29 Genitofemoral Neural Blockade
Clinically Relevant Anatomy
The genitofemoral nerve stems from the lumbar plexus. The lumbar plexus is formed by the ventral rami of L1 through the greater portion of L4. The ventral ramus of L1, which is frequently joined by a branch of T12, bifurcates into upper and lower portions (Fig. 29-1). The upper part divides into the iliohypogastric and ilioinguinal nerves as the lower part unites with a branch of the L2 ramus to form the genitofemoral nerve. Although much variation exists,1 the genitofemoral nerve often penetrates the psoas major muscle to then divide into a genital and femoral branch.
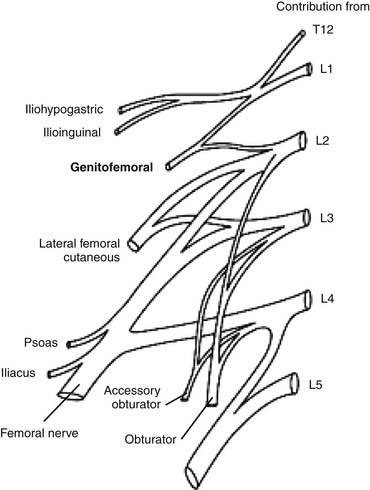
Figure 29-1 Lumbosacral anatomy of the genitofemoral nerve.
(Image courtesy of Dr. Alvin K. Antony.)
The genital branch, or external spermatic branch, is in part responsible for the cremasteric reflex by supplying the cremaster muscle. This genital branch traverses the internal inguinal ring to descend adjacent to the spermatic cord to supply the skin of the scrotum in males. In females, it accompanies the round ligament of the uterus2 to ultimately innervate the mons pubis and labia majora.
Descending on the external iliac artery and passing deep to the inguinal ligament, the femoral branch (or external lumboinguinal branch) enters the femoral sheath where it travels until it pierces the anterior layer, as well as, the fascia lata as it exits to supply skin sensation.2 Here the femoral branch supplies the skin with sensation at the anterior aspect of the femoral triangle, which is bordered by the inguinal ligament and the adductor longus and sartorius muscles.
All three of the “border” nerves (the iliohypogastric, the ilioinguinal, and the genitofemoral nerves) can cross-communicate to some extent. The exact origin, course, and distribution of each individual nerve are difficult to distinguish because communication between branches exists and a high degree of variability is present.1 This cross-communication phenomena should be noted, especially if difficulty achieving successful neural blockade is experienced.
Etiology and Pathogenesis
Genitofemoral neuralgia was first described in 1942.3 Injury to the genitofemoral nerve is almost always secondary to direct trauma. Direct trauma is almost always the result of surgery. Complications following inguinal herniorrhaphy4–11 and laparoscopic varicocelectomy12–16 are cited relatively frequently and can stem from inflammation, neuroma formation, deafferentation, or entrapment.4 Entrapment neuropathy can occur from impingement from staples or tacks which are used to affix the prosthetic mesh,17,18 the mesh itself, direct injury, or myofascial scarring.19
Additionally, it is not uncommon for genitofemoral neuralgia to be induced during performance of a lumbar sympathetic block.20–23 Lumbar sympathetic blocks, which are traditionally performed by injecting a needle from a posterior position toward the anterolateral aspect of the vertebral body, may allow for the injected solution to leak back along the needle shaft and spread toward the genitofemoral nerve,20 acting as a noxious irritant on the nerve.
Other factors, such as an abscess or mass dwelling within or near the psoas major muscle,19 complications secondary to appendectomy,9 inguinal lymph node dissection, orchiectomy, total abdominal hysterectomy, abdominoplasty, iliac crest bone graft, femoral catheter placement,8 cesarean section,24 thermal damage following radiofrequency ablation of renal cell carcinoma,25 direct injury from an inguinal herniated mass26,27 and complications from leprosy28 have also been noted.
Genitofemoral neuropathy will typically present as a neuropathic type groin pain following the distribution of the genitofemoral nerve. Pain may extend from the femoral triangle at the medial thigh to the scrotum in males or the mons pubis and labia majora in females. Although controversy exists as to which descriptors indicate a neuropathic type pain, adjectives such as “hot, burning, sensitive, and tingling” are frequently used.29
Indications
Groin pain in a genitofemoral neuroanatomic distribution with neuropathic pain features is the main indication for this block. A recent history of lower abdominal or groin trauma or surgery, especially inguinal herniorrhaphy, appendectomy, laparoscopic varicocelectomy, or cesarean section should be noted. Blocks may be used following these surgeries to augment pharmacologic pain control or during an inguinal herniorrhaphy as a local anesthetic.
