8
Head and Neck
Vestibulocochlear nerve [VIII]
Temporal and infratemporal fossae
Posterior triangle of the neck
Gaps in the pharyngeal wall and structures passing through them
ADDITIONAL LEARNING RESOURCES FOR CHAPTER 8, HEAD AND NECK, ON STUDENT CONSULT (www.studentconsult.com)
 Image Library — illustrations of head and neck anatomy, Chapter 8
Image Library — illustrations of head and neck anatomy, Chapter 8
 Self-Assessment — National Board style multiple-choice questions, Chapter 8
Self-Assessment — National Board style multiple-choice questions, Chapter 8
 Short Questions — these are questions requiring short responses, Chapter 8
Short Questions — these are questions requiring short responses, Chapter 8
 Interactive Surface Anatomy — interactive surface animations, Chapter 8
Interactive Surface Anatomy — interactive surface animations, Chapter 8
Stenosis of the internal carotid artery
Posterior communicating artery aneurysm
Regional anatomy
The head and neck are anatomically complex areas of the body. The head is composed of a series of compartments, which are formed by bone and soft tissues (Fig. 8.1). They are:
Fig. 8.1 Overall design of head and neck.
The neck extends from the head above to the shoulders and thorax below (Fig. 8.1). The neck has four major compartments (Fig. 8.2), which are enclosed by an outer musculofascial collar:
 The vertebral compartment contains the cervical vertebrae and associated postural muscles.
The vertebral compartment contains the cervical vertebrae and associated postural muscles.
Fig. 8.2 Major compartments of the neck.
HEAD
 Houses and protects the brain and all the receptor systems associated with the special senses—the nasal cavities associated with smell, the orbits with vision, the ears with hearing and balance, and the oral cavity with taste.
Houses and protects the brain and all the receptor systems associated with the special senses—the nasal cavities associated with smell, the orbits with vision, the ears with hearing and balance, and the oral cavity with taste.
NECK
 Supports and positions the head. Importantly, it enables an individual to position sensory systems in the head relative to environmental cues without moving the entire body.
Supports and positions the head. Importantly, it enables an individual to position sensory systems in the head relative to environmental cues without moving the entire body.
The head and neck together function in communication. Sounds produced by the larynx are modified in the pharynx and oral cavity to produce speech. In addition, the muscles of facial expression adjust the contours of the face to relay nonverbal signals.
SKULL
The skull has 22 bones, excluding the ossicles of the ear. Except for the mandible, which forms the lower jaw, the bones of the skull are attached to each other by sutures, are immobile, and form the cranium.
The cranium can be subdivided into:
 an upper domed part (the calvaria), which covers the cranial cavity containing the brain;
an upper domed part (the calvaria), which covers the cranial cavity containing the brain;
 a base that consists of the floor of the cranial cavity; and
a base that consists of the floor of the cranial cavity; and
 a lower anterior part—the facial skeleton (viscerocranium).
a lower anterior part—the facial skeleton (viscerocranium).
The bones forming the calvaria are mainly the paired temporal and parietal bones, and parts of the unpaired frontal, sphenoid, and occipital bones.
The bones forming the base of the cranium are mainly parts of the sphenoid, temporal, and occipital bones.
The bones forming the facial skeleton are the paired nasal bones, palatine bones, lacrimal bones, zygomatic bones, maxillae, inferior nasal conchae, and the unpaired vomer.
The mandible is not part of the cranium nor part of the facial skeleton.
Anterior view
The anterior view of the skull includes the forehead superiorly, and, inferiorly, the orbits, the nasal region, the part of the face between the orbit and the upper jaw, the upper jaw, and the lower jaw (Fig. 8.3; also see Fig. 8.4).
Fig. 8.3 Anterior view of the skull.
Imaging app
Visualizing the skull—anterior view
Fig. 8.4 Volume-rendered anterior view using multidetector computed tomography.
Frontal bone
The forehead consists of the frontal bone, which also forms the superior part of the rim of each orbit (Fig. 8.3).
Just superior to the rim of the orbit on each side are the raised superciliary arches. These are more pronounced in men than in women. Between these arches is a small depression (the glabella).
Clearly visible in the medial part of the superior rim of each orbit is the supra-orbital foramen (supra-orbital notch; Table 8.1).
Table 8.1 External foramina of the skull
|
Foramen |
Structures passing through foramen |
|
Anterior view |
|
|
Supra-orbital foramen |
Supra-orbital nerve and vessels |
|
Infra-orbital foramen |
Infra-orbital nerve and vessels |
|
Mental foramen |
Mental nerve and vessels |
|
Lateral view |
|
|
Zygomaticofacial foramen |
Zygomaticofacial nerve |
|
Superior view |
|
|
Parietal foramen |
Emissary veins |
|
Inferior view |
|
|
Incisive foramina |
Nasopalatine nerve; sphenopalatine vessels |
|
Greater palatine foramen |
Greater palatine nerve and vessels |
|
Lesser palatine foramina |
Lesser palatine nerve and vessels |
|
Pterygoid canal |
Pterygoid nerve and vessels |
|
Foramen ovale |
Mandibular nerve [V3]; lesser petrosal nerve |
|
Foramen spinosum |
Middle meningeal artery |
|
Foramen lacerum |
Filled with cartilage |
|
Carotid canal |
Internal carotid artery and nerve plexus |
|
Foramen magnum |
Continuation of brain and spinal cord; vertebral arteries and nerve plexuses; anterior spinal artery; posterior spinal arteries; roots of accessory nerve [XI]; meninges |
|
Condylar canal |
Emissary veins |
|
Hypoglossal canal |
Hypoglossal nerve [XII] and vessels |
|
Jugular foramen |
Internal jugular vein; inferior petrosal sinus; glossopharyngeal nerve [IX]; vagus nerve [X]; accessory nerve [XI] |
|
Stylomastoid foramen |
Facial nerve [VII] |
Medially, the frontal bone projects inferiorly forming a part of the medial rim of the orbit.
Laterally, the zygomatic process of the frontal bone projects inferiorly, forming the upper lateral rim of the orbit. This process articulates with the frontal process of the zygomatic bone.
Zygomatic and nasal bones
The lower lateral rim of the orbit, as well as the lateral part of the inferior rim of the orbit, is formed by the zygomatic bone (the cheekbone) (Fig. 8.3).
Superiorly, in the nasal region, the paired nasal bones articulate with each other in the midline and with the frontal bone superiorly. The center of the frontonasal suture formed by the articulation of the nasal bones and the frontal bone is the nasion.
Laterally, each nasal bone articulates with the frontal process of each maxilla.
Inferiorly, the piriform aperture is the large opening in the nasal region and the anterior opening of the nasal cavity. It is bounded superiorly by the nasal bones and laterally and inferiorly by each maxilla.
Visible through the piriform aperture are the fused nasal crests, forming the lower part of the bony nasal septum and ending anteriorly as the anterior nasal spine, and the paired inferior nasal conchae
Maxillae
The part of the face between the orbit and the upper teeth and each upper jaw is formed by the paired maxillae (Fig. 8.3).
Superiorly, each maxilla contributes to the inferior and medial rims of the orbit.
Laterally, the zygomatic process of each maxilla articulates with the zygomatic bone and medially, the frontal process of each maxilla articulates with the frontal bone.
Inferiorly, the part of each maxilla, lateral to the opening of the nasal cavity, is the body of maxilla.
On the anterior surface of the body of maxilla, just below the inferior rim of the orbit, is the infra-orbital foramen (Table 8.1).
Inferiorly, each maxilla ends as the alveolar process, which contains the teeth and forms the upper jaw.
Mandible
The lower jaw (mandible) is the most inferior structure in the anterior view of the skull (see Fig. 8.3). It consists of the body of mandible anteriorly and the ramus of mandible posteriorly. These meet posteriorly at the angle of mandible. All these parts of the mandible are visible, to some extent, in the anterior view.
The body of mandible is arbitrarily divided into two parts:
 The lower part is the base of mandible.
The lower part is the base of mandible.
 The upper part is the alveolar part of mandible
The upper part is the alveolar part of mandible
The alveolar part of mandible contains the teeth and is resorbed when the teeth are removed. The base of mandible has a midline swelling (the mental protuberance) on its anterior surface where the two sides of the mandible come together. Just lateral to the mental protuberance, on either side, are slightly more pronounced bumps (mental tubercles).
Laterally, a mental foramen (see Table 8.1) is visible halfway between the upper border of the alveolar part of mandible and the lower border of the base of mandible. Continuing past this foramen is a ridge (the oblique line) passing from the front of the ramus onto the body of mandible. The oblique line is a point of attachment for muscles that depress the lower lip.
Lateral view
The lateral view of the skull consists of the lateral wall of the cranium, which includes lateral portions of the calvaria and the facial skeleton, and half of the lower jaw (Fig. 8.5; see also Fig. 8.6):
 The mandible forms the visible part of the lower jaw.
The mandible forms the visible part of the lower jaw.
Fig. 8.5 Lateral view of the skull.
Imaging app
Visualizing the skull—lateral view
Fig. 8.6 Volume-rendered lateral view using multidetector computed technology.
Lateral portion of the calvaria
The lateral portion of the calvaria begins anteriorly with the frontal bone. In upper regions, the frontal bone articulates with the parietal bone at the coronal suture (Fig. 8.5). The parietal bone then articulates with the occipital bone at the lambdoid suture.
In lower parts of the lateral portion of the calvaria, the frontal bone articulates with the greater wing of sphenoid bone (Fig. 8.5), which then articulates with the parietal bone at the sphenoparietal suture, and with the anterior edge of the temporal bone at the sphenosquamous suture.
The junction where the frontal, parietal, sphenoid, and temporal bones are in close proximity is the pterion (Fig. 8.5). The clinical consequences of a skull fracture in this area can be very serious. The bone in this area is particularly thin and overlies the anterior division of the middle meningeal artery, which can be torn by a skull fracture in this area, resulting in an extradural hematoma.
The final articulation across the lower part of the lateral portion of the calvaria is between the temporal bone and the occipital bone at the occipitomastoid suture (Fig. 8.5).
Temporal bone
A major contributor to the lower portion of the lateral wall of the cranium is the temporal bone (Fig. 8.5), which consists of several parts:
The mastoid part is the most posterior part of the temporal bone, and is the only part of the petromastoid part of the temporal bone seen on a lateral view of the skull. It is continuous with the squamous part of the temporal bone anteriorly, and articulates with the parietal bone superiorly at the parietomastoid suture, and with the occipital bone posteriorly at the occipitomastoid suture. These two sutures are continuous with each other, and the parietomastoid suture is continuous with the squamous suture.
Inferiorly, a large bony prominence (the mastoid process) projects from the inferior border of the mastoid part of the temporal bone (Fig. 8.5). This is a point of attachment for several muscles.
Medial to the mastoid process, the styloid process projects from the lower border of the temporal bone.
Visible part of the facial skeleton
The bones of the viscerocranium visible in a lateral view of the skull include the nasal, maxilla, and zygomatic bones (Fig. 8.5) as follows:
Usually a small foramen (the zygomaticofacial foramen; see Table 8.1) is visible on the lateral surface of the zygomatic bone. A zygomaticotemporal foramen is present on the medial deep surface of the bone.
Mandible
The final bony structure visible in a lateral view of the skull is the mandible. Inferiorly in the anterior part of this view, it consists of the anterior body of mandible, a posterior ramus of mandible, and the angle of mandible where the inferior margin of the mandible meets the posterior margin of the ramus (Fig. 8.5).
The teeth are in the alveolar part of the body of mandible and the mental protuberance is visible in this view.
The mental foramen is on the lateral surface of the body and on the superior part of the ramus, a condylar and coronoid process extend upward.
The condylar process is involved in articulation of the mandible with the temporal bone, and the coronoid process is the point of attachment for the temporalis muscle.
Anatomical position of the head and major landmarks
The head is in the anatomical position when the inferior margins of the bony orbits and the superior margins of the external acoustic meatuses are in the same horizontal plane (Frankfort plane).
In addition to the external acoustic meatus and the bony margin of the orbit, other features that are palpable include the head of mandible, zygomatic arch, zygomatic bone, mastoid process, and external occipital protuberance (Fig. 8.7).
Fig. 8.7 Anatomical position of the head and major landmarks. Lateral head and neck of a man.
The head of mandible is anterior to the external ear and behind and inferior to the posterior end of the zygomatic arch. It is best found by opening and closing the jaw and palpating the head of mandible as it moves forward onto the articular tubercle and then back into the mandibular fossa, respectively.
The zygomatic arch extends forward from the region of the temporomandibular joint to the zygomatic bone, which forms a bony prominence lateral to the inferior margin of the anterior opening of the orbit.
The mastoid process is a large bony protuberance that is easily palpable posterior to the inferior aspect of the external acoustic meatus. The superior end of the sternocleidomastoid muscle attaches to the mastoid process.
The external occipital protuberance is palpable in the midline posteriorly where the contour of the skull curves sharply forward. This landmark marks the point superficially where the back of the neck joins the head.
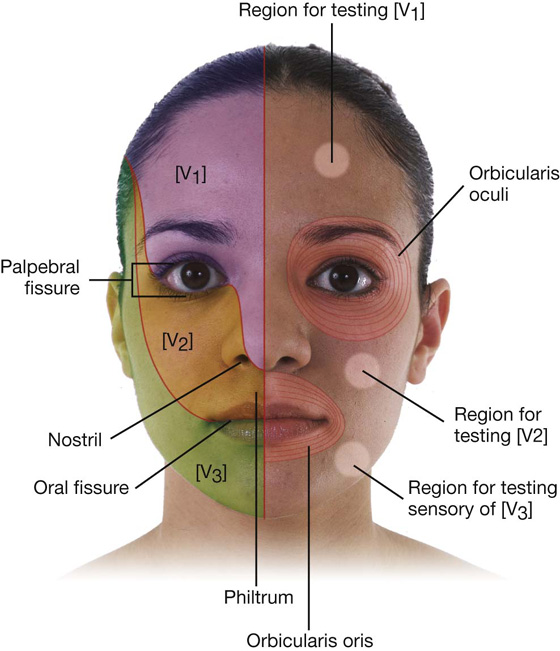
Another clinically useful feature of the head is the vertex. This is the highest point of the head in the anatomical position and marks the approximate point on the scalp where there is a transition from cervical to cranial innervation of the scalp. Anterior to the vertex the scalp and face are innervated by the trigeminal nerve [V]. Posterior to the vertex, the scalp is innervated by branches from cervical spinal nerves.
Posterior view
The occipital, parietal, and temporal bones are seen in the posterior view of the skull (Fig. 8.8).
Fig. 8.8 Posterior view of the skull.
Occipital bone
Centrally the flat or squamous part of occipital bone is the main structure in this view of the skull (Fig. 8.8). It articulates superiorly with the paired parietal bones at the lambdoid suture and laterally with each temporal bone at the occipitomastoid sutures. Along the lambdoid suture, small islands of bone (sutural bones or wormian bones) may be observed.
Several bony landmarks are visible on the occipital bone. There is a midline projection, (the external occipital protuberance) with curved lines extending laterally from it (superior nuchal lines). The most prominent point of the external occipital protuberance is the inion. About 1 inch (2.5 cm) below the superior nuchal lines, two additional lines (the inferior nuchal lines) curve laterally. Extending downward from the external occipital protuberance is the external occipital crest.
Temporal bones
Laterally, the temporal bones are visible in the posterior view of the skull, with the mastoid processes being the prominent feature (Fig. 8.8). On the inferomedial border of each mastoid process is a notch (the mastoid notch), which is a point of attachment for the posterior belly of the digastric muscle.
Superior view
The frontal bone, parietal bones, and occipital bone are seen in a superior view of the skull (Fig. 8.9). These bones make up the superior part of the calvaria, or the calva (skullcap).
Fig. 8.9 Superior view of the skull.
In an anterior to posterior direction:
 The unpaired frontal bone articulates with the paired parietal bones at the coronal suture.
The unpaired frontal bone articulates with the paired parietal bones at the coronal suture.
 The two parietal bones articulate with each other in the midline at the sagittal suture.
The two parietal bones articulate with each other in the midline at the sagittal suture.
 The parietal bones articulate with the unpaired occipital bone at the lambdoid suture.
The parietal bones articulate with the unpaired occipital bone at the lambdoid suture.
The junction of the sagittal and coronal sutures is the bregma, and the junction of the sagittal and lambdoid sutures is the lambda.
The only foramen visible in this view of the skull may be the paired parietal foramina; posteriorly, one on each parietal bone just lateral to the sagittal suture (Fig. 8.9).
The bones making up the calvaria (Fig. 8.10) are unique in their structure, consisting of dense internal and external tables of compact bone separated by a layer of spongy bone (the diploë).
Fig. 8.10 Calvaria.
Inferior view
The base of the skull is seen in the inferior view and extends anteriorly from the middle incisor teeth posteriorly to the superior nuchal lines and laterally to the mastoid processes and zygomatic arches (Fig. 8.11).
Fig. 8.11 Inferior view of the skull.
For descriptive purposes, the base of the skull is often divided into:
 an anterior part, which includes the teeth and the hard palate;
an anterior part, which includes the teeth and the hard palate;
Anterior part
The main features of the anterior part of the base of the skull are the teeth and the hard palate.
The teeth project from the alveolar processes of the two maxillae. These processes are arranged together in a U-shaped alveolar arch that borders the hard palate on three sides (Fig. 8.11).
The hard palate is composed of the palatine processes of each maxilla anteriorly and the horizontal plates of each palatine bone posteriorly.
The paired palatine processes of each maxilla meet in the midline at the intermaxillary suture, the paired maxilla and the paired palatine bones meet at the palatomaxillary suture, and the paired horizontal plates of each palatine bone meet in the midline at the interpalatine suture.
Several additional features are also visible when the hard palate is examined:
Middle part
The middle part of the base of the skull is complex:
 Forming the anterior half are the vomer and sphenoid bones.
Forming the anterior half are the vomer and sphenoid bones.
 Forming the posterior half are the occipital and paired temporal bones.
Forming the posterior half are the occipital and paired temporal bones.
Anterior half
Anteriorly, the small vomer is in the midline, resting on the sphenoid bone (Fig. 8.11). It contributes to the formation of the bony nasal septum separating the two choanae.
Most of the anterior part of the middle part of the base of the skull consists of the sphenoid bone.
The sphenoid bone is made up of a centrally placed body, paired greater and lesser wings projecting laterally from the body, and two downward projecting pterygoid processes immediately lateral to each choana.
Three parts of the sphenoid bone, the body, greater wings, and pterygoid processes, are seen in the inferior view of the skull (Fig. 8.11). The lesser wing of the sphenoid is not seen in the inferior view.
The body of the sphenoid is a centrally placed cube of bone containing two large air sinuses separated by a septum.
It articulates anteriorly with the vomer, ethmoid, and palatine bones, posterolaterally with the temporal bones, and posteriorly with the occipital bone.
Extending downward from the junction of the body and the greater wings are the pterygoid processes (Fig. 8.11). Each of these processes consists of a narrow medial plate and broader lateral plate separated by the pterygoid fossa.
Each medial plate of the pterygoid process ends inferiorly with a hook-like projection, the pterygoid hamulus, and divides superiorly to form the small, shallow scaphoid fossa.
Just superior to the scaphoid fossa, at the root of the medial plate of the pterygoid process is the opening of the pterygoid canal, which passes forward from near the anterior margin of the foramen lacerum.
Lateral to the lateral plate of the pterygoid process is the greater wing of the sphenoid (Fig. 8.11), which not only forms a part of the base of the skull, but also continues laterally to form part of the lateral wall of the skull. It articulates laterally and posteriorly with parts of the temporal bone.
Important features visible on the surface of the greater wing in an inferior view of the skull are the foramen ovale and the foramen spinosum on the posterolateral border extending outward from the upper end of the lateral plate of the pterygoid process.
Posterior half of middle part
In the posterior half of the middle part of the base of the skull are the occipital bone and the paired temporal bones (Fig. 8.11).
The occipital bone, or more specifically its basilar part, is in the midline immediately posterior to the body of the sphenoid. It extends posteriorly to the foramen magnum and is bounded laterally by the temporal bones.
Prominent on the basilar part of the occipital bone is the pharyngeal tubercle, a bony protuberance for the attachment of parts of the pharynx to the base of the skull (Fig. 8.11).
Immediately lateral to the basilar part of the occipital bone is the petrous part of the petromastoid part of each temporal bone.
Wedge-shaped in its appearance, with its apex anteromedial, the petrous part of the temporal bone is between the greater wing of the sphenoid anteriorly and the basilar part of the occipital bone posteriorly. The apex forms one of the boundaries of the foramen lacerum, an irregular opening filled in life with cartilage (Fig. 8.11).
The other boundaries of the foramen lacerum are the basilar part of the occipital bone medially and the body of the sphenoid anteriorly.
Posterolateral from the foramen lacerum along the petrous part of the temporal bone is the large circular opening for the carotid canal.
Between the petrous part of the temporal bone and the greater wing of the sphenoid is a groove for the cartilaginous part of the pharyngotympanic tube (auditory tube). This groove continues posterolaterally into a bony canal in the petrous part of the temporal bone for the pharyngotympanic tube.
