CHAPTER 5 Functional Evaluation of the Elbow
INTRODUCTION
Involvement of the upper limb accounts for about 10% of all compensation paid in the United States for disabling work-related injuries.47,67 In addition, dysfunction of the upper extremity cost about 5.5 million lost work days in 1977.66 Elbow function consists of three activities: (1) allows the hand to be positioned in space, (2) provides the power to perform lifting activities, and (3) stabilizes the upper extremity linkage for power and fine work activities. The essential joint functions are motion, strength, and stability. However, ultimately, the final determinant of function and the ability to perform activities of daily living is pain.
ELBOW MOTION
NORMAL MOTION
Normal flexion and forearm rotation at the elbow are adequately measured clinically with the handheld goniometer. Forearm rotation is measured with the elbow at 90 degrees of flexion, often with the subject holding a linear object, such as a pencil, to make the measurement more objective.79 In spite of obvious limitations, investigators have concluded that a standard handheld goniometric examination by a skilled observer allows measurement of elbow flexion-extension and pronation-supination with a margin of error of less than 5%.35,95 In fact, the flexion-extension intraobserver reliability correlation coefficient is 0.99.78 Different trained observers also provide measurements that are statistically equivalent.30,78
Normal passive elbow flexion ranges between 0 and 140 to 150 degrees.1,11,44,79 Greater variation of normal forearm rotation has been described but averages about 75 degrees pronation and 85 degrees supination.1,11,44,91
INVESTIGATIVE TECHNIQUES OF MEASURING COMPLEX ACTIVE MOTION
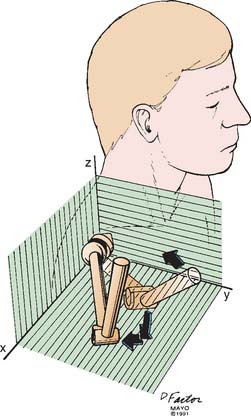
To measure the three-dimensional joint motion in daily activities, any one of several rather sophisticated experimental techniques can be used.1,95 For experimental studies, the triaxial electrogoniometer2,16,63 can simultaneously measure three-dimensional motion of more than one joint system with a high degree of reproducibility and reliability58,71 (Fig. 5-1). Video telemetry, computer-simulated motion, and electromagnetic sensors have also been developed to study three-dimensional kinematic measurement.2,71,87 Most recently, robotic techniques and miniature accelerometers and gyroscopes have been adopted to study complex upper extremity compensatory motion.49,56 For the elbow, the complex inter-relationship of shoulder and wrist function, both motion and motor activity, remains a complex and poorly understood area of investigation.32
FUNCTIONAL MOTION
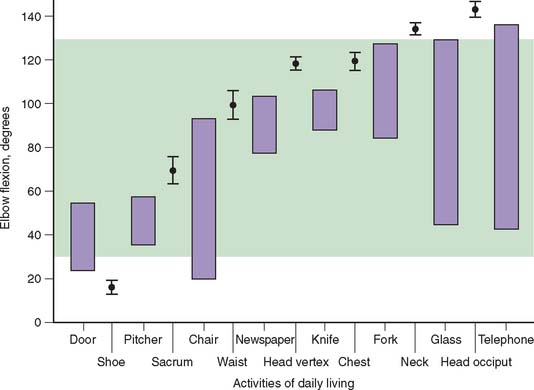
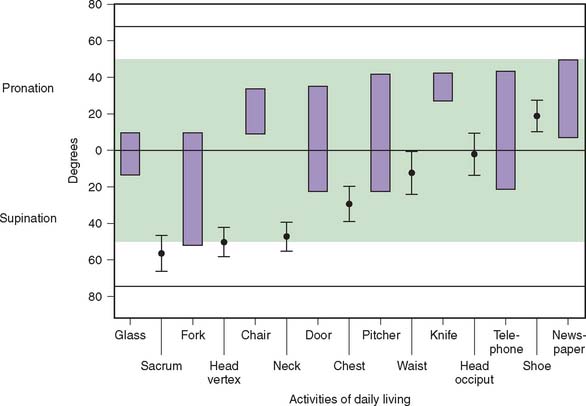
For most activities, the full potential of elbow motion is not needed or used. Loss of terminal flexion is more disabling than is the same degree of loss of terminal extension.14,70 Using the electrogoniometer just described, a study of 15 activities of daily living established that most functions can be performed using an arc of 100 degrees of flexion between 30 and 130 degrees (Fig. 5-2) and 100 degrees of forearm rotation equally divided between pronation and supination (Fig. 5-3). This has become the accepted standard for functional elbow motion.
