Chapter 69 Hematologic Manifestations of Liver Disease
Management of Coagulopathy in Liver Disease
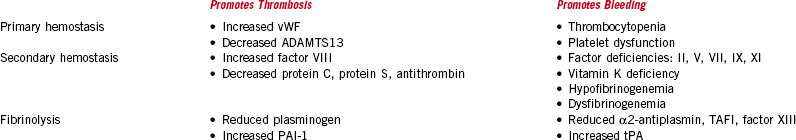
• Actively bleeding patients should be adequately resuscitated and stabilized with crystalloid or colloid solutions (or both). Admission to the intensive care setting may be appropriate.
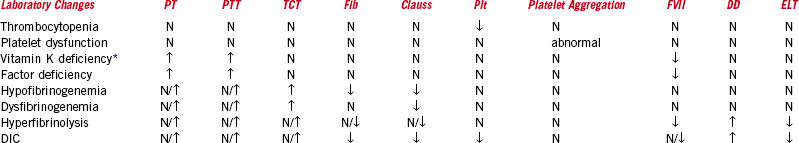
• Basic coagulation tests should be ordered to identify the cause of bleeding; these include CBC, PT (INR), PTT, thrombin clotting time, fibrinogen, D-Dimer, FDP, and mixing studies. The need for more specialized tests will be dictated by the clinical situation and response to therapy.
• It is important to identify any localized source of bleeding (e.g., varices) amenable to procedural intervention because this will assist in achieving hemostasis.
• A trial of 5 to 10 mg of vitamin K is reasonable in asymptomatic patients with prolonged PT and PTT but should be used with other therapies in actively bleeding patients.
• Platelet transfusions can be used, targeting counts greater than 50 × 109/L.
• In patients who can tolerate volume, FFP 4 to 6 units (1000-1500 mL) given over 1 to 2 hours can be used to replace coagulation factors. Coagulation parameters should be monitored to document effect and determine the timing and need for additional units.
• Dysfibrinogenemia or hypofibrinogenemia should be suspected if coagulation assays do not correct with FFP or fibrinogen levels are low, respectively. Replacement can be attempted with 10 to 20 units of cryoprecipitate while following laboratory results.
• Patients who are intravascularly overloaded or who do not respond to FFP should be considered for rFVIIa. Low doses of rFVIIa (25-50 µg/kg) are generally used, and repeated doses may be required because of the short half-life of 2 to 3 hours. rFVIIa may thus be most suitable as a temporizing measure to enable invasive procedures or hemostasis to be achieved by other means. Avoid use in the setting of DIC.