76 Facial Trauma
• Treatment of all facial injuries should initially be directed toward maintaining the airway and stabilizing life-threatening injuries.
• Facial computed tomography is routinely performed to visualize facial fractures; however, plain radiographs may be sufficient in patients with isolated facial injury and a low index of suspicion for a midface fracture or concomitant intracranial injuries.
Perspective
A person’s face is the focal point of conversation and social interaction. Within the face is embodied each person’s mode of expression and communication. The face also has a receptive importance, with many special sensory functions of the body located within the facial structures. It is not surprising that facial disfigurement harbors the potential for both physical impairment and long-term psychologic sequelae.1,2
Death from facial trauma is rare, and the severity of facial injuries is often perceived by the patient to be out of proportion to the actual injury. The goal of the emergency physician (EP) is to secure the airway, identify the injury, preserve appearance, and consult with the appropriate surgeon to determine further treatment and follow-up.3 Although zygomatic and nasal fractures may occur in isolation, any fracture of the frontal bone and maxilla must raise suspicion for the possibility of associated facial fractures, intracranial injury, and concomitant cervical spine injury.4–7 Proper diagnosis and recognition of zygoma and nasal pathology are essential for maintenance of adequate cosmetic and physiologic function. Trauma involving the mandible, the strongest facial bone, may result in fracture or dislocation. Fifty percent of mandibular fractures occur at two or more locations because of its pseudo-ring shape. Detection of one fracture site should always prompt a search for a second fracture.8
General Anatomy
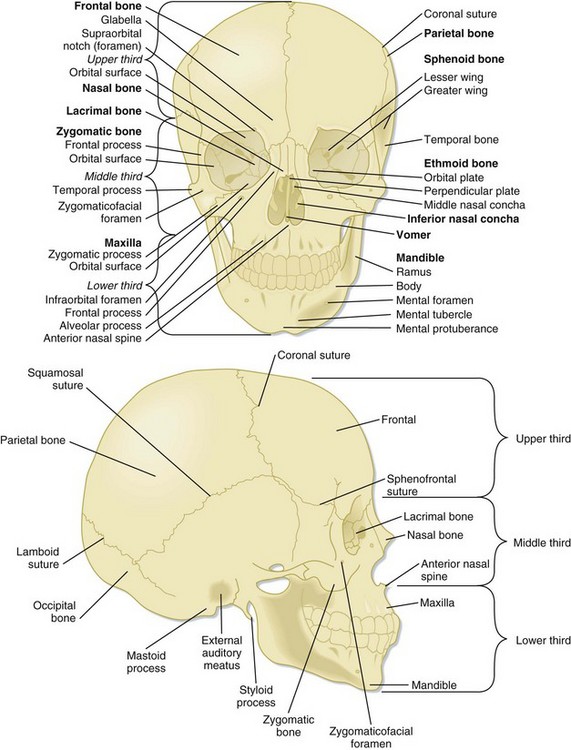
The major bones of the face create the defining features and include the frontal, nasal, zygoma, maxilla, mandible, and temporal bones. The orbit consists of the maxilla, zygoma, frontal, sphenoid, orbital, and lacrimal bones (Fig. 76.1).
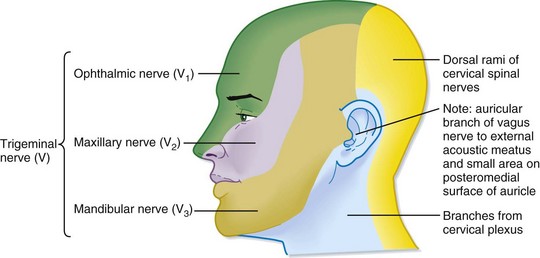
The face is conventionally divided into thirds: upper, middle, and lower. The borders of each third are loosely defined by branches of the trigeminal nerve, which provides sensory innervation to the face. Identification of the exiting foramen for the distributing branches of the trigeminal nerve (cranial nerve V) is crucial when providing local nerve anesthesia (Fig. 76.2).
