Chapter 109 Giant Retinal Tear
Introduction
Giant retinal tear by definition is a retinal tear of more than 90° circumferential extent.1 Since the posterior vitreous is detached, the vitreous gel is adherent to the anterior flap. Hence, the posterior flap has a tendency to fold over. In contrast, in a giant retinal dialysis the retina is either torn at the ora serrata or there is a break in ciliary epithelium, with the vitreous being adherent to the posterior retina.2 Thus, the posterior flap does not have the tendency to fold over, since it is supported by the vitreous gel.
The management of fresh giant retinal tear is an emergency. The delay in surgical intervention could lead to significant proliferative vitreoretinopathy (PVR) changes jeopardizing reattachment of the retina and eventual visual gain. Before the introduction of perfluorocarbon liquids by Stanley Chang,3 the management of giant retinal tears was challenging and resulted in limited success. The present day management of giant retinal tear is reasonably straightforward, with predictably good success rate.
Etiology
Most giant retinal tears are idiopathic in origin with males being at higher risk. Traumatic giant retinal tears are commonly located in the upper nasal and lower temporal quadrants and are again commoner in males. In a population-based study in the UK, Ang et al. have reported an annual incidence of 0.091 patients per 100 000 population.4 Most of the cases were idiopathic (54.8%) and males predominated (71.7%).4
The association with high myopia is well established.5 Of all retinal detachments in Marfan syndrome, 11.3% have been reportedly caused by giant retinal tears.6 Retinal detachment, especially due to giant retinal tear has been identified as an important complication of Stickler syndrome.7 Other diseases associated with occurrence of giant retinal tear include the Ehlers–Danlos syndrome,8 lens coloboma,9 and aniridia.10
Iatrogenic giant retinal tear
1. During a cataract surgery misadventure11: If attempts are made to fish around for the dislocated nucleus giant retinal tear can easily occur due to the uncontrolled vitreous traction.
2. During vitreoretinal surgery12: Circumstances that predispose to such an occurrence are:
3. Giant retinal tear has also been reported after pneumatic retinopexy and has been attributed to partly detached vitreous that exerted traction following the expansion of the bubble of expansile gas.13
4. Shinoda et al. reported the occurrence of giant retinal tear due to jamming of the 25-gauge instruments in the cannula, while operating on eyes with vitreous hemorrhage.14
5. Giant retinal tear has also been described after refractive surgery in the form of LASIK15 and phakic intraocular lens,16 although the cause and effect relationship remains debatable.
Pathogenesis
Schepens first described the important role played by the vitreous in giant retinal tear. Central vitreous liquefaction is associated with condensation in the peripheral vitreous base that leads to traction on the peripheral retina.1 As traction progresses, it is evident clinically as spreading “white-without-pressure.” Later, transvitreal contraction of the cortical gel occurs, tearing the retina along the vitreous base in a zipper fashion. Occasionally, multiple horseshoe-shaped tears may form along the posterior vitreous base and coalesce to form a giant retinal tear. Radial extensions (horns) can occur at the two ends of the giant retinal tear. Eyes with radial extension invariably have some amount of vitreous hemorrhage since the tears cut across larger blood vessels posteriorly.
History of management of giant retinal tear
The management of giant retinal tear can be divided conveniently into pre- and post-perfluorocarbon liquids (PFCL) eras. Most techniques used in the pre-PFCL era are of historic importance. However, a brief mention of these techniques is relevant in the overall understanding of the management of giant retinal tear. The primary problem faced by the surgeon was the gravity-driven tendency of the flap of the retinal tear to fold and fall back. Scleral buckles have been done for smaller extent of the tears (around 90°). A relatively shallow, but broad buckle was aimed at, so that the tendency for the flap to slip back is reduced and the inevitable central sagging of the flap is accommodated on the broad buckle.17 Attempts were also made to rotate the patient and to reposition the retinal flap with the help of an air bubble.18 Vitreoretinal surgery helped mobilize the inverted flaps of large giant retinal tears but the surgeon still faced difficulty in unrolling the same and fixing it in position. One strategy was to divide the giant retinal tear into smaller segments by pinning the edge of the tear down to the RPE/choroid complex using retinal tacks19,20 or sutures.21 This enabled routine fluid–air exchange to fix the retina without slippage of the retinal flap. Another technique involved fluid–air exchange in prone position. After a vitrectomy (and sometimes placement of buckle), the sclerotomies were closed and the patient was turned prone. Without contaminating the operative field, fluid–air exchange was then performed, with the air injection being done in front of the optic disc and fluid being evacuated from the anterior chamber.22 The air progressively attached the retina posteroanteriorly. The patient is repositioned in the supine position and internal tamponading agent was injected – gas or silicone oil as the case may be. Among all these techniques, perhaps the best attachment of the retina with no folds or slippage was seen with prone fluid–air exchange following vitrectomy. With the use of PFCLs, the surgery has become much simpler.
