis. Turning the foot or leg outward tests lateral rotation; turning the foot or leg inward tests medial rotation. In another supine test (see Figure 11-8, E), the patient is asked to flex both the hip and knee to 90° as the patient would do when being tested in sitting.61 When using this method, it must be recognized that having the patient rotate the leg outward tests medial rotation, whereas having the patient rotate the leg inward tests lateral rotation. With the patient prone, the pelvis is balanced by aligning the legs at right angles to a line joining the PSISs. The patient then flexes the knee to 90°. Again, medial rotation is being tested when the leg is rotated outward, and lateral rotation is being tested when the leg is rotated inward (see Figure 11-8, F). Usually, one of these last two methods (sitting or prone) is used to measure hip rotation, because it is easier to measure the angle when performing the test. However, in prone, the measurement is done on a straight leg, whereas in sitting or supine, rotation is measured with the hip flexed to 90°. It has been found that there is a difference in the amount of lateral rotation between the flexed (less) and straight position, whereas medial rotation shows little difference when measured in the two positions.61
Passive Movements
If the range of movement was not full and the examiner was unable to test end feel during the active movements, passive movements should be performed to determine the end feel and passive range of motion (PROM). The passive movements performed are the same as the active movements. All the movements except extension can be tested with the patient in the supine lying position.
Sutlive et al.62 have developed a clinical prediction rule for hip osteoarthritis involving active and passive movement. If four of the five variables are positive, there is a high probability of hip osteoarthritis, and diagnostic imaging should be ordered to confirm the diagnosis.
The capsular pattern of the hip is flexion, abduction, and medial rotation. These movements are always the ones most limited in a capsular pattern, although the order of restriction may vary. For example, medial rotation may be most limited, followed by flexion and abduction. The hip joint is the only joint to exhibit this altered pattern of the same movements.
The pelvis should not move during hip movements. Groin discomfort and a limited ROM on medial rotation are good indications of hip problems. Passive hip flexion, adduction, and medial rotation, if painful, may indicate acetabular rim problems or labral tears, especially if clicking and pain into the groin is elicited.63
Intra-abdominal inflammation in the lower pelvis, as in the case of an abscess, may cause pain on passive medial and lateral rotation of the hip when the patient is supine with the hip and knee at 90°.
Resisted Isometric Movements
The resisted isometric movements are performed with the patient in the supine position (Figure 11-11). The muscles of the hip play a very significant role in stabilizing the pelvis, so they must be included in any assessment dealing with issues of pelvic control. The examiner should note whether the muscles are weak or strong and tight, and whether the muscle force-couples are acting correctly.64 When dealing with these muscles and the back and abdominal muscles, the examiner must be able to answer the following three questions in the affirmative to ensure pelvic control is present:
1. Can the patient actively position the pelvis in neutral?
2. Can the patient hold the neutral position statically? (This may include distal movement.)
A, Flexion. B, Extension. C, Adduction (knee straight). D, Adduction (knee bent). E, Abduction (knee straight). F, Abduction (knee bent). G, Medial rotation. H, Lateral rotation. I, Knee flexion. J, Knee extension.
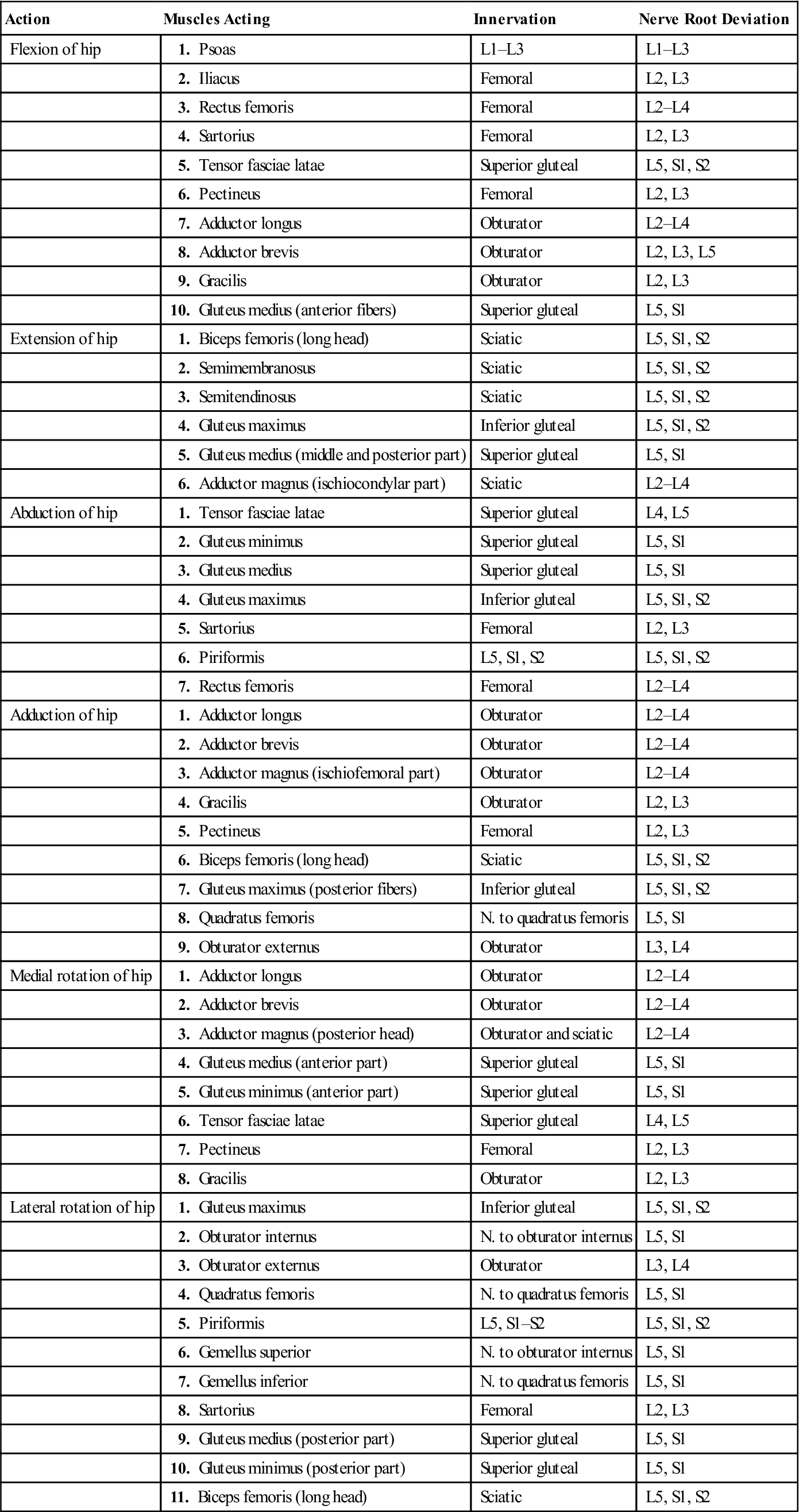
Because the hip muscles are very strong and there are many of them (Figure 11-12; Table 11-4), the examiner should position the patient’s hip properly and say to the patient, “Don’t let me move your hip,” to ensure that the movement is isometric. Delahunt et al.66 advocate testing the adductors with the hip flexed to 45° as the optimal test position (thigh adductor squeeze test). By carefully noting which movements cause pain or show weakness when the tests are done isometrically, the examiner should be able to determine which muscle, if any, is at fault (see Table 11-4). For example, the gluteus maximus is the only muscle that is involved in all of the following movements: extension, adduction, and lateral rotation. Therefore, if pain resulted from only these three movements, the examiner would suspect the gluteus maximus muscle. As with active movements, the most painful movements are performed last.
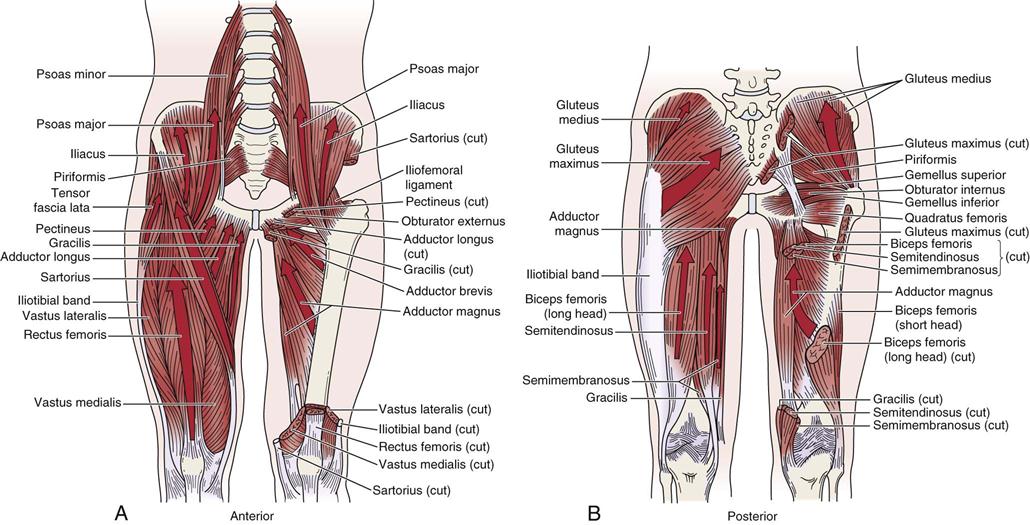
A, Anterior view. The right side shows the primary flexors and adductor muscles of the hip. Many muscles on the left side are cut to expose the adductor brevis and adductor magnus. B, Posterior view. The left side highlights the gluteus maximus and hamstring muscles (long head of biceps femoris, semitendinosis, and semimembranosus). The right side shows the hamstring muscles cut to expose the adductor magnus and short head of the biceps femoris. The right side shows the gluteus medius and five of the six short external rotators (i.e., piriformis, gemellus superior and inferior, obturator internus, and quadratus femoris). (Redrawn from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, CV Mosby, pp. 411, 419.)
