4 First-Trimester Fetal Echocardiography
I. HISTORICAL BACKGROUND
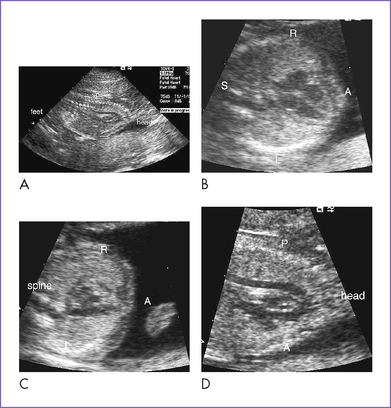
A. Normal first-trimester heart
1. Fetal cardiac anatomy was initially documented by Dolkart and Reimers in 1991, who assessed 52 fetuses ranging in gestational age from 10 to 14.9 weeks.
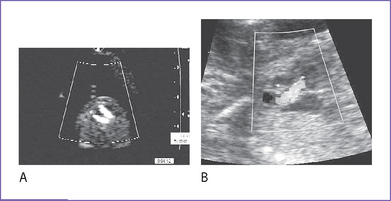
2. Normal first-trimester Doppler flow patterns were initially documented by Wladimiroff and colleagues in 1991. They assessed left and right ventricular inflow and outflow velocities in 30 fetuses ranging in gestational age from 11 to 13 weeks.
C. Transvaginal versus transabdominal approaches
1. Earlier data suggested that transabdominal imaging was less useful than transvaginal imaging for first-trimester screening.
a. Transabdominal fetal ultrasound allowed assessment of the four chambers in less than 20% at 13 to 14 weeks (Catanzarite and Quirk, 1990).
b. Transvaginal ultrasound at 13 to 14 weeks (Dolkart and Reimers, 1990; Johnson et al, 1992; Hornberger and Benacerraf, 1995).
2. More recent data suggest that transabdominal and transvaginal approaches complement each other.
a. Haak and colleagues (1992) attempted a full cardiac assessment, including a four-chamber view, aortic root, long axis of the aorta, pulmonary trunk, and great artery crossover.
b. Huggon and colleagues, 2002.
a. Hornberger and Benacerraf (1995) studied the frequency with which Doppler flow can be demonstrated and found significant improvement with gestational age.
b. Leiva and colleagues (1999) studied first-trimester changes in flow patterns.
II. LIMITATIONS
A. Reduced image resolution
1. Fetal size is a critical factor. Because this is a rapid period of general fetal growth, every week helps.
2. Fetal distance from the transducer significantly limits resolution. Transvaginal imaging should not be considered unless the fetus is less than 7 cm from the cervix.
3. Uterine anatomy can interfere with image resolution, particularly for the transvaginal approach.
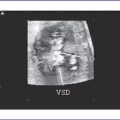
4. As a result of such limitations, ventricular septal defects, AV septal defects, and more subtle conditions such as tetralogy of Fallot with milder pulmonary outflow obstruction may be missed.
E. Safety issues
1. The operator must be aware of the acoustic output of instruments used.
a. Thermal and mechanical indices must be within recommended levels.
b. These indices provide relative risk of producing thermal or cavitation effects.
2. Risks may be greater during embryogenesis (<10 weeks; Campbell and Platt, 1999).
3. For late first-trimester assessments, use short duration of scans and limited duration of Doppler interrogation.
III. APPROACH
IV. CARDIAC PATHOLOGIES THAT CAN BE DETECTED IN THE FIRST TRIMESTER
A. Bronshtein and colleagues (1993)
1. Study included 36,323 TVG examinations in high-risk and low-risk pregnancies.
2. Isolated cardiac defect was found in 44%.
3. Extracardiac defects were found in 56% (27 of 72 karyotyped had a chromosomal abnormality).
4. Study limitations included:
a. Incomplete ascertainment of false negatives.
c. Ten had different cardiac pathology at postmortem examination or delivery.
C. Huggon and colleagues (2002)
1. Adequate transabdominal images were obtained in 402 of 478 assessed first-trimester pregnancies.
2. A normal heart was seen in 286.
a. A normal heart was verified in 189.
b. Seven had new findings later in gestation or at birth (including right aortic arch, ventricular septal defect, arch pathology, ventricular disproportion).
c. Abnormal heart was not verified in 90.
3. A definite heart defect was found in 60.
a. A defect was confirmed in 34.
b. A major lesion was identified in 33 of the 34 with a confirmed defect.
c. Important lesions were missed in 18%, including double outlet right ventricle and arch obstruction.
