Forearm, Wrist, and Hand
The hand and wrist are the most active and intricate parts of the upper extremity. Because of this, they are vulnerable to injury, which can lead to large functional difficulties, and they do not respond well to serious trauma. Their mobility is enhanced by a wide range of movement at the shoulder and complementary movement at the elbow. The 28 bones, numerous articulations, and 19 intrinsic and 20 extrinsic muscles of the wrist and hand provide a tremendous variability of movement. In addition to being an expressive organ of communication, the hand has a protective role and acts as both a motor and a sensory organ, providing information, such as temperature, thickness, texture, depth, and shape as well as the motion of an object. It is this sensual acuity that enables the examiner to accurately examine and palpate during an assessment.
The assessment of the hand and wrist should be performed with two objectives in mind. First, the injury or lesion should be assessed as accurately as possible to ensure proper treatment. Second, the examiner should evaluate the remaining function to determine whether the patient will have any incapacity in everyday life.
Although the joints of the forearm, wrist, and hand are discussed separately, they do not act in isolation but rather as functional groups. The position of one joint influences the position and action of the other joints. For example, if the wrist is flexed, the interphalangeal joints do not fully flex, primarily because of passive insufficiency of the finger extensors and their tendons. Each articulation depends on balanced forces for proper positioning and control. If this balance or equilibrium is not present because of trauma, nerve injury, or other factors, the loss of counterbalancing forces results in deformities. In addition, the entire upper limb should be considered a kinetic chain that enables the hand to be properly positioned. The actions of the shoulder, elbow, and wrist joints enable the hand to be placed on almost any area of the body.
Applied Anatomy
The distal radioulnar joint is a uniaxial pivot joint that has one degree of freedom.1 Although the radius moves over the ulna, the ulna does not remain stationary. It moves back and laterally during pronation and forward and medially during supination. The resting position of the joint is 10° of supination, and the close packed position is 5° of supination. The capsular pattern of the distal radioulnar joint is full range of motion (ROM) with pain at the extreme of rotation.
The radiocarpal (wrist) joint is a biaxial ellipsoid joint.1,2 The radius articulates with the scaphoid and lunate. The distal radius is not straight but is angled toward the ulna (15° to 20°), and its posterior margin projects more distally to provide a “buttress effect.”3 The lunate and triquetrum also articulate with the triangular cartilaginous disc (triangular fibrocartilage complex [TFCC]) (Figures 7-1 and 7-2) and not the ulna. The disc extends from the ulnar side of the distal radius and attaches to the ulna at the base of the ulnar styloid process. The disc adds stability to the wrist. It creates a close relation between the ulna and carpal bones and binds together and stabilizes the distal ends of the radius and ulna.4,5 With the disc in place, the radius bears 60% of the load and the ulna bears 40%. If the disc is removed, the radius transmits 95% of the axial load and the ulna transmits 5%.6 Therefore, the cartilaginous disc acts as a cushion for the wrist joint and as a major stabilizer of the distal radioulnar joint.3,7 The disc can be damaged by forced extension and pronation. The distal end of the radius is concave and the proximal row of carpals is convex, but the curvatures are not equal. The joint has 2° of freedom, and the resting position is neutral with slight ulnar deviation. The close packed position is extension, and the capsular pattern is equal limitation of flexion and extension.
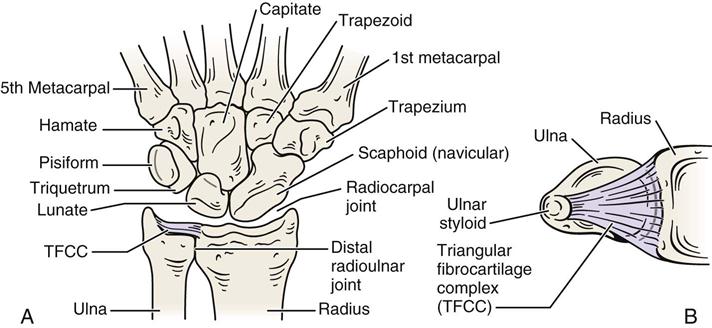
A, Palmar view. B, End view of TFCC and radius and ulna.
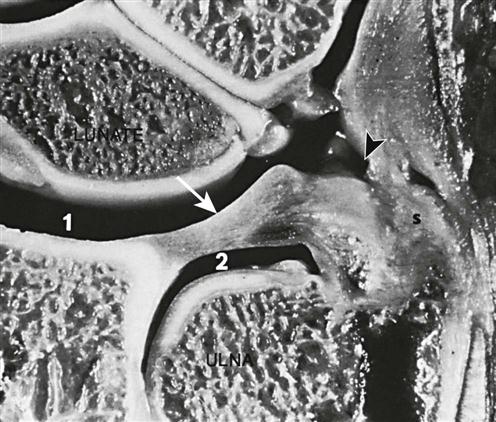
Ulnar limit of the radiocarpal compartment (coronal section). Note the extent of this compartment (1), its relationship to the inferior radioulnar compartment (2), the intervening triangular fibrocartilage (arrow), and the prestyloid recess (arrowhead), which is intimate with the ulnar styloid(s). (From Resnick D, Kransdorf MJ: Bone and joint imaging, Philadelphia, 2005, WB Saunders, p. 27.)
The stability of the carpals (wrist) is primarily maintained by a complex configuration of ligaments (Figure 7-3).8 The ligaments stabilizing the scaphoid, lunate, and triquetrum are the most important.9 Of these ligaments, the radioscapholunate ligament is one of the most important, because it is commonly injured and, when intact, maintains carpal stability.10 This ligament is most likely to be injured with a pronated fall on out-stretched hand (FOOSH) injury (wrist extension, ulnar deviation, and intercarpal supination).9,11 Lunotriquetral injuries are more likely to occur with wrist extension, radial deviation, and intercarpal supination.9 The palmar ligaments are much stronger than the dorsal ligaments. The palmar extrinsic ligaments control the movement of the wrist and scaphoid with the radioscapholunate ligament acting as a sling for the scaphoid.10 This ligament along with the radiolunate ligament allows the scaphoid to rotate around them, and both stabilize the scaphoid at the extremes of motion.10 On the ulnar side, the ligaments (palmar lunotriquetral, capitotriquetral, dorsal intercarpal, and the fibrocartilaginous disc) control the triquetrum.
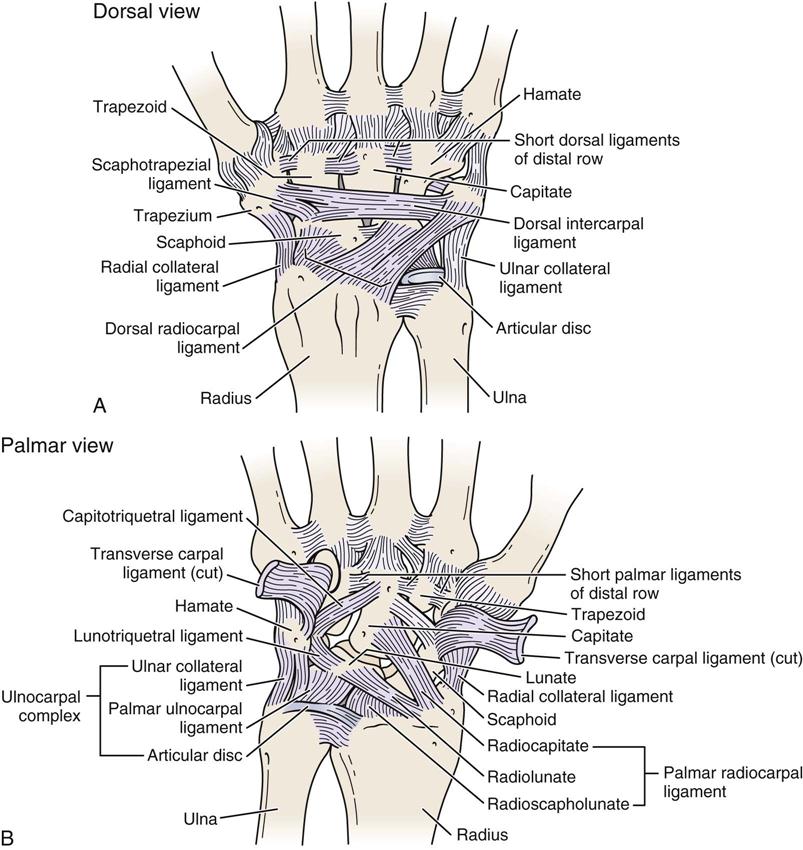
A, Dorsal aspect of the right wrist. B, Palmar aspect of the right wrist. The transverse carpal ligament has been cut and reflected to show the underlying ligaments. (Redrawn from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, CV Mosby, pp. 178–179.)
The intercarpal joints include the joints between the individual bones of the proximal row of carpal bones (scaphoid, lunate, and triquetrum) and the joints between the individual bones of the distal row of carpal bones (trapezium, trapezoid, capitate, and hamate). Perilunate injuries involve the lunate and its relation with the other carpals as well as the radius and ulna.12 They are bound together by small intercarpal ligaments (dorsal, palmar, and interosseous), which allow only a slight amount of gliding movement between the bones. The close packed position is extension, and the resting position is neutral or slight flexion. The pisotriquetral joint is considered separately, because the pisiform sits on the triquetrum and does not take a direct part in the other intercarpal movements.
The midcarpal joints form a compound articulation between the proximal and distal rows of carpal bones with the exception of the pisiform bone. On the medial side, the scaphoid, lunate, and triquetrum articulate with the capitate and hamate, forming a compound sellar (saddle-shaped) joint. On the lateral aspect, the scaphoid articulates with the trapezoid and trapezium, forming another compound sellar joint. As with the intercarpal joints, these articulations are bound together by dorsal and palmar ligaments; however, there are no interosseous ligaments between the proximal and distal rows of bones. Therefore, greater movement exists at the midcarpal joints than between the individual bones of the two rows of the intercarpal joints. The close packed position of these joints is extension with ulnar deviation, and the resting position is neutral or slight flexion with ulnar deviation.
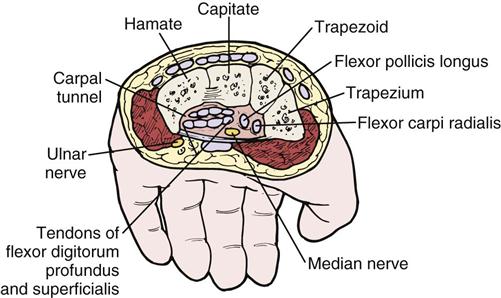
The proximal transverse arch (Figure 7-4) that forms the carpal tunnel is formed by the distal row of carpal bones. In this relatively rigid arch, the capitate bone acts as a central keystone structure.13
At the thumb, the carpometacarpal joint is a sellar joint that has 3° of freedom, whereas the second to fifth carpometacarpal joints are plane joints.14 The capsular pattern of the carpometacarpal joint of the thumb is abduction most limited, followed by extension. The resting position is midway between abduction and adduction and midway between flexion and extension. The close packed position of the carpometacarpal joint of the thumb is full opposition. For the second to fifth carpometacarpal joints, the capsular pattern of restriction is equal limitation in all directions. The bones of these joints are held together by dorsal and palmar ligaments. In addition, the thumb articulation has a strong lateral ligament extending from the lateral side of the trapezium to the radial side of the base of the first metacarpal, and the medial four articulations have an interosseous ligament similar to that found in the carpal articulation.
The carpometacarpal articulations of the fingers allow only gliding movement. The second and third carpometacarpal joints tend to be relatively immobile and are the primary “stabilizing” joints of the hand, whereas the fourth and fifth joints are more mobile to allow the hand to adapt to different shaped objects during grasping. The carpometacarpal articulation of the thumb is unique in that it allows flexion, extension, abduction, adduction, rotation, and circumduction. It is able to do this because the articulation is saddle shaped. Because of the many movements possible at this joint, the thumb is able to adopt any position relative to the palmar aspect of the hand.14
The plane intermetacarpal joints have only a small amount of gliding movement between them and do not include the thumb articulation. They are bound together by palmar, dorsal, and interosseous ligaments.
The metacarpophalangeal joints are condyloid joints. The collateral ligaments of these joints are tight on flexion and relaxed on extension. These articulations are also bound by palmar ligaments and deep transverse metacarpal ligaments. The dorsal or extensor hood (Figure 7-5) reinforces the dorsal aspect of the metacarpophalangeal joints while volar or palmar plates reinforce the palmar aspect (see Figure 7-5).3 Each joint has 2° of freedom. The first metacarpophalangeal joint has 3° of freedom, thus facilitating the movement of the carpometacarpal joint of the thumb.14 The close packed position of the first metacarpophalangeal joint is maximum opposition, and the close packed position for the second through the fifth metacarpophalangeal joints is maximum flexion.15 The resting position of the metacarpophalangeal joints is slight flexion, whereas the capsular pattern is more limitation of flexion than extension.
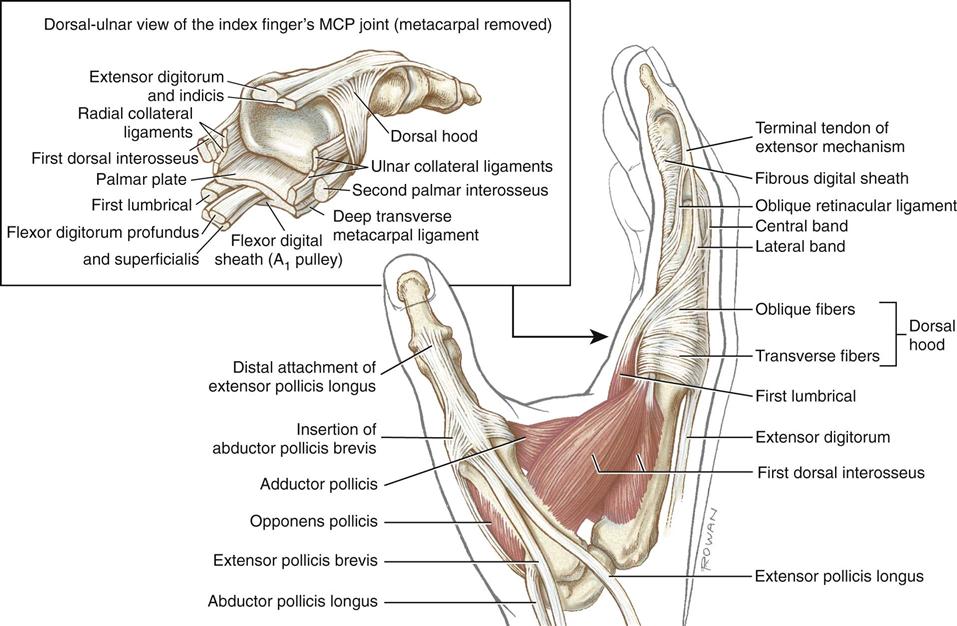
The illustration in the box highlights the anatomy associated with the metacarpophalangeal joint of the index finger. (From Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, ed 2, St Louis, 2010, CV Mosby, p. 269.)
The distal transverse arch (see Figure 7-4) passes through the metacarpophalangeal joints and has greater mobility than the proximal transverse arch allowing the hand to form or fit around different objects. The second and third metacarpophalangeal joints form the stable portion of the arch while the fourth and fifth metacarpophalangeal joints form the mobile portion (see Figure 7-27).13
The longituginal arch follows the more rigid portion of the hand running from the carpals to the carpometacarpal joints providing longitudinal stability to the hand. The second and third metacarpophalangeal joints are the keystone to both the distal transverse arch and the distal longitudinal arch.13
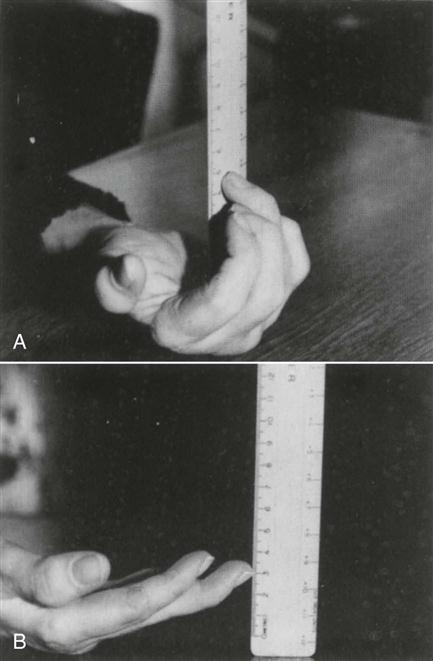
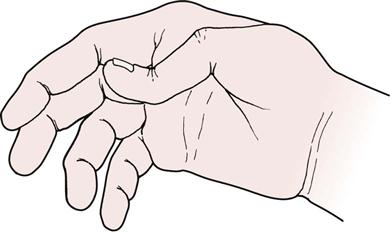
The interphalangeal joints are uniaxial hinge joints, each having 1° of freedom. The close packed position of the proximal interphalangeal joints and distal interphalangeal joints is full extension; the resting position is slight flexion. The capsular pattern of these joints in flexion is more limited than extension. The bones of these joints are bound together by a fibrous capsule and by the palmar and collateral ligaments. During flexion, there is some rotation in these joints so that the pulp of the fingers faces more fully the pulp of the thumb. If the metacarpophalangeal joints and the proximal interphalangeal joints of the fingers are flexed, they converge toward the scaphoid tubercle (Figure 7-6). This is sometimes referred to as a cascade sign. If one or more fingers do not converge, it usually indicates trauma (e.g., fracture) to the digits that has altered their normal alignment.
