30. Grief and Perinatal Loss *
Sandra L. Gardner and Lorraine A. Dickey
As a life passage, pregnancy and birth are associated with hopes and expectations and joy and happiness for the future. Even though pregnancy and birth constitute a developmental crisis and major life change, expectant parents believe the gains of a healthy, happy child and family life offset any losses. Unfortunately, not all perinatal events have a happy ending. When pregnancy fails to produce a normal, healthy infant, it is a tragedy for the parents whose expectations of childbearing have not been fulfilled. Perinatal loss also affects their friends, family, and professional care providers.
Perinatal loss may be the first time a young adult has had the experience of coping with the illness or death of a loved one. Perinatal loss is especially significant because it (1) is sudden and unexpected, (2) is the most difficult loss to resolve18; (3) interrupts the significant developmental stage of pregnancy and the situational crisis of pregnancy18; (4) is the loss of a child who did not have the opportunity to live a full life36,101; (5) prevents progression into the next developmental stage of parenting that has been anticipated and rehearsed (at least in fantasy) during the pregnancy64; and (6) represents a narcissistic loss, a loss of self, for the parents. 96,119,120 Perinatal loss also often means interpersonal exclusion from the activities of childbearing friends and siblings.
Unfortunately, loss and grief often are thought of only in relation to death. However, as final and irreversible as death is, it is just one form of separation and loss. Although less obvious, other loss situations may have an equally crucial effect. Loss comes in many forms, and during the perinatal period, may occur without necessarily resulting in death. Circumstances of perinatal loss are parallel and, at the same time, different, because they all entail grief and mourning and yet each has unique dimensions and characteristics. The process of grief, its stages, and its symptoms are reviewed as a framework for understanding one’s own feelings and those of others experiencing a loss. A desire to help and an idea of what is helpful and what is not helpful are essential for effective intervention by professionals.
THE GRIEF PROCESS
Grief, the characteristic response to the loss of a valued object, is not an intellectual and rational response. 38 Rather, it is personally experienced as the deep emotion of sadness and sorrow. To the individual, grief feels overwhelming, irrational, out of control, “crazy,” and all-consuming. Mourning occurs in phases over time. After acknowledgment that the loved object no longer exists, gradual withdrawal of emotion and feeling occurs, so that eventual psychologic investment in a new relationship is possible.
A recent literature review of the theoretical perspectives of parental grief from the United States and United Kingdom reveals a change from a traditional to a “newer” model of grief in the Anglo-American culture. 29 Traditional models of grief emphasize the severing of bonds with the deceased, whereas “newer” understandings of parental grief emphasize parents retaining a relationship with their dead child. After reviewing nursing, medical, and social science publications and choosing relevant ones, Davies states: “…the concept of continuous bonds challenges the dominant assumption that resolution of grief is achieved through severing bonds with the deceased.”29 Parents wish to know that their child’s birth and death have meaning and purpose and that their child “mattered” and will be remembered by them and by others who have been “touched” and “changed” by him or her. 19
For grief to occur, the object must have been valued by the individual so that its loss is perceived as significant and meaningful. Because, prenatally, there is an investment of love in the fetus or newborn, the neonate is a valued object. To the extent that prenatal attachment has occurred, grief should be expected and felt at the loss of the fetus or newborn. Therefore loss at birth is a significant loss of a valued (although as yet only fantasized) person.
Loss, whether real or imagined, actual or possible, is traumatic. The individual is no longer self-confident or confident about the surroundings, because both have been altered. Mourning and grief are forms of separation reactions. Fears of separation and abandonment are the universal fears of childhood regardless of age or developmental stage. Perhaps loss of a significant other awakens these childhood fears and reminds us of the basic “insecurity of all our attachments.”68
Life changes are stressful to the individual because they threaten to disrupt continuity and a state of equilibrium. 88 Significant changes in the family configuration, such as accession of a new member, are normally a stressful occasion for family members. Perinatal complication or loss is even more of a stressful event for which the family has little or no preparation. The result of a crisis may be personal growth, maintaining the status quo, regression, or mental illness. 18,89 Often outcome depends on the type of help received during the crisis.
Decreasing the element of surprise through preparation for the situation to be encountered may modulate the effect of the event. Anticipatory grief 61,79,100 functions both to prepare and to protect the individual from the pain of impending loss. Prenatal diagnostic procedures, such as ultrasonography, 75 amniocentesis, and fetoscopy, can now detect a variety of severe or lethal birth defects. When there is forewarning that the pregnancy or newborn is not healthy, the parents may begin a process of anticipatory grief and psychologically prepare for the loss of their baby while hoping for his or her survival. 7
Parental withdrawal from the relationship established during pregnancy accompanies the intense emotions of anticipatory grief. Detachment protects and defends the parent from further painful feelings associated with the investment of self in a doomed relationship. If anticipatory grief proceeds, the parent may detach to the point of being unable to reattach to the infant if he or she survives. In this situation, the infant survives but the relationship with the parents may be significantly impaired. Maintaining even a remote hope that the fetus or newborn will survive protects the parents from the full experience of grief and total detachment from the baby.
The degree of parental anticipatory grief is correlated with positive feelings about the pregnancy and the mode of delivery but not with the severity of the infant’s illness. The greater the parental investment and the higher the expectations for the pregnancy, the more anticipatory grief is associated with the development of a perinatal complication. The relative severity of the medical problem is not associated with the degree of anticipatory grief.
PERINATAL SITUATIONS IN WHICH GRIEF IS EXPECTED
Loss is a fact of life, not just of death. Every stage of development requires a loss of the privileges of the preceding stage and movement into the unknown of the next stage. Any life event involving change or loss is accompanied by grief work, including moving, divorce, separation, death of a spouse or family member, injury or illness, retirement, job change, menopause, and even success. 88 The concept of loss is even applicable to the physiologic and psychologic events of normal pregnancy and birth. Certainly, when pregnancy fails to produce a live, healthy infant, a perinatal loss situation exists (Box 30-1). These perinatal losses, including stillbirth, loss of the perfect child, and neonatal death, are discussed in detail in this chapter.
BOX 30-1
1. Pregnancy
2. Birth
A. Normal
B. Cesarean section
C. Forceps
D. Episiotomy
E. Medicated
F. Prolonged or short labor
G. Place of birth
3. Postpartum (see Chapter 29)
A. “Postpartum blues”
B. Depression
C. Psychosis
4. Abortion
5. Stillbirth
6. Loss of the perfect child
7. Neonatal death
8. Relinquishment
Stillbirth
Stillbirth is the demise of a viable fetus that occurs after fetal movement when the fetus is invested by the parents with a personality and individuality. Because stillbirth occurs later in pregnancy than most abortions, there are increased parental expectations about the baby and the birth process. Selective abortions for genetic indications often are performed in the second trimester of pregnancy and involve the death of a wanted child. Even though parents understand the validity of the reason for terminating the pregnancy, sadness, guilt, and self-doubt often accompany the decision to abort. The anxieties related to termination procedures, which may include labor and birth, and the feelings of helplessness, isolation, and depression should be acknowledged and handled as in a stillbirth.
Fetal demise in utero happens either prenatally or in the intrapartum period. For 50% of stillbirths, death was sudden, without warning, and occurred from unexplainable causes. The majority of women whose fetus has died in utero spontaneously begin labor within 2 weeks of fetal demise. Carrying the dead fetus while waiting for spontaneous labor or induction is sad and difficult for the woman and her entire family. Feelings such as helplessness, disbelief, and powerlessness characterize this period. There is often an almost uncontrollable urge to flee and escape the unpleasant situation.
For the family who experiences an intrapartum demise, the joyous expectations of labor and birth suddenly change to fear, anxiety, and dread that the “worst” could have possibly happened to them. The suddenness of fetal demise in labor and birth affects both parents and professionals with feelings of shock, denial, and anxiety. Whether the loss is an early or late fetal loss, the woman and her family maintain hope by believing that the professional has made a mistake and that the fetus is still alive. 99 The onset (or continuation) of labor is approached with both hope and dread: hope that the infant may be born alive and dread that the infant’s death will soon be a stark reality.
The discomfort of labor and birth is particularly difficult for the woman whose fetus has died, because her work will not be rewarded with a healthy infant. However, oversolicitous use of drugs at birth is not recommended, because they relegate the experience to unreality and give it a dreamlike quality. 128 Keeping parents together through this crisis is important for mutual support and sharing of the birth. 97 The deadening (and deafening) silence of a stillbirth forces the reality of the infant’s death on both the parents and the professionals present at birth. 97
In the past, at the birth of a stillborn, the mother was heavily sedated or anesthetized and the neonate was hidden and whisked away immediately. These women were often left with fears and fantasies: “Was the baby normal?” “What was the sex?” “What did the baby look like?” Seeing, touching, and holding the infant promote completion of the attachment cycle, confirm the reality of the stillbirth for both parents, and enable grief to begin. 10,99,128
Because it is easier to grieve the reality of a situation than a mystical and dreamlike fantasy, contact with the stillborn enables parents to grieve the infant’s reality rather than endure their most frightening fantasies about him or her.
After confirming the reality of the infant’s death, a search for the cause, characterized by the universal question “Why did the baby die?” begins. Either or both parents may blame themselves or feel guilty about real or imagined acts of omission or commission. An autopsy may determine the cause of death, but most often the cause is unknown, even after an autopsy. However, an autopsy may be useful in reducing parental guilt and uncertainty about future pregnancies, as well as in aiding the recovery from the loss. 72,128 The “empty tragedy” of stillbirth forces the mother to deal with both the inner loss of the fetus and the outer loss of the expected newborn. Fathers experience stillbirth as a “waste of life,” are especially appreciative of the tokens of remembrance from the baby, and need help in expressing their grief. 97
Loss of the Perfect Child
Even though pregnancy ends in the birth of a live newborn, the pregnancy outcome may not be what the parents had anticipated. Birth of an infant who does not meet parental expectations represents the realization of the parents’ worst fears: a damaged child. Newborns who are preterm, have an anomaly, are sick, or are the “wrong” gender or who ultimately die represent the loss of the fantasized perfect child.
After the birth of such a infant, parental reactions include grief and mourning for the loss of the loved object (the perfect child) while adapting to the reality and investing love in the defective baby. 42,106 This reaction is analogous to parental mourning at the death of a child. 106 However, unlike the finality of death, birth of a living, defective baby entails a persistent, constant reminder of the feelings of loss and grief because of parental investment of time, attention, and care for either a short time (preterm or sick newborn) or a lifetime (physically or mentally afflicted child). 91,106
The psychic work involved in coping with the reality of the imperfect child and the inner feelings of loss is slow and emotionally painful. 40,91 The process is gradual and proceeds at an individual pace that cannot be hurried but can be facilitated and supported. Detachment from and mourning the loss of their fantasized child is necessary before parents are able to attach to the actual child.
Birth of an imperfect infant represents multiple losses for parents. A primary narcissistic injury, a threat to the female’s self-concept as a woman and mother and the male’s self-concept as a man and a father, occurs when a less-than-perfect infant is born. 27,28,40,58 Because the child is an extension of both parents, a less-than-perfect (i.e., deformed) child is equated with the perceived less-than-perfect part of the parental self. In the mind of the parent, the imagined inadequate self has failed and caused the birth of the damaged baby. 58
Prematurity
Every woman expects to deliver a normal, healthy infant at term. Therefore the onset of premature labor is both physiologically and psychologically unexpected. Premature birth is a crisis and an emergency situation characterized by an increased concern for the survival of the newborn and often the mother. Premature labor and birth are accompanied by feelings of helplessness, isolation, failure, emptiness, and no control. 58,106 The negative and dangerous atmosphere surrounding the premature birth experience may influence the relationship with the premature infant, who also may be perceived as dangerous and negative.
Normal adaptations to pregnancy are abruptly terminated by the birth of a premature infant. 58 Prenatal fantasies about the infant and the new roles of mother and father are interrupted by a premature birth. This forces parents who are “not ready to not be pregnant” to grieve the loss of a term infant and imposes premature parenting on individuals not yet ready for the experience.
As discussed in Chapter 29, anticipatory grief is one of the normal psychologic tasks accompanying premature birth. Anticipatory grief may be decreased by early contact between parents and neonate and, conversely, increased by separation of parents from preterm newborn. 58 Prolonging anticipatory grief with failure to progress through the other tasks results in altered relationships with the parents if the preterm infant survives.
Deformed Infants or Infants with an Anomaly
In approximately 2 of every 100 births, 58 an infant is born with a birth defect. Because society values physical beauty, intelligence, and success, the birth of a physically or mentally defective baby is seen as a catastrophe in our culture. 127
Recent medical advances now make it possible to identify potential fetal problems in utero. As parents receive the information antenatally, they begin the process of anticipatory grief. They experience feelings of shock, anger, guilt, and hope. At the birth of their baby, there usually is the confirmation of the anomaly, and parents must deal with the reality of the situation. Whether anticipated or not, however, the birth of a baby with a congenital defect is accompanied by ambivalent feelings for all concerned (parents, relatives, friends, and professionals). The first reactions to the reality of the situation are feelings of disbelief and shock. Feelings of shame, revulsion, and embarrassment at creating a damaged and devalued child are common. 104 Guilt, self-blame, and a search for a cause or reason for the tragedy are intermixed with feelings of anger.
The severity of loss and feelings of disappointment heavily burden the parents, a burden they may believe that no one else has experienced. 58 Their loneliness and isolation may be intensified by their self-imposed withdrawal from others. Unlike the birth of a healthy infant, the birth of a sick baby or one with an anomaly is not celebrated by society with announcements, visits, and gifts from friends and family. The negative responses of society’s representatives (family, friends, acquaintances, and professionals) may increase the parents’ negative feelings for a defective child. 127
The extent of the infant’s anomaly cannot be used as a criterion for the degree of parental grief reaction, although a gross, visible anomaly may elicit more emotional reaction than a hidden or minor one. 58 A seemingly “minor” anomaly as defined by the professional may represent a severe impairment to individual parents. The professional, who has had more contact with infants with a wide range of anomalies, views the individual infant’s anomaly in a different context than that typical for the parents, who may have limited or no experience with a deformed child or adult. The professional also views the infant’s defect from a less personal, more objective, and less narcissistic position than the new parents.
When the newborn is sick, the degree of mourning and parental feelings of grief and loss are not equated with the severity of the neonate’s illness. 7,105 Even seemingly minor illnesses such as jaundice or respiratory difficulty requiring phototherapy or minimal oxygen supplementation are associated with parental concern for survival and feelings of grief and loss. 78 These feelings are often not acknowledged by the parents or professional care providers because of the non-serious medical nature of the condition. In the mind of the care provider, self-limiting and treatable conditions are compared with more serious and often fatal neonatal illnesses. The care provider feels relieved about the “minor” nature of the neonate’s condition and conveys this to the parents—“This is an easy condition to remedy. You don’t have anything to worry about. The baby will go home in a few days.”
Thus only the medical aspects of the newborn’s illness are dealt with, whereas parental feelings remain unspoken and unresolved. 16 In an altruistic attempt to reassure and comfort the family about the newborn’s complete recovery, the professional unwittingly may discount the parents’ real feelings. If the care provider is not concerned, parents may feel that they, too, should not be concerned and thus distrust and discount their own feelings.
Neonatal Deaths
The reactions accompanying neonatal illnesses are similar to the grief reactions experienced by parents whose infant dies. 7,123 Failure to acknowledge (even minor) neonatal illness as a loss situation and to work through the associated grief prevents parents from detaching from the image of the perfect child and taking on the sick newborn as a person to love. This may result in an aberrant parent-infant attachment. The liveborn infant who is critically ill or has a severe anomaly will be the focus of a “painful time of waiting”10 for the family. They must deal with the uncertainty of whether their child will live and be healthy, live and continue to need extensive medical or special care, or die.
More deaths occur in the first 24 hours of life than in any other period of life. Yet death of a newborn is not the expected outcome of pregnancy. The majority of neonatal losses are caused by prematurity (80% to 90%) and congenital anomalies that are incompatible with life (15% to 20%). Regardless of the cause of death, even infants who live only a short time are mourned by their parents. 56 Prenatal attachment and investment of love in the newborn result in a classic grief reaction at the newborn’s death.
Even a short period of life between birth and death gives parents an opportunity to know and take care of their infant. 108 Completion of the attachment process enables parents to psychically begin the next process of detachment. Attachment to the baby’s reality encourages detachment from that reality rather than from the parents’ most dreaded fears and fantasies about their infant. Parental contact with the child before death enables them to share life for a brief time.
In the case of multiple births, when one infant or more dies and the others live, parents simultaneously grieve the loss of the dead infant while attaching to the survivor. 60,82,83,110 In many situations of multiple birth, the surviving infant or infants are in an intensive care nursery. The diametrically opposite feelings of love and attachment and grief and detachment, as well as the anxiety associated with the care and well-being of the surviving infant, are emotionally draining for new parents. The process of grief may slow the parents’ ability to become intimately involved with their surviving infant(s). 83,84,124 They may have ambivalent feelings toward the infant(s) who survives or toward the infant(s) who dies. With the loss of one infant of a multiple birth, there is less support for the grieving parents because the frequent response is that they should be thankful for the survival of one (or more) of their infants. Research shows that the death of a twin (or higher-order multiple) is as great a loss for a mother as the death of a singleton. 82,83,110 Helpful interventions include (1) acknowledging the uniqueness of every baby; (2) viewing, holding, and photographing the babies together—living and dead; (3) private time with each deceased infant; and (4) similar mementos and keepsakes from each infant, deceased and living, given to the parents. 82.83. and 84.
Generally, death of a newborn occurs despite everything done to prevent it. This provides parents with some measure of comfort in knowing that they did everything possible. Yet when the neonate is so severely ill or deformed that a decision about initiating or continuing life support is necessary, the parents have an extra burden. The situation may involve conflicts between physicians, nurses, and family wishes, causing significant personal anguish. As part of the federal Baby Doe regulations, most hospitals now have ethics committees that address the medical, legal, and ethical controversies (see Chapter 32). The decision-making process may be collaborative, parent initiated, directive, or nondirective. 82 Regardless of who makes this decision, it is primarily the parents who will live with the ramifications of that decision. When parents are involved in the decision-making process, they wonder if theirs was the right decision regardless of the decision. Whether the baby lives or dies, they wonder how a different decision would have changed their lives.