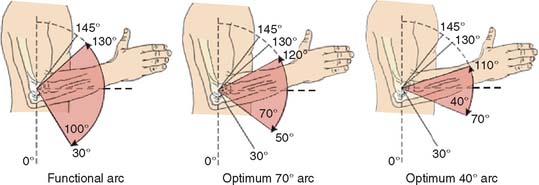
The motion requirements of the elbow joint needed for daily activities are really a measurement of the reaching ability of the hand. The extent to which this function is impaired by loss of elbow flexion or extension can be estimated analytically (Fig. 5-4). When motion is limited from 30 to 130 degrees, the potential area reached by the hand is reduced by about 20%. Thus, the range of elbow flexion between 30 and 130 degrees corresponds with about 80% of the normal reach capacity of the forearm and hand in a selected plane of shoulder motion. The functional impact of further loss of the flexion arc is also not equally distributed between flexion and extension. Our clinical experience indicates that flexion is of more value than extension in a ratio of about 2:1. Hence, a 10-degree further loss of flexion (120 degrees) is roughly equivalent to 20 degrees further loss of extension (Fig. 5-5).
The optimal position of elbow fusion to accomplish activities of daily living has been accepted as 90 degrees.86 To further assess this issue, we hypothesized that the optimal position would be associated with a minimal amount of compensatory shoulder motion.71 It was surprising to observe that for discrete and fixed positions of the elbow, increasing the amount of shoulder motion did not provide greater use or increased function. It was also noted that for greater degrees of fixed elbow flexion, efforts to perform daily functions were accompanied by a tendency of the humerus to assume a less elevated and more lateral circumduction position (Fig. 5-6). This is consistent with the mechanical functions of these two joints; a ball-and-socket joint providing rotatory motion does not provide compensatory motion for hinge-type motion that occurs only in a single plane. This investigation did confirm the accepted tenant that 90 degrees is the optimum position or “least worse” for most activities.
STRENGTH
To understand the value and limitations of clinical strength assessment, it will be helpful to briefly review the physiology of muscle contraction and major factors affecting strength.15
TYPES OF MUSCLE CONTRACTION
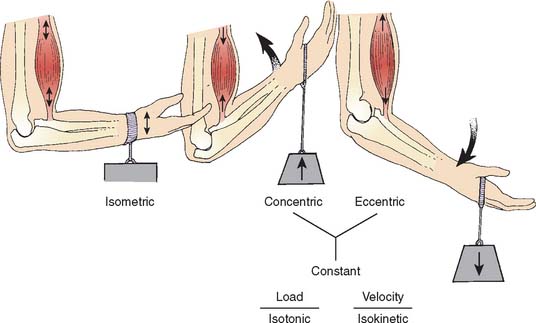
There are several types of muscle contraction classified according to changes in length, force, and velocity of contraction (Fig. 5-7).5,31,60
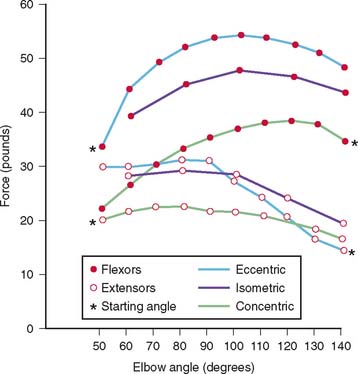
If there is no change in muscle length during a contraction, it is called isometric. When the external force exceeds the internal force of a shortened muscle and the muscle lengthens while maintaining tension, the contraction is called an eccentric, or lengthening, contraction. In contrast, if the muscle shortens while maintaining tension, a concentric contraction occurs. For elbow flexion, eccentric force exceeds isometric force by about 20%, and isometric force exceeds concentric force by about 20% (Fig. 5-8).23,85 However, it is known that eccentric exercise is associated with muscle fiber damage. This may lead to alterations in muscle receptors that can alter joint position sense.13
FORCE CONSIDERATIONS
If the muscle produces a constant internal force that exceeds the external force of the resistance, the muscle shortens, and the contraction is further characterized as isotonic. Energy use in this case is larger than that required to produce tension, which will balance the load, and the extra energy is used to shorten the muscle. If the speed of rotation of an exercising limb is predetermined and held constant, changes occur in the amount of tension developed in the muscles causing the motion. This is called an isokinetic contraction. This may be of either the concentric or eccentric type defined earlier.
