Gastrointestinal Anatomy and Physiology
The critical care nurse must have a comprehensive knowledge of the anatomy and normal function of the GI tract to facilitate assessment, diagnosis, and intervention in patients with GI dysfunction. The GI tract consists of the mouth, the esophagus, the stomach, the small intestine, and the large intestine (Fig. 28-1).
Mouth
The mouth and accessory organs, which include the lips, cheeks, gums, tongue, palate, and salivary glands, perform the initial phases of digestion, which are ingestion, mastication, and salivation.1
Ingestion and Mastication
The mouth is the beginning of the alimentary canal (see Fig. 28-1) and is the means for ingestion and entry of nutrients. The teeth cut, grind, and mix food, transforming it into a form suitable for swallowing and increasing the surface area of food available to mix with salivary secretions. Healthy dentition is vital for this process. Mucous glands located behind the tip of the tongue and serous glands located at the back of the tongue aid in the lubrication of food and in its distribution over the taste buds.2
Salivation
Salivation has an important role in the first stage of digestion because saliva lubricates the mouth, facilitates the movement of the lips and the tongue during swallowing, and washes away bacteria. Saliva consists of approximately 99.5% water,3 which contains a large amount of ions such as potassium, chloride, bicarbonate,1 thiocyanate, and hydrogen;3 immunoglobulin A, which is vital for destroying oral bacteria;1 and mucus. Approximately 1000 to 1500 milliliters (mL) of saliva is produced each day by three pairs of major salivary glands: (1) the submandibular glands, (2) the sublingual glands, and (3) the parotid glands. Parotid gland secretions are enzymatic, containing amylase (ptyalin), which begins the chemical breakdown of large polysaccharides into dextrins and sugars. The mouth and pharynx also are lined with minor salivary glands that provide additional lubrication.3
The salivary glands are regulated by the autonomic nervous system, with parasympathetic effects being predominant. Increased parasympathetic stimulation results in profuse secretions of watery saliva, whereas decreased parasympathetic stimulation results in inhibition of salivation.1,3
Esophagus
The esophagus is a hollow muscular tube that lacks cartilage. In adults, it is 23 to 25 cm (9 to 10 inches) long and 2 to 3 cm (1 inch) wide. It is the narrowest part of the digestive tube and lies posterior to the trachea and the heart, with attachments at the hypopharynx and at the cardiac portion of the stomach below the diaphragm. It begins at the level of the C6 to T1 vertebrae and extends vertically through the mediastinum and diaphragm to the level of T11.4
The esophagus has two sphincters: (1) the upper esophageal sphincter (also known as hypopharyngeal sphincter) and (2) the lower esophageal sphincter (also known as cardioesophageal or gastroesophageal sphincter).4 The upper esophageal sphincter inhibits air from entering the esophagus during respiration. The lower esophageal sphincter controls the passage of food into the stomach and prevents reflux of gastric contents.1
Swallowing
The functions of the esophagus are to accept a bolus of food from the oropharynx, to transport the bolus through the esophageal body by gravity and peristalsis, and to release the bolus into the stomach through the lower esophageal sphincter. This process is known as swallowing.5 Peristalsis consists of waves of circular muscle contractions and relaxations. Peristalsis that is initiated by swallowing is known as primary peristalsis, whereas peristalsis that is initiated by esophageal distention is known as secondary peristalsis. Peristaltic waves begin in the pharynx and move distally at a rate of 2 to 6 cm per second.1