STAGES OF GRIEF
The experience of grief is a staged process that occurs over time. To detach both externally and internally from the lost loved object, emotional investment is withdrawn so that it may be invested in new love relationships. 61 Each stage of grief represents a psychologic defense mechanism used to help the individual adapt slowly to the crisis. This slow adaptation is purposeful, because it prevents the individual psyche from being overwhelmed by the pain and anguish of loss. 81
Although the stage of grief is recognizable, the process of grief is dynamic and fluid rather than static and rigid. Parents, families, and professionals progress cyclically through the stages of grief rather than in an orderly progression from beginning to end. However, each person experiences the process of grief uniquely and at an individual rate. Knowledge of each stage is necessary to assess where an individual family member, the family as a unit, and the staff are in their grief process. This information is then used to support individuals when they are in their particular stage of grief. Rather than attempting to maneuver grieving individuals from stage to stage, contributing to their defense, or stripping individuals of their defenses, knowledgeable professionals are prepared to understand and honor the individual’s grieving process. Regardless of the type of perinatal loss, the experience of that loss through staged grief work closely parallels the grief stages described by Elisabeth Kübler-Ross. 59
The feelings of disbelief and rejection of the news are reflected in the responses “No! This couldn’t happen to me!” “It isn’t true! They’ve made a mistake!” This immediate response protects the individual from the shocking reality of loss by postponing the full effect of reality until the psyche can handle it. 99 By holding on to the fantasy of a positive outcome (e.g., the loss of the heartbeat is only temporary or the dead infant belongs to someone else), facing the awful truth and the grief associated with it is delayed at least temporarily. 99
The initial stage of grief is characterized by overwhelming feelings of being stunned and surprised. This is often seen as emotional numbness, flat affect, or immobility. 128 Emotional detachment is often expressed as an inability to cope or respond with activities of daily living, an inability to remember what others have said, and a tendency to repeat the same question. 31,36 For the tragedy to be handled in manageable pieces without overwhelming the individual, the mind may acknowledge the event only intellectually and there is a corresponding lack of emotional reaction, 128 or the event may be compartmentalized so that only a part of the situation rather than the whole becomes the focal point of attention.
Anger is the result of a gradually developing awareness of the situation’s reality. As the significance of their perinatal loss begins to dawn on them, parents (and significant others) experience the diffuse emotions of anxiety and anger. 58 With the full effect of their loss comes more focused feelings of bitterness, resentment, blame, rage, and envy of those with normal pregnancy outcomes. 59
Social prohibitions against the expression of anger, especially for women, encourage this powerful emotion to be turned inward toward the self. Anger directed inward results in depression and a deepening sense of guilt. “Why?” and “What did I do wrong or not do right to have caused this to happen?” are the hallmarks of the self-examination and self-blame that accompany perinatal loss. 58,128 Answers are often irrational and have no cause-and-effect relationship with the reality of the circumstances. Irrational, feared causes include sexual intercourse (common worry of both men and women), career (of the mother) outside the home, superstitions, dietary habits, or lifting heavy objects. 128 Ideas of punishment (for past wrongs, for negative or ambivalent feelings, or for an unwanted pregnancy) 8 are often thought to be the reason for the failed outcome. The search for a reason to answer the question “Why me?” requires correct information to dispel unrealistic fantasies of causation. However, the question does not require a literal answer (often no concrete answer exists) but is merely a wish for a change in the situation. 8
Anger directed outward is usually expressed as overt hostility to those in the immediate environment (family, children, care providers, and infant) 128 or toward God. 81 Fathers exhibit more anger than mothers do. 44 Blame and anger may be destructive forces in the relationships among family members and prevent these relationships from being a source of comfort and support. Venting of angry feelings toward professional care providers protects these family relationships for more positive interactions. Anger moves the grieving process along, but persistence of anger may prevent grief work from progressing to subsequent stages.
Bargaining may occur concomitantly with denial and shock as an attempt to prevent or at least delay the loss. Bargaining usually occurs with whoever the parents (family or staff) believe the Supreme Being is. The “Yes, but” of this stage is a form of “conditional acceptance” while still attempting to make the reality other than what it is. 8,59 With the defective infant, bargaining may take the form of shopping for a physician or searching for the magic cure. 127
The onset of depression and withdrawal marks the stage of a greater level of acceptance of the tragedy. With the true realization of the effect of the loss, the individual acknowledges that indeed there is a reason to be sad. The predominant feelings of this stage are overwhelming sorrow and sadness72 evidenced by tearfulness, crying, and weeping. 99 Feelings of helplessness, worthlessness, and powerlessness contribute to the sense that life is empty and futile. Withdrawal may be evidenced by requests to be left alone, by decreased or complete cessation of visits to the infant, and by silence. 59 The degree of withdrawal may be indicative of the depth of depression and the extent to which there is guilt and self-blame. 99
Acceptance is the resolution stage of the grief process that is heralded by resumption of usual daily activities and a noticeable decrease in preoccupation with the image of the lost infant. 61 This stage usually is not witnessed by the perinatal professionals. The acceptance stage is characterized by emotional detachment of life’s meaning from the lost relationship and reestablishing it independent of the lost object. 59,68 The lost relationship is seen in a new light—as giving meaning to the present. 68 The aggrieved person relinquishes that part of himself or herself that was defined in the lost relationship and establishes a new identity that is emotionally free to attach in another relationship.
For the family of a deformed child, acceptance is not an all-or-nothing proposition but, rather, a daily adaptation and coping with the child and the defect. 103 For the family, periods of frustration and sorrow alternate with periods of delight and enjoyment of the child. Because of the chronic sorrow experienced throughout the life of a defective child, the final stage of resolution of the family’s grief is possible only after the child’s death. 79,127
The acceptance stage represents the ability to remember both the joys and sorrows of the lost relationship without undue discomfort. 38 With gradual integration of the loss, there are progressively fewer attacks of acute, all-consuming pain. 68 When recalling the lost infant, there are fewer feelings of devastation and more a feeling of sadness. The ability to “celebrate the loss” also identifies grief resolution. Celebration of the loss does not mean recall without sadness and sorrow but with an ability to find some meaning, some good, and some positive aspects in the situation (e.g., “At least we had our child for a time, even though it was a short time”).
SYMPTOMS OF GRIEF
Although each person copes with grief in individual ways, there are expected reactions to loss situations. Knowledge of the differences and commonalities of the grief experience enables care providers to understand their own reactions, as well as to share their thoughts and feelings with the grieving family. The professional care provider must learn to “hear” what the family says about how and where each member is in the process of grief resolution. Often the “message” is not a direct reference to the loss or one’s feelings but, rather, nonverbal communication. The professional must learn to recognize that individuals often communicate more by what they do and what they omit than by what they say.
The signs and symptoms of acute grief have been well described and include both somatic and behavioral manifestations of the emotional experience of the loss (see the Critical Findings box below). The behavior of the bereaved is characterized as ambivalent. 68 In certain perinatal situations, parents simultaneously hope that the infant will live and wish for the infant to die; they want to love and care for the infant and at the same time wish to reject him or her. 58 These feelings are frightening and socially unacceptable and therefore often remain unspoken.
Signs and Symptoms of Grief
1. Somatic (physiologic)
a. Gastrointestinal system
Anorexia and weight loss
Overeating
Nausea or vomiting
Abdominal pains or feelings of emptiness
Diarrhea or constipation
b. Respiratory system
Sighing respirations
Choking or coughing
Shortness of breath
Hyperventilation
c. Cardiovascular system
Cardiac palpitations or “fluttering” in chest
“Heavy” feeling in chest
d. Neuromuscular system
Headaches
Vertigo
Syncope
Brissaud’s disease (tics)
Muscular weakness or loss of strength
2. Behavioral (psychologic)
a. Feelings of:
Guilt
Sadness
Anger and hostility
Emptiness and apathy
Helplessness
Pain, desperation, and pessimism
Shame
Loneliness
b. Preoccupation with image of the lost infant
Daydreams and fantasies
Nightmares
Longing
c. Disturbed interpersonal relationships
Increased irritability and restlessness
Decreased sexual interest and drive
Withdrawal
d. Crying
e. Inability to return to normal activities
Fatigue and exhaustion or aimless overactivity
Insomnia or oversleeping
Short attention span
Slow speech, movement, and thought process
Loss of concentration and motivation
Often the intensity of grief is greater when the relationship with and feelings about the lost person are ambivalent. 68 Even with the most positive of pregnancy outcomes, taking a newborn into the family results in ambivalent feelings for all family members. The degree of disruption that a perinatal loss brings to the family is equated with the severity of grief, especially because reproduction and a healthy perinatal outcome are highly valued in our society. 68
MALE-FEMALE DIFFERENCES
Although members of both genders have the same grief reactions, women express more symptoms (crying, sadness, anger, guilt, and use of medications) 34,50,51,70,93 than men. This difference in symptomatology does not represent a different experience of grief but merely a different expression of it. Understanding these differences and the reasons for them is crucial for care providers working with parents at the time of perinatal loss. Explaining these differences to parents is also crucial so that diverse grief responses do not become divisive in the relationship. 34,93
The father’s degree of investment in the pregnancy, impending parenthood, and the circumstances of birth all affect his feelings of loss. Because the father’s body does not directly experience the changes of pregnancy, the pregnancy initially may be less of a reality to him than to the pregnant woman. This lag in the physiologic reality contributes to a lag in the psychologic investment of the father in the baby. The father’s lag in psychologic investment often contributes to incongruent grieving, a difference in mother’s and father’s grief reactions. Fathers often comment that the infant became real when he felt the fetus move in the mother or at first sight of the new infant. Fathers who form an early attachment to the child feel sadness, disappointment, and often anger at being denied the expected son or daughter. 44,55,70,71,97 Conversely, fathers who have been normally ambivalent or overtly negative about the pregnancy may feel guilt and responsibility for the failed outcome.
Participation of the father in the events of labor and birth also influences his attachment and ultimately his feelings of loss. Exclusion decreases his involvement in these life-crisis events, whereas inclusion has many advantages for the mother, infant, and self (see Chapter 29). If the infant is ill, the father may initially have more and closer contact than the mother. 7 In the birth place, the father may see, touch, or hold the infant before the mother does. The father observes the initial resuscitation and stabilization and may accompany the infant to the nursery and on transport to a regional center. Often the father receives the first information and support about the infant’s condition and returns to the hospitalized mother with the news. This early, prolonged contact coupled with the father’s increased responsibility often contributes to the development of a closer and earlier bond between father and infant than between mother and infant. The initial lag in prenatal investment may be offset after birth by concentrated contact between the father and the baby, so that a loss is highly significant to the father.
Societal expectations about masculinity and femininity markedly influence the expression of grief. Society’s message to men starts early in life: “Big boys don’t cry” and “Don’t cry, you’ll be a sissy” (i.e., girl). The preferred male image in our society is the autonomous, independent achiever who is always strong and in control, even in the face of disaster. 44,45 In keeping with this image, the father may feel that he must make all the decisions and have all information filtered through him to protect the mother. However, this altruistic gesture prevents full disclosure to and involvement of the mother. Assuming the role of strong protector also involves a heavy price for the father in suppression of his own feelings and delay of his own grief work. 34,71,93 The role of “tower of strength” often engenders feelings of resentment from the mother. Although he attempts to live up to his (and society’s) expectations of himself, the woman views his apparent lack of feelings and emotions, especially crying, as “He doesn’t care.” A recent study showed that distress experienced by the mother but not by her partner resulted in longer-term marital dissatisfaction for the mother.
Many men have difficulty dealing with irrational behaviors, as well as with the normal ambiguity and conflict of life. This difficulty makes the emotional response of grief and its accompanying ambivalent feelings and conflicts produce discomfort and anxiety in many men. The expression of appropriate human emotions becomes threatening and makes them feel vulnerable. To decrease the anxiety associated with grief and its expression, men often deal with feelings by denying them, increasing their workload, grieving internally, or withdrawing from the situation and refusing to discuss it. 70,93
The father’s attitude and ability to communicate about the loss may help or impede the mother’s grief work. 100 Lack of communication between a couple may contribute to intense mourning, psychiatric disturbances, and severe family disruption. 56,93,118 Synchrony of grieving between the mother and the father is important in an ultimate healthy resolution for the family. 22,93 If the father denies and suppresses his own feelings of loss and grief, he may react to the normal signs and symptoms of grief in his partner as if they were abnormal. Often the father can resolve his grief faster than the mother, and he may become impatient with her continual “dwelling” on the loss. Sometimes fearing the woman’s prolonged grief, the man decides to “spare her” from his feelings and does not discuss them with her. Instead of being comforting as intended, failure to share grief leads to isolation and alienation within the relationship. 58,93
In some situations, the man may experience intense emotions several months after the death, not unlike those his partner experienced at the time of the crisis. Because these intense emotions occur so long after the crisis, he may not even associate them with the death. 31,58 A recent study found that at 30 months after the death of a baby, fathers were more distressed than the mothers, who were the more distressed initially after the death. 118
TIMING OF GRIEF RESOLUTION
Parents
Emotional recovery from the pain of perinatal loss occurs with time. There is no complete agreement on the length of time necessary for the individual to resolve grief. Indeed, a specific timetable for mourning may be impossible to establish. 8 However, some general time frames are available for the duration of a normal grief reaction.
Acute grief reactions are the most intense during the first 4 to 6 weeks after the loss, 61,68,81 with some improvement noted 6 to 10 weeks later. Normal grief reactions may be expected to last from 6 months to 1 year 6,38,58,81 or 2 years. 68 Indeed, significant losses of a spouse or child may never be completely resolved29,96,119: “I’ll never get over it.”
One parameter for differentiating normal from pathologic grief has been the length of time for grief to be resolved. Grief work may still be categorized as normal even if it lasts longer than 1 year, especially if the person is working through unresolved grief from the past. Grief work is normally energy draining. Dealing with more than one grief or loss situation compounds the intensity of mourning and may prolong the grief reaction. Because perinatal loss represents more than the loss of the newborn (loss of the perfect child, loss of plans for the future, and loss of self-esteem), feelings of sadness and depression may still be evident for a year or longer. 58,70,118,128
Sorrow and grief may even last a lifetime. For families of defective children, “chronic sorrow”31,49,79,91,106 is experienced as long as the child lives. These parents live with the constant reminder of what is not and what the child will never be and can never do. The grief of death is final—parents do the work and go on; chronic sorrow is grieving on a daily basis. Expecting the parents to adjust to or accept their child’s defect without any elements of lingering sadness is unrealistic. Although hampered by small sample sizes, research on the gender differences in chronic sorrow show more chronic sorrow in mothers than in fathers. 49,67 Chronic sorrow is a justifiable reaction to the daily stresses and coping necessary when a child is defective. The final stage of grief resolution is possible only with the finality of the death of the child.
Even when grief has been resolved, anniversary grief reactions are normal. Feelings of sadness, crying, and normal grieving behaviors may be reactivated at certain times. These anniversary reactions may not be limited to the infant’s date of death but also may be felt on the expected date of delivery, on the actual birthday, or on seeing an infant of the same age and gender as the lost infant. Holidays may also reactivate grieving behaviors, especially those that bring together family and friends and recall memories of joy and happiness.
Staff
Those sharing a crisis (complication, illness, or death) often become closely attached, so that the loss is felt not only by the family but also by the professional care providers. * Repeatedly dealing with death and deformity increases the professional’s exposure to personal feelings of grief and loss. This may be perceived either as a threat or a personal opportunity for growth. 37
The critical variable in the ability to face or assist others in handling loss is the manner in which the care providers have been able to resolve their own personal losses. Unless the care providers can cope with personal feelings of loss and grief, they may not be able to give of the “self” to others. Care given without genuine involvement and responsiveness to the family’s feelings does not facilitate and may actually impede the mourning process. Professionals who can deal honestly with their own feelings will be able to help others cope with theirs. 21,83
Helping parents deal with their grief may be difficult for professionals because of their attitudes and feelings about perinatal loss. For professionals trained to preserve life, loss of the best pregnancy outcome or death itself represents both a personal and professional failure. 58 When success is equated with life, the failure of death (or loss) is associated with feelings of guilt, anger, depression, and hostility. 128 Just when professionals are expected to be supportive and therapeutic, they may be overwhelmed with their own feelings. Professionally, the care providers may feel helpless when all efforts inevitably result in no change in the outcome.
The feelings and stages of grief experienced by the family are the same ones felt by the staff who are attached to the parents and their newborn. Many professionals working in perinatal care are of childbearing age, so identifying with the parents and their plight is relatively easy. Because the sick, deformed, or dead infant could easily be that of the staff, they share with the parents the special stress of the loss of a child. The care provider often experiences the same fantasies of blame as the parents: “What did I do (or not do) to cause this?”
Repetitive contact with loss situations and death exposes the staff to recurring feelings of frustration, guilt, self-doubt, depression, anger, classic grief reactions, helplessness, sadness, hopelessness, loneliness, and covert relief. 32 Such uncomfortable feelings often lead to behaviors of avoidance and withdrawal as a means of self-protection; this has been called “compassion fatigue.”21,83,96 Adequate medical care may be given, but psychologic care of the family may be neglected. 64 The involved primary care providers may decrease their attachment to both parents and infant when an unfavorable outcome is inevitable. Withdrawing emotional support and involvement may spare the professional but only adds to parental feelings of isolation, inadequacy, and worthlessness. Professionals who have risked family attachment and shared grief work may be more cautious in future involvements to protect themselves from the pain of loss.
Asynchrony and individual differences in handling grief reactions also may cause problems among the professional staff. Constant exposure to perinatal loss may desensitize some individuals until they are blasé or even callous about the crisis, whereas the grief reactions of others parallel the family’s reaction. Some staff members may have reached the stage of acceptance, whereas others who cannot let the infant go persist in the idea of a magical cure, a characteristic of denial. The rationale of prolonging the child’s life may in reality be prolonging death, and inevitably one needs to accept death’s finality.