Preoperative evaluation and planning
The posterior vitreous will be found to be detached in cases of giant retinal tear, unlike in dialysis. In eyes that had blunt injury, the vitreous base can be avulsed and is seen as a rope-like structure near the pars plana. In eyes with perforating injury or following cataract surgery misadventure, the vitreous could be incarcerated in the wound and is seen as a transvitreal membrane. The giant tear or dialysis is seen usually in the opposite quadrant.11
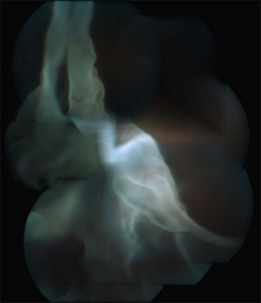
The extent of retinal detachment can vary. A dialysis can be associated with chronic partial detachments of the retina with high water marks, while giant retinal tear is usually associated with a more rapidly spreading retinal detachment. Eyes with around 90° tears are characterized by sagging of the center of the tear posteriorly but do not show inversion of flap. However, if the two ends of the giant retinal tear trail significantly posteriorly (horns), the retinal flap that is enclosed in between, can fold back. Retinal tears that are nearing 180° circumferentially will show a tendency to fold back. The inverted flap can sometimes obscure the disc (Fig. 109.1). The edge of the tear usually is scrolled inwards despite lack of obvious PVR elsewhere. The pars plana epithelium can be detached in the area of tear and sometimes beyond, due to the vitreous base traction. The anterior flap of the retina can harbor lattice degeneration. Additional horseshoe tears can be seen in other quadrants near the posterior vitreous base. A macular hole can coexist – especially in eyes that are highly myopic or where the giant retinal tear is a result of blunt injury. Significant pigment dispersal is seen in the vitreous cavity and pigment is often seen adherent to the surface of the retina. A traumatic dialysis is often associated with evidence of damage to the RPE and choroid at the site of the ora serrata.
Ultrasonographic diagnosis of giant retinal tear
In eyes with opaque media, giant retinal tear can be suspected on ultrasonography.23 A suggestive feature is a discontinuity noticed anteriorly in the retinal echo and extending more than one quadrant. Double linear echo would be seen near the disc due to the close proximity of the two layers of the retina; one representing the flap of the giant retinal tear and hence discontinuous with the globe contour and the other representing the detached retina and hence continuous with the globe contour (Fig. 109.2).
Role of nonsurgical treatment
Vitreous surgery
Role of an encircling band along with vitreoretinal surgery
Many surgeons feel comfortable placing an encircling band even in eyes undergoing vitreoretinal (VR) surgery.24 An encircling band is expected to support the vitreous base and reduce the risk of redetachment taking place from the quadrants where there is no retinal tear. However, there are reports that the success rate of surgery for fresh giant retinal tear is not reduced by not placing the buckle.25 In addition, minimally invasive vitreous surgery is possible if one is not placing the buckle.26 The trick is in the use of wide-angle system of visualization and a radical vitreous base removal. In the presence of some degree of PVR, placement of encircling band is desirable.