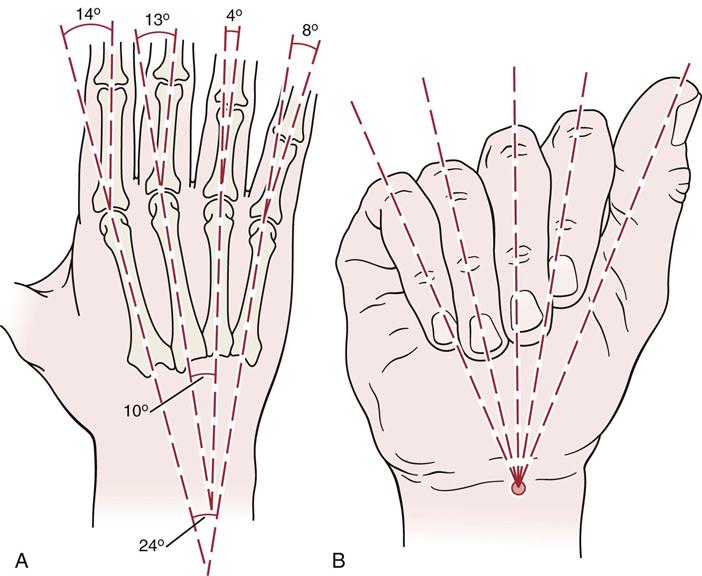
A, Normal physiological alignment. B, Oblique flexion of the last four digits. Only the index ray flexes toward the median axis. When the last four digits are flexed separately at the metacarpophalangeal and proximal interphalangeal joints, their axes converge toward the scaphoid tubercle. (Redrawn from Tubiana R: The hand, Philadelphia, 1981, WB Saunders, p. 22.)
Patient History
The assessment of the forearm, wrist, and hand often takes longer than that of other joints of the body because of the importance of the hand to everyday function and because of the many structures and joints involved.
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
1. What is the patient’s age? Certain conditions are more likely to occur at different ages. For example, arthritic changes are most commonly seen in patients who are older than 40 years of age.16
3. What was the mechanism of injury?16,17 For example, a FOOSH injury may lead to a lunate dislocation, Colles fracture, or scaphoid fracture, or extension of the fingers may cause dislocation of the fingers. A rotational force applied to the wrist or near it may lead to a Galeazzi fracture, which is a fracture of the radius and dislocation of the distal end of the ulna.
5. When did the injury or onset occur, and how long has the patient been incapacitated? These questions are not necessarily the same; for instance, a burn may occur at a certain time, but incapacity may not occur until hypertrophic scarring appears. The wrist is commonly injured by weight bearing (e.g., gymnastics), by rotational stress combined with ulnar deviation (e.g., hitting a racquet), by twisting, and by impact loading (FOOSH injury).17,18
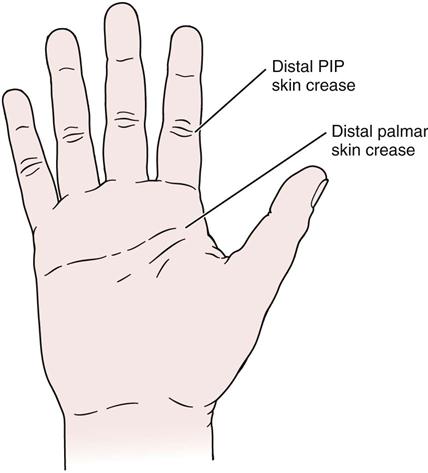
8. Which part of the forearm, wrist, or hand is injured? If the flexor tendons (which are round, have synovial sheaths, and have a longer excursion than the extensor tendons) are injured, they respond much more slowly to treatment than do extensor tendons (which are flat or ovoid). Within the hand, there is a surgical “no man’s land” (Figure 7-7), which is a region between the distal palmar crease and the midportion of the middle phalanx of the fingers. Damage to the flexor tendons in this area require surgical repair and usually lead to the formation of adhesive bands that restrict gliding. In addition, the tendons may become ischemic, being replaced by scar tissue. Because of this, the prognosis after surgery in this area is poor.
9. Does pain or abnormal sensation (e.g., tingling, pins and needles) predominate? In the hand and fingers, the examiner must take the time to differentiate exactly where the symptoms are to differentiate peripheral nerve neuropathy, nerve root symptoms, and other painful localized conditions.19,20
Observation
While observing the patient and viewing the forearms, wrists, and hands from both the anterior and posterior aspects, the examiner should note the patient’s willingness and ability to use the hand. Normally, when the hand is in the resting position and the wrist is in the normal position, the fingers are progressively more flexed as one moves from the radial side of the hand to the ulnar side. Loss of this normal attitude may be caused by pathology affecting the hand, such as a lacerated tendon, or by a contracture, such as Dupuytren contracture.
The bone and soft-tissue contours of the forearm, wrist, and hand should be compared for both upper limbs, and any deviation should be noted. The cosmetic appearance of the hand is very important to some patients. The examiner should note the patient’s reaction to the appearance of the hand and be prepared to provide a cosmetic evaluation. This evaluation should always be included with the more important functional assessment. The posture of the hand at rest often demonstrates common deformities. Are the normal skin creases present? Skin creases occur because of movement at the various joints. The examiner should note any muscle wasting on the thenar eminence (median nerve), first dorsal interosseous muscle (C7 nerve root), or hypothenar eminence (ulnar nerve) that may be indicative of peripheral nerve or nerve root injury.
Any localized swellings (e.g., ganglion) that are seen on the dorsum of the hand should be recorded (Figure 7-8).21 In the wrist and hand, effusion and synovial thickening are most evident on the dorsal and radial aspects. Swelling of the metacarpophalangeal and interphalangeal joints is most obvious on the dorsal aspect.

The dominant hand tends to be larger than the nondominant hand. If the patient has an area on the fingers that lacks sensation, this area is avoided when the patient lifts or identifies objects, and the patient uses another finger instead with normal sensitivity. Therefore, the examiner should watch for abnormal or different patterns of movement, which may indicate adaptations or modifications necessitated by the presence of pathology.
Any vasomotor, sudomotor, pilomotor, and trophic changes should be recorded. These changes may be indicative of a peripheral nerve injury, peripheral vascular disease, diabetes mellitus, Raynaud disease, or reflex neurovascular syndromes (also called complex regional pain syndrome, reflex sympathetic dystrophy, shoulder-hand syndrome, and Sudeck atrophy). The changes seen could include loss of hair on the hand, brittle fingernails, increase or decrease in sweating of the palm, shiny skin, radiographic evidence of osteoporosis, or any difference in temperature between the two limbs. Table 7-1 illustrates vasomotor, sudomotor, pilomotor, and trophic changes that occur in the hand when sympathetic nerve function has been affected.
Table 7-1
Sympathetic Changes after Nerve Injury
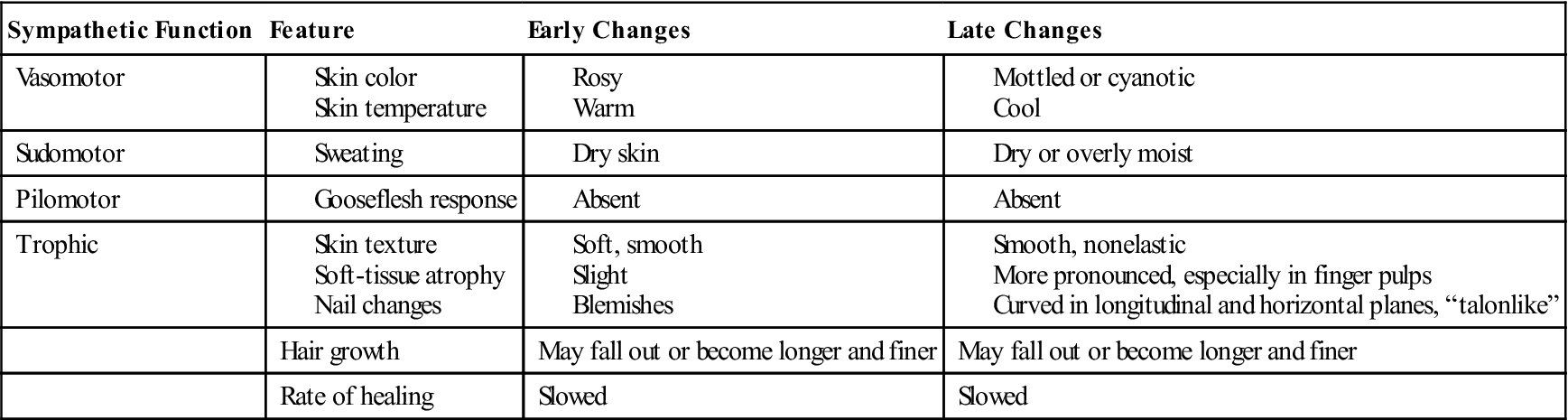
From Callahan AD: Sensibility assessment for nerve lesions-in-continuity and nerve lacerations. In Hunter J, Schneider LH, Mackin EJ, et al, editors: Rehabilitation of the hand and upper extremity, St Louis, 2002, Mosby, p. 225.
The examiner should note any hypertrophy of the fingers. Hypertrophy of the bone may be seen in Paget disease, neurofibromatosis, or arteriovenous fistula.
The presence of Heberden or Bouchard nodes (Figure 7-9) should be recorded. Heberden nodes appear on the dorsal surface of the distal interphalangeal joints and are associated with osteoarthritis. Bouchard nodes are on the dorsal surface of the proximal interphalangeal joints. They are often associated with gastrectasis and osteoarthritis.
Any ulcerations may indicate neurological or circulatory problems. Any alteration in the color of the limb with changes in position may indicate a circulatory problem.
The examiner should note any rotational or angulated deformities of the fingers, which may be indicative of previous fracture. The nail beds are normally parallel to one another. The fingers, when extended, are slightly rotated toward the thumb to aid pinch. Ulnar drift (Figure 7-10) may be seen in rheumatoid arthritis, owing to the shape of the metacarpophalangeal joints and the pull of the long tendons.
The presence of any wounds or scars should be noted because they may indicate recent surgery or past trauma. If wounds are present, are they new or old? Are they healing properly? Is the scar red (new) or white (old)? Is the scar mobile or adherent? Is it normal, hypertrophic, or keloid? Palmar scars may interfere with finger extension. Web space scars may interfere with finger separation and metacarpophalangeal joint flexion.
The examiner should take time to observe the fingernails. “Spoon-shaped” nails (Figure 7-11) are often the result of fungal infection, anemia, iron deficiency, long-term diabetes, local injury, developmental abnormality, chemical irritants, or psoriasis. They may also be a congenital or hereditary trait. “Clubbed” nails (Figure 7-12) may result from hypertrophy of the underlying soft tissue or respiratory or cardiac problems, such as chronic obstructive pulmonary disease, severe emphysema, congenital heart defects, or cor pulmonale. Table 7-2 shows other pathological processes that may affect the fingernails.

Table 7-2
| Condition | Description | Occurrence |
| Beau lines | Transverse lines or ridges marking repeated disturbances of nail growth | Systemic diseases, toxic or nutritional deficiency states of many types, trauma (from manicuring) |
| Defluvium unguium (onychomadesis) | Complete loss of nails | Certain systemic diseases, such as scarlet fever, syphilis, leprosy, alopecia areata, exfoliative dermatitis |
| Diffusion of lunula unguis | “Spreading” of lunula | Dystrophies of the extremities |
| Eggshell nails | Nail plate thin, semitransparent bluish-white with a tendency to curve upward at the distal edge | Syphilis |
| Fragilitas unguium | Friable or brittle nails | Dietary deficiency, local trauma |
| Hapalonychia | Nails very soft, split easily | Following contact with strong alkalis; endocrine disturbances, malnutrition, syphilis, chronic arthritis |
| Hippocratic nails | “Watch-glass nails” associated with “drumstick fingers” | Chronic respiratory and circulatory diseases, especially pulmonary tuberculosis; hepatic cirrhosis |
| Koilonychia | “Spoon nails;” nails are concave on the outer surface | Dysendocrinisms (acromegaly), trauma, dermatoses, syphilis, nutritional deficiencies, hypothyroidism |
| Leukonychia | White spots or striations or rarely the whole nail may turn white (congenital type) | Local trauma, hepatic cirrhosis, nutritional deficiencies, and many systemic diseases |
| Mees’ lines | Transverse white bands | Hodgkin’s granuloma, arsenic and thallium toxicity, high fevers, local nutritional derangement |
| Moniliasis of nails | Infections (usually paronychial) caused by yeast forms (Candida albicans) | Occupational (common in food-handlers, dentists, dishwashers, and gardeners) |
| Onychatrophia | Atrophy or failure of development of nails | Trauma, infection, dysendocrinism, gonadal aplasia, and many systemic disorders |
| Onychauxis | Nail plate is greatly thickened | Mild persistent trauma, systemic diseases, such as peripheral stasis, peripheral neuritis, syphilis, leprosy, hemiplegia; or at times may be congenital |
| Onychia | Inflammation of the nail matrix causing deformity of the nail plate | Trauma, infection, many systemic diseases |
| Onychodystrophy | Any deformity of the nail plate, nail bed, or nail matrix | Many diseases, trauma, or chemical agents (poisoning, allergy) |
| Onchogryposis | “Claw nails”—extreme degree of hypertrophy, sometimes with horny projections arising from the nail surface | May be congenital or related to many chronic systemic diseases (see onychauxis) |
| Onycholysis | Loosening of the nail plate beginning at the distal or free edge | Trauma, injury by chemical agents, many systemic diseases |
| Onychomadesis | Shedding of all the nails (defluvium unguium) | Dermatoses, such as exfoliative dermatitis, alopecia areata, psoriasis, eczema, nail infection, severe systemic diseases, arsenic poisoning |
| Onychophagia | Nail biting | Neurosis |
| Onychorrhexis | Longitudinal ridging and splitting of the nails | Dermatoses, nail infections, many systemic diseases, senility, injury by chemical agents, hyperthyroidism |
| Onychoschizia | Lamination and scaling away of nails in thin layers | Dermatoses, syphilis, injury by chemical agents |
| Onychotillomania | Alteration of the nail structures caused by persistent neurotic picking of the nails | Neurosis |
| Pachyonychia | Extreme thickening of all the nails; the nails are more solid and more regular than in onychogryposis | Usually congenital and associated with hyperkeratosis of the palms and soles |
| Pterygium unguis | Thinning of the nail fold and spreading of the cuticle over the nail plate | Associated with vasospastic conditions, such as Raynaud phenomenon and occasionally with hypothyroidism |
From Berry TJ: The hand as mirror of systemic disease, Philadelphia, 1963, FA Davis.
Common Hand and Finger Deformities
Ape Hand Deformity.
Wasting of the thenar eminence of the hand occurs as a result of a median nerve palsy, and the thumb falls back in line with the fingers as a result of the pull of the extensor muscles. The patient is also unable to oppose or flex the thumb (Figure 7-13).
Bishop’s Hand or Benediction Hand Deformity.
Wasting of the hypothenar muscles of the hand, the interossei muscles, and the two medial lumbrical muscles occurs because of ulnar nerve palsy (Figure 7-14). Flexion of the fourth and fifth fingers is the most obvious resulting change.

Boutonnière Deformity.
