General notes
Radiology
Contraindications
Risk due to radiation
Radiation effects on humans may be:
• hereditary, i.e. revealed in the offspring of the exposed individual, or
• somatic injuries, which fall into two groups: deterministic and stochastic.
1. Deterministic effects result in loss of tissue function, e.g. skin erythema and cataracts. If the radiation dose is distributed over a period of time, cellular mechanisms allow tissue repair. There is then greater tolerance than if the dose had been administered all at once. This implies a threshold dose above which the tissue will exhibit damage because the radiation dose exceeds the capabilities of cellular repair mechanisms.
2. Stochastic effects refer to random modifications to cell components, such as DNA mutations that can occur at any radiation dose; there is no threshold for stochastic effects.1 Stochastic effects, such as malignancy, are ‘all or none’. The cancer produced by a small dose is the same as the cancer produced by a large dose, but the frequency of occurrence is less with the smaller dose.
The current consensus held by international radiological protection organizations is that, for comparatively low doses, the risk of both radiation-induced cancer and hereditary disease is assumed to increase linearly with increasing radiation dose, with no threshold (the so-called linear no threshold model).2 It is impossible to totally avoid staff and patient exposure to radiation. The adverse effects of radiation, therefore, cannot be completely eliminated but must be minimized. There is a small but significant excess of cancers following diagnostic levels of irradiation, e.g. during childhood3 and to the female breast4 and amongst those with occupational radiation exposure.5 In the UK about 0.6% of the overall cumulative risk of cancer by the age of 75 years could be attributable to diagnostic X-rays. The most important factors which influence the risk of developing cancer after exposure to ionizing radiation are: (a) genetic considerations – specific gene mutations and family history; (b) age at exposure – children are, in general, more radiosensitive than adults; (c) sex – there is a slightly increased risk in females; (d) fractionation and protraction of exposure – higher dose and dose rate increase risk because of the influence of DNA damage.6 (Typical average effective dose equivalents for some common examinations are given in Appendix I.)
There are legal regulations which guide the use of diagnostic radiation (see Appendices II and III). These are the two basic principles:
1. Justification that a proposed examination is of net benefit to the patient.
2. ALARP – doses should be kept As Low As Reasonably Practicable; economic and social factors being taken into account.7
Justification is particularly important when considering the irradiation of women of reproductive age, because of the risks to the developing fetus. The mammalian embryo and fetus are highly radiosensitive. The potential risks of in utero radiation exposure on a developing fetus include both teratogenic and carcinogenic effects. The risk of each effect depends on the gestational age at the time of the exposure and the absorbed radiation dose. The developing fetus is most vulnerable to radiation effects on the central nervous system between 8 and 15 weeks of gestational age and the risk of development of fatal childhood cancer may be greater if exposure occurs earlier in pregnancy.8 The teratogenic risk of radiation is dose-dependent and exposure to ionizing radiation doses of less than 50 mGy has not been shown to be associated with different pregnancy outcomes compared with exposure to background radiation alone.8 The carcinogenic risk of ionizing radiation is harder to calculate accurately. It is thought that the risk for the general population of developing childhood cancer is 1 in 500.9 For a fetal radiation dose of 30 mGy the best estimate is of one excess cancer per 500 fetuses exposed,10 resulting in a doubling of the natural rate. Most diagnostic radiation procedures will lead to a fetal absorbed dose of less than 1 mGy for imaging beyond the maternal abdomen/pelvis and less than 10 mGy for direct abdominal/pelvic or nuclear medicine imaging. There are important exceptions which result in higher doses, such as CT scanning of the maternal pelvis.
Almost always, if a diagnostic radiology examination is medically indicated, the risk to the mother of not doing the procedure is greater than the risk of potential harm to the fetus. However, whenever possible, alternative investigation techniques not involving ionizing radiation should be considered before a decision to use ionizing radiation in a female of reproductive age is taken. It is extremely important to have a robust process in place that prevents inappropriate or unnecessary ionizing radiation exposure to the fetus. Joint guidance from the Health Protection Agency, the College of Radiographers and the Royal College of Radiologists recommends the following:9
1. No possibility of pregnancy – proceed with the examination.
2. Patient definitely, or probably, pregnant – review the justification for the proposed examination and decide whether to defer until after delivery, bearing in mind that delaying an essential procedure until later in pregnancy may present a greater risk to the fetus and a procedure of clinical benefit to the mother may also be of indirect benefit to her unborn child. If, after review, a procedure is still considered to be justified and is undertaken the fetal dose should be kept to the minimum consistent with the diagnostic purpose.