Staff members cannot offer support to families experiencing loss unless they receive support in dealing with their own grief reactions. 21,37,39 Those who receive support learn about their feelings and how to handle them and so have no need to displace their pain to others. The three most effective ways that neonatal intensive care unit (NICU) nurses have identified to manage their stress after a neonate’s death are (1) discussing with co-workers, (2) supporting and comforting the grieving family, and (3) talking with their own families. 32 Various formats are available for meeting staff needs, such as mutual support of colleagues or group sessions involving peer counseling on a long-term or short-term basis. 21,32,39,58,92 Group meetings provide a vehicle for support and for sharing information and feelings among staff members. 21,32,39,58,92 Facilitated by an objective person with expertise in group process and the concepts of grief, such meetings have the goal of helping the staff deal with their reactions so they will be better equipped to help the parents. Group sessions also serve to decrease stress, increase job satisfaction, and ultimately help prevent burnout. Staff members are encouraged to retain their humanity when an environment is created in which emotions are valued and their healthy expression facilitated, both at the time of loss and in its resolution. 53,92
Sharing grief work with a family gives the care provider a chance for personal growth, to review past personal losses, and to evaluate the adequacy of their resolution. Helping others with loss or grief provides the professional with the opportunity to contemplate present and future losses, including one’s own mortality. By working with those who have suffered a significant loss or death, a health care provider may gain a deeper perspective about life.
INTERVENTIONS
Those in a crisis feel an openness to help and assistance from others, so that those in the crisis emerge either stronger or weaker, depending on the help they receive. 17,89 This increased openness also makes those in a crisis more vulnerable to the reactions of others—to their facial expression, tone of voice, and choice of words. Helpful professional interventions provide psychologic assistance during a highly vulnerable period of personal development. The goals of intervention are to maintain the pre-crisis level of functioning and to improve coping and problem-solving skills beyond the pre-crisis level (i.e., to facilitate personal growth). Effective intervention is characterized by helping grief work get started, by supporting those who are grieving adaptively, and by intervening with individuals who display maladaptive reactions. 22,35
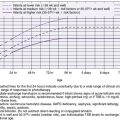
For professionals, understanding parental perspectives of the experience of death of a newborn should enable provision of more sensitive and evidence-based care for grieving families. The results of two recent research studies give some insight into what is helpful and what is not helpful for grieving families. The first study was a systematic review of 61 studies and more than 6000 parents who suffered neonatal death. 43 This study found that parents valued emotional support, grief education, and attention to mother/baby. Non-helpful and distressing behaviors from health care providers included avoidance, thoughtlessness, insensitivity, and poor staff communication. 43 Another study conducted semi-structured interviews with mothers/fathers (n = 19) a mean of 1.9 years after death of their infant. This exploratory study found a low level of grief, effective coping, and factors important to parents in end-of-life care for their infant. 14 Review of the data from this study in Table 30-1 instructs health care professionals in helpful and non-helpful interventions during the stressful experience of a dying infant. 19 Because 76% of the dying infants were in the NICU or pediatric intensive care unit (PICU) and 42% of the families had hospice/palliative care team involvement, 14 perhaps the low level of grief and the positive adaptation by this small group of parents were because of the sensitive, helpful interventions of their health care providers.
| Study Findings | Comments |
|---|---|
| 1. Parents scored significantly lower than other parents who had lost a child and other adults with grief experience. | 1. Lower levels of grief were measured by the Revised Grief Experience Inventory (RGEI), a 22-item Likert scale. |
| 2. Study investigators viewed parents as positively adapting after loss of their infant. | 2. Mean scores were 33.16 (out of a highest possible score of 36) on the Post-Death Adaptation Score, a 10-item scale rated by professionals. |
| 3. Seven important aspects of care:
A. Honesty
B. Empowered decision making
C. Parental care
D. Environment
E. Faith/trust in nursing care
F. Physicians bearing witness
G. Support from other hospital care providers
|
3. Identified by parents:
A. Parents expect professionals to be honest in giving information about the infant/condition to them.
Parental anger results when (parental) perception is that honest information was not given.
B. Parents want to be involved in medical decision making, especially about withdrawing life support. Parents who had been involved were glad they had been part of the decision process and felt supported by the medical team.
Parents felt anger and abandonment when the decision to withdraw support was not believed to be respected by professionals.
C. Parents needed care as much as their baby; when staff were insensitive to their needs, parents felt upset.
D. Parents appreciated comforts of sleep/family rooms as well as private, quiet areas where the infant died with family/parents. People present at the death were more important than the place of death.
Parents expressed fear when left at home with their dying infant; parents wished they had held the infant longer.
E. Parents had greater trust in nurses than other providers; most had positive experiences with their infant’s nurses. Parents appreciated nurses personalizing and respecting the infant (using baby’s name) as well as providing for the infant’s comfort and opportunities for parental care of their baby.
Negative experiences included mistakes in care and unprofessional behavior.
F. Parents thought it important that the physician be with them throughout the process, including being present at the time of the infant’s death. Parents perceived the absence of the physician at the time of the child’s death as negative, especially if they had been told that the physician would be there for them.
Parents found it meaningful when the physician and other medical staff had contact with them after they had gone home.
G. Parents appreciated support that they received from chaplains, social workers, and palliative care and child life workers. Parents also appreciated support and help from these providers in dealing with siblings.
|
| 4. Seven coping strategies:
A. Family support
B. Keeping the memory alive
C. Spirituality/faith
D. Altruism
E. Refocusing on life
F. Validation of decision
G. Bereavement support groups
|
4. Identified by parents:
A. Parents relied on family support to cope with the death, appreciated family presence at the hospital/home when the infant died, and found it helpful to talk to extended family about their infant. When extended family members were not supportive and avoided talking about the infant, parents were distressed.
B. All parents showed researchers mementoes of their dead infant and emphasized the importance of bringing things home (i.e., photos; plaster castings of hands/feet; blanket/clothes) from the hospital that had been used/belonged to the infant who died. Parents especially appreciated tangible reminders (i.e., garden/tree) and rituals to remember their infant.
C. All families were comforted by their religious beliefs and found meaning and purpose in their infant’s life and death. No families reported negative spiritual experience or abandonment of their religious beliefs.
D. Many parents wanted and did “give back” to the hospitals that had cared for them and their dying infants. These altruistic acts took the form of monetary and equipment donations, volunteering, and becoming resource families to other parents with sick children.
E. Presence of other children in the family assisted parents continuing to focus on life and the daily requirements of their surviving children. All parents acknowledged that having another child would never replace the infant who died.
F. Parents were comforted by autopsy results that validated that they had made the correct decision for their infant. Parents also appreciated when physicians communicated to them their support of the parents’ decision.
G. Bereavement support groups resulted in positive experiences for most families, especially in being able to talk freely about their dead infant with others who understood and were not uncomfortable. However, some parents did not feel validated in their grief/loss of an infant by other parents in the group whose children were “older” when they died.
|
Non-helpful Interventions
Caring for pregnant women and their infants is supposed to be a “happy” job. Birthing and caring for infants are supposed to be times of joy and celebration. Because no one expects death or loss to occur in maternity or nursery areas, when it does, both staff and families are shocked. To protect themselves from the reality of the situation or to “spare” the family, professionals may engage in interventions that do not help themselves or their patients. Such interventions may be meant altruistically but do not have the characteristics of effective intervention.
Maintaining the state of denial arrests grief work by preventing or delaying the acceptance of the reality of the loss situation. Progress toward resolution is not begun until the stage of disbelief is relinquished. Using drugs, not talking or crying about the loss, and using distraction all contribute to maladaptive reactions by maintaining the state of denial. The use of tranquilizers, sedatives, and other drugs does not help the recipient but, rather, benefits the giver. Excessive use of these medications prolongs the denial stage by making the feelings and emotions foggy and dreamlike. 56 The energy needed to begin the grief work is dissipated by the effect of the medications. Avoiding the reality of the situation becomes easier when mind-altering drugs make the tragedy even more unbelievable.
Not talking about the loss is a powerful way of denying that it ever existed. 83,93 The inability of professionals to acknowledge that the loss has occurred and that the family is in pain maintains denial and repression. 16 Not discussing the loss prevents parents from learning the facts and facing their reality. Because a fantasy will be created to substitute for the unknown, the fantasy of what happened and why will be worse than the reality. By receiving truthful, honest communication, parents are not left to spend energy dealing with frightening fantasies.
Professional avoidance and unwillingness to talk with parents after a loss communicate other powerful messages that impede grief work. If the loss is not important enough to discuss, then perhaps it is not important at all. Not talking about the loss serves to reduce it and communicates to the parents, “I don’t care; therefore neither should you.” Avoidance of the topic or a hurried, businesslike or social communication that skirts the issue tells the parent that grief work is dangerous, that grief emotions are dangerous, and that others are afraid of grief and those experiencing it. In essence, not discussing the loss gives a clear nonverbal message to not grieve.
An inability to cry in response to a significant loss is not helpful and impedes grief work. The prohibition against crying may have been learned early in life or may be the result of unresolved grief work. Parents may feel the need to be strong for each other, their family, or the staff and thus do not cry. Sometimes role reversal occurs, so that the grieving person feels the need to support others rather than be the recipient of support. Often the significance of parental loss is neither recognized nor acknowledged by the professional for fear that he or she will cry. Rather than talking about the loss as a technique to facilitate tears, no one says anything so no one will cry, and no one’s grief progresses through the grief stages.
Distraction is another way of denying the loss or its significance. Professionals, a spouse, or other family members try to distract parents from the feelings and emotions of acute grief by engaging in light, social conversation or by keeping them busy with work or recreation. Dealing only with the physical care and not the need for psychologic care after birth is a form of distraction used by care providers. 47 Parents are preoccupied with their shattered expectations of the past and the stark reality of the present, and they are not interested in distractions.
After an unfavorable perinatal outcome, the couple are often confused about their status: “Am I a mother or father…or not?” This experience has been called the “ambivalent transition into motherhood.”65 Failure to acknowledge the newly acquired role of mother or father (even if the fetus or newborn dies) discounts the parent’s psychologic investment in the pregnancy, fetus, and newborn. Quickly removing the infant from the maternity or nursery areas or removing all the baby items from the home negates the infant’s existence. 58 This is not helpful for grief resolution and prevents parents from making choices and decisions and thus maintaining control over the reality of the situation.
Isolation of the grieving family prevents the development of dependent relationships with others who might potentially provide support and comfort. Without others, parents cannot share their grief and may thus increase their feelings of guilt, anger, blame, and lack of self-worth at their failed pregnancy. Those directly experiencing a perinatal loss may be isolated from the rest of society, including their families, who do not view loss of a pregnancy or neonate as significant. 10,58,93 Empathy with the parents’ definition of the loss as important is necessary for society to be supportive. The goal of recent research, professional literature, and education has been to sensitize the care provider to the effect of perinatal loss. Only recently have books specifically about perinatal loss become available to inform and assist parents.
To decrease contact with the grieving mother, the staff may neglect her or perform cursory physical care, or there may be overconcern for providing physical care. 71 Assigning a room at the end of the hall, not going into the room, delaying answering requests, and placing the mother on another floor are ways of avoiding families. Use of private rooms and room assignments off the maternity floor may be helpful but may allow staff to remove the unpleasant and uncomfortable situation. Early discharge to a supportive environment may be helpful but, without plans for follow-up, may merely be a way to remove the constant, painful reminder.
Keeping the childbearing couple together throughout the perinatal events facilitates a shared experience of the reality of the situation. Separation of the mother and father or of the couple from friends, family, and other children is not helpful. Exclusion of family members from the experience also excludes them from providing support for the mother and the couple. Relaxed visiting policies and as much contact as possible between the hospitalized mother and the father (and other family members) are important. 20,83
Prohibiting contact between the parents and the infant allows fearful fantasies of the truth that are always more frightening than the reality of the situation. Delayed contact prolongs the state of disbelief and denial. 22 Restrictive visiting policies in the nursery, institutionalizing an infant without looking at all alternatives, or any other policy that separates parents from their infant does not facilitate grief. Especially in the case of a deformed, stillborn, or dead infant, the message of delayed or no contact is that the infant is too horrible and too unacceptable to be seen or touched. Because parental egos are so symbiotically attached to their offspring, an unacceptable child is equated with an unacceptable and unworthy self. The fantasy that the damaged or dead child is representative of the damaged and defective self is borne out in the behavior and separation policies of the care providers.
In an attempt to offer the grieving family comfort, friends, relatives, and even professionals often make comments that are non-supportive and non-helpful58,83:
• “Well, you’re young. You can have more babies.”
• “Just have another baby right away.”
• “Well, at least you have others at home.”
• “It’s better to lose her now when she’s a baby than when she’s 4 years old.”
• “He never would have been totally normal anyway.”
• “He was born dead. You didn’t get a chance to know or get attached to him anyway.”
• “It’s God’s will.”
Clichés and platitudes such as these do not help because of the message they give about the parents and the infant. 99 These comments at best reduce and at worst negate the effect of prenatal attachment to the fetus. The importance of psychologic investment and attachment by the parents to this fetus or newborn is said to be basically unimportant and essentially nonexistent. 58 Because infants are viewed as an extension of the parent’s self, “by a not very subtle process of identification, the parents see a part of themselves in the baby, and nobody likes to be told that part of them is better off dead.”99 Also, comforting parents whose infant has died with the information that the child was not perfect and never would have been normal and healthy reinforces their belief that they are as defective and unsatisfactory as their dead child. 58
Such comments also convey a message about the importance of an individual life. Essentially, they say that one fetus or newborn is fairly interchangeable with another. They negate the importance of and indeed the existence of the infant for the parents, siblings, family, and society. The life of the individual is devalued, because he or she is easily replaced by “another baby.” Comparing one infant’s illness or deformity with another’s is not helpful for parents whose own infant’s deformity is certainly more important than any other infant’s problem.
The power of words to help during grief is outweighed only by their power to not help. Because parents are increasingly open during a perinatal crisis, they are sensitive not only to what is said and how it is said but also to the nonverbal message. Giving premature or false reassurance may be more for relief of the professionals than for the parents. 17 Comments such as “It’s okay” and “Everything will be all right” must be genuine and timed appropriately for the parent. Telling parents that they have a child with Down syndrome and then saying “But everything will be all right” is hardly helpful. Giving reassurance that subsequent pregnancies and infants will be all right or unaffected is not helpful before the parents are ready to think about and project into the future.
The basic terminology accompanying perinatal grief situations may be upsetting to parents. Instead of dead, professionals often substitute less frightening and less final words. The use of loss when death is appropriate may be misinterpreted (especially by children). The terms lose, loss, and lost connote misplacing, so that comments such as “I’m sorry you lost your baby” may be responded to by “I didn’t lose (misplace) my baby. My child died.” Medical professionals skirt the use of the words dead, died, and die. Care providers are taught as students to use the word expired when referring to a patient who has died. Meant to soften the effect of dead, the word expired may have its own effect, as a mother whose infant son died wrote in a poem: “The baby expired they said, as if you were a credit card.”113
Other situations that do not facilitate grief work include dealing with multiple losses or stresses and ambivalence or mental illness. 128 The reaction to the loss of a significant relationship is intensified in the context of multiple losses, stresses, and problems. 83,128 Because perinatal losses represent not only a loss of the wished-for perfect child but also a threat to the parental self, self-concept, and self-worth, they represent situations of multiple loss. 119,120
Helpful Interventions
Professionals have an opportunity to make a significant difference in the outcome after the crisis of perinatal loss for the individual, the couple, and the family. A care provider who is knowledgeable about the grief process and comfortable in sharing another’s grief is equipped to assist the family and its members toward a long-term healthy adjustment rather than a dysfunctional and pathologic adjustment. Interventions that are helpful for family members also assist staff members in their own grief work.
Factors that influence an individual’s personal experience of grief (and ultimately appropriate interventions) are outlined in Box 30-2. Care for the grieving is individualized through assessing these factors, planning, and continually evaluating the individual. 34,35,83,96 Eliciting such personal information may not be as difficult as it first seems. Those in crisis often spontaneously share crucial data with little prompting. The importance of active listening to questions and comments or a more formalized therapeutic interview process may provide the needed encouragement and permission to begin communication.
BOX 30-2
1. Previous losses
a. Type
Separation
Divorce
Death
Spontaneous abortion (miscarriage)
Elective or selective abortion
Period of infertility
Relinquishment of child
Perinatal loss
b. Timing in the life cycle
Distant
Recent
c. Coping styles (of each individual and the family as a unit)
d. Grief work
Resolved
Unresolved
2. Prenatal attachment
a. Degree of psychologic investment in relationship with fetus or newborn
b. Decision making about pregnancy and infant
Planned or unplanned
Wanted or unwanted
c. Meaning of pregnancy and infant to individual and family
d. Parental expectation about childbearing
3. Nature of the current loss
a. Timing
Sudden and expected
Anticipatory grief
b. Definition and meaning of the event (death, deformity) to individual members of the family
c. Multiple losses
Self
Perfect child
d. Nature and severity
Of loss
Of defect
4. Cultural influences (also see Chapter 29)
a. On experience and the expression of grief
b. Societal expectations dictate acceptable and unacceptable behaviors of mourning
5. Strengths (individual and family)
a. Support system (family, friends, religious, community, or social agencies) mobilized when necessary
b. Stable relationships: couple supportive of each other
c. Financial stability
d. Coping abilities: can evaluate, plan for, and adjust to novel situations
e. Good health
f. Receptive and intelligent
g. Realistic expectations about childbearing and childrearing
A history of previous losses and their type and timing in the life cycle are important data for the care provider dealing with the current loss. Past experiences with a crisis or loss influence an individual’s behavioral and coping style with current problems. 121 Experiencing a previous perinatal loss affects a subsequent pregnancy. 24,95 These pregnancies are characterized by guarded emotions, marking the progress of the pregnancy and seeking out or avoiding various behaviors. 23.24.25. and 26.121 A previous perinatal loss may compound the individual’s reaction to a current loss. Dealing with problems alone, receiving help and support from others, and withdrawing altogether are possible ways of coping with the loss.
The degree of attachment and the meaning of the pregnancy and impending parenthood to the family define expectations and influence reactions if an optimal outcome does not occur. The experience of grief depends on whether the loss situation was sudden and unexpected or if there was forewarning about a problem or complication. The definition and meaning of the crisis (e.g., the nature and severity of a deformity, the finality of death, or the chronic sorrow of a defective infant) reflect the individual’s and family’s value system and previous crisis experience. The process of grief is affected by the event itself, the previous and current coping mechanisms, and the family’s definition of the event. Consideration of all of these factors is crucial in instituting appropriate intervention.
