Chapter 12 Facet (Zygapophyseal) Intraarticular Joint Injections
Cervical, Lumbar, and Thoracic
 Facet arthropathy is a significant contributor to spinal pain in the cervical, thoracic, and lumbar regions.
Facet arthropathy is a significant contributor to spinal pain in the cervical, thoracic, and lumbar regions. Intraarticular injection or medial branch block with a small volume of local anesthetic play a critical role in establishing the diagnosis because no radiographic modality, historical, or physical exam finding has proven reliable.
Intraarticular injection or medial branch block with a small volume of local anesthetic play a critical role in establishing the diagnosis because no radiographic modality, historical, or physical exam finding has proven reliable. Recent guideline statements suggested dual controlled comparative medial branch blocks with subsequent radiofrequency ablation have better evidence for outcomes, although intrarticular joint injections are more appropriate in patients who are not good candidates for radiofrequency procedures.
Recent guideline statements suggested dual controlled comparative medial branch blocks with subsequent radiofrequency ablation have better evidence for outcomes, although intrarticular joint injections are more appropriate in patients who are not good candidates for radiofrequency procedures. The specificity of diagnostic intraarticular facet injection may be increased by limiting the use of intravenous sedatives or opioids and local anesthetics for anesthesia of the needle tracks.
The specificity of diagnostic intraarticular facet injection may be increased by limiting the use of intravenous sedatives or opioids and local anesthetics for anesthesia of the needle tracks. The volume of intraarticular injection should be limited to 0.5 mL for cervical and thoracic facets and 1 mL for lumbar facets, as the cervical, thoracic, and lumbar facets can accommodate 0.5 to 1 mL, 0.75 mL, and 1.0 to 1.5 mL volume.
The volume of intraarticular injection should be limited to 0.5 mL for cervical and thoracic facets and 1 mL for lumbar facets, as the cervical, thoracic, and lumbar facets can accommodate 0.5 to 1 mL, 0.75 mL, and 1.0 to 1.5 mL volume. A reduction in concordant pain of >50% is as reliable as a >80% pain reduction in predicting therapeutic outcomes.
A reduction in concordant pain of >50% is as reliable as a >80% pain reduction in predicting therapeutic outcomes. When a steroid is used in the cervical region for therapeutic purpose, a nonparticulate injectate is recommended to avoid vascular embolization.
When a steroid is used in the cervical region for therapeutic purpose, a nonparticulate injectate is recommended to avoid vascular embolization. Lateral approach for cervical facet injection in decubitus position is easier to perform and better tolerated by patients. However, caution should be exercised to avoid parallax of fluoroscopy images at the level of injection in order to focus on the appropriate side of injection.
Lateral approach for cervical facet injection in decubitus position is easier to perform and better tolerated by patients. However, caution should be exercised to avoid parallax of fluoroscopy images at the level of injection in order to focus on the appropriate side of injection.Introduction
Spinal pain is extremely common. The incidences of pain in the neck, thoracic, and low back are estimated at 44%, 15%, and 56%, respectively, in the general population.1 Facet arthropathy is an important source of spinal pain, and facet interventions are the second most common procedure performed in the United States by pain physicians, behind epidural steroid injections. This chapter focuses on the intraarticular injections of facet joints between vertebrae C2 through S1 for diagnostic and therapeutic purposes. The injection of the atlanto-axial joint (AAJ) between vertebrae C1-C2 is discussed elsewhere.
Prevalence of Facet Joint Pain
Estimates of lumbar facetogenic pain vary, from 15% of all back pain complaints2 to 59.6% males and 66.7% females in the community based on a population study.3 The prevalence of lumbar facetogenic pain, determined by placebo-controlled diagnostic blocks using a criterion of 90% pain reduction, ranges from 27% to 40% in patients with axial low back pain.4,5 Sedation may increase false-positive rates of diagnostic blocks by 10%, but psychological comorbidity has not been shown to affect the diagnostic accuracy. Aging is positively related to the prevalence of lumbar facet arthropathy, with an occurrence of 89% in individuals 60 to 69 years old. The most common level is at L4-L5.2
The prevalence of thoracic facet pain ranges between 33% and 48% with a 95% confidence interval based on responses to comparative controlled diagnostic blocks.6 The prevalence of cervical facet pain is 30% to 70% of cases7–9 and is not significantly affected by prior surgery, psychopathology, or age. The most commonly affected facet is C4-C5 (14.62%) followed by C3-C4, C2-C3, C5-C6, and C6-C7, respectively.10 There is no proven correlation between clinical manifestation of facetogenic pain and facet arthrosis shown by imaging studies or cadaveric observations. Diagnostic block remains the best available tool to identify facetogenic pain despite its high false-positive rates (39% to 53%).
