Hand, Upper Extremity, and Microvascular Surgery
III. Carpal Fractures and Instability
IV. Metacarpal and Phalangeal Injuries
V. Tendon Injuries and Overuse Syndromes
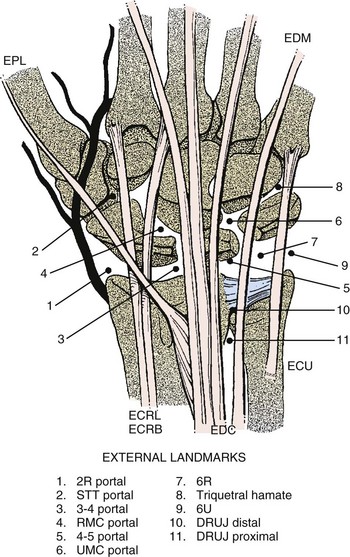
VI. Distal Radioulnar Joint, Triangular Fibrocartilage Complex, and Wrist Arthroscopy
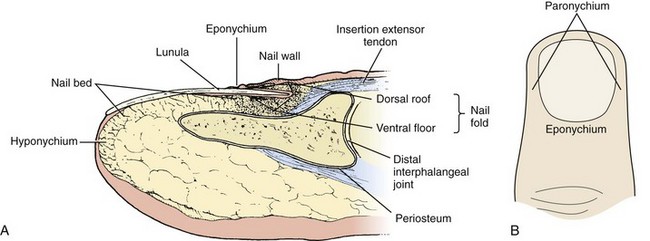
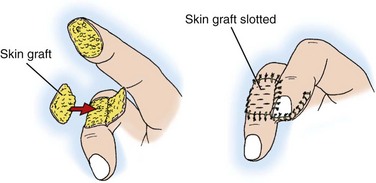
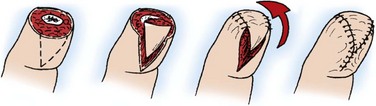
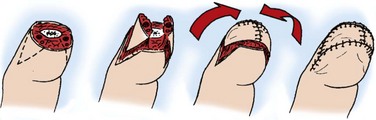
VII. Nail and Fingertip Injuries
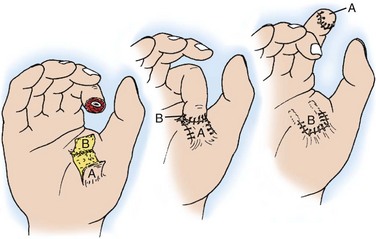
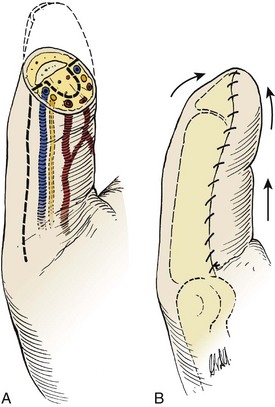
VIII. Soft Tissue Coverage and Microsurgery
XI. Nerve Injuries and Tendon Transfers
XIII. Idiopathic Osteonecrosis of the Carpus
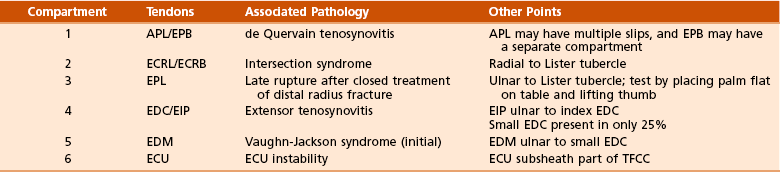
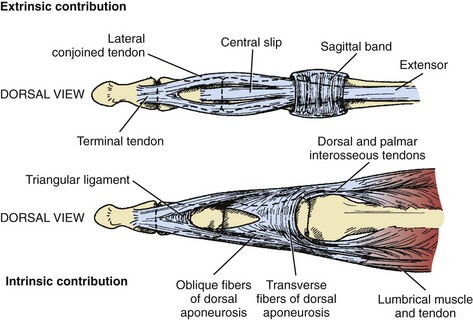
1. Extensor (dorsal) compartments of the wrist (Figure 7-1 and Table 7-1)
2. Extensor retinaculum—prevents tendon bowstringing at wrist
3. Juncturae tendinum—extensor tendon interconnections in hand that may mask proximal tendon lacerations
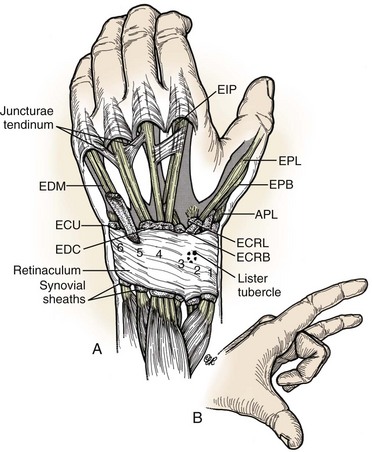
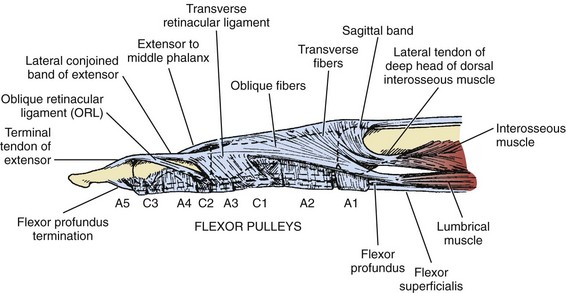
4. Sagittal bands—aid in metacarpophalangeal (MCP) joint extension, centralize the extensor mechanism, and attach to the volar plate (Figure 7-2)
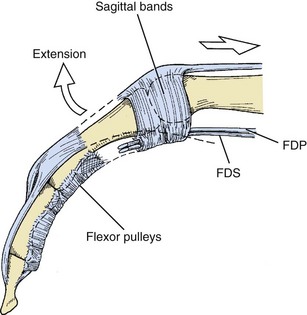
5. Central slip—inserts on base of middle phalanx (P2), aids in proximal interphalangeal (PIP) joint extension (Figure 7-3)
6. Extensor mechanism receives contributions from the intrinsic muscles—interossei and lumbricals (see Figures 7-3 and 7-4)
7. Lateral bands—receive contributions from common extensor and intrinsics, converge to form terminal extensor tendon, which inserts on base of distal phalanx (P3) (see Figures 7-3 and 7-4)
8. Transverse retinacular ligament—prevents dorsal subluxation of lateral bands (see Figure 7-4)
9. Triangular ligament—prevents volar subluxation of lateral bands (see Figure 7-3)
10. Oblique retinacular ligament (ligament of Landsmeer)—helps to link PIP and distal interphalangeal (DIP) joint extension (see Figure 7-4)
11. Grayson/Cleland ligaments—volar and dorsal to digital neurovascular bundles, respectively (Grayson is ground; Cleland is ceiling)
1. Flexor digitorum profundus (FDP)—flexes the DIP joint, aids in PIP and MCP flexion, typically shares common muscle belly in forearm
2. Flexor digitorum superficialis (FDS)—flexes the PIP joint, aids in MCP flexion, individual muscle bellies in forearm
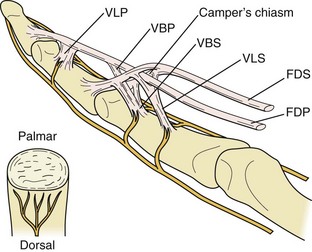
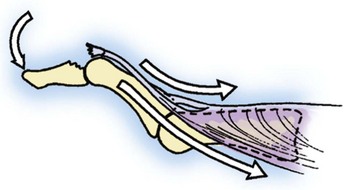
3. FDP tendon splits FDS at the Campers chiasm at level of proximal phalanx (P1) (Figure 7-5).
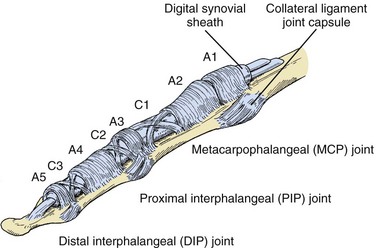
4. Flexor tendon sheath—encompasses tendons distal to MCP joint
5. Vascular supply to flexor tendons is twofold.
6. Each digit has five annular pulleys (A1 to A5) and three cruciate pulleys (C1 to C3).
7. Thumb has two annular pulleys and an oblique pulley in between that prevents bowstringing.
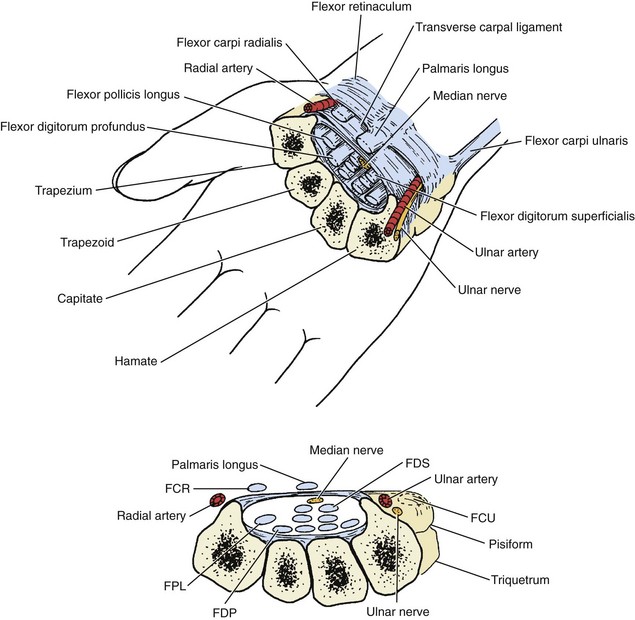
8. Carpal tunnel contains median nerve and nine flexor tendons (one flexor pollicis longus [FPL], four FDS, and four FDP tendons).
 FPL tendon—most radial structure in carpal tunnel
FPL tendon—most radial structure in carpal tunnel
 Long and ring FDS tendons are volar to index and small FDS (Figure 7-7).
Long and ring FDS tendons are volar to index and small FDS (Figure 7-7).
9. The Guyon canal (ulnar tunnel)—contains the ulnar nerve and artery
10. Linburg sign—interconnections between FPL and index FDP in forearm; unilateral in 25% to 30%, bilateral in 5% to 15%
11. Palmaris longus (PL) tendon—present 80% to 85% of the time, common source of autograft for upper extremity reconstructive procedures
12. Flexor carpi radialis (FCR)/flexor carpi ulnaris (FCU)—primary wrist flexors, insert on base of second metacarpal and pisiform, respectively
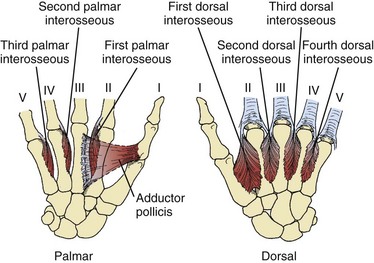
1. Four dorsal interosseous (digit abductors) and three palmar interosseous (digit adductor) muscles
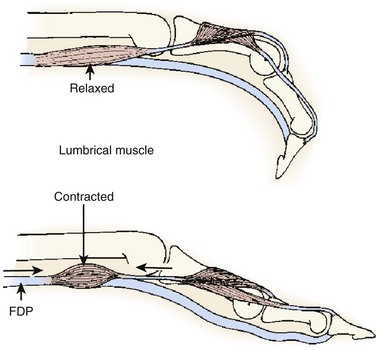
2. Lumbrical muscles originate on radial aspect of FDP tendons and pass volar to transverse metacarpal ligaments to insert on the radial aspect of the extensor hood lateral bands.
 Contribute to interphalangeal joint extension through radial lateral bands, relax extrinsic flexor system (Figure 7-9)
Contribute to interphalangeal joint extension through radial lateral bands, relax extrinsic flexor system (Figure 7-9)
3. Intrinsic tightness—PIP flexion less with MCP joints held in extension (intrinsics on stretch, extrinsics relaxed)
4. Extrinsic tightness—PIP flexion less with MCP joints held in flexion (extrinsics on stretch, intrinsics relaxed)
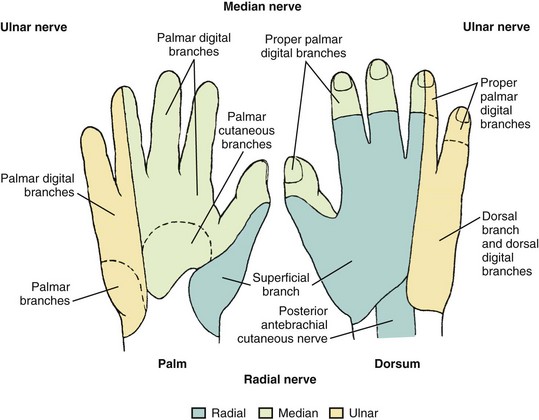
1. Entire hand supplied by branches of median, radial, and ulnar nerves
2. Sensory innervation of hand—Figure 7-10
3. Median nerve—innervates pronator teres, FDS, FCR, PL, radial two lumbricals
 Anterior interosseous branch of median nerve—innervates FPL, index and long FDP (50% of time), pronator quadratus
Anterior interosseous branch of median nerve—innervates FPL, index and long FDP (50% of time), pronator quadratus
 Palmar cutaneous branch of median nerve—usually lies between PL and FCR at distal wrist flexion crease
Palmar cutaneous branch of median nerve—usually lies between PL and FCR at distal wrist flexion crease
 Recurrent motor branch of median nerve—innervates abductor pollicis brevis, opponens pollicis, and superficial head of flexor pollicis brevis
Recurrent motor branch of median nerve—innervates abductor pollicis brevis, opponens pollicis, and superficial head of flexor pollicis brevis
4. Ulnar nerve—innervates FCU, ring/small FDP (50% of time), ulnar two lumbricals
 Deep motor branch of ulnar nerve—innervates hypothenar and interosseous muscles, adductor pollicis, and deep head of flexor pollicis brevis
Deep motor branch of ulnar nerve—innervates hypothenar and interosseous muscles, adductor pollicis, and deep head of flexor pollicis brevis
5. Martin-Gruber anastomoses—crossover variations between median and ulnar nerves, approximately 15% of population
6. Radial nerve proper—innervates lateral portion of brachialis (also musculocutaneous), triceps, anconeus, brachioradialis, extensor carpi radialis longus (ECRL)
 Divides into superficial sensory branch and posterior interosseous nerve (PIN), which innervates remaining extensor muscles
Divides into superficial sensory branch and posterior interosseous nerve (PIN), which innervates remaining extensor muscles
 Extensor carpi radialis brevis (ECRB) has variable innervation.
Extensor carpi radialis brevis (ECRB) has variable innervation.