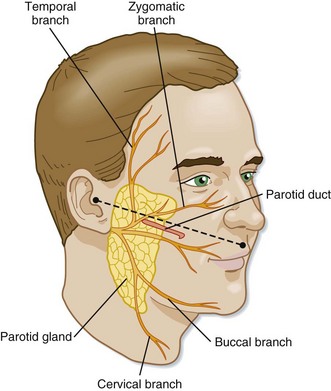
The parotid duct lies in a plane with the tragus and inferior corner of the nasal vestibule. Competency of the parotid duct must be considered in patients with deep lacerations in this region of the face (Fig. 76.3).9
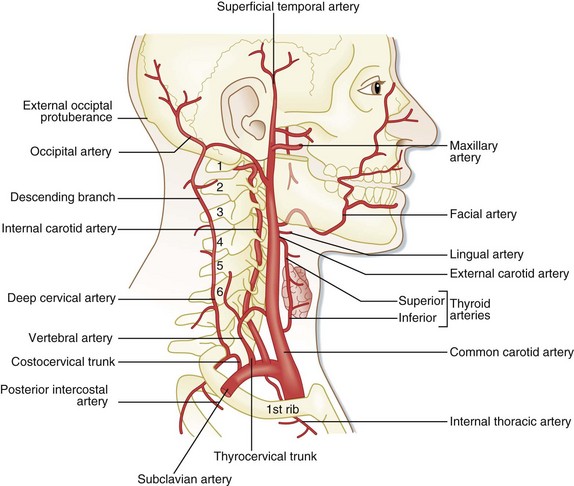
The external carotid artery is the major vascular supply to the face. This vessel provides extensive collateral supply to the midline tissues through anastomosis (Fig. 76.4).10
Approach to Multitrauma Patients with Facial Injuries
The degree of tissue distortion following facial trauma should not dissuade the EP from addressing the initial treatment priorities in patients. Though uncommon, facial trauma can be a life-threatening insult, and the EP must address life-threatening injuries before evaluating the obvious facial injury. The mere presence of a facial fracture, particularly one involving the midface, greatly increases the risk for traumatic brain injury.11,12 The energy required to fracture the midface is often transmitted to the neurocranium, and such fractures are associated with a high incidence of brain death. In general, patients with facial fractures who do not survive have higher injury severity scores and lower Glasgow Coma Scale scores and consist of an older population. Other typical concomitant injuries include pulmonary contusions, abdominal injuries, and cervical spine injuries.13 The emergence of motor vehicle air bags has decreased patient mortality. However, increased concern is warranted for injuries to the orbits, globes, facial soft tissues, and temporomandibular joints, as well as cervical fractures of the posterior arches of C1 and C2.
Treatment of bleeding must begin with inspection of the airway and maintenance of its patency. Local hemorrhage may be controlled with posterior nasal packing or insertion of a Foley catheter into the nasopharynx and inflation with air. The catheter should be gently pulled anteriorly in an attempt to close the posterior choana. Temporary external reduction of fractures may also provide stabilization of arterial injuries. Finally, surgical ligation of the external carotid artery or transcatheter arterial embolization of the maxillary artery can be performed to effect hemostasis.14 Less obvious sources of serious blood loss must be monitored (scalp lacerations, nasal fractures, mandibular fractures) because persistent bleeding may lead to hypovolemia.15
Frontal Skull Injuries
Treatment
Frontal sinus fractures are usually diagnosed by computed tomography (CT). Displaced anterior wall fractures require either immediate repair or delayed reconstruction. Conversely, frontal bone fractures that involve the posterior wall of the sinus are associated with cerebrospinal fluid (CSF) rhinorrhea; the patient will require urgent consultation with a neurosurgeon and admission to the hospital.16 Ocular trauma or sudden loss of vision associated with a frontal bone injury requires immediate ophthalmologic consultation.