Just lateral to the greater wing of the sphenoid is the squamous part of the temporal bone, which participates in the temporomandibular joint. It contains the mandibular fossa, which is a concavity where the head of the mandible articulates with the base of the skull. An important feature of this articulation is the prominent articular tubercle, which is the downward projection of the anterior border of the mandibular fossa (Fig. 8.11).
Posterior part
The posterior part of the base of the skull extends from the anterior edge of the foramen magnum posteriorly to the superior nuchal lines (Fig. 8.11). It consists of parts of the occipital bone centrally and the temporal bones laterally.
Occipital bone
The occipital bone is the major bony element of this part of the base of the skull (Fig. 8.11). It has four parts organized around the foramen magnum, which is a prominent feature of this part of the base of the skull and through which the brain and spinal cord are continuous.
The parts of the occipital bone are the squamous part, which is posterior to the foramen magnum, the lateral parts, which are lateral to the foramen magnum, and the basilar part, which is anterior to the foramen magnum (Fig. 8.11).
The squamous and lateral parts are components of the posterior part of the base of the skull.
The most visible feature of the squamous part of the occipital bone, when examining the inferior view of the skull, is a ridge of bone (the external occipital crest) that extends downward from the external occipital protuberance toward the foramen magnum. The inferior nuchal lines arc laterally from the midpoint of the crest.
Immediately lateral to the foramen magnum are the lateral parts of the occipital bones, which contain numerous important structural features.
On each anterolateral border of the foramen magnum are the rounded occipital condyles (Fig. 8.11). These paired structures articulate with the atlas (vertebra CI). Posterior to each condyle is a depression (the condylar fossa) containing a condylar canal, and anterior and superior to each condyle is the large hypoglossal canal. Lateral to each hypoglossal canal is a large, irregular jugular foramen formed by opposition of the jugular notch of the occipital bone and jugular notch of the temporal bone.
Temporal bone
Laterally in the posterior part of the base of the skull is the temporal bone. The parts of the temporal bone seen in this location are the mastoid part of the petromastoid part and the styloid process (see Fig. 8.11).
The lateral edge of the mastoid part is identified by the large cone-shaped mastoid process projecting from its inferior surface. This prominent bony structure is the point of attachment for several muscles. On the medial aspect of the mastoid process is the deep mastoid notch, which is also an attachment point for a muscle.
Anteromedial to the mastoid process is the needle-shaped styloid process projecting from the lower border of the temporal bone. The styloid process is also a point of attachment for numerous muscles and ligaments.
Finally, between the styloid process and the mastoid process is the stylomastoid foramen.
CRANIAL CAVITY
The cranial cavity is the space within the cranium that contains the brain, meninges, proximal parts of the cranial nerves, blood vessels, and cranial venous sinuses.
Roof
The calvaria is the dome-shaped roof that protects the superior aspect of the brain. It consists mainly of the frontal bone anteriorly, the paired parietal bones in the middle, and the occipital bone posteriorly (Fig. 8.12).
Fig. 8.12 Roof of the cranial cavity.
Sutures visible internally include:
 the coronal suture, between the frontal and parietal bones;
the coronal suture, between the frontal and parietal bones;
 the sagittal suture, between the paired parietal bones; and
the sagittal suture, between the paired parietal bones; and
 the lambdoid suture, between the parietal and occipital bones.
the lambdoid suture, between the parietal and occipital bones.
Visible junctions of these sutures are the bregma, where the coronal and sagittal sutures meet, and the lambda, where the lambdoid and sagittal sutures meet.
Other markings on the internal surface of the calva include bony ridges, and numerous grooves and pits (Fig. 8.12).
From anterior to posterior, features seen on the bony roof of the cranial cavity are (Fig. 8.12):
Floor
The floor of the cranial cavity is divided into anterior, middle, and posterior cranial fossae.
Anterior cranial fossa
Parts of the frontal, ethmoid, and sphenoid bones form the anterior cranial fossa (Fig. 8.13). Its floor is composed of:
 frontal bone in the anterior and lateral direction;
frontal bone in the anterior and lateral direction;
 ethmoid bone in the midline; and
ethmoid bone in the midline; and
 two parts of the sphenoid bone posteriorly, the body (midline), and the lesser wings (laterally).
two parts of the sphenoid bone posteriorly, the body (midline), and the lesser wings (laterally).
Fig. 8.13 Anterior cranial fossa.
The anterior cranial fossa is above the nasal cavity and the orbits, and it is filled by the frontal lobes of the cerebral hemispheres.
Anteriorly, a small wedge-shaped midline crest of bone (the frontal crest) projects from the frontal bone. This is a point of attachment for the falx cerebri. Immediately posterior to the frontal crest is the foramen cecum (Table 8.2). This foramen between the frontal and ethmoid bones may transmit emissary veins connecting the nasal cavity with the superior sagittal sinus.
Table 8.2 Internal foramina of the skull
|
Foramen |
Structures passing through foramen |
|
Anterior cranial fossa |
|
|
Foramen cecum |
Emissary veins to nasal cavity |
|
Olfactory foramina in cribriform plate |
Olfactory nerves [I] |
|
Middle cranial fossa |
|
|
Optic canal |
Optic nerve [II]; ophthalmic artery |
|
Superior orbital fissure |
Oculomotor nerve [III]; trochlear nerve [IV]; ophthalmic division of the trigeminal nerve [V1]; abducent nerve [VI]; ophthalmic veins |
|
Foramen rotundum |
Maxillary division of the trigeminal nerve [V2] |
|
Foramen ovale |
Mandibular division of the trigeminal nerve [V3]; lesser petrosal nerve |
|
Foramen spinosum |
Middle meningeal artery |
|
Hiatus for the greater petrosal nerve |
Greater petrosal nerve |
|
Hiatus for the lesser petrosal nerve |
Lesser petrosal nerve |
|
Posterior cranial fossa |
|
|
Foramen magnum |
End of brainstem/beginning of spinal cord; vertebral arteries; spinal roots of the accessory nerve; meninges |
|
Internal acoustic meatus |
Facial nerve [VII]; vestibulocochlear nerve [VIII]; labyrinthine artery |
|
Jugular foramen |
Glossopharyngeal nerve [IX]; vagus nerve [X]; accessory nerve [XI]; inferior petrosal sinus, sigmoid sinus (forming internal jugular vein) |
|
Hypoglossal canal |
Hypoglossal nerve [XII]; meningeal branch of the ascending pharyngeal artery |
|
Condylar canal |
Emissary vein |
Posterior to the frontal crest is a prominent wedge of bone projecting superiorly from the ethmoid (the crista galli). This is another point of attachment for the falx cerebri, which is the vertical extension of dura mater partially separating the two cerebral hemispheres.
Lateral to the crista galli is the cribriform plate of the ethmoid bone (see Fig. 8.13). This is a sieve-like structure, which allows small olfactory nerve fibers to pass through its foramina from the nasal mucosa to the olfactory bulb. The olfactory nerves are commonly referred to collectively as the olfactory nerve [I].
On each side of the ethmoid, the floor of the anterior cranial fossa is formed by relatively thin plates of frontal bone (the orbital part of the frontal bone), which also forms the roof of the orbit below. Posterior to both the frontal and ethmoid bones, the rest of the floor of the anterior cranial fossa is formed by the body and lesser wings of the sphenoid. In the midline, the body extends anteriorly between the orbital parts of the frontal bone to reach the ethmoid bone and posteriorly it extends into the middle cranial fossa.
The boundary between the anterior and middle cranial fossae in the midline is the anterior edge of the chiasmatic sulcus, a smooth groove stretching between the optic canals across the body of the sphenoid.
Lesser wings of the sphenoid
The two lesser wings of the sphenoid project laterally from the body of the sphenoid and form a distinct boundary between the lateral parts of the anterior and middle cranial fossae (see Fig. 8.13).
Overhanging the anterior part of the middle cranial fossae, each lesser wing ends laterally as a sharp point at the junction of the frontal bone and the greater wing of the sphenoid near the upper lateral edge of the superior orbital fissure that is formed between the greater and lesser wings.
Medially each lesser wing widens, curves posteriorly, and ends as a rounded anterior clinoid process (see Fig. 8.13). These processes serve as the anterior point of attachment for the tentorium cerebelli, which is a sheet of dura that separates the posterior part of the cerebral hemispheres from the cerebellum. Just anterior to each anterior clinoid process is a circular opening in the lesser wing of the sphenoid (the optic canal), through which the ophthalmic artery and optic nerve [II] pass as they exit the cranial cavity to enter the orbit. The optic canals are usually included in the middle cranial fossa.
Middle cranial fossa
The middle cranial fossa consists of parts of the sphenoid and temporal bones (Fig. 8.14).
Fig. 8.14 Middle cranial fossa.
The boundary between the anterior and middle cranial fossae in the midline is the anterior edge of the chiasmatic sulcus, which is a smooth groove stretching between the optic canals across the body of the sphenoid.
The posterior boundaries of the middle cranial fossa are formed on each side by the anterior surface, as high as the superior border of the petrous part of the petromastoid part of the temporal bone.
Sphenoid
The floor in the midline of the middle cranial fossa is elevated and formed by the body of the sphenoid. Lateral to this are large depressions formed on either side by the greater wing of the sphenoid and the squamous part of the temporal bone. These depressions contain the temporal lobes of the brain.
Sella turcica
Just posterior to the chiasmatic sulcus is the uniquely modified remainder of the body of the sphenoid (the sella turcica), which consists of a deep central area (the hypophysial fossa) containing the pituitary gland with anterior and posterior vertical walls of bone (Fig. 8.14).
Lateral projections from the corners of the tuberculum sellae (the middle clinoid processes) are sometimes evident.
The posterior wall of the sella turcica is the dorsum sellae, a large ridge of bone projecting upward and forward. At the top of this bony ridge, the lateral edges contain rounded projections (the posterior clinoid processes), which are points of attachment, like the anterior clinoid processes, for the tentorium cerebelli.
Fissures and foramina
A diagonal gap, the superior orbital fissure, separates the greater wing of the sphenoid from the lesser wing and is a major passageway between the middle cranial fossa and the orbit (Fig. 8.14; also see Table 8.2). Passing through the fissure are the oculomotor nerve [III], the trochlear nerve [IV], the ophthalmic nerve [V1], the abducent nerve [VI], and ophthalmic veins.
Posterior to the medial end of the superior orbital fissure on the floor of the middle cranial fossa is a rounded foramen projecting in an anterior direction (the foramen rotundum), through which the maxillary nerve [V2] passes from the middle cranial fossa to the pterygopalatine fossa (Fig. 8.14; also see Table 8.2).
Posterolateral to the foramen rotundum is a large oval opening (the foramen ovale), which allows structures to pass between the extracranial infratemporal fossa and the middle cranial fossa (Fig. 8.14; also see Table 8.2). The mandibular nerve [V3], lesser petrosal nerve (carrying fibers from the tympanic plexus that originally came from the glossopharyngeal nerve [IX]), and occasionally a small vessel (the accessory middle meningeal artery) pass through this foramen.
Posterolateral from the foramen ovale is the small foramen spinosum (Fig. 8.14). This opening also connects the infratemporal fossa with the middle cranial fossa. The middle meningeal artery and its associated veins pass through this foramen and, once inside, the groove for the middle meningeal artery across the floor and lateral wall of the middle cranial fossa clearly marks their path.
Posteromedial to the foramen ovale is the rounded intracranial opening of the carotid canal. Directly inferior to this opening is an irregular foramen (the foramen lacerum) (Fig. 8.14; also see Table 8.2). Clearly observed in the inferior view of the skull, the foramen lacerum is closed in life by a cartilaginous plug and no structures pass through it completely.
Temporal bone
The posterior boundary of the middle cranial fossa is formed by the anterior surface of the petrous part of the petromastoid part of the temporal bone.
Medially, there is a slight depression (trigeminal impression) in the anterior surface of the petrous part of the temporal bone (Fig. 8.14), which marks the location of the sensory ganglion for the trigeminal nerve [V].
Lateral to the trigeminal impression and on the anterior surface of the petrous part of the temporal bone is a small linear groove that passes in a superolateral direction, and ends in a foramen (the groove and hiatus for the greater petrosal nerve) (Fig. 8.14). The greater petrosal nerve is a branch of the facial nerve [VII].
Anterolateral to the groove for the greater petrosal nerve is a second, smaller groove and hiatus for the lesser petrosal nerve, a branch from the tympanic plexus carrying fibers that originally came from the glossopharyngeal nerve [IX] (Fig. 8.14).
Above and lateral to the small openings for the greater and lesser petrosal nerves, near the superior ridge of the petrous part of the temporal bone, is a rounded protrusion of bone (the arcuate eminence) produced by the underlying anterior semicircular canal of the inner ear (Fig. 8.14).
Just anterior and lateral to the arcuate eminence, the anterior surface of the petrous part of the temporal bone is slightly depressed. This region is the tegmen tympani, which marks the thin bony roof of the middle ear cavity.
Posterior cranial fossa
The posterior cranial fossa consists mostly of parts of the temporal and occipital bones, with small contributions from the sphenoid and parietal bones (Fig. 8.15). It is the largest and deepest of the three cranial fossae and contains the brainstem (midbrain, pons, and medulla) and the cerebellum.
Fig. 8.15 Posterior cranial fossa.
Boundaries
The anterior boundaries of the posterior cranial fossa in the midline are the dorsum sellae and the clivus (Fig. 8.15). The clivus is a slope of bone that extends upward from the foramen magnum. It is formed by contributions from the body of the sphenoid and from the basilar part of the occipital bone.
Laterally the anterior boundaries of the posterior cranial fossa are the superior border of the petrous part of the petromastoid part of the temporal bone.
Posteriorly the squamous part of the occipital bone to the level of the transverse groove is the major boundary, while laterally the petromastoid part of the temporal bone and small parts of the occipital and parietal bones border the fossa.
Foramen magnum
Centrally, in the deepest part of the posterior cranial fossa, is the largest foramen in the skull, the foramen magnum (Fig. 8.15; also see Table 8.2). It is surrounded by the basilar part of the occipital bone anteriorly, the lateral parts of the occipital bone on either side, and the squamous part of the occipital bone posteriorly.
The spinal cord passes superiorly through the foramen magnum to continue as the brainstem.
Also passing through the foramen magnum are the vertebral arteries, the meninges, and the spinal roots of the accessory nerve [XI].
Grooves and foramina
The clivus slopes upward from the foramen magnum. Lateral to the clivus is a groove for the inferior petrosal sinus between the basilar part of the occipital bone and the petrous part of the petromastoid part of the temporal bone (Fig. 8.15).
Laterally, across the upper half of the posterior surface of the petrous part of the temporal bone, is an oval foramen (the internal acoustic meatus) (Fig. 8.15; also see Table 8.2). The facial [VII] and vestibulocochlear [VIII] nerves, and the labyrinthine artery pass through it.
Inferior to the internal acoustic meatus, the temporal bone is separated from the occipital bone by the large jugular foramen (Fig. 8.15). Leading to this foramen from the medial side is the groove for the inferior petrosal sinus, and from the lateral side the groove for the sigmoid sinus. The sigmoid sinus passes into the jugular foramen, and is continuous with the internal jugular vein, while the inferior petrosal sinus empties into the internal jugular vein in the area of the jugular foramen. Also passing through the jugular foramen are the glossopharyngeal nerve [IX], the vagus nerve [X], and the accessory nerve [XI].
Medial to the jugular foramen is a large rounded mound of the occipital bone (the jugular tubercle). Just inferior to this, and superior to the foramen magnum, is the hypoglossal canal, through which the hypoglossal nerve [XII] leaves the posterior cranial fossa, and a meningeal branch of the ascending pharyngeal artery enters the posterior cranial fossa (Fig. 8.15).
Just posterolateral to the hypoglossal canal is the small condylar canal that, when present, transmits an emissary vein.
Squamous part of the occipital bone
The squamous part of the occipital bone has several prominent features (Fig. 8.15):
 Running upward in the midline from the foramen magnum is the internal occipital crest.
Running upward in the midline from the foramen magnum is the internal occipital crest.
The transverse and sigmoid sinuses are intradural venous sinuses.
Clinical app
Medical imaging of the head
Until two decades ago the standard method of imaging the head was plain radiography. The radiographs are taken in three standard projections—namely the posteroanterior view, the lateral view, and the Towne’s view.
Since the development of the first computed tomography (CT) scanner, cerebral CT has been the “workhorse” of neuroradiological examination. It is ideally used for head injury because the brain and its coverings can be easily and quickly examined, and blood is easily detected.
With intravenous contrast, CT angiography can be used to demonstrate the position and the size of an intracerebral aneurysm before endovascular treatment.
Magnetic resonance imaging (MRI) is unsurpassed by other imaging techniques in its ability for contrast resolution. The brain and its coverings, cerebrospinal fluid (CSF), and the vertebral column can be easily and quickly examined.
Magnetic resonance angiography has been extremely useful in determining the completeness of the intracranial vasculature (circle of Willis), which is necessary in some surgical conditions.
Initial work using ultrasound to assess the brain appeared fruitless, but with increasing probe technology it is now possible to carry out intracranial Doppler studies, which enable a surgeon to detect whether a patient is experiencing cerebral embolization from a carotid plaque.
Clinical app
Fractures of the skull vault
The skull vault is a remarkably strong structure because it protects our most vital organ, the brain. From a clinical standpoint, skull fractures alert clinicians to the nature and force of an injury and potential complications. Of key importance is the need to minimize the extent of primary brain injury and to treat potential secondary complications rather than focusing on the skull fracture. Skull fractures that have particular significance include depressed skull fractures, compound fractures, and pterion fractures.
In a depressed skull fracture, a bony fragment is depressed below the normal skull convexity. This may lead to secondary arterial and venous damage with hematoma formation. Furthermore, a primary brain injury can also result from this type of fracture.
In a compound fracture there is a fracture of the bone together with a breach of the skin, which may allow an infection to enter. Typically these fractures are associated with scalp lacerations and can usually be treated with antibiotics.
The pterion is an important circular area on the lateral aspect of the skull where the frontal, parietal, sphenoid, and temporal bones come together. Importantly, deep to the pterion is the middle meningeal artery. An injury to this point of the skull is extremely serious because damage to this vessel may produce a significant extradural hematoma, which can be fatal.
Surface anatomy
Estimating the position of the middle meningeal artery
The middle meningeal artery (Fig. 8.16) is a branch of the maxillary artery in the infratemporal fossa. It enters the skull through the foramen spinosum and is within the dura mater lining the cranial cavity.
Fig. 8.16 Estimating the position of the middle meningeal artery. Lateral head and neck of a man.
In lateral blows to the head, the middle meningeal artery can be ruptured, leading to extradural hemorrhage and eventual death if not treated.
The anterior branch of the middle meningeal artery is the part of the vessel most often torn. This branch is in the temple region of the head, approximately midway between the superior margin of the orbit and the upper part of the external ear in what is termed the pterion.
Lateral blows to the head can fracture the internal table of bone of the skull and tear the middle meningeal artery in the outer layer of dura mater that is fused to the cranium. Blood under pulsatile arterial pressure leaks out of the vessel and gradually separates the dura from the bone, forming a progressively larger extradural hematoma.
MENINGES
The brain, as well as the spinal cord, is surrounded by three layers of membranes: the meninges, Fig. 8.17A, a tough, outer layer; the dura mater, a delicate, middle layer (the arachnoid mater); and an inner layer firmly attached to the surface of the brain—the pia mater.
Fig. 8.17 Cranial meninges. A. Superior coronal view. B. Continuity with the spinal meninges.
The cranial meninges are continuous with, and similar to, the spinal meninges through the foramen magnum, with one important distinction—the cranial dura mater consists of two layers, and only one of these is continuous through the foramen magnum (Fig. 8.17B).
Cranial dura mater
The cranial dura mater is a thick, tough, outer covering of the brain. It consists of an outer periosteal layer and an inner meningeal layer (Fig. 8.17A):
 The outer periosteal layer is firmly attached to the skull, is the periosteum of the cranial cavity, contains the meningeal arteries, and is continuous with the periosteum on the outer surface of the skull at the foramen magnum and other intracranial foramina (Fig. 8.17B).
The outer periosteal layer is firmly attached to the skull, is the periosteum of the cranial cavity, contains the meningeal arteries, and is continuous with the periosteum on the outer surface of the skull at the foramen magnum and other intracranial foramina (Fig. 8.17B).
The two layers of dura separate from each other at numerous locations to form two unique types of structures (Fig. 8.17A):
 dural partitions, which project inward and incompletely separate parts of the brain;
dural partitions, which project inward and incompletely separate parts of the brain;
 intracranial venous structures (cranial venous sinuses, see pp. 437 to 439).
intracranial venous structures (cranial venous sinuses, see pp. 437 to 439).
Dural partitions
The dural partitions project into the cranial cavity and partially subdivide the cranial cavity. They include the falx cerebri, tentorium cerebelli, falx cerebelli, and the diaphragma sellae.
Falx cerebri
The falx cerebri (Fig. 8.18) is a crescent-shaped downward projection of meningeal dura mater from the dura lining the calva that passes between the two cerebral hemispheres. It is attached anteriorly to the crista galli of the ethmoid bone and frontal crest of the frontal bone. Posteriorly it is attached to and blends with the tentorium cerebelli.