Cultural practices among families and professionals often differ (see Chapter 29). 94 For example, in some cultures, it may not be acceptable to see or hold your baby (as in some Native American cultures). In the Muslim culture, the family is the primary system of support and it is rare to see a Muslim family emote publicly. It is critical for health care practitioners to recognize cultural and religious differences to minimize misinterpretations and conflicts with families. With increasing immigration, practitioners must be able to respond with a more ethnic-sensitive approach. 20,35,63,77,104 It is essential to be creative and flexible, thus respecting families’ cultural and religious belief systems. 2,117,125 Studies show that cultural differences influence (1) parental emotional response to and perception of their infant’s illness and disability, (2) parental utilization of services, (3) parental interactions with health care providers, and (4) the ceremonies and rituals surrounding death. 11,35,63
The national association Share: Pregnancy & Infant Loss Support, Inc. has revised the “Rights of Parents When a Baby Dies” and “Rights of the Infant” (Box 30-3). These documents serve as guidelines for creation of protocols, checklists, and bereavement programs; affirmation and empowering tools for bereaved parents; and communication points for parents and care providers initiating the grief process. 85
BOX 30-3
Rights of Parents
1. To be given the opportunity to see, hold, and touch their baby at any time before or after death, within reason
2. To have photographs of their baby taken and made available to the parents or held in security until the parents want to see them
3. To be given as many mementos as possible (i.e., crib card, baby beads or bracelet, ultrasound or other photographs, lock of hair, feet and hand prints, and record of weight and length)
4. To name their child and bond with him or her
5. To observe cultural and religious practices
6. To be cared for by an empathetic staff who will respect their feelings, thoughts, beliefs, and individual requests
7. To be with each other throughout hospitalization as much as possible
8. To be given time alone with their baby, allowing for individual needs
9. To be informed about the grieving process
10. To request an autopsy; in the case of a miscarriage, to request to have or not have an autopsy or pathology examination as determined by applicable law
11. To plan a farewell ritual, burial, or cremation in compliance with local and state regulations and according to their personal beliefs, religion, or cultural tradition
12. To be provided information on support resources that assist in the healing process (i.e., support groups, counseling, reading material, and perinatal loss newsletter)
Rights of the Infant
1. To be recognized as someone who was born and died
2. To be named
3. To be seen, touched, and held by the family
4. To have life-ending acknowledged
5. To be put to rest with dignity
Modified from SHARE pregnancy and infant loss support, Available at www.nationalshareoffice.org.
ENVIRONMENT
The first step in facilitating grief work is to create an environment that is supportive, permissive, and conducive to the expression of feelings. 16,21,83,93 This type of environment does not depend on physical surroundings but, rather, is created and maintained by a warm, receptive, accepting, and caring staff. Such an environment centers its concern more on the people giving and receiving care than on the tasks of care. 58 This type of environment is nonjudgmental and is characterized by an attitude of openness and freedom. 19,99 People feel safe enough to ventilate a full range of feelings—sadness, anger, despair, and even humor—without the fear of condemnation or rejection. The staff become role models of open communication, facing grief, and feeling comfortable in an uncomfortable situation. The safety of such an environment generates feelings of acceptance and understanding so that grieving and healing may proceed.
Professional presence and support are essential to families in crisis because of the increased dependency needs that accompany grief and loss. Yet certain aspects of a conducive environment such as privacy, quiet, and comfort may be difficult to obtain in a noisy and busy perinatal setting. The recommendation to never leave the family alone must be balanced with their need for privacy and personal time alone with their infant (stillborn, ill, or dying). Simply saying “I will stay with you unless you ask me to leave so that you can have some private time alone with your child” or “Would you like me to leave for a while so that you can be alone with your baby?” offers both support and privacy. Many parents later regret not having time alone and not thinking to ask to be alone with their infant.
A quiet place away from the hustle and bustle of the routine may facilitate both attachment and detachment. The mother of a stillborn child who is quickly shown her infant in the delivery room as her episiotomy is being repaired is not in an optimal physical (or psychologic) environment. Attaching to and saying good-bye to her infant are better accomplished in a quieter and more private setting with significant others present. 64,82,110 Active participation of parents at the death of their newborn may not optimally occur in a busy intensive care unit. Rather, adaptation of hospice concepts to neonatal care provides a private, homelike room, with focus on palliative (comfort) care, rather than cure, to the dying newborn and the family (see Chapter 32). 21,96,107,108 When the family is too emotionally drained, they may elect to “say good-bye” and leave the hospital before life support is removed; the nurse then disconnects, holds, and rocks the baby so the infant does not die alone. 15,83 In some situations (e.g., chromosomal anomalies), parents and professionals may opt to provide end-of-life care ideally with hospice care at home. 74
Supportive, Trusting Relationships
A relationship with a caring individual who offers consistency and support is the foundation of a therapeutic environment. During periods of crisis, when there is a temporary increase in dependency needs and feelings of loneliness, it is an adaptive behavior to seek emotional support from family, friends, and professionals. 16,68,83 Even the crisis of normal childbearing prompts many cultures to provide a doula90 to teach the new mother and give her emotional support. For a mourning family, the relationships established with helpful professionals are more important than the physical care given.
Support, “sharing one’s ego strength with another in a time of need,”46 is particularly helpful in perinatal loss because of the threat to self-concept and self-esteem suffered by parents. Support may be as simple as remaining with the parents. “Being there” indicates not only physical presence but also an emotional availability and willingness to share their experience of loss. Often professionals, family, and friends are hampered by not knowing what to say. Usually words are initially unnecessary or do not adequately describe the moment and silent presence may better convey the message. Often it is not what is said but the mere presence of loving others that conveys empathy and support to parents and colleagues. Yet presence is not enough; meaningful interaction between parents and professionals is also necessary for a trusting relationship to develop.
The initial meeting with the professionals, including verbal and nonverbal cues, leaves a lasting impression on the family. Addressing family members by name personalizes the encounter, and a brief touch or handshake represents an extension of self, a gesture of warmth, concern, and acceptance from professional to parents. An introduction that includes a brief explanation of the professional’s role in relation to them and their infant helps orient them: “Good morning, Mr. and Mrs. Black. I’m Sue, your baby’s primary nurse. That means that I will be caring for Jason while he is here and working with you.” Orientation to the physical surroundings and technical equipment eases the transition to an unfamiliar and often intimidating hospital environment. Providing physical comfort such as rocking chairs, privacy for interaction, and sleeping facilities for parents demonstrates the philosophy of the parents’ worth and importance to their infant.
Empathy, an emotional understanding and identification with the plight of another, characterizes a helping relationship. In such a relationship, “How are you?” is asked with the emphasis on you and a genuine interest in the answer—unlike a social inquiry in which an automatic “Fine” is expected. Recognition of verbal and nonverbal cues of parental feelings (e.g., “You look tired” or “I hear that you are frustrated”) communicates that these emotions are legitimate, understood, and accepted. A willingness to help, listen, console, and give encouragement and positive feedback establishes the professional as a sensitive, responsive person whom parents will trust. Supporting any and all parental involvement, supporting damaged parental egos, and helping parents succeed in the tasks of attachment and detachment are goals of effective intervention.
A qualitative study examining maternal perceptions and experiences showed that mothers had feelings of both empowerment and powerlessness with professional care after the death of their newborn. 64 Feelings of powerlessness occurred when (1) mothers felt disrespected as a person and a mother, (2) good communication between mother and professionals did not exist, and (3) the mother did not feel treated as an individual. 64 Mothers felt empowered (e.g., more confident, able to ask questions, understood and supported) when they felt that (1) professionals were “near,” both psychologically and emotionally, (2) professionals supported the mother’s self-esteem and confidence, and (3) professionals provided empathetic, comforting support. 64
The tone of in-hospital perinatal settings is often determined by the nursing staff. Generally, residents, interns, and specialists remain for short periods and the private physician or permanent medical staff are not available on a minute-to-minute basis. Development of a safe, trusting environment depends on viewing parents as essential partners in care of their baby and not as visitors or “disruptors” of the ward routine. 22 Pleasant and relaxed surroundings convey the message of hospitality and “You are welcome here.”
Both professional and nonprofessional support systems are available in the crisis of perinatal loss. Yet relating to many people during crisis is difficult for parents. Primary care (both medical and nursing) uses the same care provider for both the physiologic and psychologic care of the infant and the family. Thus the family is able to relate to as few professionals as possible. This special caring reassures parents that a few special people love, know, and are invested in their infant. Primary care providers share with the parents the joys of even small gains and the sorrows and tears of complications or death. Professionals and parents benefit from primary care systems in the emotional and psychologic satisfaction of such involvement. Yet this involvement is not without a price of vulnerability to an individual’s feelings of loss and grief. Peer support on an individual basis or in a group setting is essential in dealing with the stress of continual attachment and loss. 32
Normal grief reactions may be facilitated by nursing and medical professionals using others (social workers or counselors) when necessary. 7,21,69,83 Collaboration and consultation with these professionals help the staff gain insight into parental and personal behaviors and appropriate intervention strategies. The staff also may benefit from the expertise of a trained counselor in dealing with their own feelings of loss and grief.
PATHOLOGIC GRIEF
Maladaptive responses to perinatal loss are indications for referral for specialized care (see the Critical Findings box on p. 917). 127 Involvement of clergy and religious organizations is often comforting and supportive to the family. 73,82,112,125 Religious rituals (i.e., baptism, prayer service, or anointing) may be advocated by certain denominations and provide a measure of comfort and hope. Often parents in crisis do not think to request infant baptism or to call their priest, minister, or rabbi. Offering to call a clergy member of their choice or the hospital chaplain may be helpful. A national survey of pastoral care providers noted barriers to providing spiritual care: (1) inadequate numbers of pastoral care staff, (2) inability of health care providers to assess spiritual needs, and (3) being called “too late” to provide all the care that could have been provided. 41 Primary care providers who have shared intimately with the parents the experience of their child’s life and death may be invited to attend the funeral or memorial service. For both care providers and parents, this may represent the final act of caring for the infant. 32
Indicators of Pathologic Grief61
1. Overactivity without a sense of loss
2. Acquisition of symptoms belonging to the last illness of the deceased
3. Psychosomatic conditions
4. Altered relationships to friends and relatives
5. Furious hostility against specific others
6. Formal manner resembling schizophrenia
7. Lasting loss of social interaction patterns
8. Assuming activities detrimental to social and economic existence
9. Agitated depression
Nonprofessional support systems such as the couple, family, friends, and parent groups are often forgotten as sources of potential help to grieving parents. In our society of isolated, mobile, nuclear families, it may be erroneous to assume that a support system exists. On the other hand, it may be unrecognized because it does not fall into a traditional definition, such as the next-door neighbor or other friend who may be more supportive (and available) than the grandparents. Biologic kinship is not the only valid criterion for a support system; an emotional kinship is the most important factor.
Because professional availability and involvement with the parents is not lasting, the professional has a responsibility to identify, foster, and facilitate a nonprofessional (social) support system. Simply identifying supportive others and expecting them to automatically help in a perinatal loss situation may not be realistic. Unless those who constitute the support system are as well informed and instructed as the parents about the situation, they will not be able to offer emotional comfort. For example, if the parents wish to talk about their loss but the members of the support system empathically wish to spare them by not discussing it, no help will be given or received.
The quality and quantity of ties one has with a social network are associated with improved health status and life satisfaction. 31,110,125 For parents experiencing a perinatal loss, the quality and quantity of ties with their social network (i.e., extended family, friends, and colleagues) may be profoundly affected. In one study, most families suffered permanent loss of relationships because others were unsure of how to react, avoided talking about the baby, or made comments that diminished the intensity of the loss. 30 Fathers especially receive little personal attention as friends and colleagues focus their attention on the mother’s grief. 30,31 Because grandparents grieve for their grandchild and may feel guilt and grief for their own child, they may be emotionally unavailable to support the grieving parents. To prevent social network disruption for grieving families, health care providers can (1) share information with families about reactions to expect and reasons for these reactions, (2) support families and enable them to rebuild their networks, and (3) emphasize and support the family’s belief in their strengths and capacities. 30,31,83
Open communication between the parents is essential in preserving and fostering a close relationship by the giving and receiving of mutual support. Sharing the experience presents the couple with the opportunity for personal growth and growth as a couple. Yet the individual experience of grief within the context of a couple is too often fertile ground for misunderstanding and resentment. 93 One study showed that disruption of a couple’s sexual relationship occurred after the death of a child. 102
Parental support groups offer their members an opportunity to discuss their feelings with others who have been through similar traumas. 93,121 Knowing how others who have experienced perinatal loss have felt and dealt with similar situations is emotionally comforting and stabilizing to parents experiencing their own loss. Parents provide each other with validation for their feelings and a sense that they are not alone in their pain. Each individual has different needs, different ways of adapting to crisis, and different ways of giving and receiving support. It is essential that professionals use techniques that are real and spontaneous and not adopt words or actions that are foreign to one’s own self. Interventions must also be gauged to the parents’ needs and pace.
In one study119 and from clinical experience, fathers state that they receive most of their support from their spouse. They report that little attention is paid to fathers by hospital staff, causing more denial and difficulty expressing their grief. So that the father’s grief is not ignored, 71 it is critical for hospital staff to address the father’s feelings when addressing parental grief. 97 Suggestions to assist fathers in their grief include implementation of all-male support groups, validation of their feelings, and asking direct open-ended questions. These may include “What are you feeling right now?” “Tell me how your day is going,” and “Tell me about your coping strategies.” Health care providers can help a father by reflecting his statements, using his name, and assisting him with expressing his feelings. Fathers should be included and acknowledged in all discussions with staff 120 so that they are not “forgotten mourners.”57 A recent study documented that family adjustment after the NICU experience improved over time for mothers but deteriorated for fathers, especially if the infant had ongoing health problems. 31 Assessing the family as a unit rather than using the mother as a representative of the entire family, being cognizant of and responsive to gender differences in coping, and being supportive of family strengths and resources are recommendations for clinicians. 31
Information
Information aids in intellectually understanding the crisis, thus facilitating a sense of control over it. Actively seeking and using information enable confrontation and mastery of the crisis. Knowledge about a situation strengthens the ego, because it enables “worry work” and psychologic preparation for expected events. Because “the void of the unknown is more frightening than the known; facts are more reassuring than awesome speculations,”17 a major role of the professional is to provide and clarify facts and information relevant to the perinatal loss situation (see the Parent Teaching box at right). 16,69 In the search for meaning that always accompanies loss, medical facts may help alleviate some parental guilt about causing the tragedy. Repeating to the parents that nothing they did or did not do could have caused this problem is reassuring. Sketchy or no information only serves to contribute to parental denial of the reality or to their fantasies of causation. 99 Confronting the crisis and realizing its real element of danger and trouble starts the process of grief by giving permission for the expression of feelings of fear, sadness, and loss.
Grief
1. Grief is a normal reaction and is expected in perinatal situations: pregnancy, abortion, stillbirth, premature birth, when the baby is sick or has an anomaly, death, relinquishment, when the birth process does not meet parental expectations, and when there is postpartal depression.
2. Grief is a staged process that occurs over time and is characterized by stages: shock and disbelief, anger, bargaining, depression and withdrawal, and eventually acceptance.
3. Grief is an individualized process and may be experienced differently by the mother and father.
4. To facilitate grief reactions, the neonatal intensive care unit (NICU) will provide a safe environment for the expression of feelings, information about the infant and the infant’s condition, and supportive, trusting relationships with health care providers.
5. Seeing, touching, and holding the baby are as important to the parents of a sick or dying infant or an infant with an anomaly as they are to the parents of a healthy infant.
6. When an infant dies or is dying, parents and infant(s) have the right to interact with each other, to create memories, to involve extended family and friends, and to engage in specific religious and cultural practices.
7. Parents and families are informed about the grief process, encouraged to support and care for each other, and encouraged to identify and rely on social support systems (e.g., extended family, friends, professional support services).
Because the family as a unit, composed of the individual members, must deal with perinatal loss, professionals should encourage and support open, interfamily communications. Keeping secrets, especially between the parents, should be discouraged because this eventually undermines trust and promotes asynchronous grief work. When parents are given the same information and talk with each other about their loss and their feelings, more synchronous grief reactions develop. 58 Telling parents together with the infant present prevents misunderstanding, misinterpretations, and “shading” of information to one parent. 82 Informed parents are better able to share their experience with each other and to participate in joint decision making with the professional. 6,14
The questions “When to tell” and “How much to tell” the parents often arise. Parents should be told as soon as possible about perinatal complications or problems. 16,58 Receiving this information at the earliest possible time helps parents establish trust in the care provider, appreciate the reality of the situation, begin the grief process, and mobilize both internal and external support. Information must be given in its entirety, because attempts to “spare” parents by staging the truth serve only to undermine their trust in professional credibility. The couple’s relationship also may suffer if one parent colludes with the professional in a conspiracy of silence. This is best illustrated by the following incident:
To spare a diabetic mother from the truth about her infant’s congenitally absent limbs, the physician and the father decided to tell her about his missing legs but not the missing arm. On arriving to transport the baby, the nurse asked if the mother had been told. “Yes” was the response, so she took the infant to the mother’s room before transport. As she uncovered the infant, the mother gasped and looked at the physician and the father and said, “You lied to me. You didn’t tell me about his arm, too.”
When given the unedited truth, parents can face reality and begin the grief process without fear that something else is the matter that they are not being told. The individual’s stage of grief influences not when or what will be said but how the information will be given and received. During the initial stage of shock, information, if processed, is processed slowly. 58 Often events take on a foggy, dreamlike quality so that sensory information remembered is not believed. Yet to give no information only perpetuates this frightening feeling. Communication to those in shock and denial must proceed simply, slowly, and with much repetition and reinforcement. Giving information once does not ensure that it will be retained or understood. Repetition by the professionals is necessary for gradual acceptance of the reality of the situation. 6,14 This may be a nuisance for the professional who has already given the information and wonders why the parents cannot remember it. Parents are so shocked they do not hear what is said, and information must be patiently repeated. Even though an early contact with parents almost ensures they will be in a state of shock, the tone and content of the first meeting are not forgotten. 16,58 Initial information about the infant and his or her condition may have long-term effects on the parents’ ability to attach or detach. In the past, parents were given a pessimistic outlook with the belief that “It will be easier for them. They won’t get so involved.” Negative descriptions and initial pessimism only increase the amount of grief and detachment while effectively blocking attachment behaviors. If the sick or defective infant survives, the parents may have detached to the point of, at least emotionally, burying him or her. Knowledge of better survival rates and the quality of survival enables a truthfully optimistic outcome for many sick neonates. Therefore information must be given clearly (not medical jargon) with a minimal focus on possible complications and medical odds. 58,128
Volunteering information to parents is essential, but encouraging their questions is equally important. As the normal mechanism for adapting to crisis and gaining mastery over a situation, questions help the professional “start where the parents are” and begin communication with their concerns. Questions and comments unrelated to the discussion may indicate either failure to comprehend or failure to send the information clearly. 128
Direct questions deserve direct answers, because they indicate a readiness and desire for information. Indirect questions or comments by the parents may indicate concern about their own infant that cannot be directly expressed. “Baby Stevie (who died yesterday) had severe respiratory distress syndrome, didn’t he?” The parents want to be reassured that their infant will not die, too.