3. Low-dose examination, pregnancy cannot be excluded – a low-dose examination is defined as one in which the fetal dose is likely to be below 10 mGy. The vast majority of diagnostic examinations fall into this category. If pregnancy cannot be excluded but the patient’s menstrual period is not overdue, proceed with the examination. If the period is overdue, the patient should be treated as probably pregnant and the advice in the section above followed.
4. High-dose examination, pregnancy cannot be excluded – a high-dose procedure is defined as any examination which results in a fetal dose greater than 10 mGy (e.g. CT of the maternal abdomen and pelvis). The evidence suggests that such procedures may double the natural risk of childhood cancer if carried out after the first 3–4 weeks of pregnancy and may still involve a small risk of cancer induction if carried out in the very early stages of an unrecognized pregnancy. Either of two courses can be adopted to minimize the likelihood of inadvertent exposure of an unrecognized pregnancy: (a) apply the rule that females of childbearing potential are always booked for these examinations during the first 10 days of their menstrual cycle when conception is unlikely to have occurred; or (b) female patients of childbearing potential are booked in the normal way but are not examined and are re-booked if, when they attend, they are in the second half of their menstrual cycle and are of childbearing potential and in whom pregnancy cannot be excluded.
If the examination is necessary, evaluation of the fetal dose and associated risks by a medial physicist should be arranged, if possible, and discussed with the parents. A technique that minimizes the number of views and the absorbed dose per examination should be utilized. However, the quality of the examination should not be reduced to the level where its diagnostic value is impaired. The risk to the patient of an incorrect diagnosis may be greater than the risk of irradiating the fetus. Radiography of areas that are remote from the pelvis and abdomen may be safely performed during pregnancy with good collimation and lead protection. Royal College of Radiologists guidelines indicate that legal responsibility for radiation protection lies with the employer, the extent to which this responsibility is delegated to the individual radiologist varies. Nonetheless, all clinical radiologists carry a responsibility for the protection from unnecessary radiation of:
Contrast medium
Volumes given are for a 70-kg man.
Equipment
For many procedures this will also include a trolley with a sterile upper shelf and a non-sterile lower shelf. Emergency drugs and resuscitation equipment should be readily available (see Chapter 17).
See Chapter 9 for introductory notes on angiography catheters.
Patient preparation
1. Will admission to hospital be necessary?
2. If the patient is a woman of child-bearing age, the examination should be performed at a time when the risks to a possible fetus are minimal (see above). Any female presenting for radiography or a nuclear medicine examination at a time when her period is known to be overdue should be considered to be pregnant unless there is information indicating the absence of pregnancy. If her cycle is so irregular that it is difficult to know whether a period has been missed and it is not practicable to defer the examination until menstruation occurs, then a pregnancy test or pelvic ultrasound (US) examination may help to determine whether she is pregnant. Particular care should be taken to perform hysterosalpingography during the first 10 days of the menstrual cycle, so that the risks of mechanical trauma to an early pregnancy are reduced.
3. Except in emergencies, in circumstances when consent cannot be obtained, patient consent to treatment is a legal requirement for medical care.12 Consent should be obtained in a suitable environment and only after appropriate and relevant information has been given to the patient.13 Patient consent may be:
(a) implied consent – for a very low-risk procedure, the patient’s actions at the time of the examination will indicate whether they are content for the procedure to be performed
(b) express consent – for a procedure of intermediate risk, such as barium enema, express consent should be given by the patient, either verbally or in writing
(c) written consent – must be obtained for any procedure that involves significant risk and/or side effects. The ability to consent depends more on a person’s ability to understand and weigh up options than on age. At 16 a young person can be treated as an adult and can be presumed to have the capacity to understand the nature, purpose and possible consequences of the proposed investigation, as well as the consequences of non-investigation. Under the age of 16 years children may have the capacity to consent depending on their maturity and ability to understand what is involved. The radiologist must assess a child’s capacity to decide whether to give consent for, or refuse an investigation. If the child lacks the capacity to consent, the parent’s consent should be sought. It is usually sufficient to have consent from one parent. If the parents cannot agree, legal advice should be obtained.14 When a competent child refuses treatment, a person with parental responsibility or the court may authorize investigations or treatment which is in the child’s best interests. In Scotland the situation is different: parents cannot authorize procedures a competent child has refused. Legal advice may be helpful in dealing with these cases.