Extension of the metacarpophalangeal and distal interphalangeal joints and flexion of the proximal interphalangeal joint (primary deformity) are seen with this deformity. The deformity is the result of a rupture of the central tendinous slip of the extensor hood and is most common after trauma or in rheumatoid arthritis (Figure 7-15).
Claw Fingers.
This deformity results from the loss of intrinsic muscle action and the overaction of the extrinsic (long) extensor muscles on the proximal phalanx of the fingers. The metacarpophalangeal joints are hyperextended, and the proximal and distal interphalangeal joints are flexed (Figure 7-16). If intrinsic function is lost, the hand is called an intrinsic minus hand. The normal cupping of the hand is lost, both the longitudinal and the transverse arches of the hand (see Figure 7-4) disappear, and there is intrinsic muscle wasting. The deformity is most often caused by a combined median and ulnar nerve palsy.
Drop-Wrist Deformity.
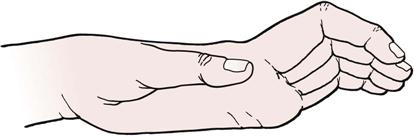
The extensor muscles of the wrist are paralyzed as a result of a radial nerve palsy, and the wrist and fingers cannot be actively extended by the patient (Figure 7-17).

Dupuytren Contracture.
This progressive disease of genetic origin results in contracture of the palmar fascia.22 There is a fixed flexion deformity of the metacarpophalangeal and proximal interphalangeal joints (Figure 7-18). Dupuytren contracture is usually seen in the ring or little finger, and the skin is often adherent to the fascia. It affects men more often than women and is usually seen in the 50- to 70-year-old age group.
Extensor Plus Deformity.
This deformity is caused by adhesions or shortening of the extensor communis tendon proximal to the metacarpophalangeal joint. It results in the inability of the patient to simultaneously flex the metacarpophalangeal and proximal interphalangeal joints, although they may be flexed individually.
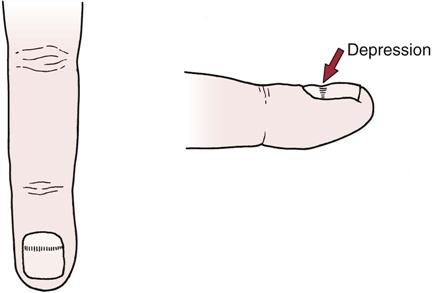
Mallet Finger.23
A mallet finger deformity is the result of a rupture or avulsion of the extensor tendon where it inserts into the distal phalanx of the finger. The distal phalanx rests in a flexed position (Figure 7-19).
Myelopathy Hand.
This deformity is a dysfunction of the hand caused by cervical spinal cord pathology in conjunction with cervical spondylosis. The patient shows an inability to extend and adduct the ring and little finger and sometimes the middle finger, especially rapidly, despite good function of the wrist, thumb, and index finger. In addition, the patient shows an exaggerated triceps reflex and positive pathological reflexes (e.g., Hoffman reflex).24
Polydactyly and Triphalangism.
Polydactyly is a congenital anomaly characterized by the presence of more than the normal number of fingers or, in the case of the foot, toes. Triphalangism implies there are three phalanges instead of the normal two as would be seen in the thumb.25
Swan Neck Deformity.
This deformity usually involves only the fingers. There is flexion of the metacarpophalangeal and distal interphalangeal joints, but the real deformity is extension of the proximal interphalangeal joint. The condition is a result of contracture of the intrinsic muscles or tearing of the volar plate and is often seen in patients with rheumatoid arthritis or following trauma (Figure 7-20).
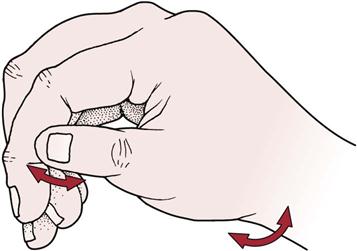
Trigger Finger.26
Also known as digital tenovaginitis stenosans, this deformity is the result of a thickening of the flexor tendon sheath (Notta’s nodule), which causes sticking of the tendon when the patient attempts to flex the finger. A low-grade inflammation of the proximal fold of the flexor tendon leads to swelling and constriction (stenosis) in the digital flexor tendon. When the patient attempts to flex the finger, the tendon sticks, and the finger “lets go,” often with a snap. As the condition worsens, eventually the finger will flex but not let go, and it will have to be passively extended until finally a fixed flexion deformity occurs. The condition is more likely to occur in middle-aged women, whereas “trigger thumb” with a flexion deformity of the interphalangeal joint is more common in young children.27 The condition usually occurs in the third or fourth finger. In adults, it is most often associated with rheumatoid arthritis and tends to be worse in the morning.
Ulnar Drift.
This deformity, which is commonly seen in patients with rheumatoid arthritis but can occur with other conditions, results in ulnar deviation of the digits because of weakening of the capsuloligamentous structures of the metacarpophalangeal joints and the accompanying “bowstring” effect of the extensor communis tendons (see Figure 7-10).
Zigzag Deformity of the Thumb.
The thumb is flexed at the carpometacarpal joint and hyperextended at the metacarpophalangeal joint (Figure 7-21). The deformity is associated with rheumatoid arthritis. A “Z” deformity is due to hypermobility and may be familial (Figure 7-22).
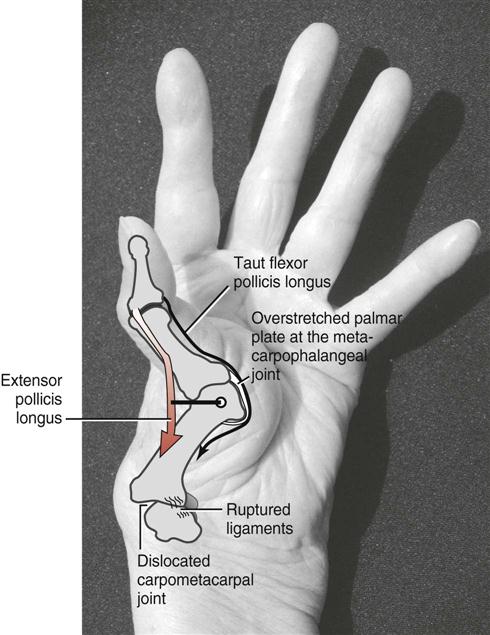
The thumb metacarpal dislocates laterally at the carpometacarpal joint, causing hyperextension at the metacarpophalangeal joint. The interphalangeal joint remains partially flexed owing to the passive tension in the stretched and taut flexor pollicis longus. Note that the “bowstringing” of the tendon of the extensor pollicis longus across the metacarpophalangeal joint creates a large extensor moment arm, thereby magnifying the mechanics of the deformity. (From Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, CV Mosby, p. 237.)
Other Physical Findings
The hand is the terminal part of the upper limb. Many pathological conditions manifest themselves in this structure and may lead the examiner to suspect pathological conditions elsewhere in the body. It is important for the examiner to take the time to view the hands when assessing any joint, especially if an abnormal pattern is presented or the history gives an indication that more than one joint may be involved. For example, if a patient presents with insidious neck pain and demonstrates nail changes that indicate psoriasis, the examiner should consider the possibility of psoriatic arthritis affecting the cervical spine as well as the hand. Some conditions involving the hand include the following:
2. The Plummer-Vinson syndrome produces spoon-shaped nails (see Figure 7-11). This condition is a dysphagia with atrophy in the mouth, pharynx, and upper esophagus.
4. Hyperthyroidism produces nail atrophy and ridging with warm, moist hands.
5. Vasospastic conditions produce a thin nail fold and pterygium (abnormal extension) of the cuticle.
6. Trauma to the nail bed, toxic radiation, acute illness, prolonged fever, avitaminosis, and chronic alcoholism produce transverse lines, or Beau lines, in the nails (Figure 7-23).
7. Many arterial diseases produce a lack of linear growth with thick, dark nails.
9. Chronic respiratory disorders produce clubbing of the nails (see Figure 7-12).
11. Congenital heart disease may produce cyanosis and nail clubbing.
12. Neurocirculatory aesthesia (loss of strength and energy) produces cold, damp hands.
13. Parkinson disease produces a typical hand tremor known as “pill rolling hand” (Figure 7-24).
14. Causalgic states produce a painful, swollen, hot hand.
15. “Opera glove” anesthesia is seen in hysteria, leprosy, and diabetes. It is a condition in which there is numbness from the elbow to the fingers (Figure 7-25).
17. Rheumatoid arthritis produces a warm, wet hand as well as joint swelling, dislocations or subluxations, and ulnar deviation or drift of the wrist (see Figure 7-10).
18. The deformed hand of Volkmann ischemic contracture is one that is very typical for a compartment syndrome after a fracture or dislocation of the elbow (Figure 7-26).28
Box 7-1 gives further examples of physical findings of the hand.
Examination
The examination of the forearm, wrist, and hand may be very extensive, or it may be limited to one or two joints, depending on the area and degree of injury. Regardless, because of its functional importance, the examiner must take extra care when examining this area. Not only must clinical limitations be determined, but functional limitations brought on by trauma, nerve injuries, or other factors must be carefully considered to have an appropriate outcome functionally, cosmetically, and clinically.
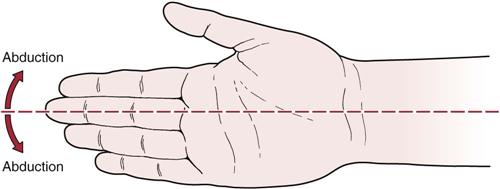
Because there are so many joints, bones, muscles, and ligaments involved, the examiner must develop a working knowledge of all of these tissues and how they interact with one another. The examiner should remember that adduction of the hand (ulnar deviation) is greater than abduction (radial deviation) because of shortness of the ulnar styloid process. Supination of the forearm is stronger than pronation, whereas abduction has a greater ROM in supination than pronation. Adduction and abduction ROM is minimal when the wrist is fully extended or flexed. Both flexion and extension at the fingers are maximal when the wrist is in a neutral position (not abducted or adducted); flexion and extension of the wrist are minimal when the wrist is in pronation.
The wrist and hand have both a fixed (stable) and a mobile segment. The fixed segment consists of the distal row of carpal bones (trapezium, trapezoid, capitate, and hamate) and the second and third metacarpals. This is the stable segment of the wrist and hand (Figure 7-27), and movement between these bones is less than that between the bones of the mobile segment. This arrangement allows stability without rigidity, enables the hand to move more discretely and with suppleness, and enhances the function of the thumb and fingers when they are used for power and/or precision grip. The mobile segment is made up of the five phalanges and the first, fourth, and fifth metacarpal bones.
The functional position of the wrist is extension to between 20° and 35° with ulnar deviation of 10° to 15°.15 This position, sometimes called the position of rest, minimizes the restraining action of the long extensor tendons and allows complete flexion of the finger; thus, the greatest power of grip occurs when the wrist is in this position (Figure 7-28). In this position, the pulps of the index finger and thumb come into contact to facilitate thumb-finger action. The position of wrist immobilization (Figure 7-29) is further extension than is seen in the position of rest with the metacarpophalangeal joints more flexed and the interphalangeal joints extended. In this way, when the joints are immobilized, the potential for contracture is kept to a minimum.
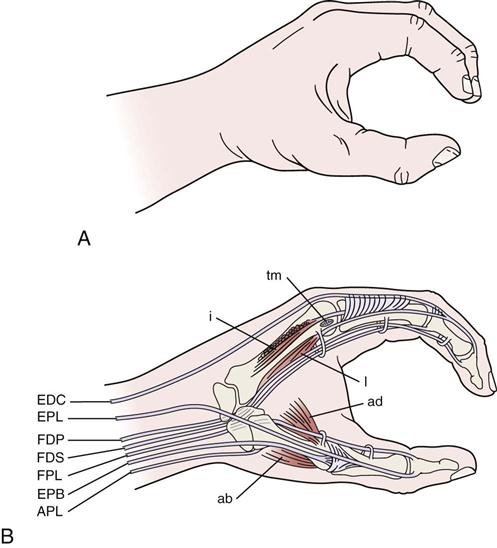
A, Normal view. B, The hand is in the position of function. Notice in particular that a very small amount of motion in the thumb and fingers is useful motion in that it can be used in pinch and grasp. Notice the close relation of the tendons to bone. The flexor tendons are held close to bone by a pulley-like thickening of the flexor sheath as represented schematically. With the hand in this position, intrinsic and extrinsic musculature is in balance, and all muscles are acting within their physiological resting length. ab, Abductor pollicis brevis; ad, adductor pollicis brevis; APL, abductor pollicis longus; EDC, extensor digitorum communis; EPB, extensor pollicis brevis; EPL, extensor pollicis longus; FDP, flexor digitorum profundus; FDS, flexor digitorum sublimis; FPL, flexor pollicis longus; i, interossei; l, lumbrical; tm, transverse metacarpal ligament;. (B, Redrawn from O’Donoghue DH: Treatment of injuries to athletes, Philadelphia, 1984, WB Saunders, p. 287.)
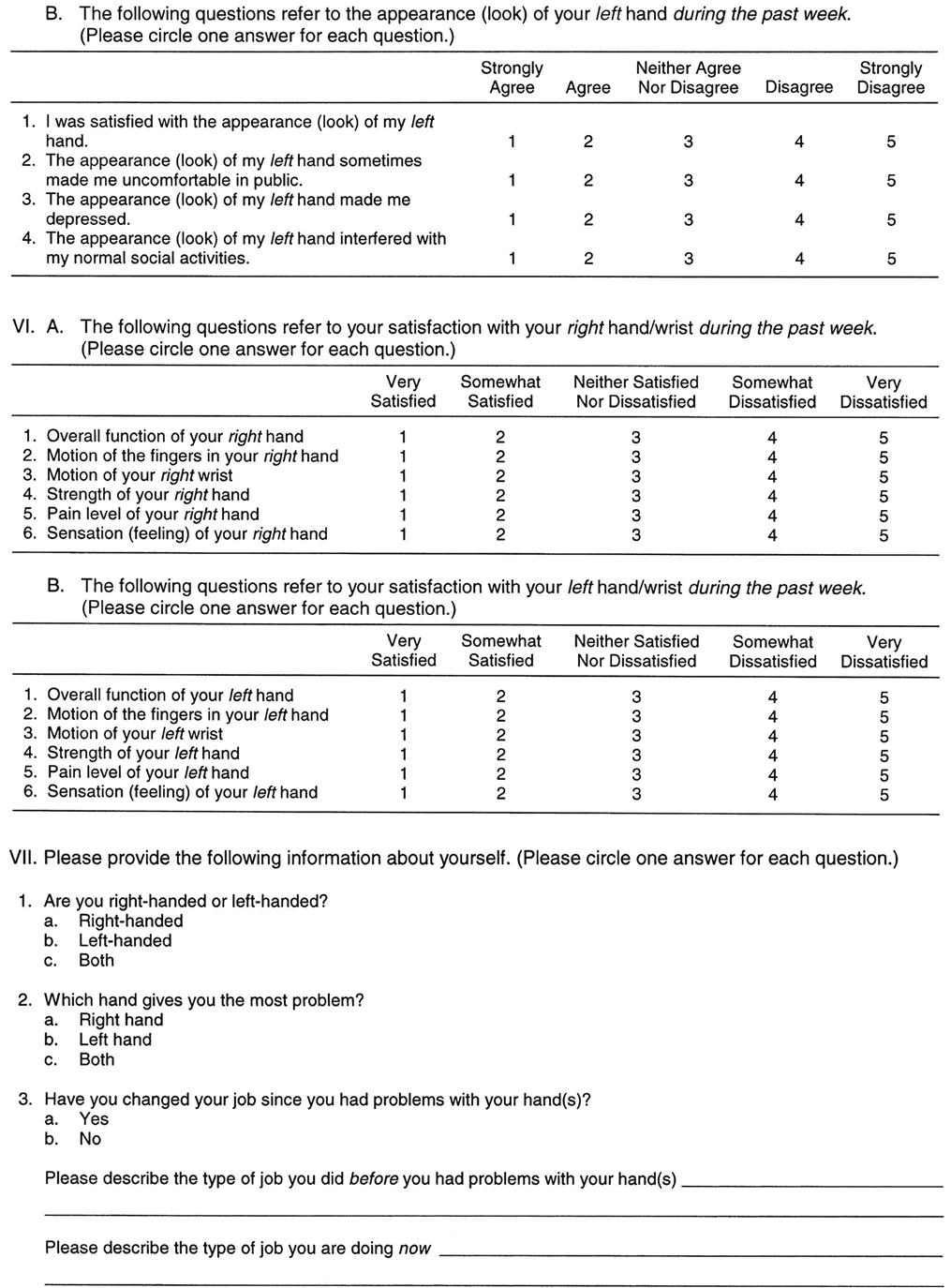
During extension at the wrist (Figure 7-30), most of the movement occurs in the radiocarpal joint (approximately 40°) and less occurs in the midcarpal joint (approximately 20°).14 The motion of extension is accompanied by slight radial deviation and pronation of the forearm. During wrist flexion (see Figure 7-30), most of the movement occurs in the midcarpal joint (approximately 40°) and less occurs in the radiocarpal joint (approximately 30°).14 This movement is accompanied by slight ulnar deviation and supination of the forearm. Radial deviation occurs primarily between the proximal and distal rows of carpal bones (0° to 20°) with the proximal row moving toward the ulna and the distal row moving radially. Ulnar deviation occurs primarily at the radiocarpal joint (0° to 37°).15
Active Movements
Active movements are sometimes referred to as physiological movements. If there is pathology to only one area of the hand or wrist, only that area needs to be assessed, provided the examiner is satisfied that the pathology is not affecting or has not affected the function of the other areas of the forearm, wrist, and hand. For example, if the patient has suffered a FOOSH injury to the wrist, the examiner spends most of the examination looking at the wrist. However, because positioning of the wrist can affect the function of the rest of the hand and forearm, the examiner must determine the functional effect of the injury to these other areas. Also, if the injury is chronic, adaptive changes may have occurred in adjacent joints.
