High-frequency ventilation
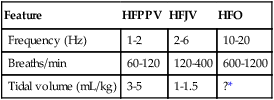
Table 160-1 compares the major types of HFV. HFPPV can be delivered by a standard mechanical ventilator, though most are not designed to achieve rates greater than 60 to 100/min.
Table 160-1
General Comparison of the Major Types of High-Frequency Ventilation
| Feature | HFPPV | HFJV | HFO |
| Frequency (Hz) | 1-2 | 2-6 | 10-20 |
| Breaths/min | 60-120 | 120-400 | 600-1200 |
| Tidal volume (mL/kg) | 3-5 | 1-1.5 | ?* |