 Terminal branch of PIN—lies at floor of fourth extensor compartment
Terminal branch of PIN—lies at floor of fourth extensor compartment
7. Proper digital nerves lie volar to proper digital arteries.
8. Vascular anatomy is covered in the section Vascular Disorders.
1. Most common fracture of the upper extremity (>300,000 per year in United States)
2. High-energy trauma in young
3. Low-energy falls in elderly persons with osteoporotic bone
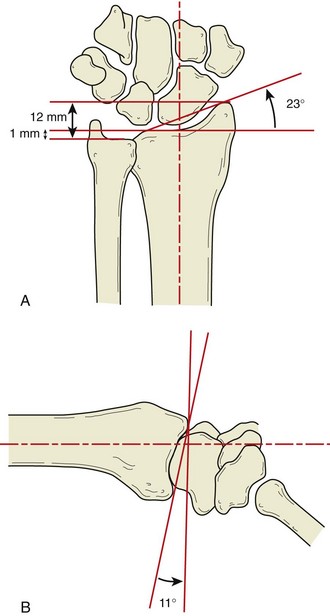
1. Distal radius articular surface—biconcave, scaphoid and lunate facets
2. Distal radioulnar joint (DRUJ)—articulation with ulna at sigmoid notch
3. Lister tubercle—small dorsal prominence, landmark for dorsal approach to wrist
4. Metaphysis—thin cortex, vulnerable to bending forces
1. Pain, swelling, and deformity at the wrist after trauma
2. Open injuries more common in young patients
3. Examine for concurrent anatomic snuffbox and ulnar-sided tenderness.
4. Evaluate the shoulder and elbow.
5. Assess median and ulnar nerve function.
 Acute carpal tunnel syndrome—characterized by progressive, evolving paresthesias and disproportionate pain; requires emergency median nerve decompression (carpal tunnel release)
Acute carpal tunnel syndrome—characterized by progressive, evolving paresthesias and disproportionate pain; requires emergency median nerve decompression (carpal tunnel release)
 Mild, vague, and nonprogressive sensory dysfunction is not indicative of acute carpal tunnel syndrome.
Mild, vague, and nonprogressive sensory dysfunction is not indicative of acute carpal tunnel syndrome.
 Ulnar nerve palsy after high-energy displaced distal radius fractures has also been described.
Ulnar nerve palsy after high-energy displaced distal radius fractures has also been described.
D Radiographic evaluation (posteroanterior, lateral, and oblique views)
5. Volar tilt (lunate fossa inclination)
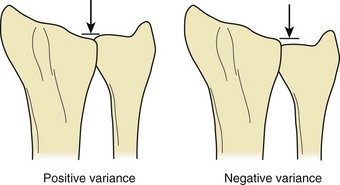
6. Ulnar variance—neutral (normal), positive, or negative
8. Associated fractures—ulnar styloid, distal ulna, carpus
 Isolated fracture of radial styloid (chauffeur’s fracture)—may be associated with scapholunate ligament disruption
Isolated fracture of radial styloid (chauffeur’s fracture)—may be associated with scapholunate ligament disruption
 Radiocarpal dislocation may be purely ligamentous or associated with styloid fractures (radial and/or ulnar).
Radiocarpal dislocation may be purely ligamentous or associated with styloid fractures (radial and/or ulnar).
9. Other imaging studies—computed tomography (CT) for detail of complex intraarticular patterns; magnetic resonance imaging (MRI) for occult fracture, bone contusion, associated soft tissue injury
2. Common eponyms (Colles, Smith, Barton, Hutchinson) predate radiography.
3. Over 10 other schemes exist (e.g., AO, Frykman, Fernandez, Melone, Mayo) but largely fail to help predict treatment or prognosis.
1. General goals—maintain reduction until union, restore function, prevent symptomatic post-traumatic radiocarpal osteoarthrosis
2. Factors considered—age, medical condition, activity demands, bone quality, fracture stability, associated injuries
 Definitive cast immobilization (favored over removable splints) sufficient in minimally displaced low-energy injuries, especially in functionally low-demand patients
Definitive cast immobilization (favored over removable splints) sufficient in minimally displaced low-energy injuries, especially in functionally low-demand patients
 Closed reduction indicated in displaced fractures with abnormal radiographic parameters, especially in functionally high-demand patients
Closed reduction indicated in displaced fractures with abnormal radiographic parameters, especially in functionally high-demand patients
 Dorsal hematoma block with local anesthetic
Dorsal hematoma block with local anesthetic
 Finger traps, upper arm counterweight for ligamentotaxis
Finger traps, upper arm counterweight for ligamentotaxis
 Recreate deformity, manipulate distal fragment.
Recreate deformity, manipulate distal fragment.
 Sugar tong plaster splint with three-point mold
Sugar tong plaster splint with three-point mold
 Keep MCP and interphalangeal joints free for motion.
Keep MCP and interphalangeal joints free for motion.
 Radiographs obtained weekly for first 3 weeks
Radiographs obtained weekly for first 3 weeks
 Loss of reduction correlates with increasing age.
Loss of reduction correlates with increasing age.
 Postreduction benchmarks (American Academy of Orthopaedic Surgeons guideline)
Postreduction benchmarks (American Academy of Orthopaedic Surgeons guideline)
 Immobilization for 6 to 8 weeks (no evidence to support any particular type)
Immobilization for 6 to 8 weeks (no evidence to support any particular type)
 Wrist and digit stiffness, muscle atrophy, and disuse osteopenia may result from prolonged immobilization.
Wrist and digit stiffness, muscle atrophy, and disuse osteopenia may result from prolonged immobilization.
 Closed reduction and percutaneous pinning (CRPP)
Closed reduction and percutaneous pinning (CRPP)
 Open reduction with internal fixation (ORIF)
Open reduction with internal fixation (ORIF)
 Approach between third and fourth extensor compartments
Approach between third and fourth extensor compartments
 Articular reduction directly visualized
Articular reduction directly visualized
 Best for dorsally displaced fractures with dorsal bony defects
Best for dorsally displaced fractures with dorsal bony defects
 Historical disadvantage—extensor tendon irritation/rupture from prominent hardware
Historical disadvantage—extensor tendon irritation/rupture from prominent hardware
 Henry approach between FCR and radial artery or through floor of FCR tendon sheath
Henry approach between FCR and radial artery or through floor of FCR tendon sheath
 Articular reduction not directly visualized, relies on fluoroscopic guidance
Articular reduction not directly visualized, relies on fluoroscopic guidance
 Fixed-angle and variable-angle plates available
Fixed-angle and variable-angle plates available
 Best for Smith and Barton fracture patterns, increasingly used for dorsally displaced injuries
Best for Smith and Barton fracture patterns, increasingly used for dorsally displaced injuries
 Evidence does not support any advantage of early versus delayed motion recovery after surgical fixation of distal radius.
Evidence does not support any advantage of early versus delayed motion recovery after surgical fixation of distal radius.
 Concurrent treatment of ulnar styloid fracture not routinely necessary
Concurrent treatment of ulnar styloid fracture not routinely necessary
 Median nerve dysfunction is the most common complication following a distal radius fracture.
Median nerve dysfunction is the most common complication following a distal radius fracture.
 Extensor pollicis longus (EPL) tendon rupture
Extensor pollicis longus (EPL) tendon rupture
 Most commonly occurs as a late complication following closed treatment because of attritional wear and/or vascular insufficiency near the Lister tubercle
Most commonly occurs as a late complication following closed treatment because of attritional wear and/or vascular insufficiency near the Lister tubercle
 Typically presents as a painless, acute loss of thumb extension
Typically presents as a painless, acute loss of thumb extension
 Treat with PL intercalary autograft or extensor indicis proprius (EIP)-to-EPL tendon transfer.
Treat with PL intercalary autograft or extensor indicis proprius (EIP)-to-EPL tendon transfer.
 Asymptomatic malunion in a functionally low-demand patient does not require treatment.
Asymptomatic malunion in a functionally low-demand patient does not require treatment.
 Low-demand patients with pain from ulnocarpal impaction may benefit from a distal ulna resection (Darrach procedure).
Low-demand patients with pain from ulnocarpal impaction may benefit from a distal ulna resection (Darrach procedure).
 A corrective radius osteotomy with ORIF and bone grafting may be indicated for high-demand patients.
A corrective radius osteotomy with ORIF and bone grafting may be indicated for high-demand patients.
 Presence of radiocarpal osteoarthrosis following intraarticular distal radius fracture with residual step-off is prevalent but does not necessarily correlate with patient-reported symptoms.
Presence of radiocarpal osteoarthrosis following intraarticular distal radius fracture with residual step-off is prevalent but does not necessarily correlate with patient-reported symptoms.
 Multiple case reports of flexor tendon ruptures after volar plating
Multiple case reports of flexor tendon ruptures after volar plating
 FPL is the most common rupture after volar locking plating.
FPL is the most common rupture after volar locking plating.
 EPL is the most common extensor tendon injured, potentially due to drill-bit penetration or prominent screws.
EPL is the most common extensor tendon injured, potentially due to drill-bit penetration or prominent screws.
 Vitamin C in doses of at least 500 mg/day may decrease the incidence of complex regional pain syndrome (disproportionate pain).
Vitamin C in doses of at least 500 mg/day may decrease the incidence of complex regional pain syndrome (disproportionate pain).
III CARPAL FRACTURES AND INSTABILITY
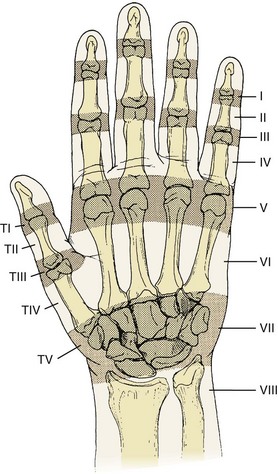
1. Eight carpal bones aligned in two rows
2. Proximal row—scaphoid, lunate, and triquetrum
3. Distal row—trapezium, trapezoid, capitate, and hamate
4. Pisiform is sesamoid within the FCU tendon.
5. Dart-thrower’s motion is combined wrist extension–radial deviation to wrist flexion–ulnar deviation.
6. Carpus has a rich vascular supply with multiple anastomoses.
7. Scaphoid, lunate, and capitate may each have large area supplied by a single interosseous vessel.
8. Some evidence suggests a proprioceptive role for the terminal branch of the posterior interosseous nerve, which may be compromised when this branch is sacrificed during dorsal approaches to the wrist.
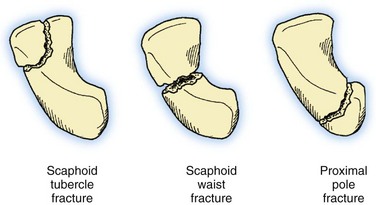
1. Most common carpal fracture (Table 7-2), accounting for up to 15% of all acute wrist injuries
Table 7-2
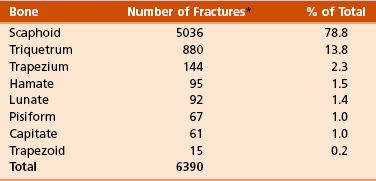
*The number of fractures represents a total of 6390 fractures compiled from three referenced studies to accumulate incidence of carpal bone fractures.
From Green DP, et al, editors: Green’s operative hand surgery, ed 5, Philadelphia, 2005, Churchill Livingstone, p 711.
 Approximately 75% covered by articular cartilage
Approximately 75% covered by articular cartilage
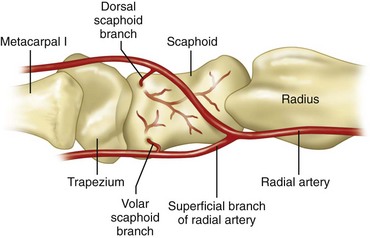
 Main blood supply comes from a dorsal branch of the radial artery, enters at dorsal ridge just distal to waist, and flows in retrograde fashion toward proximal pole.
Main blood supply comes from a dorsal branch of the radial artery, enters at dorsal ridge just distal to waist, and flows in retrograde fashion toward proximal pole.
 Additional branches off superficial volar branch of radial artery enter at distal tubercle and perfuse distal one third.
Additional branches off superficial volar branch of radial artery enter at distal tubercle and perfuse distal one third.
 Tenuous vascular anatomy renders waist and proximal pole fractures at risk for nonunion and post-traumatic osteonecrosis (Figure 7-13).
Tenuous vascular anatomy renders waist and proximal pole fractures at risk for nonunion and post-traumatic osteonecrosis (Figure 7-13).
 Suspect when chief complaint is radial-sided wrist pain after injury or trauma
Suspect when chief complaint is radial-sided wrist pain after injury or trauma
 Most common mechanism is forced hyperextension and radial deviation of the wrist.
Most common mechanism is forced hyperextension and radial deviation of the wrist.
 This results in force transmission through the radioscaphoid articulation and concentration at the scaphoid.
This results in force transmission through the radioscaphoid articulation and concentration at the scaphoid.
 Swelling, anatomic snuffbox/volar tubercle tenderness, limited wrist motion
Swelling, anatomic snuffbox/volar tubercle tenderness, limited wrist motion
 Posteroanterior, lateral, oblique, and scaphoid radiographic views
Posteroanterior, lateral, oblique, and scaphoid radiographic views
 Scaphoid view—approximately 30 degrees of wrist extension and approximately 20 degrees of ulnar deviation
Scaphoid view—approximately 30 degrees of wrist extension and approximately 20 degrees of ulnar deviation
 Radiographs initially nondiagnostic in more than 30% of cases
Radiographs initially nondiagnostic in more than 30% of cases
 With negative radiographs and high clinical suspicion, thumb spica splint immobilization and repeat examination and radiographs in 2 weeks
With negative radiographs and high clinical suspicion, thumb spica splint immobilization and repeat examination and radiographs in 2 weeks
 Bone scan, ultrasonography, CT, and MRI have all been used for earlier diagnosis.
Bone scan, ultrasonography, CT, and MRI have all been used for earlier diagnosis.
 MRI has highest sensitivity, specificity, and accuracy (all >95%) with high positive and negative predictive values.
MRI has highest sensitivity, specificity, and accuracy (all >95%) with high positive and negative predictive values.
 CT has lower predictive values.
CT has lower predictive values.
 Bone scan and ultrasonography lowest specificity and positive predictive value
Bone scan and ultrasonography lowest specificity and positive predictive value
 All of these are better for ruling out rather than ruling in a scaphoid fracture.
All of these are better for ruling out rather than ruling in a scaphoid fracture.
 Neglect of injury for 4 weeks increases nonunion rate from approximately 5% to 45%.
Neglect of injury for 4 weeks increases nonunion rate from approximately 5% to 45%.
 Cast immobilization for nondisplaced fractures
Cast immobilization for nondisplaced fractures
 There is no evidence to suggest that the type of cast affects outcome (e.g., long-arm versus short-arm, standard versus additional thumb spica component).
There is no evidence to suggest that the type of cast affects outcome (e.g., long-arm versus short-arm, standard versus additional thumb spica component).
 Expected time to union increases and overall union rate decreases as the fracture becomes more proximal.
Expected time to union increases and overall union rate decreases as the fracture becomes more proximal.
 Consequently, length of cast immobilization should be greater for more proximal fractures.
Consequently, length of cast immobilization should be greater for more proximal fractures.
 Indications include greater than 1 mm displacement, intrascaphoid angle greater than 35 degrees (humpback deformity), and trans-scaphoid perilunate dislocation.
Indications include greater than 1 mm displacement, intrascaphoid angle greater than 35 degrees (humpback deformity), and trans-scaphoid perilunate dislocation.
 Proximal pole fracture is also a relative indication
Proximal pole fracture is also a relative indication
 Minimally displaced fractures may be treated with percutaneous internal fixation.
Minimally displaced fractures may be treated with percutaneous internal fixation.
 Commonly performed via a dorsal approach
Commonly performed via a dorsal approach
 Direct visualization of the screw via a limited incision is recommended to ensure seating of the screw in subchondral bone.