Retinopexy
Endolaser is the preferred modality of retinopexy. By tilting the eye to the same side, the edge of the giant retinal tear can be kept entirely under PFCL, thus facilitating the application of the laser along its edge. In general, about 3–4 rows of burns are applied along the margin. It is best to treat 360°, including the peripheral retina, beyond the area of the giant retinal tear.27
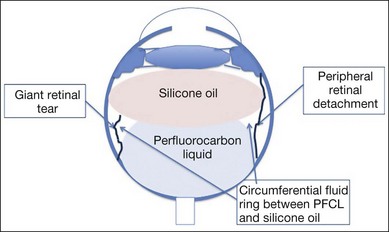
PFCL–silicone oil exchange
1. As the silicone oil is being injected, it forms initially a circular bubble. Once it contacts the central part of the upper meniscus of the PFCL, further injection tends to flatten the anterior surface of the PFCL bubble, thus spreading it over a larger surface of the retina.
2. The balanced salt solution will slowly be pushed into a circumferential ring all round, sandwiched between the oil and PFCL. One should not forget the rim of subretinal fluid that is trapped anterior to the PFCL in the area outside the giant retinal tear (Fig. 109.3).
3. Balanced salt solution (BSS), subretinal fluid, as well as PFCL can be easily sucked with both active and passive suction devices. Silicone oil will tend to block the suction device. Hence, while injecting silicone oil, a sudden rise in IOP can occur if the suction port is located within the silicone oil bubble. Failure to notice the raising IOP can result in some unpleasant consequences such as: (a) the edge of retinal flap getting sucked into the port of the suction device; (b) snapping of corneal sutures in eyes with recently repaired corneal wounds; (c) iris prolapse through a gaping scleral or corneal wound that has been made for IOL explantation.
4. Intermittent injection of silicone oil coupled with careful positioning of the suction tip at the edge of the giant retinal tear and just beyond the PFCL bubble margin will result in slow evacuation of the circumferential ring of balanced salt solution. Even the fluid located in the opposite quadrant will find its way to the site of suction and the subretinal space becomes totally dry. It is easy to distinguish between the residual fluid and silicone oil by the ease with which it finds its way into the suction port. Once all the fluid is removed, the PFCL bubble can be removed. Intermittently one can go back to the edge of the giant retinal tear to make sure that it is dry. Slow injection of the silicone oil will permit controlled removal of the PFCL and the end point is clearly visualized.
5. If the suction port is blocked with silicone oil, the IOP will rapidly rise as evidenced by appearance of central retinal artery pulsations and rapidly developing corneal edema. If the suction port is now shifted to the PFCL bubble, the block reopens as the PFCL washes the silicone oil out and one can clearly see the perfusion returning.
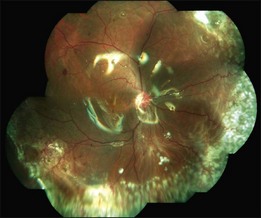
Figures 109.4 and 109.5 show pre- and postoperative photographs of a case of giant retinal tear. Note the postoperative photograph shows early PVR inferiorly.
Alternative techniques
1. PFCL as medium-term tamponade: In this technique, perfluorocarbon liquids are injected during the first stage and retained for 5–10 days. The patient is encouraged to lie in the supine position during this period. A second procedure is then performed to exchange the PFCL with gas or silicone oil.28,29
2. Air–PFCL exchange followed by air–silicone oil exchange: Some surgeons are not comfortable with direct silicone oil–PFCL exchange and perform first air–PFCL exchange followed by silicone oil–air exchange. This, however, retains the risk of retinal slippage during the first step of the procedure.
3. Use of heavy silicone oil: Densiron™ is heavier than water and is made up of perfluorohexyloctane (F6H6) and conventional silicone oil. This mixture has a specific gravity of 1.06 and a viscosity of 1480 mPas. It can be used both to settle the retina (since it is heavier than water) and can serve as internal tamponade. Unlike silicone oil, the inferior retina is better supported. There have been conflicting reports of its utility. The major concern appears to be that of significant emulsification that has been reported with Densiron even within 12 weeks of injection, leading potentially to inflammation and membrane formation.30,31
Additional steps
1. Once the whole retina is reattached following PFCL–air or silicone oil exchange, the untreated anterior retina can be treated comfortably.