Speed of Contraction
A rapidly contracting muscle generates less force than one contracting more slowly. In an isometric contraction, the velocity is zero because the resistance exceeds the ability of the muscle to move the joint. In sports, rates of motion exceeding 300 degrees per second are common. One recent study has shown that isometric training at maximum strength is more effective to increase power production than no load training at maximum velocity.88
FACTORS AFFECTING MAXIMUM MUSCLE TENSION
Muscle Length at Contraction
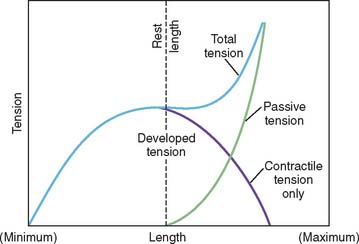
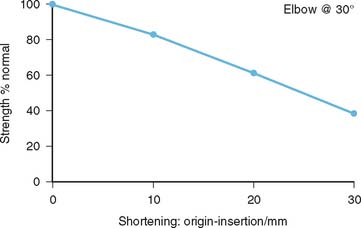
The relationship of muscle tension to muscle length is recognized by most clinicians and is presented graphically in the form of a length tension curve of an isolated muscle (Fig. 5-9).27 Recent studies suggest this concept is applicable to muscle systems at different anatomic sites.89 The exact nature of the relationship varies from muscle to muscle and from joint to joint, depending on the specific function. For example, a study in our laboratory demonstrated the relationship of triceps strength as a function of muscle shortening. A somewhat linear relationship with 1-, 2-, and 3-cm length change associated with 17%, 40%, and 63% strength reduction, respectively39 (Fig. 5-10). The length of elbow rotators change considerably over the full range of motion. The percent change at the wrist is 8; at the elbow, 55; and at the shoulder, 200.74
TECHNIQUE OF STRENGTH MEASUREMENT
In the clinic, the most common study is that of static or isometric flexion-extension strength using a simple tensiometer, or spring device (Fig. 5-11).17,52 For more accurate documentation or for investigative purposes, more sophisticated devices such as a strain gauge tensiometer25 and dynamometer21,64,76 also have been used.
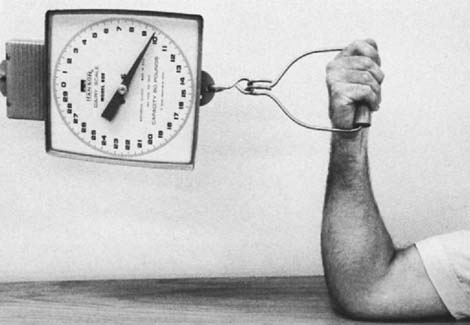
FIGURE 5-11 A simple spring tensiometer, which is used in the clinical setting to estimate elbow flexion strength.
Isokinetic strength is a more specific measurement of dynamic elbow flexion-extension function and is used more frequently today, especially for the assessment of athletic or occupational injuries. In an isokinetic muscular movement, the speed of rotation of the limb is held constant despite changes in the amount of tension developed. This isokinetic movement can be measured by means of an accommodating resistance dynamometer. Because of the accommodating load cell, the velocity of an exercising limb cannot be increased.60,72 As more force is exerted against the lever arm of the dynamometer, more resistance is encountered by the limb, and rotation occurs only at the predetermined constant speed. These devices accurately measure peak torque, the joint angle position at peak torque, the range of motion, and endurance.6 This technique is becoming increasingly useful for the measurement of elbow strength and endurance, and for more accurate study of the role of fatigue in arriving at disability estimates.84 This has proven particularly useful in assessing patients with biceps tendon reattachment.
ELBOW STRENGTH
STATIC MEASUREMENTS
Flexion Extension
Although the general tends are relatively consistent,9 absolute strength measurements are not exactly comparable owing to variations in study technique and even greater differences between individual subjects, especially correlated to body size and age.10,41
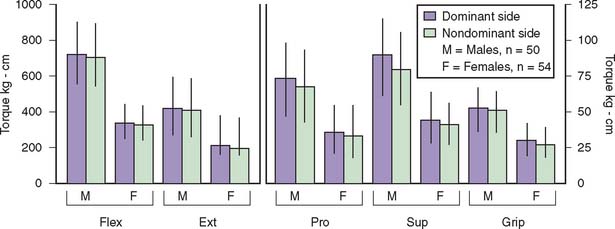
On the average, the maximum isometric torque created at the elbow joint is about 7 kg-m for men and 3.5 kg-m for women.4 Isometric muscle power is greatest during flexion at joint positions between 90 and 110 degrees.25,93 At elbow angles of 45 and 135 degrees, only about 75 percent of the maximum elbow flexion strength is generated.43,45,94 Maximum flexion strength is generated in forearm supination; forearm pronation is associated with the weakest flexion strength.18,43 Most of the torque occurs from contributions of the biceps, brachialis, and brachioradialis.28
The mean difference in isometric flexion force among the three forearm positions at various flexion angles is about 5% for women and 10% for men.25 Strengths at the neutral forearm position were slightly greater than those at the supinated and pronated positions.25,43,76,80
For elbow extension, the average maximum torque strength is about 4 kg-m for men and 2 kg-m for women (Fig. 5-12).4 Observations for 14 female and 10 male subjects showed a gradual increase in strength as the elbow was extended and the 90 degree position generates the greatest isometric extension force.20,28,53,76
In general, the dominant extremity is about 5% to 10% stronger than the nondominant side, and men are about twice as strong as women in most positions (see Fig. 5-12). The isometric force of the flexors is about 40 percent greater than the isometric force of the extensors.4,45
Supination and Pronation
The greatest supination strength is generated from the pronated position; the converse relationship is also true.17,55 In the majority of shoulder elbow positions, the average torque of supination exceeded that of pronation by about 15 to 20 degrees for males and females. This was particularly marked when the elbow was extended. On the average, isometric pronation and supination strengths for men are 80 kg-cm and 90 kg-cm, respectively, and for women are 35 kg-cm and 55 kg-cm, respectively. The dominant and nondominant strength difference in these two types of function averaged about 10% (see Fig. 5-12). In one study,83 it was found that isometric elbow strengths of rheumatoid arthritis patients decreased in proportion to an increase in the severity of x-ray findings. The flexion and supination strengths after total elbow replacement were about two times greater than before operation.
