Chapter 11. Head and Neck
Rationale
Examination of the head and neck is important in screening pediatric clients for acute disorders and long-term disabilities. The determination of disorders such as skull asymmetry can also signal the need for parent teaching.
Anatomy and Physiology
The head accounts for one fourth of the body length and one third of the body weight in the newborn infant, in comparison with one eighth of the body length and one tenth of the body weight in the adult. Head size, which is 32 to 38 cm (12.6 to 14.9 inches) at birth, normally exceeds chest circumference by 1 to 2 cm (0.4 to 0.8 inches) until 18 months of age. After 18 months, chest growth exceeds head size by 5 to 7 cm (2 to 2.76 inches) (see Appendix B for charts of head circumference norms). The newborn skull consists of separate bones that fuse when brain growth is complete. Soft, fibrous tissue joints, called sutures, separate the bones (Figure 11-1). Sutures begin to unite by 6 months of age but can be separated by increased intracranial pressure until 12 years of age.
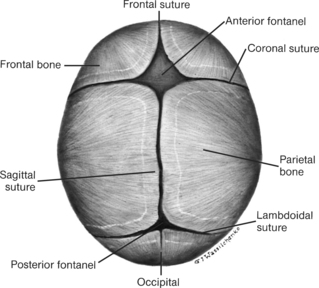 |
| Figure 11-1Location of sutures and fontanels.(From Hockenberry MJ et al: Wong’s nursing care of infants and children, ed 7, St Louis, 2003, Mosby.)Elsevier Inc. |
Fontanels are formed by the juncture of three or more skull bones (see Figure 11-1) and are felt as soft concavities. Although there are several fontanels (sagittal or parietal, sphenoidal, mastoid, anterior, and posterior), normally only the posterior and anterior fontanels can be palpated. The sagittal fontanel, located between the anterior and posterior fontanels and along the sagittal suture, can be palpated in some neonates and in some infants with Down syndrome. The posterior fontanel might be closed at birth and should always be closed by the second month. The anterior fontanel closes between 9 and 26 months of age; 90% close between 7 and 19 months.
By 4 months of age the infant should be able to hold the head erect and in midline. By 6 months no significant head lag should be noted when the child is pulled to a sitting position.
The neck in the infant and toddler is short, but by 4 years of age it assumes adult proportions. Although the thyroid gland is fully active at birth, it might not be palpable in infants and young children.
▪ Paper or narrow flexible metal tape (not cloth tape, which can stretch)
| Measurement | Findings | ||
|---|---|---|---|
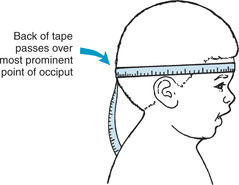
| Measure head circumference if the child is 2 years of age or younger, if the size of the child’s head warrants concern, or if there is possible concern about neurologic or developmental health issues. Place the tape around the head at points just above the eyebrows and the pinna and around the occipital prominence (Figure 11-2). If head circumference is measured daily, the head should be marked at key points to ensure consistency of measurement. Head circumference should be plotted on gender-specific charts. If the infant is premature, then the age of the infant should be corrected for prematurity and the head circumference plotted by conceptual rather than chronologic age. |
Head circumference provides an estimate of cranial volume, which reflects brain size and correlates with neurologic and developmental functions. The head can appear disproportionately large (but normal) in infants born prematurely or in children whose familial pattern exhibits large heads.
Clinical Alert
If an infant’s head circumference is above or below growth norms for the infant’s established percentile, further evaluation is indicated. An abnormally large head circumference can indicate hydrocephalus, brain tumor, cerebral gigantism, neurofibromatosis, hemorrhage, or autism. A small head circumference can indicate craniostenosis or microcephaly. Infants born to mothers who use cocaine or alcohol or who experienced intrauterine infection can have smaller head circumferences.
|
Preparation
Sit or lay the child in a comfortable position. The infant or young child might be most at ease on the parent’s lap.
Assessment of Head
| Assessment | Findings |
|---|---|
| Observe the shape and symmetry of the child’s head from different angles. If possible, also note the shape and symmetry of the parents’heads. Part the hair of the child and inspect for lesions or masses. |
Minor asymmetry in infants younger than 4 months is common and is related to molding. A head might be longer, narrower, or flatter than expected, as a result of genetic influences.
Clinical Alert
A markedly flattened occiput can be the result of persistent placement of the child in the supine position. If flattening is observed, ask the parents about the child’s preferred sleep or play position.
Parent teaching might be indicated. A flattened occiput and a small, rounded head are found with Down syndrome.
Head asymmetry can reflect premature closure of suture lines and requires further evaluation.
|
| Assessment | Findings |
|---|---|
| Palpate the skull, using the fingerpads. Palpate the suture lines in infants. |
Sutures are felt as prominent ridges or like cracks between the cranial bones. In a newborn infant the suture lines override as a result of molding, but usually flatten by 6 months.
Palpation of the suture lines can occasionally lead to slight give in the underlying bone due to osteoporosis of the outer table of bone. This is known as craniotabes. Craniotabes is sometimes found in normal infants.
