130 Heat-Related Emergencies
• Heat stroke is a life-threatening hyperthermic syndrome characterized by central nervous system dysfunction and associated multisystem organ failure.
• The main goal of therapy is rapid reduction of the patient’s core temperature to about 39° C with one of two methods—evaporative cooling or cold water immersion.
Perspective
Heat-related injury spans a wide spectrum from the unpleasant and transient conditions of heat cramps or prickly heat to the life-threatening multisystem organ failure of heat stroke. The most important risk factors for heat illness are listed in Box 130.1. Mechanisms of acclimatization are listed in Table 130.1.
| Cardiac | Increased cardiac performance: higher cardiac output |
| Vascular |
Epidemiology
Roughly 688 people die yearly of heat-related causes, Arizona has the highest incidence at 1.7 per 100,000, followed by Nevada (0.8 per 100,000) and Missouri (0.6 per 100,000).1 An estimated half of the deaths are weather related, and 5% result from being enclosed in motor vehicles, boiler rooms, or kitchens; in the remaining cases, the causes are unspecified.2 Mortality from heat stroke with appropriate treatment is reported to be between 0% and 28%.3–5
Pathophysiology of Heat Stroke
Heat itself has a direct cytotoxic effect and causes cell death over a period of 45 minutes to 8 hours at body temperatures of 41.6° C to 42° C6; below these temperatures, cell death can still occur through apoptosis.7
Figure 130.1 diagrams the current understanding of the pathophysiology of heat stroke.
Minor Heat-Related Syndromes
Presenting Signs and Symptoms
As stated earlier, heat-related illness is a continuum. Table 130.2 summarizes the various types of heat illness.
| DIAGNOSIS | KEY FEATURES | TREatMENT |
|---|---|---|
| Mild | ||
| Heat edema | Mild edema of the hands and feet as a result of interstitial edema | |
Treatment
Most minor heat-related syndromes are mild and require simple or no treatment. Treatment is summarized in Table 130.2 for these conditions.
Follow-up, Next Steps in Care, and Patient Education
![]() Patient Teaching Tips
Patient Teaching Tips
Heat Illness
The three main types of heat illness are heat cramps, heat exhaustion, and heat stroke.
Heat cramps are painful muscle spasms and a mild form of heat illness that occur when you sweat too much or do not drink enough fluids.
Heat exhaustion is due to dehydration and is more serious.
Heat stroke is marked by severe dehydration and confusion secondary to overheating; it is life-threatening.
Athletics and Strenuous Labor
Drink 500 mL of water or sports drink 2 hours before vigorous exercise or work.
Continue to replace 250 mL of fluid for every 20 minutes of exertion and replace 150% of weight loss with fluid after exertion.
Acclimatization takes at least 2 weeks, and a gradual increase in activity is recommended to safely adjust to hotter environments.
Treatment of Heat Illness
If you have serious heat illness, you may feel lightheaded, nauseated, tired, anxious, and confused.
Get out of the heat into a cool, shaded place or air-conditioned building, and take off some clothing.
Put cold water or cold wet towels on your skin, and drink cold liquids.
If you are confused or lethargic or have a fever, seek medical attention immediately.
Severe Heat-Related Syndromes
Presenting Signs and Symptoms
Heat Stroke
The classic definition of heat stroke was a core body temperature higher than 40° C, CNS dysfunction, and anhydrosis. However, many cases of heat stroke have been reported in which sweating was present and the core temperature was not higher than 40° C. Therefore, the definition has been amended to a form of hyperthermia associated with a systemic inflammatory response leading to a syndrome of multiorgan dysfunction in which encephalopathy predominates.8
Differential Diagnosis and Decision Making
Many other conditions are associated with elevated core body temperature and altered mental status. Box 130.2 contains an extensive list. The EP should regard infection as a strong possibility in patients with these signs. Toxicologic, neurologic (e.g., hemorrhage, seizures), and endocrinologic (e.g., thyroid storm) causes should also be kept in mind and appropriate neuroimaging and laboratory workup ordered. Many cases of heat stroke involve victims with concomitant substance abuse, overdose, or psychiatric illnesses. Evaluation for common overdoses, medication toxicities and substances of abuse should be performed. Additionally, heat stroke often occurs in patients who have significant comorbid conditions, such as cardiac or respiratory diseases, or have another concomitant acute illness, such as infection. Therefore, it is reasonable to assess cardiac function, perform a sepsis evaluation, and evaluate for any additional conditions that the EP suspects.