V. CURRENT INDICATIONS: HIGHEST-RISK PREGNANCIES
VI. VI. TAKE-HOME MESSAGE
A. Limitations
1. First-trimester fetal echocardiography is possible, particularly by 13 to 14 weeks.
2. Fetal echocardiography in the first trimester is limited by reduced image resolution and should at this stage, when possible, be followed up with an assessment in the second trimester.
3. Given that the first and early second trimesters are periods of rapid fetal cardiovascular growth, there is potential for significant change in chamber and great artery size and function, thus warranting reassessment in the second trimester to exclude more progressive lesions.
B. Approach
1. The transvaginal approach for fetal echocardiography is warranted in pregnancies less than 12 to 13 weeks and in patients in whom image resolution is not sufficient transabdominally at 13 to 15 weeks.
2. Transabdominal imaging might provide sufficient images in the majority of pregnancies at 14 weeks of gestation.
Achiron R, Weissman A, Rotstein Z, et al. Transvaginal echocardiographc examination of the fetal heart between 13 and 15 weeks’ gestation in a low-risk population. J Ultrasound Med. 1994;13:783-789.
Bronshtein M, Siegler E, Yoffe N, Zimmer EZ. Prenatal diagnosis of ventricular septal defect and overriding aorta at 14 weeks of gestation using transvaginal sonography. Prenat Diagn. 1990;10:697-702.
Bronshtein M, Zimmer EZ, Gerlis LM, et al. Early ultrasound diagnosis of fetal congenital heart effects in high and low-risk pregnancies. Obstet Gynecol. 1993;82:225-229.
Campbell S, Platt L. The publishing of papers on first trimester Doppler. Ultrasound Obstet Gynecol. 1999;14:159-160.
Carvahlo JS. Fetal heart scanning in the first trimester. Prenat Diagn. 2004;24:1060-1067.
Catanzarite V, Quirk JG. Second-trimester ultrasonography: Determinants of visualization of fetal anatomic structures. Am J Obstet Gynecol. 1990;163(4 Pt 1):1191-1195.
Dolkart LA, Reimers FT. Transvaginal fetal echocardiography in early pregnancy: Normative data. Am J Obstet Gynecol. 1991;165(3):688-689.
Gembruch U, Knopfle G, Chatterjee M, et al. First trimester diagnosis of fetal congenital heart disease by transvaginal 2-dimensional and Doppler echocardiography. Obstet Gynecol. 1990;78:496-498.
Haak MC, Twisk JW, Van Vugt JM. How successful is fetal echocardiographic examination in the first trimester of pregnancy? Ultrasound Obstet Gynecol. 2002;20:9-13.
Hornberger LK, Benacerraf BR. Blood flow velocities in the 10-20 weeks gestational age fetus. Circulation. 1996;94:1-236.
Hornberger LK, Benacerraf BR. Transvaginal fetal echocardiography in the delineation of cardiac anatomy and Doppler velocities at 10-14 weeks of gestation. Circulation. 1995;92:1-647.
Huggon IC, Ghi T, Cook AC, Zosmer N, et al. Fetal cardiac abnormalities identified prior to 14 weeks gestation. Ultrasound Obstet Gynecol. 2002;20:22-29.
Johnson P, Sharland G, Maxwell D, Allan L. The role of transvaginal fetal echocardiography in the early detection of congenital heart disease. Ultrasound Obstet Gynecol. 1992;3:248-251.
Leiva MC, Tolosa JE, Binotto CN, et al. Fetal cardiac development and hemodynamics in the first trimester. Ultrasound Obstet Gynecol. 1999;14(3):169-174.
Matias A, Huggon I, Areias JC, et al. Cardiac defects in chromosomally normal fetuses with abnormal ductus venosus blood flow at 10-14 weeks. Ultrasound Obstet Gynecol. 1999;14:307-310.
McAuliffe FM, Hornberger LK, Winsor S, et al. Fetal cardiac defects and increased nuchal translucency thickness: A prospective study. Am J Obstet Gynecol. 2004;191(4):1486-1490.
Wladimiroff JW, Huisman TW, Stewart PA. Fetal cardiac flow velocities in the late 1st trimester of pregnancy: A transvaginal Doppler study. J Am Coll Cardiol. 1991;17(6):1357-1359.
Yagel S, Weissman A, Rotstein Z, et al. Congenital heart defects: natural course and in utero development. Circulation. 1997;96(2):550-555.