Stomach
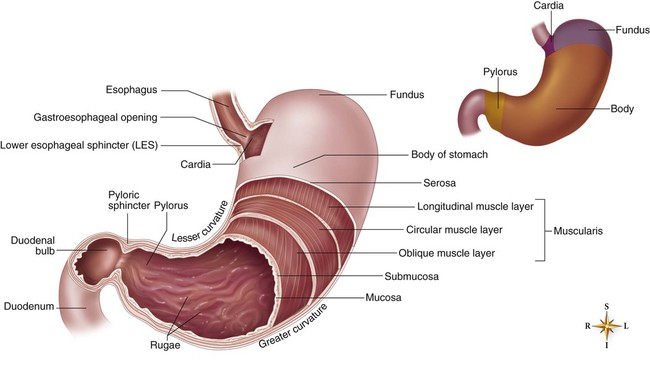
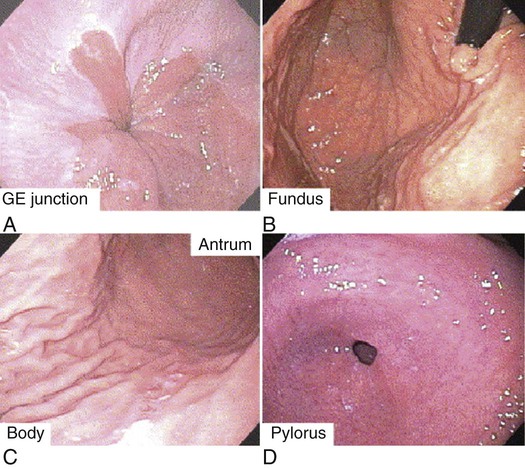
The stomach is an elongated pouch that is approximately 25 to 30 cm (10 to 12 inches) long and 10 to 15 cm (4 to 6 inches) wide at the maximal transverse diameter (Fig. 28-2). It lies obliquely beneath the cardiac sphincter at the esophagogastric junction and above the pyloric sphincter, next to the small intestine. The anatomic divisions of the stomach are the cardia (proximal end), the fundus (portion above and to the left of the cardiac sphincter), the body (middle portion), the antrum (elongated, constricted portion), and the pylorus (distal end connecting the antrum to the duodenum) (Fig. 28-3). The greater curvature, which begins at the cardiac orifice and arches backward and upward around the fundus, is in contact with the transverse colon and the pancreas at the posterior edge. The lesser curvature extends from the cardia to the pylorus. Two sphincters control the rate of food passage: (1) the lower esophageal sphincter at the esophagogastric junction and (2) the pyloric sphincter at the gastroduodenal junction.6
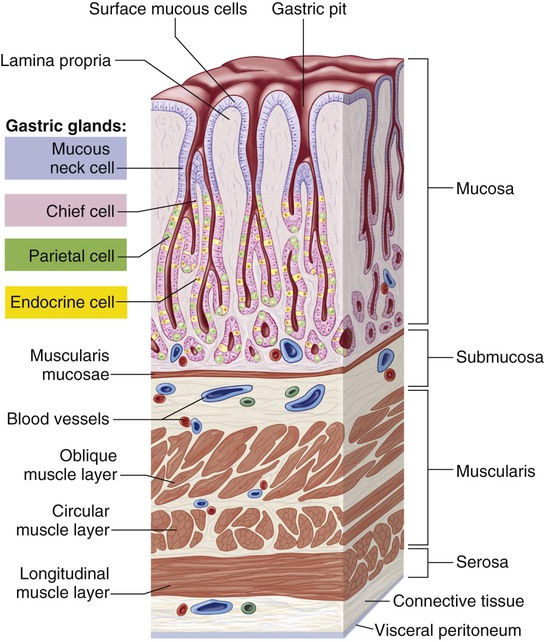
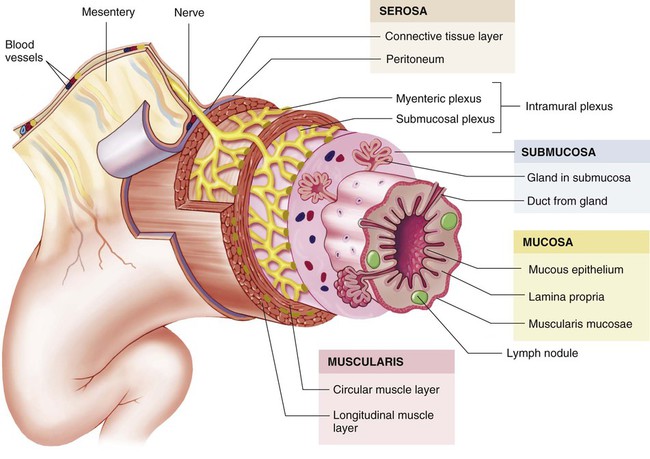
The stomach wall has four layers (Fig. 28-4). The outermost layer, the serous layer (serosa), consists of squamous epithelial tissue and continues as a double fold from the lower edge of the stomach to cover the intestine. The second layer, the muscular layer (muscularis), extends from the fundus to the antrum and consists of three smooth muscle layers, which are the longitudinal layer, the circular layer, and the oblique layer. The third layer, the submucous layer (submucosa), consists of connective tissue that contains blood vessels, lymphatics, and nerve plexuses. The innermost layer, the mucous layer (mucosa), consists of a muscular layer that is arranged in longitudinal folds, or rugae, that can expand as the stomach fills.6 This layer also contains glands that secrete about 1500 mL of gastric juice per day.7
The celiac artery provides the blood supply required for the motor and secretory activities of the stomach. The splenic vein provides venous drainage for the right side of the stomach, and the gastric vein provides it for the left.1 Numerous lymphatic channels arise in the submucosa and terminate in the thoracic duct. The stomach is innervated by the autonomic nervous system. Sympathetic fibers arise from the celiac plexus, and parasympathetic fibers arise from the gastric branch of the vagus nerve.6
The epithelial cells of the gastric mucosa are packed very close together and serve as a protective barrier, preventing diffusion of hydrogen ions into the mucosa. The surface epithelial cells produce alkaline mucus and secrete a bicarbonate-laden fluid. The mucus further protects the gastric mucosa by delaying back-diffusion of hydrogen ions and trapping them for neutralization by the secreted bicarbonate.7 The gastric mucosal cells can compensate for cell destruction. Epithelial cells are in a constant state of growth, migration, and desquamation, and they are shed at a rate of one half million cells per minute. The gastric mucosa also has the ability to increase blood flow, providing an additional buffer for acid neutralization and aiding in the removal of toxic metabolites and chloride ions from injured mucosa. The gastric mucosal cells synthesize a family of unsaturated fatty acids known as prostaglandins. Prostaglandins facilitate mucosal bicarbonate secretion and inhibit acid secretion by preventing the activation of parietal cells by histamine (a local biochemical mediator). Certain lipid-soluble substances such as alcohol, aspirin, and other nonsteroidal anti-inflammatory drugs, regurgitated bile, and uremic toxins, can break through the mucosal barrier and penetrate the cells, causing their destruction, edema, and eventual bleeding.7