TABLE 11-4
Muscles of the Hip: Their Actions, Innervation, and Nerve Root Derivation65
| Action | Muscles Acting | Innervation | Nerve Root Deviation |
| Flexion of hip | 1. Psoas | L1–L3 | L1–L3 |
| 2. Iliacus | Femoral | L2, L3 | |
| 3. Rectus femoris | Femoral | L2–L4 | |
| 4. Sartorius | Femoral | L2, L3 | |
| 5. Tensor fasciae latae | Superior gluteal | L5, S1, S2 | |
| 6. Pectineus | Femoral | L2, L3 | |
| 7. Adductor longus | Obturator | L2–L4 | |
| 8. Adductor brevis | Obturator | L2, L3, L5 | |
| 9. Gracilis | Obturator | L2, L3 | |
| 10. Gluteus medius (anterior fibers) | Superior gluteal | L5, S1 | |
| Extension of hip | 1. Biceps femoris (long head) | Sciatic | L5, S1, S2 |
| 2. Semimembranosus | Sciatic | L5, S1, S2 | |
| 3. Semitendinosus | Sciatic | L5, S1, S2 | |
| 4. Gluteus maximus | Inferior gluteal | L5, S1, S2 | |
| 5. Gluteus medius (middle and posterior part) | Superior gluteal | L5, S1 | |
| 6. Adductor magnus (ischiocondylar part) | Sciatic | L2–L4 | |
| Abduction of hip | 1. Tensor fasciae latae | Superior gluteal | L4, L5 |
| 2. Gluteus minimus | Superior gluteal | L5, S1 | |
| 3. Gluteus medius | Superior gluteal | L5, S1 | |
| 4. Gluteus maximus | Inferior gluteal | L5, S1, S2 | |
| 5. Sartorius | Femoral | L2, L3 | |
| 6. Piriformis | L5, S1, S2 | L5, S1, S2 | |
| 7. Rectus femoris | Femoral | L2–L4 | |
| Adduction of hip | 1. Adductor longus | Obturator | L2–L4 |
| 2. Adductor brevis | Obturator | L2–L4 | |
| 3. Adductor magnus (ischiofemoral part) | Obturator | L2–L4 | |
| 4. Gracilis | Obturator | L2, L3 | |
| 5. Pectineus | Femoral | L2, L3 | |
| 6. Biceps femoris (long head) | Sciatic | L5, S1, S2 | |
| 7. Gluteus maximus (posterior fibers) | Inferior gluteal | L5, S1, S2 | |
| 8. Quadratus femoris | N. to quadratus femoris | L5, S1 | |
| 9. Obturator externus | Obturator | L3, L4 | |
| Medial rotation of hip | 1. Adductor longus | Obturator | L2–L4 |
| 2. Adductor brevis | Obturator | L2–L4 | |
| 3. Adductor magnus (posterior head) | Obturator and sciatic | L2–L4 | |
| 4. Gluteus medius (anterior part) | Superior gluteal | L5, S1 | |
| 5. Gluteus minimus (anterior part) | Superior gluteal | L5, S1 | |
| 6. Tensor fasciae latae | Superior gluteal | L4, L5 | |
| 7. Pectineus | Femoral | L2, L3 | |
| 8. Gracilis | Obturator | L2, L3 | |
| Lateral rotation of hip | 1. Gluteus maximus | Inferior gluteal | L5, S1, S2 |
| 2. Obturator internus | N. to obturator internus | L5, S1 | |
| 3. Obturator externus | Obturator | L3, L4 | |
| 4. Quadratus femoris | N. to quadratus femoris | L5, S1 | |
| 5. Piriformis | L5, S1–S2 | L5, S1, S2 | |
| 6. Gemellus superior | N. to obturator internus | L5, S1 | |
| 7. Gemellus inferior | N. to quadratus femoris | L5, S1 | |
| 8. Sartorius | Femoral | L2, L3 | |
| 9. Gluteus medius (posterior part) | Superior gluteal | L5, S1 | |
| 10. Gluteus minimus (posterior part) | Superior gluteal | L5, S1 | |
| 11. Biceps femoris (long head) | Sciatic | L5, S1, S2 |
Resisted isometric flexion and extension of the knee must also be performed, because there are two joint muscles (hamstrings and rectus femoris) that act over the knee as well as the hip. If the history has indicated that concentric, eccentric, or econcentric movement causes symptoms, these movements should also be tested, but only after the isometric tests have been completed. For example, strength of the hamstrings may be determined by doing a supine plank test in which the patient is in crook lying, resting on his or her elbows (Figure 11-13).67 The patient then lifts the buttocks off the table while maintaining the body weight on the elbows and heels. The patient then alternately lifts the injured leg and then the good leg. If pain occurs at the ischial origin or in the hamstrings musculature, or if pelvic “collapse” or rotation occurs, the test is positive for weak hamstrings.
The examiner must be aware that intra-abdominal inflammation in the area of the psoas muscle may cause pain on resisted hip flexion. Intra-abdominal inflammation may also result in a rigid abdominal wall. It has been reported that hip flexors and hip extensors are almost equal in strength68 and that the adductors are 2.5 times as strong as the abductors.69 These ratios may vary depending on whether the movement is tested isometrically or isokinetically.
Functional Assessment
Hip motion is necessary for more activities than just ambulation. In fact, more hip ROM is required for activities of daily living (ADLs) than is required for gait; activities such as shoe tying, sitting, getting up from a chair, and picking up things from the floor all require a greater ROM. Table 11-5 illustrates the ranges of motion necessary for various activities. Ideally, the patient should have functional ranges of 120° of flexion, 20° of abduction, and 20° of lateral rotation.
TABLE 11-5
Range of Motion Necessary at the Hip for Selected Activities
| Activity | Average Range of Motion Necessary |
| Shoe tying | 120° of flexion |
| Sitting (average seat height) | 112° of flexion |
| Stooping | 125° of flexion |
| Squatting | 115° of flexion/20° of abduction/20° of medial rotation |
| Ascending stairs (average stair height) | 67° of flexion |
| Descending stairs (average stair height) | 36° of flexion |
| Putting foot on opposite thigh | 120° of flexion/20° of abduction/20° of lateral rotation |
| Putting on trousers | 90° of flexion |
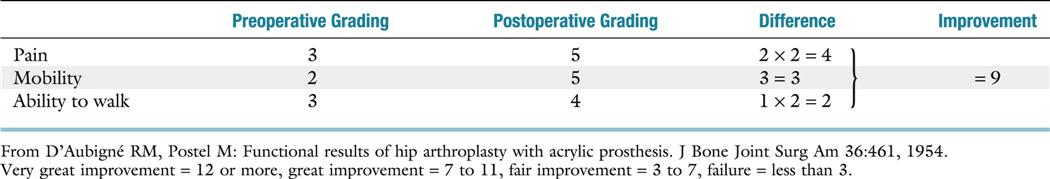
There are several numerical rating scales with which to rate hip function.70–76 These rating methods are based primarily on pain, mobility, and gait. Tables 11-6 through 11-8 and Figures 11-14 and 11-15 illustrate three different rating scales. D’Aubigné and Postel70 (see Tables 11-6 through 11-8) developed one of the first hip rating scales based on pain, mobility, and ability to walk.71 The Harris hip function scale72 (see Figure 11-14) is useful for rating hips before and after surgery. This scale is most often used because it emphasizes pain and function. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)77–82 and the Lower Extremity Function Scale (LEFS) (Figure 11-16)83–86 were developed to evaluate clinically important and patient-relevant changes in health status primarily with arthroplasties of the hip and knee. The WOMAC scale is made up of three sections with scores ranging from one (none) to five (extreme). The sum of three scores is called the index or global score. The higher the score, the greater the disability. The SF-36 questionnaire is also sometimes used as a functional assessment tool in arthroplasty cases.82,87 The Iowa scale (see Figure 11-15) provides a single rating value. The Mayo hip score73 for hip arthroplasty makes use of greater patient (functional) input and radiographic input (to predict long-term results). This score correlates well with the Harris scale.71,73 Johanson and colleagues74 developed a numerical scale that is related to what patients are able to do functionally after total hip replacement. Its value comes from its focus on the outcome from the patient’s perspective (Figure 11-17). As Burton and co-workers75 pointed out, the notion of expectations is more important than the notion of success. Table 11-9 gives a functional strength and endurance testing scheme for the hip.
TABLE 11-6
Method of Grading Functional Value of Hip*
| Grade | Pain | Mobility | Ability to Walk |
| 0 | Pain is intense and permanent | Ankylosis with bad position of the hip | None |
| 1 | Pain is severe, even at night | No movement; pain or slight deformity | Only with crutches |
| 2 | Pain is severe when walking; prevents any activity | Flexion less than 40° | Only with canes |
| 3 | Pain is tolerable with limited activity | Flexion between 40° and 60° | With one cane, for less than 1 hour; very difficult without a cane |
| 4 | Pain is mild when walking; it disappears with rest | Flexion between 60° and 80°; patient can reach own foot | A long time with a cane; a short time without cane and with limp |
| 5 | Pain is mild and inconstant; normal activity | Flexion between 80° and 90°; abduction at least 15° | Without cane but with slight limp |
| 6 | No pain | Flexion more than 90°; abduction to 30° | Normal |
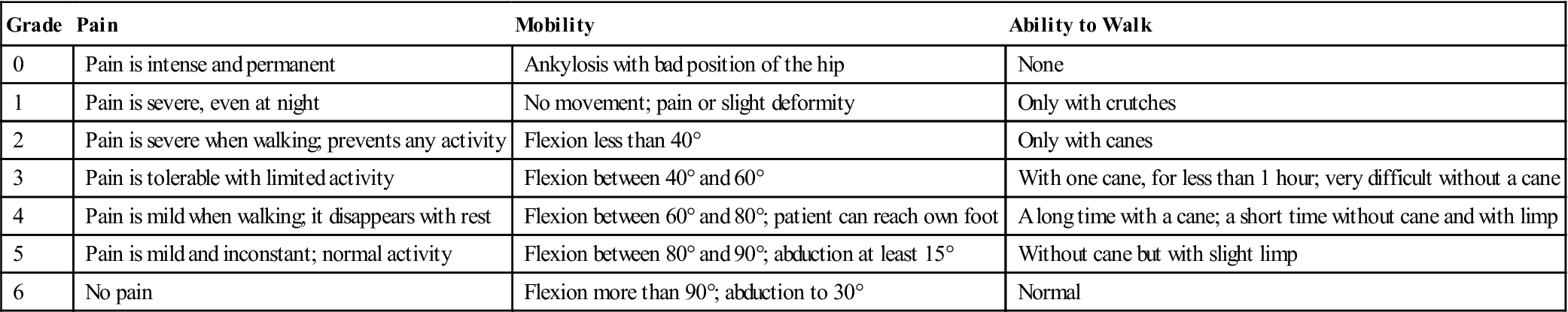
*Values used in conjunction with Table 11-7.
From D’Aubigné, RM, Postel M: Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 36:459, 1954.
TABLE 11-7
D’Aubigné and Postel Scale for Functional Grading of the Hip
| Pain (P) | Ability to Walk (W) | Mobility Normal or Nearly Normal | Grade |
| Very Good | P + W = 11 or 12 | ||
| 6 | 6 | Walk without cane, with no pain and no limp | |
| 6 | 5 | Walk without cane, with no pain but slight limp | |
| 5 | 6 | Walk without cane, with no limp but slight pain when starting | |
| Good | P + W = 10 | ||
| 5 | 5 | Walk without cane, with slight pain and slight limp | |
| 4 | 6 | Walk without cane, with pain but no limp | |
| 6 | 4* | Walk without cane, without pain; a cane used to go outdoors | |
| Medium | P + W = 9 | ||
| 5 | 4 | Slight pain; a cane is used outdoors | |
| 4 | 5 | Pain after walking some minutes; no cane is used, but there is a slight limp | |
| 6 | 3† | No pain; a cane used all the time | |
| Fair | P + W = 8 | ||
| 5 | 3 | Slight pain; a cane is used all the time | |
| 4 | 4 | Pain after walking; a cane is used outdoors | |
| ≤3 | ≤3 | Poor | P + W = 7 or less |
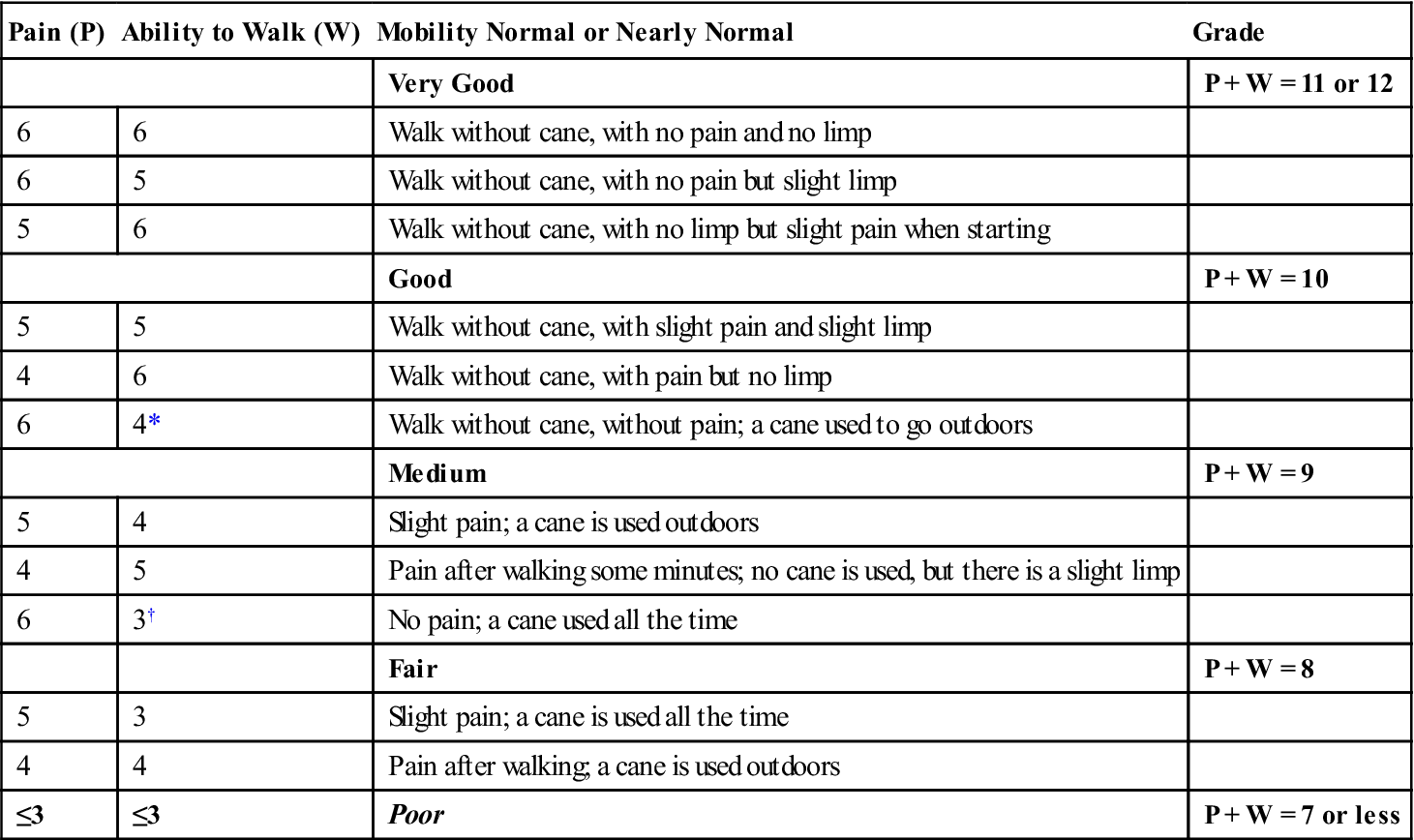
*If the mobility is reduced to 4, the result is classified one grade lower.