Direct visualization of the screw via a limited incision is recommended to ensure seating of the screw in subchondral bone.
 Formal ORIF with headless compression screw for displaced injuries
Formal ORIF with headless compression screw for displaced injuries
 Approach dictated by fracture location and surgeon preference
Approach dictated by fracture location and surgeon preference
 Volar approach potentially avoids disruption to the blood supply of the scaphoid and is the most commonly employed approach.
Volar approach potentially avoids disruption to the blood supply of the scaphoid and is the most commonly employed approach.
 Union rates of over 90% to 95% expected
Union rates of over 90% to 95% expected
 Aggressive physical therapy typically delayed until radiographic union achieved
Aggressive physical therapy typically delayed until radiographic union achieved
 Include nonunion, malunion, osteonecrosis, and post-traumatic osteoarthrosis
Include nonunion, malunion, osteonecrosis, and post-traumatic osteoarthrosis
 Symptomatic, early-stage scaphoid nonunion may be treated with ORIF and bone grafting.
Symptomatic, early-stage scaphoid nonunion may be treated with ORIF and bone grafting.
 Inlay (Russe) technique best used in cases with minimal deformity and vascularized proximal pole
Inlay (Russe) technique best used in cases with minimal deformity and vascularized proximal pole
 Scaphoid nonunion with accompanying humpback deformity requires open-wedge interposition (Fisk) graft to restore scaphoid length and angulation.
Scaphoid nonunion with accompanying humpback deformity requires open-wedge interposition (Fisk) graft to restore scaphoid length and angulation.
 Grafts obtained from distal radius or iliac crest
Grafts obtained from distal radius or iliac crest
 Most surgeons typically use supplemental headless compression screw in nonunion cases.
Most surgeons typically use supplemental headless compression screw in nonunion cases.
 Presence of intraoperative punctate bleeding is most reliable sign of vascular proximal pole.
Presence of intraoperative punctate bleeding is most reliable sign of vascular proximal pole.
 Vascularized bone grafting has gained popularity in nonunions with avascular proximal pole.
Vascularized bone grafting has gained popularity in nonunions with avascular proximal pole.
 Most commonly harvested from dorsal aspect of distal radius, based on 1,2 intercompartmental supraretinacular artery (1,2 ICSRA)
Most commonly harvested from dorsal aspect of distal radius, based on 1,2 intercompartmental supraretinacular artery (1,2 ICSRA)
 Untreated, chronic scaphoid nonunion may lead to characteristic progression of post-traumatic osteoarthrosis called scaphoid nonunion advanced collapse (SNAC) wrist.
Untreated, chronic scaphoid nonunion may lead to characteristic progression of post-traumatic osteoarthrosis called scaphoid nonunion advanced collapse (SNAC) wrist.
 Distal portion flexes, while proximal pole is tethered by intact scapholunate ligament and follows lunate into extension. This produces the humpback deformity.
Distal portion flexes, while proximal pole is tethered by intact scapholunate ligament and follows lunate into extension. This produces the humpback deformity.
 Options for treatment of SNAC wrist include radial styloidectomy, proximal row carpectomy, scaphoid excision and four-corner (bone) fusion, and total wrist fusion, depending on stage of presentation and surgeon preference.
Options for treatment of SNAC wrist include radial styloidectomy, proximal row carpectomy, scaphoid excision and four-corner (bone) fusion, and total wrist fusion, depending on stage of presentation and surgeon preference.
C Other carpal bone fractures—small fraction of wrist injuries (see Table 7-2)
1. Lunate—rarely encountered in isolation
2. Capitate neck—may occur in combination with scaphoid fracture or perilunate dislocation, treated with ORIF or intercarpal fusion
3. Triquetrum—Majority of injuries are dorsal capsular avulsion fractures (wrist sprain) and require only brief period of immobilization.
4. Hook of hamate—often from blunt trauma to palm, frequently associated with certain sports (e.g., golf, baseball, hockey, racquet sports)
 Imaging—carpal tunnel view, CT scan (Figure 7-15)
Imaging—carpal tunnel view, CT scan (Figure 7-15)
 Symptomatic patients who fail trial of cast immobilization are treated with fracture fragment excision.
Symptomatic patients who fail trial of cast immobilization are treated with fracture fragment excision.
 ORIF has been described for larger fracture fragments but has high complication rate and little clinical benefit.
ORIF has been described for larger fracture fragments but has high complication rate and little clinical benefit.
 Flexor tendon rupture may be seen with chronic nonunion.
Flexor tendon rupture may be seen with chronic nonunion.
 Be aware of the bipartite hamate, which may be differentiated from a fracture by smooth cortical surfaces.
Be aware of the bipartite hamate, which may be differentiated from a fracture by smooth cortical surfaces.
1. Disruption of normal kinematics of wrist
2. Characterized by wrist pain, loss of motion, weakness
3. If untreated, may lead to degenerative arthritis and disability
4. Spectrum of injury from occult (predynamic) to dynamic to static
5. Static instability detected on standard radiographs, whereas dynamic instability requires either stress radiographs requires either stress radiographs, cineradiography, or live fluoroscopy
6. Carpal instability dissociative (CID) describes instability between individual carpal bones of single carpal row.
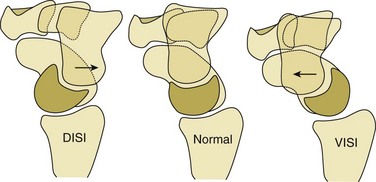
 Examples include classical patterns of dorsal intercalated segmental instability (DISI) and volar intercalated segmental instability (VISI) (Figure 7-16).
Examples include classical patterns of dorsal intercalated segmental instability (DISI) and volar intercalated segmental instability (VISI) (Figure 7-16).
7. Carpal instability nondissociative (CIND) describes instability between carpal rows, such as midcarpal or radiocarpal instability.
8. Carpal instability resulting from malunited distal radius fracture is an example of carpal instability adaptive.
9. Perilunate dislocations combine CID and CIND and are classified as carpal instability complex.
 DISI—most common form of carpal instability
DISI—most common form of carpal instability
 Scapholunate ligament disruption
Scapholunate ligament disruption
 Dorsal fibers are stronger than volar fibers.
Dorsal fibers are stronger than volar fibers.
 Secondary injury to stabilizing dorsal and/or volar extrinsic ligaments, volar scaphoid-trapezo-trapezoid ligaments
Secondary injury to stabilizing dorsal and/or volar extrinsic ligaments, volar scaphoid-trapezo-trapezoid ligaments
 Scaphoid hyperflexion and lunate hyperextension
Scaphoid hyperflexion and lunate hyperextension
 May be traumatic or result from inflammatory or crystalline arthropathy
May be traumatic or result from inflammatory or crystalline arthropathy
 Dorsal wrist pain, often with loading
Dorsal wrist pain, often with loading
 Reproduction of pain/palpable clunk with scaphoid shift test (dorsally directed pressure over volar scaphoid tubercle while wrist brought from ulnar to radial deviation subluxates or dislocates scaphoid over dorsal ridge of distal radius that when released causes scaphoid to reduce with painful clunk) (Figure 7-17)
Reproduction of pain/palpable clunk with scaphoid shift test (dorsally directed pressure over volar scaphoid tubercle while wrist brought from ulnar to radial deviation subluxates or dislocates scaphoid over dorsal ridge of distal radius that when released causes scaphoid to reduce with painful clunk) (Figure 7-17)
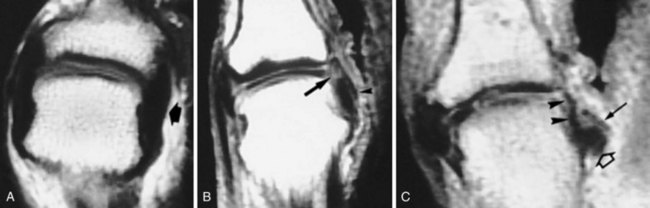
 Standard radiographs may reveal cortical ring sign (Figure 7-18), increased scapholunate angle (>70 degrees), or widened scapholunate interval (>3 mm) in static DISI.
Standard radiographs may reveal cortical ring sign (Figure 7-18), increased scapholunate angle (>70 degrees), or widened scapholunate interval (>3 mm) in static DISI.
 Bilateral clenched-fist (anteroposterior grip) comparison views may reveal a dynamic DISI with relatively widened scapholunate interval on affected side (stress radiographs).
Bilateral clenched-fist (anteroposterior grip) comparison views may reveal a dynamic DISI with relatively widened scapholunate interval on affected side (stress radiographs).
 MRI best, but not perfect, for detection of scapholunate ligament injury (see Figure 7-18)
MRI best, but not perfect, for detection of scapholunate ligament injury (see Figure 7-18)
 Gold standard is wrist arthroscopy.
Gold standard is wrist arthroscopy.
 Geissler classification (Table 7-3)
Geissler classification (Table 7-3)
Table 7-3
Geissler Classification of Arthroscopic Scapholunate Ligament Disruption
| Grade | Description |
| I | Attenuation or hemorrhage of interosseous ligament as seen from radiocarpal space. No incongruity of carpal alignment in midcarpal space. |
| II | Attenuation or hemorrhage of interosseous ligament as seen from radiocarpal space. There may be a slight gap (less than width of probe) between carpal bones in midcarpal space. |
| III | Incongruity or step-off of carpal alignment as seen from both radiocarpal and midcarpal space. Probe may be passed through gap between carpal bones. |
| IV | Incongruity or step-off of carpal alignment as seen from both radiocarpal and midcarpal space. There is gross instability with manipulation. A 2.7-mm arthroscope may be passed through the gap between carpal bones (“drive-through sign”). |
 Treatment depends on stage of instability.
Treatment depends on stage of instability.
 Partial injuries may improve with nonoperative treatment or arthroscopic débridement.
Partial injuries may improve with nonoperative treatment or arthroscopic débridement.
 Acute scapholunate ligament rupture may be amenable to primary repair.
Acute scapholunate ligament rupture may be amenable to primary repair.
 Delayed treatment may require open reduction of scapholunate interval and pinning with or without dorsal capsulodesis.
Delayed treatment may require open reduction of scapholunate interval and pinning with or without dorsal capsulodesis.
 Limited clinical data on reduction-association of scaphoid and lunate (RASL) procedure
Limited clinical data on reduction-association of scaphoid and lunate (RASL) procedure
 Tendon and bone-retinaculum-bone grafts have been attempted for scapholunate reconstruction.
Tendon and bone-retinaculum-bone grafts have been attempted for scapholunate reconstruction.
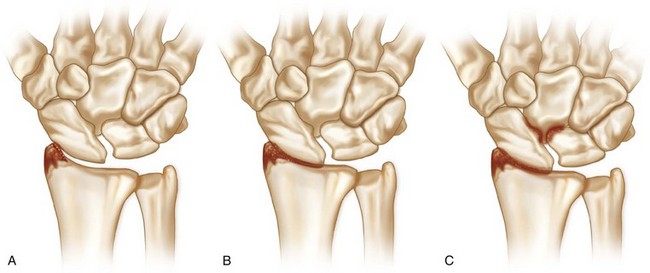
 Cases of chronic, static instability may result in scapholunate advanced collapse (SLAC wrist).
Cases of chronic, static instability may result in scapholunate advanced collapse (SLAC wrist).
 Three stages are described (Figure 7-19).
Three stages are described (Figure 7-19).
 Radioscaphoid and capitolunate joints are affected, radiolunate joint is spared.
Radioscaphoid and capitolunate joints are affected, radiolunate joint is spared.
 Treatment depends on condition of articular surfaces and competency of radioscaphocapitate ligament.
Treatment depends on condition of articular surfaces and competency of radioscaphocapitate ligament.
 Options include radial styloidectomy, proximal row carpectomy, scaphoid excision and four-corner fusion, total wrist fusion.
Options include radial styloidectomy, proximal row carpectomy, scaphoid excision and four-corner fusion, total wrist fusion.
 VISI—second most common form of carpal instability
VISI—second most common form of carpal instability
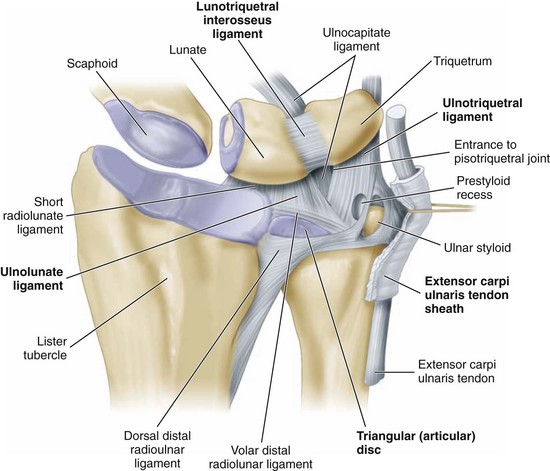
 Disruption of lunotriquetral interosseous ligament
Disruption of lunotriquetral interosseous ligament
 Volar fibers are stronger than dorsal fibers.
Volar fibers are stronger than dorsal fibers.
 Accompanying injury of the dorsal extrinsic ligaments may result in static instability.
Accompanying injury of the dorsal extrinsic ligaments may result in static instability.
 Both the scaphoid and lunate tilt volarly.
Both the scaphoid and lunate tilt volarly.
 Radiographs may show break in Gilula arc on posteroanterior view and decreased scapholunate angle on lateral view.
Radiographs may show break in Gilula arc on posteroanterior view and decreased scapholunate angle on lateral view.
 MRI may show pathology of lunotriquetral ligament.
MRI may show pathology of lunotriquetral ligament.
 Clunking wrist that may or may not be painful
Clunking wrist that may or may not be painful
 Many patient have generalized ligamentous laxity.
Many patient have generalized ligamentous laxity.
 History of trauma often absent
History of trauma often absent
 Sudden shift of proximal carpal row with active radial or ulnar deviation (cineradiographic studies)
Sudden shift of proximal carpal row with active radial or ulnar deviation (cineradiographic studies)
 Radiocarpal dislocation (CIND)
Radiocarpal dislocation (CIND)
 May be associated with intracarpal injury, acute carpal tunnel syndrome, possible compartment syndrome, other major musculoskeletal and/or organ injuries
May be associated with intracarpal injury, acute carpal tunnel syndrome, possible compartment syndrome, other major musculoskeletal and/or organ injuries
 Volar more severe than dorsal dislocation
Volar more severe than dorsal dislocation
 May be purely ligamentous or include radial and/or ulnar styloid fractures
May be purely ligamentous or include radial and/or ulnar styloid fractures
 Ulnar translocation of the carpus signifies global ligamentous disruption.
Ulnar translocation of the carpus signifies global ligamentous disruption.
 Moneim proposed two types based on accompanying intracarpal fracture or interosseous ligament injury
Moneim proposed two types based on accompanying intracarpal fracture or interosseous ligament injury
 Dumontier and Graham stressed the distinction between injuries with small versus large radial styloid fractures.
Dumontier and Graham stressed the distinction between injuries with small versus large radial styloid fractures.
 ORIF of styloid fractures may be enough to restore stability.
ORIF of styloid fractures may be enough to restore stability.