Clinical Alert
A separated sagittal suture is one of the most common findings in Down syndrome.
Craniotabes can suggest increased intracranial pressure as in hydrocephaly, infection as in syphilis, and metabolic disturbances such as rickets.
A localized, easily moveable accumulation of blood in subcutaneous tissue is indicative of a hematoma, which can result from trauma to the skull.
Single, round, nontender, moveable masses can indicate sebaceous cysts.
|
| Observe and palpate the fontanels, if open, while the infant is sitting. |
The anterior fontanel should be soft, flat, and pulsatile. The fontanel bulges slightly when the infant is crying.
Clinical Alert
A bulging fontanel can indicate increased intracranial pressure and is found in conditions such as head injury, meningitis, or neoplasm.
A depressed fontanel can indicate dehydration.
An enlarged anterior fontanel or the presence of a sagittal fontanel can indicate Down syndrome.
An enlarged posterior fontanel can suggest congenital hypothyroidism.
|
| Assessment | Findings |
|---|---|
| Measure the width and length of an open anterior fontanel. |
Until 9 to 12 months the anterior fontanel measures from 1 to 5 cm (0.4 to 2 in) in length and width.
Clinical Alert
An abnormally small or large fontanel can suggest a bone growth disorder.
|
| Percuss the parietal bone on each side by tapping the index finger against the surface. |
Percussion produces a “cracked pot” sound (Macewen’s sign) in normal infants before closure of sutures.
Clinical Alert
Presence of Macewen’s sign in older infants and children can indicate separation of sutures because of increased intracranial pressure as a result of conditions such as lead encephalopathy and brain tumor.
|
Assessment of Neck
| Assessment | Findings |
|---|---|
| Pull the infant to a sitting position while observing head control. |
The infant younger than 4 months might show some head lag when pulled to a sitting position.
Clinical Alert
Significant head lag after 6 months can indicate cerebral palsy.
|
| Put the child’s head and neck through a full range of motion. The older child should be asked to look up, down, and sideways. |
The child should exhibit no pain or limitation of movement in any direction.
Clinical Alert
Pain and resistance to flexion can indicate meningeal irritation.
|
| Assessment | Findings |
|---|---|
| Inspect the neck for lymph nodes, masses, cysts, webbing, extra folds of skin, and vein distention. |
Clinical Alert
Webbing and extra neck folds can indicate Turner’s syndrome.
Excessive and lax skin is found in children with Down syndrome.
Small, round, firm swelling felt at midline just above the thyroid cartilage in a young infant suggests a thyroglossal duct cyst.
Cervical lymphadenopathy can suggest viral or bacterial infections. General lymphadenopathy is associated with HIV infection in infants and with infectious mononucleosis in older children and adolescents. Bilateral tonsillar lymph node enlargement can indicate acute tonsillitis.
Parotid swelling and tenderness can indicate mumps, bacterial infection, or presence of a stone.
Enlarged occipital nodes can indicate rubella or roseola infantum.
Vein distention might be present with labored respirations.
|
| Palpate the trachea by placing the thumb on one of the trachea and the index finger on the other. Slide the fingers up and down while the child’s neck is slightly hyperextended. |
The trachea should be at midline or slightly to the right.
Clinical Alert
Any shift in the position of the trachea should be noted because serious lung problems might be present.
|
| Palpate the thyroid gland by standing behind the child and placing your fingers or hands gently over the area of the gland (at the base the neck). The gland rises as a mass as the child swallows. Palpation of the thyroid gland in the infant and young child is difficult because of the shortness of the neck. Infants are best examined while lying supine across a parent’s lap. |
In normal children the thyroid gland might not be felt.
Clinical Alert
An enlarged thyroid gland can indicate goiter, lymphatic thyroiditis.
|
Pain: related to physical factors.
Anxiety: related to uncertainty of diagnoses, possibility of disability.
Risk for trauma: related to balancing difficulties, cognitive difficulties, reduced coordination.
Altered tissue perfusion: related to mechanical reduction in blood flow, interruption in arterial or venous flow.
Altered health maintenance: related to perceptual or cognitive impairment.
Impaired verbal communication: related to decrease in circulation to brain, anatomic defect.
Altered family processes: related to situation transition and/or crisis, developmental crisis.
Risk for altered parenting: related to handicapping condition, developmental delay.
Risk for altered growth and development: related to effects of physical disabilities.
Hyperthermia: related to illness, trauma, increased metabolic rate.
Hypothermia: related to illness, decreased metabolic rate.
Altered comfort: pain secondary to infection, meningeal irritation.
Compromised family coping: related to situational crisis.
Fear: related to rapid onset of illness.
Hyperthermia: related to altered metabolic rates secondary to altered thyroid function.
Hypothermia: related to altered metabolic rates secondary to altered thyroid function.
Self-care deficit: related to inability or interruption in performing age-appropriate activities of daily living.
Impaired swallowing: secondary to enlarged thyroid gland, altered level of consciousness, infection, alcohol exposure.