Fig. 8.18 Dural partitions.
Tentorium cerebelli
The tentorium cerebelli (Fig. 8.18) is a horizontal projection of the meningeal dura mater that covers and separates the cerebellum in the posterior cranial fossa from the posterior parts of the cerebral hemispheres. It is attached posteriorly to the occipital bone along the grooves for the transverse sinuses. Laterally, it is attached to the superior border of the petrous part of the temporal bone, ending anteriorly at the anterior and posterior clinoid processes.
The anterior and medial borders of the tentorium cerebelli are free, forming an oval opening in the midline (the tentorial notch), through which the midbrain passes.
Falx cerebelli
The falx cerebelli (Fig. 8.18) is a small midline projection of meningeal dura mater in the posterior cranial fossa. It is attached posteriorly to the internal occipital crest of the occipital bone and superiorly to the tentorium cerebelli. Its anterior edge is free and is between the two cerebellar hemispheres.
Diaphragma sellae
The final dural projection is the diaphragma sellae (Fig. 8.18). This small horizontal shelf of meningeal dura mater covers the hypophysial fossa in the sella turcica of the sphenoid bone. There is an opening in the center of the diaphragma sellae through which passes the infundibulum, which connects the pituitary gland with the base of the brain, and any accompanying blood vessels.
Arterial supply
The arterial supply to the dura mater (Fig. 8.19) travels in the outer periosteal layer of the dura and consists of:
 anterior meningeal arteries in the anterior cranial fossa,
anterior meningeal arteries in the anterior cranial fossa,
 the middle and accessory meningeal arteries in the middle cranial fossa, and
the middle and accessory meningeal arteries in the middle cranial fossa, and
 the posterior meningeal artery and other meningeal branches in the posterior cranial fossa.
the posterior meningeal artery and other meningeal branches in the posterior cranial fossa.
Fig. 8.19 Dural arterial supply.
All are small arteries except for the middle meningeal artery, which is much larger and supplies the greatest part of the dura.
The anterior meningeal arteries are branches of the ethmoidal arteries (Fig. 8.19).
The middle meningeal artery is a branch of the maxillary artery (Fig. 8.19). It enters the middle cranial fossa through the foramen spinosum and divides into anterior and posterior branches:
The accessory meningeal artery is usually a small branch of the maxillary artery that enters the middle cranial fossa through the foramen ovale and supplies areas medial to this foramen.
The posterior meningeal artery and other meningeal branches supplying the dura mater in the posterior cranial fossa come from several sources (Fig. 8.19):
Innervation
Innervation of the dura mater (Fig. 8.20) is by small meningeal branches of all three divisions of the trigeminal nerve [V1, V2, and V3], the vagus nerve [X], and the first, second, and sometimes, third cervical nerves. (Possible involvement of the glossopharyngeal [IX] and hypoglossal nerves [XII] in the posterior cranial fossa has also been reported.)
Fig. 8.20 Dural innervation.
In the anterior cranial fossa, meningeal branches from the ethmoidal nerves, which are branches of the ophthalmic nerve [V1], supply the floor and the anterior part of the falx cerebri (Fig. 8.20).
Additionally, a meningeal branch of the ophthalmic nerve [V1] turns and runs posteriorly, supplying the tentorium cerebelli and the posterior part of the falx cerebri (Fig. 8.20).
The middle cranial fossa is supplied medially by meningeal branches from the maxillary nerve [V2] and laterally, along the distribution of the middle meningeal artery, by meningeal branches from the mandibular nerve [V3] (Fig. 8.20).
The posterior cranial fossa is supplied by meningeal branches from the first, second, and sometimes, the third cervical nerves, which enter the fossa through the foramen magnum, the hypoglossal canal, and the jugular foramen (Fig. 8.20). Meningeal branches of the vagus nerve [X] have also been described. (Possible contributions from the glossopharyngeal [IX] and hypoglossal [XII] nerves have also been reported.)
Arachnoid mater
The arachnoid mater is a thin, avascular membrane that lines, but is not adherent to, the inner surface of the dura mater (Fig. 8.21). From its inner surface, thin processes or trabeculae extend downward, cross the subarachnoid space, and become continuous with the pia mater.
Fig. 8.21 Arrangement of the meninges and spaces.
Unlike the pia, the arachnoid does not enter the grooves or fissures of the brain, except for the longitudinal fissure between the two cerebral hemispheres.
Pia mater
The pia mater is a thin, delicate membrane that closely invests the surface of the brain (Fig. 8.21). It follows the contours of the brain, entering the grooves and fissures on its surface, and is closely applied to the roots of the cranial nerves at their origins.
Meningeal spaces
Extradural space
The potential space between dura mater and bone is the extradural space. Normally, the outer or periosteal layer of dura mater is firmly attached to the bones surrounding the cranial cavity (Fig. 8.21).
Subdural space
Anatomically, a true subdural space does not exist. Blood collecting in this region (subdural hematoma) due to injury represents a dissection of the dural border cell layer, which is the innermost lining of the meningeal dura. Dural border cells are flattened cells surrounded by extracellular spaces filled with amorphous material. While very infrequent, an occasional cell junction may be seen between these cells and the underlying arachnoid layer.
Subarachnoid space
Deep to the arachnoid mater is the only normally occurring fluid-filled space associated with the meninges. It occurs because the arachnoid mater clings to the inner surface of the dura mater and does not follow the contour of the brain, while the pia mater, being against the surface of the brain, closely follows the grooves and fissures on the surface of the brain. A narrow space (the subarachnoid space) is therefore created between these two membranes (Fig. 8.21).
The subarachnoid space surrounds the brain and spinal cord and in certain locations it enlarges into expanded areas (subarachnoid cisterns). It contains cerebrospinal fluid (CSF) and blood vessels.
Cerebrospinal fluid is produced by the choroid plexus, primarily in the ventricles of the brain. It is a clear, colorless, cell-free fluid that circulates through the subarachnoid space surrounding the brain and spinal cord.
The CSF returns to the venous system through arachnoid villi. These project as clumps (arachnoid granulations) into the superior sagittal sinus, which is a dural venous sinus, and its lateral extensions, the lateral lacunae.
Clinical app
Types of intracranial hemorrhage
An extradural hemorrhage (Fig. 8.22) is caused by arterial damage and results from tearing of the branches of the middle meningeal artery, which typically occurs in the region of the pterion. Blood collects between the periosteal layer of the dura and the calvaria, and under arterial pressure slowly expands.
Fig. 8.22 Extradural hematoma. Axial CT scan of brain.
The typical history is of a blow to the head (often during a sporting activity) that produces a minor loss of consciousness. Following the injury, the patient usually regains consciousness and has a lucid interval for a period of hours. After this rapid drowsiness and unconsciousness ensue, which may lead to death.
A subdural hematoma (Fig. 8.23) is created by a hemorrhage within the dural border cell layer. The hematoma results from venous bleeding, usually from torn cerebral veins where they enter the superior sagittal sinus.
Fig. 8.23 Chronic (low-density) subdural hematoma. Axial CT scan of brain.
Patients at most risk of developing a subdural hematoma are the young and elderly. The clinical history usually includes a trivial injury followed by an insidious loss of consciousness or alteration of personality.
Subarachnoid hemorrhage (Fig. 8.24) typically results from a ruptured intracerebral aneurysm arising from the vessels supplying and around the arterial circle (of Willis), but may occur in patients who have undergone significant cerebral trauma.
Cerebrospinal fluid leak
Leakage of cerebrospinal fluid from the subarachnoid space may occur after any procedure in and around the brain, spinal cord, and meningeal membranes. These procedures include lumbar spine surgery, epidural injection, and cerebrospinal fluid aspiration.
In “cerebrospinal fluid leak syndrome,” cerebrospinal fluid leaks out of the subarachnoid space and through dura mater for no apparent reason. The clinical consequences of this include dizziness, nausea, fatigue, and metallic taste in the mouth. Other effects also include facial nerve weakness and double vision.
Clinical app
Hydrocephalus
Hydrocephalus is a dilatation of the cerebral ventricular system, which is due to either an obstruction to the flow of CSF, overproduction of CSF, or a failure of reabsorption of CSF.
Cerebrospinal fluid is secreted by the epithelial cells of the choroid plexus within ventricles of the brain. The CSF passes from the ventricles through foramina into the subarachnoid space.
The CSF circulates around the spinal cord inferiorly, envelops the brain superiorly, and is absorbed through the arachnoid granulations in the walls of the dural venous sinuses. In adults almost half a liter of CSF is produced a day.
In adults the commonest cause of hydrocephalus is an interruption of the normal CSF absorption through the arachnoid granulations. This occurs when blood enters the subarachnoid space after subarachnoid hemorrhage, passes over the brain, and interferes with normal CSF absorption. To prevent severe hydrocephalus, it may be necessary to place a small catheter through the brain into the ventricular system to drain the CSF to relieve the pressure.
In children, hydrocephalus is always dramatic in its later stages. The hydrocephalus increases the size and dimensions of the ventricle, and as a result the brain enlarges. Because the skull sutures are not fused, the head expands. Cranial enlargement in utero may make a vaginal delivery impossible, and delivery then has to be by caesarean section.
Both CT and MRI enable a radiologist to determine the site of obstruction, and in most cases the cause of the obstruction.
Clinical app
Meningitis
Meningitis is a rare infection of the leptomeninges (the leptomeninges are a combination of the arachnoid mater and the pia mater). Infection of the meninges typically occurs via a blood-borne route, though in some cases it may be by direct spread (e.g., trauma) or from the nasal cavities through the cribriform plate in the ethmoid bone.
The typical history of meningitis is nonspecific at first. The patient may have a mild headache, fever, drowsiness, and nausea. As the infection progresses, photophobia (light intolerance) and ecchymosis may ensue. Straight leg raising causes marked neck pain and discomfort (Kernig’s sign) and an emergency hospital admission is warranted.
BRAIN AND ITS BLOOD SUPPLY
Brain
The brain is a component of the central nervous system.
During development the brain can be divided into five continuous parts (Figs. 8.25, 8.26). From rostral (or cranial) to caudal they are:
 the mesencephalon (midbrain), which is the first part of the brainstem seen when an intact adult brain is examined, and is at the junction between and in both the middle and posterior cranial fossae;
the mesencephalon (midbrain), which is the first part of the brainstem seen when an intact adult brain is examined, and is at the junction between and in both the middle and posterior cranial fossae;
Fig. 8.25 Lateral view of the brain.
Fig. 8.26 Sagittal section of the brain.
Blood supply
The brain receives its arterial supply from two pairs of vessels, the vertebral and internal carotid arteries (Figs. 8.27, 8.28), which are interconnected in the cranial cavity to produce a cerebral arterial circle (of Willis).
Fig. 8.27 Arterial supply to the brain.
Imaging app
Visualizing the internal carotid and vertebral arteries
Fig 8.28 Magnetic resonance angiogram showing normal carotid and vertebral arteries.
Vertebral arteries
Each vertebral artery arises from the first part of each subclavian artery in the lower part of the neck, and passes superiorly through the transverse foramina of the upper six cervical vertebrae. On entering the cranial cavity through the foramen magnum, each vertebral artery gives off a small meningeal branch.
Continuing forward, the vertebral artery gives rise to three additional branches before joining with its companion vessel to form the basilar artery (Fig. 8.29):
 Just before the two vertebral arteries join, each gives off a posterior inferior cerebellar artery.
Just before the two vertebral arteries join, each gives off a posterior inferior cerebellar artery.
Fig. 8.29 Arteries on the base of the brain.
The basilar artery travels in a rostral direction along the anterior aspect of the pons (Fig. 8.29). Its branches in a caudal to rostral direction include the anterior inferior cerebellar arteries, several small pontine arteries, and the superior cerebellar arteries. The basilar artery ends as a bifurcation, giving rise to two posterior cerebral arteries.
Internal carotid arteries
The two internal carotid arteries arise as one of the two terminal branches of the common carotid arteries (see Figs. 8.27, 8.28). They proceed superiorly to the base of the skull where they enter the carotid canal.
Entering the cranial cavity, each internal carotid artery gives off the ophthalmic artery, the posterior communicating artery, the middle cerebral artery, and the anterior cerebral artery (Fig. 8.29).
Cerebral arterial circle
The cerebral arterial circle (of Willis) is formed at the base of the brain by the interconnecting vertebrobasilar and internal carotid systems of vessels (see Fig. 8.27). This anastomotic interconnection is accomplished by:
 an anterior communicating artery connecting the left and right anterior cerebral arteries to each other (Fig. 8.29; also see Fig. 8.27);
an anterior communicating artery connecting the left and right anterior cerebral arteries to each other (Fig. 8.29; also see Fig. 8.27);
 two posterior communicating arteries, one on each side, connecting the internal carotid artery with the posterior cerebral artery (Fig.8.29; also see Fig. 8.27).
two posterior communicating arteries, one on each side, connecting the internal carotid artery with the posterior cerebral artery (Fig.8.29; also see Fig. 8.27).
Clinical app
Endarterectomy
Endarterectomy is a surgical procedure to remove atheromatous plaque from arteries.
Atheromatous plaque occur in the subendothelial layer of vessels and consist of lipid laden macrophages and cholesterol debris. The developing plaque eventually accumulates fibrous connective tissue and calcifies. Plaque commonly occurs around vessel bifurcations, limiting blood flow, and may embolize to distal organs.
During endarterectomy, the plaque is removed and the vessel reopened. In many instances a patch of material is sewn over the hole in the vessel enabling improved flow and preventing narrowing from the suturing of the vessel.
Clinical app
Stroke
A stroke is the acute development of a focal neurological deficit as a result of localized or diffuse cerebral hypoperfusion.
The causes of stroke include cerebral thrombosis, cerebral hemorrhage, subarachnoid hemorrhage, and cerebral embolus. In the case of most strokes, small vessel cerebrovascular obstruction is caused by emboli from an atherosclerotic plaque within more proximal vessels in the neck and thorax.
Less severe strokes—transient ischemic attacks (TIAs)—are caused in the same way as strokes, but recovery is usually complete within 24 hours. They serve as a warning that treatment may be necessary.
Clinical app
Intracerebral aneurysms
Cerebral aneurysms most commonly arise from the vessels in and around the cerebral arterial circle (of Willis). They typically occur in and around the anterior communicating artery, the posterior communicating artery, the branches of the middle cerebral artery, the distal end of the basilar artery, and the posterior inferior cerebellar artery.
If the aneurysm ruptures, the patient complains of a sudden-onset “thunderclap” headache that produces neck stiffness and may induce vomiting. An initial CT scan demonstrates blood within the subarachnoid space, and this may be associated with an intracerebral bleed. Further management usually includes cerebral angiography, which enables the radiologist to determine the site, size, and origin of the aneurysm.
Venous drainage
Venous drainage of the brain begins internally as networks of small venous channels lead to larger cerebral veins, cerebellar veins, and veins draining the brainstem, which eventually empty into dural venous sinuses. The dural venous sinuses are endothelial-lined spaces between the outer periosteal and the inner meningeal layers of the dura mater, and eventually lead to the internal jugular veins.
Also emptying into the dural venous sinuses are diploic veins, which run between the internal and external tables of compact bone in the roof of the cranial cavity, and emissary veins, which pass from outside the cranial cavity to the dural venous sinuses (Fig. 8.30).
Fig. 8.30 Dural venous sinuses.
Dural venous sinuses
The dural venous sinuses include the superior sagittal, inferior sagittal, straight, transverse, sigmoid, and occipital sinuses, the confluence of sinuses, and the cavernous, sphenoparietal, superior petrosal, inferior petrosal, and basilar sinuses (Table 8.3, Fig. 8.31).
Table 8.3 Dural venous sinuses
|
Dural sinus |
Location |
Receives |
|
Superior sagittal |
Superior border of falx cerebri |
Superior cerebral, diploic, and emissary veins and CSF |
|
Inferior sagittal |
Inferior margin of falx cerebri |
A few cerebral veins and veins from the falx cerebri |
|
Straight |
Junction of falx cerebri and tentorium cerebelli |
Inferior sagittal sinus, great cerebral vein, posterior cerebral veins, superior cerebellar veins, and veins from the falx cerebri |
|
Occipital |
In falx cerebelli against occipital bone |
Communicates inferiorly with vertebral plexus of veins |
|
Confluence of sinuses |
Dilated space at the internal occipital protuberance |
Superior sagittal, straight, and occipital sinuses |
|
Transverse (right and left) |
Horizontal extensions from the confluence of sinuses along the posterior and lateral attachments of the tentorium cerebelli |
Drainage from confluence of sinuses (right-transverse and usually superior sagittal sinuses; left-transverse and usually straight sinuses); also superior petrosal sinus, and inferior cerebral, cerebellar, diploic, and emissary veins |
|
Sigmoid (right and left) |
Continuation of transverse sinuses to internal jugular vein; groove of parietal, temporal, and occipital bones |
Transverse sinuses, and cerebral, cerebellar, diploic, and emissary veins |
|
Cavernous (paired) |
Lateral aspect of body of sphenoid |
Cerebral and ophthalmic veins, sphenoparietal sinuses, and emissary veins from pterygoid plexus of veins |
|
Intercavernous |
Crossing sella turcica |
Interconnect cavernous sinuses |
|
Sphenoparietal (paired) |
Inferior surface of lesser wings of sphenoid |
Diploic and meningeal veins |
|
Superior petrosal (paired) |
Superior margin of petrous part of temporal bone |
Cavernous sinus, and cerebral and cerebellar veins |
|
Inferior petrosal (paired) |
Groove between petrous part of temporal bone and occipital bone ending in internal jugular vein |
Cavernous sinus, cerebellar veins, and veins from the internal ear and brainstem |
|
Basilar |
Clivus, just posterior to sella turcica of sphenoid |
Connect bilateral inferior petrosal sinuses and communicate with vertebral plexus of veins |
Fig. 8.31 Veins and dural venous sinuses.
Superior sagittal sinus
The superior sagittal sinus is in the superior border of the falx cerebri (Fig. 8.31). It begins anteriorly at the foramen cecum, where it may receive a small emissary vein from the nasal cavity, and ends posteriorly in the confluence of sinuses, usually bending to the right to empty into the right transverse sinus. The superior sagittal sinus communicates with lateral extensions (lateral lacunae) of the sinus containing numerous arachnoid granulations.
Inferior sagittal and straight sinuses
The inferior sagittal sinus is in the inferior margin of the falx cerebri (Fig. 8.31). It receives a few cerebral veins and veins from the falx cerebri, and ends posteriorly at the anterior edge of the tentorium cerebelli, where it is joined by the great cerebral vein and together with the great cerebral vein forms the straight sinus (Fig. 8.31).
The straight sinus continues posteriorly along the junction of the falx cerebri and the tentorium cerebelli and ends in the confluence of sinuses, usually bending to the left to empty into the left transverse sinus (Fig. 8.31).
Confluence of sinuses, transverse and sigmoid sinuses
The superior sagittal and straight sinuses, and the occipital sinus (in the falx cerebelli) empty into the confluence of sinuses, which is a dilated space at the internal occipital protuberance (Fig. 8.31) and is drained by the right and left transverse sinuses.
The paired transverse sinuses extend in horizontal directions from the confluence of sinuses where the tentorium cerebelli joins the lateral and posterior walls of the cranial cavity (Fig. 8.31).
The right transverse sinus usually receives blood from the superior sagittal sinus and the left transverse sinus usually receives blood from the straight sinus.
The transverse sinuses also receive blood from the superior petrosal sinus, veins from the inferior parts of the cerebral hemispheres and the cerebellum, and diploic and emissary veins.
As the transverse sinuses leave the surface of the occipital bone, they become the sigmoid sinuses (Fig. 8.31), which turn inferiorly, grooving the parietal, temporal, and occipital bones, before ending at the beginning of the internal jugular veins. The sigmoid sinuses also receive blood from cerebral, cerebellar, diploic, and emissary veins.
Cavernous sinuses
The paired cavernous sinuses are against the lateral aspect of the body of the sphenoid bone on either side of the sella turcica (Figs. 8.31, 8.32). They are of great clinical importance because of their connections and the structures that pass through them.
Fig. 8.32 Cavernous sinus.
The cavernous sinuses receive blood not only from cerebral veins, but also from the ophthalmic veins (from the orbit) and emissary veins (from the pterygoid plexus of veins in the infratemporal fossa). These connections provide pathways for infections to pass from extracranial sites into intracranial locations.
Structures passing through each cavernous sinus are (Fig. 8.32):
 the internal carotid artery, and
the internal carotid artery, and
Structures in the lateral wall of each cavernous sinus are, from superior to inferior (Fig. 8.32):
 the ophthalmic nerve [V1], and
the ophthalmic nerve [V1], and
These structures passing through the cavernous sinus and lateral walls are vulnerable to injury due to inflammation.
Connecting the right and left cavernous sinuses are the intercavernous sinuses on the anterior and posterior sides of the pituitary stalk (Fig. 8.31).
Sphenoparietal sinuses drain into the anterior ends of each cavernous sinus. These small sinuses are along the inferior surface of the lesser wings of the sphenoid and receive blood from the diploic and meningeal veins.