Blunt Ophthalmic and Orbital Trauma
Pathophysiology
Trauma to the eye can result from falls, motor vehicle accidents, and direct blows from an assault or a projectile object (hockey puck, baseball). Serious eye injury has been shown to most commonly be associated with midface fractures.17,18 Ocular trauma can be divided into two broad categories: direct trauma to the globe and trauma to the orbit. Direct globe trauma ranges in severity from a benign corneal abrasion to rupture of the globe. Orbital trauma involves injuries such as benign contusions and fractures with complications to surrounding structures, including the globe and extraocular muscles.
Orbital fractures are classified as “impure” when the fracture line involves the orbital rim or as “pure” in the case of a fracture with no rim involvement. Compression of the optic nerve (ocular neuropathy) can be caused by displacement of a fracture, increased pressure from a retrobulbar hemorrhage, or optic nerve hemorrhage.19 Each of these processes has the potential to lead to rapidly progressive visual loss and is an ophthalmologic emergency.
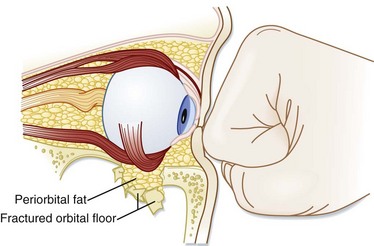
The mechanism of orbital blowout fractures was investigated by Waterhouse et al. via the same principles as Le Fort a century earlier (see later).20 Waterhouse investigated the two possible mechanisms for an orbital blowout fracture, the hydraulic and buckling theories. The hydraulic mechanism occurs when the vector of the force directed onto an uninjured globe is transmitted to the fixed orbital walls; it results in a large fracture of the inferior or medial orbital wall, or both (Fig. 76.5). This mechanism is commonly associated with herniation of the orbital contents through the fractured orbital wall, hence the term blowout. The buckling mechanism, in contrast, occurs when a traumatic force is directed to the inferior orbital rim and causes only the inferior floor of the orbit to buckle, or fracture, with no associated herniation of the orbital contents.
Presenting Signs and Symptoms
Key points in the patient’s history include the following:
• Binocular diplopia (blurring of vision when both eyes are open) is indicative of an ocular muscle imbalance between the two eyes as a consequence of muscle entrapment, contusion, or displacement of the globe secondary to edema from surrounding structures.
• Monocular diplopia (blurring of vision when only one eye is open) is often indicative of lens dislocation, hyphema, or partial globe rupture.
• Flashing lights, or floaters, can be consistent with a retinal tear, retinal detachment, or vitreous hemorrhage.
• Any loss of perception of light or identification of colors or the presence of central scotomata without association with pain is indicative of optic neuropathy. Absence of light perception following an orbital fracture is a poor prognostic indicator for recovery of vision.
• Rapid loss of vision in one eye associated with edema, proptosis, and tension on palpation should heighten suspicion for the presence of a retrobulbar hematoma.
• Pain with eye movement is commonly associated with an orbital fracture.
Treatment
Management of blowout fractures is complicated.21 The presence of an orbital fracture with findings of herniation on clinical or radiographic examination requires immediate surgical consultation to guide the treatment plan. Immediate indications for surgical intervention include muscular entrapment with gaze restriction or acute enophthalmos. Contraindications to surgery include globe rupture, hyphema, and retinal tears. These injuries should prompt emergency ophthalmologic consultation. An ophthalmologist should also be contacted for patients with evidence of lens dislocation, laceration of the cornea or sclera, or rapid loss of visual acuity.