During the crisis of perinatal loss, interpersonal communication is difficult. Therefore as few professionals as possible should relay information to the parents. Primary care providers (nurse and physician) should coordinate and provide continuity in giving information to parents because individual care providers will supply information about the same topic in different ways. 22,83 The use of varied terms, inflections, and attitudes by a multitude of professionals becomes a monumental source of confusion and anxiety for parents. A trusted relationship14,16,19 with a primary nurse and physician through whom all communication flows minimizes unnecessary anxiety and concern for parents. It is essential that the nurse (or primary nurse) be present and assist the physician in communication with the parents. Any anxiety-producing information (poor prognosis, complication, or impending death) may not be heard or understood initially by the parents. The nurse must know exactly what information was given and how the parents were given this information. After the physician departs, the nurse must be able to offer clarification, explanation, and support to the distraught parents. Nothing is more distressing than finding a crying, upset mother who is unable to relate what the physician said, why she is upset, or even if she understood what was said.
No family or parent should have to wonder and worry about a dreaded or feared outcome without being given the proper information. If the primary care physician is unavailable to speak with the family, then someone from the health care team must assume this responsibility. No mother whose infant is ill, deformed, or dead should awaken from an anesthetized birth to find her physician absent and the nurses unable to answer “How’s my baby?” A plan of action for telling individual parents must be decided and agreed on by all care providers.
Parents are interested in the daily (or hourly) progress of their infant, including both positive and negative developments. A crisis or negative development in an infant’s condition is important for parents to know about as soon as possible. They are then able to participate and care for their infant through the difficulty and to trust professional communication. Parents should have unlimited access to phone or personal contact with the staff in the perinatal care setting. Phone calls to the hospital from concerned parents should be possible any time of the day or night. The knowledge that information about their infant and access to a caring professional are available at any hour often is enough to comfort parents of a critically ill infant.
Lactation suppression for the mother of a dying newborn often has been a forgotten aspect of care. 76 Engorgement creates a feedback mechanism to the maternal brain that leads to cessation of milk production; however, painful engorgement should be avoided. Using a breast pump to remove enough milk to relieve pressure and discomfort but not enough to empty the breasts will gradually result in a decrease in milk production. If the mother pumps till she is comfortable, gradually prolongs the intervals between pumping, and pumps for shorter periods, lactation gradually is suppressed. Use of a well-fitting and supportive bra relieves the discomfort/pain of heavy breasts. A recent study comparing the use of breast binding to a supportive bra found that the breast-binding group had greater breast pain/tenderness, leakage, and use of other pain-relief measures; the study recommendation was to discontinue breast binding for the more comfortable and efficacious supportive bra. 111 Mothers who have pumped and stored breast milk may wish to donate it to a mother’s milk bank. A mother also may wish to continue pumping to be a human milk donor. These options should be sensitively discussed with the mother of the dying infant.
ENCOURAGING EXPRESSION OF EMOTIONS
Because grief is an emotional reaction to loss, expression of these emotions is necessary for grief work to begin and proceed. Verbalizing thoughts and feelings provides an outlet for the intense emotions accompanying grief and signifies to others that emotional support is needed. 16 For some, the open expression of emotions may be difficult because of influence from their culture, gender-specific roles, and social status. Yet the containment of intense feelings uses a great deal of emotional and physical energy that could be more productively used in moving on with the grief work. Those who are stoic and noncommunicative have symptoms of grief for a longer period than those who freely express their feelings and emotions. 9
Experiencing the loss of an infant initiates an “ambivalent transition” into motherhood in a short period. 65 These women often feel totally confused, with broken expectations and elusive grief: “Have I or have I not become a mother?” Supporting families provides them with an opportunity to talk about their infant, confirming the baby’s life as important, although short. This process assists parents to attach and subsequently begin the grieving process. 126
Talking about the loss helps parents validate and assimilate the experience. Timing and events are clarified, including forgotten details, by discussion with each other and with their care providers. Confronting the reality enables them to work through the shock and disbelief, verbalize their fears and disappointments, and begin to cry and grieve. Expression of feelings gradually permits a clarification of the meaning of the loss to the parents. Talking lightens the burden of loss, because every time the experience is shared with another, half of the experience and the accompanying emotions are given away. Telling, retelling, reviewing, and reliving the experience are all necessary ways to understand and gain mastery over a frightening and most often unexpected situation. 16
Verbal and nonverbal cues tell professionals where the parents are in their grief process. To elicit feelings, the professional may verbalize his or her own perceptions and observations:
• “Mrs. Green, you sound tense (upset, tired) today.”
• “Mr. Brown, you look worried today.”
• “I’m sorry that your baby died.”
These statements indicate the listening ear and observing eye of one who cares. They set the stage for communication: “It’s okay to talk with me about how you are feeling, because I acknowledge your pain.”
Feeling scared, alone, and out of control, parents often deny their feelings under direct questioning. Thus “Do you think you did or didn’t do something to cause your baby’s problem?” may be answered negatively, even though parents are consumed with guilt. Direct questioning places parents in an awkward and vulnerable position of revealing their most personal doubts and fears. Direct questions may be reworded with safer and more indirect statements:
• “Most parents feel overwhelmed and sad when their baby is sick.”
• “Many parents wonder if the cause of their baby’s death is something they did or didn’t do.”
• “It is helpful to many parents to talk about their doubts and fears. These feelings are common and normal in such a difficult situation.”
The professional gives parents information about the feelings and emotions commonly felt in similar situations. Because there is safety in numbers, if “most” or “many” parents feel this way and it is expected, then it might be safe to share their feelings. Validating parents’ reactions as appropriate reassures them that they are not crazy. With this type of invitation, the feelings may be free to come spilling forth or the parents may need time to establish a relationship with this professional before they are ready to talk about such personal emotions.
Empathetic actions and comments may open communication pathways with parents. 16 A professional presence that is warm and caring may facilitate more communication than any words. Touching or holding grieving parents may help feelings be expressed. Nonverbal cues such as nodding, direct eye contact, uninterrupted attention, and the physical closeness of pulling up a chair and sitting down give positive feedback to verbal communication and indicate active listening by the professional.
Crying is the expression of feelings of sadness, sorrow, and intense longing that accompany the pain of loss. 61,128 A healthy catharsis, crying should be expected and encouraged in any loss situation. Yet the cultural, gender-specific, and professional taboos against crying have defined it as an unacceptable and inappropriate response and one that should be suppressed. Because tears are healing and therapeutic, professionals must learn to be comfortable with the crying of others. “Don’t cry” is often heard from those attempting to comfort grieving parents (or colleagues). This is an admonition against the behavior rather than an empathetic comment. “It’s okay to cry” or “Go ahead and cry; let it out” gives permission and acceptance to the behavior and the need for it.
By expecting tears, providing a safe environment for their expression, and encouraging the behavior by words and actions, the professional may facilitate crying in both mothers and fathers. Too often, tears are blocked in a relationship in which one partner (usually the man) is expected to be stoic and in control, whereas the other’s (usually the woman’s) tears are defined as too upsetting or difficult. Because the ability to cry is a healthy response, the couple must be encouraged to use this outlet together.
In the past, crying in the presence of patients and their families was defined as “unprofessional.” Yet the cool, controlled exterior defined as “professional” was seen by others as noncaring and nonfeeling. When the professional cries with the parents, it is an acceptable expression of genuine emotion, a demonstration of empathy, and a role model of the appropriateness of tears given the situation. Parents do not define the tears of care providers as weak or unprofessional. Rather, they feel a special bond of love and care with professionals who have been free enough to share their grief. 16,83,93 Instead of relearning that crying is acceptable, many parents and care providers must learn for the first time.
Talking and crying about the loss are easier to facilitate than is the expression of anger. 47 Because of the social expectations of dependency of the patient role and real or imagined consequences of retaliation (against the infant or against job status), perinatal care settings are not safe environments for the expression of anger. Parents (and colleagues) will be able to vent anger only in an environment free of punishment or retaliation for their behaviors. It is the responsibility of the professionals to create an environment that allows open expression of negative criticism and anger.
SEEING AND TOUCHING
Seeing and touching are as important to the parents of a sick, deformed, or dead infant as they are to the parents of a normal, healthy one. In the past, fear that seeing a deformed or dead infant would intensify grief and be overly upsetting resulted in no contact between parents and their newborn. Despite the fact that many mothers wished to see their infants, the prevailing practice was to discourage and prevent it. Often no information, including sex or physical characteristics, was given to grieving parents, who were left to fantasize about their newborn’s problems or cause of death. More recently, research and practice indicate that parental contact with the infant does not cause “unduly upsetting immediate reactions or appear to result in pathologic mourning.”56
Recently, researchers in the United Kingdom have evaluated mothers and fathers who have seen and held their infants after stillbirth. In several of their studies, they have correlated posttraumatic stress symptoms in both mothers and fathers114,115 and disorganized maternal-infant attachment51 in subsequent pregnancies to seeing/holding their stillborn infant. While remarking that seeing/holding the dead infant is culturally entrenched and highly valued by parents, these researchers warn that this practice is associated, in their studies, with psychologic sequelae and that these practices were based only on clinical impression without empirical evidence of benefit. 6 However, other research cited in Table 30-1 shows how this small sample of well-adjusted and low-grieving parents valued holding their infant, being present at the time of death with family/friends, and keeping mementoes and the memory of their child alive. 14 The sequelae of seeing/holding a stillborn and the sequelae of seeing/holding a live infant who has died may not be similar; clearly more research is necessary.
The British researchers, 6 who found psychologic sequelae of parental contact with their stillborn infant, state that many parents experience great meaning and treasure the memory of time with their dead infant. They concede that some parents would choose to have contact with their dead infants, regardless of potentially harmful outcomes. They also state that parental decision to see/hold the dead infant may be heavily influenced by attending staff who may expose reluctant parents to their dead baby. Clearly, the decision to see and touch their infant is ultimately a parental one. 6,128 Making decisions for parents is not the professional’s role; making decisions with parents is the professional’s role. Each parent must make the decision for himself or herself; neither may decide for the other. Altruistic others, such as professionals, the spouse, or other family members, must not usurp the right to individual decision making. Often, in an attempt to protect the mother, the father or the professional decides that she should not have contact with her infant. They either actually discourage it or do nothing to facilitate it. Mothers who have not seen their infants always know who prohibited it. The couple’s relationship may suffer irreparable damage if one decides for the other, even if the motive is altruistic. The professional’s role is to facilitate a healthy decision by each parent so that their individual needs to see or to not see the infant are met.
Parents may not realize that seeing and touching their infant is an option, or they may just be too overwhelmed or afraid to ask if it is possible. Instead of waiting for parents to ask, the professional care provider takes a more active role by offering the possibility to the parents: “Would you like to hold your baby?”
Time is often necessary to make the decision, because initially parents are ambivalent about seeing and holding a deformed or dead infant. Most mothers and fathers want to see their child but fear what they might see and how they may feel. The care provider may alleviate the parents’ ambivalence by acknowledging that being with the infant will be difficult but that the professional will remain with them unless asked to leave. The emotional support of the physical presence of an empathetic professional may allay the fear of becoming out of control. The professional can reassure the family by explaining what they will see before they hold their infant. Making such a crucial decision in the initial stages of loss is difficult. Giving parents information about the positive aspects of seeing and holding the infant in facilitating their grief process helps make their decision an informed one. 96,128
Seeing the infant brings the dreaded impossibility of perinatal loss into stark reality. 128 Parents confirm with their own eyes that the infant is alive or dead or normal or abnormal. Contact enables claiming behaviors and identification of the infant as their own. While holding their infant, parents examine it and begin to recognize familiar family characteristics: “She has my long fingers and her father’s red hair.” Even small, severely deformed, or macerated infants can be recognized and claimed by the parents as part of their family. The normal, endearing characteristics that identify the child as “mine” are remembered.
Parental contact confirms the infant’s own reality and eliminates the prenatal fantasy of the expected child. For the parents of an infant with an anomaly, grief work about the fantasized perfect child may begin so that the actual child may become the object of love. Early and frequent contact between the parents and the infant encourages a realistic perspective of the infant’s problems. A stillborn or aborted fetus may be physically normal rather than the deformed infant imagined by the parents. Seeing the infant allays doubts and fears about the infant’s normal state and about the parents’ ability to subsequently have a normal child. 99 Seeing and touching enable parents to grieve the infant’s reality rather than a feared and dreaded, and thus more frightening, fantasy. It is easier to grieve a real infant than a mystical, dreamlike fantasy of the infant. 58
Whether the ultimate decision is to see or to not see the infant, the professional must honor and respect that choice. 128 Cultural taboos against viewing dead bodies may preclude some parents from seeing and touching their infant. Yet many such cultures support their members by formalizing the grief process in sanctioned ritual and ceremony. For those parents who decide to not see and touch, the professional should reassure them of their infant’s normal condition (e.g., “He had 10 fingers and toes.”). Describe the infant in as much detail as necessary to give parents a mental picture. Include gender, size, hair color, skin, weight, and distinguishing characteristics. A simple, realistic description of any anomaly is also helpful, because the fantasy of the defect is worse than its reality.
Adequate preparation for the first encounter with their infant includes a description of everything parents will see, hear, and feel. 128 Verbal preparation for viewing an infant with a congenital anomaly includes not only a simple description of the abnormality but also the infant’s normal characteristics. Seeing a picture of the abnormality first may help parents prepare for seeing their infant. Remaining with the parents at the initial visit, the professional describes the anomaly and points out normal findings. Focusing by parents on the normal familial characteristics helps in attaching to the less-than-perfect baby. Although parents of a dead, deformed infant view the abnormality, they often focus on the normal traits and remember him or her not as “monstrous” but as beautiful.
For those who have never seen a dead body, the mind may invent frightening images and sensations. Certainly, “dead” is associated with the temperature sensation of cold. However, a newborn who has been placed under a radiant warmer or in an incubator may feel warm rather than cold shortly after death, hence the statement by a mother, “You couldn’t be dead. You feel so warm.” The professional must touch the infant and prepare the parents for the tactile sensation of warm or cold: “The baby will feel warm to you because she (or he) has been under the radiant warmer.”
To prepare parents for seeing their infant, the professional must observe the baby. Color, skin condition, and size must all be described and are not shocking with adequate preparation: maceration—“peeling of the skin”; peripheral shutdown—“the blue-white discoloration”; and the small size—“as long as the length of my hand.” Any equipment that must remain on the body should be described and explained before viewing. Even an umbilical cord clamp may cause concern in a parent who has never seen one. The reason for not removing equipment also must be explained. Respectful care of the infant’s body after death shows respect for the person of the infant and for the grieving parents. Attention to details such as wrapping the infant in a blanket rather than a surgical drape or towel, cleaning the infant, and holding the infant in a cuddling position indicates care and concern.
Parents whose infant has died, is deformed, or is ill proceed with attachment behaviors of seeing and touching in the same manner as parents of normal, healthy infants. 58 Touching is important, but the distinction must be made between touching and holding. Cradling one’s infant is quite different from merely touching with a hand. Holding the infant, whether healthy, sick, or dead, for the first time is a momentous event. Touching the infant who has died is not sufficient; parents must be given the opportunity to hold and cuddle the child before, during, and after death. Other parenting behaviors, such as bathing and dressing their infant, also should be offered to parents. 52,55,108
Parents of a dead infant may need more than one chance to see and touch the infant. The first time, they attach to the reality of their infant. Subsequent encounters allow a final chance to see and hold their child. Parents have described the initial encounter as saying “Hello” and the subsequent one as saying “Good-bye.” Some parents may be able to accomplish closure with one visit, whereas others who might benefit from a final visit may not ask or think to ask. Offering another contact with their infant leaves the decision with the parents.
The emotional effect of seeing the infant requires support, time, and permission to cry. Attaching is a process that occurs over time. Providing parents sufficient time with their infant takes precedence over paperwork, ward routine, or taking the infant to the morgue. Parents have indicated a need to hold their infant for a longer time and not feel pushed by care providers. 52,65 Even infants who have been removed to the morgue may be returned if parents need more time and contact for detachment. 64
When an infant dies, opportunities for memories are limited. Professionals have the responsibility of helping parents make memories so that they will have a tangible person to mourn. Encouraging parents to name their infant gives the infant a separate identity, which helps facilitate the grieving process. Tangible mementos may include photographs, handprints and footprints, a lock of hair, hand/foot castings, 54,83,116 measurements of the infant, identification bands, the blanket the infant was wrapped in, a blessing or baptismal certificate, and birth and death certificates. Parents find most beneficial the interventions that acknowledged the infant (e.g., photographs, holding the infant, and receiving personal mementos). 14,52,55,64,86 Even when parents say they do not want mementos, the mementos should be kept in hospital files and the parents made aware that they will be available to them in the future if they want them. 64 Taking pictures of the infant, obtaining other mementos, and telling the parents that such mementos will be available to them on request not only respect their immediate decision to not see or have information on the infant but also provide a mechanism for them to “know” their infant at a later date if they wish to do so.
Before an infant is transported to a newborn special care unit, photographs should be taken and given to the parents to promote bonding. If the infant remains hospitalized for a long time or requires surgery, pictures taken at weekly intervals or before and after surgery can help confirm the reality of the child’s condition and progress and assist with bonding, as well as the grief process. Despite the outcome, parents will appreciate some lasting record of their child’s life.
The staff who provide emotional support for parents must also receive support from each other. Expecting the staff to immediately return to work is unrealistic. Such an emotional experience takes time and space for decompression, which is facilitated by the use of exercise, crying, and being alone for quiet time. 32 A recent study of staff and family perceptions of palliative care showed that interdisciplinary staff felt inexperienced in communicating with families about sensitive end-of-life issues and inexperienced in pain management and received inadequate education and support to deal with these families and their own personal pain. 21
OPEN VISITING AND CAREGIVING POLICIES
Perinatal care settings with open visiting and caregiving policies foster a shared family experience and support from others. Regardless of the type of perinatal loss, no mother should experience it alone—a spouse, friend, family member, or identified supportive other should remain with her. 52,120 Members of the mother’s support system will also need an outlet for the expression of their grief.