Superior and inferior petrosal sinuses
The superior petrosal sinuses drain the cavernous sinuses into the transverse sinuses. Each superior petrosal sinus begins at the posterior end of the cavernous sinus, passes posterolaterally along the superior margin of the petrous part of each temporal bone, and connects to the transverse sinus (Fig. 8.31). The superior petrosal sinuses also receive cerebral and cerebellar veins.
The inferior petrosal sinuses also begin at the posterior ends of the cavernous sinuses. These bilateral sinuses pass posteroinferiorly in a groove between the petrous part of the temporal bone and the basal part of the occipital bone, ending in the internal jugular veins. They assist in draining the cavernous sinuses, and also receive blood from cerebellar veins, and veins from the internal ear and brainstem.
Basilar sinuses connect the inferior petrosal sinuses to each other and to the vertebral plexus of veins. They are on the clivus, just posterior to the sella turcica of the sphenoid bone (Fig. 8.31).
Clinical app
Emissary veins
Emissary veins connect extracranial veins with intracranial veins and are important clinically because they can be a conduit through which infections can enter the cranial cavity. Emissary veins lack valves, as do the majority of veins in the head and neck.
Clinical app
Head injury
Head trauma is a common injury and is a significant cause of morbidity and death. At the time of the initial head injury two processes take place.
 First the primary brain injury may involve primary axonal and cellular damage, which results from the shearing deceleration forces within the brain. These injuries are generally not repairable. Further primary brain injuries include intracerebral hemorrhage and penetrating injuries, which may directly destroy gray and white matter.
First the primary brain injury may involve primary axonal and cellular damage, which results from the shearing deceleration forces within the brain. These injuries are generally not repairable. Further primary brain injuries include intracerebral hemorrhage and penetrating injuries, which may directly destroy gray and white matter.
Clinical app
Concussion
Concussion (mild traumatic brain injury [MTBI]) is the most common type of traumatic brain injury. The injury typically results from a rapid deceleration of the head, or by a rotation of the brain within the cranial cavity. General symptoms of MTBI can include post-traumatic amnesia, confusion, loss of consciousness, headache, dizziness, vomiting, lack of motor coordination, and light sensitivity. The diagnosis of concussion, MTBI, is based upon the event, the current neurological status, and the state of consciousness of the patient.
CRANIAL NERVES
The 12 pairs of cranial nerves are part of the peripheral nervous system (PNS) and pass through foramina or fissures in the cranial cavity. All nerves except one, the accessory nerve [XI], originate from the brain.
In addition to having similar somatic and visceral components as spinal nerves, some cranial nerves also contain special sensory and motor components (Tables 8.4, 8.5).
Table 8.4 Cranial nerve functional components
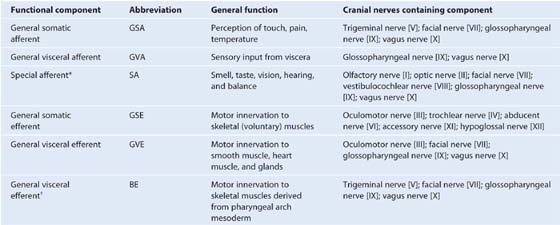
Table 8.5 Cranial nerves (see Table 8.4 for abbreviations)
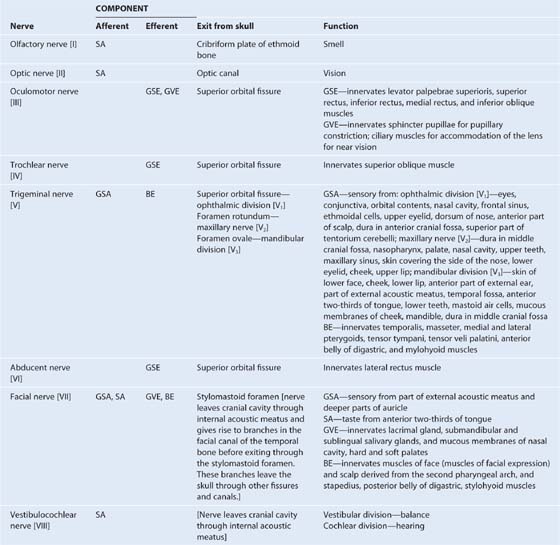
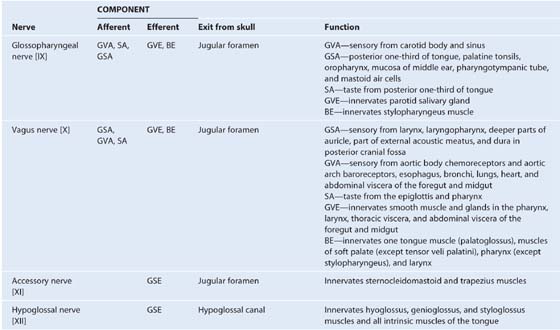
The special sensory components are associated with hearing, seeing, smelling, balancing, and tasting.
Special motor components include those that innervate skeletal muscles derived embryologically from the pharyngeal arches and not from somites.
In human embryology, six pharyngeal arches are designated, but the fifth pharyngeal arch never develops. Each of the pharyngeal arches that does develop is associated with a developing cranial nerve or one of its branches. These cranial nerves carry efferent fibers that innervate the skeletal musculature derived from the pharyngeal arch.
Innervation of the musculature derived from the five pharyngeal arches that do develop is as follows:
 first arch—trigeminal nerve [V3],
first arch—trigeminal nerve [V3],
 second arch—facial nerve [VII],
second arch—facial nerve [VII],
 third arch—glossopharyngeal nerve [IX],
third arch—glossopharyngeal nerve [IX],
 fourth arch—superior laryngeal branch of the vagus nerve [X],
fourth arch—superior laryngeal branch of the vagus nerve [X],
 sixth arch—recurrent laryngeal branch of the vagus nerve [X].
sixth arch—recurrent laryngeal branch of the vagus nerve [X].
Olfactory nerve [I]
The olfactory nerve [I] carries special afferent (SA) fibers for the sense of smell. Its sensory neurons have:
 peripheral processes that act as olfactory receptors in the nasal mucosa, and
peripheral processes that act as olfactory receptors in the nasal mucosa, and
 central processes that return information to the brain.
central processes that return information to the brain.
The receptors are in the roof and upper parts of the nasal cavity and the central processes, after joining into small bundles, enter the cranial cavity by passing through the cribriform plate of the ethmoid bone (Fig. 8.33). They terminate by synapsing with secondary neurons in the olfactory bulbs (Fig. 8.34).
Fig. 8.33 Cranial nerves exiting the cranial cavity.
Fig. 8.34 Cranial nerves on the base of the brain.
Optic nerve [II]
The optic nerve [II] carries SA fibers for vision. These fibers return information to the brain from photoreceptors in the retina. Neuronal processes leave the retinal receptors, join into small bundles, and are carried by the optic nerves to other components of the visual system in the brain. The optic nerves enter the cranial cavity through the optic canals (Fig. 8.33).
Oculomotor nerve [III]
The oculomotor nerve [III] carries two types of fibers:
 General somatic efferent (GSE) fibers innervate most of the extra-ocular muscles.
General somatic efferent (GSE) fibers innervate most of the extra-ocular muscles.
The oculomotor nerve [III] leaves the anterior surface of the brainstem between the midbrain and the pons (Fig. 8.34). It enters the anterior edge of the tentorium cerebelli, continues in an anterior direction in the lateral wall of the cavernous sinus (Figs. 8.33, 8.34; also see Fig. 8.32), and leaves the cranial cavity through the superior orbital fissure.
In the orbit, the GSE fibers in the oculomotor nerve innervate levator palpebrae superioris, superior rectus, inferior rectus, medial rectus, and inferior oblique muscles.
The GVE fibers are preganglionic parasympathetic fibers that synapse in the ciliary ganglion and ultimately innervate the sphincter pupillae muscle, responsible for pupillary constriction, and the ciliary muscles, responsible for accommodation of the lens for near vision (Table 8.6).
Table 8.6 Parasympathetic ganglia of the head
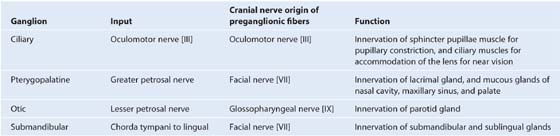
Trochlear nerve [IV]
The trochlear nerve [IV] is a cranial nerve that carries GSE fibers to innervate the superior oblique muscle, an extra-ocular muscle in the orbit. It arises in the midbrain and is the only cranial nerve to exit from the posterior surface of the brainstem (Fig. 8.34). After curving around the midbrain, it enters the inferior surface of the free edge of the tentorium cerebelli, continues in an anterior direction in the lateral wall of the cavernous sinus (Figs. 8.33, 8.34; also see Fig. 8.32), and enters the orbit through the superior orbital fissure.
Trigeminal nerve [V]
The trigeminal nerve [V] is the major sensory nerve of the head, and also innervates muscles that move the lower jaw. It carries general somatic afferent (GSA) and branchial efferent (BE) fibers:
The trigeminal nerve exits from the anterolateral surface of the pons as a large sensory root and a small motor root (Fig. 8.34). These roots continue forward out of the posterior cranial fossa and into the middle cranial fossa by passing over the medial tip of the petrous part of the temporal bone (Fig. 8.33).
In the middle cranial fossa the sensory root expands into the trigeminal ganglion (Fig. 8.33), which contains cell bodies for the sensory neurons in the trigeminal nerve and is comparable to a spinal ganglion. The ganglion is in a depression (the trigeminal depression) on the anterior surface of the petrous part of the temporal bone in a dural cave (the trigeminal cave). The motor root is below and completely separate from the sensory root at this point.
Arising from the anterior border of the trigeminal ganglion are the three terminal divisions of the trigeminal nerve, which in descending order are:
 the ophthalmic nerve (ophthalmic division [V1]),
the ophthalmic nerve (ophthalmic division [V1]),
 the maxillary nerve (maxillary division [V2]), and
the maxillary nerve (maxillary division [V2]), and
 the mandibular nerve (mandibular division [V3]).
the mandibular nerve (mandibular division [V3]).
Ophthalmic nerve [V1]
The ophthalmic nerve [V1] passes forward in the dura of the lateral wall of the cavernous sinus (see Fig. 8.32), leaves the cranial cavity, and enters the orbit through the superior orbital fissure.
The ophthalmic nerve [V1] carries sensory branches from the eyes, conjunctiva, and orbital contents, including the lacrimal gland. It also receives sensory branches from the nasal cavity, frontal sinus, ethmoidal cells, falx cerebri, dura in the anterior cranial fossa and superior parts of the tentorium cerebelli, upper eyelid, dorsum of the nose, and the anterior part of the scalp.
Maxillary nerve [V2]
The maxillary nerve [V2] passes forward in the dura mater of the lateral wall of the cavernous sinus just inferior to the ophthalmic nerve [V1] (see Fig. 8.32), leaves the cranial cavity through the foramen rotundum, and enters the pterygopalatine fossa.
The maxillary nerve [V2] receives sensory branches from the dura in the middle cranial fossa, the nasopharynx, the palate, the nasal cavity, teeth of the upper jaw, maxillary sinus, and skin covering the side of the nose, the lower eyelid, the cheek, and the upper lip.
Mandibular nerve [V3]
The mandibular nerve [V3] leaves the inferior margin of the trigeminal ganglion and leaves the skull through the foramen ovale.
The motor root of the trigeminal nerve also passes through the foramen ovale and unites with the sensory component of the mandibular nerve [V3] outside the skull. Thus the mandibular nerve [V3] is the only division of the trigeminal nerve that contains a motor component.
Outside the skull the motor fibers innervate the four muscles of mastication (temporalis, masseter, and medial and lateral pterygoids), as well as the tensor tympani, the tensor veli palatini, the anterior belly of the digastric, and the mylohyoid muscles.
The mandibular nerve [V3] also receives sensory branches from the skin of the lower face, cheek, lower lip, anterior part of the external ear, part of the external acoustic meatus and the temporal region, the anterior two-thirds of the tongue, the teeth of the lower jaw, the mastoid air cells, the mucous membranes of the cheek, the mandible, and dura in the middle cranial fossa.
Abducent nerve [VI]
The abducent nerve [VI] carries GSE fibers to innervate the lateral rectus muscle in the orbit. It arises from the brainstem between the pons and medulla and passes forward, piercing the dura covering the clivus (see Figs. 8.33, 8.34). Continuing upward in a dural canal, it crosses the superior edge of the petrous temporal bone, enters and crosses the cavernous sinus (see Fig. 8.32) just inferolateral to the internal carotid artery, and enters the orbit through the superior orbital fissure.
Facial nerve [VII]
The facial nerve [VII] carries GSA, SA, GVE, and BE fibers:
 The SA fibers are for taste from the anterior two-thirds of the tongue.
The SA fibers are for taste from the anterior two-thirds of the tongue.
The facial nerve [VII] attaches to the lateral surface of the brainstem, between the pons and medulla oblongata (see Fig. 8.34). It consists of a large motor root and a smaller sensory root (the intermediate nerve):
 The larger motor root contains the BE fibers.
The larger motor root contains the BE fibers.
The motor and sensory roots cross the posterior cranial fossa and leave the cranial cavity through the internal acoustic meatus (see Fig. 8.33). After entering the facial canal in the petrous part of the temporal bone, the two roots fuse and form the facial nerve [VII]. Near this point the nerve enlarges as the geniculate ganglion, which is similar to a spinal ganglion containing cell bodies for sensory neurons.
At the geniculate ganglion, the facial nerve [VII] turns and gives off the greater petrosal nerve, which carries mainly preganglionic parasympathetic (GVE) fibers (Table 8.6).
The facial nerve [VII] continues along the bony canal, giving off the nerve to stapedius and the chorda tympani, before exiting the skull through the stylomastoid foramen.
The chorda tympani carries taste (SA) fibers from the anterior two-thirds of the tongue and preganglionic parasympathetic (GVE) fibers destined for the submandibular ganglion (Table 8.6).
Vestibulocochlear nerve [VIII]
The vestibulocochlear nerve [VIII] carries SA fibers for hearing and balance, and consists of two divisions:
 a vestibular component for balance, and
a vestibular component for balance, and
 a cochlear component for hearing.
a cochlear component for hearing.
The vestibulocochlear nerve [VIII] attaches to the lateral surface of the brainstem, between the pons and medulla, after emerging from the internal acoustic meatus and crossing the posterior cranial fossa (see Figs. 8.33, 8.34). The two divisions combine into the single nerve seen in the posterior cranial fossa within the substance of the petrous part of the temporal bone.
Glossopharyngeal nerve [IX]
The glossopharyngeal nerve [IX] carries GVA, GSA, SA, GVE, and BE fibers:
 The GVA fibers provide sensory input from the carotid body and sinus.
The GVA fibers provide sensory input from the carotid body and sinus.
 The SA fibers are for taste from the posterior one-third of the tongue.
The SA fibers are for taste from the posterior one-third of the tongue.
 The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the parotid salivary gland.
The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the parotid salivary gland.
The glossopharyngeal nerve [IX] arises as several rootlets on the anterolateral surface of the upper medulla oblongata (see Fig. 8.34). The rootlets cross the posterior cranial fossa and enter the jugular foramen (see Fig. 8.33). Within the jugular foramen, and before exiting from it, the rootlets merge to form the glossopharyngeal nerve.
Within or immediately outside the jugular foramen are two ganglia (the superior and inferior ganglia), which contain the cell bodies of the sensory neurons in the glossopharyngeal nerve [IX].
Tympanic nerve
Branching from the glossopharyngeal nerve [IX] either within or immediately outside the jugular foramen is the tympanic nerve. This branch re-enters the temporal bone, enters the middle ear cavity, and participates in the formation of the tympanic plexus. Within the middle ear cavity it provides sensory innervation to the mucosa of the cavity, pharyngotympanic tube, and mastoid air cells.
The tympanic nerve also contributes GVE fibers, which leave the tympanic plexus in the lesser petrosal nerve—a small nerve that exits the temporal bone, enters the middle cranial fossa, and descends through the foramen ovale to exit the cranial cavity carrying preganglionic parasympathetic fibers to the otic ganglion (see Table 8.6).
Vagus nerve [X]
The vagus nerve [X] carries GSA, GVA, SA, GVE, and BE fibers:
 The SA fibers are for taste around the epiglottis and pharynx.
The SA fibers are for taste around the epiglottis and pharynx.
The vagus nerve arises as a group of rootlets on the anterolateral surface of the medulla oblongata just inferior to the rootlets arising to form the glossopharyngeal nerve [IX] (see Fig. 8.34). The rootlets cross the posterior cranial fossa and enter the jugular foramen (see Fig. 8.33). Within this foramen, and before exiting from it, the rootlets merge to form the vagus nerve [X]. Within or immediately outside the jugular foramen are two ganglia, the superior (jugular) and inferior (nodose) ganglia, which contain the cell bodies of the sensory neurons in the vagus nerve [X].
Accessory nerve [XI]
The accessory nerve [XI] is a cranial nerve that carries GSE fibers to innervate the sternocleidomastoid and trapezius muscles. It is a unique cranial nerve because its roots arise from motor neurons in the upper five segments of the cervical spinal cord. These fibers leave the lateral surface of the spinal cord and, joining together as they ascend, enter the cranial cavity through the foramen magnum (see Fig. 8.34). The accessory nerve [XI] continues through the posterior cranial fossa and exits through the jugular foramen (see Fig. 8.33). It then descends in the neck to innervate the sternocleidomastoid and trapezius muscles from their deep surfaces.
Cranial root of the accessory nerve
Some descriptions of the accessory nerve [XI] refer to a few rootlets arising from the caudal part of the medulla oblongata on the anterolateral surface just inferior to the rootlets arising to form the vagus nerve [X] as the “cranial” root of the accessory nerve (see Fig. 8.34). Leaving the medulla, the cranial roots course with the “spinal” roots of the accessory nerve [XI] into the jugular foramen, at which point the cranial roots join the vagus nerve [X]. As part of the vagus nerve [X], they are distributed to the pharyngeal musculature innervated by the vagus nerve [X] and are therefore described as being part of the vagus nerve [X].
Hypoglossal nerve [XII]
The hypoglossal nerve [XII] carries GSE fibers to innervate all intrinsic and most of the extrinsic muscles of the tongue. It arises as several rootlets from the anterior surface of the medulla, passes laterally across the posterior cranial fossa and exits through the hypoglossal canal (see Figs. 8.33, 8.34). This nerve innervates the hyoglossus, styloglossus, and genioglossus muscles and all intrinsic muscles of the tongue.
Clinical app
Cranial nerve lesions
|
Clinical findings |
Example of lesion |
|
|
Olfactory nerve [I] |
Loss of smell (anosmia) |
Injury to the cribriform plate; congenital absence |
|
Optic nerve [II] |
Blindness/visual field abnormalities, loss of pupillary constriction |
Direct trauma to the orbit; disruption of the optic pathway |
|
Oculomotor nerve [III] |
Dilated pupil, ptosis, loss of normal pupillary reflex, eye moves down inferiorly and laterally (down and out) |
Pressure from an aneurysm arising from the posterior communicating, posterior cerebral, or superior cerebellar artery; pressure from a herniating cerebral uncus (false localizing sign); cavernous sinus mass or thrombosis |
|
Trochlear nerve [IV] |
Inability to look inferiorly when the eye is adducted (down and in) |
Along the course of the nerve around the brainstem; orbital fracture |
|
Trigeminal nerve [V] |
Loss of sensation and pain in the region supplied by the three divisions of the nerve over the face; loss of motor function of the muscles of mastication on the side of the lesion |
Typically, in the region of the trigeminal ganglion, though local masses around the foramina through which the divisions pass can produce symptoms |
|
Abducent nerve [VI] |
Inability of lateral eye movement |
Brain lesion or cavernous sinus lesion extending onto the orbit |
|
Facial nerve [VII] |
Paralysis of facial muscles |
Damage to the branches within the parotid gland |
|
Vestibulocochlear nerve [VIII] |
Progressive unilateral hearing loss and tinnitus (ringing in the ear) |
Tumor at the cerebellopontine angle |
|
Glossopharyngeal nerve [IX] |
Loss of taste to the posterior one-third of the tongue and sensation of the soft palate |
Brainstem lesion; penetrating neck injury |
|
Vagus nerve [X] |
Soft palate deviation with deviation of the uvula to the normal side; vocal cord paralysis |
Brainstem lesion; penetrating neck injury |
|
Accessory nerve [XI] |
Paralysis of sternocleidomastoid and trapezius muscles |
Penetrating injury to the posterior triangle of the neck |
|
Hypoglossal nerve [XII] |
Atrophy of ipsilateral muscles of the tongue and deviation toward the affected side; speech disturbance |
Penetrating injury to the neck and skull base pathology |
FACE
A face-to-face meeting is an important initial contact between individuals. Part of this exchange is the use of facial expressions to convey emotions. In fact, a physician can gain important information about an individual’s general health by observing a patient’s face.
Thus an understanding of the unique organization of the various structures between the superciliary arches superiorly, the lower edge of the mandible inferiorly, and as far back as the ears on either side—the area defined as the face—is particularly useful in the practice of medicine.
Muscles
The muscles of the face (Table 8.7, Fig. 8.35) develop from the second pharyngeal arch and are innervated by branches of the facial nerve [VII]. They are in the superficial fascia, with origins from either bone or fascia, and insertions into the skin.
