CHAPTER 9 Gastric Bypass
INDICATIONS FOR SURGERY
Obesity: The specific indications for bariatric surgery continue to evolve. The National Institutes of Health issued a consensus statement in 1991 that established guidelines for identifying patients for whom the benefits of surgery outweigh the associated risks (Box 9-1). Importantly, patients weighing more than 600 pounds exceed the maximum weight capacity of many operating tables and may require staged therapy (including dietary modification) before a definitive surgery.
PREOPERATIVE EVALUATION
COMPONENTS OF THE PROCEDURE AND APPLIED ANATOMY
Preoperative Considerations
Patient Positioning and Preparation
Roux-en-Y Gastric Bypass
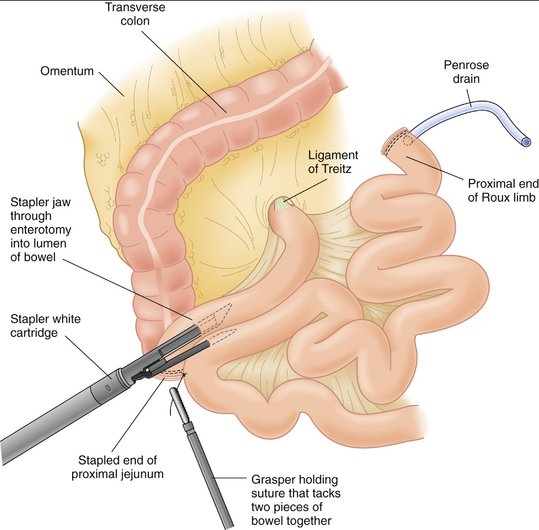
Roux-en-Y gastric bypass (Fig. 9-1) has three major components: (1) construction of the gastric pouch, (2) division of the small bowel and creation of the Roux limb, and (3) creation of an anastomosis between the gastric pouch and jejunum (gastojejunostomy). Approaches to gastric bypass include: (1) laparoscopic, (2) hand-assisted laparoscopic, and (3) open. Specific techniques related to port placement and incisions for each approach are discussed first, followed by a discussion of the components of the procedure common to all three.
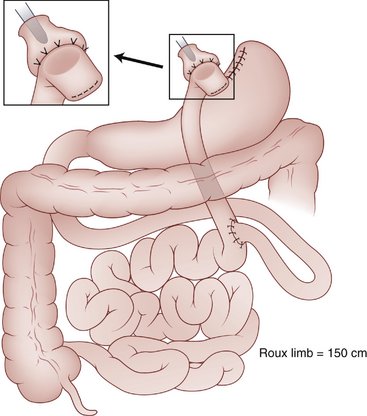
Figure 9-1 Roux-en-Y gastric bypass.
(From Kendrick ML, Dakin GF: Surgical approaches to obesity. Mayo Clin Proc 81[10 Suppl]:S18–S24, 2006.)
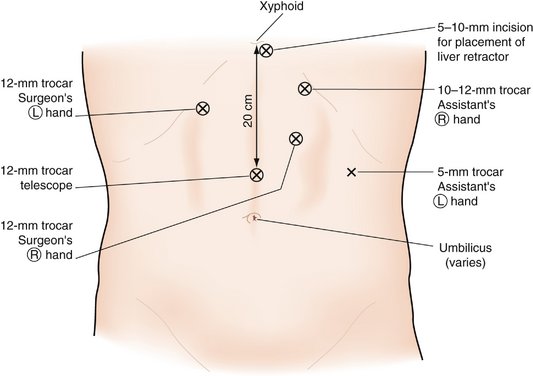
Figure 9-2 Trocar placement for laparoscopic Roux-en-Y gastric bypass.
(From Townsend CM, Beauchamp RD, Evers BM, Mattox KL [eds]: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 17th ed. Philadelphia, Saunders, 2004.)
Laparoscopic Adjustable Gastric Band
The laparoscopic adjustable gastric band has gained popularity in recent years as an alternative to RYGBP (Fig. 9-4). The band can be placed laparoscopically, with or without a hand port.
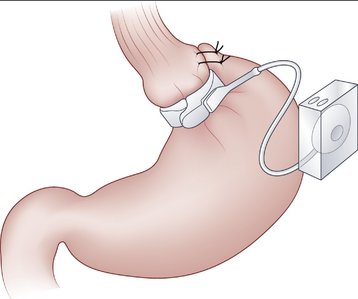
Figure 9-4 A diagram of the completed adjustable gastric band.
(From Kendrick ML, Dakin GF: Surgical approaches to obesity. Mayo Clin Proc 81[10 Suppl]:S18–S24, 2006.)
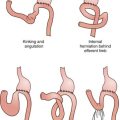
COMPLICATIONS
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753-761.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724-1737.
Kendrick ML, Dakin GF. Surgical approaches to obesity. Mayo Clin Proc. 2006;81(10 Suppl):S18-S24.
Malinowski SS. Nutritional and metabolic complications of bariatric surgery. Am J Med Sci. 2006;331:219-225.
Schirmer BD. Morbid obesity. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 17th ed. Philadelphia: Saunders; 2004:357-399.