Women suffering the grief of perinatal loss should be given a choice about their room assignment. Arbitrary removal from the obstetric unit may deny the mother’s maternity: “Am I a mother or not?” It also may escalate her feelings of failure, guilt, and worthlessness as a woman and a mother. Because she did not produce a normal, healthy infant, she may feel punished and banished from the maternity area by isolation on another floor. Her care may be entrusted to those without expertise in the physiologic and psychologic care of the normal postpartum period, much less a postpartum complicated by loss. Placement at the end of the hall far from the nurses’ station, with the door closed and no company from staff and family, only increases her feelings of loneliness and isolation. Yet being on a happy maternity floor with normal, healthy infants and their mothers may be an exceedingly difficult and constant reminder of her loss and even complicate her recovery. 56 Information about the advantages and disadvantages of staying or leaving the maternity ward should be given by the professional. The mother, knowing what will be helpful, makes the decision. 128
The alternative to maternal hospitalization is early discharge as soon as medically possible so the mother may join her infant when the infant has been transported to another hospital. Early discharge also facilitates an easier mobilization of supportive others in the familiar surroundings of home. Removal from the constant reminder of one’s failure (i.e., other healthy infants) may let the grief work begin. 128 Early discharge is not therapeutic when the professional assumes there is a support system to provide care and no one is available. Without a plan for follow-up care and contact, early discharge merely relocates the problem.
Caregiving is as important for the parents of a sick, deformed, or dead infant as it is for the parents of a normal infant. Open visiting and caregiving policies increase interaction between the parents and their infant by actively involving them in the reality of their child’s illness, deformity, or impending death. Even if the child lives only a short time, parental access and taking care of the infant complete the attachment process and enable them to begin the detachment of grief work. Even minimal caregiving helps parents overcome their sense of helplessness and be comforted by “We did all that we could have done. We cared; we made a difference to our baby.” Active parental involvement decreases poor outcomes such as aberrant parenting styles, attachment problems, and unresolved grief. 14,58
The loneliness and isolation of death are decreased for both parents and infant when they are together at the time of death. Parents are often comforted and relieved that their fantasy of the agony of the death scene is not borne out in the quiet, peaceful reality of death. 58 Having experienced the beginning of life together, parents who are present at the ending of life can feel a sense of closure and completion. Parents who can share even a brief life with their baby and the moment of death can face death’s finality knowing they did not abandon their infant but provided him or her love and care. 64 Parents who are not present at death may take care of the infant afterward by seeing and holding him or her.
Parents should be given the opportunity to make final plans for their deceased infant. 83 The planning will help them face the death and facilitate the grief process. For many parents, this is their first experience with death and making final arrangements and they are not aware of the options. It is helpful to provide the family with detailed, specific verbal and written information about cremation, burial, funeral, or hospital disposal. 18,52,83
A funeral may be chosen for religious reasons or as a declaration of the fetus or newborn as a person befitting burial rather than disposal. Burial leaves a specific place of remembrance and recognition that this infant lived. Care for the infant after death may include funeral arrangements, such as choosing the clothes or bathing and even dressing the infant. If parents choose not to have a funeral, they may wish to have a memorial service or do something special, such as plant a rosebush or tree, in memory of their infant. Regardless of their decision, the birth and death of their baby constitute a life event for the family, and one must recognize it.
AUTOPSY87
For parents who experience a stillbirth, spontaneous abortion, or neonatal death, knowing why the infant was deformed or died eases their recovery from grief. 58 In the search for a cause, many parents blame themselves for doing too much or too little to favorably influence the outcome. A recent study showed that neonatal autopsies reveal important new information in 26% of the cases. 12 Knowing why the infant died or the converse, that not even the “experts” know why the infant died, may help assuage their personal feelings of guilt and failure.
Approaching the family for permission for an autopsy must be done by the primary care providers (physician and nurse) with the utmost tact and respect for the family’s feelings. Too often the permission for autopsy is denied because of the way the subject is broached by professionals. Telling the family about their infant’s death in one breath and asking for an autopsy with the next breath is not appropriate. Parents need time to deal with the reality of the death, including seeing and holding their infant and being with each other and supportive others before they are even ready to think about an autopsy. Consideration of the family’s feelings and stage of grief greatly enhances communication with the professional. Reasons for the autopsy, including a possible answer to the question of why their infant died or was deformed, are important to discuss in a relaxed and unhurried manner. 3 Parents may feel rushed to make a decision without clearly understanding the advantages and disadvantages and resist the emotional topic of a postmortem examination. Time for discussion with an empathetic professional, as well as between themselves, facilitates an informed parental decision; sometimes consultation with a religious leader is necessary.
The professional who receives permission for an autopsy is then obliged to discuss with the parents all findings. 3,56 This may entail more than one meeting with the parents, because they should be informed of the findings as soon as they are available. 82 Therefore the professional may meet with them within 24 hours of completing the autopsy to discuss gross and preliminary findings and again 2 to 8 weeks later to discuss microscopic results. 58,72 Autopsy data may indicate either a condition that has implications for subsequent pregnancies or one that has little chance of recurrence. 3 The need for genetic counseling for future pregnancies may be evident from autopsy results. 87 Discussing the results with the report in hand and offering parents a copy for future reference are also important.
ANTICIPATORY GUIDANCE
Encounters with parents after the death of their infant give professionals the opportunity for anticipatory guidance/information about what to expect from themselves and from others. 52,55 Reactions to perinatal loss differ markedly, so family, friends, and acquaintances may not act as parents might expect. Some will be supportive and emotionally empathetic, especially if they have suffered a perinatal loss. Others will be uncomfortable and, not knowing what to say or do, may choose to avoid the couple and never mention the loss, even in future conversations. Those who are unaware of the loss may question the newly nonpregnant parents about the new infant. These inquiries are both awkward and painful.
Knowledge of the universal feelings and behaviors associated with grief gives comfort and relief to parents. Knowing what to expect from grief (i.e., how it progresses and how long it takes) is valuable to those who are or will be experiencing it. 43,55,58,83,128 Knowing the stages of grief and that the accompanying behaviors and emotions are normal decreases the feeling of “going crazy.” Recovery from the loss takes time and cannot be hurried or ignored. The most difficult time is immediately after birth and the first few months after the loss (2 to 4 months). 48 The emotions of grief begin to lessen toward the end of the first year.
Parents should be encouraged to support and care for each other in their time of loss. Professionals should advocate mutual support by a free expression of feelings and emotions between the parents. Although parents need each other during grief, they also need an identified support system with whom to talk and cry. Reaching outside of the nuclear family to friends, extended family, and professionals should be encouraged. 14,31,83 Professionals have a responsibility to ask to whom parents turn for help and support in a crisis. If there are no identified supportive others, parents must know whom to call for help in the initial bereavement period.
Anticipatory guidance is also essential at the discharge of an infant with an anomaly, a preterm, or a previously ill newborn. Knowing what to expect when going home with an infant with a defect or an infant who has been hospitalized for months makes the transition from hospital to society easier for parents. Evaluation of the grief process, the attachment level of the parents to a less-than-perfect infant, and the presence or potential for postpartum depression (see Chapter 29) is vital.
LONG-TERM FOLLOW-UP CARE
Follow-up care and contact with professionals are needed by grieving parents. 14,31,52,82,83 A recent study of bereaved parents highlights their needs for follow-up: (1) appointments should be scheduled with the neonatologist soon after the baby’s death and certainly within 2 months, even if autopsy results are unavailable and (2) in a setting away from the hospital; (3) families value the professionals’ efforts to determine how they are coping; (4) families value full, frank, sensitively delivered information and reassurance that enable them to understand what happened and assess their future risks; and (5) families do not want false reassurances, half truths, and broken promises. 72 Follow-up meetings function as a catharsis for parents, as well as an opportunity for assessment, counseling (psychologic and genetic), and possibly referral. Primary care providers (physicians, nurses, and social workers) from the perinatal care setting may provide follow-up. One study documented a significant decrease in the intensity of a mother’s grief after stillbirth when she received one telephone call from the physician. 81 For the family, relating to providers with whom a relationship has been established may be easier than establishing a new relationship with a stranger. 14,19,83 However, being with those who are associated with the loss event may be uncomfortable for the parents at the height of their grief. For the professional, the ability to continue to be a source of help and comfort to families with whom one has established a relationship may help complete their grief reactions. Maintaining contact with the family may be painful as the professional relives the feelings of grief and loss associated with sharing their tragedy. Although painful, this re-experience of intense feelings gives both parents and professionals another opportunity to work toward grief resolution.
When and where to provide continuing care for families are crucial questions. Contact in the perinatal care setting both at the time of death and daily until discharge provides immediate care. However, when discharged, too often the family returns home alone to face weeks and months of unsupported and lonely grief. Without feedback about their normal reaction and society’s expectation that they will shortly be “back to normal,” they are abandoned to their emotions. They suffer in silence and often drift apart in their misery. With their support system withdrawn but still feeling overwhelmed with grief, parents describe the period between 2 and 4 months after the loss as the most difficult time. 56 At 2 months after perinatal loss, parents show increased symptoms of anxiety and depression that are reduced by 8 months but still higher than in parents not experiencing perinatal loss. 118 Follow-up care from professionals is most meaningful and needed by parents during this period when they feel deserted by previously supportive others. 52 Parents experience a need for spiritual support weeks and months after the loss. Meeting with families sooner (within weeks of their loss) may alleviate the effect of decreasing support as the months go by. The professional who acknowledges the withdrawal of others but can be relied on to be available provides the parents with the emotional anchor of long-term care and support.
Breaking appointments or continually not being available may be resistance to follow-up contact with the professionals but also represents a reluctance to return to the perinatal care setting with its painful memories. A visit from the professional in the home provides a nonthreatening, familiar environment for follow-up care. The more comfortable home environment enables assessment of family interactions and facilitates communication at the “feeling” level.
Each family member and the family as a unit must be assessed for their place in the grief process as follows:
• In what stage of grief is each family member?
• Is anyone “stuck” in a stage of grief?
• Are behaviors appropriate for normal grief reactions, or do altered behaviors represent pathologic grief reactions?
• Do altered behaviors warrant referral for further treatment and evaluation?
• Do the caregiving and attachment behaviors of the parents reflect resolution of grief over loss of the perfect child and adoption of the less-than-perfect child as the love object?
Just because everything was progressing normally at previous encounters does not mean that it should be assumed to still be so. As the flood of initial grief subsides, problems and questions that were not considered suddenly become of great concern. For the first time in months, the regressive behavior of siblings not only may be noticed but also may be extremely annoying to parents. The beginning of grief resolution may allow future projections such as “When can I have another baby?” or the dread of the painful anniversary of the loss.
Referral to public health nurses or visiting nursing services in the community for follow-up care is appropriate. However, a written referral alone is not enough. Involving them in the hospital care and discharge planning is essential for a smooth transition to home care. Having the new professional meet the family in the hospital with the primary care providers facilitates trust transference from the familiar to the unfamiliar. Traditionally, home care providers have been involved in care of normal mothers and infants in the community. Involvement in perinatal loss situations requires knowledge about the process of grief and willingness to share the grief of the parents. Because these may be new skills for many, continuing education programs that teach the theory and skills of effective intervention help the professional be more comfortable with a perinatal loss situation.
Additional expertise may be warranted when the professional recognizes signs and symptoms of pathologic grief, delayed or absent grief, or concurrent multiple stresses or losses. Parents may not be ready for genetic counseling, infant stimulation programs, or financial programs until months later. Between 3 and 6 months after their loss, parents may be ready to reach outside of the nuclear and extended family for help and support for the first time. 93 Suggesting a local hospital support group or the local chapter of a national support organization may at first be met with resistance. Leaving the names and phone numbers of such organizations ensures that the parents have the information at their disposal when they are ready to use it. Until their own support system has withdrawn, parents may not be ready for a support group of other parents. 93
Throughout this section, examples of what to say and how to say it have been used to illustrate helpful interventions for grieving families. It is essential to state that there are no “scripts.” Parents do not say one thing and the professionals answer with a parroted response. Each encounter is a unique situation consisting of distinct parental and professional personalities. Each situation must be evaluated separately and individual interventions instituted. 52,83 It is recommended that the professional learn by observing an experienced colleague with grieving families and that the professional “practice” with role playing and situation solving before actually attempting to intervene with the parents. Use of formalized education about grief, loss, and bereavement is also recommended for health care providers. 43,69
Innovative bereavement programs have been developed to provide families and staff with support and follow-up care. 35,52,93 Such programs35,52 provide education and assistance to the health care providers who care for the family at the time of their infant’s death. There is follow-up care to the family for up to 1 year after the death of their infant. 52 These programs provide the needed support, education, and help to families, as well as to staff. Use of a couples-oriented program enables the following93:
• Participation in the group at 3 to 5 months after the loss when most other support systems have ceased
• Ability of partners to share with the group and each other gender-related differences in grief experiences
• Opportunity for men to share and hear about other men’s feelings and coping skills
• Couples to learn to tolerate their differences in grief processing and to process their grief together
• Enhancement and preservation of the couple’s relationship
CHILDREN AND GRIEF
Explaining and helping a surviving child to understand the loss of an infant is an enormous task for parents. 108 Facilitating the child’s normal feelings of sadness, worry, and anger after a loss may be difficult for parents who fear being flooded with their own emotions. Unresolved grief from the parents’ own childhood may prevent the expression of grief by their children.
To maintain the myth of childhood (innocent happiness), children are often shielded from any knowledge about death, even when it is an inevitable event in their lives. Thus children are prevented from full realization, validation, and expression of their feelings and emotions. They cannot formalize and express their grief over the loss of a significant person.
Even though adults are encouraged to cry, talk, and gradually understand and integrate their feelings of grief, no one helps the child deal with the same frightening feelings. No one discusses the loss with the child, because “He might cry” and because of the adult’s inadequacy and lack of understanding of how to respond and what to say. No amount of secrecy or denial of the situation will hide the fact that the child is being excluded from an important family event.
Attempts to protect children from feelings of grief and mourning because of death or other important losses isolate the child. Age and developmentally appropriate explanations include the child in the family’s experience, rather than separating and excluding him from what is happening. Shielding children from the knowledge of death denies them the reality of life and the opportunity for personal growth and mastery of the experience. Like the subject of sex, death is taboo for children.
A child’s grief and mourning in response to perinatal loss depend on his cognitive and developmental level, the extent of prenatal attachment and expectation about the infant, the degree of ambivalent feelings, and the response of his or her parents to the death. Because the child’s understanding of death differs from that of adults, knowledge of the stages of growing awareness is essential for both parents and professionals working with children experiencing grief (see the Critical Findings box on p. 929). 1 Regardless of age or developmental stage, the universal fear of childhood is the fear of separation and abandonment. For a young child (younger than 5 years), the loss of the infant is experienced indirectly through parental grief. A young child reacts to the emotional withdrawal of grieving parents and fears loss of them (and their love).
Although children at different developmental stages have their own conceptions of death, adults must provide them with the facts about the situation in language that they can understand. They may benefit from guidance by the nurse, social worker, or other health professional about beneficial approaches to facilitate the child’s grief work. The professional serves as a resource, role model, and support system to parents caring for their surviving children. Printed materials are also available to assist parents in helping their other children understand death (see “Resource Materials for Parents” at the end of this chapter). Age-appropriate storybooks concerning death can facilitate grief discussion and elicit questions and feelings from children.
Just as grieving adults need repetition, children need repeated explanations and discussions about the loss. Constantly in a state of developmental flux, the child attempts to view the loss in new ways as a result of increasing maturation. Asking questions (usually at inopportune times) and making comments about the infant are ways the child continues to process the experience, often long after the parents have completed it. These questions and comments may seem endless and resurrect the parent’s own grief. The child’s inquiries must be encouraged and supported so that he or she knows that talking about the loss or death is acceptable. Exploring the child’s feelings for fears of causation, guilt, or the wonder if “death is catching” enables them to be dealt with appropriately. Truthful discussion with the child dispels the worst fears and fantasies and replaces them with reality that is “not too horrible to discuss” with parents. If the cause of the infant’s death is known, it is explained to the child in simple, direct terms: “Baby Bobby couldn’t breathe by himself because his lungs were sick. His sick lungs only happen to little babies.”
A Child’s Developing Concept of Death
| Age | Cognitive Understanding | How Experienced |
|---|---|---|
| Infant (to 12 mo) | None |
Indirectly through parental grief expressed in:
Emotional withdrawal
Inability to provide concern and continuity in caregiving behaviors
Overconcern for fear of recurrent loss
|
| Toddler (1-3 yr) |
Little understanding of cause and effect
Death may be confused with sleeping or being away
|
React to changes in behavior of grieving parents and reflect their feelings and anxiety |
| Preschooler (3-6 yr) |
View death as a temporary state and not an inevitable occurrence
Believe that they are the center of the universe and can do anything, and that thinking is doing (thoughts have the power of actions)
|
Expect the dead to return—ask questions about “when?” |
| School age (6-12 yr) |
Understand that death is inevitable and irreversible; 6- to 9-yr-olds personify death as a separate person (skeleton; bogeyman)
About 8 yrs old: “death phobia,” a normal developmental stage characterized by preoccupation with thoughts of own death and that of loved one
Reasons concretely with ability to see cause-and-effect relationships
|
Realize death occurs in adults like parents and even in children; realize death is permanent, not temporary state
May show interest in biologic aspects of death and details of funeral
|
| Adolescent (12 yr) | Able to think abstractly about death like the adult; philosophic reasoning | Similar to that in adult |
In one study, bereaved children had more frequent health care contacts for symptoms (e.g., abdominal pain, enuresis, headaches, insomnia) with no organic cause in the year after their loss. 62 Subsequent illness may precipitate worry by the child that he or she, too, will die. Often this fear is not verbalized but acted out by significant behavioral changes such as withdrawal, clinging, whining, or overactivity that is uncharacteristic for the child. Verbal reassurance that the child will not die and a reminder that “the baby died of a sickness that only little babies get; big boys and girls can’t get it” are helpful.