4. If an interventional procedure carries a risk of causing bleeding then the patient’s blood clotting should be measured before proceeding. If a bleeding disorder is discovered, or if the patient is being treated with anticoagulant therapy, the appropriate steps should be taken to normalize clotting before performing the procedure.
5. Cleansing bowel preparation may be used prior to investigation of the gastrointestinal tract or when considerable fecal loading obscures other intra-abdominal organs. For other radiological investigations of abdominal organs, bowel preparation is not always necessary, and when given may result in excessive bowel gas. Bowel gas may be reduced if the patient is kept ambulant prior to the examination and those who routinely take laxatives should continue to do so.
6. Previous films and notes should be obtained.
7. Premedication will be necessary for painful procedures or where the patient is unlikely to cooperate for any other reason. Suggested premedication for adults and children is described in Chapter 18.
Preliminary images
The purpose of these films is:
1. to make any final adjustments in exposure factors, centring, collimation and patient position, for which purpose the film should always be taken using the same equipment as will be used for the remainder of the procedure
2. to exclude prohibitive factors such as residual barium from a previous examination or excessive fecal loading
3. to demonstrate, identify and localize opacities which may be obscured by contrast medium
Every radiographic view taken should have on it the patient’s name, registration number, date and a side marker. The examination can only proceed if satisfactory preliminary films have been obtained.
Additional techniques or modifications of technique
Complications
Complications may be considered under the following three headings:
Due to the anaesthetic
Anaesthetic lozenges contribute to the total dose. Symptoms of excessive dose are of paraesthesia and muscle twitching which may progress to convulsions, cardiac arrhythmias, respiratory depression and death due to cardiac arrest. Treatment is symptomatic and includes adequate oxygenation.
References
1. Tramblay, E, Thérasse, E, Thomassin-Nagarra, E, et al. Quality initiatives: Guidelines for use of medical imaging during pregnancy and lactation. Radiographics. 2012; 32:897–911.
2. Wakeford, R. Cancer risk modelling and radiological protection. J Radiol Prot. 2012; 32(1):N89–N93.
3. Pearce, MS, Salotti, JA, Little, MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012; 380(9840):499–505.
4. Einstein, AJ, Henzlova, MJ, Rajagopalan, S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007; 298(3):317–323.
5. Muirhead, CR, O’Hagan, JA, Haylock, RGE, et al. Mortality and cancer incidence following occupational radiation exposure: third analysis of the National Registry for Radiation Workers. Br J Cancer. 2009; 100(1):206–212.
6. Hricak, HH, Brenner, DJ, Adelstein, SJ, et al. Managing radiation use in medical imaging: a multifaceted challenge. Radiology. 2011; 258:889–905.
7. International Commission on Radiological Protection. The optimization of radiological protection: broadening the process. ICRP publication 101. Ann ICRP. 2006; 36(3):69–104.
8. Wang, PI, Chong, ST, Kielar, AZ, et al. Imaging of pregnant and lactating patients: Evidence-based review and recommendations, Parts 1 and 2. Am J Roentgenol. 2012; 198:778–792.
9. Advice from the Health Protection Agency, The Royal College of Radiologists and the College of Radiographers. Protection of Pregnant Patients during Diagnostic Medical Exposures to Ionising Radiation. www. rcr. uk/docs/radiology/pdf/HPA_Diagnostic_Pregnancy. pdf, 2009.
10. International Commission on Radiological Protection. Pregnancy and medical radiation. Ann ICRP. 2000; 30(1):1–43.
11. Royal College of Radiologists, Good Practice Guide for Clinical Radiologists. 2nd ed, 2012. www. rcr. ac. uk/docs/radiology/pdf/BFCR(12)1_GoodPractice. pdf
12. The Royal College of Radiologists. Standards for Patient Consent Particular to Radiology. London: The Royal College of Radiologists; 2005.
13. General Medical Council. Consent: Patients and Doctors Making Decisions Together. London: General Medical Council; 2008.
14. General Medical Council. 0–18 years: Guidance for all Doctors. London: General Medical Council; 2007.
Radionuclide imaging
Radiopharmaceuticals
Radioactive injections
In the UK, the Administration of Radioactive Substances Advisory Committee (ARSAC) advises the health ministers on the Medicines (Administration of Radioactive Substances) Regulations 1978 (MARS). These require that radioactive materials may only be administered to humans by a doctor or dentist holding a current ARSAC certificate or by a person acting under their direction. Administration of radioactive substances can only be carried out by an individual who has received appropriate theoretical and practical training, as specified in the Ionising Radiation (Medical Exposure) Regulations 20001 (see Appendix III). These will place responsibilities on the referrer to provide medical data to justify the exposure, the practitioner (ARSAC licence holder) to justify individual exposure, and operators (persons who carry out practical aspects relating to the exposure).