DYNAMIC FUNCTION
Fatigue is an important consideration in altered function because routine activities require repetitive actions, some of which may exceed one million cycles per year.22
The relative value of static and dynamic testing modalities is a debated issue. Motzkin and colleagues65 studied the relationship between isometric and isokinetic fatigue and found no consistent relationship. One reason for this is the marked variation even in test-retest studies of the same function.33 The one reliable association is that the eccentric contracture provides the greatest torque strength for both isometric and isokinetic testing modes.33,65
The relationship between strength and speed of movement is undefined.4 Many investigations support the hypothesis that maximum strength and the rate of movement are independent of each other.68,73 In a recent study,29 isokinetic peak torque and work were greater at the slower speed, as opposed to power, which was significantly greater at the faster speed.
ADDITIONAL VARIABLES OF STRENGTH ASSESSMENT
In addition to the factors discussed, other confounding variables to strength testing include motivation, the learning effect of repetitive tests,51,59,81 the psychological benefit derived from repetitive testing,37,54 and the influence of the time of day,58 age, and even body size.10,41 The motivation factor is a variable that is well recognized but is difficult to control, quantitate, or eliminate.19,50,85 The rate of attaining maximum strength during repetitive exertion has been suggested as a possible objective criterion for judging whether a subject is voluntarily exerting full muscular strength or is not giving an honest effort.50 The eccentric:concentric strength ratios as well as the difference between these ratios at the high and the low speeds were highly effective in distinguishing maximal from submaximal efforts,24 and we do currently use this information clinically to assess for “functional” behavior.
STABILITY
By virtue of the inherent stability afforded by the joint articulation, clinical instability of the elbow may be a perplexing problem (see Chapters 28 through 30). Ligamentous injury most commonly occurs in association with radial head fracture42,82 or elbow dislocation. Recurrent dislocations, however, occur in only 1% to 2% of patients.54 In fact, recurrent instability at the elbow is most commonly a rotatory instability due to insufficiency of the lateral ulnar collateral ligament69 and is discussed at length in Chapter 48. The clinical concept of complex instability is becoming more recognized. The “unhappy triad” refers specifically to fractures of the radial head and coronoid in association with collateral ligament injury. Quantification of instability is difficult; studies are being conducted to understand instability, but no well-defined standard exists to clinically grade this parameter (see Chapter 4).8
FUNCTIONAL EVALUATION OF THE ELBOW
PERFORMANCE INDICES
An objective and reproducible means of evaluating the elbow by considering all of these features of function is obviously desirable. A tradeoff exists between a complex but detailed assessment protocol and one that is simple but not sufficiently thorough. A complete and comprehensive assessment that might be useful in a research facility is not practical clinically. For a clinician, a meaningful rating system should be both complete and readily amenable to an office practice (Table 5-1). A single parameter or index composed of all pertinent variables should accurately reflect the gradation of objective function, as discussed earlier. To be of further value, the rating system should include consideration of the presence of pain and specific daily functions that serve as surrogates to several functional variables as they apply to a discrete activity. Finally, it is also realized that no index or system is capable of discriminating changes in function of the full spectrum of pathology. A tool to describe the state of an athlete with tennis elbow is not adequate to describe the dysfunction of rheumatoid arthritis.
TABLE 5-1 Characteristics and Implications of Patient Assessment Tools
| Trait | Implication |
|---|---|
| Short | High compliance |
| Reflects reality | Valid to draw conclusions |
| Easy | Nonambiguous questions |
| Reliable |
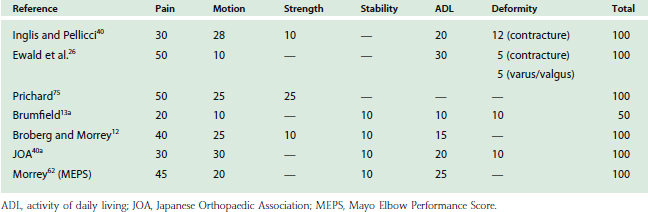
To date, most proposed rating systems consider both objective function and subjective features (motion, strength, stability, pain, and the ability to perform daily activities).77 Most systems have been developed to document the effectiveness of surgical intervention (Table 5-2).26,40,75 Broberg and Morrey12 first described a system designed to be applicable not only to joint replacement but also to other reconstructive procedures. However, as noted earlier, it is obvious that no single rating system is both simple and also sensitive enough to distinguish the status and change of function of the person crippled by rheumatoid arthritis and of the professional tennis player with epicondylitis. Nonetheless, I (B.F.M.) have found that a modification of the simple system reported by Broberg has met my clinical needs over the last several years. The currently employed system is termed the Mayo Elbow Performance Score (MEPS) (Tables 5-2 and 5-3).62 Any discussion of a system or index to summarize function should be subjected to (1) test and retest reliability, (2) internal consistency, and (3) validity.