The normal feelings that accompany grief should be acknowledged and explained to the child. “Mommy and Daddy feel sad that Baby Jean died. Sometimes we will cry because we feel sad. It’s okay to cry when you feel sad.” Permission for the expression of the child’s feelings should also be given verbally: “You might feel sad, too. It’s okay for you to cry when you’re sad. Then we will talk about how you are feeling.” Encouraging children to draw or write their feelings is another way of giving them permission to express their grief.
Using words such as “went away,” “expired,” “lost,” or “went to sleep” is dangerous in describing death to children. Because young children are concrete and literal, they think they might die if they “go to sleep” or that anyone who leaves them is in danger of dying. Children also relate current experiences to past ones and interpret “lost” quite literally. In the mind of the child, if the parent only searched well enough, the misplaced (i.e., “lost”) child would be found.
Including children at funeral or memorial services facilitates their grief and prevents exclusion from a significant family event. Consideration of the family value system, age of the child, and religious custom must enter into the decision to include the child. Adequate preparation includes a discussion of everything the child will see, hear, and feel, including the normal adult emotions of crying and sadness. An adult besides the grieving parents should accompany the child to reiterate what is happening and to meet the child’s physical and psychologic needs. Adult support is necessary so that the child can express and deal with his or her feelings.
Helping children with their grief is also therapeutic for parents. Assisting children to master the crisis of loss ultimately augments the parents’ self-esteem and restores confidence in their parenting skills. 58 Parents can deal in a healthy way with their own grief when they can facilitate the grief of their other children. Qualitative studies reveal parental spiritual needs and support of siblings after a perinatal loss73:
• Recognition and acknowledgment of the child’s grief, which included listening and answering questions honestly; interpreting and acknowledging the meaning of the child’s behaviors; shielding from the insensitivity of others; and knowing when support of the child would be more effectively handled by someone outside the immediate household
• Inclusion of the child in family events, rituals, and practices such as visiting, holding, and touching the baby in the hospital; attending the funeral/memorial service; and visiting the gravesite
• Keeping the baby alive in the family’s memory by encouraging questions and comments about the baby; expressing feelings about the loss; including in viewing photos and personal items of the baby; and recognizing the deceased infant in birthday/holiday celebrations
PATHOLOGIC GRIEF
The absence of grief when it would be expected is not a healthy sign but, rather, a cause for concern. 56 The emotions of grief and their expression are healing. Early and full expression of grief is associated with an optimal outcome. 58 However, many people in grief-producing situations attempt to avoid the pain of grief and the expression of emotions, the result of which prolongs mourning, delays a return to the previous lifestyle, prevents the creation of new attachments and relationships, and ultimately results in pathologic grief (see the list on p. 917). 58
Not grieving precludes opportunities for growth and change. No new coping styles will be attempted. No novel alternatives to problem solving and adapting to a crisis will be added to the repertoire of behavior for future use. In other words, those who choose not to do grief work say “no” to their own potential and remain frozen in development. 77 Under the stress of not resolving their grief, some may even regress in their development.
Reproductive loss is a blow to self-concept and self-esteem, as well as loss of the infant. Blocking appropriate feelings of loss, grief, and anger results in a significant decrease in one’s sense of self-esteem. 28 After death of their neonates, 33% of mothers suffered severe and tragic outcomes (including psychoses, phobias, anxiety attacks, and deep depression) (see Chapter 29). 58,128 Those who cannot effectively resolve their grief may suffer lifelong emotional damage68; however, some empirical research shows that those who suppress feelings of grief may recover with relatively few difficulties. 6
Not working through grief associated with repetitive contact with perinatal loss also affects the staff. 37 To cope with feelings, they may hide behind a “professional” demeanor characterized by decreased spontaneity and withdrawal. Such a provider defends against the repeated pain of loss by emotional dissociation from the situation. The real self does not respond; instead, the professional stays in the role of the omnipotent, unemotional physician or nurse. The result, self-alienation, eventually desensitizes the professional to the experience and ultimately prevents any empathy with the experience of others. 53 Emotions that cannot be acknowledged or expressed healthily are vented in ways that may be destructive to relationships in personal and professional life.
Unresolved grief does not disappear and is not dissipated. The emotions accompanying grief may never be expressed but are not forgotten by the unconscious mind. Containment of these emotions through repression or suppression takes psychic energy. A conscious, intentional decision to postpone or dismiss grief to meet others’ needs or to meet immediate demands of the loss situation (e.g., funeral arrangements/care of a surviving multiple) is called delayed grief.61,68,83 For a period of time (days, weeks, or longer), there is little or no grief response when such a reaction would be expected and appropriate. Delayed grief also may be the result of repression—the unconscious content seems to have a life and energy of its own that become the sources of later emotional conflict.
Grief that is inhibited and never resolved is called abortive.68 Those who have aborted their grief work often live bereft of joie de vivre with no interest, concern, or enthusiasm for life. Chronic grief is characterized by an indefinite prolonging of the acute stage of depression. 68 Indeed, chronic depression may be traceable to unresolved grief from the past.
Grief that is not resolved remains buried in the psyche, waiting for an opportunity to “rear its ugly head.” A current loss may remind the psyche of the unmourned grief from a previous loss or losses. 36 As the two (or more) losses become intertwined and are experienced as one and the same, repressed emotions of unresolved grief pour forth. Grieving more than one loss or a lifetime of losses is more difficult and emotionally draining than grieving one event at a time. 36 Cumulative grief work also may be occurring when a current loss of seemingly little importance overwhelms the person with intense emotions. 36,68 This flood of emotions seems disproportionate to the current loss and is only peripherally related to it. The unconscious, unresolved grief is finally uncovered when the individual is flooded with emotions. Thus the emotional components of any grief reaction may be influenced by aspects of unresolved grief from the past. 121
Grief and loss events of the perinatal period have been equated only for a relatively short time (≈30 years). Because loss during the perinatal period is a common experience, many childbearing and older women (and men) have never grieved over their spontaneous abortion, stillbirth, or neonatal death, even 10 to 20 years after its occurrence. Parents in a current perinatal loss situation also may be dealing with unresolved grief from a previous perinatal loss. Unresolved grief (whether from perinatal or other loss events of life) may become available for resolution in subsequent crisis events. A mother who delivers a normal healthy newborn, yet is depressed postpartally, may not have postpartum depression. Instead, she may be grieving the unresolved loss of a spontaneous abortion, therapeutic abortion, or other perinatal loss. The normal grief reaction accompanying relinquishment may persist and often leads to chronic unresolved grief that may present itself during and after a subsequent pregnancy. 5 Her depressed mood could also be resulting from unresolved grief from the loss of a parent, spouse, or child. Depressed menopausal women may be experiencing the cumulative effects of a lifetime of unresolved grief (see the Critical Findings box below).
Symptoms of Unresolved Grief
1. Vivid memory for the details of the perinatal loss event
2. Flashback to the event
3. Anniversary grief (date of birth or expected date of delivery)
4. Emotions of grief (sadness, anger, or crying) when talking about loss
5. Intense emotions with subsequent loss or crisis
Recognizing unresolved grief has implications for facilitating grief work in a current loss, episodic care, and health maintenance. The energy to keep unresolved emotions restrained could better be used in personal growth and development, grieving, and maintaining and establishing relationships. The lifelong stress of unresolved grief contributes to both psychologic and physical illness, including increased death rates and an earlier death. 88
Not grieving a perinatal loss affects the individual involved and the relationships with significant others, including present and future children. Asynchronous grief and the absence of grief in one or more family members weaken and strain family relationships. 31,58 The irritability and preoccupation of normal grief may overly disrupt the family. Differences may be magnified to the extent that major rifts and disruptions in the relationship occur, resulting in increased incidence of separation and divorce. 58
Exclusive dedication to the care of a deformed or ill infant to the detriment of other family relationships is symptomatic of a pathologic grief reaction. 58,106,127 The parent who neglects other children, the couple’s relationship, and social outlets is so overwhelmed with guilt about having caused the baby’s defect that nothing else in life matters. This guilty attachment and exclusive dedication are ways of avoiding grief work. 106 Other forms of pathologic reactions include parental rejection and intolerance of the deformed or ill infant. 58
The parent who is emotionally withdrawn and unavailable to the family because of chronic grief and depression cannot attach to and care for present or subsequent children. Aberrant parenting styles (resulting in a vulnerable, battered, or failure-to-thrive child) may be the result of prolonged separation, unresolved grief, or grief that has progressed beyond the anticipatory phase, so that emotional ties with the infant have been severed. 58 These difficulties with caring and parenting may affect the deformed or ill child and all the children in the family. In turn, these children may grow up unable to parent subsequent generations because of the type of ineffectual parenting they received. Parents who grieve inappropriately may leave their children a legacy of psychosocial problems such as difficulty with separation, independence, and control (e.g., school phobia and toilet training); failure to thrive; and sleep disturbances.
Planning for a new pregnancy and another baby should begin after the grief process for the lost infant is complete (about 6 months to 1 year), so that parents are emotionally ready to invest in a relationship with another fetus/newborn. 58 However, because the decision to become pregnant is highly personal and individual, many women are pregnant within 6 months to 1 year after a perinatal loss. 50,95 Some women see a subsequent pregnancy as a “cure” for their overwhelming feelings of emptiness and failure, 122 whereas others are averse to a subsequent pregnancy. Pregnancy after a perinatal loss is characterized by (1) increased pregnancy anxiety, a heightened fear, concern, and vigilance about the pregnancy and baby; (2) comparisons of current and previous pregnancies; (3) less attachment to the current versus the previous pregnancy; (4) a desire to see and phone the health care provider more often; (5) a desire for more prenatal testing; and (6) the subsequent pregnancy possibly being the precipitating event for posttraumatic stress disorder (PTSD) in both mothers and fathers. * Mothers appreciate being educated by their health care providers about the benefits and risks of subsequent pregnancies so that they can make an informed choice. 33 Benefits of postponing pregnancy include (1) enabling physiologic recovery from pregnancy before another is attempted; (2) enabling psychologic recovery, progression of grief work, and an optimal state to emotionally invest in a new pregnancy and newborn; (3) avoiding anniversary dates with the second pregnancy/child; and (4) improving the maternal-infant relationship—less anxiety, overprotectiveness, overindulgence, and hypervigilance. 80,121 The time necessary for physical and emotional recovery varies widely, and parents may benefit from interconceptual counseling after a perinatal loss. 121
REFERENCES
1. American Academy of Pediatrics, The pediatrician and childhood bereavement, Pediatrics 114 (2004) 1126.
2. American Academy of Pediatrics, Committee on Pediatric Workforce, Ensuring culturally effective pediatric care: implications for education and health policy, Pediatrics 114 (2004) 1677.
3. American Academy of Pediatrics and The American College of Obstetricians and Gynecologists, Guidelines for perinatal care,. ed 6 ( 2007)The Academy, Elk Grove, Ill.
4. Armstrong, D.S., Perinatal loss and parental distress after the birth of a healthy infant, Adv Neonatal Care 7 (2007) 200.
5. Askren, H.; Bloom, K., Post adoptive reactions of the relinquishing mother: a review, J Obstet Gynecol Neonatal Nurs 28 (1999) 395.
6. Badenhorst, W.; Hughes, P., Psychological aspects of perinatal loss, Best Pract Res Clin Obstet Gynaecol 21 (2007) 249.
7. Benfield, D.; Leib, S.; Reuter, J.; et al., Grief response of parents after referral of the critically ill newborn to a regional center, N Engl J Med 294 (1976) 975.
8. Berezin, N., After a loss in pregnancy, help for families affected by a miscarriage, a stillbirth, or the loss of a newborn,. ( 1982)Fireside Books, New York.
9. Bibring, G.L., The death of an infant: a psychological study, N Engl J Med 283 (1970) 370.
10. Borg, S.; Lasker, J., When pregnancy fails: families coping with miscarriage, stillbirth, and infant death,. ( 1981)Beacon Press, Boston.
11. Bracht, M.; Kandankery, A.; Nodwell, S.; et al., Cultural differences and parental responses to the preterm infant at risk: strategies for supporting families, Neonatal Netw 21 (2002) 31.
12. Brodlie, M.; Laing, I.; Keeling, J.; et al., Ten years of neonatal autopsies in tertiary referral centre: retrospective study, BMJ 324 (2002) 761.
13. Broen, A.; Moum, T.; Bodtker, A.; et al., Psychological impact on women of miscarriage versus induced abortion: a 2 year follow up study, Psychosom Med 66 (2004) 265.
14. Brosig, C.L.; Pierucci, R.L.; Kupst, M.J.; et al., Infant end-of-life care: the parent’s perspective, J Perinatol 27 (2007) 510.
15. Burkes, N., Saying good-bye, Neonatal Netw 23 (2004) 75.
16. Byrnes, A.; Berk, N.; Cooper, M.; et al., Parental evaluation of informing interviews for cleft lip or palate, Pediatrics 112 (2003) 308.
17. Cadden, V., Crisis in the family, In: (Editor: Caplan, G.) Principles of preventive psychiatry ( 1964)Basic Books, New York.
18. Caplan, G., Principles of preventive psychiatry. ( 1964)Basic Books, New York.
19. Carter, B.S., Neonatal and infant death: what bereaved parents can teach us, J Perinatol 27 (2007) 467.
20. Clements, P.; Vigil, G.; Manno, M.; et al., Cultural perspectives of death, grief and bereavement, J Psychosoc Nurs 41 (2003) 18.
21. Contro, N.; Larson, J.; Scofield, S.; et al., Hospital staff and family perspectives regarding quality of pediatric palliative care, Pediatrics 114 (2004) 1248.
22. Costello, A.C.; Gardner, S.L.; Merenstein, G.B., Perinatal grief and loss, J Perinatol 8 (1988) 41.
23. Cote-Arsenault, D., The influence of perinatal loss on anxiety in multigravidas, J Obstet Gynecol Neonatal Nurs 32 (2003) 623.
24. Cote-Arsenault, D.; Donato, K.L.; Earl, S.S., Watching and worrying: early pregnancy after loss experiences, MCN: Am J Matern Child Nurs 31 (2006) 356.
25. Cote-Arsenault, D.; Marshall, R., One foot in and one foot out: weathering the storm of pregnancy after perinatal loss, Res Nurs Health 23 (2000) 473.
26. Cote-Arsenault, D.; Morrison-Beedy, D., Women’s voices: reflecting back on pregnancy after perinatal loss, J Nurs Scholar 33 (2001) 239.
27. Cummings, S.T., The impact of the child’s defect on the father, Am J Orthop 46 (1976) 246.
28. Cummings, S.T.; Bayley, H.C.; Rie, H.E., Effects of the child’s deficiency on the mother: a study of mothers of mentally retarded, chronically ill, and neurotic children, Am J Orthopsychiatry 36 (1966) 595.
29. Davies, R., New understanding of parental grief: literature review, J Adv Nurs 46 (2004) 506.
30. de Montigny, F.; Beaudet, L.; Dumas, L., A baby has died: the impact of perinatal loss on family social networks, J Obstet Gynecol Neonatal Nurs 28 (1999) 151.
31. Doucette, J.; Pinelli, J., The effects of family resources, coping, and strains on family adjustment 18 to 24 months after the NICU experience, Adv Neonatal Care 4 (2004) 92.
32. Downey, V.; Bengiamin, M.; Heuer, L.; et al., Dying babies and associated stress in NICU nurses, Neonatal Netw 14 (1995) 41.
33. Downie, J.; Letendre, A., Parent’s experiences of mid-wife managed care following the loss of a baby in a previous pregnancy, J Adv Nurs 39 (2002) 127.
34. Dyer, K.A., Identifying, understanding, and working with grieving parents in the NICU. I. Identifying and understanding loss and the grief response, Neonatal Netw 24 (2005) 35.
35. Dyer, K.A., Identifying, understanding, and working with grieving parents in the NICU. II. Strategies, Neonatal Netw 24 (2005) 27.
36. Eason, W.M., The dying child,. ( 1970)Charles C Thomas, Springfield, Ill.
37. Egan, K.; Arnold, R., Grief and bereavement, Am J Nurs 103 (2003) 42.
38. Engel, G.L., Grief and grieving, Am J Nurs 64 (1964) 93.
39. Ewing, A.; Carter, B.S., Once again, Vanderbilt NICU in Nashville leads the way in nurse’s emotional support, Pediatr Nurs 30 (2004) 471.
40. Feudtner, C., Grief-love: contradictions in the lives of fathers of children with disabilities, Arch Pediatr Adolesc Med 156 (2002) 643.
41. Feudtner, C.; Haney, J.; Dimmers, M., Spiritual care needs of hospitalized children and their families: a national survey of pastoral care providers’ perceptions, Pediatrics 111 (2003) e67.
42. Gardner, S.L.; Merenstein, G.B., Helping families deal with perinatal loss, Neonatal Netw 5 (1986) 17.
43. Gold, K.J., Navigating care after a baby dies: a systematic review of parent experiences with health providers, J Perinatol 27 (2007) 230.
44. Goldbach, K.R.; Dunn, D.S.; Toedter, L.J.; et al., The effects of gestational age and gender on grief after pregnancy loss, Am J Orthop 61 (1991) 461.
45. Goldberg, H., The hazards of being male,. ( 1976)Sanford J. Greenberger, New York.
46. Gonzalez, M.T., Nursing support of the family with an abnormal infant, Hosp Top 15 (1971) 68.
47. Griffin, T., Facing challenges to family-centered care. II. Anger in the clinical setting, Pediatr Nurs 29 (2003) 212.
48. Harmon, R.; Glicken, A.; Siegel, R., Neonatal loss in the intensive care nursery: effects of maternal grieving and a program for intervention, J Am Acad Child Psychiatry 23 (1984) 68.
49. Hobdell, E., Chronic sorrow and depression in parents of children with neural tube defects, J Neurosci Nurs 36 (2004) 82.
50. Hughes, P.; Turton, P.; Evans, C., Stillbirth as a risk factor for anxiety and depression in the next pregnancy: does time since loss make a difference?BMJ 318 (1999) 1721.
51. Hughes, P.; Turton, P.; Hopper, R.N.; et al., Disorganized attachment behaviour in infants born subsequent to stillbirth, J Child Psychol Psychiatry 42 (2001) 791.