†If the mobility is reduced to 3 or less, the result is classified two grades lower.
Adapted from D’Aubigné, RM, Postel M: Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 36:460, 1954.
TABLE 11-8
Method of Evaluating Improvement Brought About by Operation in Problems of the Hip (Relative Result)
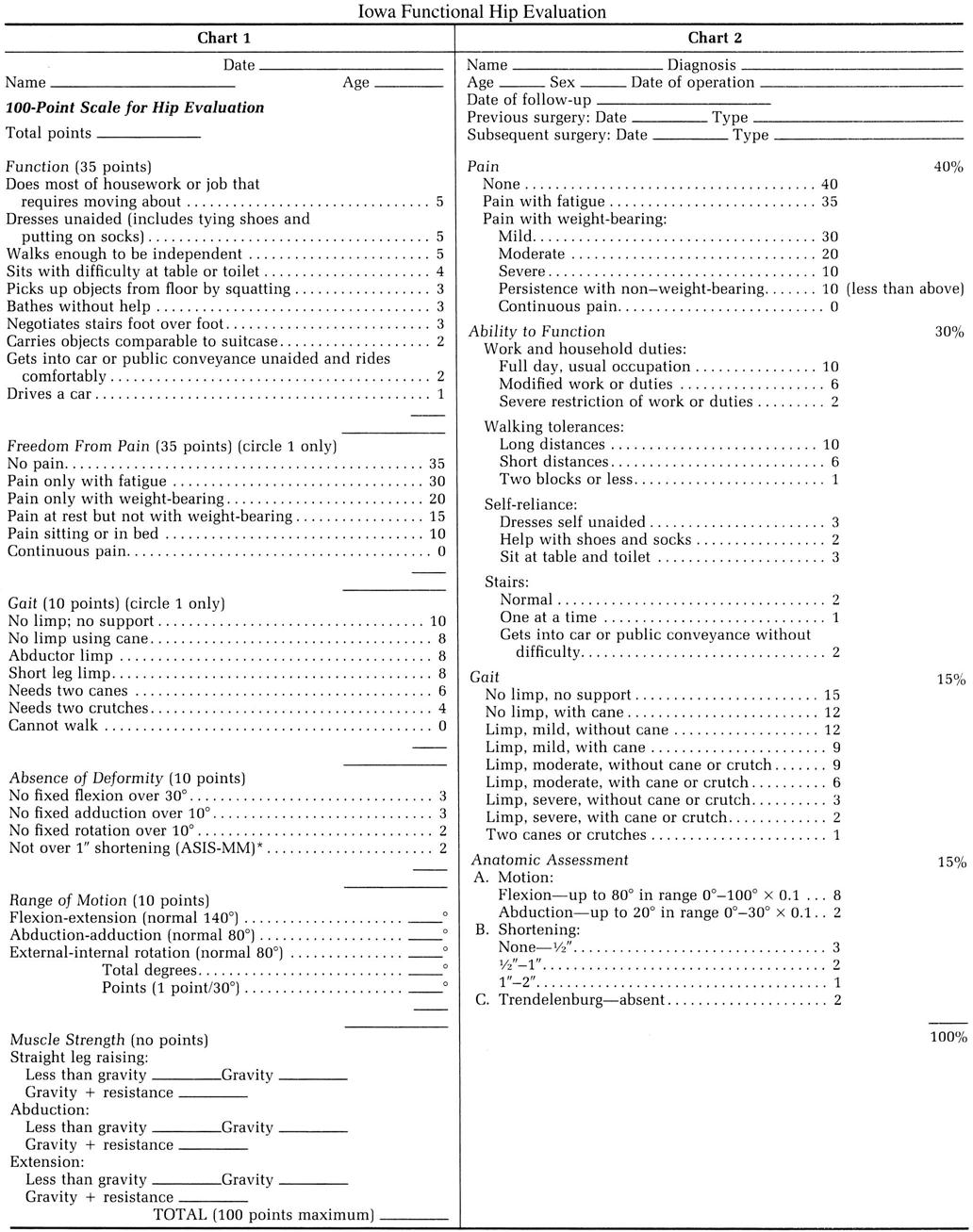
ASIS-MM, Anterior superior iliac spine to medial malleolus. (Modified from Larson CB: Rating scale for hip disabilities. Clin Orthop 31:86, 1963.)
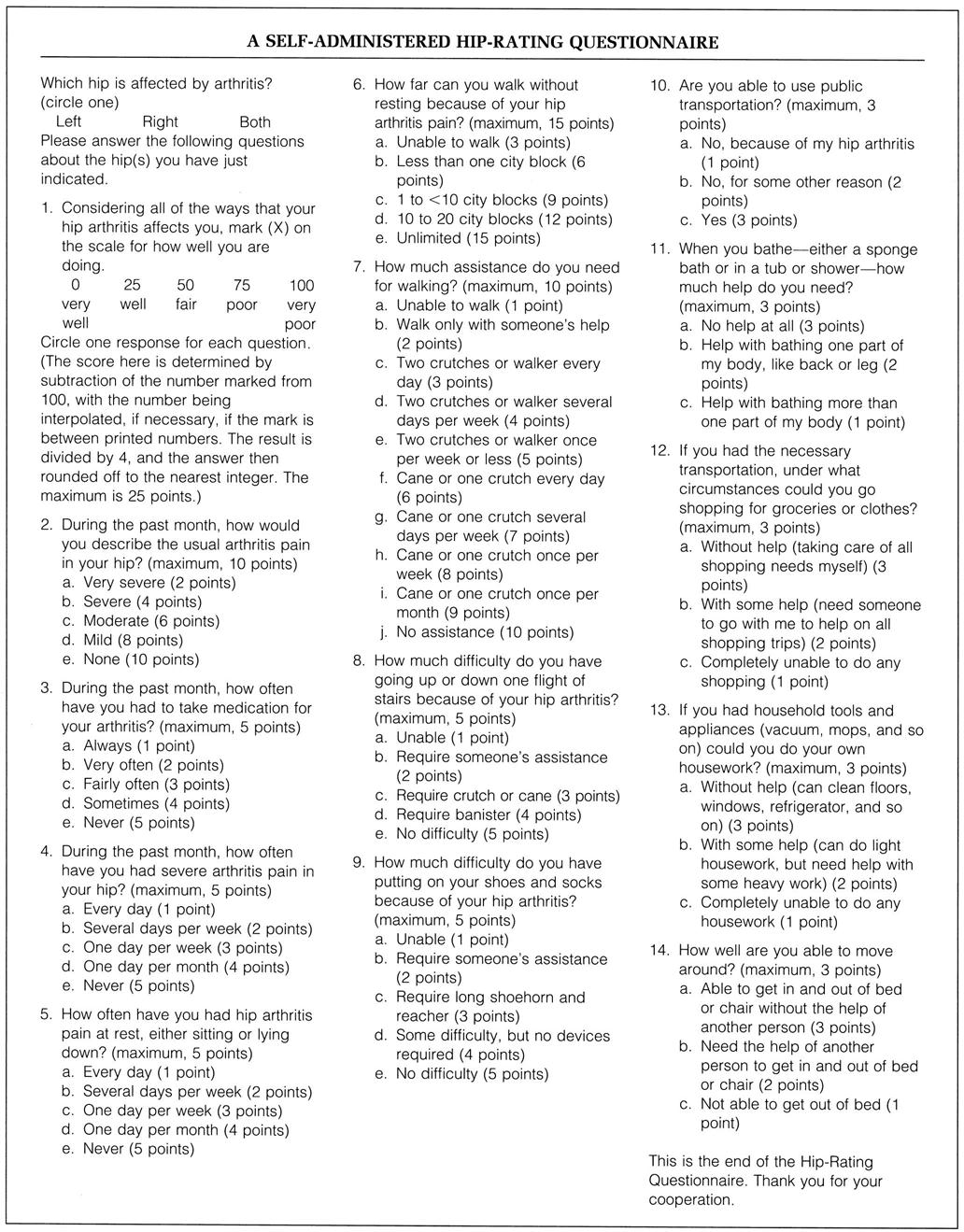
The maximum score is 100 points, and the minimum is 16 points. The point values of the answers are not shown in the questionnaire that is administered to patients. (From Johanson NA, Charlson ME, Szatrowski TP, et al: A self-administered hip-rating questionnaire for the assessment of outcome after total hip replacement. J Bone Joint Surg Am 74:589, 1992.)
TABLE 11-9
| Starting Position | Action | Functional Test |
| Standing | Lift foot onto 20-cm step and return (hip flexion-extension) | 5 to 6 Repetitions: Functional 3 to 4 Repetitions: Functionally fair 1 to 2 Repetitions: Functionally poor 0 Repetitions: Nonfunctional |
| Standing | Sit in chair and return to standing (hip extension-flexion) | 5 to 6 Repetitions: Functional 3 to 4 Repetitions: Functionally fair 1 to 2 Repetitions: Functionally poor 0 Repetitions: Nonfunctional |
| Standing | Lift leg to balance on one leg keeping pelvis straight (hip abduction) | Hold 1 to 1.5 minutes: Functional Hold 30 to 59 seconds: Functionally fair Hold 1 to 29 seconds: Functionally poor Cannot hold: Nonfunctional |
| Standing | Walk sideways 6 m (hip adduction/abduction) | 6 to 8 m one way: Functional 3 to 6 m one way: Functionally fair 1 to 3 m one way: Functionally poor 0 m: Nonfunctional |
| Standing | Test leg off floor (patient may hold onto something for balance) medially rotate non–weight-bearing hip | 10 to 12 Repetitions: Functional 5 to 9 Repetitions: Functionally fair 1 to 4 Repetitions: Functionally poor 0 Repetitions: Nonfunctional |
| Standing | Test leg off floor (patient may hold onto something for balance) laterally rotate non–weight-bearing hip | 10 to 12 Repetitions: Functional 5 to 9 Repetitions: Functionally fair 1 to 4 Repetitions: Functionally poor 0 Repetitions: Nonfunctional |
Data from Palmer ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, JB Lippincott, pp. 251–254.