Genitofemoral nerve infiltration used concomitantly with femoral nerve blocks in outpatients undergoing long saphenous vein stripping have been shown to result in a significantly faster recovery time, fewer complications, superior pain control, and better patient satisfaction when compared to spinal anesthesia.30
Diagnostically, blocks can be used to help achieve a more accurate utilization of further invasive interventions. Following failure of conservative measures of groin pain, a patient’s response to a peripheral neural blockade can be evaluated and, if temporary success is found, neurolysis,31 cryoneurolysis,32 or neurectomy33–35 may be indicated. As noted earlier, it is important to maintain an understanding of the ambiguous, overlapping distribution of the iliohypogastric, ilioinguinal, and genitofemoral nerves in the groin region and a neural blockade may need to be applied to each nerve to achieve successful pain control. Moreover, an MRI, CT, and EMG can aid in determining whether involvement of a lumbar radiculopathy, abscess, or malignancy exists.
Technique
Multiple techniques exist to access the branches of the genitofemoral nerve. Traditionally, the patient is placed supine and major anatomic landmarks including the anterior superior iliac spine, pubic tubercle, inguinal ligament, inguinal or femoral crease, and femoral artery are identified by palpation. If pain is experienced from nerve traction, a pillow may be placed underneath the patient’s knees to induce hip flexion and alleviate the tension placed at the anterior aspect of the groin. The genital branch is blocked by locating a point immediately lateral to the pubic tubercle and inferior to the inguinal ligament (Fig. 29-2). Following sterilization of the skin in this area, a 1.5- to 2-inch needle containing 5 to 10 mL of 1% preservative-free lidocaine is injected through the skin and subcutaneous area subsequent to aspiration.19,30,36 If an inflammatory component is noted, 40 to 80 mg of methylprednisolone or triamcinolone can be added to augment the anesthetic solution.36
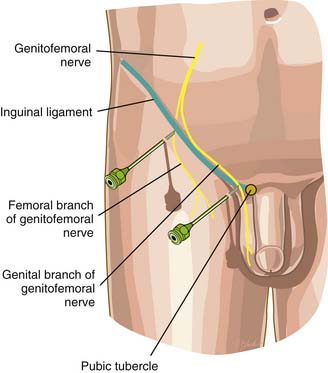
Figure 29-2 Genitofemoral nerve block.
(From Waldman SD: Atlas of Interventional Pain Management, 2nd ed. Philadelphia, Elsevier,1998, p 305.)
A trans-psoas technique, in which the patient lies prone and a 5- to 6-inch 21- to 22-gauge needle is introduced paravertebrally, approximately 5 cm from midline at the level of the L3-L4 interspace, is also used. The needle is then advanced toward the transverse process of either L3 or L4 and the depth of the transverse process is noted. The needle is withdrawn and marked at twice the depth of the transverse process. It is then reinserted to pass perpendicularly between the transverse processes and through the quadratus lumborum where loss of resistance will identify the first psoas muscle compartment. The needle continues to be further advanced until a second loss of resistance is noted, indicating the space located anteriorly to the psoas major muscle. Here, 2 to 3 mL of local anesthetic is deposited.19,37
An alternative technique for blocking the genital branch under high-frequency ultrasound guidance has been suggested as being superior when compared to the traditional blind method. As explained by Peng38:
“The orientation of the (linear) probe is perpendicular to the inguinal ligament. The final position of the probe is about 1 finger-breadth lateral to the pubic tubercle. However, inexperienced practitioners may have difficulty visualizing the spermatic cord, which is oval or circular in shape with 1 or 2 arteries within it (the testicular artery and the artery to vas deferens). The vas deferens is often seen as a thick tubular structure within the spermatic cord. It is suggested to start scanning with the probe in the internal inguinal ring, at which the femoral artery can be visualized in the longitudinal scan (along the length of the femoral artery). By moving the probe in the cephalad direction, the artery is seen as diving deep toward the inguinal ligament. At this point, an oval or circular structure can easily be seen superficial to the femoral artery. The probe is then moved slightly in the medial direction away from the femoral artery. An out-of-plane technique is also used with the needle approaching the skin from the lateral aspect of the probe.”