 May also require direct ligamentous repair and/or external fixation to neutralize forces
May also require direct ligamentous repair and/or external fixation to neutralize forces
 Carpal instability adaptive from distal radius malunion
Carpal instability adaptive from distal radius malunion
 Perilunate dislocations (carpal instability complex)
Perilunate dislocations (carpal instability complex)
 Potentially devastating injuries resulting from forced dorsiflexion, ulnar deviation, and supination of wrist
Potentially devastating injuries resulting from forced dorsiflexion, ulnar deviation, and supination of wrist
 Approximately 25% of cases may be missed in the emergency department
Approximately 25% of cases may be missed in the emergency department
 Mayfield described four stages of perilunar disruption of ligamentous constraints, proceeding in counterclockwise direction
Mayfield described four stages of perilunar disruption of ligamentous constraints, proceeding in counterclockwise direction
 Stage I—scapholunate disruption
Stage I—scapholunate disruption
 Stage II—scaphocapitate disruption
Stage II—scaphocapitate disruption
 Stage III—lunotriquetral disruption
Stage III—lunotriquetral disruption
 Stage IV—circumferential disruption
Stage IV—circumferential disruption
 Lesser-arc injuries—purely ligamentous
Lesser-arc injuries—purely ligamentous
 Greater-arc injuries—carpal fracture
Greater-arc injuries—carpal fracture
 May attempt immediate closed reduction, especially in setting of acute carpal tunnel syndrome
May attempt immediate closed reduction, especially in setting of acute carpal tunnel syndrome
 Stable closed reduction may allow for delayed definitive surgical management, but there is no role for closed treatment alone.
Stable closed reduction may allow for delayed definitive surgical management, but there is no role for closed treatment alone.
IV METACARPAL AND PHALANGEAL INJURIES
1. Most frequently encountered injuries of skeletal system
2. Vast majority treated nonoperatively
 Many initially splinted with hand in intrinsic-plus or “safe” position
Many initially splinted with hand in intrinsic-plus or “safe” position
3. Surgical intervention may be indicated in open injuries, intraarticular fractures, irreducible fractures, digit malrotation, and multiple fractures.
4. Digit rotation assessed statically with wrist tenodesis and dynamically as patient initiates making a fist
5. Goals of treatment are stable reduction, edema control, and early range of motion.
 Most commonly occurs in index or middle finger
Most commonly occurs in index or middle finger
 Greater than 1 mm of articular step-off may warrant ORIF.
Greater than 1 mm of articular step-off may warrant ORIF.
 Severe open or comminuted fractures (e.g., gunshot wounds) may be treated with spanning external fixation.
Severe open or comminuted fractures (e.g., gunshot wounds) may be treated with spanning external fixation.
 Most frequently involves the ring and small finger
Most frequently involves the ring and small finger
 “Boxer’s fracture”—metacarpal neck fracture of the small finger
“Boxer’s fracture”—metacarpal neck fracture of the small finger
 Intrinsic muscles are major deforming force leading to apex dorsal angulation.
Intrinsic muscles are major deforming force leading to apex dorsal angulation.
 Check rotation, MCP joint extensor lag.
Check rotation, MCP joint extensor lag.
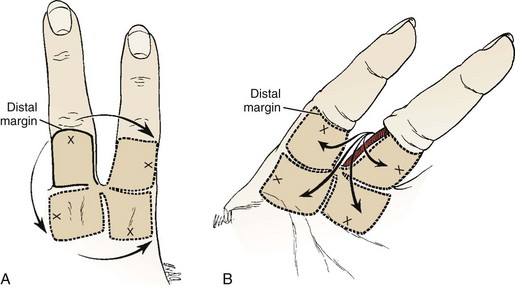
 Many treated with closed reduction (Jahss maneuver) and 3 to 4 weeks of immobilization (Figure 7-21)
Many treated with closed reduction (Jahss maneuver) and 3 to 4 weeks of immobilization (Figure 7-21)
 Suggested acceptable angulation of each metacarpal neck
Suggested acceptable angulation of each metacarpal neck
 Small finger less than 70 degrees (controversial)
Small finger less than 70 degrees (controversial)
 Greater compensation from more mobile fourth and fifth carpometacarpal (CMC) joint
Greater compensation from more mobile fourth and fifth carpometacarpal (CMC) joint
 May be transverse, oblique, or spiral
May be transverse, oblique, or spiral
 May be associated with higher risk of malrotation
May be associated with higher risk of malrotation
 Suggested acceptable angulation of each metacarpal shaft
Suggested acceptable angulation of each metacarpal shaft
 Every 2 mm of metacarpal shortening leads to 7 degrees of extensor lag.
Every 2 mm of metacarpal shortening leads to 7 degrees of extensor lag.
 Up to 5 mm is acceptable without significant functional deficit.
Up to 5 mm is acceptable without significant functional deficit.
 Irreducible fractures are treated with CRPP or ORIF.
Irreducible fractures are treated with CRPP or ORIF.
 Prominent dorsal plates may interfere with extensor tendon function and necessitate later removal after union.
Prominent dorsal plates may interfere with extensor tendon function and necessitate later removal after union.
 Multiple metacarpal shaft fractures are unstable injuries that often necessitate surgical intervention regardless of deformity.
Multiple metacarpal shaft fractures are unstable injuries that often necessitate surgical intervention regardless of deformity.
4. Metacarpal base fracture and CMC joint dislocation
 Stable, minimally displaced fractures of metacarpal base are typically treated nonoperatively.
Stable, minimally displaced fractures of metacarpal base are typically treated nonoperatively.
 Ring and small CMC joint fracture-dislocations often result from higher-energy mechanisms.
Ring and small CMC joint fracture-dislocations often result from higher-energy mechanisms.
 Small-finger CMC joint fracture-dislocation is termed a “reverse” or “baby” Bennett fracture.
Small-finger CMC joint fracture-dislocation is termed a “reverse” or “baby” Bennett fracture.
 Accompanying distal row carpal fractures may be seen.
Accompanying distal row carpal fractures may be seen.
 Attempt at closed reduction is warranted, but these unstable injuries often require surgical stabilization.
Attempt at closed reduction is warranted, but these unstable injuries often require surgical stabilization.
 Delayed treatment, painful malunion, or post-traumatic osteoarthrosis may require arthrodesis.
Delayed treatment, painful malunion, or post-traumatic osteoarthrosis may require arthrodesis.
 Most common pattern is extraarticular epibasal fracture.
Most common pattern is extraarticular epibasal fracture.
 Up to 30 degrees of angulation acceptable secondary to compensatory CMC joint motion
Up to 30 degrees of angulation acceptable secondary to compensatory CMC joint motion
 Excessive angulation may lead to MCP joint hyperextension and requires CRPP.
Excessive angulation may lead to MCP joint hyperextension and requires CRPP.
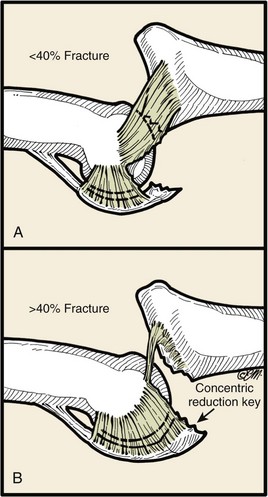
 Bennett fracture is an intraarticular fracture-dislocation.
Bennett fracture is an intraarticular fracture-dislocation.
 Abductor pollicis longus (APL) and thumb extensors cause proximal, dorsal, and radial displacement of the metacarpal shaft.
Abductor pollicis longus (APL) and thumb extensors cause proximal, dorsal, and radial displacement of the metacarpal shaft.
 Adductor pollicis causes supination and adduction of the metacarpal shaft.
Adductor pollicis causes supination and adduction of the metacarpal shaft.
 Anterior oblique or “beak” ligament keeps the volar-ulnar base fragment reduced to trapezium.
Anterior oblique or “beak” ligament keeps the volar-ulnar base fragment reduced to trapezium.
 CRPP or ORIF is chosen based on size of fragment.
CRPP or ORIF is chosen based on size of fragment.
 Rolando fracture is a comminuted intraarticular fracture that may be in shape of Y or T (Figure 7-22).
Rolando fracture is a comminuted intraarticular fracture that may be in shape of Y or T (Figure 7-22).
6. Skier’s or gamekeeper’s thumb
 Acute (skier’s) or chronic (gamekeeper’s) injury to the thumb MCP joint ulnar collateral ligament (UCL)
Acute (skier’s) or chronic (gamekeeper’s) injury to the thumb MCP joint ulnar collateral ligament (UCL)
 Competent UCL is critical for strong, effective pinch.
Competent UCL is critical for strong, effective pinch.
 Mechanism of injury is usually forceful thumb hyperextension and/or hyperabduction.
Mechanism of injury is usually forceful thumb hyperextension and/or hyperabduction.
 Spectrum of injury potentially involving proper UCL, accessory UCL, and volar plate
Spectrum of injury potentially involving proper UCL, accessory UCL, and volar plate
 Radiographs should be obtained before stress examination to rule out bony avulsion injury.
Radiographs should be obtained before stress examination to rule out bony avulsion injury.
 Stress joint with radial deviation both at neutral and 30 degrees of flexion.
Stress joint with radial deviation both at neutral and 30 degrees of flexion.
 Instability in 30 degrees of flexion indicates injury to proper UCL.
Instability in 30 degrees of flexion indicates injury to proper UCL.
 Additional instability in neutral indicates additional injury to accessory UCL and/or volar plate.
Additional instability in neutral indicates additional injury to accessory UCL and/or volar plate.
 Threshold is greater than 35 degrees of opening or greater than 20 degrees difference compared to uninjured thumb.
Threshold is greater than 35 degrees of opening or greater than 20 degrees difference compared to uninjured thumb.
 Differentiation between complete and partial tears is difficult to determine by physical examination alone.
Differentiation between complete and partial tears is difficult to determine by physical examination alone.
 Partial injuries may be initially treated with thumb spica cast immobilization for 4 to 6 weeks.
Partial injuries may be initially treated with thumb spica cast immobilization for 4 to 6 weeks.
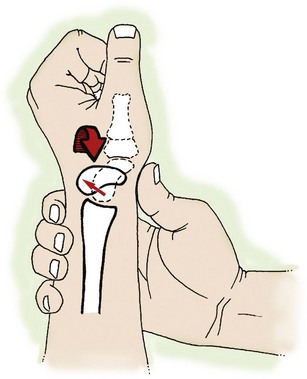
 In over 85% of cases, a complete injury is accompanied by a Stener lesion, in which the adductor pollicis aponeurosis is interposed between the avulsed UCL and its insertion site on the base of the proximal phalanx (Figure 7-23).
In over 85% of cases, a complete injury is accompanied by a Stener lesion, in which the adductor pollicis aponeurosis is interposed between the avulsed UCL and its insertion site on the base of the proximal phalanx (Figure 7-23).
 Presence of a Stener lesion may be palpable on examination, prevents proper healing, and requires surgical intervention to reattach the ligament through drill holes or suture anchor.
Presence of a Stener lesion may be palpable on examination, prevents proper healing, and requires surgical intervention to reattach the ligament through drill holes or suture anchor.
 A displaced avulsion fracture of the base of the proximal phalanx may occasionally require ORIF if large enough fragment.
A displaced avulsion fracture of the base of the proximal phalanx may occasionally require ORIF if large enough fragment.
 Chronic UCL injuries require ligament reconstruction with either adjacent joint capsule or tendon graft with or without pinning of joint
Chronic UCL injuries require ligament reconstruction with either adjacent joint capsule or tendon graft with or without pinning of joint
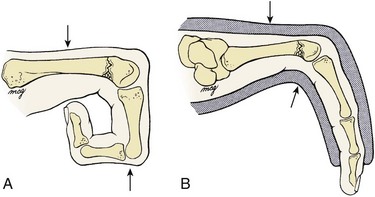
 Classified as simple or complex
Classified as simple or complex
 Dorsal dislocations are most common.
Dorsal dislocations are most common.
 Index, small fingers most frequently involved
Index, small fingers most frequently involved
 In simple dislocation, P1 is perched on metacarpal and closed reduction usually possible
In simple dislocation, P1 is perched on metacarpal and closed reduction usually possible
 Longitudinal traction and MCP hyperextension avoided
Longitudinal traction and MCP hyperextension avoided
 Direct pressure over P1 with wrist in flexion to relax extrinsic flexors
Direct pressure over P1 with wrist in flexion to relax extrinsic flexors
 In complex dislocation, P1 and metacarpal are in bayonet position and interposition of volar plate and/or sesamoids likely
In complex dislocation, P1 and metacarpal are in bayonet position and interposition of volar plate and/or sesamoids likely
 Most common hand injury in both amateur and professional fighters
Most common hand injury in both amateur and professional fighters
 The extensor hood of the MCP joint is ruptured, leading to increased risk of chondral injury and osteoarthrosis of the joint.
The extensor hood of the MCP joint is ruptured, leading to increased risk of chondral injury and osteoarthrosis of the joint.
 Presents with swelling, reduced range of motion, and occasional extensor lag
Presents with swelling, reduced range of motion, and occasional extensor lag
 Fractures of P1 deform with apex volar angulation.
Fractures of P1 deform with apex volar angulation.
 Fractures of P2 deform with apex dorsal or volar angulation.
Fractures of P2 deform with apex dorsal or volar angulation.
 Majority treated nonoperatively if less than 10 degrees of angulation and no rotational deformity
Majority treated nonoperatively if less than 10 degrees of angulation and no rotational deformity
 Three weeks of immobilization followed by aggressive motion recovery
Three weeks of immobilization followed by aggressive motion recovery
 Radiographic union lags behind clinical union by several weeks.
Radiographic union lags behind clinical union by several weeks.
 Irreducible or unstable fracture patterns may require surgery.
Irreducible or unstable fracture patterns may require surgery.
 Dorsal dislocation—most common
Dorsal dislocation—most common
 Injury to volar plate and at least one collateral ligament
Injury to volar plate and at least one collateral ligament
 “Simple” dislocation—middle phalanx in contact with condyles of proximal phalanx
“Simple” dislocation—middle phalanx in contact with condyles of proximal phalanx
 “Complex” dislocation—base of middle phalanx no longer in contact with condyle of proximal phalanx, giving a bayonet appearance
“Complex” dislocation—base of middle phalanx no longer in contact with condyle of proximal phalanx, giving a bayonet appearance
 Volar plate acts as block to reduction if longitudinal traction applied.
Volar plate acts as block to reduction if longitudinal traction applied.
 Reduction via hyperextension of middle phalanx followed by a palmar force
Reduction via hyperextension of middle phalanx followed by a palmar force
 Short-term buddy taping is sufficient aftercare.
Short-term buddy taping is sufficient aftercare.
 Persistent instability is rare but may be treated by dorsal block splinting.
Persistent instability is rare but may be treated by dorsal block splinting.
 Persistent swelling and soreness for months is common.
Persistent swelling and soreness for months is common.
 Irreducible complex dislocations require open reduction via a dorsal approach and incision between the central slip and lateral band.
Irreducible complex dislocations require open reduction via a dorsal approach and incision between the central slip and lateral band.
11. PIP joint fracture-dislocation
 Inappropriate recognition and treatment of these injuries may result in significant functional deficits.
Inappropriate recognition and treatment of these injuries may result in significant functional deficits.