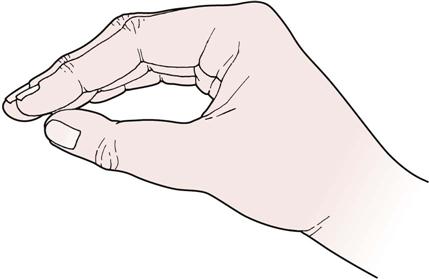
Examination is accomplished with the patient in the sitting position. As always, the most painful movements are done last. When the examiner is determining the movements of the hand, the middle finger is considered to be midline (Figure 7-31). Wrist flexion decreases as the fingers are flexed just as finger flexion decreases as the wrist flexes, and movements of flexion and extension are limited, usually by the antagonistic muscles and ligaments. In addition, pathology to structures other than the joint may restrict ROM (e.g., muscle spasm, tight ligaments/capsules). If the examiner suspects these structures, passive movement end feels will help differentiate the problem. The patient should actively perform the various movements. Initially, the active movements of the forearm, wrist, and hand may be performed in a “scanning” fashion by having the patient make a fist and then open the hand wide. As the patient does these two movements, the examiner notes any restrictions, deviations, or pain. Depending on the results, the examiner can then do a detailed examination of the affected joints. This detailed examination is initiated by selection of the appropriate active movements to be performed, keeping in mind the effect one joint can have on others.
The middle finger provides a central reference from which the other fingers abduct and adduct.
Active pronation and supination of the forearm and wrist are approximately 85° to 90°, although there is variability between individuals and it is more important to compare the movement with that of the normal side. Approximately 75° of supination or pronation occurs in the forearm articulations. The remaining 15° is the result of wrist action. If the patient complains of pain on supination, the examiner can differentiate between the distal radioulnar joint and the radiocarpal joints by passively supinating the ulna on the radius with no stress on the radiocarpal joint. If this passive movement is painful, the problem is in the distal radioulnar joint, not the radiocarpal joints. The normal end feel of both movements is tissue stretch, although in thin patients, the end feel of pronation may be bone-to-bone.
Radial and ulnar deviations of the wrist are 15° and 30° to 45°, respectively. The normal end feel of these movements is bone-to-bone.
Wrist flexion is 80° to 90°; wrist extension is 70° to 90°. The end feel of each movement is tissue stretch. Midcarpal instability may be evident on ulnar deviation. If there is midcarpal instability as the wrist is taken into ulnar deviation, the proximal row of carpals stays flexed longer and then audibly snaps or clunks into dorsiflexion (known as a “catch up clunk”).9,29,30 Instability at the radiocarpal and midcarpal joints involving groups of bones may be called carpal instability nondissociative (CIND). If there is instability of one bone relative to the other bones in the same row, it may be called carpal instability dissociative (CID).31
Flexion of the fingers occurs at the metacarpophalangeal joints (85° to 90°), followed by the proximal interphalangeal joints (100° to 115°) and the distal interphalangeal joints (80° to 90°). This sequence enables the hand to grasp large and small objects. Extension occurs at the metacarpophalangeal joints (30° to 45°), the proximal interphalangeal joints (0°), and the distal interphalangeal joints (20°). Hyperextension at the proximal interphalangeal joints can lead to a swan neck deformity. This hyperextension is usually prevented by the volar plates.3 The end feel of finger flexion and extension is tissue stretch. Finger abduction occurs at the metacarpophalangeal joints (20° to 30°); the end feel is tissue stretch. Finger adduction (0°) occurs at the same joint.
The digits are medially deviated slightly in relation to the metacarpal bones (see Figure 7-6). When the fingers are flexed, they should point toward the scaphoid tubercle. In addition, the metacarpals are at an angle to each other. These positions increase the dexterity of the hand and oblique flexion of the medial four digits but contribute to deformities (e.g., ulnar drift) in conditions, such as rheumatoid arthritis.
Thumb flexion occurs at the carpometacarpal joint (45° to 50°), the metacarpophalangeal joint (50° to 55°), and the interphalangeal joint (80° to 90°). It is associated with medial rotation of the thumb as a result of the saddle shape of the carpometacarpal joint. Extension of the thumb occurs at the interphalangeal joint (0° to 5°); it is associated with lateral rotation. Flexion and extension take place in a plane parallel to the palm of the hand. Thumb abduction is 60° to 70°; thumb adduction is 30°. These movements occur in a plane at right angles to the flexion-extension plane.15 The thumb is controlled by three nerves, a situation that is unique among the digits. The radial nerve controls extension and opening of the thumb as it does for the other digits. The ulnar nerve controls adduction, produces closure of pinch, and gives power to the grip; the median nerve controls flexion and opposition, producing precision with any grip.3 The intrinsic muscles are stronger than the extrinsic muscles of the thumb; the opposite is true for the fingers.3
If the history has indicated that combined or repetitive movements and/or sustained postures have resulted in symptoms, these movements should also be tested.
The examiner must be aware that active movements may be affected because of neurological as well as contractile tissue problems. For example, the median nerve is sometimes compressed as it passes through the carpal tunnel (Figure 7-32), affecting its motor and sensory distribution in the hand and fingers. The condition is referred to as carpal tunnel syndrome.
If the patient does not have full active ROM and it is difficult to measure ROM because of swelling, pain, or contracture, the examiner can use a ruler or tape measure to record the distance from the fingertip to one of the palmar creases (Figure 7-33).32 This measurement provides baseline data for any effect of treatment. It is important to note on the chart which crease was used in the measurement. The majority of functional activities of the hand require that the fingers and thumb to open at least 5 cm (2 inches), and the fingers should be able to flex within 1 to 2 cm (0.4 to 0.8 inch) of the distal palmar crease.33
Passive Movements
If, when watching the patient perform the active movements, the examiner believes the ROM is full, overpressure can be gently applied to test the end feel of the joint in each direction. If the movement is not full, passive movements must be carefully performed by the examiner to test the end feel. At the same time, the examiner must watch for the presence of a capsular pattern. The passive movements are the same as the active movements, and the examiner must remember to test each individual joint.
The capsular pattern of the distal radioulnar joint is full ROM with pain at the extremes of supination and pronation. At the wrist, the capsular pattern is equal limitation of flexion and extension. At the metacarpophalangeal and interphalangeal joints, the capsular pattern is flexion more limited than extension. At the trapeziometacarpal joint of the thumb, the capsular pattern is abduction more limited than extension.
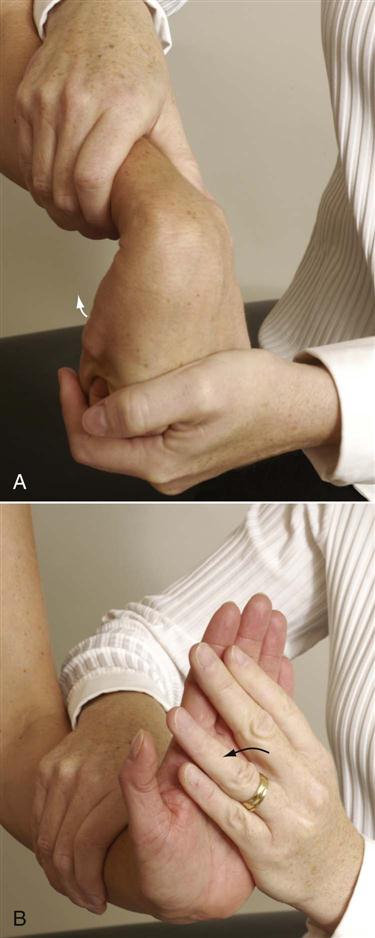
In some cases, the examiner may want to test the length of the long extensor and flexor muscles of the wrist (Figure 7-34). If the length of the muscles is normal, the passive range on testing is full and the end feel is the normal joint tissue stretch end feel. If the muscles are tight, the end feel is muscle stretch, which is not as “stretchy” as tissue or capsular stretch, and the ROM is restricted.
To test the length of the long wrist extensors, the patient is placed in supine lying with the elbow extended. The examiner passively flexes the fingers and then flexes the wrist.34 If the muscles are tight, wrist flexion is restricted.
To test the length of the long wrist flexors, the patient is placed in supine lying with the elbow extended. The examiner passively extends the fingers and then extends the wrist.34 If the muscles are tight, wrist extension is limited.
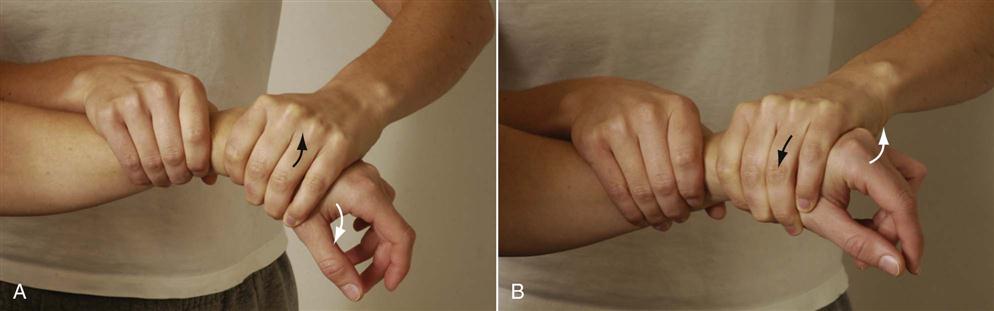
Conjunct rotation can be tested by folding and fanning the hand (Figure 7-35). To do this, the examiner holds the scaphoid and trapezium with the index and middle finger of one hand and the pisiform and hamate of the other hand while the capitate is held with the thumbs on the dorsum of the hand. The examiner then folds and fans the hand feeling the movement.35
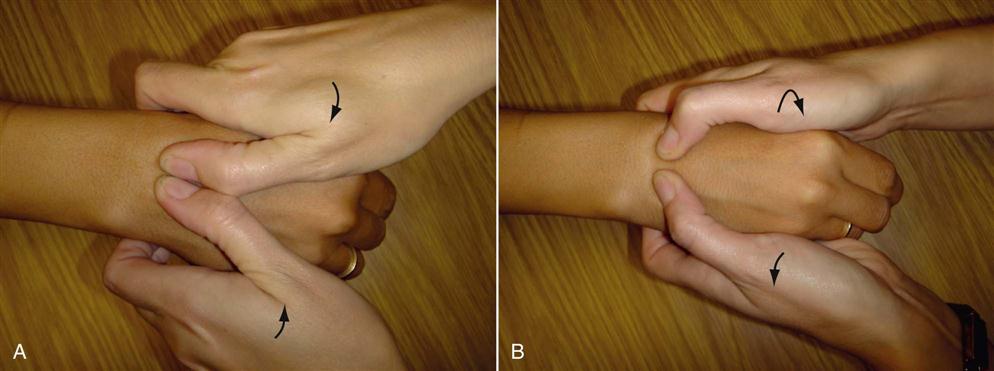
 Figure 7-35 A, Fanning of the hand. B, Folding of the hand.
Figure 7-35 A, Fanning of the hand. B, Folding of the hand.Resisted Isometric Movements
As with the active movements, the resisted isometric movements to the forearm, wrist, and hand are done with the patient in the sitting position. Not all resisted isometric movements need to be tested, but the examiner must keep in mind that the actions of the fingers and thumb and the wrist are controlled by extrinsic muscles (wrist, fingers, thumb) and intrinsic muscles (fingers, thumb), so injury affecting these structures requires testing of the appropriate muscles. The movements must be isometric and must be performed in the neutral position (Figures 7-36 and 7-37). If the history has indicated that concentric, eccentric, or econcentric movements have caused symptoms, these different types of resisted movement should be tested, but only after the movements have been tested isometrically.
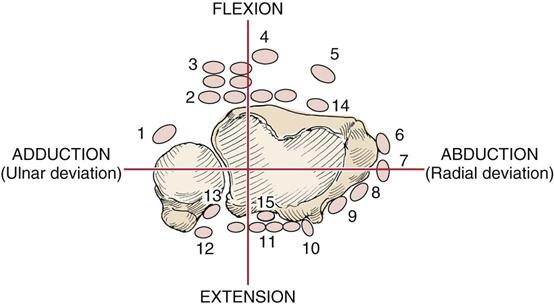
1, Flexor carpi ulnaris; 2, flexor digitorum profundus; 3, flexor digitorum superficialis; 4, palmaris longus; 5, flexor carpi radialis; 6, abductor pollicis longus; 7, extensor pollicis brevis; 8, extensor carpi radialis longus; 9, extensor carpi radialis brevis; 10, extensor pollicis longus; 11, extensor digitorum; 12, extensor digiti minimi; 13, extensor carpi ulnaris; 14, flexor pollicis longus; 15, extensor indices.