Zygoma Injury
Pathophysiology
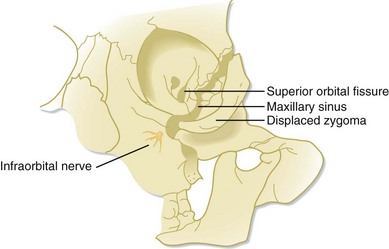
Zygoma fractures are the result of an anterolateral force applied to the midface by falls, deceleration injuries, or assault by blunt objects, including a fist. The zygoma is a thick bone. A direct blow to the zygoma may not necessarily result in a fracture but instead may transmit the force to adjacent weaker areas of the orbit and maxilla and cause a complex fracture. Inward and downward displacement of the zygoma in relation to its articulating surfaces results in the classic zygomaticomaxillary complex fracture, also called a tripod or malar fracture (Fig. 76.6).22 Comminuted fractures of the zygoma are associated with penetrating trauma, such as gunshot wounds.
Presenting Signs and Symptoms
Common symptoms with fracture of the zygoma include the following:
• Difficulty opening the jaw secondary to the origin of the masseter (trismus)
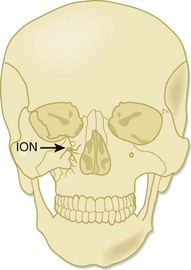
• Paresthesia in the distribution of the inferior orbital nerve (Fig. 76.7)
• Binocular diplopia as a result of entrapment of intraocular muscles
Treatment
Initial management of patients with zygomaticomaxillary complex fractures should include prompt diagnosis and exclusion of ocular muscle entrapment or intracranial injuries. If subcutaneous emphysema is present, antibiotics should be initiated immediately; amoxicillin is an effective first-line agent.23
Maxillary and Midface Injuries
Pathophysiology
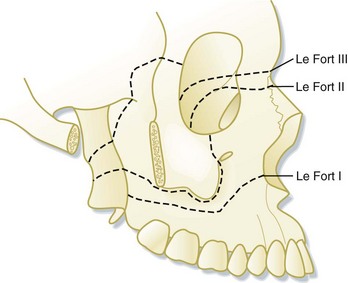
Le Fort Classification
Maxillary fractures resulting from severe blows to the head have traditionally been classified according to the Le Fort classification scheme established by René Le Fort in 1901. Le Fort was a French surgeon who induced trauma in 35 cadaveric heads by striking them with a bat or smashing them against a table edge. Next, Le Fort boiled the heads to remove the soft tissue and documented the fracture lines. In his classic treatise on the subject, Le Fort illustrated three predictable midface fracture lines. These injuries rarely occur in isolation, but they are often used as a reference to describe maxillary trauma (Fig. 76.8).
Presenting Signs and Symptoms
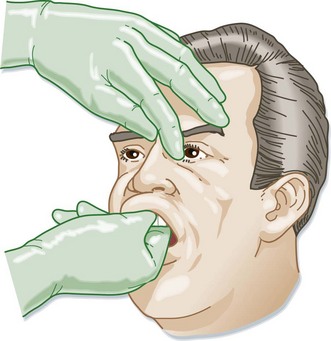
The EP should place one hand on the patient’s forehead to stabilize the head while grasping the upper palate by the anterior teeth with the other hand. Gentle back-and-forth pressure should be applied while palpating the midface for movement (Fig. 76.9). If motion of the midface structures is detected with this technique, further classification of the extent of the injury should be performed by localization of the nasal ridge or inferior orbital rims with the other hand. If CSF rhinorrhea is suspected, testing the fluid for glucose or the halo sign may be undertaken; however, both these assessments have a high false-positive rate and are considered unreliable. If a fracture is highly suspected or if CT is planned, manipulation of the midface offers little benefit and may cause increased bleeding.24
Treatment
If hemostasis of the nares cannot be achieved, a Foley catheter should be carefully advanced into the nasopharynx and inflated with air (overinflation may result in septal necrosis). The catheter should be gently pulled anteriorly in an attempt to close the posterior choana. Once the catheter is in place, the nasal cavity can be packed with gauze or nasal tampons for control of anterior epistaxis. The physician must be careful when advancing any tube through the nares because violation of the anterior cranial base can allow passage of the catheter into the cranium. If bleeding is not controlled with Foley catheters and packing, embolization of bleeding vessels with possible surgical exploration and ligation of vessels should occur. Emergency consultation with ear, nose, and throat (ENT), plastic surgery, and interventional radiology services should be considered early if the patient requires angiography. Regardless of the severity of bleeding, all patients with facial fractures should be reevaluated for hemorrhage every 30 minutes for a period of up to 6 hours.25
Nasal Injuries
Pathophysiology
Nasal bone fractures are commonly the result of sports-related trauma, assault, and motor vehicle crashes. The force required to fracture the nasal bone ranges from 16 to 66 kPa, the least of any facial bone.28 Simple deviated nasal fractures are the result of a lateral force against the nasal prominence. More complex nasoorbitoethmoid fractures are due to a stronger force directed toward the bridge of the nose with displacement of the bone segments posteriorly. This type of fracture is frequently associated with other facial and brain injuries.