Several walking tests have been developed, especially for the elderly, to give an indication of musculoskeletal functional impairment of the lower limb and may be included in any assessment involving injury to the low limb joints.88 These include the Timed “Up and Go” test (TUG test),88–91 13-metre walk test,88 6-minute walk test (6MWT),88,92–96 self-paced walk test,91,97–99 2-minute walk test,92 10-metre walk test, 12-minute walk test92 and sit to stand.91
If the patient is able to perform normal active movements with little difficulty, the examiner may use a series of functional tests to determine whether increased intensity of activity produces pain or other symptoms. These tests must be geared to the individual patient.100 Older persons should not be expected to perform the last six activities unless they have been doing these movements or similar ones in the recent past.
Special Tests
Only those tests that the examiner believes are necessary should be performed when assessing the hip. Most tests are done primarily to confirm a diagnosis or to determine pathology and should not be used as “stand alone” tests when considering a diagnosis.101 As with all special tests, if the test is positive, it is highly suggestive that the problem exists, but if it is negative, it does not necessarily rule out the problem. Therefore, special tests should not be taken in isolation but should be used to support the history, observation, and clinical examination.
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the hip are available on the Evolve website.
APPENDIX 11-1
Reliability, Validity, Specificity, and Sensitivity of Special/Diagnostic Tests Used in the Hip
| CRAIG’S TEST |
| Reliability |
| FUNCTIONAL SQUAT |
| Reliability |
| HIP FLEXION |
| Reliability |
| HIP SCOUR TEST |
| Reliability |
| PATRICK’S TEST (FABER OR FIGURE-FOUR TEST) |
| Reliability |
| RADIOGRAPHIC DIAGNOSIS AND CLASSIFICATION OF TROCHLEA DYSPLASIA |
| Reliability |
| SELF-PACED WALK TEST (40 M) |
| Reliability |
| SIX MINUTE WALK TEST |
| Reliability |
| STAIR MEASURE (NINE STEPS/20 CM HEIGHT/STEP) |
| Reliability |
| SUPINE LEG LENGTH |
| Reliability |
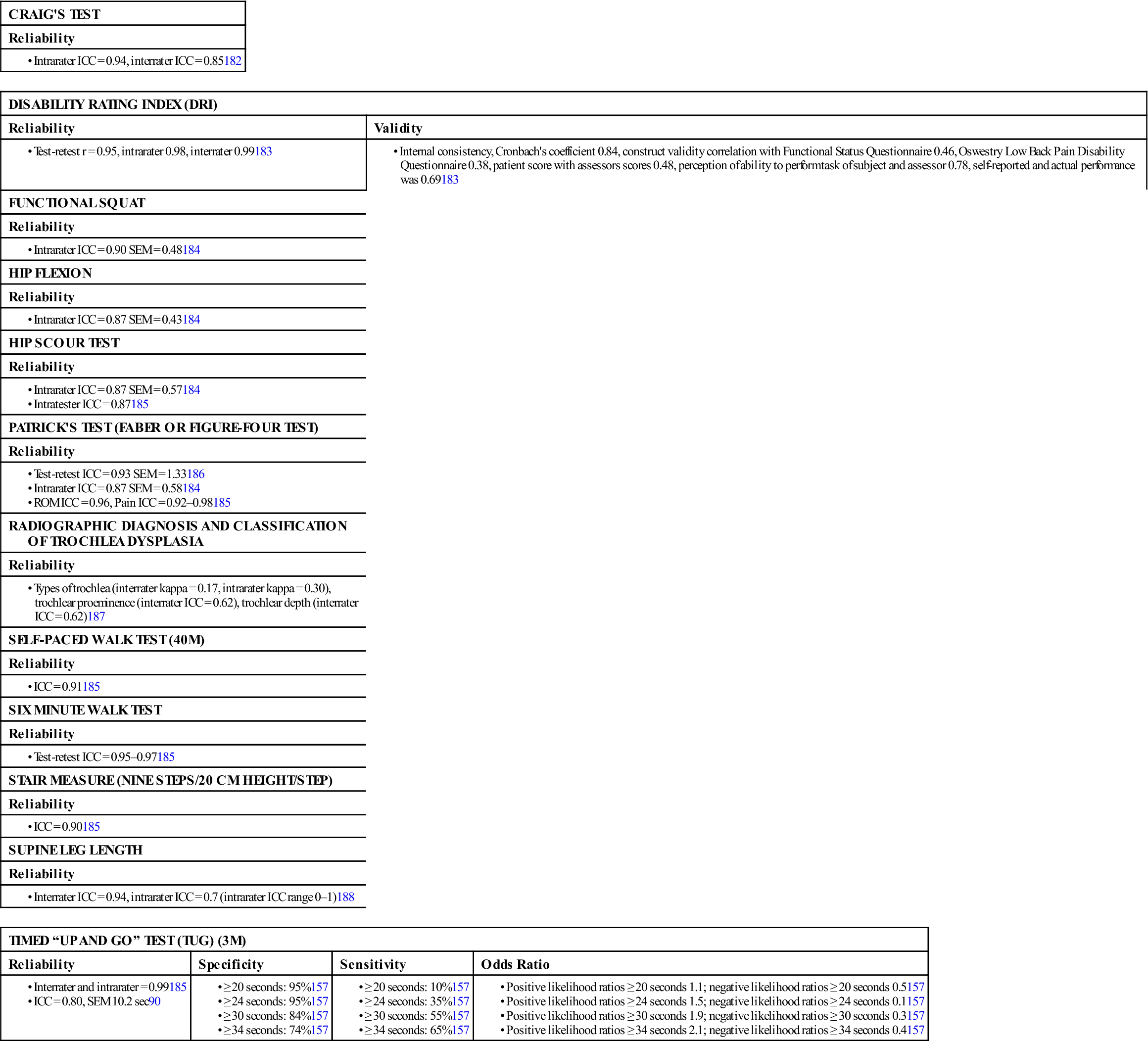
ICC, Intraclass correlation coefficient; ROM, range of motion; SEM, standard error of measurement.
Tests for Hip Pathology
 Bryant’s Triangle.
Bryant’s Triangle.
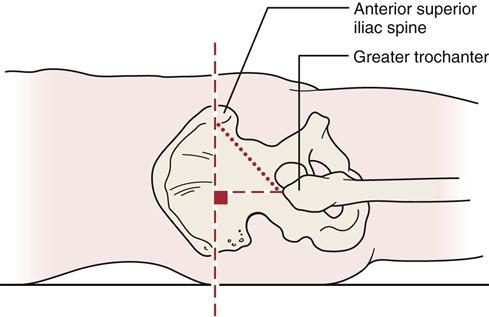
With the patient lying supine, the examiner drops an imaginary perpendicular line from the ASIS of the pelvis to the examining table.104 A second imaginary line is projected up from the tip of the greater trochanter of the femur to meet the first line at a right angle (Figure 11-18). This line is measured, and the two sides are compared. Differences may indicate conditions, such as coxa vara or CDH. This measurement can be done with radiographs, in which case the lines may be drawn on the radiograph.
 Craig’s Test.
Craig’s Test.
Craig’s test measures femoral anteversion or forward torsion of the femoral neck (Figure 11-19). Anteversion of the hip is measured by the angle made by the femoral neck with the femoral condyles (Figure 11-20). It is the degree of forward projection of the femoral neck from the coronal plane of the shaft (Figure 11-21), and it decreases during the growing period. At birth, the mean angle is approximately 30°; in the adult, the mean angle is 8° to 15° (Figure 11-22). Increased anteversion leads to squinting patellae and toeing-in (Figure 11-23).105 Excessive anteversion is twice as common in girls as in boys. A common clinical finding of excessive anteversion is excessive medial hip rotation (more than 60°) and decreased lateral rotation in extension.105 Gelberman et al.106 pointed out, however, that rotation should be viewed both in neutral (as in the Craig’s test) and with 90° of hip flexion, because rotation shows greater variability in flexion. They felt that greater medial rotation than lateral rotation in both positions was a better indicator of increased femoral anteversion. In retroversion, the plane of the femoral neck rotates backward in relation to the coronal condylar plane (see Figure 11-23) or the acetabulum itself may be retroverted.49,104,106–109
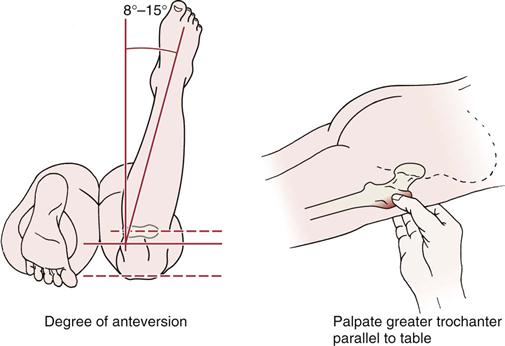
 Figure 11-19 Craig’s test to measure femoral anteversion.
Figure 11-19 Craig’s test to measure femoral anteversion.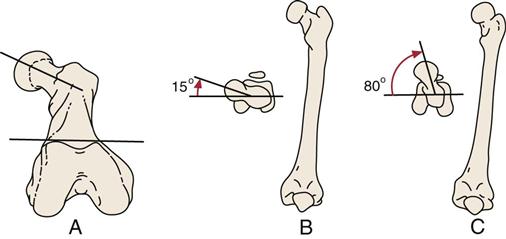
A, Femoral anteversion angle. B, Normal angle. C, Excessive angle. (A, Redrawn from the American Orthopaedic Association: Manual of Orthopaedic Surgery, Chicago, 1979, AOA, p. 45.)
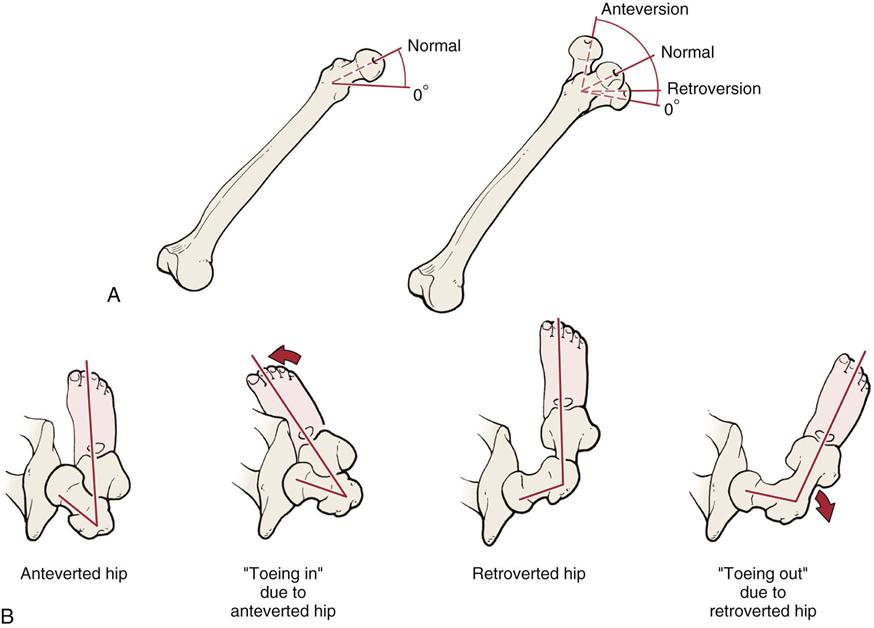
A, Positions of femoral neck. B, Different foot positions with anteversion and retroversion at the hip (coronal views). (Redrawn from Echternach J, editor: Physical therapy of the hip, New York, 1990, Churchill Livingstone, p. 25.)
For Craig’s test, which has been found to correlate well with x-rays (within 4°) in children,110 the patient lies prone with the knee flexed to 90°. The examiner palpates the posterior aspect of the greater trochanter of the femur. The hip is then passively rotated medially and laterally until the greater trochanter is parallel with the examining table or reaches its most lateral position. The degree of anteversion can then be estimated, based on the angle of the lower leg with the vertical.111 The test is also called the Ryder method for measuring anteversion or retroversion.