TABLE 5-3 Mayo Elbow Performance Score
| Function | Points | Definition (Points) |
|---|---|---|
| Pain | 45 |
Classification: excellent, >90; good, 75–89; fair, 60–74; poor, <60.
Furthermore, it is highly desirable to be able to determine the index from patient input above, either in person or by questionnaire. The characteristics of an effective functional evaluation scheme are shown in Table 5-1. In most systems,26,75 pain accounts for the majority of the overall score. Because pain improvement is the most common outcome of intervention, one can bias the appearance of the success of a procedure by overweighing pain in the index calculation. Furthermore, I believe that it is important for the specific functional index used in a clinical practice to represent all functions of the elbow joint as accurately as possible. Thus, those indexes that do not consider strength and stability, except as how they relate to activities of daily living, may not be as comprehensive as those that consider these specific joint functions.23 The functions of motion, strength, and stability are also tested and, hence, duplicated by the ability to perform activities of daily living. Thus, this latter category is really a surrogate for the other three. The issue of a reliable, comprehensive, and yet simple method of determining functional assessment remains unanswered for the elbow and, at the present time, is the subject of discussion and investigation by the American Shoulder and Elbow Surgeons. Turchin and colleagues90 recently conducted an extensive assessment of the published elbow rating scores. Although there is a lack of agreement in the aggregate scores, there is good correlation with the individual raw aggregate scores. The most important message is that which reinforces the observation made earlier; there is no one system that accurately reflects therapeutic value for all conditions: athletic, arthritic, traumatic, and the like. In fact, a self administered questionnaire to assess ulnar nerve function has recently been demonstrated to be reproducible and valid.61
OUTCOME MEASURES
The flurry of activity over the last decade has been productive in first producing useful general tools of assessment such as the Short Form-3643,46,92 and the Western Ontario and McMaster University Osteoarthritis Index (WOMAC). The WOMAC is designed principally to asses hip and knee function.33 More specific to the elbow and upper extremity, the American Shoulder and Elbow Surgeons described a patient- and physician-administered assessment tool,48 and a global strategy of documenting upper extremity function including the shoulder, elbow and hand (DASH) has been developed38 by the American Academy of Orthopedic Surgeons in conjunction with the Canadian Institute for Work and Health.38 The DASH continues to be assessed and refined to further enhance its relevance.7
Ultimately, the goal is to measure disease and intervention impact on function36 and quality of life.3 The Patient-Related Elbow Evaluation is a short form using the Visual Analogue Scale to describe pain and daily function.57 The goal is to include patient-specific symptoms as well as components of the functional status including physical, social, and psychological aspects to determine the impact of treatment. The value of specific intervention on quality of life has also been undertaken recently.3 As implied earlier, accurately demonstrating this relationship is surprisingly complex, but by carefully using existing metrics, investigators have objectively documented the positive impact of elbow joint replacement.3 What remains is to also demonstrate the cost effectiveness of interventions and ultimately be in a position to compare selection factors, techniques, implants, and the like by objective and subjective outcome standards.
1 American Academy of Orthopaedic Surgeons. Joint Motion: Method of Measuring and Recording. Chicago: American Academy of Orthopaedic Surgeons, 1965.
2 An K.-N., Jacobsen M.C., Berglund L.J., Chao E.Y. Application of a magnetic tracking device to kinesiologic studies. J. Biomechan.. 1988;21:613.
3 Angst F., John M., Pap G., Mannion A.F., Herren D.B., Flury M., Aeschlimann A., Schwyzer H.-K., Simmen B.R. Comprehensive assessment of clinical outcome and quality of life after total elbow arthroplasty. Arthritis & Rheum.. 2005;53(1):73.
4 Askew L.J., An K.N., Morrey B.F., Chao E.Y. Functional evaluation of the elbow. Normal motion requirements and strength determinations. Orthop. Trans.. 1981;5:304.
5 Astrand P.O., Rodahl K. Textbook of Work Physiology. New York: McGraw-Hill, 1970.
6 Barnes W.S. The relationship between maximum isokinetic strength and isometric endurance. Res. Q. Exerc. Sport. 1980;51:714.
7 Beaton D., Schemitsch E. Measures of health-related quality of life and physical function. Clin Orthop. 2003;413:90-105.
8 Beingessner D.M., Dunning C.E., Stacpoole R.A., Johnson J.A., King G.J. The effect of coronoid fractures on elbow kinematics and stability. Clin. Biomech.. 2007;22:183.
9 Berger R.A. Comparison of static and dynamic strength increases. Res. Q.. 1962;33:329.
10 Bilodeau M., Henderson T.K., Nolta B.E., Pursley P.J., Sandfort G.L. Effect of aging on fatigue characteristics of elbow flexor muscles during sustained submaximal contraction. J. Appl. Physiol.. 2001;91:2654.