Gastric Secretion
The stomach has two types of glands—oxyntic (also known as gastric glands), and pyloric—that contain cells of various types that secrete 1500 to 2400 mL of gastric juice into the lumen per day, depending on the diet and other stimuli.7 Gastric juice is composed of hydrochloric acid (HCl), pepsin (necessary for the breakdown of protein), mucus, intrinsic factor (necessary for vitamin B12 absorption), sodium, and potassium. Pepsinogen, secreted by the chief cells of the stomach lining, is converted to its active form, pepsin, in the acidic environment of the stomach.1 The cardiac glands secrete mucus and pepsinogen. The oxyntic glands contain parietal cells, which secrete HCl and intrinsic factor, and chief cells, which secrete pepsinogen. Pyloric glands contain mucous cells, which secrete mucus and pepsinogen, and G-cells, which secrete gastrin (Table 28-1).6 Gastric glands are stimulated by the parasympathetic stimulation and gastrin and inhibited by gastric-inhibitory peptide and enterogastrone. Histamine and entero-oxyntin also stimulate the parietal cells to produce acid, and secretin stimulates the chief cells to produce pepsinogen.1
TABLE 28-1
| SOURCE | HORMONE | STIMULUS FOR SECRETION | ACTION |
| Mucosa of the stomach | Gastrin | Presence of partially digested proteins in the stomach | Stimulates gastric glands to secrete hydrochloric acid and pepsinogen; growth of gastric mucosa; promotes gastric motility |
| Histamine | Acid in the stomach | Stimulates acid secretion | |
| Somatostatin | Acid in the stomach | Inhibits acid and pepsinogen secretion and release of gastrin | |
| Acetylcholine | Vagus and local nerves in stomach | Stimulates release of pepsinogen and acid secretion | |
| Gastrin-releasing peptide (bombesin) | Vagus and local nerves in stomach | Stimulates gastrin and release of pepsinogen and acid secretion | |
| Mucosa of the small intestines | Motilin | Presence of acid and fat in the duodenum | Increases gastrointestinal (GI) motility |
| Secretion | Presence of chyme (acid, partially digested proteins, and fats) in the duodenum | Stimulates pancreas to secrete alkaline pancreatic juice and liver to secrete bile; decreases GI motility; inhibits gastrin and gastric acid secretion | |
| Cholecystokinin | Presence of chyme (acid, partially digested proteins, and fats) in the duodenum | Stimulates gallbladder to eject bile and pancreas to secrete alkaline fluid; decreases gastric motility; constricts pyloric sphincter; inhibits gastrin; delays gastric emptying | |
| Enteroglucogon | Intraluminal fats and carbohydrates | Weakly inhibits gastric and pancreatic secretion and enhances insulin release, lipolysis, ketogenesis, and glycogenolysis; delays gastric emptying | |
| Gastric-inhibitory peptide (GIP) | Fat and glucose in small intestine | Inhibits gastric secretion and gastric emptying, stimulates insulin release | |
| Peptide YY | Intraluminal fat and bile acids | Inhibits postprandial gastric acid and pancreatic secretion and delays gastric and small bowel emptying | |
| Pancreatic polypeptide | Protein, fat, and glucose in small intestine | Decreases pancreatic bicarbonate | |
| Vasoactive intestinal peptide | Intestinal mucosa and muscle | Relaxes intestinal smooth muscle, increases blood flow |
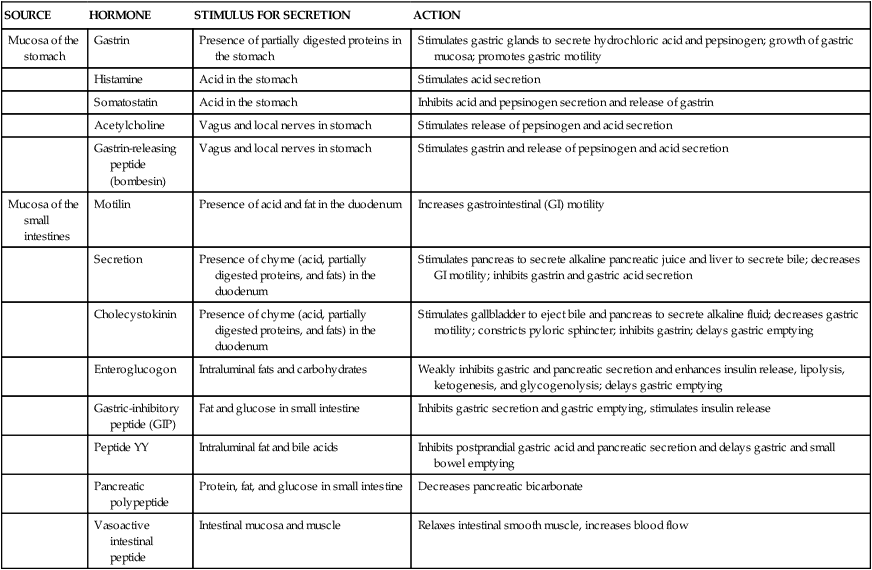
Modified from Johnson LR. Gastrointestinal Physiology. 7th ed. St. Louis: Mosby; 2007.
Data from Schubert ML, Peura DA. Control of gastric acid secretion in health and disease. Gastroenterology. 2008;134(7):1842-1860; Wren AM, Bloom SR. Gut hormones and appetite control. Gastroenterology. 2007;132(6):2116-2130.