 Dial Test of the Hip.112
Dial Test of the Hip.112
The patient lies supine with the hips in neutral (i.e., no rotation). The examiner medially rotates the limb and then releases it allowing the leg to go into lateral rotation. If the patient’s leg passively rotates greater than 45° from vertical in the axial plane and if, on testing, there is no mechanical end point, the test is positive for hip instability (Figure 11-24). Both limbs are compared starting with the unaffected side.
 Flexion-Adduction Test.113
Flexion-Adduction Test.113
This test is used in older children and young adults as a test for hip disease. The patient lies supine while the examiner flexes the patient’s hip to at least 90° with the knee flexed (Figure 11-25). The examiner then adducts the flexed leg. Normally, the knee will pass over the opposite hip without rolling the pelvis. In pathological hips, adduction is limited and accompanied by pain or discomfort.
 Foveal Distraction Test.12
Foveal Distraction Test.12
The patient is in supine. The examiner abducts the hip to 30° and applies an axial traction to the leg which reduces intra-articular pressure (Figure 11-26). Relief of pain indicates the pain is intra-articular.

 Hip Scour Test.
Hip Scour Test.
Maitland114 called the flexion-adduction test the quadrant or scouring test. He felt the test stressed or compressed the femoral neck against the acetabulum, or pinched adductor longus, pectineus, iliopsoas, sartorius or tensor fascia lata. The patient lies supine. The examiner flexes and adducts the patient’s hip so that the hip faces the patient’s opposite shoulder and resistance to the movement is felt (Figure 11-27). As slight resistance is maintained, the patient’s hip is taken into abduction while maintaining flexion in an arc of movement. As the movement is performed, the examiner should look for any irregularity in the movement (e.g., “bumps”), pain, or patient apprehension, which may give an indication of where the pathology is occurring in the hip.114 This motion also causes impingement of the femoral neck against the acetabular rim and pinches the adductor longus, pectineus, iliopsoas, sartorius, and/or tensor fascia lata. Therefore, it should be performed with care.39–41

 Figure 11-27 Hip scour test.
Figure 11-27 Hip scour test. Log Roll Test.
Log Roll Test.
The patient lies supine with both lower extremities extended. The examiner passively medially and laterally rotates the femur to end range comparing both hips (Figure 11-28). If a click is present, it may indicate a labral tear. The maneuver also shows hip rotational mobility, and if restricted or painful, indicates hip pathology.10,115,116
 McCarthy Hip Extension Sign.10,117,118
McCarthy Hip Extension Sign.10,117,118
The patient lies supine on the bed with both hips flexed. The examiner then takes the good hip and extends it from the flexed position, first with the hip in lateral rotation, and then repeats the test with the hip in medial rotation. The non-test leg is kept in flexion. The test is repeated with the affected hip. A positive test would be the reproduction of the patient’s pain. The test is designed to simulate normal walking and creates a force double the patient’s body weight across the hip.12 McCarthy et al.117 believed there were three positive tests that would help to predict labral pathology: 1) pain with the McCarthy hip extension test (Figure 11-29), 2) painful impingement with hip flexion abduction and lateral rotation (the anterior labial tear test), and 3) inguinal pain on resisted straight leg raise (Stinchfield resisted hip flexion test).
 Nélaton’s Line.
Nélaton’s Line.
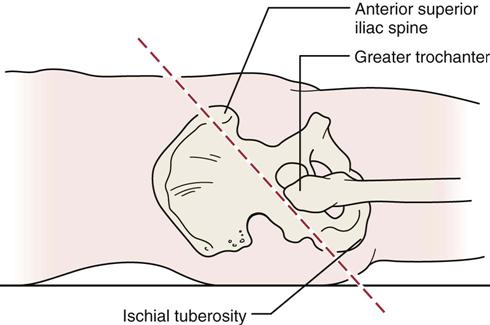
Nélaton’s line is an imaginary line drawn from the ischial tuberosity of the pelvis to the ASIS of the pelvis on the same side (Figure 11-30).107 If the greater trochanter of the femur is palpated well above the line, it is an indication of a dislocated hip or coxa vara. The two sides should be compared.
 Patrick’s Test (FABER or Figure-4 Test).
Patrick’s Test (FABER or Figure-4 Test).
The patient lies supine, and the examiner places the patient’s test leg so that the foot of the test leg is on top of the knee of the opposite leg (Figure 11-31). The examiner then slowly lowers the knee of the test leg toward the examining table. A negative test is indicated by the test leg’s knee falling to the table or at least being parallel with the opposite leg. A positive test is indicated by the test leg’s knee remaining above the opposite straight leg. If positive, the test indicates that the hip joint may be affected, that there may be iliopsoas spasm, or that the sacroiliac joint may be affected. Flexion, abduction, and external rotation (FABER) is the position of the hip at which the patient begins the test. The test is sometimes referred to as Jansen’s test.119
Rotational Deformities.
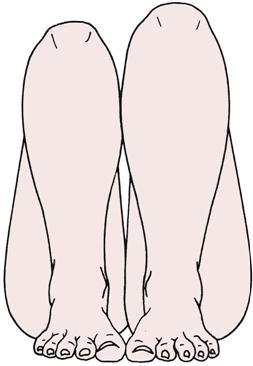
Rotational deformities can occur anywhere between the hip and the foot (Table 11-10). Many of these deformities are hereditary. The patient lies supine with the lower limbs straight while the examiner looks at the patellae.108 If the patellae face in (squinting patellae), it is a possible indication of medial rotation of the femur or the tibia. If the patellae face up, out, and away from each other (“frog eyes” or “grasshopper eyes”), it is a possible indication of lateral rotation of the femur or the tibia. If the tibia is affected, the feet face in (“pigeon toes”) for medial rotation and face out more than 10° for excessive lateral rotation of the tibia (Figure 11-32) while the patellae face straight ahead. Normally, the feet angle out 5° to 10° (Fick angle) for better balance.
TABLE 11-10
| Malalignment | Related Posture | Possible Compensating Postures |
| Excessive anteversion | Toeing-in Subtalar pronation Lateral patellar subluxation Medial tibial torsion Medial femoral torsion |
Lateral tibial torsion Lateral rotation at knee Lateral rotation of tibia, femur, and/or pelvis Lumbar rotation on same side |
| Excessive retroversion | Toeing-out Subtalar supination Lateral tibial torsion Lateral femoral torsion |
Medial rotation at knee Medial rotation of tibia, femur, and/or pelvis Lumbar rotation on opposite side |
| Coxa vara | Pronated subtalar joint Medial rotation of leg Short ipsilateral leg Anterior pelvic rotation |
Ipsilateral subtalar supination Contralateral subtalar pronation Ipsilateral plantar flexion Contralateral genu recurvatum Contralateral hip and/or knee flexion Ipsilateral posterior pelvic rotation and ipsilateral lumbar rotation |
| Coxa valga | Supinated subtalar joint Lateral rotation of leg Long ipsilateral leg Posterior pelvic tilt |
Ipsilateral subtalar pronation Contralateral subtalar supination Contralateral plantar flexion Ipsilateral genu recurvatum Ipsilateral hip and/or knee flexion Ipsilateral anterior pelvic rotation and contralateral lumbar rotation |
Adapted from Reigger-Krugh C, Keysor, JJ: Skeletal malalignments of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther 23:166–167, 1996.
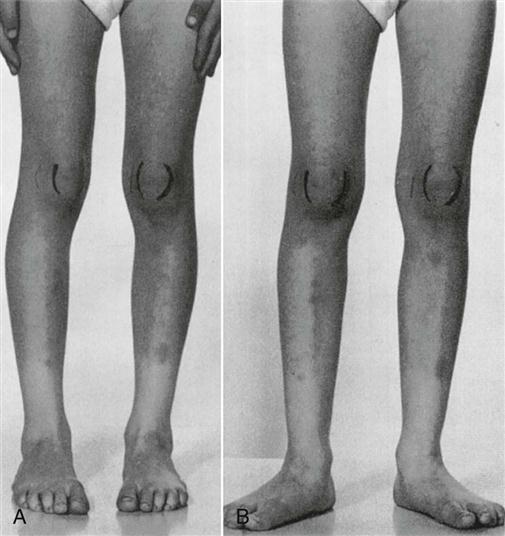
A, With the knees in full extension and the feet aligned (pointing straight forward), the legs appear bowed and the patellae face inward (squinting patella). B, On lateral rotation of the hips so that the patellae are facing to the front, the feet and legs point outward and the bowleg appearance is corrected. (From Tachdjian MO: Pediatric orthopedics, Philadelphia, 1990, WB Saunders, p. 2802.)
 Stinchfield Resisted Hip Flexion Test.120–122
Stinchfield Resisted Hip Flexion Test.120–122
The patient lies supine and then actively elevates the straight leg (i.e., flexes the hip) to about 20° to 30° while the examiner applies gentle resistance. In a positive test, pain may be referred into the sensory distribution of the femoral, obturator, or sciatic nerves. A positive test indicates intra-articular pathology, which may include a labral tear, synovitis, arthritis, occult femoral neck fractures, iliopsoas tendinitis/bursitis, and prosthetic failure or loosening.123
 Torque Test.
Torque Test.
The patient lies supine close to the edge of the examining table with the femur of the test leg extended over the edge of the table (Figure 11-33). The test leg is extended until the pelvis (i.e., the ASIS) begins to move. The examiner uses one hand to medially rotate the femur to the end of range and the other hand to apply a slow posterolateral pressure along the line of the neck of the femur for 20 seconds to stress the capsular ligaments and test the stability of the hip joint.124

Tests for Impingement
 Anteroposterior Impingement Test.47,51
Anteroposterior Impingement Test.47,51
This test is a test for hip dysplasia (e.g., acetabular retroversion), slipped capital femoral epiphysis, and femoroacetabular impingement.59 The patient lies supine with the hip flexed to 90°. The examiner then medially rotates and adducts the hip which leads to impingement of femoral neck against the acetabular rim (Figure 11-34, A). Forced medial rotation can lead to a labral lesion, chondral lesion, or both. Pain is a positive sign. The hip is similarly tested in different degrees of flexion (45° to 120°) with pain increasing with increased flexion.59
 Posteroinferior Impingement Test.47,51,112
Posteroinferior Impingement Test.47,51,112
This test is a test for global acetabular over coverage (e.g., coxa profunda, coxa protrusio), global femoral neck offset abnormalities, and posterior acetabular cartilage damage. The test is also positive in people who place the hip in extremes of ROM (e.g., ballet dancers, martial artists, hockey goal tenders, mountain climbers, yoga practitioners, long striding runners).59 The patient lies supine with the legs hanging free over the edge of the bed to ensure maximum hip extension. The examiner then laterally rotates the hip quickly (Figure 11-34, B). Deep seated groin or buttock pain is an indication of posteroinferior impingement.47,51,59
The dynamic internal (medial) rotation impingement (DIRI) test ![]() and the dynamic external (lateral) rotation impingement test (DEXRIT)
and the dynamic external (lateral) rotation impingement test (DEXRIT) ![]() are modifications of the previous two tests that are commonly used in arthroscopies of the hip.12 In both cases, the patient is in supine lying. The examiner takes the test hip into 90° of flexion. For the DIRI test, the hip is passively moved through a wide arc of adduction and medial rotation while for DEXRIT, the hip is passively moved through a wide arc of abduction and lateral rotation. Pain is a positive test.
are modifications of the previous two tests that are commonly used in arthroscopies of the hip.12 In both cases, the patient is in supine lying. The examiner takes the test hip into 90° of flexion. For the DIRI test, the hip is passively moved through a wide arc of adduction and medial rotation while for DEXRIT, the hip is passively moved through a wide arc of abduction and lateral rotation. Pain is a positive test.