Activity administered
The maximum activity values quoted in the text are those currently recommended as diagnostic reference levels in the ARSAC Guidance Notes.2 The unit used is the SI unit, the megabecquerel (MBq). Millicuries (mCi) are still used in some countries, notably the US; 1 mCi = 37 MBq.
Aftercare
Radiation safety
Special instructions should be given to patients who are breastfeeding regarding expression of milk and interruption of feeding.2 Precautions may have to be taken with patients leaving hospital or returning to wards, depending upon the radionuclide and activity administered. These precautions were reviewed following the introduction of the Ionising Radiation Regulations 1999 and the adoption of lower dose limits to members of the public, and appropriate guidance has been published.3
References
1. The Ionising Radiation (Medical Exposure) Regulations. London: HMSO, 2000.
2. Administration of Radioactive Substances Advisory Committee. Notes for Guidance on the Clinical Administration of Radiopharmaceuticals and use of Sealed Radioactive Sources. Didcot: NRPB; 1998.
3. Working Party of the Radiation Protection Committee of the British Institute of Radiology. Patients leaving hospital after administration of radioactive substances. Br J Radiol. 1999; 72:121–125.
Computed tomography
Patient preparation
Many CT examinations require little physical preparation. An explanation of the procedure, the time it is likely to take, the necessity for immobility and the necessity for breath-holding whilst scanning chest and abdomen should be given. Waiting times should be kept to a minimum, as a long wait may increase anxiety. The patient should be as pain-free as is practical but too heavy sedation or analgesia may be counter-productive – patient cooperation is often required. Children under the age of 4 years will usually need sedation (see Chapter 18). Children should also have an intravenous (i.v.) cannula inserted at the time sedation is administered or local anaesthetic cream applied to two sites if i.v. contrast medium is needed. If these simple steps are taken, the number of aborted scans will be reduced and the resultant image quality improved.
Intravenous contrast medium
Many CT examinations will require i.v. contrast medium. Essential information should be obtained from the patient and appropriate guidelines followed (see Chapter 2). An explanation of the need for contrast enhancement should be given to the patient.
Oral contrast medium
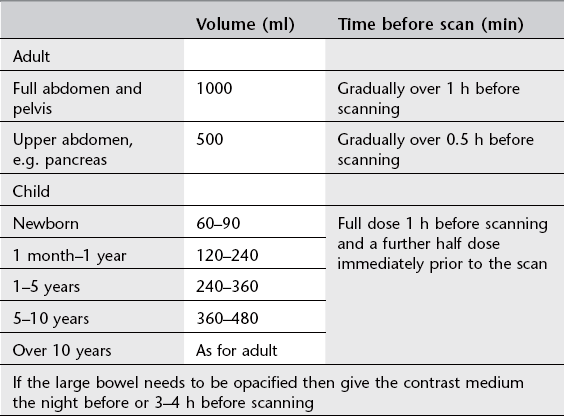
For examinations of the abdomen, opacifying the bowel satisfactorily can be problematic. Plain water is recommended as a negative oral contrast medium for CT of the stomach and duodenum. Satisfactory opacification of the small and large bowel can be problematic. Water-soluble contrast medium (e.g. 20 ml Urografin 150 diluted in 1 l of orange squash to disguise the taste, preflavoured contrast such as 20 ml Gastromiro diluted in 1 l of water) or low-density barium suspensions (2% w/v) can be used. Timing of administration is given in Table 1.1. Doses of contrast media in children depend upon age.
Magnetic resonance imaging
Patient preparation
As for CT scanning, a full description of the purpose and nature of the examination should be given to the patient and waiting times kept to a minimum. Some patients find the interior of the scanner a very disconcerting environment, and report claustrophobic and even acute anxiety symptoms. This may occur in as many as 10% of patients. Most of these patients are able to complete their examination, but approximately 1% of investigations may have to be curtailed as a result. To decrease the number of scans aborted, the counselling of, explanation to and reassurance of patients by well-trained staff should be routine. A small number of adult patients may require sedation before an MRI scan is undertaken. Sedation or general anaesthesia is often required for MRI scans in young children; details of suggested protocols are given in Chapter 18.
