31
Folliculitis
Superficial Folliculitis
• Common; characterized by follicular papules or pustules that are often on an erythematous base.
• Often pruritic, sometimes painful.
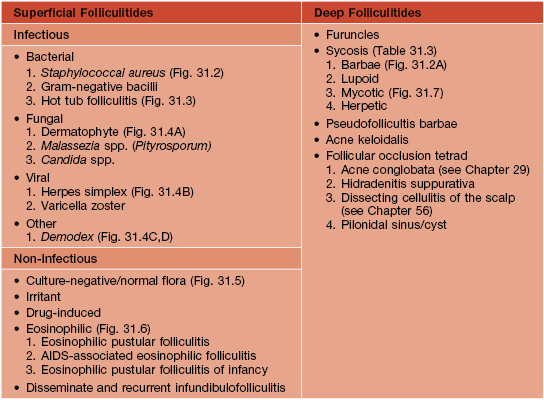
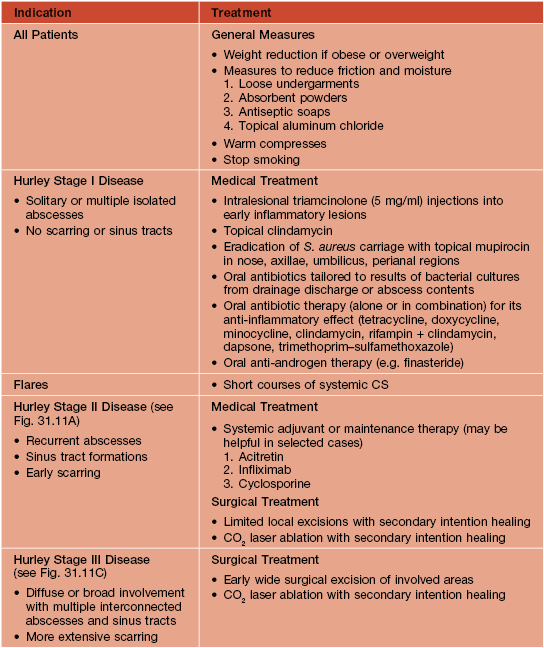
• Multiple, less common etiologies (Table 31.1), requiring a systematic approach for adequate diagnosis and treatment (Fig. 31.1; Table 31.2).
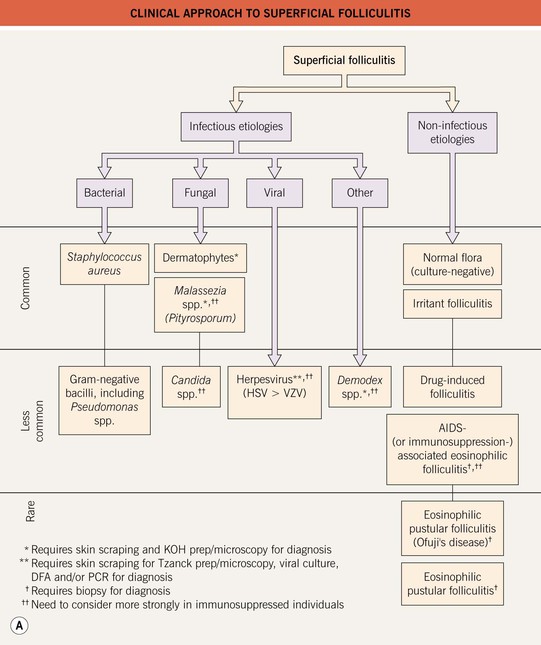
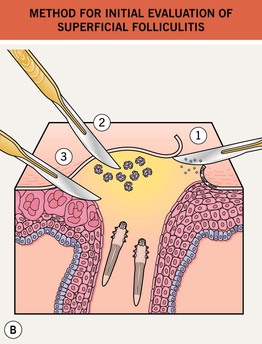
Fig. 31.1 Superficial folliculitis – clinical approach and initial evaluation. A Clinically, edematous lesions of folliculitis are most suggestive of eosinophilic folliculitis, Demodex folliculitis, and Pseudomonas ‘hot tub’ folliculitis. B If considering dermatophytes, Malassezia spp., or Candida spp., then obtain scrapings from the peripheral scale and the roof of the follicular pustule for KOH (potassium hydroxide) microscopy (1). If considering bacterial etiologies, and depending on the host, the pustular fluid should be sent for gram stain, culture, and sensitivity (2). If considering viral etiologies, the base of the unroofed lesion should be vigorously scraped in order to collect the viral-laden keratinocytes for Tzanck prep/microscopy, viral culture, DFA (direct fluorescent antibody), and/or PCR (polymerase chain reaction) (3). Likewise, if considering Demodex folliculitis, scrape the base of the lesion vigorously for KOH microscopy (3) (see Fig. 31.4D).