Table 7-3 shows the muscles and their actions for differentiation during resisted isometric testing. If measured by test instruments, the strength ratio of wrist extensors to wrist flexors is approximately 50%, whereas the strength ratio of ulnar deviators to radial deviators is approximately 80%. The greatest torque is produced by the wrist flexors, followed by the radial deviators, ulnar deviators, and finally the wrist extensors.36
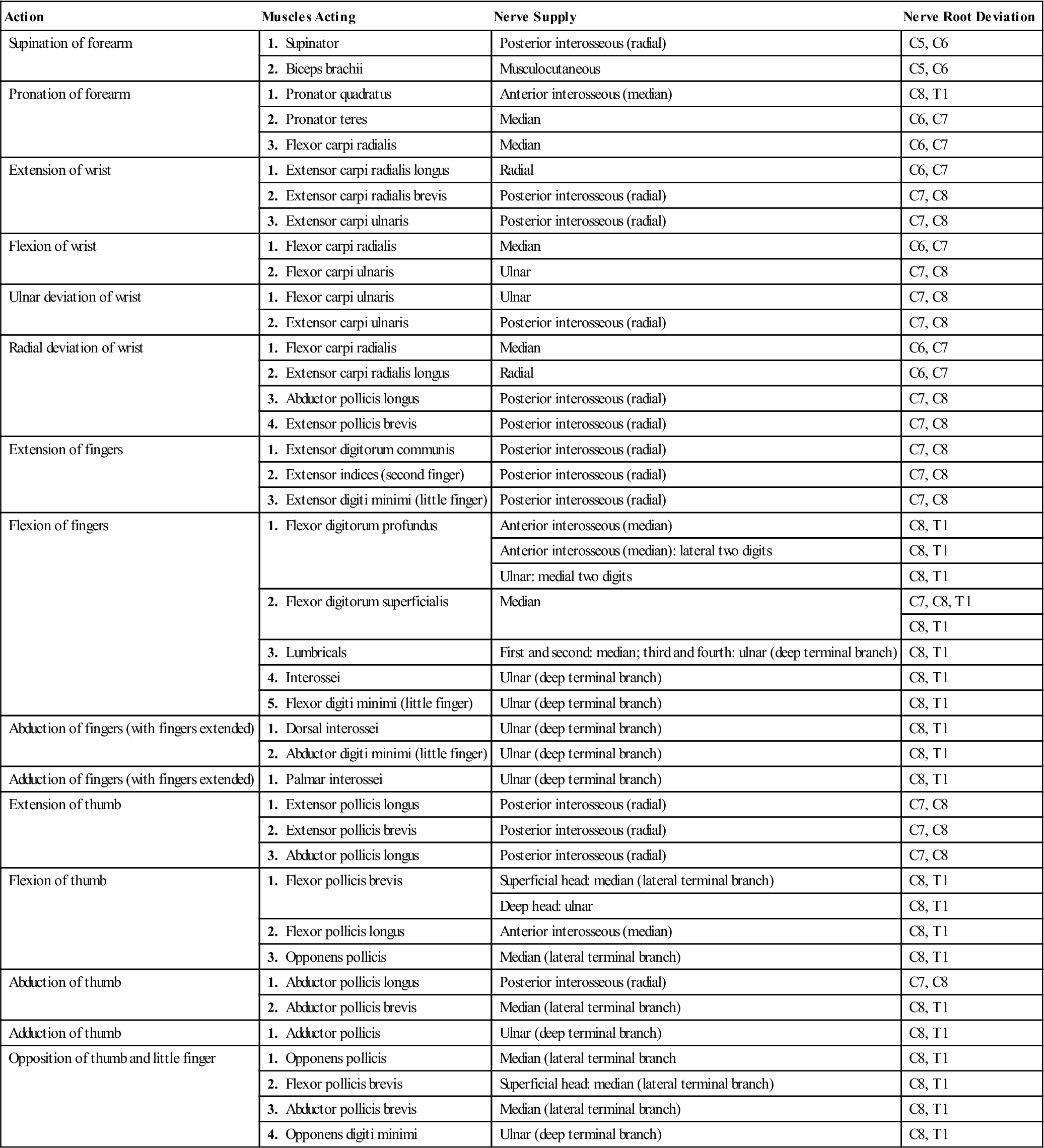
Table 7-3
Muscles of the Forearm, Wrist, and Hand: Their Actions, Nerve Supply, and Nerve Root Derivation
| Action | Muscles Acting | Nerve Supply | Nerve Root Deviation |
| Supination of forearm | 1. Supinator | Posterior interosseous (radial) | C5, C6 |
| 2. Biceps brachii | Musculocutaneous | C5, C6 | |
| Pronation of forearm | 1. Pronator quadratus | Anterior interosseous (median) | C8, T1 |
| 2. Pronator teres | Median | C6, C7 | |
| 3. Flexor carpi radialis | Median | C6, C7 | |
| Extension of wrist | 1. Extensor carpi radialis longus | Radial | C6, C7 |
| 2. Extensor carpi radialis brevis | Posterior interosseous (radial) | C7, C8 | |
| 3. Extensor carpi ulnaris | Posterior interosseous (radial) | C7, C8 | |
| Flexion of wrist | 1. Flexor carpi radialis | Median | C6, C7 |
| 2. Flexor carpi ulnaris | Ulnar | C7, C8 | |
| Ulnar deviation of wrist | 1. Flexor carpi ulnaris | Ulnar | C7, C8 |
| 2. Extensor carpi ulnaris | Posterior interosseous (radial) | C7, C8 | |
| Radial deviation of wrist | 1. Flexor carpi radialis | Median | C6, C7 |
| 2. Extensor carpi radialis longus | Radial | C6, C7 | |
| 3. Abductor pollicis longus | Posterior interosseous (radial) | C7, C8 | |
| 4. Extensor pollicis brevis | Posterior interosseous (radial) | C7, C8 | |
| Extension of fingers | 1. Extensor digitorum communis | Posterior interosseous (radial) | C7, C8 |
| 2. Extensor indices (second finger) | Posterior interosseous (radial) | C7, C8 | |
| 3. Extensor digiti minimi (little finger) | Posterior interosseous (radial) | C7, C8 | |
| Flexion of fingers | 1. Flexor digitorum profundus | Anterior interosseous (median) | C8, T1 |
| Anterior interosseous (median): lateral two digits | C8, T1 | ||
| Ulnar: medial two digits | C8, T1 | ||
| 2. Flexor digitorum superficialis | Median | C7, C8, T1 | |
| C8, T1 | |||
| 3. Lumbricals | First and second: median; third and fourth: ulnar (deep terminal branch) | C8, T1 | |
| 4. Interossei | Ulnar (deep terminal branch) | C8, T1 | |
| 5. Flexor digiti minimi (little finger) | Ulnar (deep terminal branch) | C8, T1 | |
| Abduction of fingers (with fingers extended) | 1. Dorsal interossei | Ulnar (deep terminal branch) | C8, T1 |
| 2. Abductor digiti minimi (little finger) | Ulnar (deep terminal branch) | C8, T1 | |
| Adduction of fingers (with fingers extended) | 1. Palmar interossei | Ulnar (deep terminal branch) | C8, T1 |
| Extension of thumb | 1. Extensor pollicis longus | Posterior interosseous (radial) | C7, C8 |
| 2. Extensor pollicis brevis | Posterior interosseous (radial) | C7, C8 | |
| 3. Abductor pollicis longus | Posterior interosseous (radial) | C7, C8 | |
| Flexion of thumb | 1. Flexor pollicis brevis | Superficial head: median (lateral terminal branch) | C8, T1 |
| Deep head: ulnar | C8, T1 | ||
| 2. Flexor pollicis longus | Anterior interosseous (median) | C8, T1 | |
| 3. Opponens pollicis | Median (lateral terminal branch) | C8, T1 | |
| Abduction of thumb | 1. Abductor pollicis longus | Posterior interosseous (radial) | C7, C8 |
| 2. Abductor pollicis brevis | Median (lateral terminal branch) | C8, T1 | |
| Adduction of thumb | 1. Adductor pollicis | Ulnar (deep terminal branch) | C8, T1 |
| Opposition of thumb and little finger | 1. Opponens pollicis | Median (lateral terminal branch | C8, T1 |
| 2. Flexor pollicis brevis | Superficial head: median (lateral terminal branch) | C8, T1 | |
| 3. Abductor pollicis brevis | Median (lateral terminal branch) | C8, T1 | |
| 4. Opponens digiti minimi | Ulnar (deep terminal branch) | C8, T1 |
Functional Assessment (Grip)
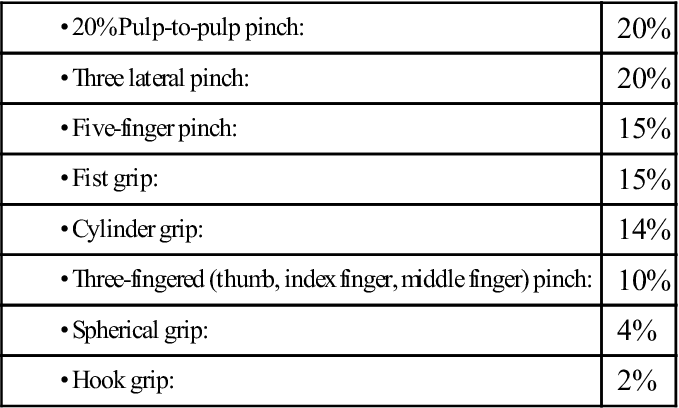
Having completed the basic movement testing of active, passive, and resisted isometric movements, the examiner then assesses the patient’s functional active movements. Functionally, the thumb is the most important digit. Because of its relation with the other digits, its mobility, and the force it can bring to bear, its loss can affect hand function greatly. The index finger is the second most important digit because of its musculature, its strength, and its interaction with the thumb. Its loss greatly affects lateral and pulp-to-pulp pinch and power grip. In flexion, the middle finger is strongest, and it is important for both precision and power grips. The ring finger has the least functional role in the hand. The little finger, because of its peripheral position, greatly enhances power grip, affects the capacity of the hand, and holds objects against the hypothenar eminence.3 In terms of functional impairment, the loss of thumb function affects about 40% to 50% of hand function. The loss of index finger function accounts for about 20% of hand function; the middle finger, about 20%; the ring finger, about 10%; and the little finger, about 10%. Loss of the hand accounts for about 90% loss of upper limb function.37
Hand function can be quickly assessed by performing a number of movements to test overall function of the wrist and hand (functional hand and wrist scan) (Figure 7-38).
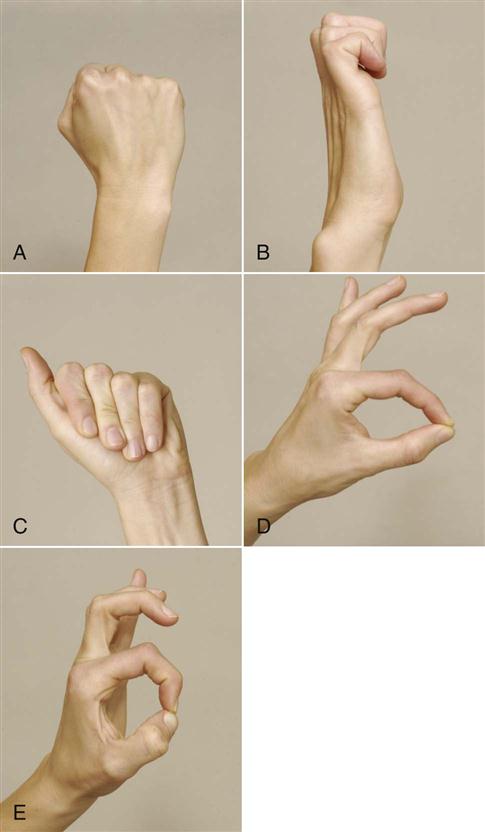
A, Standard fist. B, Hook grasp fist. C, Straight fist. D, Pulp-to-pulp pinch. E, Tip-to-tip pinch.
Although the wrist, hand, and finger joints have the ability to move through a relatively large ROM, most functional daily tasks do not require full ROM. The optimum functional ROM at the wrist is approximately 10° flexion to 35° extension along with 10° of radial deviation and 15° of ulnar deviation.38–41 Normally, the wrist is held in slight extension (10° to 15°) and slight ulnar deviation and is stabilized in this position to provide maximum function for the fingers and thumb. Excessive radial deviation, like ulnar drift of the fingers, can affect grip strength adversely.42 Functional flexion at the metacarpophalangeal and proximal interphalangeal joints is approximately 60°. Functional flexion at the distal interphalangeal joint is approximately 40°. For the thumb, functional flexion at the metacarpophalangeal and interphalangeal joints is approximately 20°.33 Within these ROMs, the hand is able to perform most of its grip15,43 and other functional activities.
The thumb, although not always used in gripping, adds another important dimension when it is used. It gives stability and helps control the direction in which the object moves. Both of these factors are necessary for precision movements. The thumb also increases the power of a grip by acting as a buttress, resisting the pressure of an object held between it and the fingers.
The nerve distribution and the functions of the digits also present interesting patterns. Flexion and sensation of the ulnar digits are controlled by the ulnar nerve and are more related to power grip. Flexion and sensation of the radial digits are controlled by the median nerve and are more related to precision grip. The muscles of the thumb, often used in both types of grip, are supplied by both nerves. In all cases of gripping, opening of the hand or release of grip depends on the radial nerve.
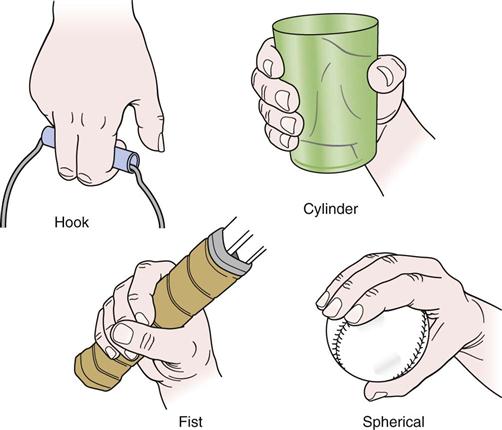
Power Grip.
A power grip requires firm control and gives greater flexor asymmetry to the hand (Figure 7-39). During power grip, the ulnar side of the hand works with the radial side to give stronger stability. The ulnar digits tend to work together to provide support and static control.3,15,43,44 This grip is used whenever strength or force is the primary consideration. With this grip, the digits maintain the object against the palm; the thumb may or may not be involved, and the extrinsic (forearm) muscles are more important. The combined effect of joint position brings the hand into line with the forearm. For a power grip to be formed, the fingers are flexed and the wrist is in ulnar deviation and slightly extended. Examples of power grips include the hook grasp, in which all or the second and third fingers are used as a hook controlled by the forearm flexors and extensors. The hook grasp may involve the interphalangeal joints only or the interphalangeal and metacarpophalangeal joints (the thumb is not involved). In the cylinder grasp, a type of palmar prehension, the thumb is used, and the entire hand wraps around an object. With the fist grasp, or digital palmar prehension, the hand moves around a narrow object. Another type of power grip is the spherical grasp, another type of palmar prehension, in which there is more opposition and the hand moves around the sphere.
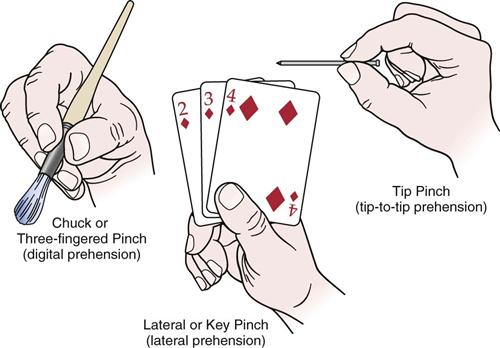
Precision or Prehension Grip.
The precision grip is an activity limited mainly to the metacarpophalangeal joints and involves primarily the radial side of the hand (Figure 7-40).15,43,44 This grip is used whenever accuracy and precision are required. The radial digits (index and long fingers) provide control by working in concert with the thumb to form a “dynamic tripod” for precision handling.3 With precision grips, the thumb and fingers are used and the palm may or may not be involved; there is pulp-to-pulp contact between the thumb and fingers, and the thumb opposes the fingers. The intrinsic muscles are more important in precision than in power grips. The thumb is essential for precision grips, because it provides stability and control of direction and can act as a buttress, providing power to the grip.3 There are three types of pinch grip. The first is called a three-point chuck, three-fingered, or digital prehension, in which palmar pinch, or subterminal opposition, is achieved. With this grip, there is pulp-to-pulp pinch, and opposition of the thumb and fingers is necessary (e.g., holding a pencil). This grip is sometimes called a precision grip with power. The second pinch grip is termed lateral key, pulp-to-side pinch, lateral prehension, or subterminolateral opposition. The thumb and lateral side of the index finger come into contact. No opposition is needed. An example of this movement is holding keys or a card. The third pinch grip is called the tip pinch, tip-to-tip prehension, or terminal opposition. With this positioning, the tip of the thumb is brought into opposition with the tip of another finger. This pinch is used for activities requiring fine coordination rather than power.
Testing Grip Strength
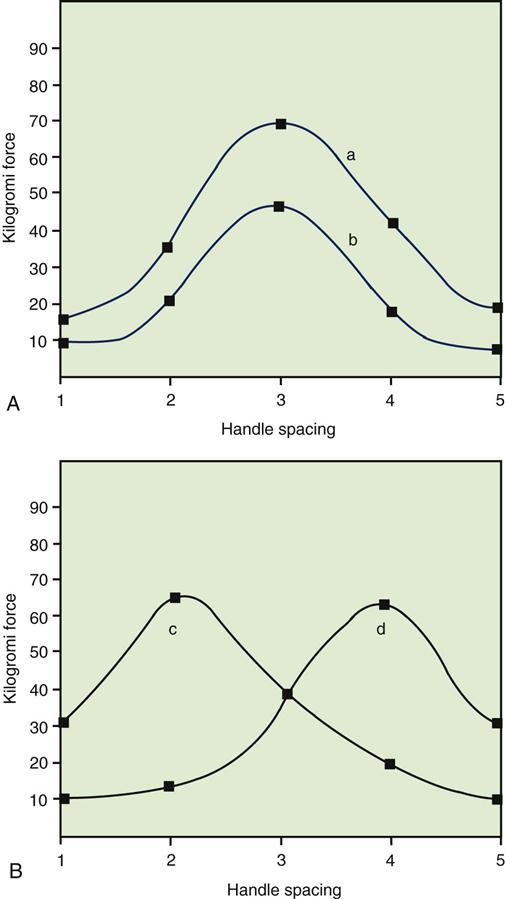
When testing grip strength using the grip dynamometer, the examiner should use the five adjustable hand spacings in consecutive order with the patient grasping the dynamometer with maximum force (Figure 7-41). Both hands are tested alternately, and each force is recorded.47,48 Care must be taken to ensure that the patient does not fatigue. The results normally form a bell curve (Figure 7-42) with the greatest strength readings at the middle (second and third) spacings and the weakest at the beginning and at the end. There should be a 5% to 10% difference between the dominant and nondominant hands.49 With injury, the bell curve should still be present, but the force exerted is less. If the patient does not exert maximum force for each test, the typical bell curve will not be produced, nor will the values obtained be consistent. Discrepancies of more than 20% in a test-retest situation indicate that the patient is not exerting maximal force.48,50 Usually, the mean value of three trials is recorded, and both hands are compared.33 Table 7-4 gives normal values by age group and gender.