11 Boone D.C., Azen S.P. Normal range of motion of joints in male subjects. J. Bone Joint Surg.. 1979;61A:756.
12 Broberg M.A., Morrey B.F. Results of treatment of fracture dislocations of the elbow. Clin. Orthop.. 1987;216:109.
13 Brockett C., Warren N., Gregory J.E., Morgan D.L., Proske U. A comparison of the effects of concentric versus eccentric exercise on force and position sense at the human elbow joint. Brain Res.. 1997;771:251.
13a Brumfield R.H. Rancho Los Amigo Functional Test. Contemp. Gerontol.. 1984;8:67.
14 Carstam N. Operative treatment of fractures of the head and neck of the radius. Acta Orthop. Scand.. 1950;19:502.
15 Chao E.Y. Experimental Methods for Biomechanical Measurements of Joint Kinematics. In CRC Handbook of Engineering in Medicine and Biology, Section B: Instruments and Measurements. West Palm Beach: CRC Press; 1978.
16 Chao E.Y., An K.N., Askew L.J., Morrey B.F. Electrogoniometer for the measurement of human elbow joint rotation. J. Biomech. Eng.. 1980;102:301.
17 Clarke H.H., Bailey T.L. Strength curves for fourteen joint movements. J. Assoc. Phys. Ment. Rehabil.. 1950;4:12.
18 Clarke H.H., Elkins E.C., Martin G.M., et al. Relationship between body position and the application of muscle power to movements of the joint. Arch. Phys. Med.. 1950;31:81.
19 Cooper D.F., Grimby G.F., Jones D.A., Edwards R.H. Perception of effort in isometric and dynamic muscular contraction. Eur. J. Appl. Physiol.. 1979;41:173.
20 Currier D.P. Maximal isometric tension of the elbow extensor at various positions, Part I. Assessment by cable tensiometer. Phys. Ther.. 1972;52:1043.
21 Darcus H.D. The maximum torques developed in pronation and supination of the right hand. J. Anat.. 1951;85:55.
22 Davis P.R. Some Significant Aspect of Normal Upper Limb Functions. Conference on Joint Replacement of the Upper Extremity. London: Institute of Mechanical Engineers, 1977.
23 Doss W.S., Karpovich P.V. A comparison of concentric, eccentric, and isometric strength of the elbow flexion. J. Appl. Physiol.. 1965;20:351.
24 Dvir Z. An isokinetic study of submaximal effort in elbow flexion. Perceptual and Motor Skills. 1997;84(3 Pt 2):1431.
25 Elkins E.C., Leden U.M., Wakim K.G. Objective recording of the strength of normal muscles. Arch. Phys. Med.. 1951;32:639.
26 Ewald F.C., Scheinberg R.D., Poss R., Thomas W.H., Scott R.D., Sledge C.B. Capitellocondylar total elbow arthroplasty: Two to five year follow up in rheumatoid arthritis. J. Bone Joint Surg.. 1980;62A:1259.
27 Fick K.: Handbuch der Anatomie und Mechanic der Gelenke, Vol. 3. Jena, 1911.
28 Funk, D.: EMG Investigation of Muscular Contractions About the Human Elbow. MS Thesis, Mayo Graduate School of Medicine, 1984.
29 Gallagher M.A., Cuomo F., Polonsky L., Berliner K., Zuckerman J.D. Effects of age, testing speed, and arm dominance on isokinetic strength of the elbow. J. Shoulder Elbow Surg.. 1997;6:340.
30 Gajdosik R.L., Bohannon R.W. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys. Ther.. 1987;67:1867.
31 Gowitzke B.A., Miller M. Understanding the Scientific Basis of Movement, 2nd ed. Baltimore: Williams & Wilkins, 1980.
32 Gribble P.L., Ostry D.J. Independent coactivation of shoulder and elbow muscles. Experimental Brain Res.. 1998;123(3):355.
33 Griffin J.W. Differences in elbow flexion torque measured concentrically, eccentrically, and isometrically. Phys. Ther.. 1987;67:1205.
34 Grootendorst P., Marshall D., Pericak D., Bellamy N., Feeny D., Rottance G.W. A model to estimate health utilities index mark 3 utility scores from WOMAC index scores in patients with osteoarthritis of the knee. J. Rheumatol.. 2007;34:534.
35 Hellebrandt F.A., Duvall E.N., Moore M.L. The measurement of joint motion: part III. Reliability of goniometry. Phys. Ther. Rev.. 1949;29:302.
36 Hildebrand K.A., Patterson S.D., Regan W.D., McDermid J.C., King G.J.W. Functional outcome of semiconstrained total elbow arthroplasty. J. Bone Joint Surg.. 2000;82A:1379-1386.
37 Hood L.B., Forward E.M.M. Strength variations in two determinations of maximal isometric contractions. J. Am. Phys. Ther. Assoc.. 1965;45:1046.