Table 31.2
Clinical features and treatment of selected superficial folliculitides.
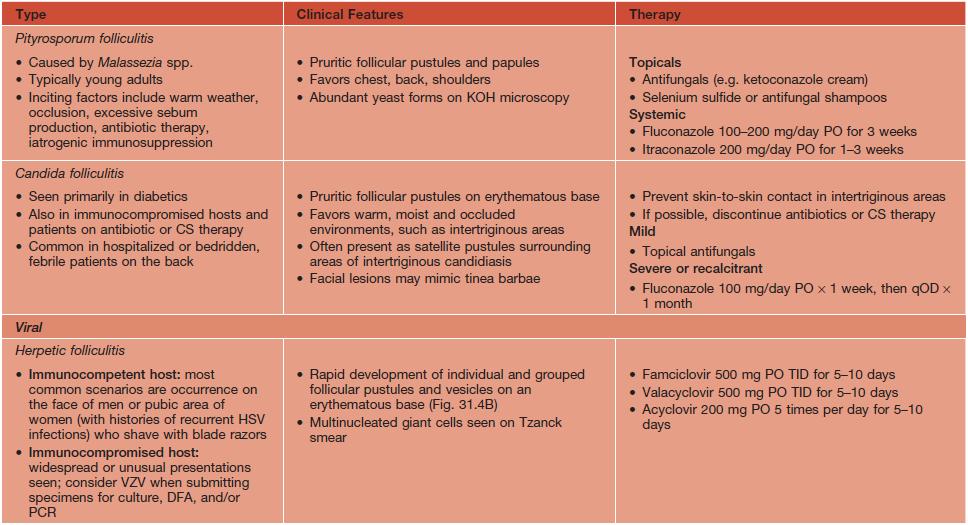
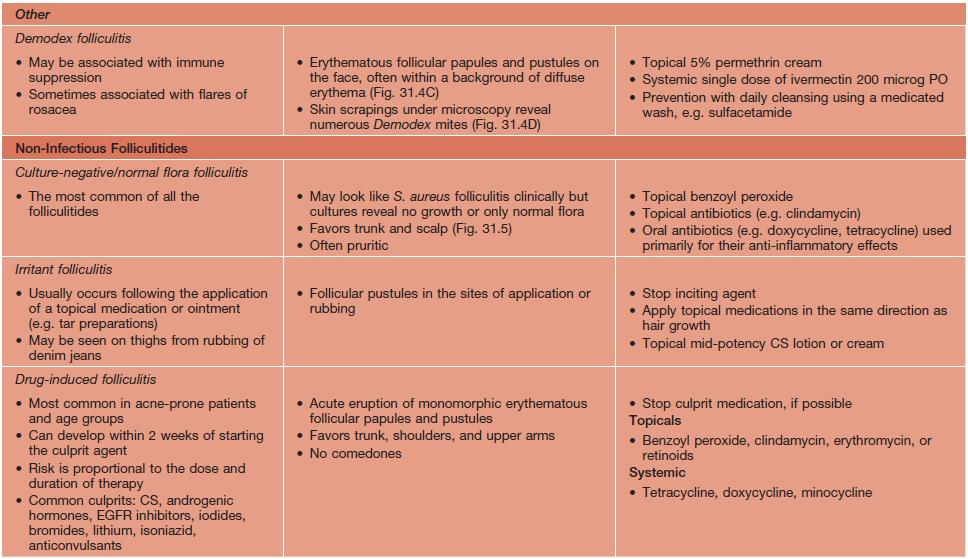
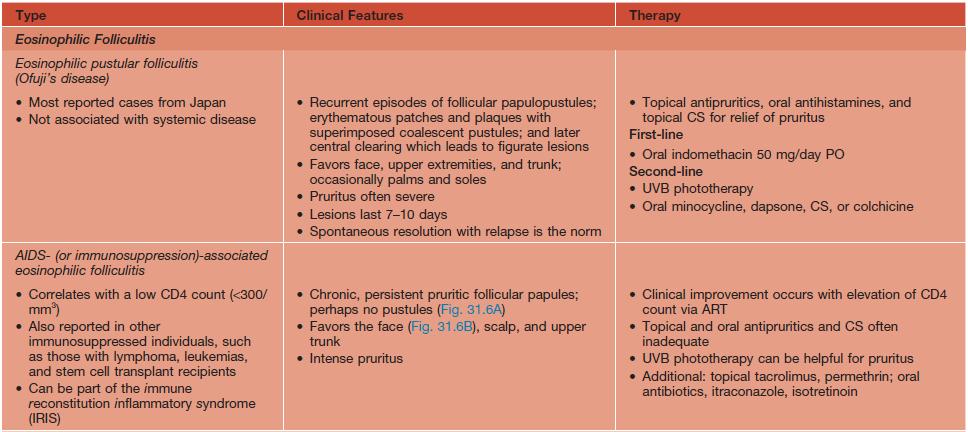
* Bleach bath involves mixing  cup of household bleach into a half-filled, regular-sized bathtub.
cup of household bleach into a half-filled, regular-sized bathtub.
PO, orally; BID, twice daily; KOH, potassium hydroxide; qOD, every other day; VZV, varicella zoster virus; DFA, direct fluorescence antibody; PCR, polymerase chain reaction; TID, three times a day; ART, antiretroviral treatment.



Fig. 31.2 Folliculitis due to Staphylococcus aureus. A Folliculitis of the beard area with discrete papulopustules seen posteriorly. Centrally, there is deeper involvement with plaque formation (sycosis barbae). B Widespread follicular pustules limited to the back of a sedated psychiatric patient. On closer examination (C), the characteristic follicular papulopustules on an erythematous base are seen, along with a collarette of scale on an older lesion, located centrally in the photo. B, C, Courtesy, Julie V. Schaffer, MD.