The pH of gastric juice is 1.0, but when mixed with food, it rises to 2.0 to 3.0. Gastric juice dissolves soluble foods and has bacteriostatic action against swallowed microorganisms. The composition of gastric secretions depends on a variety of factors, including flow rate, volume, and the time of day. Pain, fear, or rage can inhibit gastric secretion, whereas aggression or hostility can stimulate it.1
Gastric Motility
The functions of the stomach include food storage, digestion, and emptying. The stomach receives food through the lower esophageal sphincter, stores it for a period, and mixes it with gastric secretions. The food is then ground into a semifluid consistency called chyme, which is delivered through the pylorus to the duodenum. Gastric motility is regulated by the autonomic nervous system, digestive hormones, and neural reflexes. Gastrin, motilin (see Table 28-1), and parasympathetic stimulation increase gastric motility, whereas secretin, cholecystokinin, enterogastrone, gastric-inhibitory peptide (see Table 28-1), and sympathetic stimulation decrease it. The ileogastric reflex inhibits gastric motility when the ileum is distended.8
Small Intestine
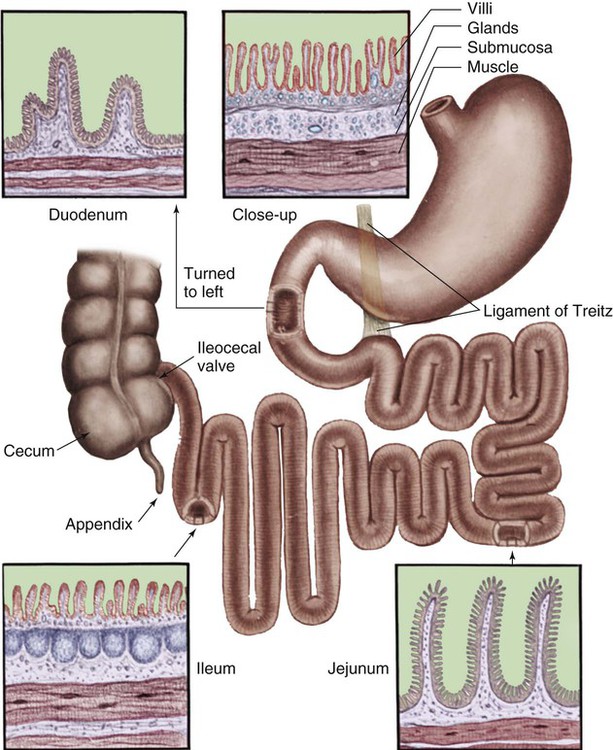
The small intestine, a coiled, folded tube that is approximately 7 m (22 to 23 feet) long, extends from the pyloric sphincter to the cecum and fills most of the abdominal cavity. It has three anatomic divisions: (1) the duodenum, (2) the jejunum, and (3) the ileum. The duodenum, shaped like the letter C, begins at the pyloric sphincter of the stomach and ends at the ligament of Treitz. It is 30 cm (12 inches) long and 4 cm (1 to 1.5 inches) wide.9 The jejunum, which is 250 cm (8 to 9 feet) long and 4 cm (1 to 1.5 inches) wide, lies in the left iliac and umbilical regions. The ileum, which is 375 cm (12 feet) long and 2.5 cm (1 inch) wide, lies in the hypogastric, right iliac, and pelvic regions. Although the demarcating line between the jejunum and the ileum is somewhat arbitrary, the ileum is narrower than the jejunum. The ileocecal valve, located at the terminal end of the ileum at the junction of the cecum and colon, controls the flow of small bowel contents into the large intestine and prevents reflux (Fig. 28-5).1
The small intestine has four layers (Fig. 28-6). The outermost layer, the serous layer (serosa), is a continuation of the serous coat surrounding the stomach. The second layer, the muscular layer (muscularis), consists of two smooth muscle layers called the longitudinal and circular layers. The third layer, the submucous layer (submucosa), consists of connective tissue that contains blood vessels, lymphatics, glands, and nerve plexuses. The innermost layer, the mucous layer (mucosa), consists of simple columnar epithlelium.5 The mucosa and submucosa are arranged in circular folds (plicae circulares),5 which are largest and most numerous in the jejunum and upper ileum.1 These folds are covered by a second series of projectile-like folds called villi, which are in constant motion—constricting, lengthening, and shortening (villous movement). The four to five million villi (see Fig. 28-5) give the intestine a velvety appearance; they are more numerous and larger in the jejunum than in the ileum. Villi contain a network of capillaries and blind lymphatic vessels called lacteals. The outer layer of the villus is composed of microvilli. The circular folds of the small intestine, along with the villi and microvilli, increase the digestive-absorptive surface of the small intestine 600 times.9,10
The gastroduodenal artery provides the blood supply for the duodenum, and branches of the superior mesenteric artery provide for the jejunum and the ileum. The superior mesenteric vein provides for venous drainage of the small intestine.11 Numerous lymphatic channels arise in the submucosa and terminate in the thoracic duct. The small intestine is extrinsically innervated by the autonomic nervous system. Sympathetic fibers arise from the celiac plexus, whereas parasympathetic fibers arise from the gastric branch of the vagus nerve. Intrinsic innervation, which initiates motor functions, is provided by Auerbach’s plexus and Meissner’s plexus, which are located in the intestinal wall.1
Intestinal Secretion