Tests for Labral Lesions
Acetabular labral tears rarely occur without some structural osseous abnormality often accompanied by a history of the patient repeatedly going into extreme ranges of motion especially rotation.46 These tears may be accompanied by damage to the acetabular cartilage.46,125
 Anterior Labral Tear Test (Flexion, Adduction, and Internal Rotation [FADDIR] Test).10,27,33,51,126
Anterior Labral Tear Test (Flexion, Adduction, and Internal Rotation [FADDIR] Test).10,27,33,51,126
This test, also called the anterior apprehension test,127 is used to test for anterior–superior impingement syndrome, anterior labial tear, and iliopsoas tendinitis. The patient is placed in supine position. The examiner takes the hip into full flexion, lateral rotation, and full abduction as a starting position. The examiner then extends the hip combined with medial rotation and adduction (Figure 11-35). A positive test is indicated by the production of pain, the reproduction of the patient’s symptoms with or without a click, or apprehension. The test places the greatest strain on the anterolateral labrum, and the examiner should be careful to equate any findings with the patient’s symptoms.10,116
 Posterior Labral Tear Test.27,51
Posterior Labral Tear Test.27,51
The patient is placed in supine position. The examiner takes the hip into full flexion, adduction, and medial rotation as a starting position. The examiner then takes the hip into extension combined with abduction and lateral rotation (Figure 11-36). A positive test is indicated by the production of groin pain, patient apprehension, or the reproduction of the patient’s symptoms, with or without a click. A positive test is an indication of a labral tear, anterior hip instability, or posterior–inferior impingement. The test is sometimes called the posterior apprehension test if apprehension occurs toward the end of ROM when doing the test.
Tests for Femoral Neck Stress Fractures
 Fulcrum Test of the Hip.
Fulcrum Test of the Hip.
The fulcrum test128 is used to assess for possible stress fracture of the femoral shaft. The patient sits with the knees bent over the end of the bed with feet dangling. The examiner places an arm under the patient’s thigh to act as a fulcrum (Figure 11-37). The fulcrum arm is moved from distal to proximal along the thigh as gentle pressure is applied to the dorsum of the knee with the examiner’s opposite hand. If a stress fracture is present, the patient complains of a sharp pain and expresses apprehension when the fulcrum arm is under the fracture site. A bone scan confirms the diagnosis.
 Heel Strike Test.12
Heel Strike Test.12
The patient is lying supine. The examiner firmly strikes the heel to stimulate heel strike during walking. Pain in the groin may be suggestive of a femoral neck stress fracture. A single leg hop (see Chapter 12) would have the same effect with a positive test showing pain in the groin.
 Patellar-Pubic Percussion Sign.101,129
Patellar-Pubic Percussion Sign.101,129
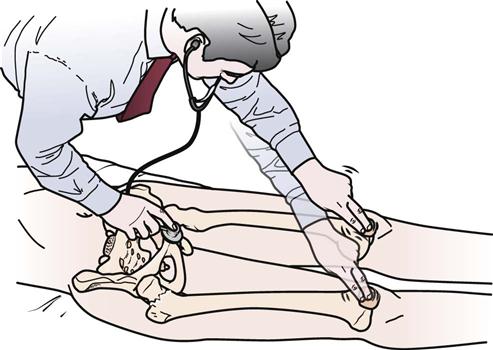
The patient lies supine with the legs extended. The examiner places the bell of the stethoscope over the symphysis pubis. The examiner then percusses each patella with a finger starting with the uninvolved side. Both sides are compared for differences in pitch and loudness. Normally, the sounds are equal. If bone pathology is present (e.g., hip fracture) the affected side has a duller sound (Figure 11-38).
Pediatric Tests for Hip Pathology
Orthopedic tests are commonly performed in newborns to detect problems, especially CDH or developmental dysplasia of the hip (DDH) that covers more than congenital problems, which may be amenable to conservative treatment if caught early.130–132
 Abduction Test (Harts’ Sign).133
Abduction Test (Harts’ Sign).133
If CDH is not diagnosed early or there is DDH, parents often note that when they change the child’s diapers, one leg does not abduct as far as the other one.131 This is the basis for this test. The child lies supine with the hips and knees flexed to 90°. The examiner then passively abducts both legs, noting any asymmetry or limitation of movement. In addition, if one hip is dislocated, the child often demonstrates asymmetry of fat folds in the gluteal and upper leg area because of the “riding up” of the femur on the affected side.
 Barlow’s Test.
Barlow’s Test.
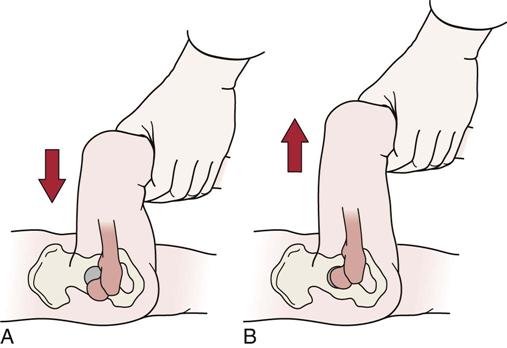
Barlow’s test is a modification of Ortolani’s test108 (Figure 11-39) used for DDH.131 The infant lies supine with the legs facing the examiner. The hips are flexed to 90°, and the knees are fully flexed. Each hip is evaluated individually while the examiner’s other hand steadies the opposite femur and the pelvis. The examiner’s middle finger of each hand is placed over the greater trochanter, and the thumb is placed adjacent to the inner side of the knee and thigh opposite the lesser trochanter. The hip is taken into abduction while the examiner’s middle finger applies forward pressure behind the greater trochanter. If the femoral head slips forward into the acetabulum with a click, clunk, or jerk, the test is positive, indicating that the hip was dislocated. This part of the test is identical to Ortolani’s test. The examiner then uses the thumb to apply pressure backward and outward on the inner thigh. If the femoral head slips out over the posterior lip of the acetabulum and then reduces again when pressure is removed, the hip is classified as unstable. The hip is not dislocated but is dislocatable. The procedure is repeated for the other hip.
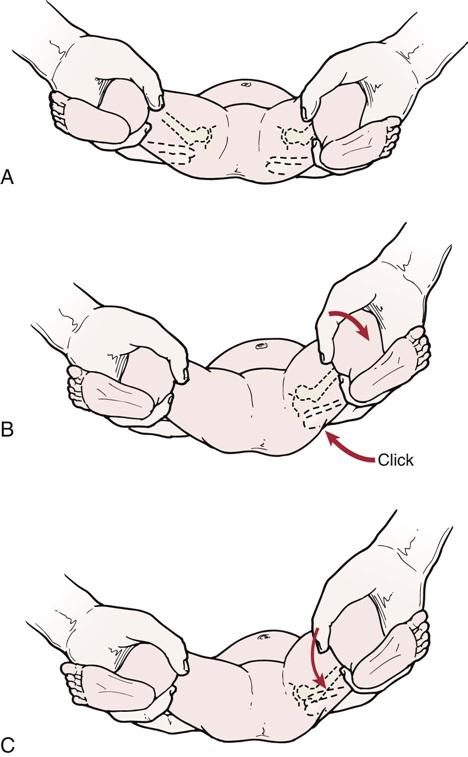
A, In the newborn, the two hips can be equally flexed, abducted, and laterally rotated without producing a “click.” B, Ortolani’s sign or first part of Barlow’s test. C, Second part of Barlow’s test.
This test may be used for infants up to 6 months of age. It should not be repeated too often, because it may result in a dislocated hip as well as articular damage to the head of the femur.134
 Galeazzi Sign (Allis or Galeazzi Test).
Galeazzi Sign (Allis or Galeazzi Test).
The Galeazzi test is good only for assessing unilateral CDH or unilateral DDH and may be used in children from 3 to 18 months of age.122 The child lies supine with the knees flexed and the hips flexed to 90°. A positive test is indicated if one knee is higher than the other (Figure 11-40).
 Ortolani’s Sign.
Ortolani’s Sign.
Ortolani’s test can determine whether an infant has a CDH (see Figures 11-39, A and B).106 With the infant supine, the examiner flexes the hips and grasps the legs so that the examiner’s thumbs are against the insides of the knees and thighs, and the fingers are placed along the outsides of the thighs to the buttocks. With gentle traction, the thighs are abducted and pressure is applied against the greater trochanters of the femora. Resistance to abduction and lateral rotation begins to be felt at approximately 30° to 40°. The examiner may feel a click, clunk, or jerk, which indicates a positive test and that the hip has reduced; in addition, increased abduction of the hip is obtained. The femoral head has slipped over the acetabular ridge into the acetabulum, and normal abduction of 70° to 90° can be obtained.
This test is valid only for the first few weeks after birth and only for dislocated and lax hips, not for dislocations that are difficult to reduce. The examiner should take care to feel the quality of the click. Soft clicks may occur without dislocation and are thought to be caused by the iliofemoral ligament’s clicking over the anterior surface of the head of the femur as it is laterally rotated. Soft clicking usually occurs without the prior resistance that is seen with dislocations. By repeated rotation of the hip, the exact location of the click can be palpated. However, Ortolani’s test should not be repeated too often because it could lead to damage of the articular cartilage of the femoral head. As with all clinical tests, if the test is positive, it is highly suggestive that the problem (i.e., CDH) exists, but if it is negative, it does not necessarily rule out the problem.
 Telescoping Sign (Piston or Dupuytren’s Test).133
Telescoping Sign (Piston or Dupuytren’s Test).133
The telescoping sign is evident in a child with a dislocated hip. The child lies in the supine position. The examiner flexes the knee and hip to 90°. The femur is pushed down onto the examining table. The femur and leg are then lifted up and away from the table (Figure 11-41). With the normal hip, little movement occurs with this action. With the dislocated hip, however, there is a lot of relative movement. This excessive movement is called telescoping, or pistoning.
Tests for Leg Length
There are two types of leg length discrepancy. The first, called true leg length discrepancy or true shortening, is caused by an anatomic or structural change in the lower leg resulting from congenital maldevelopment (e.g., adolescent coxa vara, congenital hip dysplasia, bony abnormality) or trauma (e.g., fracture). Because an anatomic short leg results, the spine and pelvis are often affected, leading to lateral pelvic tilt and scoliosis.135,136
The second type of leg length discrepancy is called functional leg length discrepancy or functional shortening, and it is the result of compensation for a change that may have occurred because of positioning rather than structure. For example, a functional leg length discrepancy could occur because of unilateral foot pronation or spinal scoliosis.135,136
 True Leg Length.
True Leg Length.
Before any measuring is done, the examiner must set the pelvis square, level, or in balance with the lower limbs.137–139 The legs should be 15 to 20 cm (4 to 8 inches) apart and parallel to each other (Figure 11-42). If the legs are not placed in proper relation to the pelvis, apparent shortening of the limb may occur. The lower limbs must be placed in comparable positions relative to the pelvis, because abduction of the hip brings the medial malleolus closer to the ASIS on the same side and adduction of the hip takes the medial malleolus farther from the ASIS on the same side. If one hip is fixed in abduction or adduction as a result of contracture or some other cause, the normal hip should be adducted or abducted an equal amount to ensure accurate leg length measurement.