Fig. 31.3 Pseudomonas ‘hot tub’ folliculitis. A, B Edematous follicular papules on the flank that begin to develop 2–3 days following the use of a hot tub. The number and size can vary. B, Courtesy, Kalman Watsky, MD.



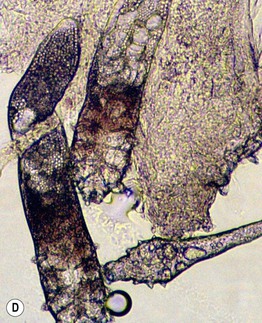
Fig. 31.4 Folliculitis – fungal, viral, and ectoparasitic. A Firm follicular papules of dermatophyte folliculitis (Majocchi’s granuloma) in the setting of extensive tinea corporis. B Follicular herpes simplex viral infection in an immunocompromised host. C Edematous papules of Demodex folliculitis superimposed on the characteristic background erythema. D Microscopic findings of follicular contents obtained via scraping of Demodex folliculitis. B, Courtesy, Karynne O. Duncan, MD. C, Courtesy, Kalman Watsky, MD.

Fig. 31.5 Culture-negative folliculitis. Follicular pustules with an erythematous rim are present on the upper back. The differential diagnosis is primarily folliculitis due to Staphylococcus aureus and acne.


Fig. 31.6 AIDS-associated eosinophilic folliculitis. A Multiple follicular papules on the chest in the setting of AIDS. There are two punch biopsy sites. Note the edematous nature of some of the lesions. B Multiple pruritic follicular papules on the face of an HIV-infected woman. There is also post-inflammatory hyperpigmentation.