Establishing Diagnosis
Numerous studies have attempted to determine the historical, or physical, and radiographic findings that correlate with pain associated with facet arthropathy. None has been proven specific, sensitive, and reliable.2 Consequently, diagnosis is primarily based on pain reduction and mobility improvement in response to controlled diagnostic facet blocks.4,6,11 The diagnosis of facetogenic pain is suggested by controlled comparative (lidocaine/bupivacaine) medial branch blocks. A criterion of 80% pain reduction and the ability to perform maneuvers that were painful before the diagnostic intervention are commonly used. However, a recent study suggests that using 50% pain reduction as a criterion for positive diagnostic block is just as effective as using 80% pain reduction in predicting the outcomes of medial branch radiofrequency ablation.12
Even though facetogenic pain is primarily determined by diagnostic blocks, clinical findings from history and physical examinations usually help physicians decide if diagnostic facet blocks are warranted. For example, pain from the AAJ is typically provoked by head rotation with the neck slightly flexed forward. This information may lead to an AAJ block rather than a cervical facet block. Therefore, taking the patient history and performing a physical examination is still an indispensable step in establishing a diagnosis of facet pain. Pain referral patterns for cervical and thoracic facet pain have been generated,2,13–15 as shown in Fig. 12-1.
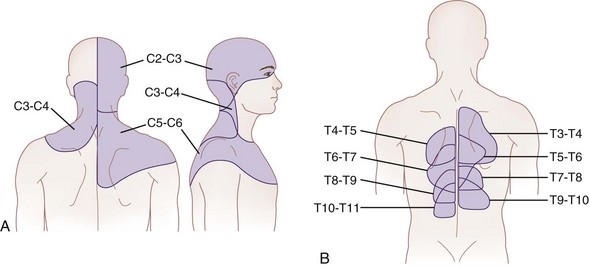
Fig. 12-1 Maps of referred pain from the cervical (A) and thoracic (B) facets.
(Part A adapted from Bogduk N, Marland A: The cervical zygapophysial joints as a source of neck pain, Spine 13:610-617, 1988; part B adapted from Dreyfuss P, Tibiletti C, Dreyer SJ: Thoracic zygapophyseal joint pain patterns: a study in normal volunteers, Spine 19:807-811, 1994.)
Cervical Facet Pain
Restricted range of motion is not pathognomonic for facet pain and can present in a variety of neck disorders, such as whiplash injury. Point tenderness was recently evaluated in 33 patients by assessing pain pressure thresholds in symptomatic and asymptomatic facets joints.16 Although the pain pressure thresholds are significantly lower in patients with neck pain, this approach is not diagnostic for cervical facet joint pain. Neck point tenderness can be indicative of myofascial pain or associated with tension headache.17 No provocative tests tend to produce pain in the referral patterns. As a general rule, the upper facet joints may cause headache, and the lower joints may have pain referred to the shoulder in a nondermatomal distribution. Cervical radicular pain is usually absent.
Thoracic Facet Pain
Pain from thoracic facet joints may be provoked by facet capsule distention,14 such as extension, lateral bending, and twisting or paraspinal pressure overlying the facet joints. Pain is often nonradicular, and there is no associated weakness.
Lumbar Facet Pain
Lumbar facet joint pain is typically described as back pain with or without nondermatomal leg pain above the knee. Paraspinal tenderness overlying the facets produced by pressure is suggestive.18 Facet pain is typically not confined to a dermatomal distribution (nonradicular). Motor function and reflex assessment are usually intact.