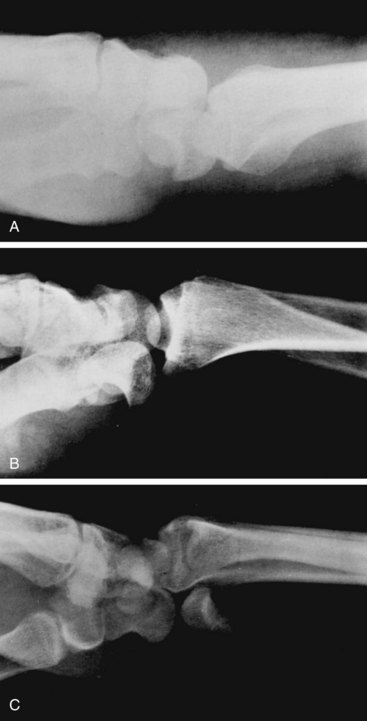
 Dorsal dislocation accompanied by fracture at P2 base (Figure 7-24)
Dorsal dislocation accompanied by fracture at P2 base (Figure 7-24)
 Hastings classification based on amount of P2 articular surface involvement (Table 7-4)
Hastings classification based on amount of P2 articular surface involvement (Table 7-4)
Table 7-4
Classification of PIP Joint Fracture-Dislocations (Hastings)
| Type | Amount of P2 Articular Surface Involved | Treatment |
| I—Stable | <30% | Dorsally based extension block splint |
| II—Tenuous | 30%-50% | If reducible in flexion, dorsally based extension block splint |
| III—Unstable | >50% | ORIF, hamate autograft, or volar plate arthroplasty |
ORIF, open reduction with internal fixation; PIP, proximal interphalangeal; P2, middle phalanx.
 Treatment options include dorsal block splinting, ORIF, and volar plate arthroplasty.
Treatment options include dorsal block splinting, ORIF, and volar plate arthroplasty.
 Regardless of treatment, maintenance of adequate joint reduction is the most important factor for favorable long-term outcome.
Regardless of treatment, maintenance of adequate joint reduction is the most important factor for favorable long-term outcome.
 Highly comminuted “pilon” fractures may be treated with the dynamic distraction external fixation method for ligamentotaxis and early range of motion.
Highly comminuted “pilon” fractures may be treated with the dynamic distraction external fixation method for ligamentotaxis and early range of motion.
 Chronic PIP fracture-dislocations are best treated with volar plate arthroplasty or arthrodesis.
Chronic PIP fracture-dislocations are best treated with volar plate arthroplasty or arthrodesis.
12. DIP dislocation and distal phalanx fractures
 DIP dislocation is treated with closed reduction followed by immobilization in slight flexion with a dorsal splint for 2 weeks.
DIP dislocation is treated with closed reduction followed by immobilization in slight flexion with a dorsal splint for 2 weeks.
 Irreducible DIP dislocations are typically due to interposition of the volar plate; treatment is via open reduction and extraction of the volar plate.
Irreducible DIP dislocations are typically due to interposition of the volar plate; treatment is via open reduction and extraction of the volar plate.
 May accompany extensive soft tissue and/or nail bed disruption in severe fingertip injuries
May accompany extensive soft tissue and/or nail bed disruption in severe fingertip injuries
 Open injuries initially treated with irrigation and débridement, reduction, nail bed repair (if necessary), antibiotics, tetanus prophylaxis, and splinting
Open injuries initially treated with irrigation and débridement, reduction, nail bed repair (if necessary), antibiotics, tetanus prophylaxis, and splinting
 Unstable, displaced fractures of the distal phalanx may require percutaneous pinning to support the nail bed repair.
Unstable, displaced fractures of the distal phalanx may require percutaneous pinning to support the nail bed repair.
 A stable tuft fracture is more common with these injuries and requires no specific treatment apart from temporary splinting.
A stable tuft fracture is more common with these injuries and requires no specific treatment apart from temporary splinting.
 Soft tissue loss treated accordingly
Soft tissue loss treated accordingly
 Highly comminuted injuries with significant soft tissue loss may be more amenable to revision amputation (shortening and closure).
Highly comminuted injuries with significant soft tissue loss may be more amenable to revision amputation (shortening and closure).
 For further details see the section “Nail and Fingertip Injuries”
For further details see the section “Nail and Fingertip Injuries”
V TENDON INJURIES AND OVERUSE SYNDROMES
1. Description and treatment are based on zones of injury (Figure 7-25).
2. Most commonly injured digit is long finger.
3. Partial lacerations less than 50% of tendon width do not require direct repair if patient can extend finger against resistance.
4. After direct suture repair of complete lacerations or those constituting more than 50% of tendon width, rehabilitation is based on zone of injury.
 Disruption of terminal extensor tendon at or distal to the DIP joint
Disruption of terminal extensor tendon at or distal to the DIP joint
 Sudden forced flexion of the extended fingertip
Sudden forced flexion of the extended fingertip
 Patient cannot actively extend at DIP joint, and finger remains in flexed posture.
Patient cannot actively extend at DIP joint, and finger remains in flexed posture.
 May be accompanied by bony avulsion injury from dorsal base of P3 (bony mallet)
May be accompanied by bony avulsion injury from dorsal base of P3 (bony mallet)
 If detected within 12 weeks of injury, closed management with full-time DIP joint extension splinting for at least 6 weeks, followed by part-time splinting for an additional 4 to 6 weeks
If detected within 12 weeks of injury, closed management with full-time DIP joint extension splinting for at least 6 weeks, followed by part-time splinting for an additional 4 to 6 weeks
 No consensus on best type of splint to use
No consensus on best type of splint to use
 Hyperextension should be avoided; skin necrosis can occur.
Hyperextension should be avoided; skin necrosis can occur.
 Maintenance of PIP joint motion often overlooked
Maintenance of PIP joint motion often overlooked
 A nondisplaced, bony mallet finger may also be treated with extension splinting until fracture union.
A nondisplaced, bony mallet finger may also be treated with extension splinting until fracture union.
 A relative surgical indication is a displaced bony mallet injury with significant volar subluxation of P3.
A relative surgical indication is a displaced bony mallet injury with significant volar subluxation of P3.
 Chronic mallet finger detected more than 12 weeks after injury
Chronic mallet finger detected more than 12 weeks after injury
 Closed treatment only if joint supple, congruent, and without arthritic changes
Closed treatment only if joint supple, congruent, and without arthritic changes
 Prolonged DIP flexion may lead to swan neck deformity (Figure 7-26), caused by dorsal subluxation of lateral bands and corresponding PIP joint hyperextension.
Prolonged DIP flexion may lead to swan neck deformity (Figure 7-26), caused by dorsal subluxation of lateral bands and corresponding PIP joint hyperextension.
 A painful, stiff, arthritic DIP joint is treated with arthrodesis.
A painful, stiff, arthritic DIP joint is treated with arthrodesis.
 Occurs over middle phalanx of digit or over proximal phalanx of thumb
Occurs over middle phalanx of digit or over proximal phalanx of thumb
 Mechanism of injury usually involves a dorsal laceration or crush component.
Mechanism of injury usually involves a dorsal laceration or crush component.
 Partial disruptions (<50%) are treated nonoperatively with local wound care and early mobilization.
Partial disruptions (<50%) are treated nonoperatively with local wound care and early mobilization.
 Direct repair may be attempted for greater than 50% lacerations.
Direct repair may be attempted for greater than 50% lacerations.
 Some surgeons will temporarily pin across terminal joint after direct repair.
Some surgeons will temporarily pin across terminal joint after direct repair.
 Occurs over PIP joint of digit (central slip) or MCP joint of thumb
Occurs over PIP joint of digit (central slip) or MCP joint of thumb
 Open injuries are directly repaired if possible.
Open injuries are directly repaired if possible.
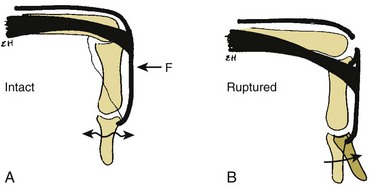
 For closed injuries, the Elson test is performed by flexing the patient’s PIP joint 90 degrees over the edge of a table and asking patient to extend the PIP joint against resistance (Figure 7-27).
For closed injuries, the Elson test is performed by flexing the patient’s PIP joint 90 degrees over the edge of a table and asking patient to extend the PIP joint against resistance (Figure 7-27).
 If the central slip is intact, the DIP joint will remain supple.
If the central slip is intact, the DIP joint will remain supple.
 If the central slip is ruptured, the DIP joint will be rigid.
If the central slip is ruptured, the DIP joint will be rigid.
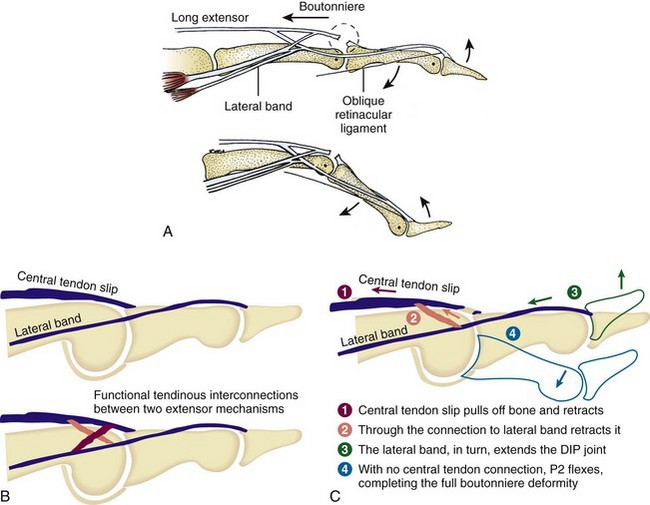
 An acute boutonniere deformity results from central slip disruption and volar subluxation of the lateral bands, resulting in DIP hyperextension (Figure 7-28).
An acute boutonniere deformity results from central slip disruption and volar subluxation of the lateral bands, resulting in DIP hyperextension (Figure 7-28).
 Closed injuries are treated with full-time PIP extension splinting for at least 6 weeks, followed by part-time splinting for an additional 4 to 6 weeks.
Closed injuries are treated with full-time PIP extension splinting for at least 6 weeks, followed by part-time splinting for an additional 4 to 6 weeks.
 Chronic (untreated) boutonniere deformity
Chronic (untreated) boutonniere deformity
 May require dynamic splinting or serial casting to achieve maximal passive motion first
May require dynamic splinting or serial casting to achieve maximal passive motion first
 A painful, stiff, arthritic PIP joint is treated with arthrodesis.
A painful, stiff, arthritic PIP joint is treated with arthrodesis.
 Occurs over proximal phalanx of digit or over the metacarpal of thumb
Occurs over proximal phalanx of digit or over the metacarpal of thumb
 Treatment is similar to that for injuries in zone II.
Treatment is similar to that for injuries in zone II.
 A common complication in this zone is adhesion formation, with resulting loss of digital flexion.
A common complication in this zone is adhesion formation, with resulting loss of digital flexion.
 Occurs over MCP joint of digit or over CMC joint of thumb
Occurs over MCP joint of digit or over CMC joint of thumb
 Lacerations involving more than 50% of the tendon substance should be repaired.
Lacerations involving more than 50% of the tendon substance should be repaired.
 Early mobilization and dynamic splinting is advocated.
Early mobilization and dynamic splinting is advocated.
 A fight bite requires surgical débridement of the MCP joint with loose or delayed wound closure.
A fight bite requires surgical débridement of the MCP joint with loose or delayed wound closure.
 A sagittal band rupture (“flea-flicker” injury) may result from forced extension of flexed digit.
A sagittal band rupture (“flea-flicker” injury) may result from forced extension of flexed digit.
 Rupture of the stronger radial fibers may lead to extensor tendon subluxation/dislocation
Rupture of the stronger radial fibers may lead to extensor tendon subluxation/dislocation
 Finger will be held in flexed position at MCP joint with no active extension
Finger will be held in flexed position at MCP joint with no active extension
 Passive extension of the MCP joint is possible, and the patient can then usually maintain the finger in an extended position
Passive extension of the MCP joint is possible, and the patient can then usually maintain the finger in an extended position
 Acute injuries may be treated with 4-6 weeks of extension splinting of the MCP joint (one of the only exceptions to splinting the MCP joints in flexion)
Acute injuries may be treated with 4-6 weeks of extension splinting of the MCP joint (one of the only exceptions to splinting the MCP joints in flexion)
 Failure of nonoperative management or missed injuries with delayed diagnosis may require repair or reconstruction of the sagittal band
Failure of nonoperative management or missed injuries with delayed diagnosis may require repair or reconstruction of the sagittal band
 Occurs over metacarpal and represents most frequently injured zone
Occurs over metacarpal and represents most frequently injured zone
 Associated lacerations of superficial veins and nerves are likely.
Associated lacerations of superficial veins and nerves are likely.
 Direct repair is indicated when the disruption constitutes more than 50% of the tendon substance.
Direct repair is indicated when the disruption constitutes more than 50% of the tendon substance.
 Early protected motion advocated postoperatively
Early protected motion advocated postoperatively
 Dynamic splinting may offer better short-term range of motion and strength without increased complications over static splinting.
Dynamic splinting may offer better short-term range of motion and strength without increased complications over static splinting.
 The prognosis is good in the absence of concurrent skeletal injury.
The prognosis is good in the absence of concurrent skeletal injury.
 Zone VII injury occurs at the level of the wrist joint, and zone VIII injury occurs in the distal forearm at the musculotendinous junction.
Zone VII injury occurs at the level of the wrist joint, and zone VIII injury occurs in the distal forearm at the musculotendinous junction.
 Lacerations at wrist level are usually associated with extensor retinaculum disruption, and postoperative adhesions are common.
Lacerations at wrist level are usually associated with extensor retinaculum disruption, and postoperative adhesions are common.
 The retinaculum should be repaired to prevent tendon bowstringing.
The retinaculum should be repaired to prevent tendon bowstringing.
 Static immobilization with the wrist held in extension and the MCP joints partially flexed is advised for the first 3 weeks, followed by protected motion.
Static immobilization with the wrist held in extension and the MCP joints partially flexed is advised for the first 3 weeks, followed by protected motion.
 The results of surgical repair in these zones are not as good as those in zones IV, V, and VI.
The results of surgical repair in these zones are not as good as those in zones IV, V, and VI.
 This injury usually results from volar lacerations, and concomitant neurovascular injury is common.
This injury usually results from volar lacerations, and concomitant neurovascular injury is common.
 Rather than attempting to probe wounds acutely, note the resting posture of the hand and check the tenodesis effect with passive wrist flexion and extension.
Rather than attempting to probe wounds acutely, note the resting posture of the hand and check the tenodesis effect with passive wrist flexion and extension.
 Each digit is then tested in isolation for active DIP and PIP flexion, especially in setting of multiple digit trauma.
Each digit is then tested in isolation for active DIP and PIP flexion, especially in setting of multiple digit trauma.
 The profundus tendons (middle through small) typically share a common muscle belly so that DIP flexion of each digit must be tested while blocking the other digits in extension.
The profundus tendons (middle through small) typically share a common muscle belly so that DIP flexion of each digit must be tested while blocking the other digits in extension.
 The superficialis tendons have independent muscle bellies and may be tested without blocking other digits.
The superficialis tendons have independent muscle bellies and may be tested without blocking other digits.
 Patial lacerations may be associated with gap formation or triggering with nonoperative treatment.
Patial lacerations may be associated with gap formation or triggering with nonoperative treatment.
 Triggering may be alleviated by trimming tendon ends under flexor tendon sheath.