38 Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder, and Hand). The Upper Extremity Collaborative Group (UECG). Am. J. Indust. Med.. 1996;29:602.
39 Hughes R.E., Schneeberger A.G., An K.-N., Morrey B.F., O’Driscoll S.W. Reduction of triceps muscle force after shortening of the distal humerus: A computational model. J. Shoulder Elbow Surg.. 1997;6:444.
40 Inglis A.E., Pellicci P.M. Total elbow replacement. J. Bone Joint Surg.. 1980;62A:1252.
40a Japanese Orthopaedic Association Elbow Evaluation Sheet. Jpn. Orthop. Assoc.. 1992;66:596.
41 Jaric S., Radosavljevic-Jaric S., Johansson H. Muscle force and muscle torque in humans require different methods when adjusting for differences in body size. European J. Appl. Physiol.. 2002;87:304.
42 Johansson O. Capsular and ligament injuries of the elbow joint. Acta Orthop. Scand. Suppl.. 1962;287:1.
43 Jorgensen K., Bankov S. Maximum strength of elbow flexors with pronated and supinated forearm. Med. Sport Biomech.. 1971;6:174.
44 Kapandji I.A. The Physiology of the Joints. Vol. I: Upper Limb, 2nd ed. Baltimore: Williams & Wilkins, 1970.
45 Karpovich P.V., Singh M. Isotonic and isometric forces of forearm flexors and extensors. J. Appl. Physiol.. 1966;21:1435.
46 Katz J.N., Larson M.G., Phillips C.B., Fossel A.H., Liang M.H. Comparative measurement sensitivity of short and longer health status instruments. Med. Care.. 1992;30:917.
47 Kelsey J.L., Pastides H., Kreiger N., Harris C., Chernow R.A. Upper Extremity Disorders. A Study of Their Frequency and Cost in the United States. St. Louis: C. V. Mosby Co., 1980.
48 King G.J.W., Richards R.R., Zuckerman J.D., Blasier R., Dillman C., Friedman R.J., et al. Research Committee, American Shoulder and Elbow Surgeons. A standardized method for assessment of elbow function. J. Shoulder Elbow Surg. 1999;8:351.
49 Kodek T., Munih M. Quantification of shoulder and elbow passive moments in the sagittal plane as a function of adjacent angle fixations. Technol. Health Care. 2003;11:89.
50 Kroemer K.H.E., Marras W.S. Towards an objective assessment of the “maximal voluntary contraction” component in routine muscle strength measurements. Eur. J. Appl. Physiol. 1980;45:1.
51 Kroll W. Reliability variations of strength in test-retest situations. Res. Q. 1963;34:50.
52 Larson C.L., Nelson R.C. An analysis of strength, speed and acceleration of elbow flexion. Arch. Phys. Med. Rehabil. 1969;50:274.
53 Liberson W.T., Dondey M., Asa M.M. Brief repeated isometric maximal exercises. Am. J. Phys. Med. 1962;41:3.
54 Linschied R.L., Wheeler D.K. Elbow dislocations. J. A. M. A. 1965;194:1171.
55 Little A.D., Lehmkuhl D. Elbow extension force: measured in three test positions. J. Am. Phys. Ther. Assoc. 1966;46:7.
56 Luinge H.J., Veltink P.H., Baten C.T. Ambulatory measurement of arm orientation. J. Biomechanics. 2007;40:78.
57 MacDermid J.C. Outcome evaluation in patients with elbow pathology: issues in instrument development and evaluation. J. Hand Ther. 2001;14:105.
58 McGarvey S., Morrey B.F., Askew L.J., An K.N. Reliability of isometric strength testing: temporal factors and strength variation. Clin. Orthop. Rel. Res. 1984;185:301.
59 Masley J.W., Hairabedian A., Donaldson D.N. Training in relation to strength, speed and coordination. Res. Q. 1953;24:308.
60 Moffroid M., et al. Rehabilitation. Monograph 40: Guidelines for Clinical Use of Isokinetic Exercise. New York: Institute of Rehabilitation Medicine, New York University Medical Center, 1969.
61 Mondelli M., Padua L., Giannini F., Bibbo G., Aprile I., Rossi S. A self-administered questionnaire of ulnar neuropathy at the elbow. Neurol. Sci. 2006;27:402.
62 Morrey B.F. Functional evaluation of the elbow. In Morrey B.F., editor: The Elbow and Its Disorders, 2nd ed., Philadelphia: W.B. Saunders Co, 1993.
63 Morrey B.F., Askew L.J., An K.N., Chao E.Y. A biomechanical study of normal elbow motion. J. Bone Joint Surg. 1981;63A:872.
64 Morrey B.F., Chao E.Y., Hui F.C. Biomechanical study of the elbow following excision of the radial head. J. Bone Joint Surg. 1979;61A:63.