The small intestine has two major types of glands: (1) Brunner’s glands and (2) intestinal glands. Brunner’s glands lie in the mucosa of the duodenum and secrete mucus, an alkaline fluid (pH of 9) that neutralizes chyme and protects the mucosa.10 Intestinal glands are found in pits of the submucosa and are called the crypts of Lieberkühn. These crypts secrete 2 to 3 liters (L) per day of yellow fluid containing enzymes that assist in nutrient digestion.7
Intestinal Motility
Intestinal motility consists of two separate motions: (1) peristalsis and (2) haustral segmentation. Peristalsis is sequential contraction and relaxation of short segments of the small intestine that facilitate digestion and absorption. Haustral segmentation is rhythmic contractions that facilitate the mixing and forward movement of chyme. It is controlled by Auerbach’s plexus. Intestinal motility is also affected by neural reflexes located along the length of the small intestine. Motility is inhibited by the intestino-intestinal reflex, which is activated by distention of the small intestine, and is stimulated by the gastroileal reflux, which is initiated by an increase in gastric motility.12
Digestion and Absorption
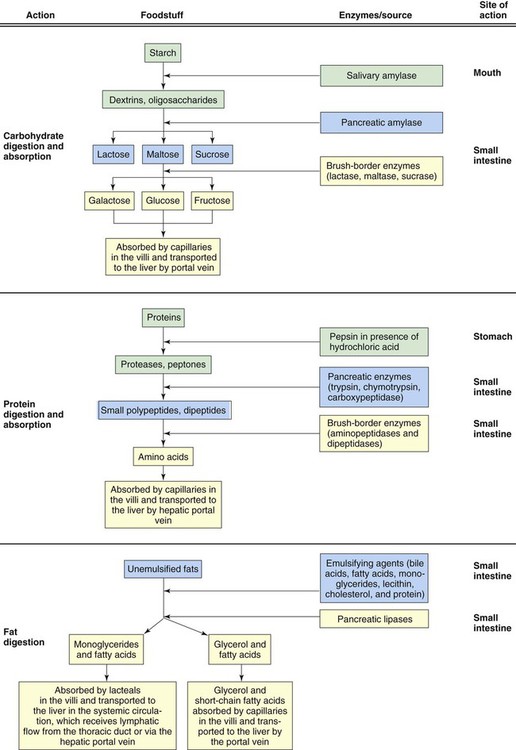
The functions of the small intestine include digestion and absorption. Digestion, which involves breaking down large molecules into small ones, is essential for nutrient absorption from the small intestine (Fig. 28-7). Maintenance of pH and osmolality is crucial for digestion in the small intestine. The entry of chyme into the duodenum stimulates the production of secretin, which stimulates the pancreas to secrete a highly alkaline fluid into the duodenum. In the small intestine, chyme mixes with pancreatic enzymes, intestinal enzymes, and bile from the liver and gallbladder, and it is then reduced to absorbable elements of proteins, fats, and carbohydrates. The nutrients are absorbed through the villi and transported to the liver by the portal system for further processing. The small intestine absorbs up to 8 L of fluid per day, passing only a small part of this fluid into the large intestine. In addition to the nutrients, electrolytes, water, components of saliva, gastric juice, and bile, intestinal and pancreatic secretions are also absorbed.1
Large Intestine
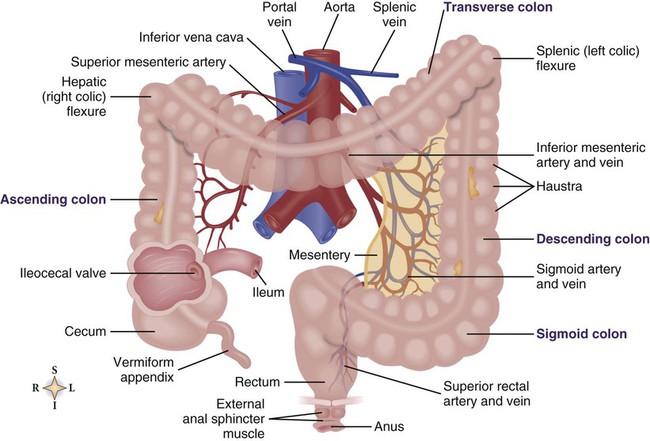
The large intestine, which extends from the ileocecal valve to the anus, is approximately 90 to 150 cm (4 to 5 feet) long and 4 to 6 cm (2 inches) in diameter. It is divided into the ascending colon, the hepatic flexure, the transverse colon, the splenic flexure, the descending colon, the sigmoid colon, the rectum, and the anal canal (Fig. 28-8).10
The colon has four layers. The outermost layer, the serous layer (serosa), is formed from the visceral peritoneum and covers most of the large intestine, with the exclusion of the sigmoid colon. The second layer, the muscular layer (muscularis), consists of two smooth muscle layers: the longitudinal and the circular muscles. These muscles work together to propel fecal matter through the colon and to “knead” the stool into a compact bolus. The longitudinal muscle consists of three muscular bands that stretch from the cecum to the distal sigmoid colon. These muscular bands create sacculations of haustra, important clinical features that normally are apparent on a barium enema radiograph. Haustra aid segmentation so that absorption of fluid from the fecal bolus is achieved. The third layer, the submucous layer (submucosa), consists of connective tissue that contains blood vessels, lymphatics, glands, and nerve plexuses. The innermost layer, the mucous layer (mucosa), is lined with simple columnar epithelial cells and contains deep crypts of Lieberkühn that are lined with mucus-producing goblet cells. The mucus eases the passage of the fecal material and protects the mucosal surface from trauma.10
Arterial blood is supplied to the colon from branches of the superior and inferior mesenteric arteries. Venous drainage occurs through the branches of the superior and inferior mesenteric veins into the portal system. The colon is intrinsically innervated by Auerbach’s plexus, which controls secretion and motility and is extrinsically innervated by the autonomic nervous system. The sympathetic and parasympathetic branches of the autonomic system innervate the colon, regulating motility. Sympathetic stimulation inhibits colonic activity and constricts the anal sphincters, whereas parasympathetic stimulation increases colonic activity and secretion and relaxes the anal sphincters.9