Arm should be held at the patient’s side with elbow flexed at approximately 90° when grip is measured.
Table 7-4
Normal Values by Age Group (Years) and Gender for Combined Right and Left Hand Grip Strength (kg)
| AGES 15 TO 19 | AGES 20 TO 29 | AGES 30 TO 39 | AGES 40 TO 49 | AGES 50 TO 59 | AGES 60 TO 69 | |||||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| Excellent | ≥113 | ≥71 | ≥124 | ≥71 | ≥123 | ≥73 | ≥119 | ≥73 | ≥110 | ≥65 | ≥102 | ≥60 |
| Above average | 103–112 | 64–70 | 113–123 | 65–70 | 113–122 | 66–72 | 110–118 | 65–72 | 102–109 | 59–64 | 93–101 | 54–59 |
| Average | 95–102 | 59–63 | 106–112 | 61–64 | 105–112 | 61–65 | 102–109 | 59–64 | 96–101 | 55–58 | 86–92 | 51–53 |
| Below average | 84–94 | 54–58 | 97–105 | 55–60 | 97–104 | 56–60 | 94–101 | 55–58 | 87–95 | 51–54 | 79–85 | 48–50 |
| Poor | ≤83 | ≤53 | ≤96 | ≤54 | ≤96 | ≤55 | ≤93 | ≤54 | ≤86 | ≤50 | ≤78 | ≤47 |
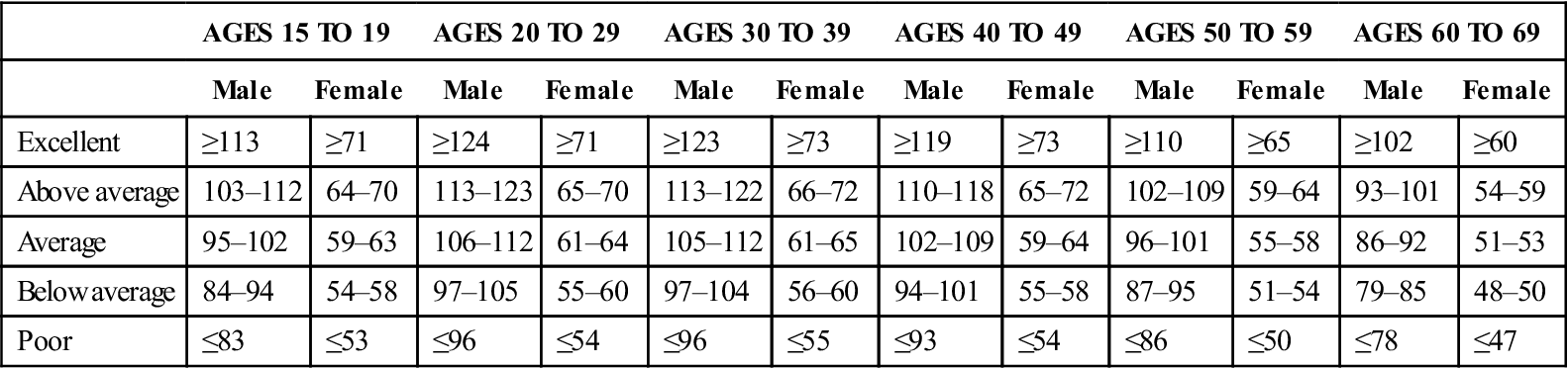
Modified from Canadian Standardized Test of Fitness: Operations Manual, Ottawa, Fitness and Amateur Sport Canada, 1986, p. 36.
Testing Pinch Strength
The strength of the pinch may be tested with the use of a pinch meter (Figure 7-43). Average values are given for pulp-to-pulp pinch of each finger with the thumb (Table 7-5), lateral prehension (Table 7-6), and pulp-to-pulp pinch (Table 7-7) for different occupational levels. Normally, the mean value of three trials is recorded, and both hands are compared.

Table 7-5
Average Strength of Chuck (Pulp-to-Pulp) Pinch with Separate Digits (100 Subjects)
| PULP-TO-PULP PINCH (kg) | ||||
| MALE HAND | FEMALE HAND | |||
| Digit | Major | Minor | Major | Minor |
| II | 5.3 | 4.8 | 3.6 | 3.3 |
| III | 5.6 | 5.7 | 3.8 | 3.4 |
| IV | 3.8 | 3.6 | 2.5 | 2.4 |
| V | 2.3 | 2.2 | 1.7 | 1.6 |
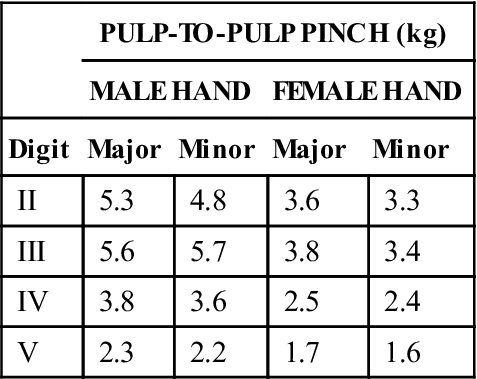
From Hunter J, Schneider LH, Mackin EJ, et al, editors: Rehabilitation of the hand: surgery and therapy, St Louis, 1990, CV Mosby, p. 115.
Table 7-6
Average Strength of Lateral Prehension Pinch by Occupation (100 Subjects)
| LATERAL PREHENSION PINCH (kg) | ||||
| MALE HAND | FEMALE HAND | |||
| Occupation | Major | Minor | Major | Minor |
| Skilled | 6.6 | 6.4 | 4.4 | 4.3 |
| Sedentary | 6.3 | 6.1 | 4.1 | 3.9 |
| Manual | 8.5 | 7.7 | 6.0 | 5.5 |
| Average | 7.5 | 7.1 | 4.9 | 4.7 |
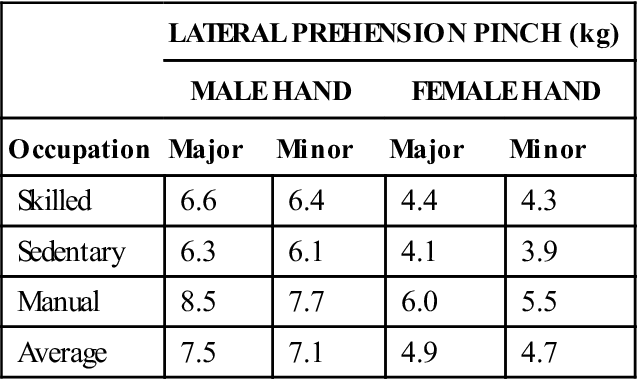