Table 8.7 Muscles of the face
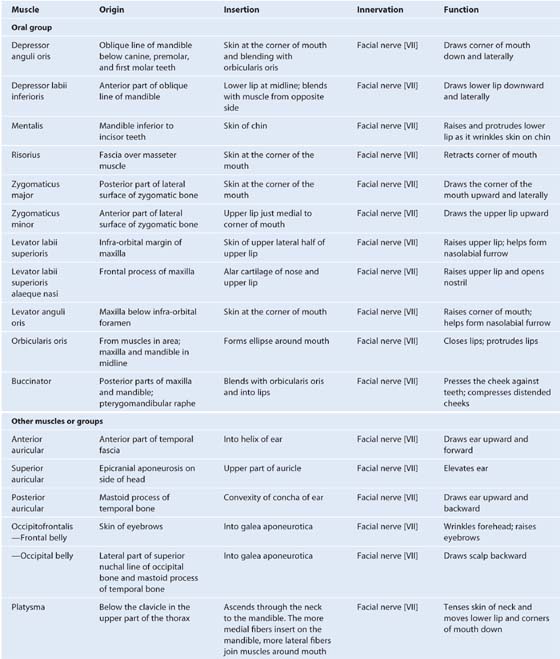
Fig. 8.35 Facial muscles.
Orbital group
Two muscles are associated with the orbital group—the orbicularis oculi and the corrugator supercilii.
The orbicularis oculi is a large muscle that completely surrounds each orbital orifice and extends into each eyelid (Table 8.7; also see Fig. 8.36). It closes the eyelids. It has two major parts:
Fig. 8.36 Orbital group of facial muscles.
The second muscle in the orbital group is the much smaller corrugator supercilii (Table 8.7; also see Fig. 8.36), which is deep to the eyebrows and the orbicularis oculi muscle and is active when frowning.
Nasal group
Three muscles are associated with the nasal group—the nasalis, the procerus, and the depressor septi nasi (Table 8.7, Fig. 8.37). The largest and best developed of the muscles of the nasal group is the nasalis, which is active when the nares are flared (Table 8.7, Fig. 8.37).
Fig. 8.37 Nasal group of facial muscles.
The procerus is a small muscle superficial to the nasal bone and is active when an individual frowns (Table 8.7, Fig. 8.37).
The final muscle in the nasal group is the depressor septi nasi, another muscle that assists in widening the nares (see Table 8.7, Fig. 8.37).
Oral group
The muscles in the oral group move the lips and cheek. They include the orbicularis oris and buccinator muscles, and a lower and upper group of muscles (Fig. 8.38; also see Table 8.7). Many of these muscles intersect just lateral to the corner of the mouth on each side at a structure termed the modiolus. The orbicularis oris is a complex muscle consisting of fibers that completely encircle the mouth (Fig. 8.38; also see Table 8.7). Its function is apparent when pursing the lips, as occurs during whistling.
Fig. 8.38 Oral group of facial muscles.
The buccinator forms the muscular component of the cheek and is used every time air expanding the cheeks is forcefully expelled (Table 8.7, Figs. 8.38, 8.39).
Fig. 8.39 Buccinator muscle.
Lower group of oral muscles
The muscles in the lower group consist of the depressor anguli oris, depressor labii inferioris, and mentalis (Table 8.7, Fig. 8.38). The depressor anguli oris is active during frowning. The depressor labii inferioris depresses the lower lip and moves it laterally, and the mentalis helps position the lip when drinking from a cup or when pouting.
Upper group of oral muscles
The muscles of the upper group of oral muscles consist of risorius, zygomaticus major, zygomaticus minor, levator labii superioris, levator labii superioris alaeque nasi, and levator anguli oris (Table 8.7, Fig. 8.38). The risorius helps produce a grin; the zygomaticus major and zygomaticus minor help produce a smile; the levator labii superioris deepens the furrow between the nose and the corner of the mouth during sadness; the levator labii superioris alaeque nasi may assist in flaring the nares; and the levator anguli oris elevates the corner of the mouth and may help deepen the furrow between the nose and the corner of the mouth during sadness.
Other muscles or muscle groups
Several additional muscles or groups of muscles not in the area defined as the face, but derived from the second pharyngeal arch and innervated by the facial nerve [VII], are considered muscles of facial expression. They include the platysma, auricular, and occipitofrontalis muscles (Table 8.7, Fig. 8.35). The platysma is a large, thin sheet of muscle in the superficial fascia of the neck. It tenses the skin of the neck and can move the lower lip and corners of the mouth down.
Three muscles associated with the ear are also in the group of “other muscles of facial expression.” These are the anterior, superior, and posterior auricular muscles (Table 8.7, Fig. 8.40).
Fig. 8.40 Auricular muscles.
The occipitofrontalis is the final muscle in this category and is associated with the scalp (Table 8.7; see Fig. 8.35). It consists of a frontal belly anteriorly and an occipital belly posteriorly. An aponeurotic tendon connects the two.
Parotid gland
The parotid glands are the largest of the three pairs of main salivary glands in the head and numerous structures pass through them. They are anterior to and below the lower half of the ear, superficial, posterior, and deep to the ramus of mandible (Fig. 8.41). They extend down to the lower border of the mandible and up to the zygomatic arch. Posteriorly they cover the anterior part of the sternocleidomastoid muscle and continue anteriorly to halfway across the masseter muscle.
Fig. 8.41 Parotid gland. A. Lateral view. B. Cross-section.
The parotid duct leaves the anterior edge of the parotid gland midway between the zygomatic arch and the corner of the mouth (see Fig. 8.41). It crosses the face in a transverse direction and, after crossing the medial border of the masseter muscle, turns deeply into the buccal fat pad and pierces the buccinator muscle. It opens into the oral cavity near the second upper molar tooth.
Important relationships
Several major structures enter and pass through or pass just deep to the parotid gland. These include the facial nerve [VII], the external carotid artery and its branches, and the retromandibular vein and its tributaries (see Fig. 8.41).
Facial nerve
The facial nerve [VII] exits the skull through the stylomastoid foramen and then passes into the parotid gland, where it usually divides into upper and lower trunks. These pass through the substance of the parotid gland, where there may be further branching and anastomosing of the nerves.
Five terminal groups of branches of the facial nerve [VII]—the temporal, zygomatic, buccal, marginal mandibular, and cervical branches—emerge from the upper, anterior, and lower borders of the parotid gland (see Fig. 8.41).
External carotid artery and its branches
The external carotid artery enters into or passes deep to the inferior border of the parotid gland (see Fig. 8.41). As it continues in a superior direction, it gives off the posterior auricular artery before dividing into its two terminal branches (the maxillary and superficial temporal arteries) near the lower border of the ear:
 The maxillary artery passes horizontally, deep to the mandible.
The maxillary artery passes horizontally, deep to the mandible.
Retromandibular vein and its tributaries
The retromandibular vein is formed in the substance of the parotid gland when the superficial temporal and maxillary veins join together (see Fig. 8.41), and pass inferiorly in the substance of the parotid gland. It usually divides into anterior and posterior branches just below the inferior border of the gland.
Arterial supply
The parotid gland receives its arterial supply from the numerous arteries that pass through its substance (see above).
Innervation
Sensory innervation of the parotid gland is provided by the auriculotemporal nerve, which is a branch of the mandibular nerve [V3]. This division of the trigeminal nerve exits the skull through the foramen ovale.
The auriculotemporal nerve also carries secretomotor fibers to the parotid gland. These postganglionic parasympathetic fibers have their origin in the otic ganglion associated with the mandibular nerve [V3] and are just inferior to the foramen ovale.
Preganglionic parasympathetic fibers to the otic ganglion come from the glossopharyngeal nerve [IX].
Clinical app
Parotid gland—tumors and stones
The parotid gland is the largest of the paired salivary glands and is enclosed within the investing layer of deep cervical fascia.
The parotid gland produces a watery saliva and salivary amylase, which are necessary for food bolus formation, oral digestion, and smooth passage of the bolus into the upper gastrointestinal tract.
The commonest tumors of the parotid gland (Fig. 8.42) are benign and typically involve the superficial gland. These include pleomorphic adenoma and part of the adenolymphoma. Their importance is in relation to their anatomical position. Critically, the relationship of the tumor to the branches of the facial nerve [VII] must be defined because resection may damage the facial nerve [VII].
Fig. 8.42 Tumor in parotid gland. Axial CT scan.
It is not uncommon for stones to develop within the parotid gland. They typically occur within the main confluence of the ducts and within the main parotid duct. The patient usually complains of intense pain when salivating and tends to avoid foods that produce this symptom. The pain can be easily reproduced in the clinic by squirting lemon juice into the patient’s mouth.
Innervation
During development a cranial nerve becomes associated with each of the pharyngeal arches. Because the face is primarily derived from the first and second pharyngeal arches, innervation of neighboring facial structures varies as follows:
 The trigeminal nerve [V] innervates facial structures derived from the first arch.
The trigeminal nerve [V] innervates facial structures derived from the first arch.
 The facial nerve [VII] innervates facial structures derived from the second arch.
The facial nerve [VII] innervates facial structures derived from the second arch.
Sensory innervation
Because the face is derived developmentally from a number of structures originating from the first pharyngeal arch, cutaneous innervation of the face is by branches of the trigeminal nerve [V].
The trigeminal nerve [V] divides into three major divisions—the ophthalmic [V1], maxillary [V2], and mandibular [V3] nerves—before leaving the middle cranial fossa (Fig. 8.43). Each of these divisions passes out of the cranial cavity to innervate a part of the face, so most of the skin covering the face is innervated by branches of the trigeminal nerve [V]. The exception is a small area covering the angle and lower border of the ramus of mandible and parts of the ear, which are innervated by the trigeminal [V], facial [VII], vagus [X], and cervical nerves.
Fig. 8.43 Trigeminal nerve [V] leaving the skull.
Ophthalmic nerve [V1]
The ophthalmic nerve [V1] exits the skull through the superior orbital fissure and enters the orbit (Fig. 8.43). Its branches that innervate the face include (Fig. 8.44):
 the external nasal nerve, which supplies the anterior part of the nose.
the external nasal nerve, which supplies the anterior part of the nose.
Fig. 8.44 Cutaneous distribution of the trigeminal nerve [V].
Maxillary nerve [V2]
The maxillary nerve [V2] exits the skull through the foramen rotundum. Branches (see Fig. 8.43) that innervate the face include (Fig. 8.44):
 the large infra-orbital nerve, which exits the maxilla through the infra-orbital foramen and immediately divides into multiple branches to supply the lower eyelid, cheek, side of the nose, and upper lip (Fig. 8.44).
the large infra-orbital nerve, which exits the maxilla through the infra-orbital foramen and immediately divides into multiple branches to supply the lower eyelid, cheek, side of the nose, and upper lip (Fig. 8.44).
Mandibular nerve [V3]
The mandibular nerve [V3] exits the skull through the foramen ovale. Branches (see Fig. 8.43) innervating the face include (Fig. 8.44):
 the buccal nerve, which is on the surface of the buccinator muscle supplying the cheek; and
the buccal nerve, which is on the surface of the buccinator muscle supplying the cheek; and
Clinical app
Trigeminal neuralgia
Trigeminal neuralgia (tic douloureux) is a complex sensory disorder of the sensory root of the trigeminal nerve. Typically the pain is in the region of the mandibular [V3] and maxillary [V2] nerves, and is typically of sudden onset, excruciating in nature, and may be triggered by touching a sensitive region of skin.
Motor innervation
The muscles of the face, as well as those associated with the ear and the scalp, are derived from the second pharyngeal arch. The cranial nerve associated with this arch is the facial nerve [VII] and therefore branches of the facial nerve [VII] innervate all these muscles (Fig. 8.45A).
Fig. 8.45 Facial nerve [VII] on the face. A. Terminal branches. B. Branches before entering the parotid gland.
The facial nerve [VII] exits the posterior cranial fossa through the internal acoustic meatus. It passes through the temporal bone, giving off several branches, and emerges from the base of the skull through the stylomastoid foramen (Fig. 8.45B). At this point it gives off the posterior auricular nerve. This branch passes upward, behind the ear, to supply the occipital belly of the occipitofrontalis muscle of the scalp and the posterior auricular muscle of the ear.
The main stem of the facial nerve [VII] then gives off another branch, which innervates the posterior belly of the digastric muscle and the stylohyoid muscle. At this point, the facial nerve [VII] enters the deep surface of the parotid gland (Fig. 8.45B).
Once in the parotid gland, the main stem of the facial nerve [VII] usually divides into upper (temporofacial) and lower (cervicofacial) branches. As these branches pass through the substance of the parotid gland, they may branch further or take part in an anastomotic network (the parotid plexus).
Whatever types of interconnections occur, five terminal groups of branches of the facial nerve [VII]—the temporal, zygomatic, buccal, marginal mandibular, and cervical branches—emerge from the parotid gland (Fig. 8.45A).
Although there are variations in the pattern of distribution of the five terminal groups of branches, the basic pattern is as follows:
 Buccal branches emerge from the anterior border of the parotid gland to supply muscles in the cheek, the upper lip, and the corner of the mouth.
Buccal branches emerge from the anterior border of the parotid gland to supply muscles in the cheek, the upper lip, and the corner of the mouth.
 Cervical branches emerge from the inferior border of the parotid gland to supply the platysma.
Cervical branches emerge from the inferior border of the parotid gland to supply the platysma.
Vessels
The arterial supply to the face is primarily from branches of the external carotid artery, though there is some limited supply from a branch of the internal carotid artery.
Similarly, most of the venous return is back to the internal jugular vein, though some important connections from the face result in venous return through a clinically relevant intracranial pathway involving the cavernous sinus.
Arteries
Facial artery
The facial artery is the major vessel supplying the face (Fig. 8.46A). It branches from the anterior surface of the external carotid artery (Fig. 8.46B), passes up through the deep structures of the neck, and appears at the lower border of the mandible after passing posterior to the submandibular gland. Curving around the inferior border of the mandible just anterior to the masseter, where its pulse can be felt, the facial artery then enters the face (Fig. 8.46B). From this point, the facial artery runs upward and medially in a tortuous course. It passes along the side of the nose and terminates as the angular artery at the medial corner of the eye.
Fig. 8.46 Vasculature of the face. A. Lateral view. B. Branches of the maxillary artery.
Along its path the facial artery is deep to the platysma, risorius, and zygomaticus major and minor, superficial to the buccinator and levator anguli oris, and may pass superficially to or through the levator labii superioris.
Branches of the facial artery include the superior and inferior labial branches and the lateral nasal branch (Fig. 8.46B).
The labial branches arise near the corner of the mouth:
 The inferior labial branch supplies the lower lip.
The inferior labial branch supplies the lower lip.
 The superior labial branch supplies the upper lip and also provides a branch to the nasal septum.
The superior labial branch supplies the upper lip and also provides a branch to the nasal septum.
Near the midline, the superior and inferior labial branches anastomose with their companion arteries from the opposite side of the face. This provides an important connection between the facial arteries and the external carotid arteries of opposite sides.
The lateral nasal branch is a small branch arising from the facial artery as it passes along the side of the nose. It supplies the lateral surface and dorsum of the nose.
Transverse facial artery
Another contributor to the vascular supply of the face is the transverse facial artery (Fig. 8.46A,B), which is a branch of the superficial temporal artery (the smaller of the two terminal branches of the external carotid artery).
The transverse facial artery arises from the superficial temporal artery within the substance of the parotid gland, passes through the gland, and crosses the face in a transverse direction. Lying on the superficial surface of the masseter muscle, it is between the zygomatic arch and the parotid duct.
Branches of the maxillary artery
The maxillary artery, the larger of the two terminal branches of the external carotid artery, gives off several small branches that contribute to the arterial supply to the face (Fig. 8.46):
 The mental artery enters the face through the mental foramen and supplies the chin.
The mental artery enters the face through the mental foramen and supplies the chin.
Branches of the ophthalmic artery
Three small arteries from the internal carotid artery also contribute to the arterial supply of the face. These vessels arise from the ophthalmic artery, a branch of the internal carotid artery, after the ophthalmic artery enters the orbit:
 The zygomaticofacial and zygomaticotemporal arteries come from the lacrimal branch of the ophthalmic artery (Fig. 8.46A), enter the face through the zygomaticofacial and zygomaticotemporal foramina, and supply the area of the face over the zygomatic bone.
The zygomaticofacial and zygomaticotemporal arteries come from the lacrimal branch of the ophthalmic artery (Fig. 8.46A), enter the face through the zygomaticofacial and zygomaticotemporal foramina, and supply the area of the face over the zygomatic bone.
 The dorsal nasal artery, a terminal branch of the ophthalmic artery, exits the orbit in the medial corner, and supplies the dorsum of the nose (Fig. 8.46A).
The dorsal nasal artery, a terminal branch of the ophthalmic artery, exits the orbit in the medial corner, and supplies the dorsum of the nose (Fig. 8.46A).
Other branches of the ophthalmic artery (the supra-orbital and supratrochlear arteries) supply the anterior scalp.
Veins
Facial vein
The facial vein is the major vein draining the face (Fig. 8.47). Its point of origin is near the medial corner of the orbit as the supratrochlear and supra-orbital veins come together to form the angular vein. This vein becomes the facial vein as it proceeds inferiorly and assumes a position just posterior to the facial artery. The facial vein descends across the face with the facial artery until it reaches the inferior border of the mandible. Here the artery and vein part company and the facial vein passes superficial to the submandibular gland to enter the internal jugular vein.
Fig. 8.47 Intracranial venous connections.
Throughout its course, the facial vein receives tributaries from veins draining the eyelids, external nose, lips, cheek, and chin that accompany the various branches of the facial artery.
Transverse facial vein
The transverse facial vein is a small vein that accompanies the transverse facial artery in its journey across the face (see Fig. 8.46). It empties into the superficial temporal vein within the substance of the parotid gland.
Intracranial venous connections
As it crosses the face, the facial vein has numerous connections with venous channels passing into deeper regions of the head (see Fig. 8.47):
 Near the medial corner of the orbit, it communicates with ophthalmic veins.
Near the medial corner of the orbit, it communicates with ophthalmic veins.
 In the area of the cheek, it communicates with veins passing into the infra-orbital foramen.
In the area of the cheek, it communicates with veins passing into the infra-orbital foramen.
All these venous channels have interconnections with the intracranial cavernous sinus through emissary veins that connect intracranial with extracranial veins. There are no valves in the facial vein or any other venous channels in the head, so blood can move in any direction. Because of the interconnections between the veins, infections of the face, primarily above the mouth (i.e., the “danger area”) should be handled with great care to prevent the dissemination of infectious material in an intracranial direction.
Lymphatic drainage
Lymphatic drainage from the face primarily moves toward three groups of lymph nodes (Fig. 8.48):
Fig. 8.48 Lymphatic drainage of the face.
Clinical app
Facial nerve [VII] palsy (Bell’s palsy)
The complexity of the facial nerve [VII] is demonstrated by the different pathological processes and sites at which these processes occur.
A primary brainstem lesion affecting the motor nucleus of the facial nerve (VII) would lead to ipsilateral (same side) weakness of the whole face. However, because the upper part of the nucleus receives motor input from the left and right cerebral hemispheres, a lesion occurring above the nucleus leads to contralateral lower facial weakness. In this example, motor innervation to the upper face is spared because the upper part of the nucleus receives input from both hemispheres. Preservation and loss of the special functions are determined by the extent of the lesion.
Lesions at and around the geniculate ganglion
Typically lesions at and around the geniculate ganglion are accompanied by loss of motor function on the whole of the ipsilateral (same) side of the face. Taste to the anterior two-thirds of the tongue, lacrimation, and some salivation also are likely to be affected because the lesion is proximal to the greater petrosal and chorda tympani branches of the nerve.
Lesions at and around the stylomastoid foramen
Lesions at and around the stylomastoid foramen are the commonest abnormality of the facial nerve [VII] and usually result from a viral inflammation of the nerve within the bony canal before exiting through the stylomastoid foramen. Typically the patient has an ipsilateral loss of motor function of the whole side of the face, which produces an unusual appearance. Lacrimation and taste may not be affected if the lesion remains distal to the greater petrosal and chorda tympani branches that originate deep in the temporal bone.
Surface anatomy
Major features of the face
The major features of the face are those related to the anterior openings of the orbit, the nasal cavities, and the oral cavity (Fig. 8.49).
Fig. 8.49 Major features of the face. Anterior head and neck of a woman.
The palpebral fissures are between the upper and lower eyelids and can be opened and closed. The oral fissure is the gap between the upper and lower lips and can also be opened and closed.
The sphincter muscles of the oral and palpebral fissures are the orbicularis oris and orbicularis oculi muscles, respectively. These muscles are innervated by the facial nerve [VII].
The nares are the anterior apertures of the nasal cavities and are continuously open.
The vertical groove in the midline between the external nose and the upper lip is the philtrum.
Sensory innervation of the face is carried by the trigeminal nerve [V]. The three divisions of this nerve are represented on the face and can be tested by touching the forehead (the ophthalmic nerve [V1]), the anterior cheek (the maxillary nerve [V2]), and skin over the anterior body of the mandible (the mandibular nerve [V3]).

 Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases the cranial cavity,
the cranial cavity, two ears,
two ears, two orbits,
two orbits, two nasal cavities, and
two nasal cavities, and an oral cavity.
an oral cavity.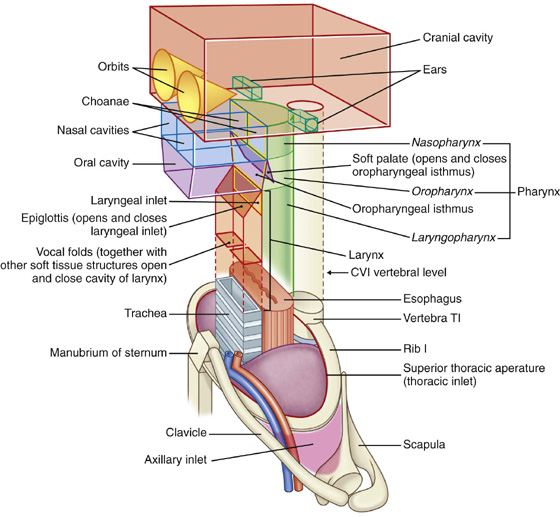
 The visceral compartment contains important glands (thyroid, parathyroid, and thymus), and parts of the respiratory and digestive tracts (larynx and pharynx) that pass between the head and thorax.
The visceral compartment contains important glands (thyroid, parathyroid, and thymus), and parts of the respiratory and digestive tracts (larynx and pharynx) that pass between the head and thorax. The two vascular compartments, one on each side, contain the major blood vessels and the vagus nerve.
The two vascular compartments, one on each side, contain the major blood vessels and the vagus nerve.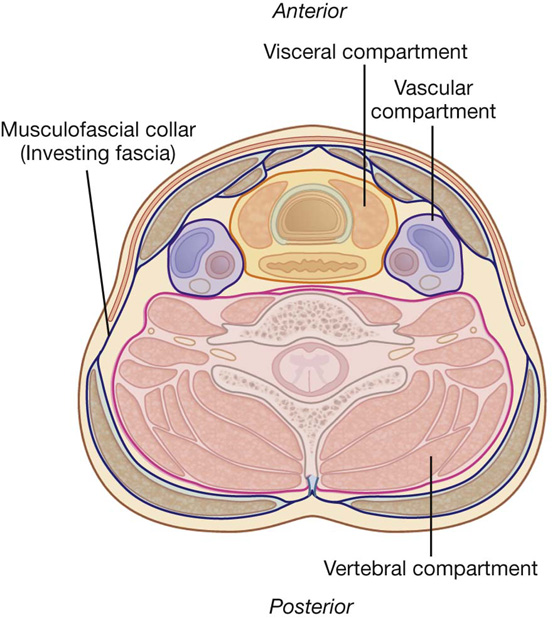
 Contains the upper parts of the respiratory and digestive systems—the nasal and oral cavities—which have structural features for modifying the air or food passing into each system.
Contains the upper parts of the respiratory and digestive systems—the nasal and oral cavities—which have structural features for modifying the air or food passing into each system. Contains specialized structures (pharynx and larynx) that connect the upper parts of the digestive and respiratory tracts (nasal and oral cavities) in the head, with the esophagus and trachea, which begin relatively low in the neck and pass into the thorax.
Contains specialized structures (pharynx and larynx) that connect the upper parts of the digestive and respiratory tracts (nasal and oral cavities) in the head, with the esophagus and trachea, which begin relatively low in the neck and pass into the thorax.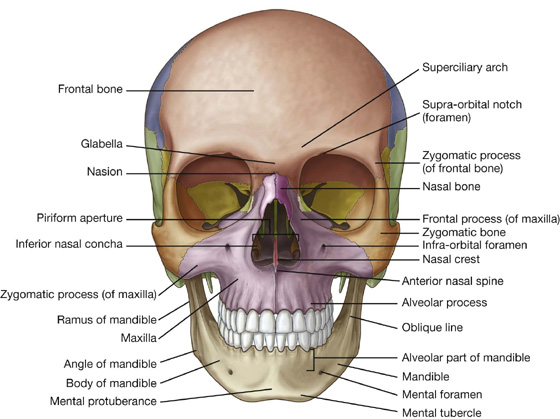
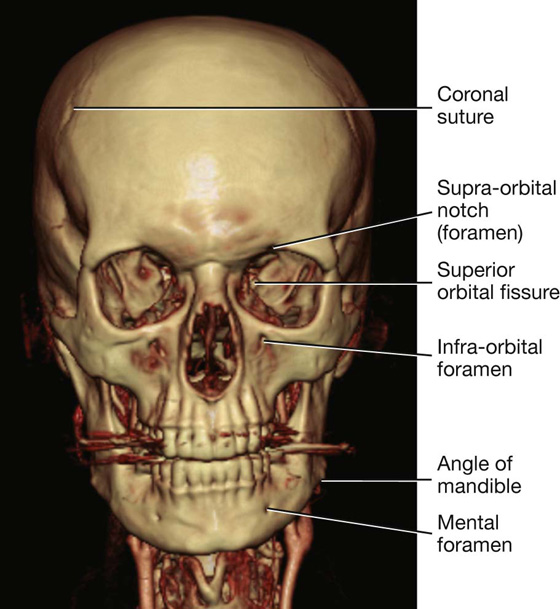
 Bones forming the lateral portion of the calvaria include the frontal, parietal, occipital, sphenoid, and temporal bones.
Bones forming the lateral portion of the calvaria include the frontal, parietal, occipital, sphenoid, and temporal bones. Bones forming the visible part of the facial skeleton include the nasal, maxilla, and zygomatic bones.
Bones forming the visible part of the facial skeleton include the nasal, maxilla, and zygomatic bones.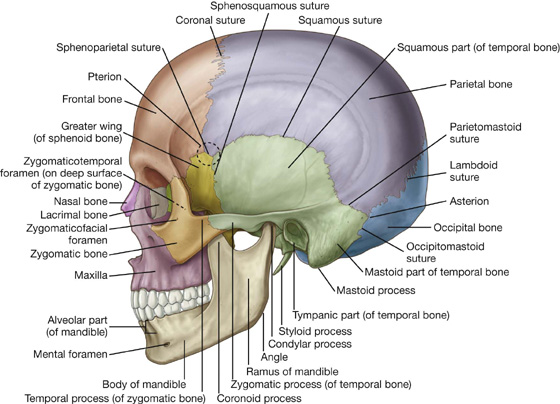
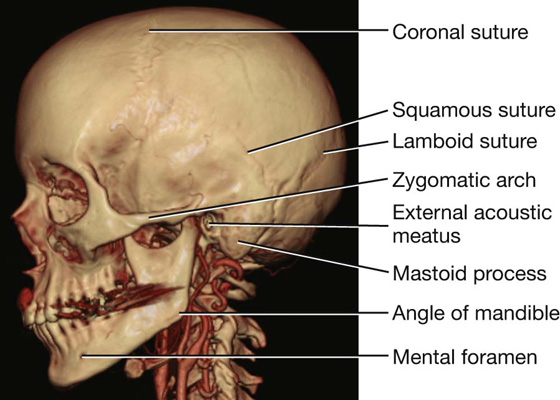
 The squamous part has the appearance of a large flat plate, forms the anterior and superior parts of the temporal bone, contributes to the lateral wall of the cranium, and articulates anteriorly with the greater wing of the sphenoid bone at the sphenosquamous suture, and with the parietal bone superiorly at the squamous suture.
The squamous part has the appearance of a large flat plate, forms the anterior and superior parts of the temporal bone, contributes to the lateral wall of the cranium, and articulates anteriorly with the greater wing of the sphenoid bone at the sphenosquamous suture, and with the parietal bone superiorly at the squamous suture. The zygomatic process is an anterior bony projection from the lower surface of the squamous part of the temporal bone that initially projects laterally and then curves anteriorly to articulate with the temporal process of the zygomatic bone to form the zygomatic arch.
The zygomatic process is an anterior bony projection from the lower surface of the squamous part of the temporal bone that initially projects laterally and then curves anteriorly to articulate with the temporal process of the zygomatic bone to form the zygomatic arch. Immediately below the origin of the zygomatic process from the squamous part of the temporal bone is the tympanic part of the temporal bone, and clearly visible on the surface of this part is the external acoustic opening leading to the external acoustic meatus (ear canal).
Immediately below the origin of the zygomatic process from the squamous part of the temporal bone is the tympanic part of the temporal bone, and clearly visible on the surface of this part is the external acoustic opening leading to the external acoustic meatus (ear canal). The petromastoid part, which is usually separated into a petrous part and a mastoid part for descriptive purposes.
The petromastoid part, which is usually separated into a petrous part and a mastoid part for descriptive purposes. a nasal bone anteriorly;
a nasal bone anteriorly; the maxilla with its alveolar process containing teeth forming the upper jaw; anteriorly, it articulates with the nasal bone; superiorly, it contributes to the formation of the inferior and medial borders of the orbit; medially, its frontal process articulates with the frontal bone; laterally, its zygomatic process articulates with the zygomatic bone;
the maxilla with its alveolar process containing teeth forming the upper jaw; anteriorly, it articulates with the nasal bone; superiorly, it contributes to the formation of the inferior and medial borders of the orbit; medially, its frontal process articulates with the frontal bone; laterally, its zygomatic process articulates with the zygomatic bone; the zygomatic bone, an irregularly shaped bone with a rounded lateral surface that forms the prominence of the cheek, is a visual centerpiece in this view; medially, it assists in the formation of the inferior rim of the orbit through its articulation with the zygomatic process of the maxilla; superiorly, its frontal process articulates with the zygomatic process of the frontal bone assisting in the formation of the lateral rim of the orbit; laterally, seen prominently in this view of the skull, the horizontal temporal process of the zygomatic bone projects backward to articulate with the zygomatic process of the temporal bone and so form the zygomatic arch.
the zygomatic bone, an irregularly shaped bone with a rounded lateral surface that forms the prominence of the cheek, is a visual centerpiece in this view; medially, it assists in the formation of the inferior rim of the orbit through its articulation with the zygomatic process of the maxilla; superiorly, its frontal process articulates with the zygomatic process of the frontal bone assisting in the formation of the lateral rim of the orbit; laterally, seen prominently in this view of the skull, the horizontal temporal process of the zygomatic bone projects backward to articulate with the zygomatic process of the temporal bone and so form the zygomatic arch.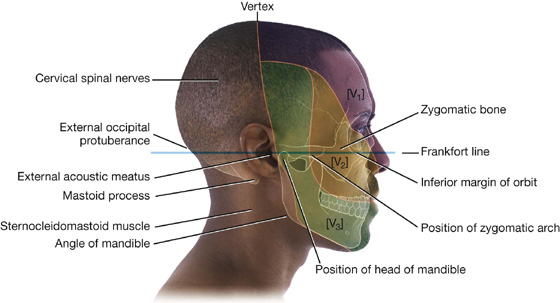
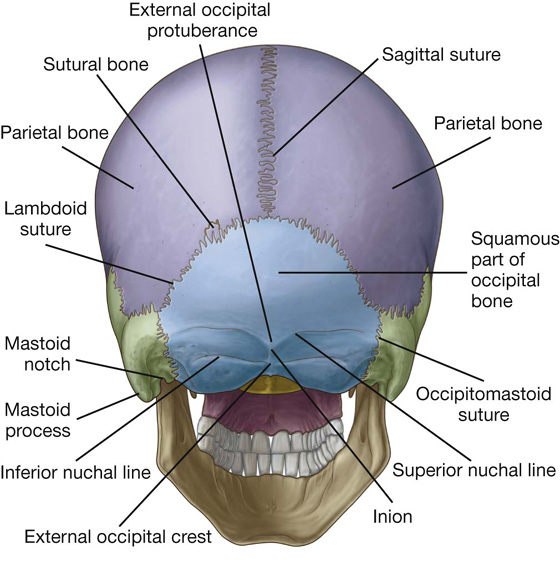
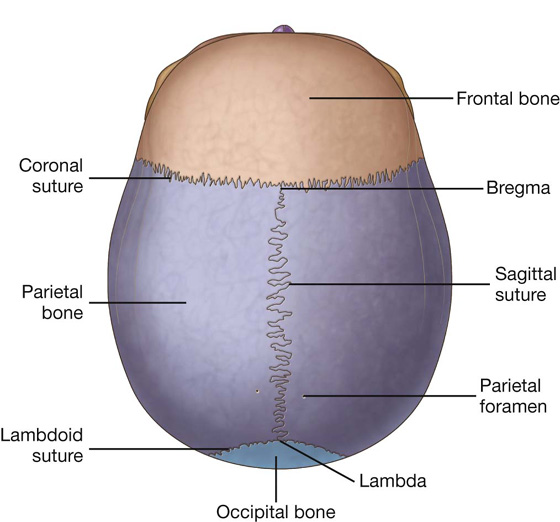
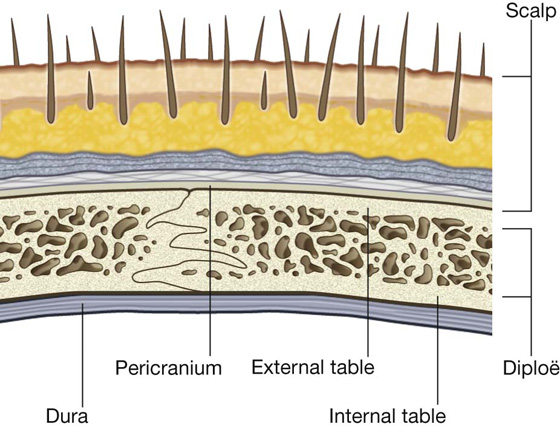
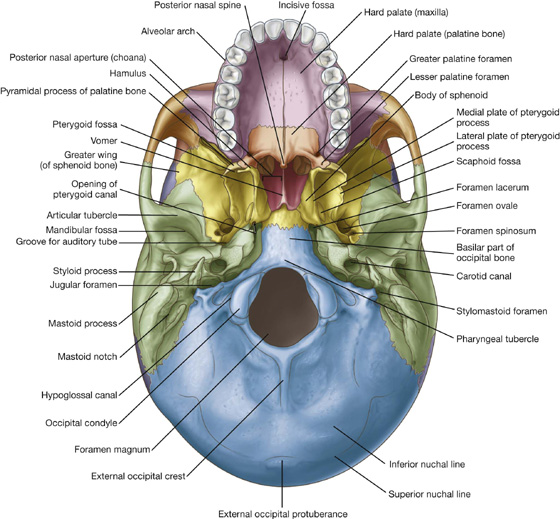
 a middle part, which extends from behind the hard palate to the anterior margin of the foramen magnum; and
a middle part, which extends from behind the hard palate to the anterior margin of the foramen magnum; and a posterior part, which extends from the anterior edge of the foramen magnum to the superior nuchal lines.
a posterior part, which extends from the anterior edge of the foramen magnum to the superior nuchal lines. The incisive fossa in the anterior midline immediately posterior to the teeth, the walls of which contain incisive foramina (the openings of the incisive canals, which are passageways between the hard palate and nasal cavity).
The incisive fossa in the anterior midline immediately posterior to the teeth, the walls of which contain incisive foramina (the openings of the incisive canals, which are passageways between the hard palate and nasal cavity). The greater palatine foramina near the posterolateral border of the hard palate on each side, which lead to greater palatine canals.
The greater palatine foramina near the posterolateral border of the hard palate on each side, which lead to greater palatine canals. Just posterior to the greater palatine foramina, the lesser palatine foramina in the pyramidal process of each palatine bone, which lead to lesser palatine canals.
Just posterior to the greater palatine foramina, the lesser palatine foramina in the pyramidal process of each palatine bone, which lead to lesser palatine canals. A midline pointed projection (the posterior nasal spine) in the free posterior border of the hard palate.
A midline pointed projection (the posterior nasal spine) in the free posterior border of the hard palate.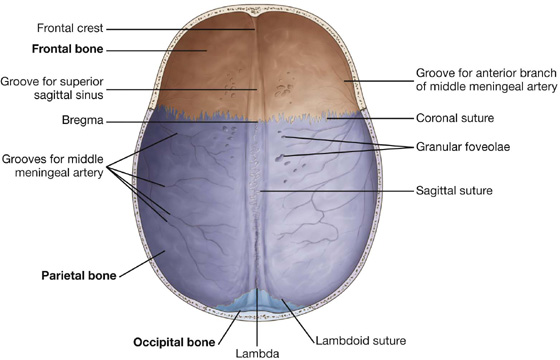
 a midline ridge of bone extending from the surface of the frontal bone (the frontal crest), which is a point of attachment for the falx cerebri (a specialization of the dura mater that partially separates the two cerebral hemispheres);
a midline ridge of bone extending from the surface of the frontal bone (the frontal crest), which is a point of attachment for the falx cerebri (a specialization of the dura mater that partially separates the two cerebral hemispheres); at the superior point of the termination of the frontal crest the beginning of the groove for the superior sagittal sinus, which widens and deepens posteriorly and marks the position of the superior sagittal sinus (an intradural venous structure);
at the superior point of the termination of the frontal crest the beginning of the groove for the superior sagittal sinus, which widens and deepens posteriorly and marks the position of the superior sagittal sinus (an intradural venous structure); on either side of the groove for the superior sagittal sinus throughout its course, a small number of depressions and pits (the granular foveolae), which mark the location of arachnoid granulations (prominent structures readily identifiable when a brain with its meningeal coverings is examined; the arachnoid granulations are involved in the reabsorption of cerebrospinal fluid); and
on either side of the groove for the superior sagittal sinus throughout its course, a small number of depressions and pits (the granular foveolae), which mark the location of arachnoid granulations (prominent structures readily identifiable when a brain with its meningeal coverings is examined; the arachnoid granulations are involved in the reabsorption of cerebrospinal fluid); and on the lateral aspects of the roof of the cranial cavity, smaller grooves created by various meningeal vessels.
on the lateral aspects of the roof of the cranial cavity, smaller grooves created by various meningeal vessels.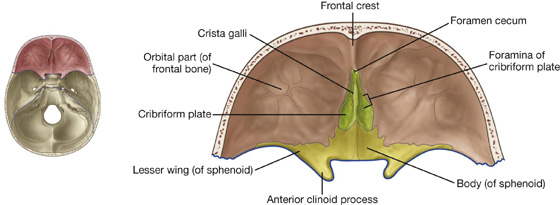
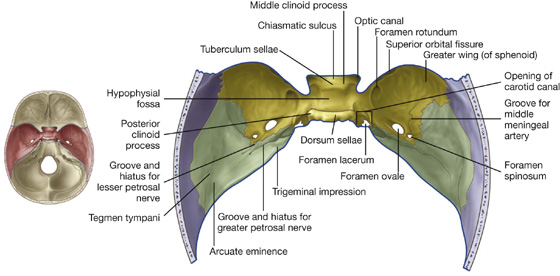
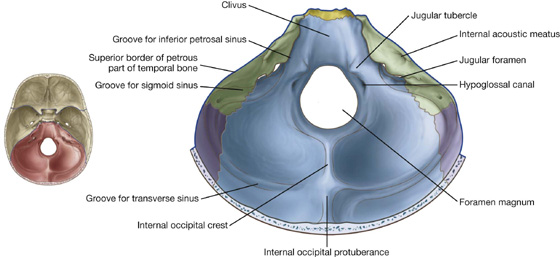
 On either side of the internal occipital crest, the floor of the posterior cranial fossa is concave to accommodate the cerebellar hemispheres.
On either side of the internal occipital crest, the floor of the posterior cranial fossa is concave to accommodate the cerebellar hemispheres. The internal occipital crest ends superiorly in a bony prominence (the internal occipital protuberance).
The internal occipital crest ends superiorly in a bony prominence (the internal occipital protuberance). Extending laterally from the internal occipital protuberance are grooves produced by the transverse sinuses, which continue laterally, eventually joining a groove for each sigmoid sinus; each of these grooves then turns inferiorly toward the jugular foramina.
Extending laterally from the internal occipital protuberance are grooves produced by the transverse sinuses, which continue laterally, eventually joining a groove for each sigmoid sinus; each of these grooves then turns inferiorly toward the jugular foramina.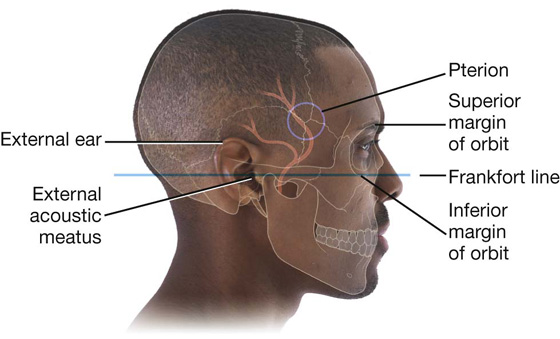
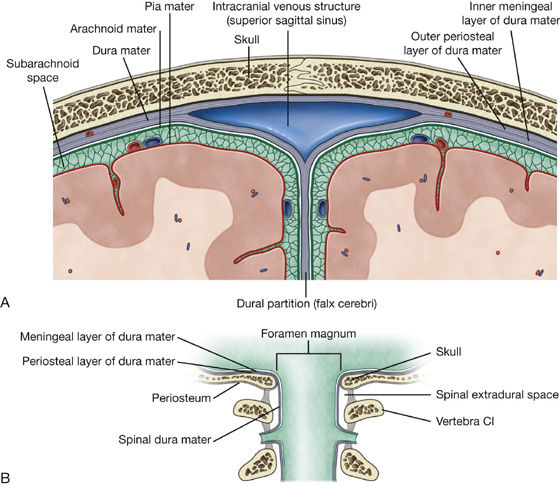
 The inner meningeal layer is in close contact with the arachnoid mater and is continuous with the spinal dura mater through the foramen magnum.