Presenting Signs and Symptoms
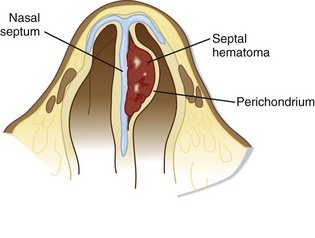
Each naris must be inspected carefully with a nasal speculum to evaluate for a septal hematoma. A sepal hematoma is a collection of blood between the mucoperichondrium or mucoperiosteum of the nasal septum and septal cartilage. A septal hematoma appears as a purple, bulging oval structure on the nasal septum that invades the midline (Fig. 76.10). Failure to promptly identify and treat a septal hematoma can lead to necrosis of the septum and potentially a saddle nose deformity.
Treatment
The EP should not attempt reduction of closed nasal fractures. Given the extensive edema that generally ensues before the patient arrives at the emergency department (ED), the EP will be unable to approximate realignment of the nasal septum.29 Epistaxis should be dealt with during the clinical evaluation. Analgesia should be adequately addressed during the patient’s visit and at follow-up.
Lower Face Injuries
Pathophysiology
The location of mandibular fractures has some correlation to the insult received.30 High-velocity forces directed to the chin result in symphysis or condylar fractures (or both), and a high proportion of these injuries result in comminuted fractures. In contrast, assault-related injuries are more commonly associated with fractures of the angle and ramus. The location of trauma impact does not necessarily correlate with the location of the fracture site because the force of the impact can be transmitted to a distant area.
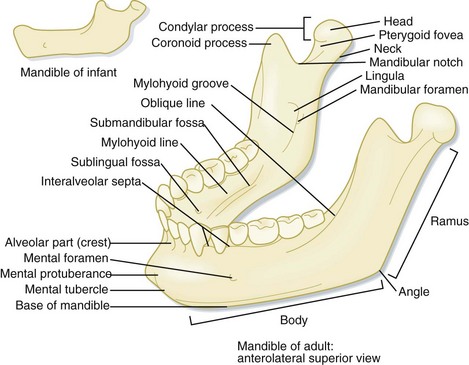
Anatomy
The mandible is a horseshoe-shaped bone and appears similar to the letter L from a lateral view (Fig. 76.11). It has 16 tooth sockets innervated by the inferior alveolar nerve. The mandible articulates with the temporal bone bilaterally via a ginglymoarthrodial (hinge and sliding) joint to form the temporomandibular joint. The arterial supply to the mandible is via branches of the maxillary artery.
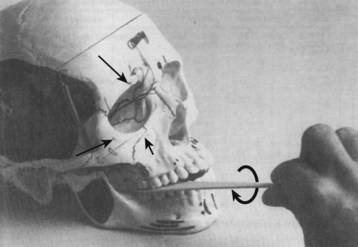
Presenting Signs and Symptoms
If the clinical findings are misleading, one can perform the tongue blade test, which has been demonstrated by Alonso and Purcell to have high sensitivity in screening for mandibular fractures.31 The test is performed by placing a wooden tongue blade between the molars (Fig. 76.12). The patient is instructed to bite down, and the examiner exerts a twisting motion in an effort to crack the wooden blade between the patient’s teeth. If the EP is unable to crack the blade between the patient’s teeth during the twisting motion—because of pain or malocclusion—a positive test is confirmed with subsequent enhanced suspicion for a mandibular fracture.