52. Jansen, J., A bereavement model for the intensive care nursery, Neonatal Netw 22 (2003) 17.
53. Jourard, S., The transparent self. ( 1971)Van Nostrand Reinhold, New York; (revised edition).
54. Jung, A.; Milne, P.; Wilcox, J.; et al., Neonatal hand casting method, J Perinatol 23 (2003) 519.
55. Kavanaugh, K.; Hershberger, P., Perinatal loss in low-income African American parents, J Obstet Gynecol Neonatal Nurs 34 (2005) 595.
56. Kennell, J.H.; Slyter, H.; Klaus, M.H., The mourning response of parents to death of a newborn infant, N Engl J Med 283 (1970) 344.
57. Kitson, C., Commentary on: Fathers experienced in stillbirth as a waste of life and needed to protect their partners and express grief in their own way, Evid Based Nurs 5 (2002) 61.
58. Klaus, M.; Kennell, J., Parent-infant bonding. ed 2 ( 1982)Mosby, St Louis.
59. Kübler-Ross, E., On death and dying,. ( 1969)Macmillan, New York.
60. Leonard, L., Prenatal behavior of multiples: implications for families and nurses, J Obstet Gynecol Neonatal Nurs 31 (2002) 248.
61. Lindemann, E., Symptomatology and management of acute grief, Am J Psychiatry 101 (1944) 141.
62. Lloyd-Williams, M.; Wilkinson, C.; Lloyd-Williams, F., Do bereaved children consult the primary health care team more frequently?Eur J Cancer Care 7 (1998) 120.
63. Lobar, S.; Youngblut, J.; Brooten, D., Cross-cultural beliefs, ceremonies and rituals surrounding death of a loved one, Pediatr Nurs 32 (2006) 44.
64. Lundqvist, A.; Nilstun, T.; Dykes, A., Both empowered and powerless: mother’s experience of professional care when their newborn dies, Birth 29 (2002) 3.
65. Lundqvist, A.; Nilstun, T.; Dykes, A., Experiencing neonatal death: an ambivalent transition into motherhood, Pediatr Nurs 28 (2003) 621.
66. Maifield, M.; Hahn, S.; Titler, M.; et al., Decision making regarding multifetal reduction, J Obstet Gynecol Neonatal Nurs 32 (2003) 357.
67. Mallow, G.; Bechtel, G., Chronic sorrow: the experience of parents with children who are developmentally disabled, J Psychosoc Nurs 27 (1999) 31.
68. Marris, P., Loss and change,. ( 1974)Pantheon Books, New York.
69. Matzo, M.; Sherman, D.; Lo, K.; et al., Strategies for teaching loss, grief and bereavement, Nurse Educ 28 (2003) 71.
70. McCarthy, M., Gender differences in reactions to perinatal loss: a qualitative study of couples. ( 2002)California School of Professional Psychology, San Diego, Calif; doctoral dissertation.
71. McCreight, B., A grief ignored: narratives of pregnancy loss from a male perspective, Sociol Health Illn 26 (2004) 326.
72. McHaffie, H.; Laing, I.; Lloyd, D., Follow up care of bereaved parents after treatment withdrawal from newborns, Arch Dis Child Fetal Neonatal Ed 84 (2001) F125.
73. Meert, K.; Thurston, C., Spiritual needs of bereaved parents: a qualitative study, Pediatr Res 55 (2004) 378.
74. Milstein, J., Detoxifying death in the neonate: in search of meaningfulness at the end of life, J Perinatol 23 (2003) 333.
75. Mitchell, L., Women’s experiences of unexpected ultrasound findings, J Midwifery Womens Health 49 (2004) 228.
76. Moore, D.; Catlin, A., Lactation suppression: forgotten aspect of care for the mother of a dying child, Pediatr Nurs 29 (2003) 383.
77. Moore, M.; Moos, M., Cultural competence in the care of childbearing families,. ( 2003)March of Dimes Birth Defects Foundation, New York.
78. Nystrom, K.; Axelsson, K., Mother’s experience of being separated from their newborns, J Obstet Gynecol Neonatal Nurs 31 (2002) 275.
79. Ohlshansky, S., Chronic sorrow: a response to having a mentally defective child, Soc Case 43 (1962) 190.
80. O’Leary, J., Grief and its impact on prenatal attachment in the subsequent pregnancy, Arch Womens Ment Health 7 (2004) 7.
81. Parkes, C.M., Bereavement: studies of grief in adult life. ( 1972)International Universities Press, New York.
82. Pector, E., Views of bereaved multiple-birth parents on life support decisions, the dying process, and discussions surrounding death, J Perinatol 24 (2004) 4.
83. Pector, E., How bereaved multiple-birth parents cope with hospitalization, homecoming, disposition for deceased, and attachment to survivors, J Perinatol 24 (2004) 714.
84. Pector, E.; Smith-Levitin, M., Bereavement in multiple birth. I. General considerations, Female Patient 26 (2001) 31.
85. Primeau, M.; Lamb, J., When a baby dies: rights of the baby and parents, J Obstet Gynecol Neonatal Nurs 24 (1995) 206.
86. Primeau, M.; Recht, C., Professional bereavement photos: one aspect of a perinatal bereavement program, J Obstet Gynecol Neonatal Nurs 23 (1994) 22.
87. Putman,, M., Perinatal perimortem and postmortem examination: obligations and considerations for perinatal, neonatal and pediatric clinicians, Adv Neonatal Care 7 (2007) 281.
88. Rahe, R.; Meyer, M.; Smith, M.; et al., Social stress and illness onset, J Psychosom Res 8 (1964) 35.
89. Rapaport, L., The state of crisis: some theoretical considerations, In: (Editor: Parad, H.) Crisis intervention ( 1965)Family Service Association of America, New York.
90. Raphael, D., The tender gift: breastfeeding. ( 1973)Schocken Books, New York.
91. Ray, L., Parenting and childhood chronicity: making visible the invisible work, J Pediatr Nurs 17 (2002) 424.
92. Reddick, B.; Catlin, E.; Jellinek, M., Crisis within crisis recommendations for defining, preventing, and coping with stressors in the NICU, J Clin Ethic 12 (2001) 254.
93. Reilly-Smorawski, B.; Armstrong, A.; Catlin, E., Bereavement support for couples following death of a baby: program development and 14-year exit analysis, Death Stud 26 (2002) 21.
94. Roberts, K., Providing culturally sensitive care to the childbearing Islamic family: Part II, Adv Neonatal Care 3 (2003) 250.
95. Robertson, P.; Kavanaugh, K., Supporting parents during and after a pregnancy subsequent to a perinatal loss, J Perinat Neonatal Nurs 12 (1998) 63.
96. Romesberg, T., Understanding grief: a component of neonatal palliative care, J Hosp Palliat Care Nurs 6 (2004) 161.
97. Samuelsson, M.; Radestad, I.; Segesten, K., A waste of life: fathers’ experience of losing a child before birth, Birth 28 (2001) 124.
98. Sandelowski, M.; Barroso, J., The travesty of choosing after positive prenatal diagnosis, J Obstet Gynecol Neonatal Nurs 34 (2005) 307.
99. Saylor, D., Nursing response to mothers of stillborn infants, J Obstet Gynecol Neonatal Nurs 8 (1977) 39.
100. Schoenberg, B.A., Anticipatory grief. ( 1974)Columbia University Press, New York.
101. Schoenberg, B.A.; Carr, A.; Perety, D.; et al., Loss and grief: psychological management in medical practice. ( 1970)Columbia University Press, New York.
102. Schwab, R., Effects of a child’s death on the marital relationship: a preliminary study, Death Stud 16 (1992) 141.
103. Seidman, R.; Kleine, P., A theory of transformed parenting: parenting a child with developmental delay/mental retardation, Nurs Res 44 (1995) 38.
104. Shah, M., Transcultural aspects of perinatal health care: a resource guide,. ( 2004)National Perinatal Association, Washington, DC.
105. Simons, C.; Ritchie, S.; Mullett, M., Parents’ perceptions of medical diagnoses and related issues for their high-risk infants, J Pediatric Health Care 12 (1998) 118.
106. Solnit, A.; Stark, M., Mourning and the birth of a defective child, Psychoanal Study Child 16 (1961) 523.
107. Stringer, M.; Shaw, V.; Savani, R., Comfort care of neonates at the end of life, Neonatal Netw 23 (2004) 41.
108. Sudia-Robinson, T., Palliative care, In: (Editors: Kenner, C.; McGrath, J.) Developmental care of newborns and infants: a guide for health professionals, ( 2004)Mosby, St Louis.
109. Swanson, K.; Karmali, Z.; Powell, S.; et al., Miscarriage effects on couples’ interpersonal and sexual relationships during the first year after loss: women’s perspectives, Psychosom Med 65 (2003) 902.
110. Swanson, P.; Pearsall-Jones, J.; Hay, D., How mothers cope with the death of a twin or higher multiple, Twin Res 5 (2002) 156.
111. Swift, K.; Janke, J., Breast binding…is it all that it’s wrapped up to be?J Obstet Gynecol Neonatal Nurs 32 (2003) 332.
112. Taylor, L.; Scott, S.; Leuthner, S., Experience of prenatal palliative care consultation, Pediatr Res 31 (2004) 72.
113. Traxler, P., Poem for my son, blood calendar. ( 1975)William Morrow, New York.
114. Turton, P.; Badenhorst, W.; Hughes, P.; et al., The psychological impact of stillbirth on fathers in subsequent pregnancy and puerperium, Br J Psychiatry 188 (2006) 165.
115. Turton, P.; Hughes, P.; Evans, C.; et al., Incidence, correlates and predictors of post-traumatic stress disorder in the pregnancy after stillbirth, Br J Psychiatr 178 (2001) 556.
116. Ufema, J., A need for gentleness, Nursing 34 (2004) 66.
117. Van, P.; Meleis, A., Coping with grief after involuntary pregnancy loss: perspectives of African American women, J Obstet Gynecol Neonatal Nurs 32 (2003) 28.
118. Vance, J.; Boyle, F.; Najman, J.; et al., Couple distress after sudden infant or perinatal death: a 30-month follow up, J Paediatr Child Health 38 (2002) 368.
119. Wagner, T.; Higgins, P.; Wallerstedt, C., Perinatal death: how fathers grieve, J Perinatal Educ 6 (1997) 4.
120. Wallerstedt, C.; Higgins, P., Facilitating perinatal grieving between the mother and the father, J Obstet Gynecol Neonatal Nurs 25 (1996) 389.
121. Wallerstedt, C.; Lilley, M.; Baldwin, K., Interconceptional counseling after perinatal and infant loss, J Obstet Gynecol Neonatal Nurs 32 (2003) 533.
122. Wheeler, S., A loss of innocence and a gain in vulnerability: subsequent pregnancy after a loss, Illness Crisis Loss 8 (2000) 310.
123. Whitfield, M., Psychosocial effects of intensive care on infants and families after discharge, Semin Neonatol 8 (2003) 185.
124. Wilson, A.L.; Fenton, L.J.; Stevens, D.C.; et al., The death of a newborn twin: an analysis of parental bereavement, Pediatrics 70 (1982) 587.
125. Wilson, S.; Miles, M., Spirituality in African-American mothers coping with a seriously ill infant, J Soc Pediatr Nurses 6 (2001) 116.
126. Workman, E., Guiding parents through the death of their infant, J Obstet Gynecol Neonatal Nurs 30 (2001) 569.
127. Young, R.K., Chronic sorrow: parent’s response to the birth of a child with a defect, MCN Am J Matern Child Nurs J 2 (1977) 38.
128. Zahourek, R.; Jensen, J., Grieving and the loss of the newborn, Am J Nurs 73 (1973) 836.
RESOURCE MATERIALS FOR PARENTS
Balter, L., A funeral for Whiskers. ( 1991)Barron’s Educational Services, New York.
Berezin, N., After a loss in pregnancy. ( 1982)Fireside Books, New York.
Borg, S.; Lasker, J., When pregnancy fails. ( 1981)Beacon Press, Boston.
Boyle, F., Mothers bereaved by stillbirth, neonatal death, or sudden infant death syndrome. ( 1997)Aldershot, Ashgate, United Kingdom.
Brown, L.; Brown, M., When dinosaurs die: a guide to understanding death. ( 1996)Little, Brown, Boston.
Burns, L.; Ilse, S., Miscarriage: a shattered dream. ( 2000)Wintergreen Press, Maple Plain, Minn.
Buscaglia, L., The fall of Freddie the leaf. ( 1982)Slack, Thorofare, NJ.
Cardin, N., Tears of sorrow, seeds of hope. A Jewish spiritual companion for infertility and pregnancy loss. ( 2001)Jewish Light Publishing, Woodstock, Vt.
Case, B., Living without your twin. ( 2001)Tibbutt, Portland, Ore.
Cirulli, C., Pregnancy after loss: a guide to pregnancy after a miscarriage, stillbirth, or infant death. ( 1999)Berkeley Books, New York.
Davis, D., Empty cradle, broken heart. ( 2000)Fulcrum Publishing, Golden, Colo.
Davis, D.; Stein, M., Parenting your premature baby and child: the emotional journey. ( 2004)Fulcrum Books, Golden, Colo.
Dyer Dyer, K.A., Journey of hearts, Website:www.journeyofhearts.org.
Eddy, M.L.; Raydo, L., Making loving memories: a gentle guide to what you can do when your baby dies. ( 1990)Centering Corp, Omaha, Neb.
Eldon, K.; Eldon, A., Angel catcher: a journal of loss and remembrance. ( 1998)Chronicle Books, San Francisco.
Emswiler, M.; Emswiler, J., Guiding your child through grief. ( 2000)Bantam Trade, New York.
Grollman, E., Talking about death: a dialogue between parent and child. ( 1990)Beacon Press, Boston.
Grollman, E., Straight talk about death to teenagers. ( 1993)Beacon Press, Boston.
Harrison, H., The premature baby book. ( 1983)St Martin’s Press, New York.
Isle, S., Empty arms. ( 1996)Wintergreen Press, Maple Plain, Minn.
Leon, I.C., When a baby dies: psychotherapy for pregnancy and newborn loss. ( 1990)Yale University Press, New Haven, Conn.
Limbo, R.; Wheeler, S., When a baby dies: a handbook for healing and helping. ( 1998)Lutheran Hospital—La Crosse, La Crosse, Wis.
Linden, D.; Paroli, E.; Doron, M., The essential guide for parents of premature babies. ( 2000)Pocket Books, New York.
March of Dimes, The bereavement kit. ( 2002)March of Dimes Birth Defects Foundation, New York.
Miller, S., Finding hope when a child dies. ( 1999)Simon & Schuster, New York.
Mundy, M., Sad isn’t bad: a good-grief guidebook for kids dealing with loss. ( 1999)Abbey Press, St. Meinrad, Ind; (Elf-Help Books for kids).
Pector Pector, E., Multiplicity: resources for loss, prematurity and special needs, Website:www.synspectrum.com/multiplicity.html.
Read, B.; Bryan, E.; Hallett, F., When a twin or triplet dies. ( 1997)The Multiple Births Foundation, London.
Shriver, M., What’s heaven?. ( 1999)Golden Books, New York.
Standucher, C., Men and grief. ( 1991)New Harbinger Publications, Oakland, Calif.
Thomas, P., I miss you: a first look at death. ( 2001)Barron’s Educational Series, Hauppauge, NY.
Tracy, A.; Maroney, D., Your premature baby and child. ( 1999)Berkley Books, New York.
Woodward, J., The lone twin: understanding twin bereavement and loss. ( 1998)Free Association Books, London.
Zaichkin, J., Newborn intensive care: what every parent needs to know. ed 3 ( 2009)NICU Inc, Petaluma, Calif.
VIDEOS, DVDS, AND PROFESSIONAL MODULES
Gemma, P.; Arnold, J., Loss and grieving in pregnancy and the first year of life: a caring resource for nurses. ( 2003)March of Dimes, White Plains, NY.
Grieving in the NICU, Supporting families and the health team when a baby dies and Grieving in the NICU: mending broken hearts when a baby dies, Website:www.grievingforbabies.org.
What do I tell my children?. ( 1990)Life-cycle Productions, Newton, Mass.
When a baby dies. ( 1991)Resolve Through Sharing, La Crosse Lutheran Hospital, La Crosse, Wis.
NATIONAL ORGANIZATIONS
American Academy of Pediatrics, The pediatrician and childhood bereavement, Pediatrics 105 (2000) 445.
Angel babies forever loved, Website:www.angels4ever.com/multiples.
A place to remember, de-Ruyter-Nelson Publications, Inc., 1885 University Ave., Suite 110, St Paul, MN 55104; Phone: (800) 631-0973, Website:www.aplacetoremember.com.
Association for Death Education and Counseling, Website:www.adec.org.
Bereavement Services/RTS, 1910 South Ave, La Crosse, WI 54601; Phone: (608) 791-4747, Website:www.gundluth.org/bereave.
Center for Loss in Multiple Birth: Inc, Website:www.climb-support.org.
Centering Corp. and Grief Digest, Box 3367, Omaha, NE 68103-0367; Phone: (402) 553-1200; Website:www.centering.org.
Climb, Inc., Center for Loss in Multiple Birth, Inc, PO Box 91377, Anchorage, AK 99509; Phone: (907) 222-5321, Website:www.climb-support.org.
Hygeia Foundation, Inc, Website:www.hygeia.org.
March of Dimes Birth Defects Foundation, 1275 Mamaroneck Ave., White Plains, NY; Phone: 1-888-663-4637, Website:www.marchofdimes.com/loss.
Memories Unlimited, Inc: 9511 Johnson Point Loop NE, Olympia, WA 98516-9529; Phone: (360) 491-9819.
Mothers in Support and Sympathy (MISS) Foundation, Website:www.missfoundation.org.
Parents of Stillborn, 5570 South Langston Road, Seattle, WA, 98718; Phone: (206) 772-5338.
Perinatal Hospice, Website:www.perinatalhospice.org.
Pregnancy Loss and Infant Death Alliance, Website:www.plida.org.
Remember When, (Video and DVD tributes), Phone (720) 859-1122, Website:www.rememberwhenvideo.com.
RTS Bereavement Program, Website:www.bereavementprograms.com.
SHARE Pregnancy and Infant Loss Support, Inc, St Joseph’s Health Center, 300 First Capitol Drive, St Charles, MO 63301; Phone: (800) 821-6819, Website:www.nationalshareoffice.com.
The Compassionate Friends, Inc, PO Box 3696, Oak Brook, IL 60522-3696; Phone: (630) 990-0010, Website:www.compassionatefriends.org.