Colonic Motility
Colonic motility consists of haustral shuttling and peristalsis. Haustral shuttling, a variation of haustral segmentation, consists of the contraction and relaxation of the circular muscle. It moves the contents of the colon back and forth to facilitate the grinding of food masses and fluid absorption. Peristalsis is produced primarily by the longitudinal muscles and propels the fecal bolus forward. Mass peristalsis is a strong, slow contraction in which the distal left colon contracts en masse to move the fecal bolus into the rectum.13
Resorption
The major functions of the colon are resorption of water, sodium, chloride, glucose, and urea; dehydration of undigested residue; putrefaction of contents by bacteria; movement of the fecal bolus through the colon; and elimination of the fecal mass. The colon receives approximately 1000 to 2000 mL of chyme per day, and all but 50 to 250 mL of it is absorbed in the ascending and transverse colon.5
The colon contains billions of anaerobic bacteria that putrefy remaining proteins and indigestible residue; synthesize folic acid, vitamin K, nicotinic acid, riboflavin, and some B vitamins; and convert urea salts to ammonium salts and ammonia for absorption into the portal circulation.1 Common colonic bacteria include Bacteroides, Lactobacillus, and Clostridium.14
Accessory Organs
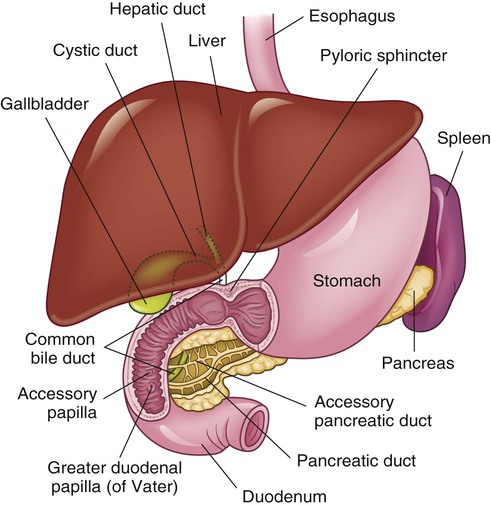
The accessory organs of digestion are the liver, the biliary system, and the pancreas (Fig. 28-9).
Liver
The liver is the largest internal organ in the body. Weighing 1200 to 1600 g (3 to 4 pounds), it is friable and dark red in color and has a soft-solid consistency. Located in the right upper abdominal quadrant, it fits snugly against the right interior diaphragm. The liver is surrounded by connective tissue known as Glisson’s capsule, which is covered by serosa and contains blood vessels and lymphatics. The peritoneum covering the liver forms the falciform ligament, which attaches the liver to the anterior portion of the abdomen between the diaphragm and umbilicus and divides the liver into two main lobes, right and left (see Fig. 28-8). The right lobe, which is six times larger than the left, has three sections: the right lobe proper, the caudate lobe, and the quadrate lobe. The left lobe is divided into two sections. Each lobe is divided into numerous lobules.10,15
The liver receives one third of the total cardiac output from two major sources: (1) the hepatic artery, which provides oxygenated blood; and (2) the portal vein, which is supplied with nutrient-rich blood from the gut, pancreas, spleen, and stomach (Fig. 28-10). The portal vein, which accounts for 75% of the total liver blood flow, branches into sinusoids to transport blood to each lobule. Unlike capillaries, sinusoids lack a definite cell wall but contain a lining of phagocytic (Kupffer) cells and some nonphagocytic cells of modified epithelium. Sinusoids empty blood into an intralobular vein in the center of the lobule. Intralobular veins empty into larger veins and then into the hepatic vein, which empties on the posterior surface of the liver and eventually into the vena cava. The hepatic artery also divides and subdivides between the lobules, supplying sinusoids with oxygenated blood before emptying into the hepatic vein. Lymphatic spaces are located between liver cells. Lymph drains into lymphatic vessels that surround the hepatic vein and bile ducts.15
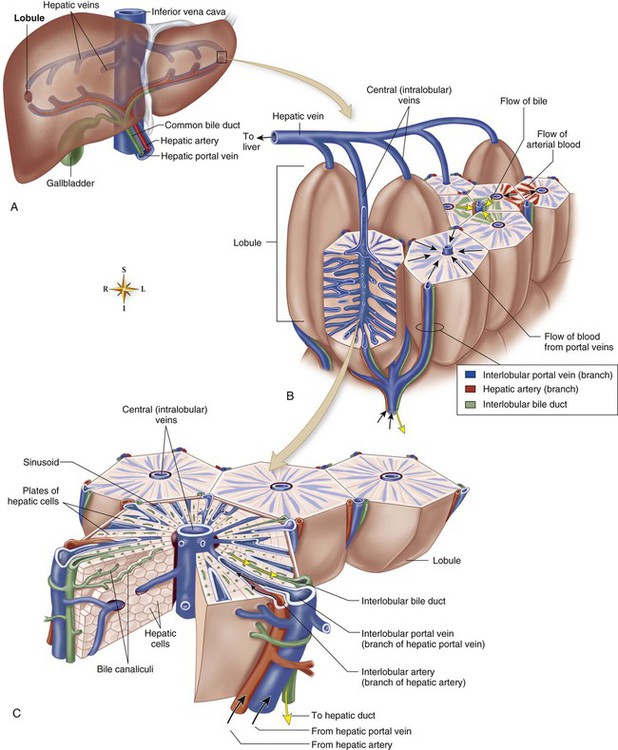
A, This diagram shows the location of liver lobules relative to the overall circulatory scheme of the liver. B and C, Enlarged views of several lobules show how blood from the hepatic portal veins and hepatic arteries flows through sinusoids and, thus, past plates of hepatic cells toward a central vein in each lobule (black arrows). Hepatic cells form bile, which flows through bile canaliculi toward hepatic ducts that eventually drain the bile from the liver (yellow arrows). (From Patton KT, Thibodeau GA. Anatomy & Physiology. 8th ed. St. Louis: Mosby; 2013.)