Box 130.2 Differential Diagnosis of Heat Stroke
Tips and Tricks
Both neuroleptic malignant syndrome and heat stroke cause altered mental status and hyperthermia; unlike patients with heat stroke, however, all patients with neuroleptic malignant syndrome also have extrapyramidal rigidity.
Hospital maintenance often has large fans used to dry hospital floors, which can be used to enhance evaporative cooling of a patient with heat illness.
Diagnostic Testing
Heat stroke is a clinical diagnosis, but associated multiorgan dysfunction may be present. Therefore, the EP must assess the patient for the severity of dysfunction to provide appropriate supportive management. Examples of multiorgan dysfunction seen in patients with heat stroke are listed in Box 130.3.
Treatment
Prehospital Management
Continuous monitoring and assessment of core body temperature every 5 to 10 minutes are also recommended. The ability and resources to execute these measures will vary significantly according to the setting (wilderness versus an ironman triathlon medical tent), but even simple measures such as those recommended by the Israeli defense forces—splashing 20 to 40 mL of water on the skin and fanning the person or driving the person in an open car—effectively cool the core body temperature at a rate of 0.14° C/min.9
Hospital Management
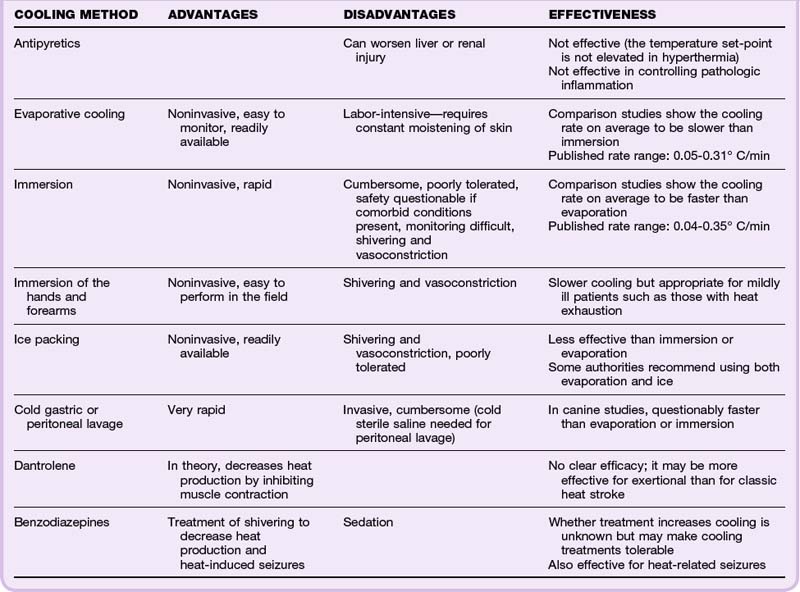
The EP’s main goal is to cool the core body temperature to 38.5° C or 39° C as quickly as possible. Active cooling is not continued to normothermic temperatures to avoid the risk of overshooting and causing hypothermia. Usually, significant improvement is noted in the patient’s cardiovascular stability and mental status immediately after cooling. Methods of body cooling are defined in Table 130.3.
| Immersion | Placement of the body into a bath of cold or iced water |
| Immersion of extremities | Putting only the hands and forearms in iced water |
| Evaporative cooling | Spraying tepid water or placing a wet sheet on the skin with a fan to facilitate evaporation |
| Ice packing | Application of ice or cold packs to the groin, axilla, and neck |
| Invasive measures | |
| Gastric lavage | Lavage with iced water via a nasogastric tube |
| Peritoneal lavage | Lavage with sterile cold water |
| Dantrolene, 2-4 mg/kg | Decreases muscle contraction and, in theory, reduces heat production |
| Benzodiazepines | Theoretically, control shivering and heat production |
Debate and research continue about which cooling method is most effective and safest in treating heat stroke. Current research does not definitively answer the question of whether water immersion or evaporative cooling is significantly more effective. However, most evidence indicates that cold water immersion is superior for exertional heat stroke and that the cooler the immersion water bath, the faster the cooling,5,10,11 whereas for classic heat stroke both methods are thought to be equally effective. Additionally, if temperature can be reduced within 30 to 60 minutes, the risk for mortality is decreased.11 The choice often depends on which method can be instituted more quickly and effectively. Cold water immersion may be most useful when planned in advance for event medicine and other field applications. Evaporative cooling with the application of ice packs is a practical and effective method that can be instituted with equipment normally available in the emergency department (ED). Ice packs, wet sheets, and a fan will provide rapid cooling. Table 130.4 lists the advantages, disadvantages, and efficacy of various cooling methods.