Triggering may be alleviated by trimming tendon ends under flexor tendon sheath.
 Standard of care for lacerations greater than 60% of tendon width is simultaneous core and epitendinous repair within 3 weeks, but preferrably within 7 to 10 days of injury.
Standard of care for lacerations greater than 60% of tendon width is simultaneous core and epitendinous repair within 3 weeks, but preferrably within 7 to 10 days of injury.
 Basic surgical techniques of flexor tendon repair
Basic surgical techniques of flexor tendon repair
 Strength of repair proportional to number of suture strands that cross repair site
Strength of repair proportional to number of suture strands that cross repair site
 High-caliber (e.g., 5-0 instead of 6-0) suture material decreases gap formation and increases strength and stiffness.
High-caliber (e.g., 5-0 instead of 6-0) suture material decreases gap formation and increases strength and stiffness.
 A locking-loop configuration decreases gap formation.
A locking-loop configuration decreases gap formation.
 Epitendinous repair decreases gap size and increases overall strength by 10% to 50%.
Epitendinous repair decreases gap size and increases overall strength by 10% to 50%.
 Purchase, defined as the longitudinal distance from cut tendon end to transverse component of the core suture, should be 0.7 to 1.2 cm.
Purchase, defined as the longitudinal distance from cut tendon end to transverse component of the core suture, should be 0.7 to 1.2 cm.
 Dorsally placed core sutures are stronger.
Dorsally placed core sutures are stronger.
 Repair of the flexor tendon sheath has no effect on flexor tendon repair.
Repair of the flexor tendon sheath has no effect on flexor tendon repair.
 An atraumatic minimal-touch technique minimizes adhesions.
An atraumatic minimal-touch technique minimizes adhesions.
 To prevent tendon bowstringing, A2 and A4 pulleys should be preserved in digits and oblique pulley preserved in thumb.
To prevent tendon bowstringing, A2 and A4 pulleys should be preserved in digits and oblique pulley preserved in thumb.
 Risk of tendon rupture greatest 3 weeks after repair, and failure typically occurs at suture knots.
Risk of tendon rupture greatest 3 weeks after repair, and failure typically occurs at suture knots.
 In general, early protected range of motion is advocated to increase tendon excursion, decrease adhesion formation, and increase repair strength.
In general, early protected range of motion is advocated to increase tendon excursion, decrease adhesion formation, and increase repair strength.
 Use of an active flexion protocol postoperatively requires a minimum four-strand repair with epitendinous suture.
Use of an active flexion protocol postoperatively requires a minimum four-strand repair with epitendinous suture.
 Young children cannot comply with protected motion protocols and require cast immobilization for 4 weeks.
Young children cannot comply with protected motion protocols and require cast immobilization for 4 weeks.
 Abundant research continues to be focused on flexor tendon injuries.
Abundant research continues to be focused on flexor tendon injuries.
 No repair tissue matches the strength and stiffness of a normal uninjured tendon.
No repair tissue matches the strength and stiffness of a normal uninjured tendon.
 Intrinsic healing is directed by tendon fibroblasts (tenocytes).
Intrinsic healing is directed by tendon fibroblasts (tenocytes).
 Extrinsic healing potential is limited.
Extrinsic healing potential is limited.
 Tendon healing is strongly influenced by biomechanical stimuli, and early mobilization has been shown to decrease adhesion formation and increase the strength of repair tissue.
Tendon healing is strongly influenced by biomechanical stimuli, and early mobilization has been shown to decrease adhesion formation and increase the strength of repair tissue.
 Many recent studies have investigated the use of growth factor augmentation of flexor tendon repair, but no definitive conclusions can be made at this point.
Many recent studies have investigated the use of growth factor augmentation of flexor tendon repair, but no definitive conclusions can be made at this point.
 Treatment according to Verdan zones (Figure 7-29)
Treatment according to Verdan zones (Figure 7-29)
 Zone I injury (“rugger jersey” finger)
Zone I injury (“rugger jersey” finger)
 Closed FDP avulsion occurring distal to the FDS insertion
Closed FDP avulsion occurring distal to the FDS insertion
 Mechanism of injury is forced extension of the DIP joint during grasping.
Mechanism of injury is forced extension of the DIP joint during grasping.
 The ring finger is involved in 75% of cases.
The ring finger is involved in 75% of cases.
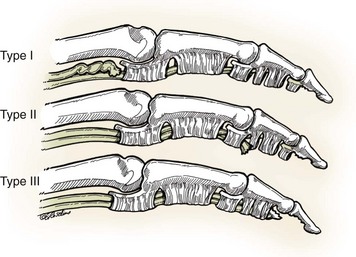
 Leddy and Packer classification (Figure 7-30)
Leddy and Packer classification (Figure 7-30)
 Type I injuries, in which the FDP is retracted to the palm, require direct repair within 7 to 10 days.
Type I injuries, in which the FDP is retracted to the palm, require direct repair within 7 to 10 days.
 Type II injuries may be directly repaired up to 6 weeks later, because the intact vincula prevent FDP retraction proximal to the PIP joint.
Type II injuries may be directly repaired up to 6 weeks later, because the intact vincula prevent FDP retraction proximal to the PIP joint.
 Type III injuries associated with small bony avulsion fragment with little retraction and may be successfully repaired up to 6 weeks after injury
Type III injuries associated with small bony avulsion fragment with little retraction and may be successfully repaired up to 6 weeks after injury
 Profundus advancement of 1 cm or more carries a risk of DIP joint flexion contracture or quadrigia.
Profundus advancement of 1 cm or more carries a risk of DIP joint flexion contracture or quadrigia.
 If full PIP flexion is present, chronic injuries may be treated with observation or DIP arthrodesis in a functional position.
If full PIP flexion is present, chronic injuries may be treated with observation or DIP arthrodesis in a functional position.
 Zone II injury (“no man’s land”)
Zone II injury (“no man’s land”)
 Occurs within the flexor tendon sheath between the FDS insertion and the distal palmar crease
Occurs within the flexor tendon sheath between the FDS insertion and the distal palmar crease
 Both the FDS and FDP may be injured in this zone.
Both the FDS and FDP may be injured in this zone.
 Tendon lacerations may be at a different level than the skin laceration, depending on the position of the finger when the laceration occurred.
Tendon lacerations may be at a different level than the skin laceration, depending on the position of the finger when the laceration occurred.
 Direct repair of both tendons with a core and epitendinous suture technique followed by an early mobilization protocol is typically advocated.
Direct repair of both tendons with a core and epitendinous suture technique followed by an early mobilization protocol is typically advocated.
 Results of treatment in this zone have been historically poor and attributed to the high rate of adhesion formation at the pulleys and associated digital neurovascular injuries.
Results of treatment in this zone have been historically poor and attributed to the high rate of adhesion formation at the pulleys and associated digital neurovascular injuries.
 Advances in postoperative rehabilitation have improved the clinical outcomes, although up to 50% of patients require subsequent tenolysis to enhance active motion at least 3 months after repair.
Advances in postoperative rehabilitation have improved the clinical outcomes, although up to 50% of patients require subsequent tenolysis to enhance active motion at least 3 months after repair.
 Occurs between the distal palmar crease and the distal end of the carpal tunnel
Occurs between the distal palmar crease and the distal end of the carpal tunnel
 Compared with zone II injuries, the results of direct repair are much better.
Compared with zone II injuries, the results of direct repair are much better.
 Lumbrical muscles originate from the radial aspect of FDP tendons in zone III.
Lumbrical muscles originate from the radial aspect of FDP tendons in zone III.
 Zone I injuries—occur distal to interphalangeal joint
Zone I injuries—occur distal to interphalangeal joint
 Zone II injuries—occur between interphalangeal and MCP joints
Zone II injuries—occur between interphalangeal and MCP joints
 Two most common postoperative rehabilitation protocols are those of Kleinert and Duran.
Two most common postoperative rehabilitation protocols are those of Kleinert and Duran.
 Kleinert protocol employs dynamic splinting, which allows for active digit extension and passive digit flexion.
Kleinert protocol employs dynamic splinting, which allows for active digit extension and passive digit flexion.
 Duran protocol requires strict patient compliance because other hand is used to perform passive digital flexion exercises.
Duran protocol requires strict patient compliance because other hand is used to perform passive digital flexion exercises.
 Both programs restrict active flexion for approximately 6 weeks.
Both programs restrict active flexion for approximately 6 weeks.
 Newer protocols add components of early active digital flexion with the hope of further reducing adhesion formation and increasing tendon excursion.
Newer protocols add components of early active digital flexion with the hope of further reducing adhesion formation and increasing tendon excursion.
 These protocols require stronger repair methods, such as the use of more than four core strands.
These protocols require stronger repair methods, such as the use of more than four core strands.
 Indicated for failed primary repair or chronic, untreated injuries
Indicated for failed primary repair or chronic, untreated injuries
 Requirements include supple skin, a sensate digit, adequate vascularity, and full passive range of motion of adjacent joints.
Requirements include supple skin, a sensate digit, adequate vascularity, and full passive range of motion of adjacent joints.
 The majority of cases require two-stage reconstruction.
The majority of cases require two-stage reconstruction.
 In stage I, a temporary silicone (Hunter) rod is implanted, secured distally, and allowed to glide proximally.
In stage I, a temporary silicone (Hunter) rod is implanted, secured distally, and allowed to glide proximally.
 Stage II is performed at least 3 months later, after full passive range of motion has been attained and a sheath has formed around the silicone rod.
Stage II is performed at least 3 months later, after full passive range of motion has been attained and a sheath has formed around the silicone rod.
 Postoperative rehabilitation is intensive, and subsequent tenolysis is needed more than 50% of the time.
Postoperative rehabilitation is intensive, and subsequent tenolysis is needed more than 50% of the time.
C Stenosing tenosynovitis (trigger finger)
1. Most common in women over 50 years of age
2. Common in diabetic patients and patients with inflammatory arthropathy
3. May simply result from repetitive grasping activities (idiopathic form)
4. Inflammation of the flexor tendon sheath, which inhibits the smooth gliding motion of flexor tendons in the digits or thumb
5. Initially characterized by pain and tenderness at the distal palm near the A1 pulley
6. If left untreated, stenosing tenosynovitis may lead to catching and locking of the digit as the space available for the flexor tendon narrows.
7. Green classification (Table 7-5)
Table 7-5
Classification of Trigger Digit (Green)
| Grade | Description |
| I | Pain and tenderness at the A1 pulley |
| II | Catching of digit |
| III | Locking of digit; passively correctable |
| IV | Fixed, locked digit |
8. Ring finger most common in adults
9. Many respond to corticosteroid injection into flexor tendon sheath.
10. Failure of nonoperative management treated surgically with release of A1 pulley
1. Attritional and degenerative condition affecting the first extensor compartment (APL/EPB)
2. Commonly affects middle-age women
3. Other high-risk groups—new mothers, golfers, and racquet-sport athletes
4. Dorsoradial wrist tenderness, swelling, crepitus
5. Finkelstein test and/or Eichoff maneuver places first extensor compartment tendons under maximum tension and exacerbates symptoms.
6. Nonoperative management includes rest, activity modification, thumb spica splinting/bracing, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroid injections into the first dorsal extensor compartment.
7. When these measures fail, surgical release of the first extensor compartment may be performed.
 Dorsal retinaculum is released to prevent volar tendon subluxation.
Dorsal retinaculum is released to prevent volar tendon subluxation.
 Anatomic variation within the first extensor compartment is frequently encountered in recalcitrant cases.
Anatomic variation within the first extensor compartment is frequently encountered in recalcitrant cases.
 Complications of operative treatment include iatrogenic injury to the superficial sensory radial nerve, tendon subluxation, complex regional pain syndrome, and recurrence from incomplete release.
Complications of operative treatment include iatrogenic injury to the superficial sensory radial nerve, tendon subluxation, complex regional pain syndrome, and recurrence from incomplete release.
1. Tenosynovitis and/or bursitis occurring at the junction between the first and second extensor compartments, where APL and EPB tendons cross ECRL and ECRB
2. Affects rowers, weight lifters, football lineman, martial artists, and golfers
3. Tenderness, swelling, and crepitus are localized to an area approximately 4 to 5 cm proximal to the radiocarpal joint.
4. Initially treated with ice, splinting, NSAIDs, corticosteroid injection into the second extensor compartment
5. When nonoperative measures fail, surgical release of the second extensor compartment and débridement of inflamed bursae may be effective.
1. Overuse syndrome from repetitive resisted wrist flexion
2. Most frequently described for FCU but may also involve FCR
3. Acute onset of wrist pain, swelling, and discoloration that mimics infection or crystalline arthropathy in severity
4. Fluffy calcium deposits may be detected on plain radiographs
5. Usually responds to short course of oral steroids or high-dose NSAIDs, ice, and immobilization
G ECU tendonitis and subluxation
1. ECU tendon held tightly within a groove in the distal ulna, tethered by a fibroosseous sheath
2. Overuse tendonitis often affects racquet-sport athletes.
3. MRI may reveal thickening (hypertrophy), partial longitudinal tears, or generalized increased signal intensity within tendon.
4. Nonoperative management with rest, activity modification, splinting, NSAIDs, and corticosteroid injections recommended
5. Traumatic subluxation of ECU tendon may result from forceful hypersupination and ulnar deviation of wrist.
 A painful audible snap or visible dislocation may be induced with reproduction of this mechanism on physical examination.
A painful audible snap or visible dislocation may be induced with reproduction of this mechanism on physical examination.
 If diagnosed early, long-arm cast immobilization (or Muenster splint) with the wrist held in pronation and slight radial deviation can be attempted.
If diagnosed early, long-arm cast immobilization (or Muenster splint) with the wrist held in pronation and slight radial deviation can be attempted.
 Chronic cases require either direct repair or reconstruction of the overlying extensor retinaculum, often accompanied by deepening of the ulnar groove.
Chronic cases require either direct repair or reconstruction of the overlying extensor retinaculum, often accompanied by deepening of the ulnar groove.
 Wrist arthroscopy reveals concurrent triangular fibrocartilage complex (TFCC) tears in ~50% of cases.
Wrist arthroscopy reveals concurrent triangular fibrocartilage complex (TFCC) tears in ~50% of cases.
VI DISTAL RADIOULNAR JOINT, TRIANGULAR FIBROCARTILAGE COMPLEX, AND WRIST ARTHROSCOPY
1. Radius rotates about a fixed ulna at the DRUJ.
2. Ulnar variance measures the distance in millimeters between the distal aspect of the ulnar head and the articular surface of the distal radius (Figure 7-31).
 Determined on posteroanterior radiograph of wrist with forearm in neutral
Determined on posteroanterior radiograph of wrist with forearm in neutral
 There is relative positive ulnar variance with forearm in pronation and negative ulnar variance with forearm in supination.
There is relative positive ulnar variance with forearm in pronation and negative ulnar variance with forearm in supination.
3. The TFCC stabilizes the DRUJ and transmits 20% of axial load at the wrist (neutral ulnar variance).
4. Components of the TFCC include the dorsal and volar radioulnar ligaments, the articular disc, a meniscus homologue, the ECU subsheath, and the origins of the ulnolunate and ulnotriquetral ligaments.