Nutrient Metabolism
The liver plays a key role in metabolizing and storing carbohydrates, fats, proteins, and vitamins. Glycogen, the stored form of glucose, can be synthesized from glucose or from protein, fat, or lactic acid. Glycogen is broken down to glucose by the liver to maintain normal blood glucose levels. The liver also has a vital role in amino acid metabolism and can synthesize amino acids from metabolites of carbohydrates and fats or can deaminate amino acids to produce ketoacids and ammonia, from which urea is formed. In fat metabolism, the liver hydrolyzes triglycerides to glycerol and fatty acids in the process of ketogenesis and synthesizes phospholipids, cholesterol, and lipoproteins.10,15
Hematologic Function
The liver synthesizes plasma proteins such as globulins and albumin, which are important in maintaining the normal osmotic balance of blood. It also synthesizes a number of clotting factors, including fibrinogen and prothrombin. Kupffer cells destroy worn red blood cells, and hepatocytes conjugate bilirubin (byproduct of red cell destruction) for excretion.10,15
Bile
The production of bile makes the liver a vital organ in digestion and absorption. The major components of bile are bile pigments, bile salts, cholesterol, neutral fats, phospholipids, inorganic salts, fatty acids, mucin, conjugated bilirubin, lecithin, and water. Traces of albumin, gammaglobulin, urea, nitrogen, and glucose are also present in bile. The principal electrolytes of bile are sodium, chloride, and bicarbonate.15
Bile emulsifies fat globules and absorbs fat-soluble vitamins. Bile salts also serve as an excretion route for bilirubin, cholesterol, and various hormones. Approximately 80% of bile salts are actively resorbed in the distal ileum and are recycled to the liver through the enterohepatic circulation; only 20% are lost in feces.1
Bilirubin
The primary bile pigment, bilirubin, is formed from the heme portion of hemoglobin during the degradation of red blood cells by Kupffer cells. When released into the bloodstream, bilirubin binds to albumin as fat-soluble, unconjugated bilirubin. Taken up by liver hepatocytes, unconjugated bilirubin is conjugated with glucuronic acid to form water-soluble, conjugated bilirubin, which is then excreted through hepatic ducts into the large intestine. If the amount of bilirubin sent to the liver is in excess, the ability of the liver to conjugate the bilirubin may be taxed; free, unconjugated or indirect bilirubin appears in the blood. High levels of unconjugated bilirubin in the blood suggest hepatocellular dysfunction, whereas high levels of conjugated bilirubin suggest biliary tract obstruction.1
Biliary System
The biliary system (Fig. 28-11) consists of the gallbladder and its related ductal system, including the hepatic, cystic, and common bile ducts. The hepatic duct, from the liver, joins the cystic duct, from the gallbladder, to form the common bile duct, which empties into the duodenum. The common bile duct is surrounded by Oddi’s sphincter, which pierces the wall of the duodenum and controls the flow of bile into the duodenum. The gallbladder is a pear-shaped organ that is 7 to 10 cm (3 to 4 inches) long and 2.5 to 3.5 cm (approximately 1 inch) wide, lying on the underside of the liver (see Fig. 28-9). It is attached to the liver by connective tissue, peritoneum, and blood vessels.10,16
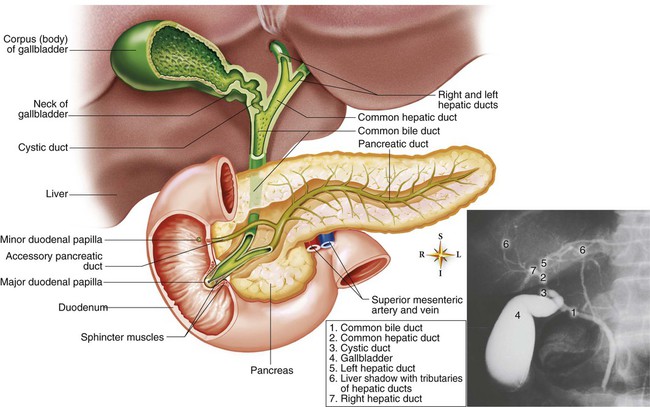
Bile
The main functions of the gallbladder are to collect, concentrate, acidify, and store bile. Bile is continuously formed in the liver and excreted into the hepatic duct for transport to the gallbladder through the cystic duct. The gallbladder can store up to 90 mL of bile and concentrate it approximately 15 to 29 times by removing approximately 90% of the water. Cholesterol and pigment are likewise concentrated. Bile, which is golden or orange-yellow in the liver, becomes dark brown when concentrated in the gallbladder. By altering its shape and volume, the gallbladder regulates pressure within the biliary system. Relaxation of the sphincter of Oddi is coordinated with gallbladder contraction through the regulatory action of cholecystokinin. Such factors as sight, smell, and taste can stimulate gallbladder contraction, whereas fear or excitement can decrease contraction. After a meal, the amount of bile entering the duodenum increases as a result of enhanced liver secretion and gallbladder contraction. Intestinal secretion of cholecystokinin and secretin, high levels of bile salts in the blood, and vagal stimulation increase biliary secretion.15