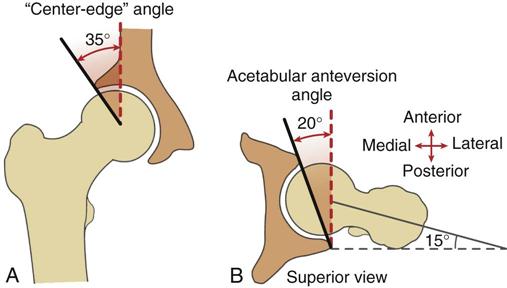
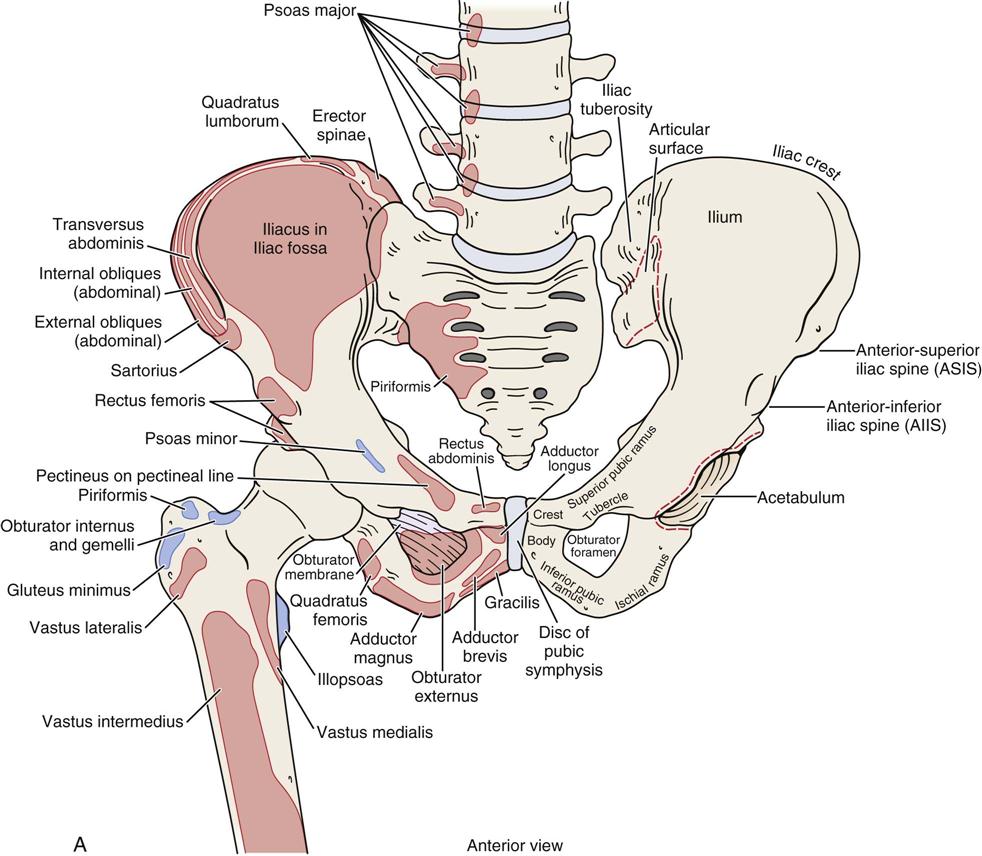
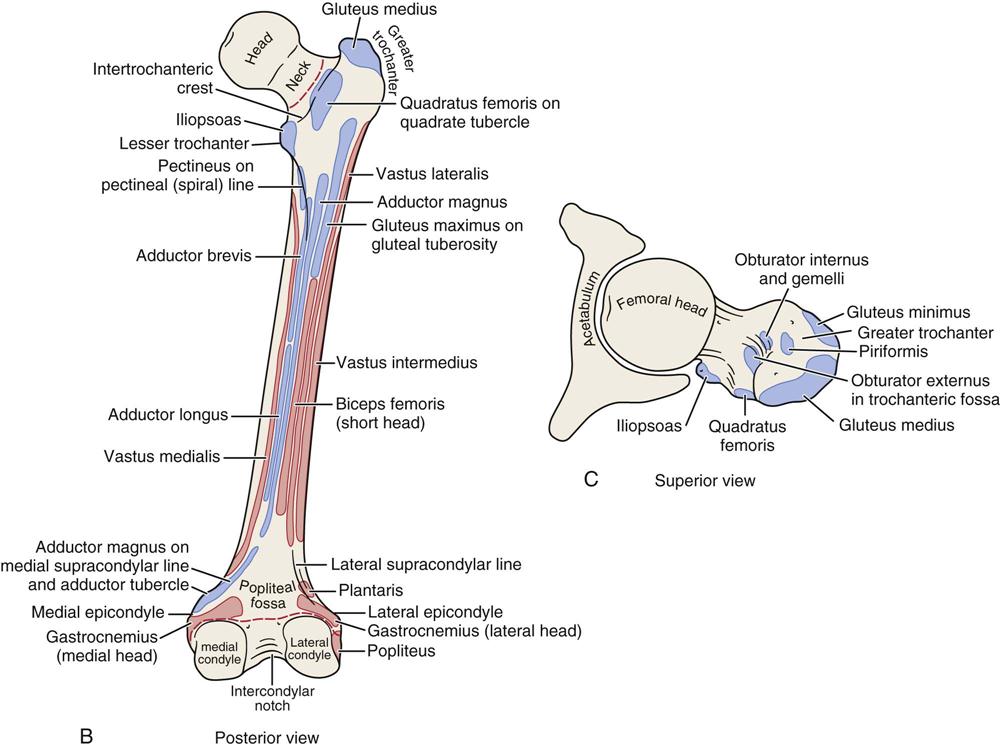
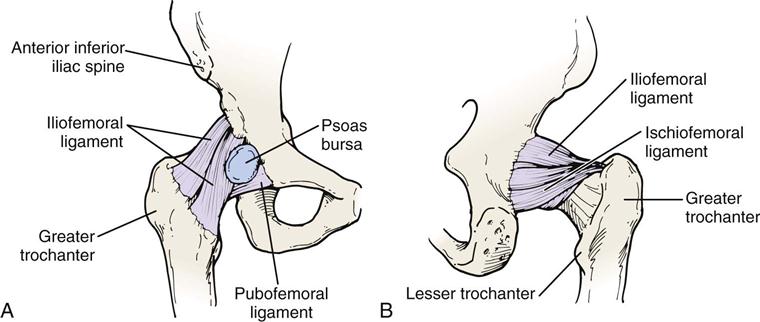
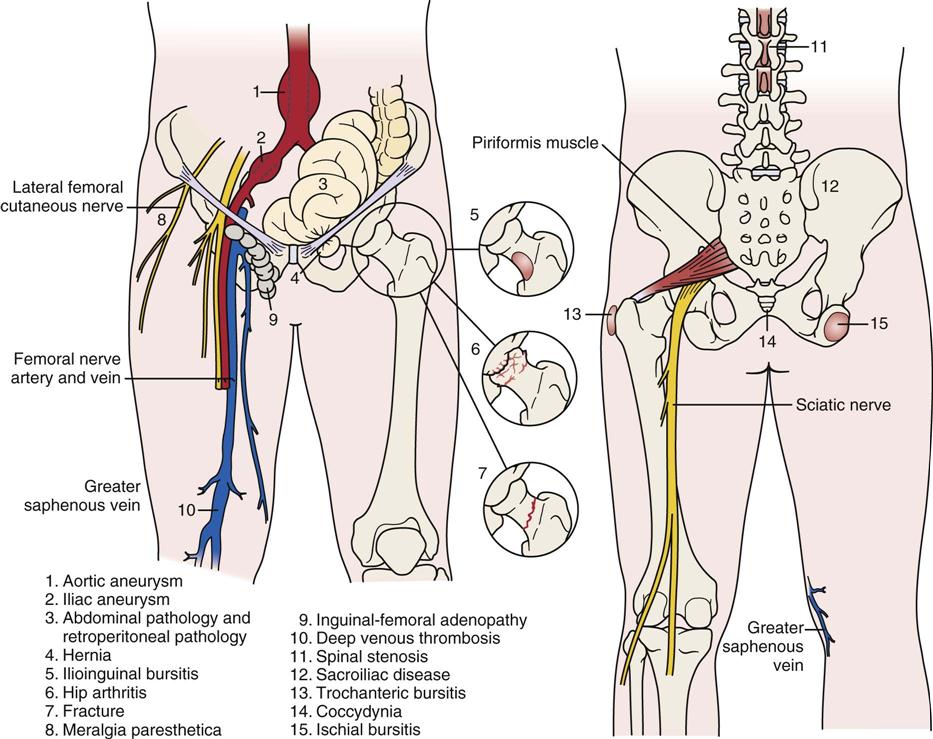

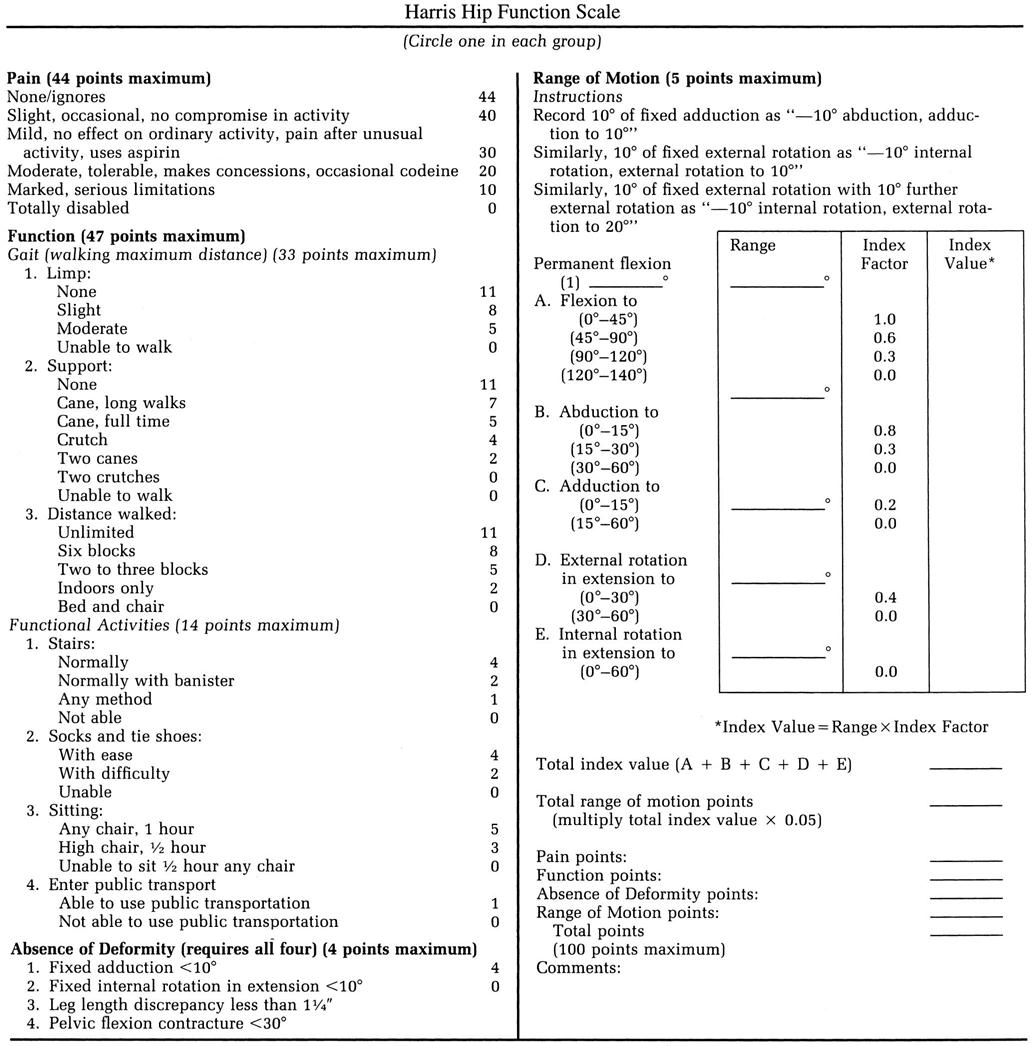
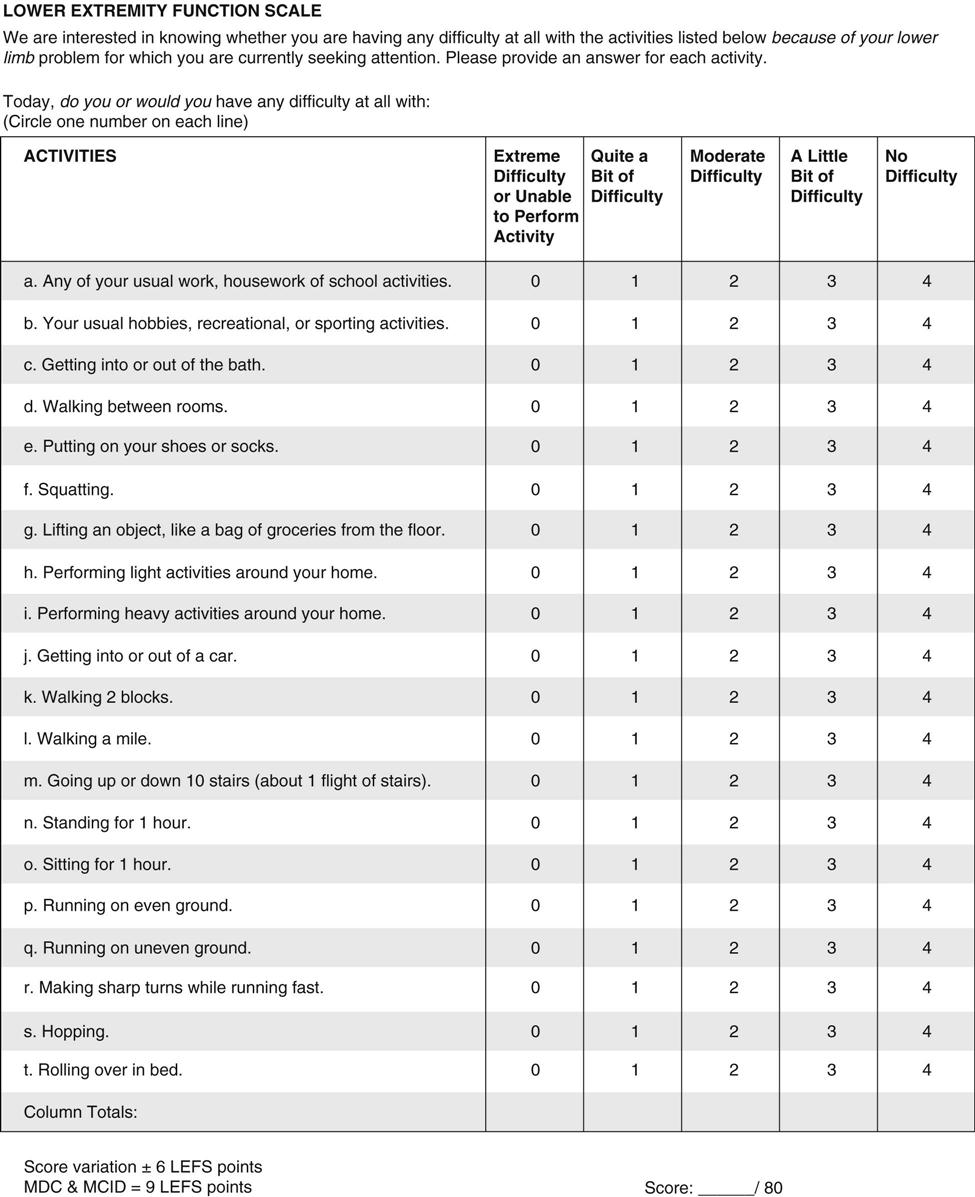
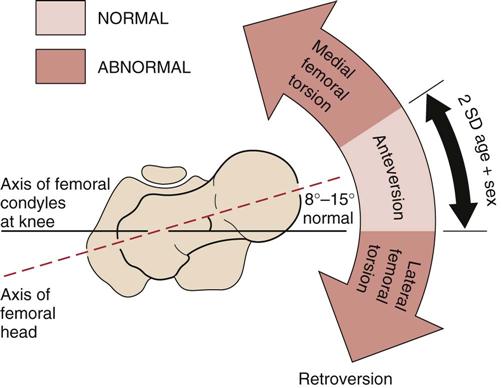
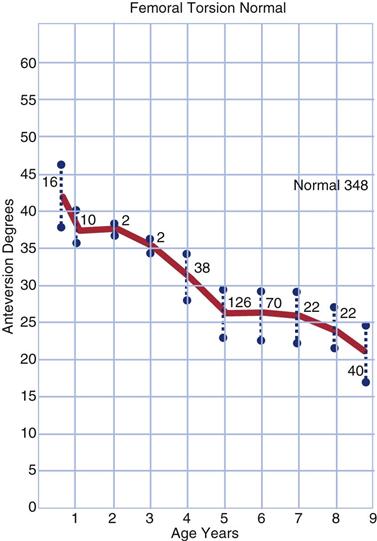
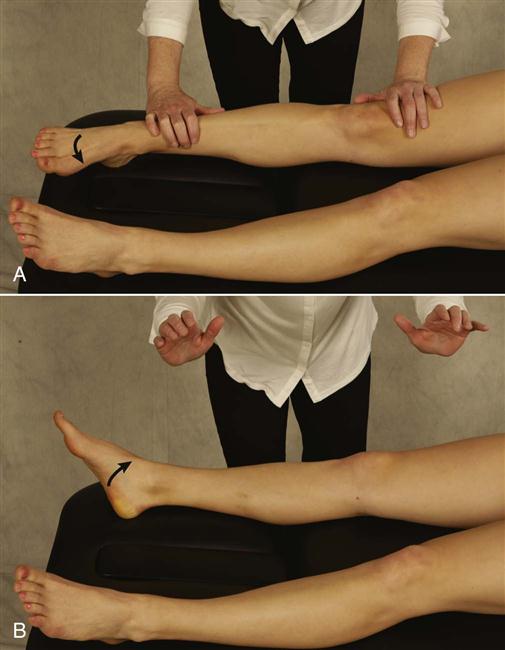
 Figure 11-24