Safety in magnetic resonance imaging
Effects due to magnetic fields
Biological effects
Despite extensive research, no significant deleterious physiological effects have yet been proven.1 There have been reports of temporary minor changes, such as alteration in electrocardiogram (T-wave elevation) presumed to be due to electrodynamic forces on moving ions in blood vessels which might result in a reduction of blood-flow velocity. Temporary and dose-correlated vertigo and nausea in patients exposed to static fields higher than 2 T have been found.2 However, studies of volunteers exposed to 8 T static magnetic fields have shown no clinically significant effect on heart rate, respiratory rate, systolic and diastolic blood pressure, finger pulse oxygenation levels and core body temperature.3 Teratogenesis in humans is thought unlikely at the field strengths used in clinical MRI.
Non-biological effects
There are two main areas of concern:
1. Ferromagnetic materials may undergo rotational or translational movement as a result of the field. Rotational movement occurs as a result of an elongated object trying to align with the field. This may result in displacement of the object, and applies to certain types of surgical clip. Not all materials implanted are ferromagnetic and many are only weakly so. Each type should be checked individually for any such risk. In many cases, postoperative fibrosis (greater than 6 weeks) is strong enough to anchor the material so that no danger of displacement exists. Translational movement occurs when loose ferromagnetic objects are attracted to the field. Objects such as paperclips or hairgrips may reach considerable speeds and could potentially cause severe damage to patient or equipment, the so-called missile effect. In general, no object or equipment should be brought into the MRI environment unless it is proven to be:
• MRI safe (no known hazard in all MRI environments) or
• MRI conditional (no known hazard in a specified MRI environment with specified conditions of use).4
2. Electrical devices such as cardiac pacemakers may be affected by static field strengths. Most modern pacemakers have a sensing mechanism that can be bypassed by a magnetically operated relay triggered by fields as low as 5 gauss. Relay closure can be expected in virtually all conventional cardiac pacemakers placed in the bore of the magnet and these patients must not enter the controlled MRI area. Recent engineering advances have produced the first generation of MRI conditional cardiac pacemaker devices but great care must still be taken.5
Gradient field
Biological effects
The rapidly switched magnetic gradients used in MRI can induce electric fields in a patient which may result in nerve or muscle stimulation, including cardiac muscle stimulation. The strength of these is dependent on the rate of change of the field and the size of the subject.6 Studies have shown that the threshold for peripheral nerve stimulation is lower than that for cardiac or brain stimulation.7 Although possible cardiac fibrillation or brain stimulation are major safety issues, peripheral nerve stimulation is a practical concern because, if sufficiently intense, it can be intolerable and result in termination of the examination. Recommendations for safety limits on gradient fields state that the system must not have a gradient output that exceeds the limit for peripheral nerve stimulation.6 This will protect against cardiac fibrillation.
Radiofrequency field
Radiofrequency energy at frequencies above 10 MHz, deposited in the body during an MRI examination, will be converted to heat, which will be distributed by connective heat transfer through blood flow. Energy deposited in this way is calculated as the average energy dissipated in the body per unit of mass and time, the specific absorption rate (SAR). SAR values are dependent on the magnetic field strength and may be fourfold higher in a 3-T scanner than a 1.5-T scanner.8 Guidelines on radiofrequency exposure are designed to limit the rise in temperature of the skin, body core and local tissue to levels below those where systemic heat overload or thermal-induced local tissue damage occur. The extent to which local temperature rises depends on the SAR and on the blood flow and vascularity of the tissue. Areas of particular concern include those most sensitive to heat such as the hypothalamus and poorly perfused regions such as the lens of the eye.
For whole-body exposures, no adverse health effects are expected if the increase in body core temperature does not exceed 1°C. In the case of infants and those with circulatory impairment, the temperature increase should not exceed 0.5°C. With regard to localized heating temperatures, measured temperature in focal regions of the head should be less than 38°C, of the trunk less than 39°C, and in the limbs less than 40°C.6
Recommendations for safety
Detailed MRI safety recommendations have been published by the American College of Radiology.9 It is essential that all MRI units have clear MRI safety policies and protocols, including a detailed screening questionnaire for all patients and staff (Table 1.2).