5. Periphery is well vascularized, whereas the radial central portion is relatively avascular (Figure 7-32).
1. Classified as traumatic (class I) or degenerative (class II)
2. Further divided by Palmer into subtypes based on the specific location within the complex (Tables 7-6 and 7-7)
Table 7-6
Class I: Traumatic TFCC Injuries
| Class | Characteristics | Treatment |
| IA | Central perforation or tear | Resection of an unstable flap back to a stable rim |
| IB | Ulnar avulsion with or without ulnar styloid fracture | Repair of the rim to its origin at the ulnar styloid |
| IC | Distal avulsion (origins of UL and UT ligaments) | Advancement of the distal volar rim to the triquetrum (bone anchor) |
| ID | Radial avulsion (involving the dorsal and/or volar radioulnar ligaments) | Direct repair to the radius to preserve the TFCC contribution to DRUJ stability |
Table 7-7
Class II: Degenerative TFCC Tears (Ulnocarpal Impaction Syndrome)
| Class | Characteristics |
| IIA | TFCC wear (thinning) |
| IIB | IIA + lunate and/or ulnar chondromalacia |
| IIC | TFCC perforation + lunate and/or ulnar chondromalacia |
| IID | IIC + LT ligament disruption |
| IIE | IID + ulnocarpal and DRUJ arthritis |
DRUJ, distal radioulnar joint; LT, lunotriquetral; TFCC, triangular fibrocartilage complex.
3. Class and location of the tear have important implications for treatment.
4. Value of MRI is increasing with regard to overall detection and localization of TFCC pathology.
5. All acute traumatic TFCC injuries are initially managed with immobilization and NSAIDs.
6. When nonoperative management fails to relieve persistent symptoms, wrist arthroscopy and/or open repair is indicated.
7. Arthroscopic trampoline test is performed to assess TFCC resiliency by balloting central portion with small probe.
 Central class IA tears are inherently stable and may simply be débrided when persistently symptomatic.
Central class IA tears are inherently stable and may simply be débrided when persistently symptomatic.
 Peripheral class IB tears are amenable to arthroscopic or open repair.
Peripheral class IB tears are amenable to arthroscopic or open repair.
 Concurrent fractures of ulnar styloid with persistent instability are either excised or internally fixed.
Concurrent fractures of ulnar styloid with persistent instability are either excised or internally fixed.
 Rare class IC tears are managed by either arthroscopic or open repair.
Rare class IC tears are managed by either arthroscopic or open repair.
 Class ID tears are frequently associated with distal radius fractures and often respond to reduction of radius.
Class ID tears are frequently associated with distal radius fractures and often respond to reduction of radius.
 Patients who undergo repair of a traumatic TFCC tear within 3 months of injury should expect to regain 80% of wrist range of motion and grip strength.
Patients who undergo repair of a traumatic TFCC tear within 3 months of injury should expect to regain 80% of wrist range of motion and grip strength.
 Degenerative class II tears are associated with positive ulnar variance, increased ulnocarpal loading, and ulnocarpal impaction syndrome from abutment of the ulnar head into the proximal carpal row.
Degenerative class II tears are associated with positive ulnar variance, increased ulnocarpal loading, and ulnocarpal impaction syndrome from abutment of the ulnar head into the proximal carpal row.
 Patients present with chronic ulnar-sided wrist pain, increased with forearm rotation and grip.
Patients present with chronic ulnar-sided wrist pain, increased with forearm rotation and grip.
 Pain with loading wrist in extension and ulnar deviation
Pain with loading wrist in extension and ulnar deviation
 In addition to detectable TFCC pathology, MRI may demonstrate focal increased signal in lunate and/or ulnar head at point of chronic impaction.
In addition to detectable TFCC pathology, MRI may demonstrate focal increased signal in lunate and/or ulnar head at point of chronic impaction.
 When conservative management fails, the goal of surgery is reduction of ulnocarpal loading.
When conservative management fails, the goal of surgery is reduction of ulnocarpal loading.
C DRUJ instability and post-traumatic osteoarthritis
 Acute dislocation of DRUJ can occur alone or in combination with ulnar styloid (base), radial shaft (Galeazzi), or Essex-Lopresti injuries.
Acute dislocation of DRUJ can occur alone or in combination with ulnar styloid (base), radial shaft (Galeazzi), or Essex-Lopresti injuries.
 Isolated dislocations may be treated by closed reduction and immobilization.
Isolated dislocations may be treated by closed reduction and immobilization.
 Closed reduction may be impeded by interposition of the ECU tendon.
Closed reduction may be impeded by interposition of the ECU tendon.
 Concurrent distal ulna fractures and TFCC tears may require open or arthroscopic treatment.
Concurrent distal ulna fractures and TFCC tears may require open or arthroscopic treatment.
 In a Galeazzi injury, ORIF of the radial shaft is followed by assessment of DRUJ stability.
In a Galeazzi injury, ORIF of the radial shaft is followed by assessment of DRUJ stability.
 An unstable DRUJ may require TFCC repair and/or temporary radioulnar pinning proximal to the joint with the forearm immobilized in relative supination.
An unstable DRUJ may require TFCC repair and/or temporary radioulnar pinning proximal to the joint with the forearm immobilized in relative supination.
 Chronic DRUJ instability may result from distal radius malunion, ulnar styloid nonunion, or large TFCC/ligamentous disruptions.
Chronic DRUJ instability may result from distal radius malunion, ulnar styloid nonunion, or large TFCC/ligamentous disruptions.
 Subtle chronic instability of the DRUJ may be evaluated on sequential CT scans with the forearm held in a neutral position, full supination, and full pronation and compared with the contralateral side (>50% translation is abnormal).
Subtle chronic instability of the DRUJ may be evaluated on sequential CT scans with the forearm held in a neutral position, full supination, and full pronation and compared with the contralateral side (>50% translation is abnormal).
 When chronic instability results from soft tissue incompetence, TFCC repair or ligament reconstruction (Adams) with a palmaris tendon autograft may be indicated.
When chronic instability results from soft tissue incompetence, TFCC repair or ligament reconstruction (Adams) with a palmaris tendon autograft may be indicated.
 A severely angulated distal radius malunion necessitates corrective osteotomy and appropriate treatment of resulting positive ulnar variance.
A severely angulated distal radius malunion necessitates corrective osteotomy and appropriate treatment of resulting positive ulnar variance.
2. Post-traumatic DRUJ osteoarthritis
 Maximize nonoperative management.
Maximize nonoperative management.
 Distal ulna resection (the Darrach procedure) is typically reserved for low-demand, elderly patients and may lead to painful proximal ulna stump instability.
Distal ulna resection (the Darrach procedure) is typically reserved for low-demand, elderly patients and may lead to painful proximal ulna stump instability.
 Hemiresection or interposition arthroplasty maintains the ulnar insertion of the TFCC and prevents radioulnar impingement by soft tissue (ECU tendon or capsular flap) interposition.
Hemiresection or interposition arthroplasty maintains the ulnar insertion of the TFCC and prevents radioulnar impingement by soft tissue (ECU tendon or capsular flap) interposition.
 Fusion of the DRUJ with creation of a proximal pseudarthrosis at the ulnar neck is termed the Sauve-Kapandji procedure.
Fusion of the DRUJ with creation of a proximal pseudarthrosis at the ulnar neck is termed the Sauve-Kapandji procedure.
 Early results of metallic ulnar head prosthetic replacement are promising, but no long-term studies have been performed to date.
Early results of metallic ulnar head prosthetic replacement are promising, but no long-term studies have been performed to date.
 Creation of a one-bone forearm eliminates forearm rotation altogether and remains the ultimate salvage operation for persistent pain or other complications.
Creation of a one-bone forearm eliminates forearm rotation altogether and remains the ultimate salvage operation for persistent pain or other complications.
1. Indicated for the diagnosis of unexplained wrist pain
3. May assist in the treatment of distal radius and scaphoid fractures
4. Traction tower, 2.7-mm 30-degree arthroscope
5. Arthroscopic portals (Figure 7-33)
6. Radiocarpal and midcarpal joint inspected systematically
7. Injury to superficial sensory nerves is most common complication.
VII NAIL AND FINGERTIP INJURIES
1. Fingertip injuries are most common hand injuries seen in emergency departments.
2. Long finger is most commonly involved digit.
3. These injuries may be broadly classified as those with and those without soft tissue loss.
4. Crush injuries without extensive soft tissue loss may result in nail plate avulsions, nail matrix lacerations, and distal phalanx (tuft) fractures.
5. Distal phalanx fractures are typically reduced when the nail bed is repaired, but large, displaced fragments may require percutaneous pinning.
1. Nail plate is composed of keratin and originates from germinal matrix proximal to nail fold.
2. Sterile matrix lies directly beneath nail plate and contributes keratin to increase plate thickness.
3. Crescent-shaped white lunula is seen through proximal nail plate at junction of sterile and germinal matrices.
4. Hyponychium lies between distal nail bed and skin of fingertip, serving as a barrier to microorganisms.
5. The eponychium, also called the cuticle, is at distal margin of proximal nail fold.
1. A small subungual hematoma constituting less than 50% of nail area may be treated without nail plate removal.
2. Subungual hematomas greater than 50% of nail area require nail plate removal for repair of underlying nail matrix lacerations.
 Acute repair offers best results.
Acute repair offers best results.
 Tetanus prophylaxis and antibiotics given
Tetanus prophylaxis and antibiotics given
 A digital block should be administered, and a Penrose drain may be used as a temporary finger tourniquet.
A digital block should be administered, and a Penrose drain may be used as a temporary finger tourniquet.
 If it is still available, the nail plate is removed and soaked in Betadine.
If it is still available, the nail plate is removed and soaked in Betadine.
 The wound is débrided and thoroughly irrigated.
The wound is débrided and thoroughly irrigated.
 Sterile and/or germinal matrix repaired with 6-0 or smaller absorbable suture under loupe magnification
Sterile and/or germinal matrix repaired with 6-0 or smaller absorbable suture under loupe magnification
 The eponychial fold is then splinted open with the Betadine-soaked nail plate, piece of aluminum foil, or nonadherent gauze to allow new nail plate to grow distally from germinal matrix.
The eponychial fold is then splinted open with the Betadine-soaked nail plate, piece of aluminum foil, or nonadherent gauze to allow new nail plate to grow distally from germinal matrix.
 A single-institution, randomized controlled trial has demonstrated faster healing using 2-octylcyanoacrylate (Dermabond) compared to suture repair.
A single-institution, randomized controlled trial has demonstrated faster healing using 2-octylcyanoacrylate (Dermabond) compared to suture repair.
3. If significant nail matrix has been lost, options include a split-thickness matrix graft from an adjacent injured finger or transfer of the nail matrix from second toe.
4. Nail plate deformities, especially nail ridging, are very common after crush injuries and nail bed repair.
5. A hook nail may result from a tight nail bed repair, distal advancement of the matrix, or loss of underlying bony support.
6. Patients should be counseled about high incidence of fingertip hypersensitivity and/or cold intolerance for up to 1 year.
7. Complete growth of a new nail plate takes 3 to 6 months, depending on the age of the patient.
D Fingertip injuries with tissue loss
1. Treatment of these injuries may be time intensive and challenging.
2. The general principles of treatment include preservation of digit length, maintenance of sensate fingertip pulp, prevention of joint contracture, and eventual pain-free use of digit.
3. The correct characterization of the injury is critical and guides treatment.
 Fingertip injuries without exposed bone
Fingertip injuries without exposed bone
 These may be allowed to heal by secondary intention if less than 1 cm2 of the tip or pulp is involved.
These may be allowed to heal by secondary intention if less than 1 cm2 of the tip or pulp is involved.
 Otherwise, skin or composite grafts may be required.
Otherwise, skin or composite grafts may be required.
 Full-thickness skin grafts are best for the fingertip because they provide better durability, minimal contraction, and superior sensibility compared with the split-thickness variety.
Full-thickness skin grafts are best for the fingertip because they provide better durability, minimal contraction, and superior sensibility compared with the split-thickness variety.
 Fingertip injuries with exposed bone
Fingertip injuries with exposed bone
 Characterized by the orientation of tissue loss
Characterized by the orientation of tissue loss
 Dorsal skin and subcutaneous tissue elevated superficial to the paratenon from adjacent digit to create a bed for the injured fingertip
Dorsal skin and subcutaneous tissue elevated superficial to the paratenon from adjacent digit to create a bed for the injured fingertip
 Donor site is covered with a split-thickness skin graft.
Donor site is covered with a split-thickness skin graft.
 The flap is split during a separate procedure 2 to 3 weeks later (Figure 7-35).
The flap is split during a separate procedure 2 to 3 weeks later (Figure 7-35).
 Best reserved for volar oblique injuries to the index or long digits
Best reserved for volar oblique injuries to the index or long digits
 Flap is lifted parallel to the proximal thumb crease and split after 2 to 3 weeks (Figure 7-36).
Flap is lifted parallel to the proximal thumb crease and split after 2 to 3 weeks (Figure 7-36).
 Potential complications include donor site tenderness and PIP contracture (especially in older patients).
Potential complications include donor site tenderness and PIP contracture (especially in older patients).
 Transverse or dorsal oblique digit injury
Transverse or dorsal oblique digit injury
 May be performed to preserve length and cover transverse or dorsal oblique fingertip injuries
May be performed to preserve length and cover transverse or dorsal oblique fingertip injuries
 A wide volar flap is lifted off the distal phalanx, with a tapered base created at the level of the DIP flexion crease.
A wide volar flap is lifted off the distal phalanx, with a tapered base created at the level of the DIP flexion crease.
 Flap is advanced over the fingertip toward the dorsal side, and a tension-free closure is made (Figure 7-37).
Flap is advanced over the fingertip toward the dorsal side, and a tension-free closure is made (Figure 7-37).
 Kutler popularized two separate smaller V-Y advancements from the lateral aspects of the digit to cover transverse fingertip injuries (Figure 7-38).
Kutler popularized two separate smaller V-Y advancements from the lateral aspects of the digit to cover transverse fingertip injuries (Figure 7-38).
 Alternatively, these injuries are treated by bone shortening and conversion to a volar coverage option.
Alternatively, these injuries are treated by bone shortening and conversion to a volar coverage option.
 Shortening and closing an injury that acutely violates the FDP insertion may result in a lumbrical-plus finger.
Shortening and closing an injury that acutely violates the FDP insertion may result in a lumbrical-plus finger.
VIII SOFT TISSUE COVERAGE AND MICROSURGERY
 Management begins with thorough assessment of wound, including size, location, involvement of deep structures, and presence of contamination.
Management begins with thorough assessment of wound, including size, location, involvement of deep structures, and presence of contamination.
 Standard of care involves early débridement and administration of antibiotics.
Standard of care involves early débridement and administration of antibiotics.
 Complex wounds may require several surgical débridements to remove nonviable tissue.
Complex wounds may require several surgical débridements to remove nonviable tissue.
 A clean wound bed is essential before any definitive coverage procedure.
A clean wound bed is essential before any definitive coverage procedure.
 Infection rates increase dramatically if coverage is delayed longer than 1 week after injury.
Infection rates increase dramatically if coverage is delayed longer than 1 week after injury.
 Goals of soft tissue reconstruction
Goals of soft tissue reconstruction
 Provide coverage of deep structures (e.g., bone, cartilage, tendons, nerves, blood vessels)
Provide coverage of deep structures (e.g., bone, cartilage, tendons, nerves, blood vessels)
 Create a barrier to microorganisms, restore dynamic function of the limb, and prevent joint contracture
Create a barrier to microorganisms, restore dynamic function of the limb, and prevent joint contracture
 Options for soft tissue reconstruction
Options for soft tissue reconstruction
 Choice of definitive procedure is guided by wound characteristics and patient factors.