Anatomy of the Facet Joints
The facet joints have rich innervation, including encapsulated, unencapsulated, and free nerve endings.2 These innervations provide nociception through C and A-δ afferents as well as proprioception through low-threshold, rapidly adapting mechanoreceptors.19 Immunocytochemistry of facet joints demonstrated the presence of substance P, calcitonin-gene-related peptide, and neuropeptide Y, suggesting pain transmission and sympathetic fibers.20–22 Facet joint distraction in rats produces spinal astrocyte activation and persistent mechanical allodynia.23 The expression of a binding protein BiP, also known as growth-related protein 78, is upregulated 2.1-fold in the dorsal root ganglion after painful distraction injury to the rat C6-C7 facet, indicating neuronal stress activation.24 Cytokines and neurotrophic factors are upregulated in dorsal root ganglion neurons in models of facet joint inflammation.25–28
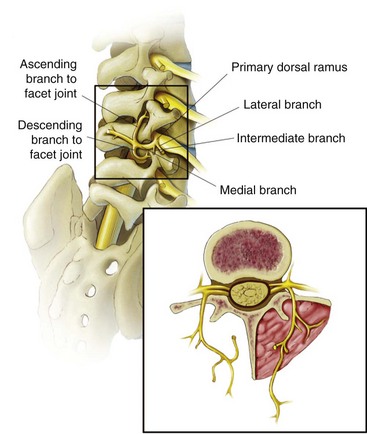
The architecture and orientation of the facet joint vary with function and position along the vertebral column.29–31 The lumbar facet joint can accommodate an average of 1 to 1.5 mL fluid. The joint is C shaped and is encased posteriorly in a fibrous capsule of approximately 1 mm thick composed of collagenous tissue. The lumbar facet joint is supported posteriorly by multifidus muscle, superiorly and inferiorly by fibroadipose menisci forming subcapsular recesses, and anteriorly by the ligamentum flavum.31 The inferior portion of the joint is larger than the superior portion. Any given facet joint has dual innervation from two segmental medial branch nerves: one arising at the given level and one from one segment above as shown in Fig. 12-2. Consequently, a given medial branch nerve innervates two facet joints, the ascending branch to the caudal portion of the facet above and the descending branch to superior portion of the facet below. For example, the L3 medial branch nerve courses along the junction of the superior articular process and the transverse process of L4 under the mamilloaccessory ligament, supplying the caudal portion of the ipsilateral L3-L4 facet joint, and then courses caudally to supply the ipsilateral superior portion of the L4-L5 facet joint. Conversely, the L3-L4 facet has dual innervation from the L2 and L3 medial branches.
Guidelines for Intervention
Randomized controlled trials report equivocal findings regarding the efficacy of facet joint steroid injections compared with facet saline injections regarding pain relief for patients with low back pain (Category C2 evidence). However, studies with observational findings for facet joint injections indicate that pain scores are improved over baseline scores for assessment periods of 1-6 months (Category B2 evidence). … Intraarticular facet joint injections may be used for symptomatic relief of facet-mediated pain.32
In addition, a recent prospective study tested intraarticular injection of hylan G-F 20 in patients with painful lumbar facet joint arthropathy and reported significant improvement in pain scores, quality of life, and opioid consumption for 6 months.33 Studies of injecting nonsteroid agents may represent a new direction of intraarticular facet therapy.
The American Society of Interventional Pain Physicians did not recommend intraarticular injections for either diagnostic or therapeutic benefit.34 The International Spine Intervention Society described guidelines for thoracic intraarticular facet joint blocks as an emerging procedure and did not comment on intraarticular lumbar or cervical facet joint blocks.35 Both guidelines suggest better evidence (level I or II) with medial branch blocks for diagnosis and radiofrequency ablation for therapeutic benefit after two positive comparative controlled diagnostic blocks using 80% pain reduction. However, for patients who are not ideal candidates for radiofrequency ablation, such as those with pacemakers, intraarticular facet block with a mixture of local anesthetic and steroid is a viable option.