The inner meningeal layer is in close contact with the arachnoid mater and is continuous with the spinal dura mater through the foramen magnum.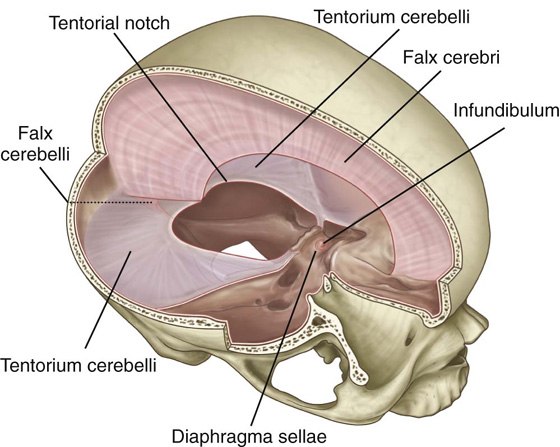
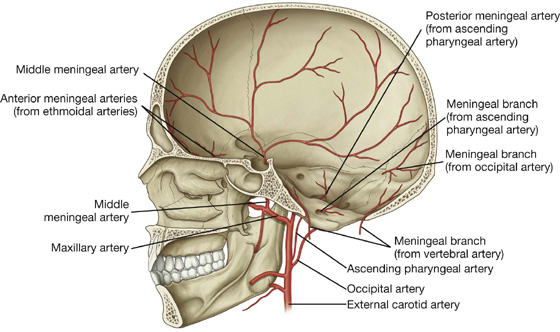
 The anterior branch passes in an almost vertical direction to reach the vertex of the skull, crossing the pterion during its course.
The anterior branch passes in an almost vertical direction to reach the vertex of the skull, crossing the pterion during its course. The posterior branch passes in a posterosuperior direction, supplying this region of the middle cranial fossa.
The posterior branch passes in a posterosuperior direction, supplying this region of the middle cranial fossa. The posterior meningeal artery, the terminal branch of the ascending pharyngeal artery, enters the posterior cranial fossa through the jugular foramen.
The posterior meningeal artery, the terminal branch of the ascending pharyngeal artery, enters the posterior cranial fossa through the jugular foramen. A meningeal branch from the ascending pharyngeal artery enters the posterior cranial fossa through the hypoglossal canal.
A meningeal branch from the ascending pharyngeal artery enters the posterior cranial fossa through the hypoglossal canal. Meningeal branches from the occipital artery enter the posterior cranial fossa through the jugular foramen and the mastoid foramen.
Meningeal branches from the occipital artery enter the posterior cranial fossa through the jugular foramen and the mastoid foramen. A meningeal branch from the vertebral artery arises as the vertebral artery enters the posterior cranial fossa through the foramen magnum.
A meningeal branch from the vertebral artery arises as the vertebral artery enters the posterior cranial fossa through the foramen magnum.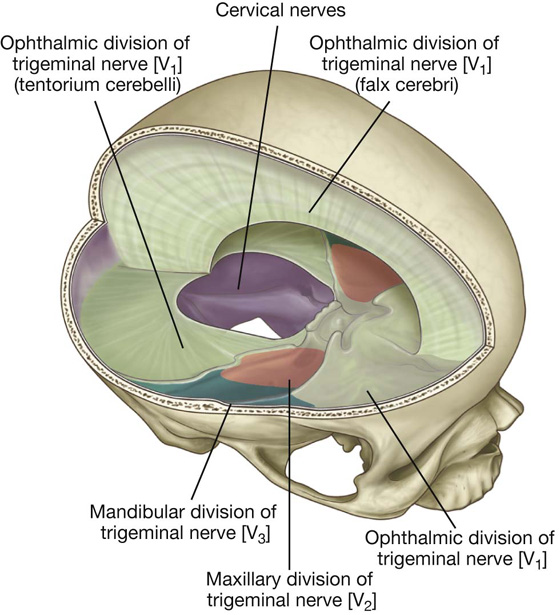
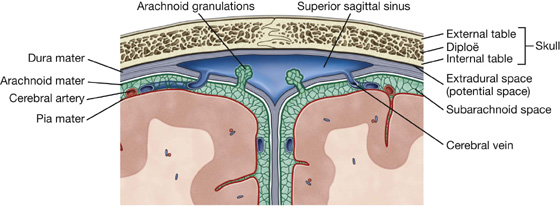
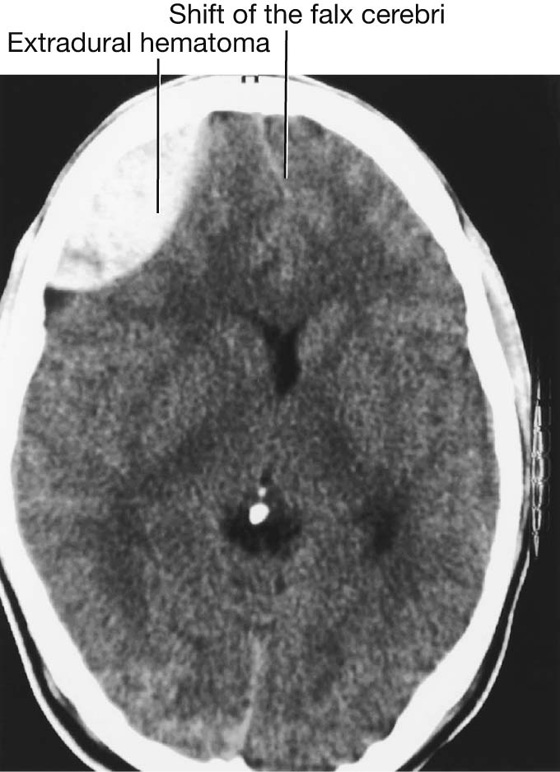
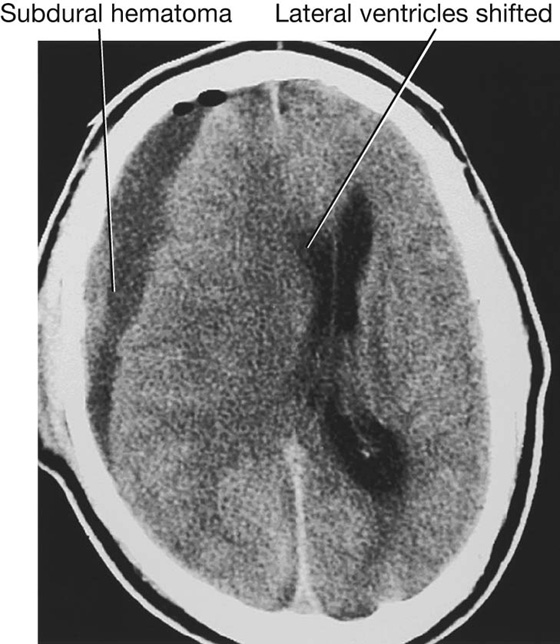
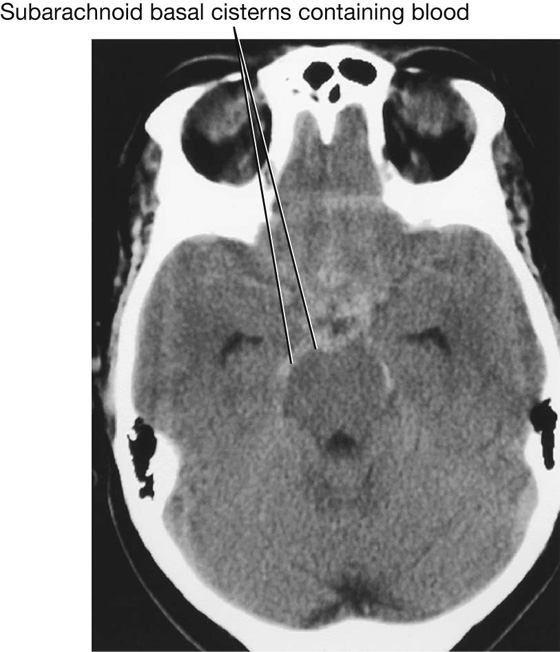
 the telencephalon (cerebrum), which becomes the large cerebral hemispheres, the surface of which consists of elevations (gyri) and depressions (sulci) and is partially separated by a deep longitudinal fissure, and which fill the area of the skull above the tentorium cerebelli and are subdivided into lobes based on their position.
the telencephalon (cerebrum), which becomes the large cerebral hemispheres, the surface of which consists of elevations (gyri) and depressions (sulci) and is partially separated by a deep longitudinal fissure, and which fill the area of the skull above the tentorium cerebelli and are subdivided into lobes based on their position. the diencephalon, which is hidden from view in the adult brain by the cerebral hemispheres, consists of the thalamus, hypothalamus, and other related structures, and classically is considered to be the most rostral part of the brainstem. (However, in common use today, the term brainstem usually refers to the midbrain, pons, and medulla);
the diencephalon, which is hidden from view in the adult brain by the cerebral hemispheres, consists of the thalamus, hypothalamus, and other related structures, and classically is considered to be the most rostral part of the brainstem. (However, in common use today, the term brainstem usually refers to the midbrain, pons, and medulla); the metencephalon, which gives rise to the cerebellum (consisting of two lateral hemispheres and a midline part in the posterior cranial fossa below the tentorium cerebelli) and the pons (anterior to the cerebellum, a bulging part of the brainstem in the most anterior part of the posterior cranial fossa against the clivus and dorsum sellae); and
the metencephalon, which gives rise to the cerebellum (consisting of two lateral hemispheres and a midline part in the posterior cranial fossa below the tentorium cerebelli) and the pons (anterior to the cerebellum, a bulging part of the brainstem in the most anterior part of the posterior cranial fossa against the clivus and dorsum sellae); and the myelencephalon (medulla oblongata), the caudal most part of the brainstem, which ends at the foramen magnum or the uppermost rootlets of the first cervical nerve and to which cranial nerves VI to XII are attached.
the myelencephalon (medulla oblongata), the caudal most part of the brainstem, which ends at the foramen magnum or the uppermost rootlets of the first cervical nerve and to which cranial nerves VI to XII are attached.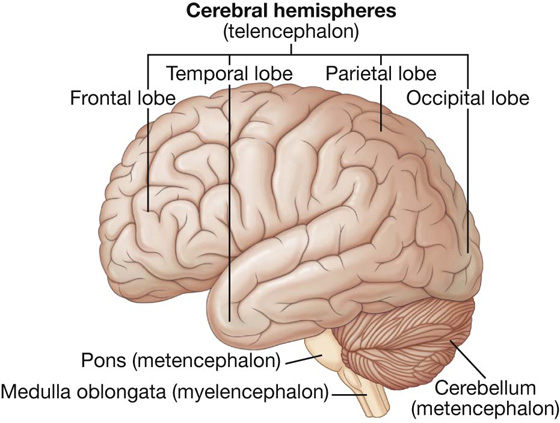
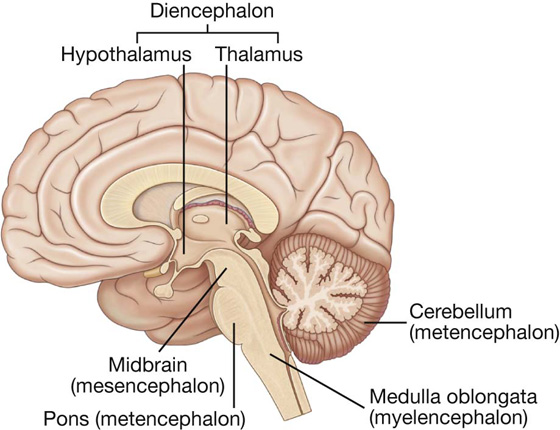
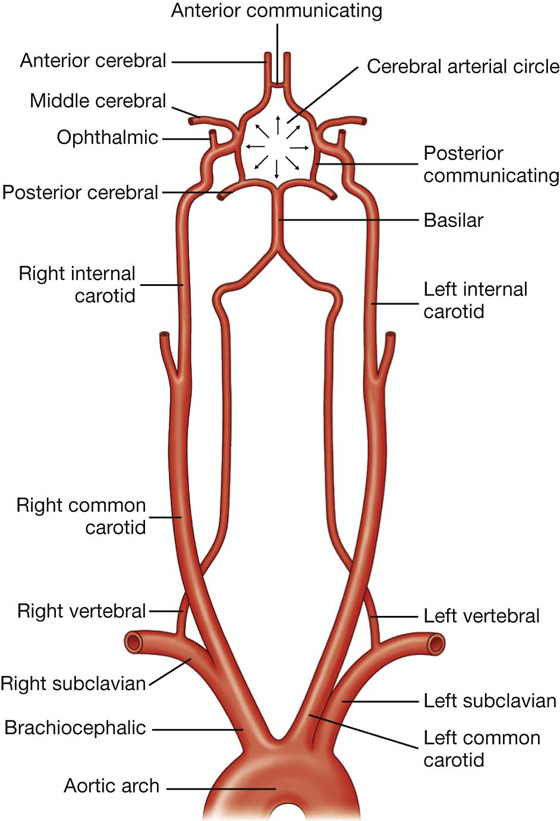
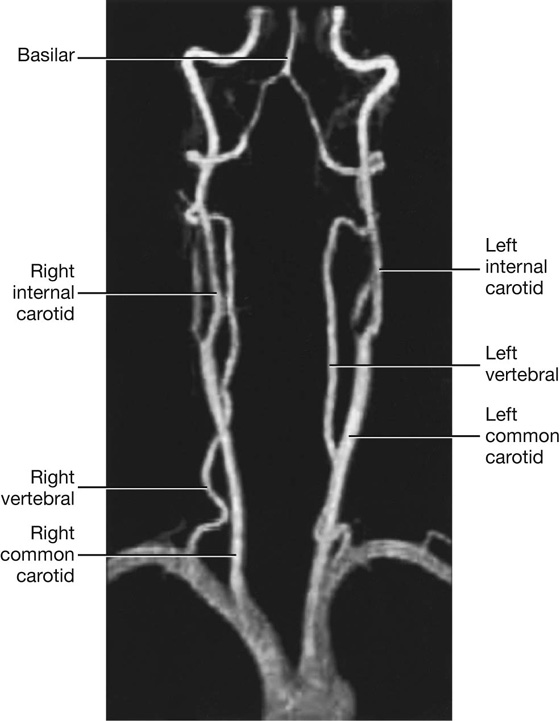
 One branch joins with its companion from the other side to form the single anterior spinal artery, which then descends in the anterior median fissure of the spinal cord.
One branch joins with its companion from the other side to form the single anterior spinal artery, which then descends in the anterior median fissure of the spinal cord. A second branch is the posterior spinal artery, which passes posteriorly around the medulla then descends on the posterior surface of the spinal cord in the area of the attachment of the posterior roots—there are two posterior spinal arteries, one on each side (although the posterior spinal arteries can originate directly from the vertebral arteries, they more commonly branch from the posterior inferior cerebellar arteries).
A second branch is the posterior spinal artery, which passes posteriorly around the medulla then descends on the posterior surface of the spinal cord in the area of the attachment of the posterior roots—there are two posterior spinal arteries, one on each side (although the posterior spinal arteries can originate directly from the vertebral arteries, they more commonly branch from the posterior inferior cerebellar arteries).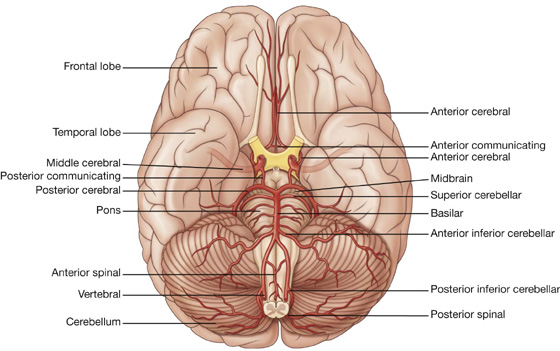
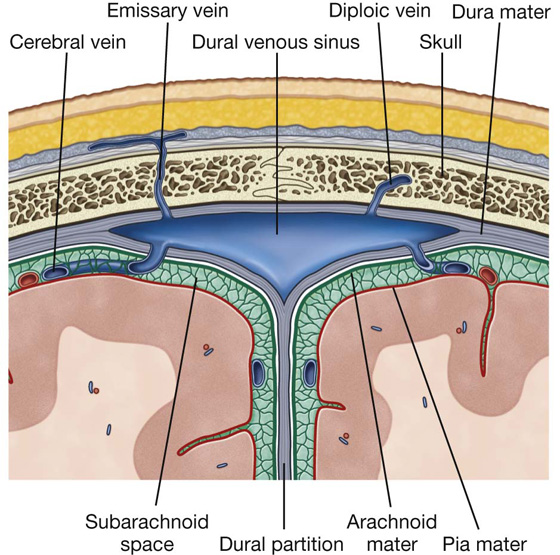
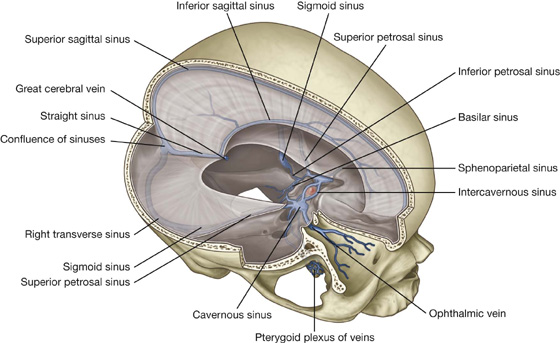
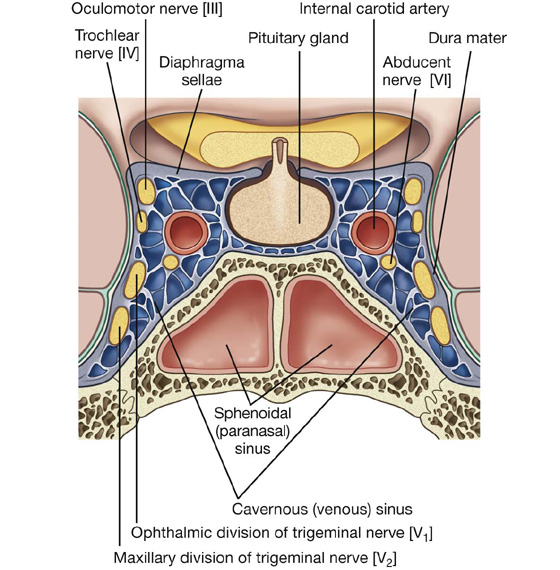
 the abducent nerve [VI].
the abducent nerve [VI]. the oculomotor nerve [III],
the oculomotor nerve [III], the trochlear nerve [IV],
the trochlear nerve [IV], the maxillary nerve [V2].
the maxillary nerve [V2]. The secondary injuries are sequelae of the initial trauma. They include scalp laceration, fracture of the cranial vault, disruption of intracerebral arteries and veins, intracerebral edema, and infection. In most cases these can be treated if diagnosed early, and rapid and effective treatment will significantly improve the patient’s recovery and prognosis.
The secondary injuries are sequelae of the initial trauma. They include scalp laceration, fracture of the cranial vault, disruption of intracerebral arteries and veins, intracerebral edema, and infection. In most cases these can be treated if diagnosed early, and rapid and effective treatment will significantly improve the patient’s recovery and prognosis.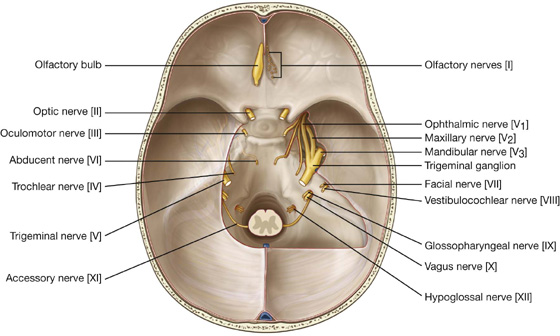
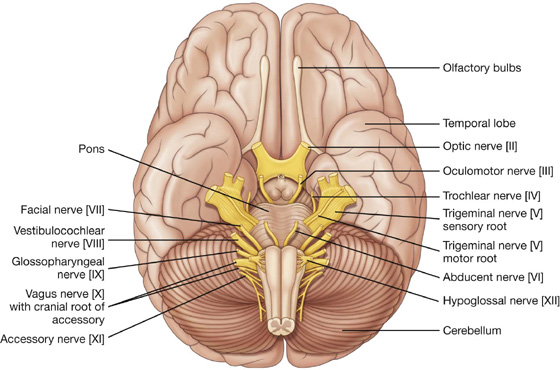
 General visceral efferent (GVE) fibers are part of the parasympathetic part of the autonomic division of the PNS.