Hypotension
Hypotension is a common problem in patients with heat stroke and should be treated aggressively with fluid boluses, which are generally adequate. Central venous pressure of 3 to 8 mm Hg is targeted.5 If the patient’s blood pressure remains unresponsive, vasopressors are indicated. One study used isoproterenol (β-adrenergic agonist) to increase peripheral blood flow and cutaneous circulation, but this agent is used infrequently and is unlikely to result in a significant rise in blood pressure.12 An α-adrenergic agent (e.g., dopamine, which is commonly used) may be more effective in raising blood pressure but has the theoretic disadvantage of causing peripheral vasoconstriction and hence diminishing cutaneous perfusion when given in higher doses.
Follow-up, Next Steps in Care, and Patient Education
Prognosis
The prognosis of patients with heat exhaustion and more mild forms of heat illness is good, and no long-term morbidity is anticipated. The prognosis of patients with heat stroke depends on the severity, underlying comorbid conditions, and time elapsed until appropriate cooling. Mortality between 0% and 28% with appropriate treatment is reported. Survivors of exertional heatstroke that is treated aggressively rarely have long-term sequelae, whereas up to one third of survivors of classic heat stroke will have moderate to severe neurologic sequelae.1 Independent risk factors for mortality include hypotension (systolic blood pressure < 90 mm Hg), temperature higher than 42° C, and a Glasgow Coma Scale score lower than 12.4.
Pitfalls
![]() Priority Actions
Priority Actions
Use advanced cardiac life support principles to assess and monitor cardiac and respiratory stability.
Obtain intravenous access, as well as cardiac and core temperature monitoring, and place a Foley catheter for monitoring urine output and core temperature continuously.
Start cooling measures immediately, preferably in the field if possible with either immersion or evaporative cooling.
Actively cool the patient as quickly and safely as possible to a core temperature of 38.5° C to 39° C.
Continue monitoring for rebound hyperthermia.
Assess for other organ dysfunction and intercurrent illness.
Bouchama A, Dehbi M, Chaves-Carballo E. Cooling and hemodynamic management in heatstroke: practical recommendations. Crit Care. 2007;11:R54.
Lugo-Amador NM, Rauthenhaus T, Moyer P. Heat-related illness. Emerg Med Clin North Am. 2004;22:305–327.
Smith JE. Cooling methods used in the treatment of exertional heat illness. Br J Sports Med. 2005;39:503–507.
1 Centers for Disease Control and Prevention (CDC). Heat-related deaths—United States, 1999-2003. MMWR Morb Mortal Wkly Rep. 2006;55(29):796–798.
2 Centers for Disease Control and Prevention (CDC). Heat-related deaths—four states, July-August 2001, and United States 1979-1999. MMWR Morb Mortal Wkly Rep. 2002;51(26):567–570.
3 Lugo-Amador NM, Rauthenhaus T, Moyer P. Heat-related illness. Emerg Med Clin North Am. 2004;22:305–327.
4 LoVecchio F, Pizon A, Berrett C, et al. Outcomes after environmental hyperthermia. Am J Emerg Med. 2007;25:442–445.
5 Bouchama A, Dehbi M, Chaves-Carballo E. Cooling and hemodynamic management in heatstroke: practical recommendations. Crit Care. 2007;11:R54.
6 Bynum GD, Pandolf KB, Schuette WH, et al. Induced hyperthermia in sedated humans and the concept of critical thermal maximum. Am J Physiol. 1978;235:R228–R236.
7 Sakaguchi Y, Stephens LC, Makino M, et al. Apoptosis in tumors and normal tissues induced by whole body hyperthermia in rats. Cancer Res. 1995;55:5459–5464.
8 Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–1988.
9 Hadad E, Rav-Acha M, Heled Y, et al. Heat stroke: a review of cooling methods. Sports Med. 2004;34:501–511.
10 McDermott BP, Casa DJ, Ganio MS, et al. Acute whole-body cooling for exercise induced hyperthermia: a systematic review. J Athl Train. 2009;44:84–93.
11 Smith JE. Cooling methods used in the treatment of exertional heat illness. Br J Sports Med. 2005;39:503–507.
12 O’Donnell TF, Clowes GHA. The circulatory abnormalities of heat stroke. N Engl J Med. 1972;287:734–737.