2. In aphakic eyes, a peripheral iridectomy is done inferiorly to reduce the risk of pupillary block. This step is best done before exchanging the PFCL with silicone oil. In oil-filled aphakic eyes, iridectomy can still be done, by filling the anterior chamber first with Balanced salt solution (BSS) and then nibbling away the iris at 6 o’clock by placing the cutter behind the iris.
3. Where phacoemulsification has been done in the beginning of the surgery and IOL implantation is planned, this step is best done just before PFCL–air or silicone oil exchange. Alternatively, one can implant the IOL as the first step of the surgery along with the phacoemulsification and then proceed with the vitreoretinal surgery. However, the additional optical interfaces are avoided if the IOL is placed subsequent to reattachment of the retina.
4. Management of associated macular hole: A macular hole not uncommonly co-exists with giant retinal tear, especially in traumatized eyes and highly myopic eyes. Once the retina is mobilized, internal limiting membrane can be peeled around the macular hole. A small bubble of PFCL placed on the macular area helps achieve this goal. Staining of the ILM can be done with “Brilliant blue”™ under the PFCL bubble. By injecting small quantities of the dye with the PFCL bubble in place, one can avoid the migration of the dye into the subretinal space. Some eyes with high myopia and extensive chorioretinal atrophy in the macular area, may develop large macular holes. In these eyes, the aim of treatment would be to seal the hole with laser since there are high chances of recurrence of retinal detachment.
Results
In the pre-vitrectomy era, Schepens and Freeman could achieve successful reattachment only in two out of 14 eyes.32 Machemer reported a final success rate of 43% following vitrectomy with prone fluid–gas exchange and use of SF6 gas, although intraoperative success was achieved in 12 of the 14 cases.33 Aylward et al. reported a success rate of 89% in traumatic giant retinal tears using vitrectomy and silicone oil tamponade.34 Batman et al. reported no difference in success rate between silicone oil and long-acting gas tamponade.35
The routine use of encirclage continues to be debated, with Goezinne et al. reporting higher failure rate in the absence of encirclage,24 while Kreiger and Lewis25 (11 eyes) and Hoffman and Sorr36 (six eyes) reported success without buckle. Loewenstein et al. compared perfluoroperhydrophenanthrene and perfluoro-octane and found no statistically significant difference between the two groups.37 The overall success was 71.7% and 78.3%, respectively in the two groups. But the authors found greater incidence of retained perfluorophenanthrene compared with perfluoro-octane. This was attributed to perfluorophenanthrene’s greater specific gravity, lesser vapor pressure and less prominent interface with balance salt solution. Al-Khairi et al. analyzed the prognostic factors associated with surgical results and identified phakic/clear lens at presentation, unfolded flap of the giant retinal tear, absence of postoperative cataract, and absence of postoperative PVR to be associated with better than 20/200 vision.38 They also found that placement of encircling band and use of silicone oil tamponade were associated with higher anatomical reattachment with one procedure.
Management of fellow eye
In a study of the natural history of the fellow eyes, Freeman reported a 14% incidence of giant retinal tear and 36% incidence of other retinal tears.8,39 High-risk fellow eyes include high myopia, eyes with progressively increasing white without pressure areas with sharp posterior margin and increased vitreous condensation and patients with Wagner–Stickler syndrome. In a series of 204 patients with Type 1 Stickler syndrome, Ang et al. reported a risk reduction from 73% to 6.5% by performing prophylactic 360° cryopexy posterior to the ora serrata. Posterior lesions were not treated in this study.7 Wolfensberger et al. have reported a series of 48 eyes with giant retinal tear where the fellow eye was prophylactically treated with 360° cryopexy.40 They found an 8% (four eyes) incidence of retinal breaks (three with retinal detachment) over an 84-month follow-up period, where one patient had giant retinal tear posterior to the treated area. Based on their data, the authors believe that there is justification for prophylactic treatment.
While Freeman advocated prophylactic buckling along with cryopexy,39 most surgeons have resorted to only cryopexy or laser photocoagulation without scleral buckling.38,40,41 Laser has the advantage of being an outpatient procedure and can be spaced over two or more sittings in an attempt to reduce the inflammation caused by the treatment.