Follow-up, next Steps in Care, and Patient Education
![]() Priority Actions
Priority Actions
Suspicious mechanism of injury? Is the patient being physically abused? Unwitnessed head, neck, and facial injuries, particularly in women, should raise concern for interpersonal violence.
Typical concomitant injuries in a patient with facial trauma include contusions, intracranial pathology, and abdominal and cervical spine injuries.
Is the patient experiencing sudden loss of vision or eye pain? Increased retrobulbar pressure from a hematoma or emphysema can lead to acute and permanent loss of vision.
Pain with eye movement? Does the patient have muscle entrapment?
Loss of sensation in the nerve distribution?
Does the patient have malocclusion? Consider a mandibular or maxillary fracture.
Lacerations through the vermilion border require extra attention to detail with surgical closure. Slight misalignment at the time of wound closure may result in substantial cosmetic implications.
Competency of the parotid duct must be considered with all deep cheek lacerations.
Do not attempt to realign a fractured nose in the emergency department.
Does the patient have a septal hematoma?
Tips and Tricks
Identification of the exiting foramen for the distributing branches of the trigeminal nerve is crucial when providing regional anesthesia.
Severe epistaxis may be controlled with a Foley catheter advanced into the nasopharynx, inflated, and retracted against the nasopharynx as a posterior nasal pack.
Upward gaze palsy with vertical diplopia is consistent with dysfunction or entrapment of the inferior rectus muscle and suggestive of an orbital blowout fracture.
Pain with eye movement is indicative of an orbital fracture.
Intraoral examination of the zygoma is accomplished by placing a gloved finger along the superior and lateral aspect of the maxillary molars.
Any palpation of subcutaneous air in the face is indicative of sinus disruption with a midface fracture
Antibiotic prophylaxis for basilar skull fractures has not been shown to decrease the risk for meningitis.
Treatment of eyebrow lacerations does not require shaving the brow hairs. Additionally, sutures should be placed parallel to the hair follicles.
Dean NR, Ledgard JP, Katsaros J. Massive hemorrhage in facial fracture patients: definition, incidence, and management. Plast Reconstr Surg. 2009;123:680–690.
Howes DS, Dowling PJ. Oral facial emergencies: triage and initial evaluation of the oral facial emergency. Emerg Med Clin North Am. 2000;18:371–378.
Parry M. Maxillofacial trauma—developments, innovations, and controversies. Injury. 2009;40:1252–1259.
1 Bisson JI, Shepherd JP, Dhutia M. Psychological sequelae of facial trauma. J Trauma. 1997;43:496–500.
2 Wu V, Huff H, Bhandari M. Pattern of physical injury associated with intimate partner violence in women presenting to the emergency department: a systematic review and meta-analysis. Trauma Violence Abuse. 2010;11:71–82.
3 Shepherd SM, Lippe MS. Maxillofacial trauma: evaluation and management by the emergency physician. Emerg Med Clin North Am. 1987;5:371–392.
4 Alvi A, Doherty T, Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003;113:102–106.
5 Kraus JF, Rice TM, Peek-Asa C, et al. Facial trauma and the risk of intracranial injury in motorcycle riders. Ann Emerg Med. 2003;41:18–26.
6 Nakhgevany KB, LiBassi M, Esposito B. Facial trauma in motor vehicle accidents: etiologic factors. Am J Emerg Med. 1994;12:160–163.
7 Plaisier BR, Punjabi AP, Super DM, et al. The relationship between facial fractures and death from neurologic injury. J Oral Maxillofac Surg. 2000;58:708–712.