Indications and Contraindications
Facet interventions are indicated in patients with moderate to severe spinal pain that is somatic and nonradicular (or headache), lasts longer than 3 months in duration, with functional limitation or impairment; failure of more conservative therapies (exercise, physical therapy, simple analgesics); and lack of evidence supporting primarily a discogenic, myofascial, or radicular pain source. Importantly, the patient should have the ability to undergo physical therapy after the intervention.34,35
Contraindications include anything that would preclude neuraxial procedures, such as lack of informed consent; hemodynamic instability; coagulopathy or thrombocytopenia; pregnancy; infection overlying the puncture site; inability to see target site secondary to hardware; inability of the patient to lie in the procedure position; or allergy to contrast, steroids, local anesthetics, and so on. Readers are referred to American Society of Regional Anesthesia and Pain Medicine guidelines for regional anesthesia and anticoagulation.36
Equipment
Anesthesia monitors for ECG, pulse oximetry, and blood pressure
22- or 25-gauge 3.5-inch spinal needle
26-gauge 1-inch needle for subcutaneous infiltration
1% lidocaine for subcutaneous infiltration (methylparaben free)
0.5% bupivacaine (methylparaben free)
Triamcinolone 40 mg or dexamethasone 7.5 mg
Low osmolar nonionic contrast media or iso-osmolar nonionic contrast media 3 mL
Three sterile Luer lock 3-mL syringes
Betadine, alcohol, or Hibiclens prep
Sterile drape or sterile towels
Lead apron, thyroid shield, lead glasses
Techniques for Facet Joint Injection
Cervical Facet
Lateral Approach
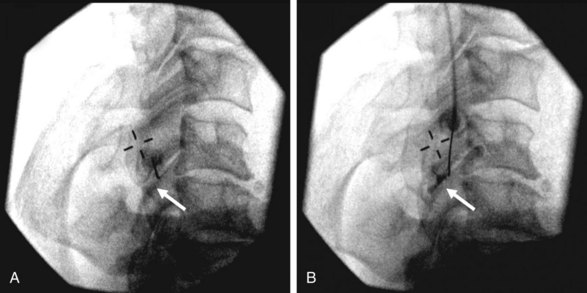
The patient is self-positioned in the lateral decubitus position with the symptomatic side up. The head is placed in the neutral position or slightly extended to the contralateral side (supporting side) to facilitate needle placement. The site is prepped and draped in sterile fashion. The articular pillars and vertebral endplates are aligned under lateral view of fluoroscopy so there is no parallax at the level of the injection site. After the targeted facet has been identified, a radiopaque marker is placed on the skin to localize the entry point, where 1 mL of 1% lidocaine is injected and a 25-gauge 3.5-inch spinal needle is advanced in plane coaxial approach to contact the targeted facet joint under intermittent fluoroscopy guidance. Nonionic contrast of 0.1 to 0.2 mL is injected under a “live” fluoroscopic view to ensure intraarticular filling without vascular spread as shown in Fig. 12-3 (compare A and B, before and after 0.1 mL contrast injection at the C4-C5 facet as indicated by the arrows). The joint accommodates between 0.5 to 1 mL of volume. After proper needle position has been confirmed, 0.5 mL of local anesthetic is injected for diagnostic purposes or a combination of 0.5 mL of local anesthetic and steroid is injected for therapeutic purposes. The needle is then slowly removed, the skin is cleaned, and a bandage is applied, and the patient is transported to the postblock recovery area. It is noteworthy that a true lateral view is critically important to avoid inadvertent entry of the needle into the spinal canal. Also, the needle should first contact the articular pillar of the targeted facet joint and then walk off the pillar to enter the joint to avoid overshoot of the needle into the spinal canal.
Lumbar Facet
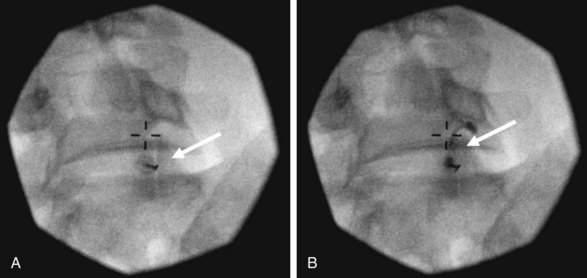
The patient is self-positioned prone. The skin is prepped and draped in sterile fashion. The targeted facet is identified with fluoroscopy, and the C-arm is rotated ipsilateral oblique (25 to 35 degrees) to “open” the facet joint (Fig. 12-4). Sometimes a caudocranial angulation of the C-arm (image intensifier toward the head) is required to better visualize the joint space in between the superior and inferior articular processes. The needle is advanced in a coaxial manner with intermittent fluoroscopy to enter in caudal pole of the facet joint. The lumbar facet joint accommodates 1 to 1.5 mL of volume. After the needle has been engaged, 0.1 mL of contrast may be injected, confirming intraarticular spread as shown in Fig. 12-4 (compare A and B, before and after contrast injection at the L5-S1 facet as indicated by the arrows). After proper needle position has been confirmed, for diagnostic purposes, 0.5 mL of local anesthetic is injected; for therapeutic purposes, a combination of 0.5 to 1 mL of local anesthetic and steroid is injected. The needle is then slowly removed, a bandage is applied, and the patient is transported to the postblock recovery area.