From Hunter J, Schneider LH, Mackin EJ, et al, editors: Rehabilitation of the hand: surgery and therapy, St Louis, 1990, CV Mosby, p. 114.
Table 7-7
Average Strength of Chuck (Pulp-to-Pulp) Pinch by Occupation (100 Subjects)
| PULP-TO-PULP PINCH (kg) | ||||
| MALE HAND | FEMALE HAND | |||
| Occupation | Major | Minor | Major | Minor |
| Skilled | 7.3 | 7.2 | 5.4 | 4.6 |
| Sedentary | 8.4 | 7.3 | 4.2 | 4.0 |
| Manual | 8.5 | 7.6 | 6.1 | 5.6 |
| Average | 7.9 | 7.5 | 5.2 | 4.9 |
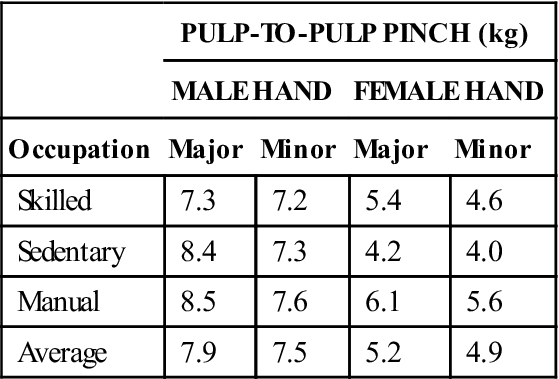
From Hunter J, Schneider LH, Mackin EJ, et al, editors: Rehabilitation of the hand: surgery and therapy, St Louis, 1990, CV Mosby, p. 114.
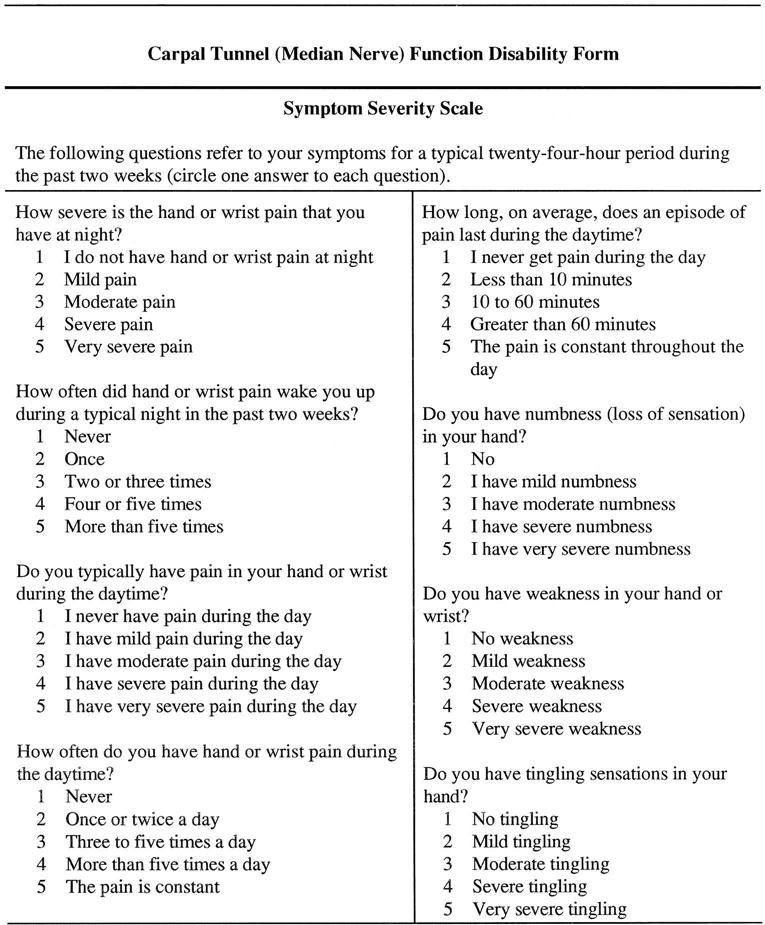
Other Functional Testing Methods
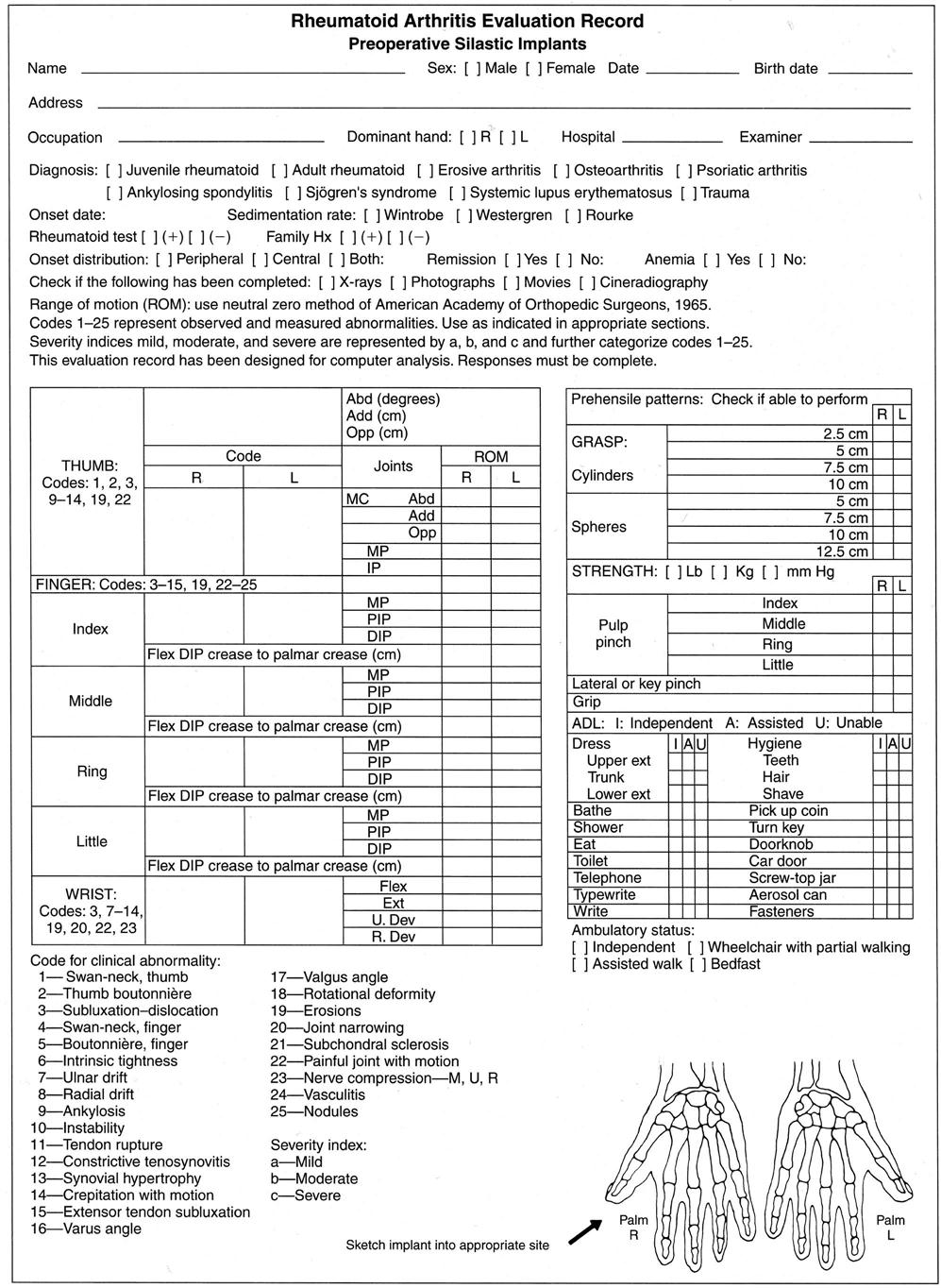
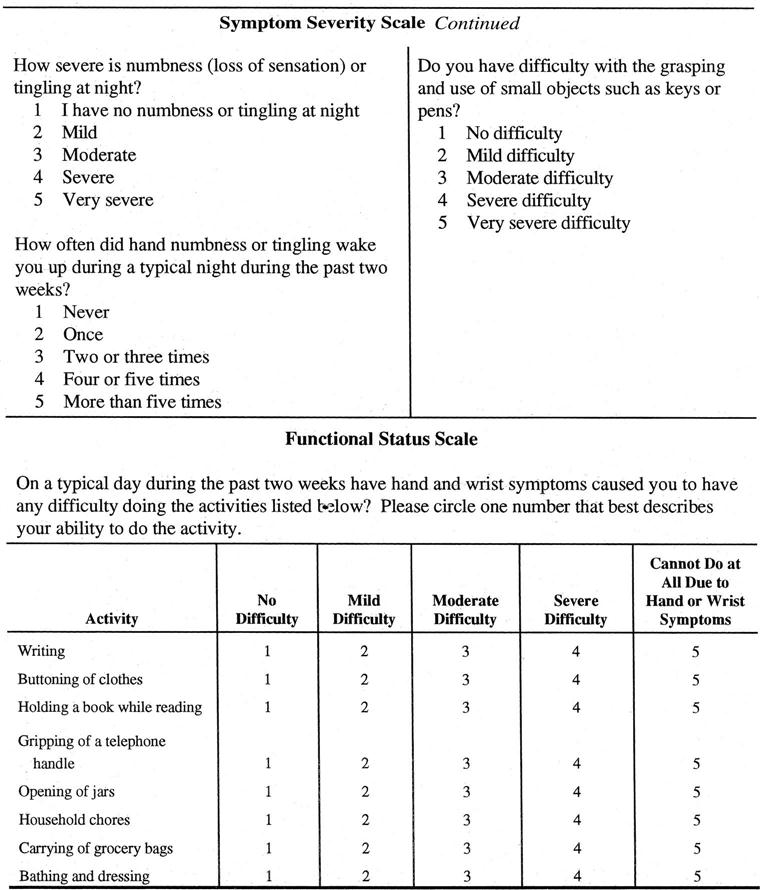
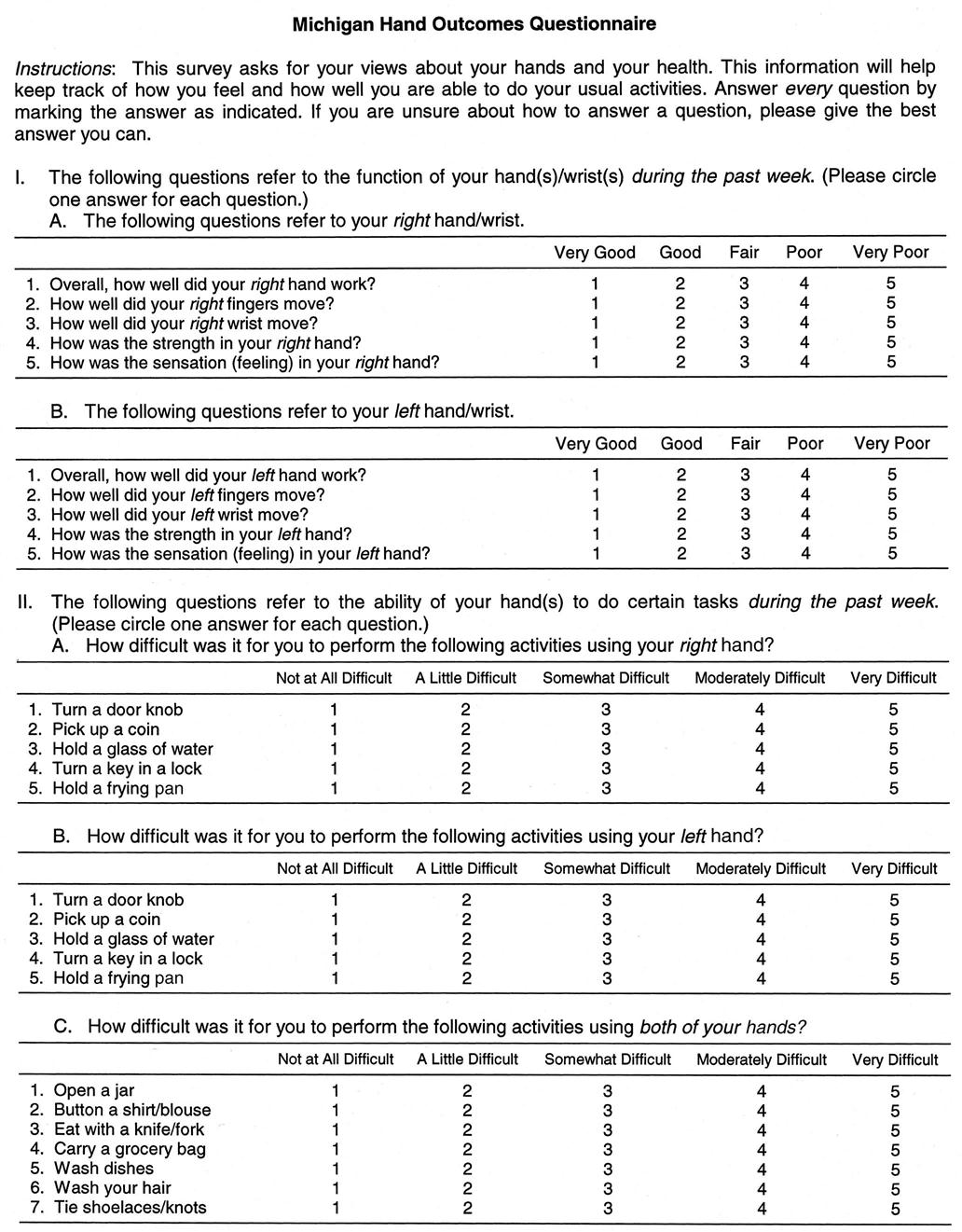
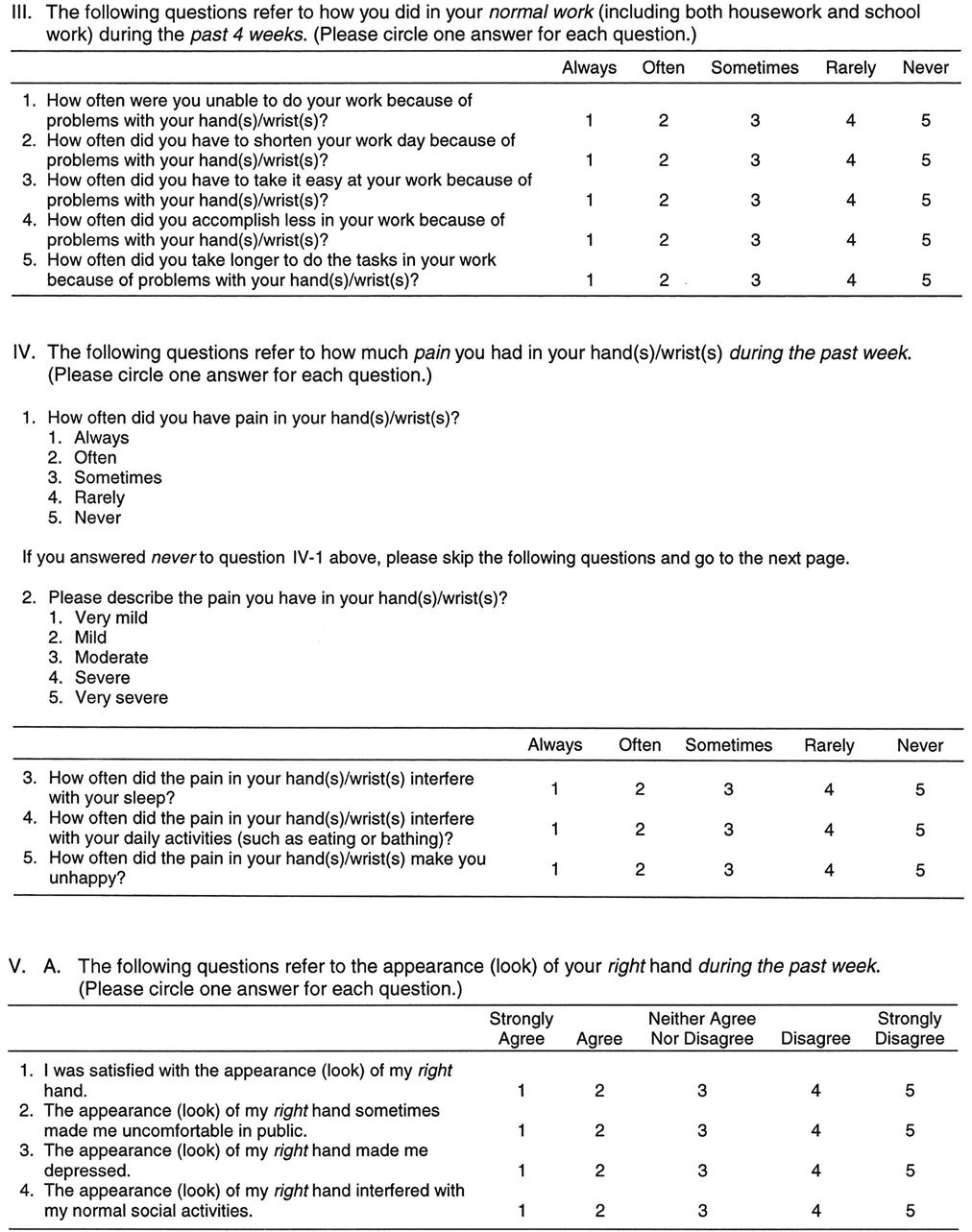
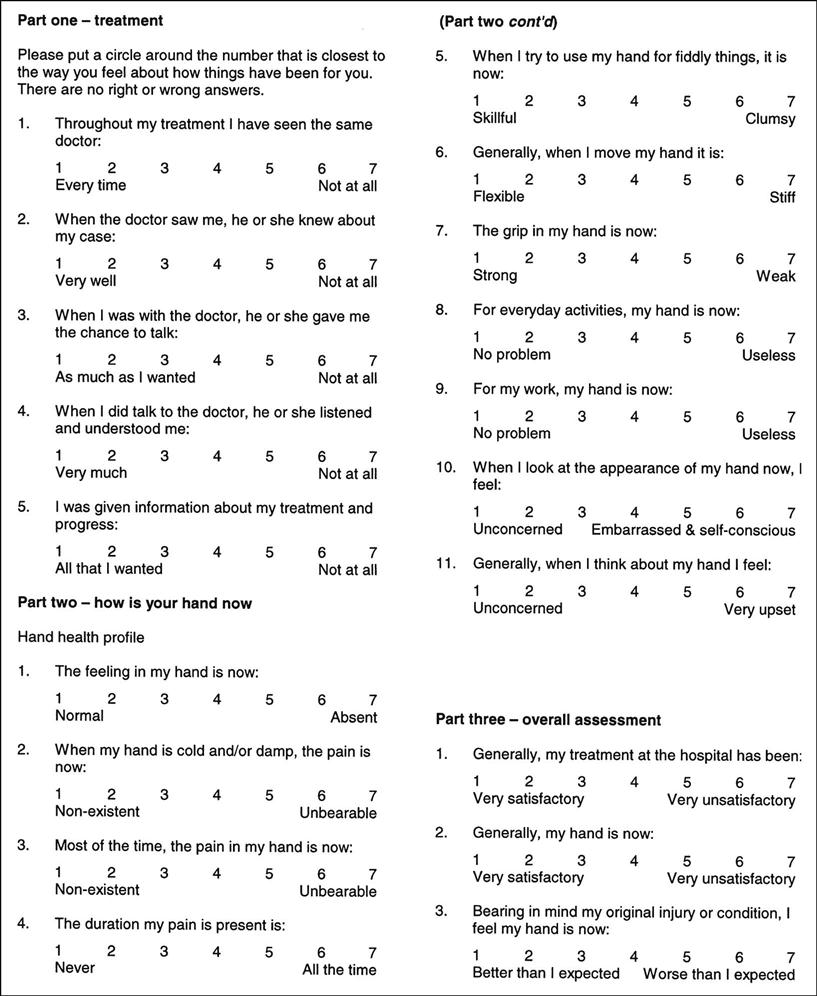
In addition to testing grip and pinch strength, the examiner may want to perform a full functional assessment of the patient. Figures 7-44 and 7-45 give examples of functional assessment forms for the hand. These forms are not numerical scoring charts, but they do include some functional aspects. Levine, et al.51 have developed a severity questionnaire including a functional component to measure severity of symptoms and functional disability for a nerve—in this case, the median nerve in the carpal tunnel (Figure 7-46). Chung, et al.52 have developed a very comprehensive hand outcomes questionnaire—the Michigan Hand Outcomes Questionnaire, which gives the patient’s evaluation of his or her outcome based on overall hand function, activities of daily living (ADLs), pain, work performance, esthetics, and patient satisfaction (Figure 7-47). Likewise, Dias, et al.53 have developed the Patient Evaluation Measure (PEM) Questionnaire (Figure 7-48). Table 7-8 provides a functional testing method. These strength values would be considered normal for an average population. They would be considered low for an athletic population or for persons in occupations subjecting the forearm, wrist, and hand to high repetitive loads.
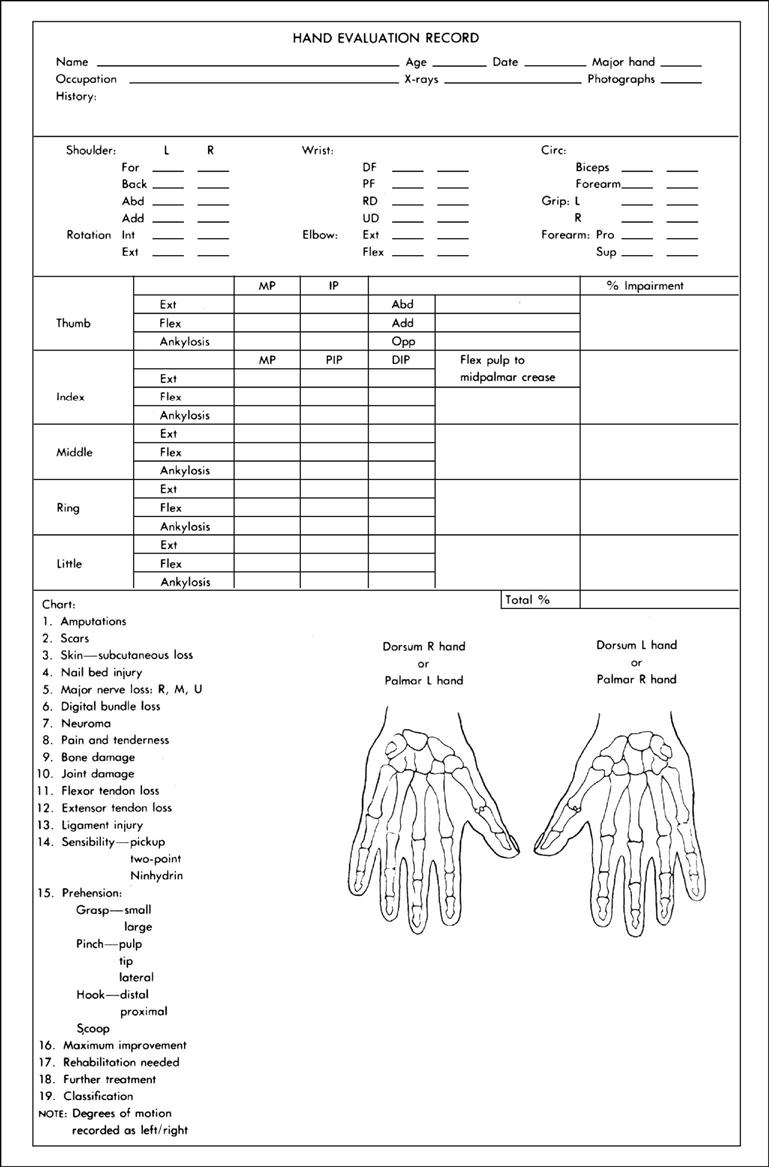
This form is designed for posttraumatic conditions and other disorders of the hand. (Modified from Swanson AB: Flexible implant resection arthroplasty in the hand and extremities, St Louis, 1973, CV Mosby.)