8 Parry M. Maxillofacial trauma—developments, innovations, and controversies. Injury. 2009;40:1252–1259.
9 Hallock GG. Microsurgical repair of the parotid duct. Microsurgery. 1992;13:243–246.
10 Kerwin AJ, Bynoe RP, Murray AJ, et al. Liberalized screening for blunt carotid and vertebral artery injuries is justified. J Trauma. 2001;51:308–314.
11 Ardekian L, Rosen D, Klein Y, et al. Life-threatening complications and irreversible damage following maxillofacial trauma. Injury. 1998;29:253–256.
12 Howes DS, Dowling PJ. Oral facial emergencies: triage and initial evaluation of the oral facial emergency. Emerg Med Clin North Am. 2000;18:371–378.
13 Hackl W, Fink C, Hausberger K, et al. The incidence of combined facial and cervical spine injuries. J Trauma. 2001;50:41–45.
14 Bynoe RP, Kerwin AJ, Parker HH, 3rd., et al. Maxillofacial injuries and life-threatening hemorrhage: treatment with transcatheter arterial embolization. J Trauma. 2003;55:74–79.
15 Dean NR, Ledgard JP, Katsaros J. Massive hemorrhage in facial fracture patients: definition, incidence, and management. Plast Reconstr Surg. 2009;123:680–690.
16 Lauder A, Jalisi S, Speigel J, et al. Antibiotic prophylaxis in the management of complex midface and frontal sinus trauma. Laryngoscope. 2010;120:1940–1945.
17 Joondeph BC. Blunt ocular trauma. Emerg Med Clin North Am. 1988;6:147–167.
18 Larian B, Wong B, Crumley RL, et al. Facial trauma and ocular/orbital injury. J Craniomaxillofac Trauma. 1999;5:15–24.
19 Wang BH, Robertson BC, Girotto JA, et al. Traumatic optic neuropathy: a review of 61 patients. Plast Reconstr Surg. 2001;107:1655–1664.
20 Waterhouse N, Lyne J, Urdang M, et al. An investigation into the mechanism of orbital blowout fractures. Br J Plast Surg. 1999;52:607–612.
21 Mathog RH. Management of orbital blowout fractures. Otolaryngol Clin North Am. 1991;24:79–91.
22 Zingg M, Laedrach K. Classification and treatment of zygomatic fractures: a review of 1025 cases. J Oral Maxillofac Surg. 1992;50:778–790.
23 Iqbal HA, Chaudhry S. Choice of operative method for management of isolated zygomatic bone fractures; evidence based study. J Pak Med Assoc. 2009;59:615–618.
24 Bagheri SC, Holmgren E, Katemani D, et al. Comparison of the severity of bilateral Le Fort injuries in isolated midface trauma. J Oral Maxillofac Surg. 2005;63:1123–1129.
25 Greene D, Raven R, Carvalho G, et al. Epidemiology of facial injury in blunt assault. Determinants of incidence and outcome in 802 patients. Arch Otolaryngol Head Neck Surg. 1997;123:923–928.
26 Villalobos T, Arango C, Kubilis P, et al. Antibiotic prophylaxis after basilar skull fractures: a meta-analysis. Clin Infect Dis. 1998;27:364–369.
27 Abubaker AO. Use of prophylactic antibiotics in preventing infection of traumatic injuries. Dent Clin North Am. 2009;53:707–715.
28 Holt GR. Biomechanics of nasal septal trauma. Otolaryngol Clin North Am. 1999;32:615–619.
29 Mondin V, Rinaldo A, Ferlito A. Management of nasal bone fractures. Am J Otolaryngol. 2005;26:181–185.
30 Tessier P. The classic reprint: experimental study of fractures of the upper jaw. 3. René Le Fort, M.D., Lille, France. Plast Reconstr Surg. 1972;50:600–607.
31 Alonso LL, Purcell TB. Accuracy of the tongue blade test in patients with suspected mandibular fracture. J Emerg Med. 1995;13:297–304.