When correctly positioned, 5 mL of local anesthetic deposited inside and 5 mL deposited outside the spermatic cord should then take place. This external deposit is to ensure access because anatomic anomalies of the genital branch location are often encountered.38 The femoral branch can be blocked by implementing a fanlike infiltration into the subcutaneous tissue of 10 to 15 mL of local anesthetic in the medial, caudad, and cephalad direction at the lateral border of the femoral artery at the inguinal crease.19
Treatment Options
Other treatments to help manage pain induced by genitofemoral neuropathy are mentioned in the literature. Gabapentin, a calcium channel alpha2-delta ligand, may play a beneficial role39 and is indicated for first-line treatment in neuropathic pain management.40 A peripheral nerve stimulator, which requires placement directly on the nerve, has been shown to be effective in the treatment of genitofemoral neuralgia secondary to hernioplasty.41 Additional options that have been shown to be effective are neurolysis,31 cryoanalgesia (the application of cold to nerve tissues for the purpose of disrupting nerve structures but maintaining the myelin sheath and endoneurium intact),32 and neurectomy.11,33,34
1. Rab M., Ebmer J., Dellon A.L. Anatomic variability of the ilioinguinal and genitofemoral nerve: Implications for the treatment of groin pain. Plast Reconstr Surg. 2001;108(6):1618-1623.
2. Gray H., Lewis W.H. Anatomy of the Human Body, 20th ed. Philadelphia: Lea & Febiger; 1918.
3. Magee R.K. Genitofemoral causalgia: A new syndrome. Can Med Assoc J. 1942;46:326-329.
4. Rho R.H., Lamer T.J., Fulmer J.T. Treatment of genitofemoral neuralgia after laparoscopic inguinal herniorrhaphy with fluoroscopically guided tack injection. Pain Med. 2001;2(3):230-233.
5. Aroori S., Spence R.A. Chronic pain after hernia surgery—an informed consent issue. Ulster Med J. 2007;76(3):136-140.
6. Starling J.R., Harms B.A., Schroeder M.E., Eichman P.L. Diagnosis and treatment of genitofemoral and ilioinguinal entrapment neuralgia. Surgery. 1987;102(4):581-586.
7. Aasvang E., Kehlet H. Surgical management of chronic pain after inguinal hernia repair. Br J Surg. 2005;92(7):795-801.
8. Nahabedian M.Y., Dellon A.L. Outcome of the operative management of nerve injuries in the ilioinguinal region. J Am Coll Surg. 1997;184(3):265-268.
9. Lyon E.K. Genitofemoral causalgia. Can Med Assoc J. 1945;53:213-216.
10. Tetik C., Arregui M.E., Dulucq J.L., et al. Complications and recurrences associated with laparoscopic repair of groin hernias. A multi-institutional retrospective analysis. Surg Endosc. 1994;8(11):1316-1322.
11. Harms B.A., DeHaas D.R.Jr., Starling J.R. Diagnosis and management of genitofemoral neuralgia. Arch Surg. 1984;119(3):339-341.
12. Chrouser K., Vandersteen D., Crocker J., Reinberg Y. Nerve injury after laparoscopic varicocelectomy. J Urol. 2004;172(2):691-693.
13. Jarow J.P., Assimos D.G., Pittaway D.E. Effectiveness of laparoscopic varicocelectomy. Urology. 1993;42(5):544-547.
14. Muensterer O.J. Genitofemoral nerve injury after laparoscopic varicocelectomy in adolescents. J Urol. 2008;180(5):2155-2157.
15. Poulsen E.U., Willumsen H., Colstrup H., Jensen K.M. Varicocele of the testis. A comparison between laparoscopic and conventional surgery. Ugeskr Laeger. 1994;156(39):5683-5685.
16. Podkamenev V.V., Stalmakhovich V.N., Urkov P.S., et al. Laparoscopic surgery for pediatric varicoceles: Randomized controlled trial. J Pediatr Surg. 2002;37(5):727-729.
17. Seid A.S., Amos E. Entrapment neuropathy in laparoscopic herniorrhaphy. Surg Endosc. 1994;8(9):1050-1053.
18. Rosenberger R.J., Loeweneck H., Meyer G. The cutaneous nerves encountered during laparoscopic repair of inguinal hernia: New anatomical findings for the surgeon. Surg Endosc. 2000;14(8):731-735.