Pancreas
The pancreas is a soft, lobulated, fish-shaped gland (see Fig. 28-11) lying beneath the duodenum and the spleen (see Fig. 28-9). The pinkish-yellow organ is 15 to 20 cm (6 to 8 inches) long and 5 cm (1 to 1.5 inches) wide. Its anatomic divisions include the head, which lies in the C-shaped curve of the duodenum to which it is attached; the body, the main part of the gland, which extends horizontally across the abdomen and is largely hidden behind the stomach; and the tail, a thin, narrow portion in contact with the spleen. The main pancreatic duct, called the duct of Wirsung, traverses the entire length of the organ. The duct of Wirsung empties exocrine secretions into the ampulla of Vater, which is the same lumen draining the common bile duct, at the entrance to the duodenum.10
The internal structural unit of the pancreas is the lobule, consisting of numerous small ducts with secretory cells called tubuloacinar cells. Each acinus has a small duct that empties into lobular ducts. Lobules are joined by connective tissue into lobes, which unite to form the gland. The ducts from each lobule empty into the duct of Wirsung.10
Arterial blood supply to the pancreas is provided by branches of the superior mesenteric artery and celiac arteries. Venous drainage of the head of the pancreas occurs through the portal vein, and drainage of the body and tail occurs through the splenic vein. The pancreas is innervated by the autonomic nervous system. Sympathetic stimulation decreases pancreatic secretion, and parasympathetic stimulation increases it.10
Exocrine Functions
Exocrine functions of the pancreas are limited to digestion. Acinar cells secrete pancreatic juice, which consists of water, sodium bicarbonate, and electrolytes at a highly alkaline pH. Enzymes produced in the pancreas include trypsin, chymotrypsin, carboxypeptidase, amylase, and lipase. The pancreas also produces a trypsin inhibitor that prevents activation of trypsinogen (inactive form of trypsin), which inhibits autodigestion. Autodigestion is the underlying cause of acute pancreatitis. Pancreatic exocrine function is regulated by digestive hormones. Signals provided primarily by the intestinal hormones secretin and cholecystokinin stimulate the pancreas to secrete pancreatic juice. The two hormones potentiate each other’s effects on the pancreas.17
Endocrine Functions
Endocrine tissue in the pancreas consists of spherical islets called islets of Langerhans, which are embedded within the lobules of acinar tissue throughout the pancreas, especially in the distal body and tail. Endocrine products include insulin, which is produced in beta cells; glucagon, which is produced in alpha cells; and gastrin. All of these hormones are secreted directly into the bloodstream.17
Summary
Anatomy
• The gastrointestinal (GI) tract consists of the mouth (lips, cheeks, gums, tongue, palate, and salivary glands), the esophagus, the stomach, the small intestine, and the large intestine.
• The accessory organs of digestion are the liver, the biliary system, and the pancreas.
Physiology
• The major function of the GI tract is digestion.
• Digestion is the conversion of ingested nutrients into simpler forms that can be transported from the tract’s lumen to the portal circulation and then used in metabolic processes.
• The mouth and accessory organs perform the initial phases of digestion, which are ingestion, mastication, and salivation.
• The functions of the stomach include food storage, digestion, and emptying.
• Gastric motility is regulated by the autonomic nervous system, digestive hormones, and neural reflexes.
• The functions of the small intestine include digestion and absorption.
• Intestinal motility consists of peristalsis and haustral segmentation.
• The major functions of the colon include resorption of water, sodium, chloride, glucose, and urea; dehydration of undigested residue; putrefaction of contents by bacteria; movement of the fecal bolus through the colon; and elimination of the fecal mass.
• Colonic motility consists of haustral shuttling and peristalsis.
• The functions of the liver include metabolism and storage of carbohydrates, fats, proteins, and vitamins; synthesis of plasma proteins; detoxification of drugs and toxins; and the production of bile.
• The main functions of the gallbladder are to collect, concentrate, acidify, and store bile.
• The main functions of the pancreas are digestion and glucose regulation.