Table 1.2
Questions which should be included in a screening questionnaire for magnetic resonance imaging patients and staff
| Question to patient or staff member | Action |
| Do you have a pacemaker or have you had a heart operation? | Pacemaker – if present patient must not enter controlled area Heart operation – establish if any metal valve prosthesis, intravascular device or recent metallic surgical clip insertion and check MR compatibility |
| Could you possibly be pregnant? | See text |
| Have you ever had any penetrating injury, especially to the eyes, even if it was years ago? | Establish details. If necessary arrange X-ray of orbits or relevant area to determine if there is any metallic foreign body |
| Have you ever had any operations to your head, chest or neck? | Find out details. If any metallic aneurysm or haemostatic clips or metallic prosthesis/implant then check MR compatibility |
| Do you have any joint replacements or any other body implants? | Check details of surgery and MR compatibility of joint replacement or implant |
| Have you removed all metal objects and credit cards from your clothing and possessions? | This must be done before entering the controlled area |
Implants
As mentioned above, persons with pacemakers must not enter the restricted area. All other persons must be screened to ensure there is no danger from implanted ferromagnetic objects, such as aneurysm clips, prosthetic heart valves, intravascular devices or orthopaedic implants. Where an object is not known to be ‘MRI safe’ or ‘MRI conditional’, then the person should not be scanned. Lists of safe and unsafe implants are available10 and should be consulted for each individual object.
Pregnancy
The developing fetus and embryo are susceptible to a variety of teratogens, including heat, being most sensitive during organogenesis. Increased static magnetic field strength, flip angle or number of radiofrequency pulses and decreased spacing between pulses will increase the SAR and therefore the radiofrequency energy deposited as heat on the fetus.11 Although no conclusive evidence of teratogenesis exists in humans, scanning should be avoided, particularly during the first trimester, unless alternative diagnostic procedures would involve the exposure of the fetus to ionizing radiation. Before a pregnant patient is accepted for an MRI examination, a risk–benefit analysis of the request should be made. Pregnant staff members are advised to remain outside the controlled area (10 gauss line) and to avoid exposure to gradient or RF fields.
MRI contrast agents should only be used during pregnancy with extreme caution11 (see Chapter 2).
References
1. Hartwig, V, Giovannetti, G, Vanello, N, et al. Biological effects and safety in magnetic resonance imaging: a review. Int J Res Public Health. 2009; 6(6):1778–1798.
2. De Vocht, F, Stevens, T, van Wendel De Joode, B, et al. Acute neurobehavioral effects of exposure to static magnetic fields: analysis of exposure–response relations. J Magn Reson Imaging. 2006; 23:291–297.
3. Chakeres, DW, Kangarlu, A, Boudoulas, H, et al. Effect of static magnetic field exposure of up to 8T on sequential human vital sign measurements. J Mag Res Imaging. 2003; 18(3):346–352.
4. Shellock, FG, Spinazzi, A. MRI Safety Update 2008: Part 2, Screening Patients for MRI. Am J Roentgenol. 2008; 191(4):1140–1149.
5. Shinbane, JS, Colletti, PM, Shellock, FG. Magnetic resonance imaging in patients with cardiac pacemakers: era of “MR Conditional” designs. J Cardiovasc Magn Reson. 2011; 13(1):63.
6. The International Commission on Non-Ionizing Radiation Protection. Medical magnetic resonance (MR) procedures: protection of patients. Health Physics. 2004; 87(2):197–216.
7. Nyenhuis, JA, Bourland, JD, Kildishev, AV, et al. Health effects and safety of intense gradient fields. In: Shellock FG, ed. Magnetic Resonance Procedures: Health Effects and Safety. New York: CRC Press; 2001:31–53.
8. Chavhan, GB, Babyn, PS, Singh, M, et al. MR imaging at 3. 0T in children: technical differences, safety issues, and initial experience. RadioGraphics. 2009; 29(5):1451–1466.
9. Kanal, E, Barkovich, AJ, Bell, C, et al. ACR guidance document for safe MR practices. Am J Roentgenol. 2007; 188(6):1447–1474.
10. Shellock, FG, Reference Manual for Magnetic Resonance Safety, Implants, and devices. Biomedical Research Publishing Company, Los Angeles, 2007. www. mrisafety. com
11. Wang, PI, Chong, ST, Kielar, AZ, et al. Imaging of pregnant and lactating patients: Part 1, Evidence-based review and recommendations. Am J Roentgenol. 2012; 198(4):778–784.
Ultrasonography
Children
US examination in children can, in most cases, be performed with no preparation apart from explanation and reassurance to both child and parent. In some cases where the child is excessively frightened or where immobility is required, sedation may be necessary. With echocardiography in infants, sedation is essential to obtain optimal recordings. The sedation regimens described in Chapter 18 may be used.