65 Motzkin N.E., Cahalan T.D., Morrey B.F., An K.N., Chao E.Y. Isometric and isokinetic endurance testing of the forearm complex. Am. J. Sports Med. 1991;19:107.
66 Salter N. The effect on muscle strength of maximum isometric and isotonic contractions at different repetition rates. J. Physiol. (London). 1955;130:109.
67 National Safety Council, 1976. Cited by Kelsey et al. (op. cit.).
68 Nelson R.C., Fahrney R.A. Relationship between strength and speed of elbow flexion. Res. Q.. 1963;36:455.
69 O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J. Bone Joint Surg.. 1991;73A:440.
70 Ogilvie W.H. Discussion on minor injuries of the elbow joint. Proc. R. Soc. Med.. 1930;23:306.
71 O’Neill O., Morrey B.F., Tanaka S., An K.N. Compensatory motion in the upper extremity following elbow arthrodesis. Clin. Orthop.. 1992;281:89.
72 Osternig L.R., Bates B.T., James S.L. Isokinetic and isometric torque force relationships. Arch. Phys. Med. Rehabil.. 1977;58:254.
73 Pierson W.R., Rasch P.J. Strength and speed. Perceptual motor skills.. 1962;14:144.
74 Pigeon P., Yahia L., Feldman A.G. Moment arms and lengths of human upper limb muscles as functions of joint angles. J. Biomechan.. 1996;29:1365.
75 Pritchard R.W. Total elbow arthroplasty. In: Joint Replacement in the Upper Limb. London: Mechanical Engineering Publications; 1977:67.
76 Provins K.A., Salter N. Maximum torque exerted about the elbow joint. J. Appl. Physiol.. 1955;7:393.
77 Richards R.R., An K.N., Bigliani L.U., Friedman R.J., Gartsman G.M., Gristina A.G., Iannotti J.P., Mow V.C., Sidles J., Zuckerman J.D. A standarized method of the assessment of shoulder function. J. Shoulder Elbow Surg.. 1994;3:347.
78 Rothstein J.M., Miller P.J., Roettger R.F. Goniometric reliability in a clinical setting. Phys. Ther.. 1983;63:1611.
79 Russe O. An Atlas of Examination, Standard Measurements and Diagnosis in Orthopedics and Traumatology. Vienna: Hans Huber, 1972.
80 Salter N. The effect on muscle strength of maximum isometric and isotonic contractions at different repetition rates. J. Physiol. (London). 1955;130:109.
81 Schenck J.M., Forward E.M. Quantitative strength changes with test repetitions. J. Am. Phys. Ther. Assoc. 1965;45:562.
82 Schwab G.H., Bennett J.B., Woods G.W., Tullos H. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin. Orthop. 1980;146:42.
83 Shigeyama Y., Inoue H., Hashizume H., Nagashima H., Senda M. Muscle strength in rheumatoid elbow: quantitative measurement and comparison to Larsen’s x-ray grade. Acta Medica Okayama. 1997;51:267.
84 Simmons J.W., Rath D., Merta R. Calculation of disability using the Cybex II system. xOrthopedics. 1982;5:181.
85 Singh M., Karpovich P.V. Isotonic and isometric forces of forearm flexors and extensors. J. Appl. Physiol. 1966;21:1435.
86 Snider W.J., Dewitt H.J. Functional study for optimum position for elbow arthrodesis on ankylosis. J. Bone Joint Surg. 1973;55A:1305.
87 Tanaka S., An K.-N., Morrey B.F. Kinematics and laxity of ulnohumeral joint under valgus-varus stress. J. Musculoskeletal. Res. 1998;2:45.
88 Toji H., Suei K., Kaneko M. Effects of combined training loads on relations among force, velocity, and power development. Can. J. Appl. Physiol. 1997;22:328.
89 Tracy B.L., Mehoudar P.D., Ortega J.D. The amplitude of force variability is correlated in the knee extensor and elbow flexor muscles. Experimental Brain Res. 2007;176:448.
90 Turchin D.C., Beaton D.E., Richards R.R. Validity of observer-based aggregate scoring systems as descriptors of elbow pain, function, and disability. J. Bone Joint Surg. 1998;80A:154.
91 Wagner C. Determination of the rotatory flexibility of the elbow joint. Eur. J. Appl. Physiol. 1977;37:47.
92 Ware J.E., Snow K.K., Kosinski M., Gandek B. SF-36 health survey: Manual and interpretation guide, 2nd ed. Lincoln, RI: QualityMetric Inc., 2000.
93 Williams M., Stutzman L. Strength variation through the range of joint motion. Phys. Ther. Rev. 1959;39:145.
94 Williams M., Toberlin J.A., Robertson K.J. Muscle force curves of school children. Phys. Ther. 1965;45:539.
95 Wilmer H.A., Elkins E.C. An optical goniometer for observing range of motion of joints. Arch. Phys. Med. 1947;28:695.
96 Worshal D. The reliability of isometric strength gain in therapeutic assessment. Am. Correct. Ther. J. 1979;33:188.