19. Vloka J.D., Hadzic A. Obturator and Genitofemoral Nerve Blocks. Tech Reg Anesth Pain Manag. 1999;3(1):28-32.
20. Datta S., Pai U. Paradiscal extraforaminal technique for lumbar sympathetic block: Report of a proposed new technique utilizing a cadaver study. Pain Physician. 2004;7(1):53-57.
21. Sayson S.C., Ramamurthy S., Hoffman J. Incidence of genitofemoral nerve block during lumbar sympathetic block: Comparison of two lumbar injection sites. Reg Anesth. 1997;22(6):569-574.
22. Dirim A., Kumsar S. Iatrogenic ureteral injury due to lumbar sympathetic block. Scand J Urol Nephrol. 2008;4:395-396.
23. Kim W.O., Yoon K.B., Kil H.K., Yoon D.M. Chemical lumbar sympathetic block in the treatment of plantar hyperhidrosis: A study of 69 patients. Dermatol Surg. 2008;34(10):1340-1345.
24. Ducic I., Moxley M., Al-Attar A. Algorithm for treatment of postoperative incisional groin pain after cesarean delivery or hysterectomy. Obstet Gynecol. 2006;108(1):27-31.
25. Boss A., Clasen S., Kuczyk M., et al. Thermal damage of the genitofemoral nerve due to radiofrequency ablation of renal cell carcinoma: A potentially avoidable complication. AJR Am J Roentgenol. 2005;185(6):1627-1631.
26. Bademkiran F., Tataroglu C., Ozdedeli K., et al. Electrophysiological evaluation of the genitofemoral nerve in patients with inguinal hernia. Muscle Nerve. 2005;32(5):600-604.
27. Soyer T., Tosun A., Aydin G., et al. Evaluation of genitofemoral nerve motor conduction in inguinoscrotal pathologies. J Pediatr Surg. 2008;43(8):1540-1542.
28. Agrawal S.K., Singal A., Pandhi D., Oberoi S. Involvement of genitofemoral nerve with genital lesions in lepromatous leprosy. Indian J Lepr. 2004;76(1):71-77.
29. Jensen M.P. Review of measures of neuropathic pain. Curr Pain Headache Rep. 2006;10(3):159-166.
30. Vloka J.D., Hadzic A., Mulcare R., et al. Femoral and genitofemoral nerve blocks versus spinal anesthesia for outpatients undergoing long saphenous vein stripping surgery. Anesth Analg. 1997;84(4):749-752.
31. Weksler N., Klein M., Gurevitch B., et al. Phenol neurolysis for severe chronic nonmalignant pain: Is the old also obsolete. Pain Med. 2007;8(4):332-337.
32. Trescot A.M. Cryoanalgesia in interventional pain management. Pain Physician. 2003;6(3):345-360.
33. Murovic J.A., Kim D.H., Tiel R.L., Kline D.G. Surgical management of 10 genitofemoral neuralgias at the Louisiana State University Health Sciences Center. Neurosurgery. 2005;56(2):298-303.
34. Krahenbuhl L., Striffeler H., Baer H.U., Buchler M.W. Retroperitoneal endoscopic neurectomy for nerve entrapment after hernia repair. Br J Surg. 1997;84(2):216-219.
35. Kennedy E.M., Harms B.A., Starling J.R. Absence of maladaptive neuronal plasticity after genitofemoral-ilioinguinal neurectomy. Surgery. 1994;116(4):665-670.
36. Waldman S.D. Atlas of Interventional Pain Management, 2nd ed. Philadelphia: Elsevier; 1998. p 302
37. Hartrick C.T. Genitofemoral nerve block: A transpsoas technique. Reg Anesth. 1994;19(6):432-433.
38. Peng P.W., Tumber P.S. Ultrasound-guided interventional procedures for patients with chronic pelvic pain—a description of techniques and review of literature. Pain Physician. 2008;11(2):215-224.
39. Benito-Leon J., Picardo A., Garrido A., Cuberes R. Gabapentin therapy for genitofemoral and ilioinguinal neuralgia. J Neurol. 2001;248(10):907-908.
40. Dworkin R.H., O’Connor A.B., Backonja M., et al. Pharmacologic management of neuropathic pain. Evidence-based recommendations. Pain. 2007;132(3):237-251.
41. Walter J., Reichart R., Vonderlind C., Kuhn S.A., Kalff R. Neuralgia of the genitofemoral nerve after hernioplasty: Therapy by peripheral nerve stimulation. Chirurg. 2009;80(8):741-744.