Despite these publications, one has to remember that there is still no consensus on: (1) the need for prophylaxis; (2) modality of treatment (cryopexy or laser); (3) where to treat (ora or equator); and (4) what to treat (visible lattice degenerations/visible areas of white without pressure or just 360° treatment). In a review of literature on interventions for prevention of giant retinal tear in the fellow eye, Ang et al. did not find conclusive evidence to support or refute the value of prophylaxis.42 In Stickler syndrome however, the evidence is more strongly in favor of offering prophylaxis for the fellow eye.7
1 Freeman HM, Schepens CL, Couvillion GC. Current management of giant retinal breaks. II. Trans Am Acad Ophthalmol Otolaryngol. 1970;74:59–74.
2 Smiddy WE, Gree WR. Retinal dialysis: pathology and pathogenesis. Retina. 1982;2:94–116.
3 Chang S. Low viscosity liquid fluorochemicals in vitreous surgery. Am J Ophthalmol. 1987;103:38–43.
4 Ang GS, Townend J, Lois N. Epidemiology of giant retinal tears in the United Kingdom: The British giant retinal tear epidemiology eye study (BGEES). Inv Ophthalmol Vis Sci. 2010;51:4781–4787.
5 Schepens CL, Dobble JG, McMeel JW. Retinal detachments with giant breaks: preliminary report. Trans Am Acad Ophthalmol Otolaryngol. 1962;66:471–479.
6 Sharma T, Gopal L, Shanmugam MP, et al. Retinal detachment in Marfan’s syndrome: clinical characteristics and outcome. Retina. 2002;22:423–428.
7 Ang A, Poulson AV, Goodburn SF, et al. Retinal detachment and prophylaxis in Type 1 Stickler syndrome. Ophthalmology. 2008;115:164–168.
8 Freeman HM. Fellow eyes of giant retinal breaks. Trans Am Ophthalmol Soc. 1978;76:343–382.
9 Hovland KR, Schepens CL, Freeman HM. Developmental giant retinal tears associated with lens coloboma. Arch Ophthalmol. 1968;80:325–331.
10 Dowler JG, Lyons CJ, Cooling RJ. Retinal detachment and giant retinal tears in aniridia. Eye. 1995;9:268–270.
11 Aaberg TM, Jr., Rubsamen PE, Flynn HW, Jr., et al. Giant retinal tear as a complication of attempted removal of intravitreal lens fragments during cataract surgery. Am J Ophthalmol. 1997;124:222–226.
12 Abu el-Asrar AM. Giant retinal tears after pars plana vitrectomy. Eye. 1997;11:325–327.
13 Yam JC, Liu DTL, Lee VYW, et al. Giant retinal tear after pneumatic retinopexy. Acta Ophthalmol. 2008;86:232–233.
14 Shinoda H, Nakajima T, Shinoda K, et al. Jamming of 25-gauge instruments in the cannula during vitrectomy for vitreous hemorrhage. Acta Ophthalmol. 2008;86:160–164.
15 Al Rashaed S, Abboud E, Al-Dhibi H. Bilateral retinal detachment after laser in situ keratomileusis. Ophthalmic Surg Lasers Imaging. 2009;40:180–184.
16 Georgalas I, Petrou P, Papaconstantinou D, et al. Bilateral giant tear – associated retinal detachment following Artisan phakic intra ocular lens implantation for correction of moderate myopia. Acta Ophthalmol. 2010;88:43–44.
17 Mehta MC, Hirose T, Schepens CL. ‘Giant retinal tears’. In: Schepens CL, Hartnett ME, Hirose T. Schepens’ retinal detachment and allied diseases. 2nd ed. Boston: Butterworth Heinemann; 2000:421–433.
18 Norton EW Aabert T, Fung W, et al. Giant retinal tears: I Clinical management with intravitreal air. Am J Ophthalmol. 1969;68:1011–1021.
19 Ando F, Kando J. A plastic tack for the treatment of retinal detachment with giant tear. Am J Ophthalmol. 1983;95:260–261.