Figure 11-24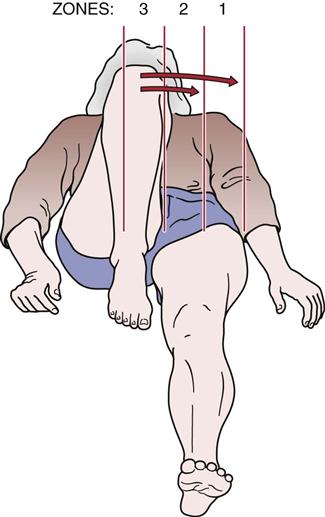
 Figure 11-25
Figure 11-25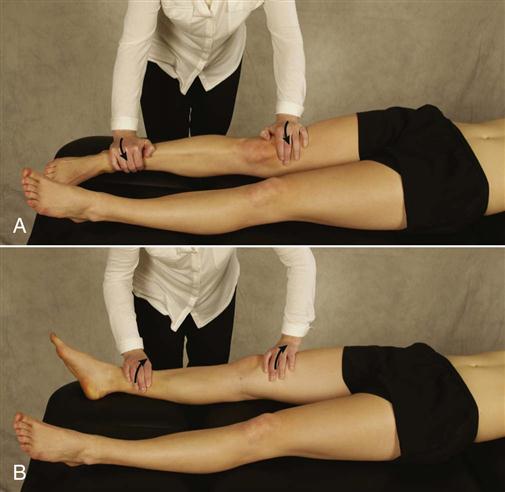
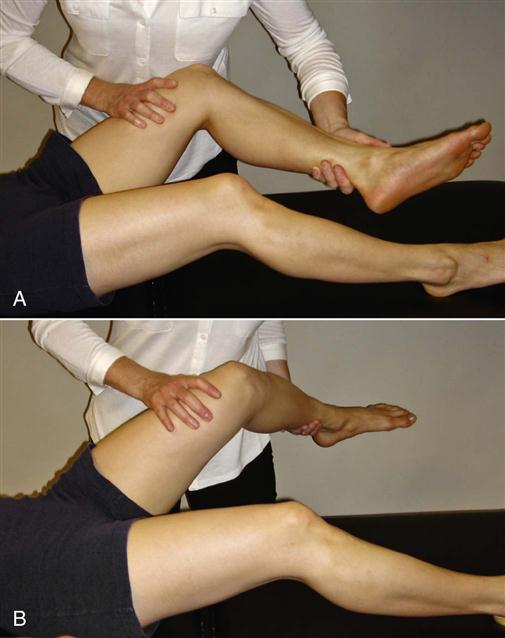
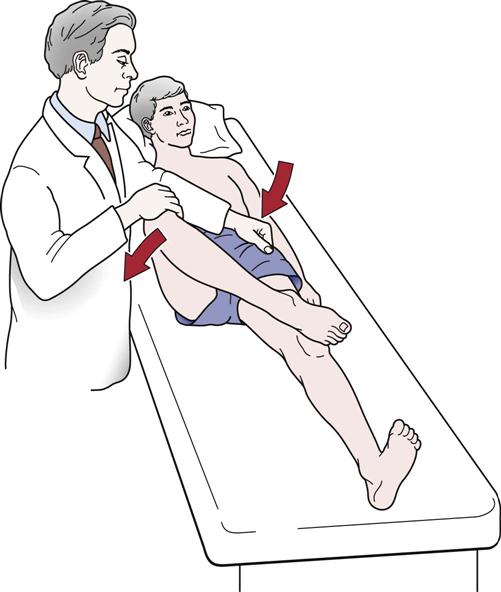
 Figure 11-31
Figure 11-31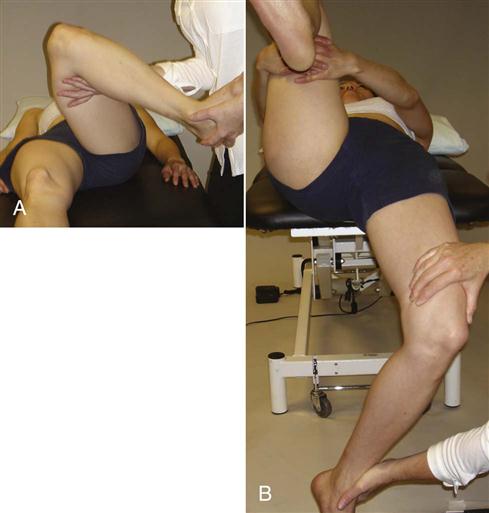
 Figure 11-34
Figure 11-34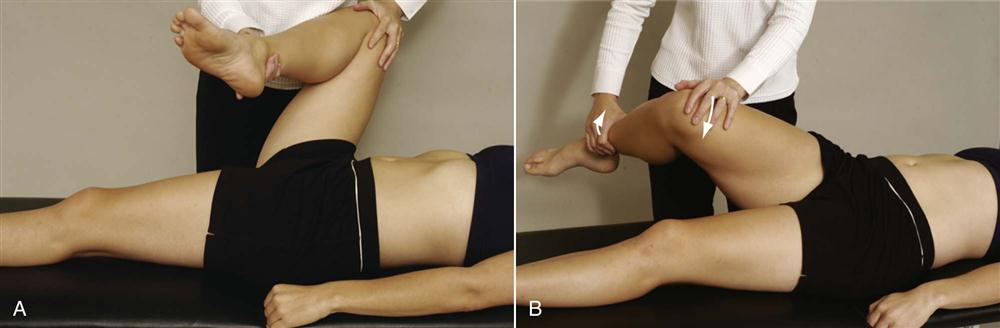
 Figure 11-35
Figure 11-35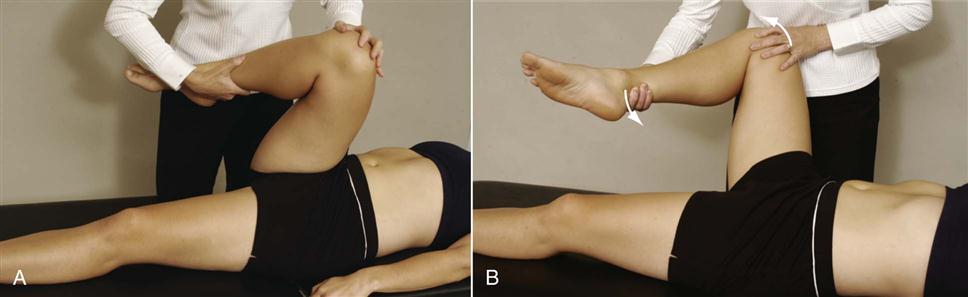
 Figure 11-36
Figure 11-36