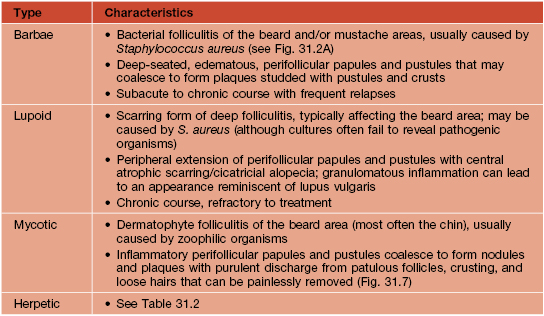
Deep Folliculitis
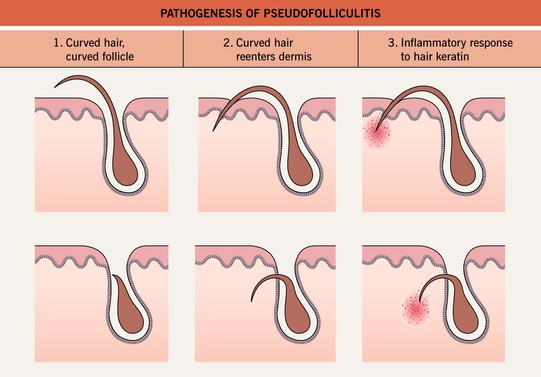
Pseudofolliculitis Barbae (PFB)
• A common, chronic inflammatory disorder occurring most often in the beard area of men who shave.
• The proposed etiology is tightly curled hairs that curve back into the skin when shaved (Fig. 31.8).
• Lesions range from inflammatory papules and pustules to firm papules and keloidal scars (Fig. 31.9).
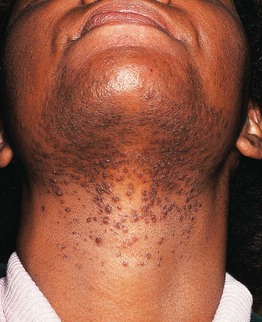
Fig. 31.9 Pseudofolliculitis barbae. Multiple firm hyperpigmented papules on the lower face and neck (beard distribution). Courtesy, A. Paul Kelly, MD.
• Intervention during the acute phase of PFB is essential.
• In addition, shaving techniques can be optimized (Table 31.4) and other treatments may provide some control (Table 31.5).
Table 31.4
Advice on shaving methods for patients with pseudofolliculitis barbae.
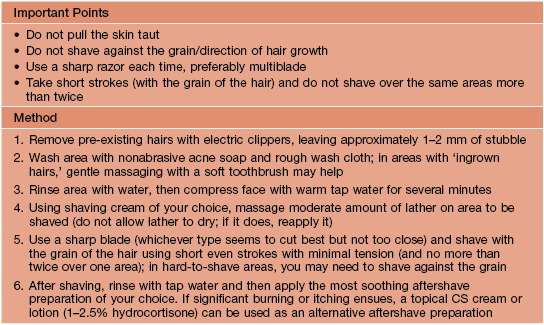
Courtesy, A. Paul Kelly, MD.
Table 31.5
Therapeutic approach to pseudofolliculitis barbae.
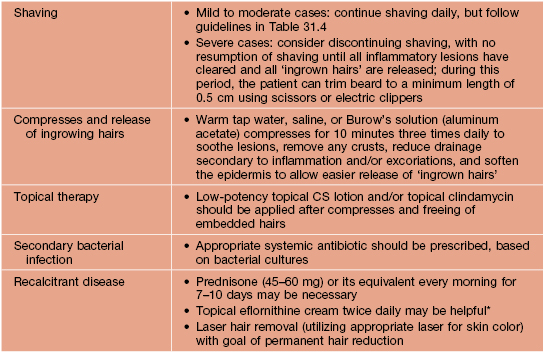
* Based on case series.
Courtesy, A. Paul Kelly, MD.
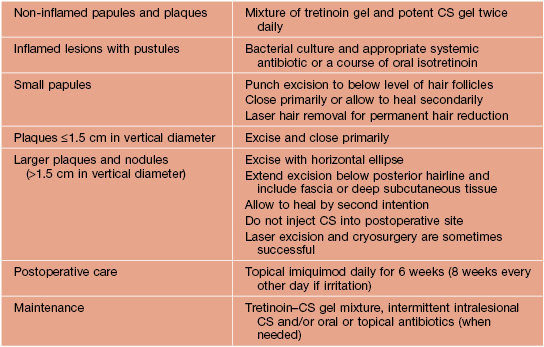
Acne Keloidalis
• Begins as a chronic folliculitis of the posterior neck and occipital scalp; with time, keloidal papules and plaques develop (Fig. 31.10).