Table 7-8
Functional Testing of the Wrist and Hand
| Starting Position | Action | Functional Test |
| 1. Forearm supinated, resting on table | Wrist flexion | |
| 2. Forearm pronated, resting on table | Wrist extension lifting 1 to 2 lbs | |
| 3. Forearm between supination and pronation, resting on table | Radial deviation lifting 1 to 2 lbs | |
| 4. Forearm between supination and pronation, resting on table | Thumb flexion with resistance from rubber band* around thumb | |
| 5. Forearm resting on table, rubber band around thumb and index finger | Thumb extension against resistance of rubber band* | |
| 6. Forearm resting on table, rubber band around thumb and index finger | Thumb abduction against resistance of rubber band* | |
| 7. Forearm resting on table | Thumb adduction, lateral pinch of piece of paper | |
| 8. Forearm resting on table | Thumb opposition, pulp-to-pulp pinch of piece of paper | |
| 9. Forearm resting on table | Finger flexion, patient grasps mug or glass using cylindrical grasp and lifts off table | |
| 10. Forearm resting on table | Patient attempts to put on rubber glove keeping fingers straight | |
| 11. Forearm resting on table | Patient attempts to pull fingers apart (finger abduction) against resistance of rubber band* and holds | |
| 12. Forearm resting on table | Patient holds piece of paper between fingers while examiner pulls on paper |
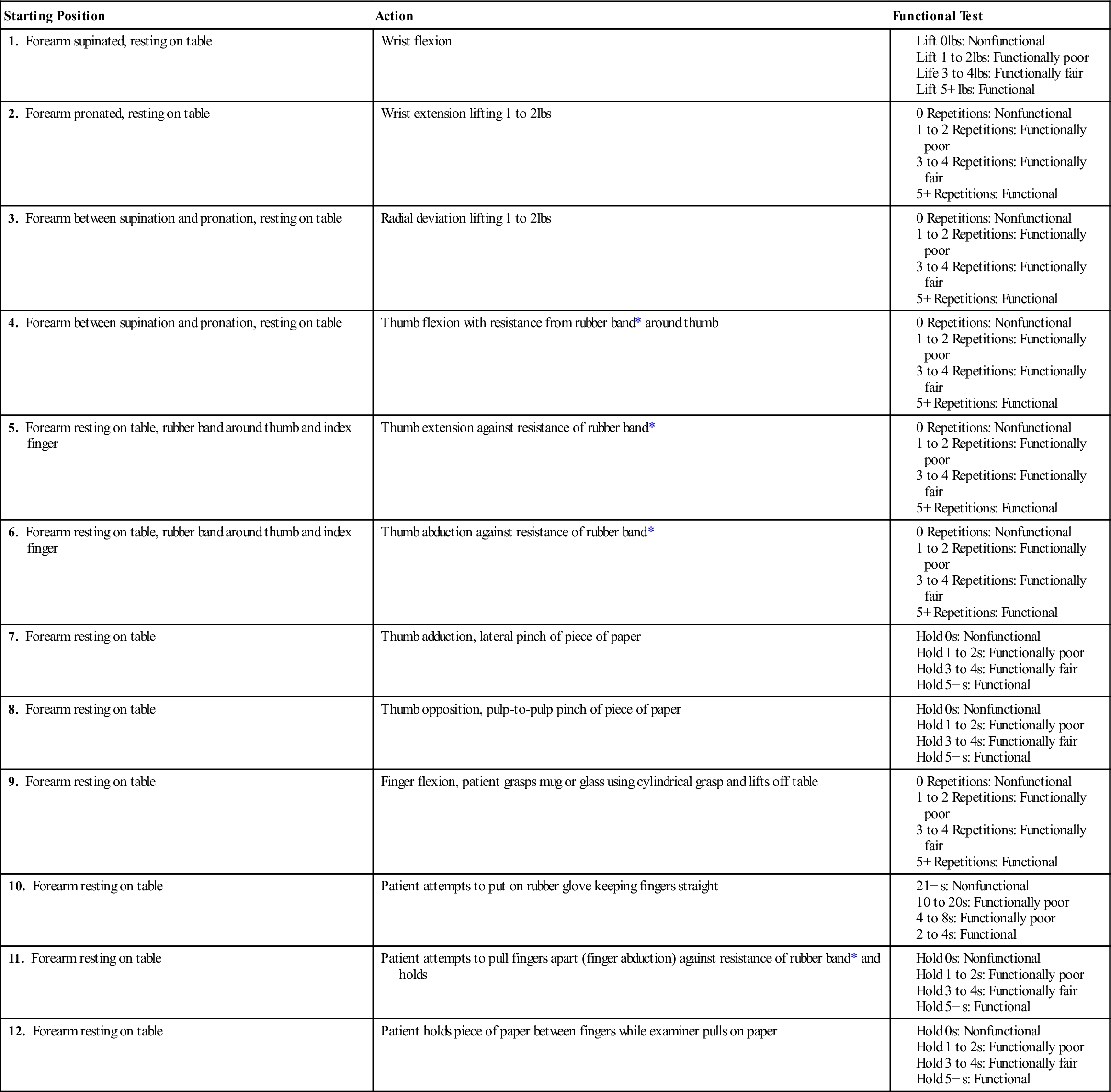
*Rubber band should be at least 1 cm wide.
Data from Palmer ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, JB Lippincott, pp. 140–144.
Functional coordinated movements may be tested by asking the patient to perform simple activities, such as fastening a button, tying a shoelace, or tracing a diagram. Different prehension patterns are used regularly during daily activities.46
These tests may also be graded on a four-point scale.47 This scale is particularly suitable if the patient has difficulty with one of the subtests, and the subtests can be scale-graded:
As part of the functional assessment, manual dexterity tests may be performed. Many standardized tests have been developed to assess manual dexterity and coordination. If comparison with other subjects is desired, the examiner must ensure that the patient is compared with a similar group of patients in terms of age, disability, and occupation. Each of these tests has its supporters and detractors. Some of the more common tests include the ones that follow.
Jebson-Taylor Hand Function Test.
This easily administered test involves seven functional areas: 1) writing; 2) card turning; 3) picking up small objects; 4) simulated feeding; 5) stacking; 6) picking up large, light objects; and 7) picking up large, heavy objects. The subtests are timed for each limb. This test primarily measures gross coordination, assessing prehension and manipulative skills with functional tests. It does not test bilateral integration.33,54–56 Anyone wishing to perform the test should consult the original article57 for details of administration.
Minnesota Rate of Manipulation Test.
This test involves five activities: 1) placing, 2) turning, 3) displacing, 4) one-hand turning and placing, and 5) two-hand turning and placing. The activities are timed for both limbs and compared with normal values. The test primarily measures gross coordination and dexterity.33,54,55
Purdue Pegboard Test.
This test measures fine coordination with the use of small pins, washers, and collars. The assessment categories of the test are: 1) right hand, 2) left hand, 3) both hands, 4) right, left, and both, and 5) assembly. The subtests are timed and compared with normal values based on gender and occupation.33,54,55
Crawford Small Parts Dexterity Test.
This test measures fine coordination, including the use of tools such as tweezers and screwdrivers to assemble things, to adjust equipment, and to do engraving.33,54
Simulated Activities of Daily Living Examination.
This test consists of nineteen subtests, including standing, walking, putting on a shirt, buttoning, zipping, putting on gloves, dialing a telephone, tying a bow, manipulating safety pins, manipulating coins, threading a needle, unwrapping a Band-Aid, squeezing toothpaste, and using a knife and fork. Each subtask is timed.46
Moberg’s Pickup Test.
An assortment of nine or ten objects (e.g., bolts, nuts, screws, buttons, coins, pens, paper clips, keys) is used. The patient is timed for the following tests:
1. Putting objects in a box with the affected hand
2. Putting objects in a box with the unaffected hand
3. Putting objects in a box with the affected hand with eyes closed
The examiner notes which digits are used for prehension. Digits with altered sensation are less likely to be used. The test is used for median or combined median and ulnar nerve lesions.58
Box and Block Test.
This is a test for gross manual dexterity in which 150 blocks, each measuring 2.5 cm (1 inch) on a side, are used. The patient has 1 minute in which to individually transfer the blocks from one side of a divided box to the other. The number of blocks transferred is given as the score. Patients are given a 15-second practice trial before the test.56
Nine-Hole Peg Test.
This test is used to assess finger dexterity. The patient places nine 3.2-cm (1.3-inch) pegs in a 12.7 × 12.7 cm (5 × 5 inch) board and then removes them. The score is the time taken to do this task. Each hand is tested separately.56
Special Tests
For the forearm, wrist, and hand, no special tests exist that are commonly done with each assessment. Depending on the history, observation, and examination to this point, certain special tests may be performed. The examiner picks the appropriate test or tests to help confirm the diagnosis. As with all special tests, however, the examiner must keep in mind that they are confirming tests. When they are positive, they are highly suggestive that the problem exists, but if they are negative, they do not rule out the problem. This is especially true for the tests of neurological dysfunction.
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the forearm, wrist and hand are available on the Evolve website.
APPENDIX 7-1
| ABDUCTOR POLLICIS BREVIS STRENGTH | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| ABDUCTOR POLLICIS BREVIS WEAKNESS | ||
| Specificity | Sensitivity | Odds Ratio |
| ANATOMICAL SNUFF BOX | ||
| Specificity | Sensitivity | Odds Ratio |
| BALLOTTEMENT TEST | ||
| Specificity | Sensitivity | Odds Ratio |
| BOX AND BLOCK TEST | |
| Reliability | Validity |
| DURKAN’S TEST | ||
| Specificity | Sensitivity | Odds Ratio |
| FIGURE OF EIGHT METHOD (HAND SIZE) | |
| Reliability | Validity |
| KEY PINCH STRENGTH | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| LATERAL PINCH STRENGTH | |||
| Reliability | |||
| MODIFIED ALLEN TEST | |||
| Validity | Specificity | Sensitivity | Odds Ratio |
| MODIFIED JEBSEN TEST OF HAND FUNCTION | |
| Reliability | Validity |
| MOTOR POWER | |
| Reliability | |
| MURPHY’S SIGN | ||
| Specificity | Sensitivity | Odds Ratio |
| NINE HOLD PEG TEST | |
| Reliability | Validity |
| PAIN WITH LONGITUDINAL COMPRESSION OF THUMB | ||
| Specificity | Sensitivity | Odds Ratio |

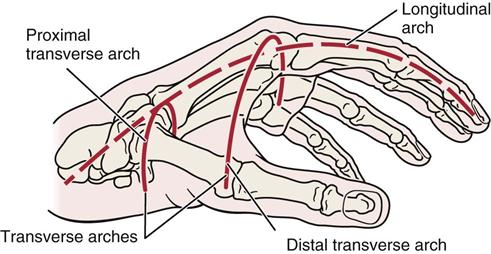
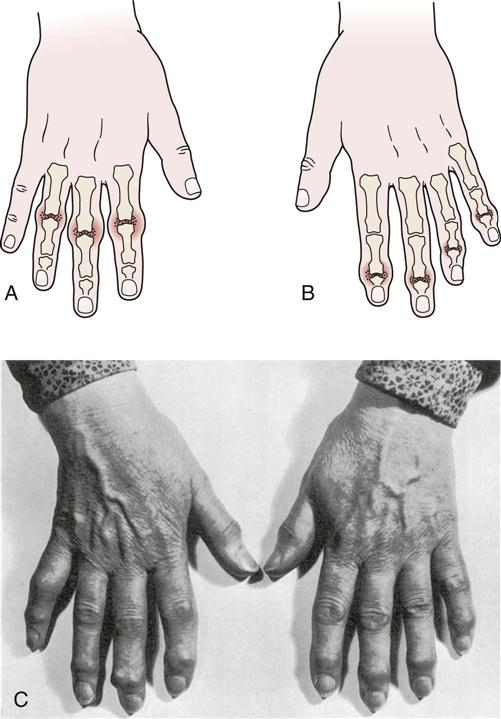

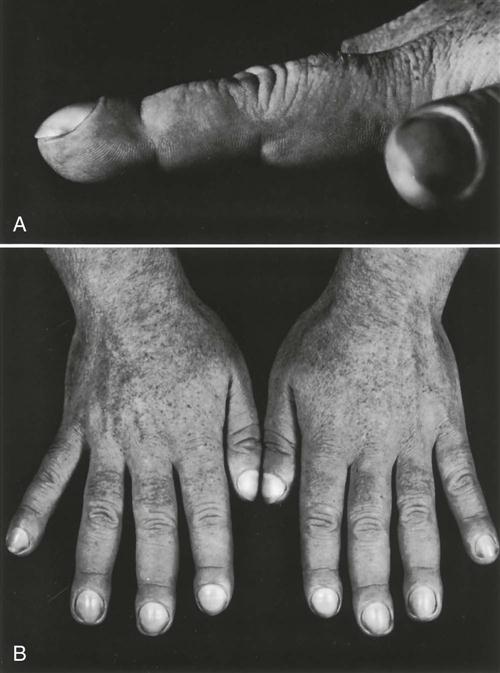
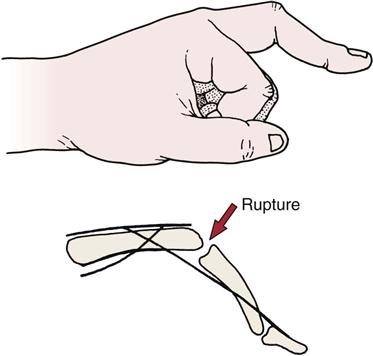
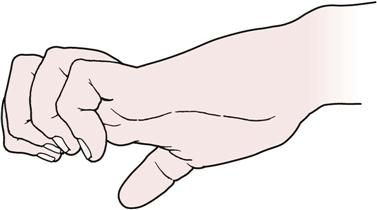
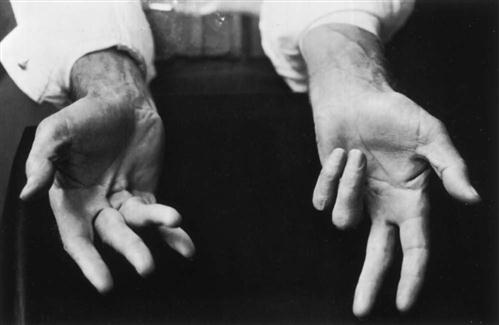
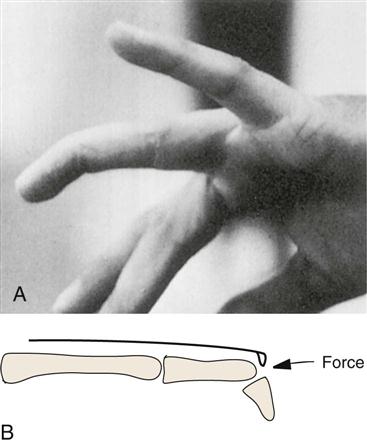
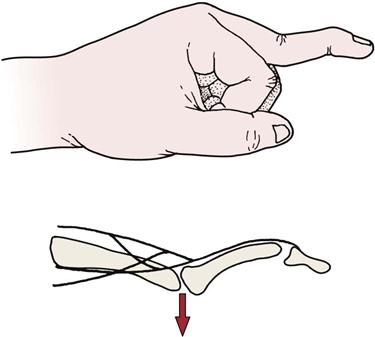
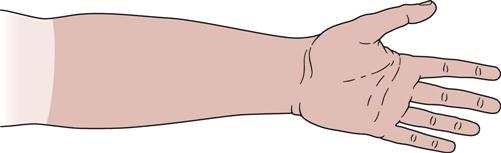
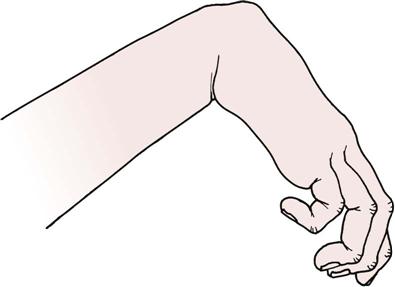
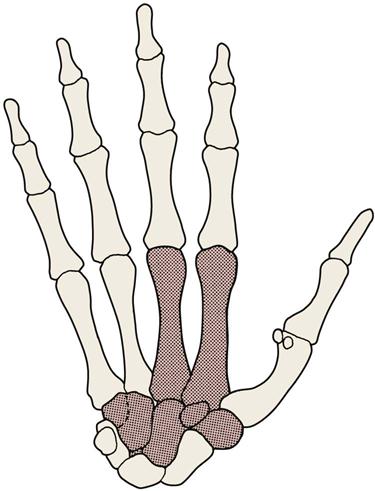
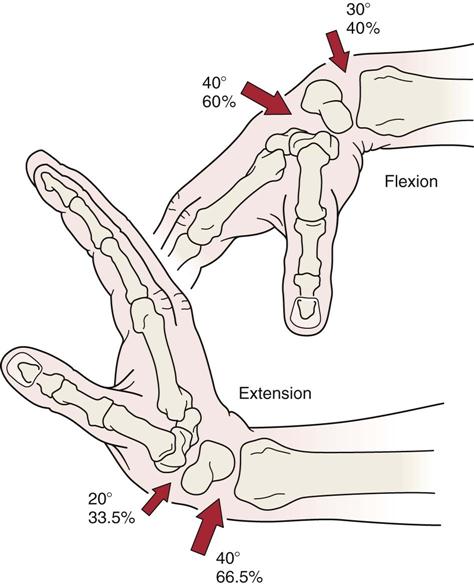
 Figure 7-30
Figure 7-30