20 Javey G, Schwartz SG, Flynn HW, Jr., et al. Lack of toxicity of stainless steel retinal tacks 21 years of follow-up. Ophthalmic Surg Lasers Imaging. 2009;40:75–76.
21 Federman JL, Shakin JL, Lanning RC. The microsurgical management of giant retinal tears with trans-scleral retinal sutures. Ophthalmology. 1982;89:832–838.
22 Freeman HM, Castillejos ME. Current management of giant retinal breaks: Results with vitrectomy and total fluid air exchange in 95 eyes. Trans Am Ophthalmol Soc. 1981;79:89–102.
23 Jalkh AE, Jabbour N, Avila MP, et al. Ultrasonographic findings in eyes with giant retinal tears and opaque media. Retina. 1983;3:154–158.
24 Goezinne F, Heij EC, Berendschot TT, et al. Low redetachment rate due to encircling scleral buckle in giant retinal tears treated with vitrectomy and silicone oil. Retina. 2008;28:485–492.
25 Kreiger AE, Lewis H. Management of giant retinal tears without scleral buckling. Use of radical dissection of the vitreous base and perfluoro-octane and intraocular tamponade. Ophthalmology. 1992;99:491–497.
26 Oliveira LB, Reis PA. Silicone oil tamponade in 23-gauge transconjunctival sutureless vitrectomy. Retina. 2007;27:1054–1058.
27 Ambresin A, Wolfensberger TJ, Bovey EH. Management of giant retinal tears with vitrectomy, internal tamponade, and peripheral 360 degree retinal photocoagulation. Retina. 2003;23:622–628.
28 Ventura MC, Melo C, Escariao P, et al. Perfluoroctane liquid as a short-term vitreous-retinal tamponade in the postoperative period in patients with retinal detachment due to giant tears. Arq Bras Oftalmol. 2007;70:495–500.
29 Sirmaharaj M, Balachnadran C, Chan WC, et al. Vitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tears. Br J Ophthalmol. 2005;89:1176–1179.
30 Majid MA, Hussin HM, Biswas S, et al. Emulsification of Densiron-68 used in inferior retinal detachment surgery. Eye. 2008;22:152–157.
31 Gerding H, Timmernann H, Hefner L, et al. Heavy internal tamponade for cases with complicated retinal detachment. Klin Monbl Augerheilkd. 2011;228:273–276.
32 Schepens CL, Freeman HM. Current management of giant retinal breaks. Ophthalmology. 1967;71:474–487.
33 Machemer R. Retinal tears 180 degrees and greater- management with vitrectomy and intravitreal gas. Arch Ophthalmol. 1976;94:1340.
34 Aylward GW, Cooling RJ, Leaver PK. Trauma induced retinal detachment associated with giant retinal tears. Retina. 1993;13:136–141.
35 Batman C, Cekic O. Vitrectomy with silicone oil or long acting gas in eyes with giant retinal tear. Retina. 1999;19:175–180.
36 Hoffman ME, Sorr EM. Management of giant retinal tear without scleral buckling. Retina. 1986;6:197–204.
37 Loewenstein A, Humayun MS, de Juan E, Jr., et al. Perfluoroperhydrophenanthrene versus perfluoro-n-octane in vitreoretinal surgery. Ophthalmology. 2000;107:1078–1082.
38 Al-Khairi AM, Al-Kahtani E, Kangave D, et al. Prognostic factors associated with outcomes after giant retinal tear management using perfluorocarbon liquids. Eur J Ophthalmol. 2008;18:270–277.
39 Freeman HM. Fellow eyes of giant retina breaks. Modern problems in ophthalmology. 1979;20:267–274.
40 Wolfensberger TJ, Aylward GW, Leaver PK. Prophylactic 360 degrees cryotherapy in fellow eyes of patients with spontaneous giant retinal tears. Ophthalmology. 2003;110:1175–1177.
41 Pollack A, Milstein A, Oliver M, et al. Circumferential argon laser photocoagulation for prevention of retinal detachment. Eye. 1994;8:419–422.
42 Ang GS, Townend J, Lois N. Interventions for prevention of giant retinal tear in the fellow eye. Cochrane Database of Systematic Reviews. 2, 2009. CD006909