Outcomes Evidence
There was limited evidence supporting intraarticular anesthetic or steroid injection for diagnostic or therapeutic purposes.5,6,11 Nevertheless, intraarticular injection can be used in patients who are not ideal candidates for radiofrequency ablation of the facet medial branches, such as those with pacemakers. Furthermore, lumbar facet intraarticular injection of hylan G-F 20 appears effective in pain reduction, improving quality of life, and reducing opioid consumption for 6 months.33
Risk and Complication Avoidance
Facet joint injection is generally considered to be a very safe procedure. However, significant complications have been reported, including spinal cord injury associated with cervical facet injection and pneumothorax associated with thoracic facet injections.37 Vascular injection of local anesthetics or steroids is a concern associated with spinal procedures. The radicular arteries are the main source of blood to the spinal cord and usually enter the spinal canal in the cervical region through the neuroforamen accompanying the C4-C6 nerve roots.38 Pneumothorax is a concern for any paraspinal thoracic procedure. Other complications reported after facet injections include spondylodiscitis, meningitis and chemical meningism, septic arthritis, and epidural abscess.37 Postdural puncture headache has also been reported.39 The effect on the hypothalamic–pituitary–adrenal axis is likely similar to that of epidural steroid injections.40
Many of these complications may be prevented by observing strict aseptic techniques and by performing the procedures with clear understanding of the anatomy and the techniques. Adequate monitoring, early detection, aggressive treatment, and accurate documentation are required when complications do occur to minimize the adverse outcomes.37
1 Linton SJ, Hellsing AL, Hallden K. A population based study of spinal pain among 35-45-year-old individuals. Spine. 1998;23:1457-1463.
2 Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106:591-614.
3 Kalichman L, Li L, Kim DH, et al. Facet joint osteoarthritis and low back pain in the community-based population. Spine. 2008;33:2560-2565.
4 Datta S, Lee M, Falco FJ, et al. Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions. Pain Physician. 2009;12:437-460.
5 Schwarzer AC, Wang S, Bogduk N, et al. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995;54:100-106.
6 Alturi S, Datta S, Falco FJE, Lee M. Systematic review of diagnostic utility and therapeutic effectiveness of thoracic facet joint interventions. Pain Physician. 2008;11:611-629.
7 Manchikanti L, Manchikanti KN, Pampati V, et al. The prevalence of facet-joint-related chronic neck pain in postsurgical and nonpostsurgical patients: a comparative evaluation. Pain Pract. 2008;8:5-10.
8 Lord SM, Barnsley L, Wallis BJ, Bogduk N. Chronic zygapophysial joint pain after whiplash: A placebo-controlled prevalence study. Spine. 1996;21:1737-1744.
9 Manchukonda R, Manchikanti KN, Cash KA, et al. Facet joint pain in chronic spinal pain: An evaluation of prevalence and false-positive rate of diagnostic blocks. J Spinal Disord Tech. 2007;20:539-545.
10 Lee MJ, Riew KD. The prevalence cervical facet arthrosis: an osseous study in a cadaveric population. Spine J. 2009;9:711-714.
11 Falco FJ, Erhart S, Wargo BW, et al. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician. 2009;12:323-344.
12 Cohen SP, Stojanovic MP, Crooks M, et al. Lumbar zygapophysial (facet) joint radiofrequency denervation success as a function of pain relief during diagnostic medial branch blocks: a multicenter analysis. Spine J. 2008;8:498-504.
13 Bogduk N, Marsland A. The cervical zygapophysial joints as a source of neck pain. Spine. 1988;13:610-617.
14 Dreyfuss P, Tibiletti C, Dreyer SJ. Thoracic zygapophyseal joint pain patterns: a study in normal volunteers. Spine. 1994;19:807-811.
15 Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns: a study in normal volunteers. Spine. 1990;15:453-457.