Fig. 31.10 Acne keloidalis. A Keloidal papulonodules and a large plaque of the occipital scalp, associated with scarring alopecia. Note the tufts of hair at the superior border of the scar (arrows). B A close-up view, showing an admixture of follicular papules, crusted papules, and firm fibrotic hyperpigmented papules on the posterior neck and occipital scalp. There is associated alopecia. A, Courtesy, A. Paul Kelly, MD; B, Courtesy, A. Paul Kelly, MD, and Amy McMichael, MD.
• Seen almost exclusively in males of African descent.
• Lesions are usually pruritic and sometimes painful and disfiguring.
• The sooner this condition is treated, the less likely it will become disfiguring.
• Prevention is important, and patients should avoid mechanical irritation of the posterior hairline.
Hidradenitis Suppurativa
• Favors females > males and persons of African descent; onset at or soon after puberty.
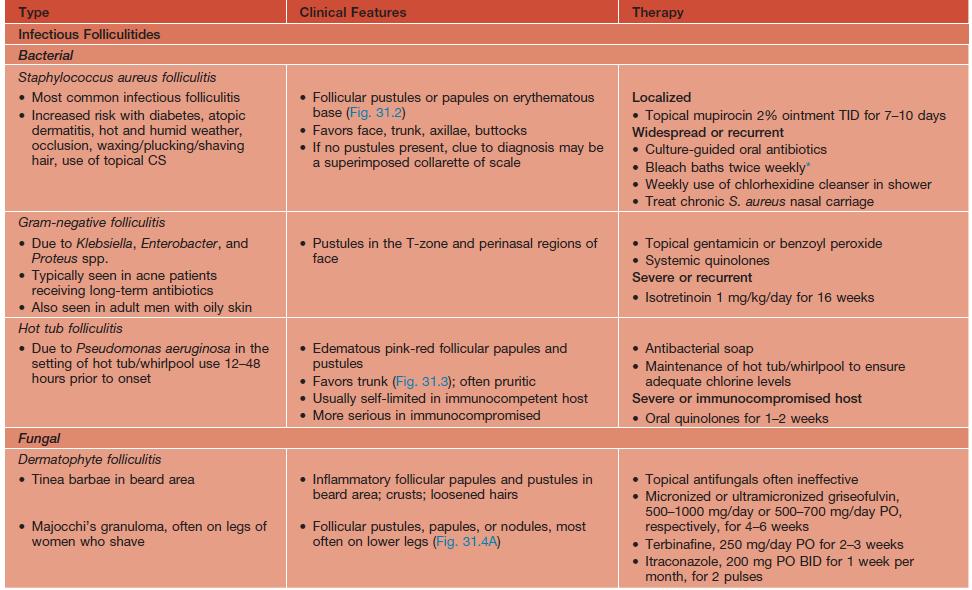
• Initially inflammatory nodules and sterile abscesses arise in the axillae, groin, perianal, and/or inframammary areas; often very painful (Fig. 31.11A).



Fig. 31.11 Hidradenitis suppurativa. A Papulopustules, nodules, sinus tracts, and scarring in the axilla (Hurley stage II). B Superficial sinus tracts that serve as a clue to the diagnosis, even in the absence of active disease. C Severe disease (Hurley stage III) with inflammatory nodules, hypertrophic scarring, draining fistulae. and sinus tract formation of the perianal region, buttocks, and upper thighs. This is the type of patient who is at risk for the development of squamous cell carcinoma and secondary amyloidosis. A, Courtesy, Kalman Watsky, MD.
• With time sinus tracts (Fig. 31.11B) and hypertrophic scars develop (Fig. 31.11C); chronic, malodorous drainage also occurs.
• DDx: staphylococcal furunculosis, Crohn’s disease, granuloma inguinale, mycetoma, and scrofuloderma (a form of tuberculous lymphadenitis with cutaneous extension).
• Rx: difficult to treat and no one perfect treatment exists; surgical excision the closest thing to a ‘cure’ (Table 31.7).
• Avoid incision and drainage, as may lead to further scarring and sinus tract formation
For further information see Ch. 38. From Dermatology, Third Edition.