General visceral efferent (GVE) fibers are part of the parasympathetic part of the autonomic division of the PNS. The GSA fibers provide sensory input from the face, anterior one-half of the scalp, mucous membranes of the oral and nasal cavities and the paranasal sinuses, the nasopharynx, part of the ear and external acoustic meatus, part of the tympanic membrane, orbital contents and conjunctiva, the dura mater in the anterior and middle cranial fossae, and possibly the mastoid air cells;
The GSA fibers provide sensory input from the face, anterior one-half of the scalp, mucous membranes of the oral and nasal cavities and the paranasal sinuses, the nasopharynx, part of the ear and external acoustic meatus, part of the tympanic membrane, orbital contents and conjunctiva, the dura mater in the anterior and middle cranial fossae, and possibly the mastoid air cells; The BE fibers innervate the muscles of mastication, the tensor tympani, the tensor veli palatini, the mylohyoid, and the anterior belly of the digastric.
The BE fibers innervate the muscles of mastication, the tensor tympani, the tensor veli palatini, the mylohyoid, and the anterior belly of the digastric. The GSA fibers provide sensory input from part of the external acoustic meatus and deeper parts of the auricle.
The GSA fibers provide sensory input from part of the external acoustic meatus and deeper parts of the auricle. The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the lacrimal gland, submandibular and sublingual salivary glands, glands in the mucous membranes of the nasal cavity, and hard and soft palates.
The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the lacrimal gland, submandibular and sublingual salivary glands, glands in the mucous membranes of the nasal cavity, and hard and soft palates. The BE fibers innervate the muscles of the face (muscles of facial expression) and scalp derived from the second pharyngeal arch, and the stapedius, the posterior belly of the digastric, and the stylohyoid muscles.
The BE fibers innervate the muscles of the face (muscles of facial expression) and scalp derived from the second pharyngeal arch, and the stapedius, the posterior belly of the digastric, and the stylohyoid muscles. The intermediate nerve contains the SA fibers for taste, the parasympathetic GVE fibers, and the GSA fibers.
The intermediate nerve contains the SA fibers for taste, the parasympathetic GVE fibers, and the GSA fibers. The GSA fibers provide sensory input from posterior one-third of the tongue, palatine tonsils, oropharynx, and mucosa of the middle ear, mastoid air cells, and pharyngotympanic tube.
The GSA fibers provide sensory input from posterior one-third of the tongue, palatine tonsils, oropharynx, and mucosa of the middle ear, mastoid air cells, and pharyngotympanic tube. The BE fibers innervate the muscle derived from the third pharyngeal arch (the stylopharyngeus muscle).
The BE fibers innervate the muscle derived from the third pharyngeal arch (the stylopharyngeus muscle). The GSA fibers provide sensory input from the larynx, laryngopharynx, deeper parts of the auricle, part of the external acoustic meatus, and the dura mater in the posterior cranial fossa.
The GSA fibers provide sensory input from the larynx, laryngopharynx, deeper parts of the auricle, part of the external acoustic meatus, and the dura mater in the posterior cranial fossa. The GVA fibers provide sensory input from the aortic body chemoreceptors and aortic arch baroreceptors, and the esophagus, bronchi, lungs, heart, and abdominal viscera in the foregut and midgut.
The GVA fibers provide sensory input from the aortic body chemoreceptors and aortic arch baroreceptors, and the esophagus, bronchi, lungs, heart, and abdominal viscera in the foregut and midgut. The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate smooth muscle and glands in the pharynx, larynx, thoracic viscera, and abdominal viscera of the foregut and midgut.
The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate smooth muscle and glands in the pharynx, larynx, thoracic viscera, and abdominal viscera of the foregut and midgut. The BE fibers innervate one muscle of the tongue (palatoglossus), the muscles of the soft palate (except tensor veli palatini), pharynx (except stylopharyngeus), and larynx.
The BE fibers innervate one muscle of the tongue (palatoglossus), the muscles of the soft palate (except tensor veli palatini), pharynx (except stylopharyngeus), and larynx.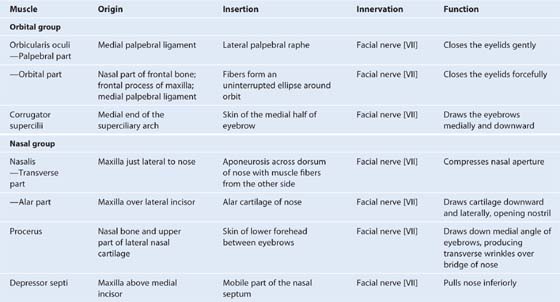
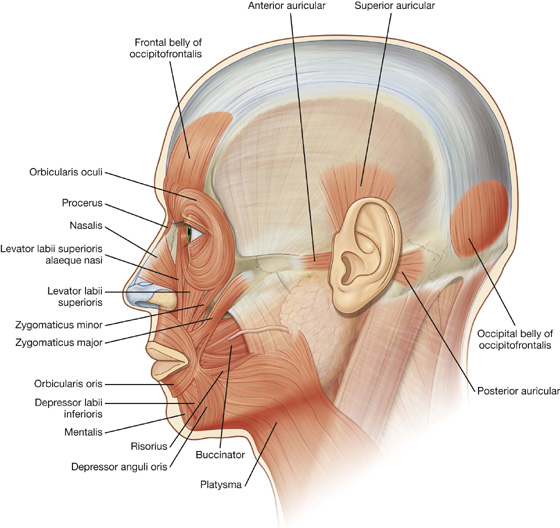
 the outer orbital part; and
the outer orbital part; and the inner palpebral part.
the inner palpebral part.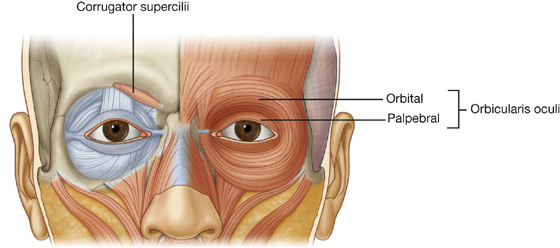
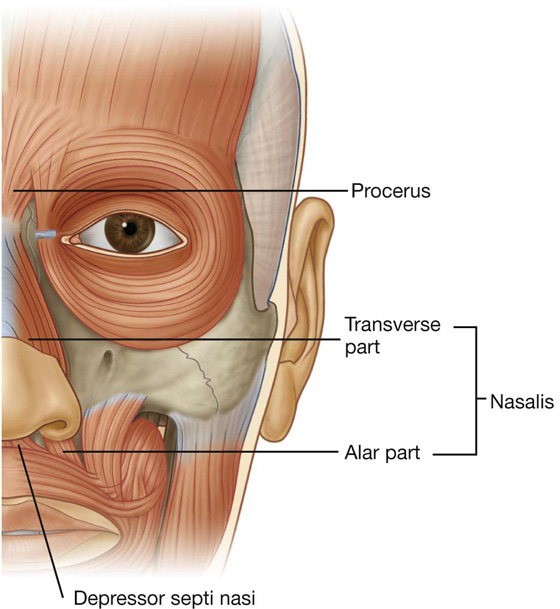
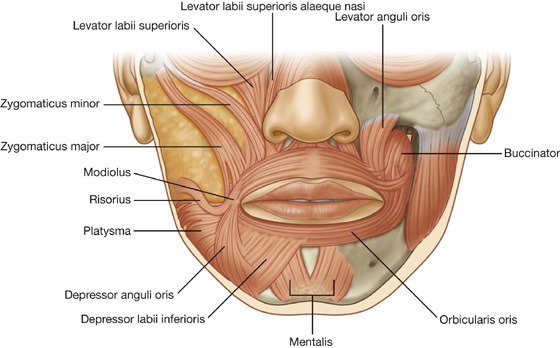
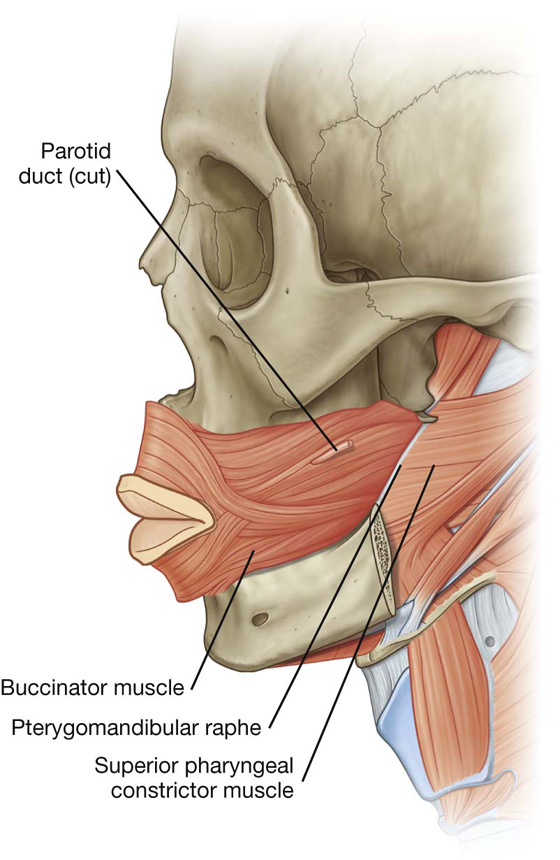
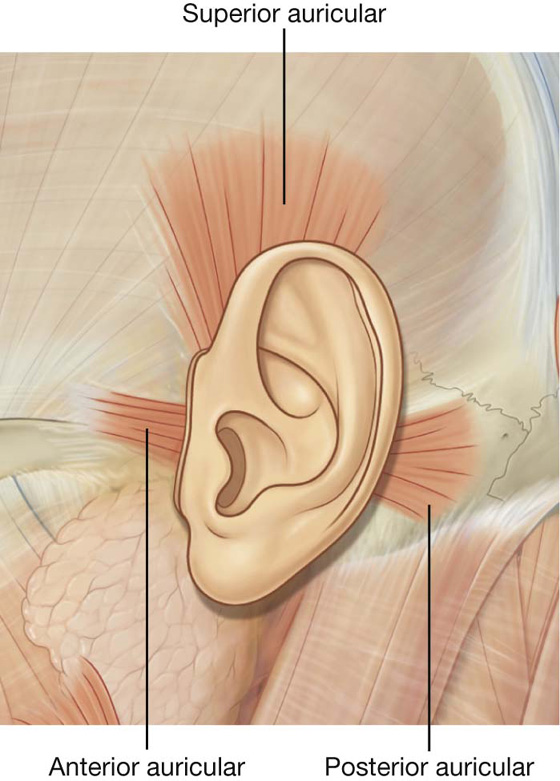
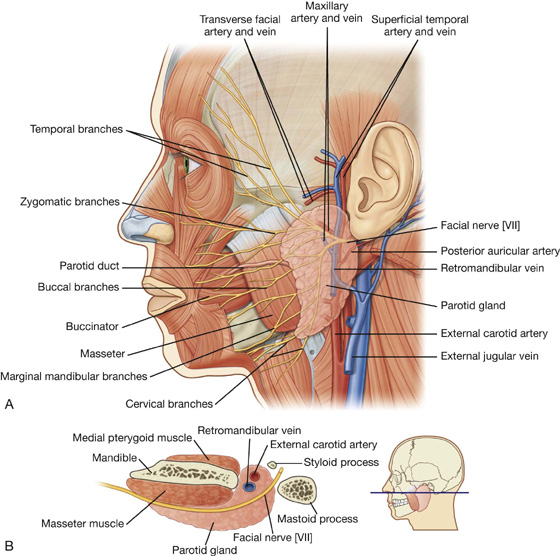
 The superficial temporal artery continues in a superior direction and emerges from the upper border of the gland after giving off the transverse facial artery.
The superficial temporal artery continues in a superior direction and emerges from the upper border of the gland after giving off the transverse facial artery.
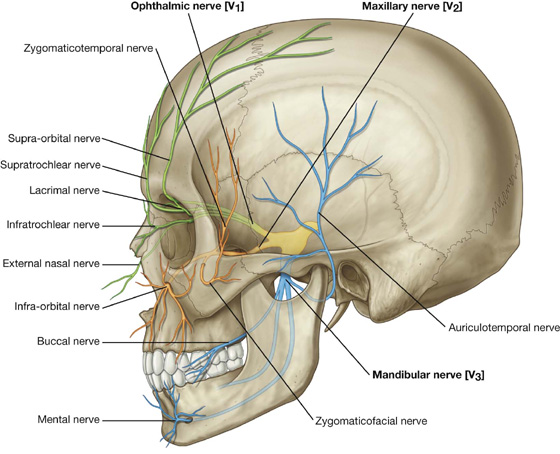
 the supra-orbital and supratrochlear nerves, which leave the orbit superiorly and innervate the upper eyelid, forehead, and scalp;
the supra-orbital and supratrochlear nerves, which leave the orbit superiorly and innervate the upper eyelid, forehead, and scalp; the infratrochlear nerve, which exits the orbit in the medial angle to innervate the medial half of the upper eyelid, the skin in the area of the medial angle, and the side of the nose;
the infratrochlear nerve, which exits the orbit in the medial angle to innervate the medial half of the upper eyelid, the skin in the area of the medial angle, and the side of the nose; the lacrimal nerve, which exits the orbit in the lateral angle to innervate the lateral half of the upper eyelid and the skin in the area of the lateral angle; and
the lacrimal nerve, which exits the orbit in the lateral angle to innervate the lateral half of the upper eyelid and the skin in the area of the lateral angle; and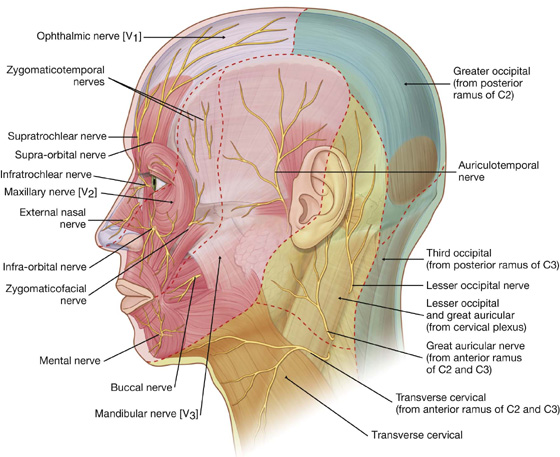
 a small zygomaticotemporal branch, which exits the zygomatic bone and supplies a small area of the anterior temple above the zygomatic arch;
a small zygomaticotemporal branch, which exits the zygomatic bone and supplies a small area of the anterior temple above the zygomatic arch; a small zygomaticofacial branch, which exits the zygomatic bone and supplies a small area of skin over the zygomatic bone; and
a small zygomaticofacial branch, which exits the zygomatic bone and supplies a small area of skin over the zygomatic bone; and the auriculotemporal nerve, which enters the face just posterior to the temporomandibular joint, passes through the parotid gland, and ascends just anterior to the ear to supply the external acoustic meatus, the surface of the tympanic membrane (eardrum), and a large area of the temple;
the auriculotemporal nerve, which enters the face just posterior to the temporomandibular joint, passes through the parotid gland, and ascends just anterior to the ear to supply the external acoustic meatus, the surface of the tympanic membrane (eardrum), and a large area of the temple; the mental nerve, which exits the mandible through the mental foramen and immediately divides into multiple branches to supply the skin and mucous membrane of the lower lip and skin of the chin.
the mental nerve, which exits the mandible through the mental foramen and immediately divides into multiple branches to supply the skin and mucous membrane of the lower lip and skin of the chin.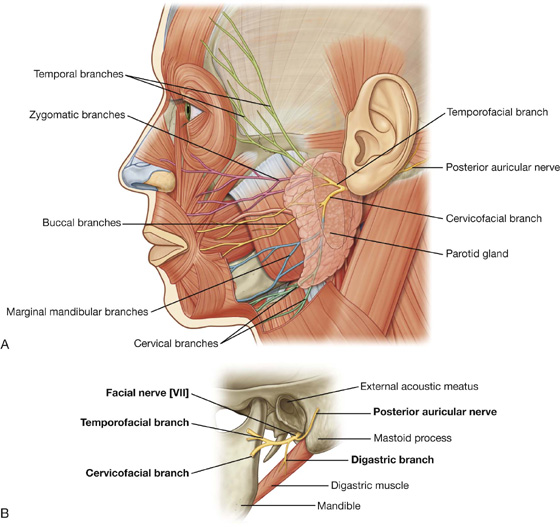
 Temporal branches exit from the superior border of the parotid gland to supply muscles in the area of the temple, forehead, and supra-orbital area.
Temporal branches exit from the superior border of the parotid gland to supply muscles in the area of the temple, forehead, and supra-orbital area. Zygomatic branches emerge from the anterosuperior border of the parotid gland to supply muscles in the infra-orbital area, the lateral nasal area, and the upper lip.
Zygomatic branches emerge from the anterosuperior border of the parotid gland to supply muscles in the infra-orbital area, the lateral nasal area, and the upper lip. Marginal mandibular branches emerge from the anteroinferior border of the parotid gland to supply muscles of the lower lip and chin.
Marginal mandibular branches emerge from the anteroinferior border of the parotid gland to supply muscles of the lower lip and chin.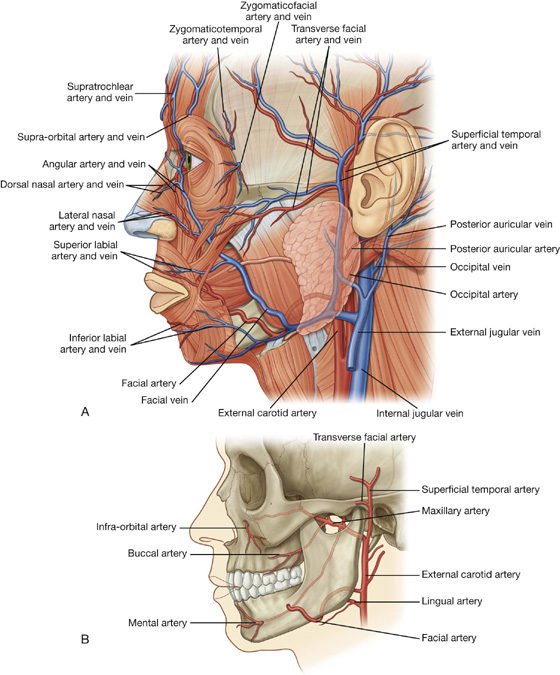
 The infra-orbital artery enters the face through the infra-orbital foramen and supplies the lower eyelid, upper lip, and the area between these structures.
The infra-orbital artery enters the face through the infra-orbital foramen and supplies the lower eyelid, upper lip, and the area between these structures. The buccal artery enters the face on the superficial surface of the buccinator muscle and supplies structures in this area.
The buccal artery enters the face on the superficial surface of the buccinator muscle and supplies structures in this area.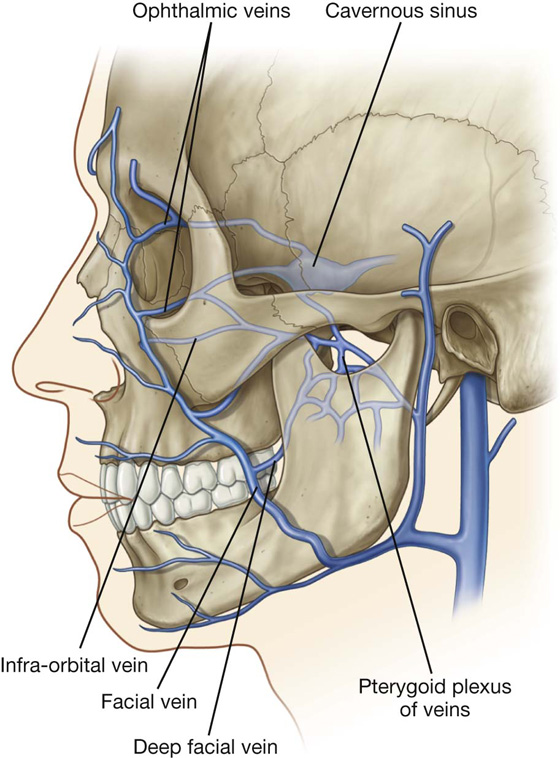
 It communicates with veins passing into deeper regions of the face (i.e., the deep facial vein connecting with the pterygoid plexus of veins).
It communicates with veins passing into deeper regions of the face (i.e., the deep facial vein connecting with the pterygoid plexus of veins). submental nodes inferior and posterior to the chin, which drain lymphatics from the medial part of the lower lip and chin bilaterally;
submental nodes inferior and posterior to the chin, which drain lymphatics from the medial part of the lower lip and chin bilaterally; submandibular nodes superficial to the submandibular gland and inferior to the body of the mandible, which drain the lymphatics from the medial corner of the orbit, most of the external nose, medial part of the cheek, the upper lip and the lateral part of the lower lip that follow the course of the facial artery;
submandibular nodes superficial to the submandibular gland and inferior to the body of the mandible, which drain the lymphatics from the medial corner of the orbit, most of the external nose, medial part of the cheek, the upper lip and the lateral part of the lower lip that follow the course of the facial artery; pre-auricular and parotid nodes anterior to the ear, which drain lymphatics from most of the eyelids, a part of the external nose, and the lateral part of the cheek.
pre-auricular and parotid nodes anterior to the ear, which drain lymphatics from most of the eyelids, a part of the external nose, and the lateral part of the cheek.