16 Siegenthaler A, Eichenberger U, Schmidlin K, et al. What does local tenderness say about the origin of pain? An investigation of cervical zygapophysial joint pain. Anesth Analg. 2010;110:923-927.
17 Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(suppl 1):9-160.
18 Cohen SP, Hurley RW, Christo PJ, et al. Clinical predictors of success and failure for lumbar facet radiofrequency denervation. Clin J Pain. 2007;23:45-52.
19 Cavanaugh JM, Ozaktay AC, Yamashita HT, King AI. Lumbar facet pain: biomechanics, neuroanatomy and neurophysiology. J Biomech. 1996;29:1117-1119.
20 Ashton IK, Ashton BA, Gibson SJ, et al. Morphological basis for back pain: the demonstration of nerve fibers and neuropeptides in the lumbar facet joint capsule but not in the ligamentum flavum. J Orthop Res. 1992;10:72-78.
21 Bucknill AT, Coward K, Plumpton C, et al. Nerve fibers in lumbar spine structures and injured spinal roots express the sensory neuron-specific sodium channels SNS/PN3 and NaN/SNS2. Spine. 2002;27:135-140.
22 Miyagi M, Ohtori S, Ishikawa T, et al. Up-regulation of TNF alpha in DRG satellite cells following lumbar facet joint injury in rats. Eur Spine J. 2006;15:953-958.
23 Dong L, Odeleye A, Jordan-Sciutto KL, Winkelstein BA. Painful facet injury induces neuronal stress activation in the DRG: Implications for cellular mechanism of pain. Neurosci Lett. 2008;443:90-94.
24 Fukui S, Ohseto K, Shiotani M. Patterns of pain induced by distending the thoracic zygapophyseal joints. Reg Anesth. 1997;22:332-336.
25 Cavanaugh JM, Lu Y, Chen C, Kallakuri S. Pain generation in lumbar and cervical facet joints. J Bone Joint Surg Am. 2006;88:63-67.
26 Ohtori S, Takahashi K, Chiba T, et al. Sensory innervation of the cervical facet joints in rats. Spine. 2001;26:147-150.
27 Cavanaugh JM, Ozaktay AC, Yamashita HT, King AI. Lumbar facet pain: biomechanics, neuroanatomy and neurophysiology. J Biomech. 1996;29:1117-1129.
28 Masharawi Y, Rothschild B, Dar G, et al. Facet orientation in the thoracolumbar spine: Three dimensional anatomic and biochemical analysis. Spine. 2004;29:1755-1763.
29 Punjabi MM, Oxland T, Takata K, et al. Articular facets of the human spine. Quantitative three-dimensional anatomy. Spine. 1993;18:1298-1310.
30 Rathmell JP. Atlas of image-guided intervention in regional anesthesia and pain medicine. Philadelphia: Lippincott; 2006.
31 Bogduk N. Clinical anatomy of the lumbar spine and sacrum, ed 3. Edinburgh: Churchill Livingstone; 1997. pp 33-42
32 Practice guidelines for chronic pain management. an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;112:810-833.
33 DePalma MJ, Ketchum JM, Queler ED, Trussell BS. Prospective pilot study of painful lumbar facet joint arthropathy after intra-articular injection of hylan G-F 20. PM R. 2009;1:908-915.
34 Manchikanti L, Boswell MV, Singh V, et al. comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12:699-802.
35 Bogduk N. International Spine Intervention Society: Practice guidelines: spinal diagnostics and treatment procedures. Kentfield, CA: Standards Committee of the International Spine Intervention Society; 2004.
36 Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: ASRA evidence-based guidelines (third edition). Reg Anesth Pain Med. 2010;35:64-101.
37 Cheng J, Abdi S. Complications of joint, tendon and muscle injections. Tech Reg Anesth Pain Manag. 2007;11:141-147.
38 Chakravorty BG. Arterial supply of the cervical spinal cord (with special reference to the radicular arteries). Anat Rec. 1970;170:311-329.
39 Cohen SP. Postdural puncture headache and treatment following successful lumbar facet block. Pain Digest. 1994;4:283-284.
40 Kay J, Findling JW, Raff H. Epidural triamcinolone suppresses the pituitary-adrenal axis in human subjects. Anesth Analg. 1994;79:501-505.