Choice of definitive procedure is guided by wound characteristics and patient factors.
 Primary closure of a traumatic wound is generally not advised unless the wound is minimally contaminated and can be closed within 6 hours of injury.
Primary closure of a traumatic wound is generally not advised unless the wound is minimally contaminated and can be closed within 6 hours of injury.
 Wounds may be allowed to heal by secondary intention, a process involving wound granulation, epithelialization, and contraction.
Wounds may be allowed to heal by secondary intention, a process involving wound granulation, epithelialization, and contraction.
 Bone, nerve, vessel, tendon must not be exposed.
Bone, nerve, vessel, tendon must not be exposed.
 Regular dressing changes or vacuum-assisted closure (VAC) devices necessary to promote this type of healing
Regular dressing changes or vacuum-assisted closure (VAC) devices necessary to promote this type of healing
 Autografts may be either split-thickness skin grafts or full-thickness skin grafts.
Autografts may be either split-thickness skin grafts or full-thickness skin grafts.
 Both types require clean wound bed without exposed bone or tendon.
Both types require clean wound bed without exposed bone or tendon.
 Skin grafts are prone to early failure from shear stress and hematoma formation.
Skin grafts are prone to early failure from shear stress and hematoma formation.
 Preferred for dorsal hand wounds
Preferred for dorsal hand wounds
 Meshed grafts provide a greater surface area and typically have better “take” because of a lower incidence of hematoma formation and infection.
Meshed grafts provide a greater surface area and typically have better “take” because of a lower incidence of hematoma formation and infection.
 Preferred for volar hand and fingertip wounds
Preferred for volar hand and fingertip wounds
 More durable, contract less, and provide better sensibility
More durable, contract less, and provide better sensibility
 Less contraction with higher total percentage of dermis grafted, early grafting, and pressure application during remodeling phase
Less contraction with higher total percentage of dermis grafted, early grafting, and pressure application during remodeling phase
 Proximal forearm, medial arm and hypothenar aspect of the hand are common donor sites.
Proximal forearm, medial arm and hypothenar aspect of the hand are common donor sites.
 Allografts may be used as temporary measure to prepare a wound bed for later autografting.
Allografts may be used as temporary measure to prepare a wound bed for later autografting.
 A flap is a unit of tissue supported by blood vessels and moved from a donor site to a recipient site to cover a defect.
A flap is a unit of tissue supported by blood vessels and moved from a donor site to a recipient site to cover a defect.
 This unit may be composed of one tissue type or a composite of several tissue types that may include skin, fascia, muscle, tendon, nerve, or bone.
This unit may be composed of one tissue type or a composite of several tissue types that may include skin, fascia, muscle, tendon, nerve, or bone.
 Transfer of vascularized tissue promotes healing and lowers the secondary infection rate.
Transfer of vascularized tissue promotes healing and lowers the secondary infection rate.
 Flap reconstruction indicated when wound has exposed bone (stripped of periosteum), tendon (stripped of paratenon), cartilage, or an orthopaedic implant
Flap reconstruction indicated when wound has exposed bone (stripped of periosteum), tendon (stripped of paratenon), cartilage, or an orthopaedic implant
 Flaps may be classified by their vascular supply, tissue type, donor site, and method of transfer.
Flaps may be classified by their vascular supply, tissue type, donor site, and method of transfer.
 Flap classification by blood supply
Flap classification by blood supply
 Flap classification by tissue type
Flap classification by tissue type
 Cutaneous flaps include skin and subcutaneous tissue.
Cutaneous flaps include skin and subcutaneous tissue.
 Fasciocutaneous flaps include fascia with overlying skin and subcutaneous tissue.
Fasciocutaneous flaps include fascia with overlying skin and subcutaneous tissue.
 Musculocutaneous flaps include muscle with the overlying skin, subcutaneous tissue, and fascia.
Musculocutaneous flaps include muscle with the overlying skin, subcutaneous tissue, and fascia.
 Osteocutaneous flap composed of a portion of bone with overlying soft tissue
Osteocutaneous flap composed of a portion of bone with overlying soft tissue
 Innervated flaps preserve the nerve supply with the tissue unit.
Innervated flaps preserve the nerve supply with the tissue unit.
 Flap classification by donor site
Flap classification by donor site
 Local flap—provided by tissue adjacent to or near the defect
Local flap—provided by tissue adjacent to or near the defect
 Transposition flaps are geometric in design and may be either axial or random pattern with regard to blood supply.
Transposition flaps are geometric in design and may be either axial or random pattern with regard to blood supply.
 Limbs should always be equal, but the flap cut angles may vary to change the amount of desired lengthening.
Limbs should always be equal, but the flap cut angles may vary to change the amount of desired lengthening.
 Theoretically 30 degrees, 45 degrees, 60 degrees yields 25%, 50%, 75% lengthening, respectively, along the line of the central limb (Figure 7-40).
Theoretically 30 degrees, 45 degrees, 60 degrees yields 25%, 50%, 75% lengthening, respectively, along the line of the central limb (Figure 7-40).
 Rotation flaps are not geometric and are universally random pattern with regard to blood supply.
Rotation flaps are not geometric and are universally random pattern with regard to blood supply.
 Length of rotated flap should not exceed the width of its base, for doing so will exceed the capacity of the microcirculation to maintain tissue viability.
Length of rotated flap should not exceed the width of its base, for doing so will exceed the capacity of the microcirculation to maintain tissue viability.
 Advancement flaps such as V-Y and Moberg types proceed in straight line to fill defect.
Advancement flaps such as V-Y and Moberg types proceed in straight line to fill defect.
 Axial flag flaps are based on the dorsal digital artery (Figure 7-41).
Axial flag flaps are based on the dorsal digital artery (Figure 7-41).
 Fillet flap, taken from an amputated digit, occasionally salvaged for initial coverage of a mangled hand
Fillet flap, taken from an amputated digit, occasionally salvaged for initial coverage of a mangled hand
 Used when local flaps are either inadequate or unavailable for soft tissue coverage
Used when local flaps are either inadequate or unavailable for soft tissue coverage
 For example, a degloved or burned hand may be placed in a raised pocket of tissue in the abdomen or groin.
For example, a degloved or burned hand may be placed in a raised pocket of tissue in the abdomen or groin.
 Several weeks later, the flap is divided and the donor site either skin grafted or allowed to heal by secondary intention.
Several weeks later, the flap is divided and the donor site either skin grafted or allowed to heal by secondary intention.
 Alternatively, the defect site may be dissected away from the distant pocket of skin. In this case the donor site is primarily closed, and the defect may require a split-thickness skin graft over the vascularized granulation tissue.
Alternatively, the defect site may be dissected away from the distant pocket of skin. In this case the donor site is primarily closed, and the defect may require a split-thickness skin graft over the vascularized granulation tissue.
 Flap classification by method of transfer
Flap classification by method of transfer
 Flap reconstruction may be performed in a single stage or in two stages, like the previously mentioned abdominal or groin pocket flap.
Flap reconstruction may be performed in a single stage or in two stages, like the previously mentioned abdominal or groin pocket flap.
 In most instances, the donor tissue remains attached to the native vasculature.
In most instances, the donor tissue remains attached to the native vasculature.
 Alternatively, free flaps (free tissue transfer) are distant axial-pattern flaps raised on a named arteriovenous pedicle.
Alternatively, free flaps (free tissue transfer) are distant axial-pattern flaps raised on a named arteriovenous pedicle.
 Free flaps are then divided and reanastomosed to donor vessels near the defect but away from the zone of injury.
Free flaps are then divided and reanastomosed to donor vessels near the defect but away from the zone of injury.
 Most frequently used donors for use in the upper extremity include
Most frequently used donors for use in the upper extremity include
 Gracilis (medial femoral circumflex artery)
Gracilis (medial femoral circumflex artery)
 Latissimus dorsi (thoracodorsal artery)
Latissimus dorsi (thoracodorsal artery)
 Serratus anterior (the serratus branch of the subscapular artery)
Serratus anterior (the serratus branch of the subscapular artery)
 Anterolateral thigh (descending branch of lateral femoral circumflex artery)
Anterolateral thigh (descending branch of lateral femoral circumflex artery)
 Patients typically monitored postoperatively in intensive care unit
Patients typically monitored postoperatively in intensive care unit
 The room is kept warm for vasodilation.
The room is kept warm for vasodilation.
 Main cause of free-flap failure is inadequate arterial blood flow.
Main cause of free-flap failure is inadequate arterial blood flow.
 Persistent vasospasm may lead to thrombosis at the anastomosis.
Persistent vasospasm may lead to thrombosis at the anastomosis.
 Hypotension must be avoided and the patient kept well hydrated.
Hypotension must be avoided and the patient kept well hydrated.
 Vasoconstrictive agents such as nicotine and caffeine are restricted.
Vasoconstrictive agents such as nicotine and caffeine are restricted.
B Traumatic upper extremity amputation
1. Indications and contraindications
 Primary indications to attempt replantation
Primary indications to attempt replantation
 Relative indication is a level distal to the FDS insertion (zone I).
Relative indication is a level distal to the FDS insertion (zone I).
 Primary contraindications to replantation
Primary contraindications to replantation
 Patients with multisystem traumatic injuries and those with multiple medical comorbidities or disabling psychiatric conditions may be poor candidates for attempted replantation.
Patients with multisystem traumatic injuries and those with multiple medical comorbidities or disabling psychiatric conditions may be poor candidates for attempted replantation.
 Part should be wrapped in moist gauze (normal saline or lactated Ringer solution) and placed within a sealed plastic bag, which is then placed in an ice-water bath.
Part should be wrapped in moist gauze (normal saline or lactated Ringer solution) and placed within a sealed plastic bag, which is then placed in an ice-water bath.
 Although controversial, replantation is not recommended if warm ischemia time is more than 6 hours for an amputation level proximal to the carpus or more than 12 hours for an amputated digit.
Although controversial, replantation is not recommended if warm ischemia time is more than 6 hours for an amputation level proximal to the carpus or more than 12 hours for an amputated digit.
 Cold ischemia times of less than 12 hours for an amputation level proximal to the carpus or less than 24 hours for an amputated digit may still permit successful replantation, highlighting the importance of appropriate cooling of the amputated part.
Cold ischemia times of less than 12 hours for an amputation level proximal to the carpus or less than 24 hours for an amputated digit may still permit successful replantation, highlighting the importance of appropriate cooling of the amputated part.
3. Operative sequence of replantation
 Most reliable methods are close observation of color, capillary refill, and tissue turgor.
Most reliable methods are close observation of color, capillary refill, and tissue turgor.
 Measuring oxygen saturation by pulse oximetry and measuring skin surface temperature are safe, noninvasive, reproducible monitoring methods.
Measuring oxygen saturation by pulse oximetry and measuring skin surface temperature are safe, noninvasive, reproducible monitoring methods.
 Either a drop in temperature of more than 2° C in 1 hour or a temperature of less than 30° C indicates decreased digital perfusion.
Either a drop in temperature of more than 2° C in 1 hour or a temperature of less than 30° C indicates decreased digital perfusion.
 Others advocate placement of implantable venous Doppler probe.
Others advocate placement of implantable venous Doppler probe.
 Most frequent cause of early (within 12 hours) replantation failure is arterial thrombosis from persistent vasospasm.
Most frequent cause of early (within 12 hours) replantation failure is arterial thrombosis from persistent vasospasm.
 Arterial insufficiency suggested by pale skin color, decreased or absent capillary refill, loss of Doppler-measurable signal.
Arterial insufficiency suggested by pale skin color, decreased or absent capillary refill, loss of Doppler-measurable signal.
 Consider releasing constricting bandages, place extremity in dependent position, administer heparin, perform stellate ganglion block.
Consider releasing constricting bandages, place extremity in dependent position, administer heparin, perform stellate ganglion block.
 If these measures fail, exploration and attempt at reanastomosis warranted
If these measures fail, exploration and attempt at reanastomosis warranted
 Failure after 12 hours is typically secondary to venous congestion or thrombosis.
Failure after 12 hours is typically secondary to venous congestion or thrombosis.
 Venous insufficiency suggested by ruborous skin color, increased capillary refill, tissue engorgement
Venous insufficiency suggested by ruborous skin color, increased capillary refill, tissue engorgement
 May subsequently diminish arterial inflow
May subsequently diminish arterial inflow
 Remove dressings and elevate extremity.
Remove dressings and elevate extremity.
 Late complications include tendon adhesions, bone nonunion, and neuroma formation.
Late complications include tendon adhesions, bone nonunion, and neuroma formation.
 Factor most predictive of digit survival after replantation is mechanism of injury.
Factor most predictive of digit survival after replantation is mechanism of injury.
 Next most important factor is probably ischemia time.
Next most important factor is probably ischemia time.
 Clean, transverse amputations with cold ischemia time less than 8 hours survive replantation in more than 90% of cases.
Clean, transverse amputations with cold ischemia time less than 8 hours survive replantation in more than 90% of cases.
 After 8 hours, the success rate drops to approximately 75%.
After 8 hours, the success rate drops to approximately 75%.
 Replanted digits typically regain 50% total active motion and static two-point discrimination of approximately 10 mm.
Replanted digits typically regain 50% total active motion and static two-point discrimination of approximately 10 mm.
 Long-term cold intolerance almost universal, regardless of whether amputated digit is replanted or revised
Long-term cold intolerance almost universal, regardless of whether amputated digit is replanted or revised
8. Forearm and arm replantation
 Arterial inflow established before skeletal stabilization with the use of shunts, if necessary, to minimize ischemia time
Arterial inflow established before skeletal stabilization with the use of shunts, if necessary, to minimize ischemia time
 Post replantation fasciotomies performed to prevent reperfusion-induced compartment syndrome
Post replantation fasciotomies performed to prevent reperfusion-induced compartment syndrome
 Muscle necrosis may lead to myoglobinuria and life-threatening renal failure.
Muscle necrosis may lead to myoglobinuria and life-threatening renal failure.
 Elevated postoperative serum potassium level may be prognostic of replantation failure.
Elevated postoperative serum potassium level may be prognostic of replantation failure.
 Late complications include infection, Volkmann ischemic contracture, and insignificant functional recovery.
Late complications include infection, Volkmann ischemic contracture, and insignificant functional recovery.
 Controversial procedure that introduces potentially life-threatening complications from postoperative immunosuppression for a condition that is not itself life threatening
Controversial procedure that introduces potentially life-threatening complications from postoperative immunosuppression for a condition that is not itself life threatening
 Occurring around the world with more frequency, including the United States, at specialized centers with abundant resources
Occurring around the world with more frequency, including the United States, at specialized centers with abundant resources
 Bilateral transplants have been performed with good survivorship, including one above the elbow.
Bilateral transplants have been performed with good survivorship, including one above the elbow.
 Newer immunosuppressive protocols are less toxic and may lead to less long-term morbidity.
Newer immunosuppressive protocols are less toxic and may lead to less long-term morbidity.
 Still debatable whether this tremendously expensive endeavor is superior to an upper limb prosthetic
Still debatable whether this tremendously expensive endeavor is superior to an upper limb prosthetic