Face and neck
11.1
Orbital mass lesions
Lesions involving the globe
1. Retinoblastoma – usually presents with white pupil; 20–40% bilateral, 10% have family history; four main subgroups:
(c) Chromosomal – associated with partial deletion of chromosome 13.
(d) ‘Trilateral’ retinoblastoma – bilateral retinoblastoma with pineal tumour.
90% show (various patterns of) calcification.
2. Melanoma – increased incidence from middle age; avidly enhances; may be high signal on precontrast T1 if melanotic.
Intraconal lesions
Conal lesions
2. Thyroid eye disease – enlargement of muscles; swelling of intraorbital fat.
3. Rhabdomyosarcoma – 10% arise in orbit, 50% < 7 years of age; rapid-onset proptosis with deviation of globe; although arises in muscle most of tumour usually extraconal; differentiation between orbital and extraorbital (parameningeal) origin important as treatment differs.
Extraconal lesions
1. Orbital cellulitis and abscess – coronal sections with contrast most sensitive, especially for small subperiosteal collections; secondary to paranasal sinus infection.
4. Dermoid – commonest at external angle.
5. Lymphangioma/lymphaemangioma.
6. Direct extension of lacrimal gland tumour.
7. Langerhans’ cell histiocytosis.
11.2
Optic nerve glioma versus optic nerve sheath meningioma – clinical and radiological differentiation
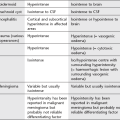
| Glioma | Meningioma |
| 50% < 5 years of age | Usually middle-aged women |
| ± Bilateral | Usually unilateral |
| Slowly progressive, painless loss of vision; central scotoma Childhood tumours may remain quiescent for years, particularly in the presence of NF Adult tumours more aggressive |
Slowly progressive, painless loss of vision; proptosis |
| Neurofibromatosis*: NF-1 in 25%; 15% of NF-1 have optic nerve glioma; bilateral disease strongly suggests neurofibromatosis | Neurofibromatosis (1 or 2) in 4–6%; bilateral disease may occur with or without NF |
| No orbital hyperostosis | Hyperostosis |
| Widened optic canal in 90% but intracranial extension is unusual | Widened optical canal in 10% |
| Kinking and buckling of the optic nerve is common. Smooth outline | Straight optic nerve, but tumour may be eccentric |
| Well-defined margins | More infiltrative Localized or fusiform thickening |
| Calcification rare without prior radiotherapy | Calcification (linear, plaque-like or granular) more common |
| Isointense to brain on T1W MRI; hyperintense on T2W MRI | Similar signal to optic nerve on most unenhanced MR pulse sequences |
| Variable contrast enhancement with mottled lucencies due to mucinous degeneration | Diffuse homogeneous enhancement ± serrated margins |
| Negative image of optic nerve within the tumour (tram-track sign) |
11.5
Enlarged optic foramen
Normal range = 4.4–6 mm; ≥ 7 mm, or greater than 1 mm difference with asymptomatic side = abnormal.
11.6
Enlarged superior orbital fissure
11.8
Orbital hyperostosis
Chung, E. M., Smirniotopoulos, J. G., Specht, C. S., et al. From the archives of the AFIP: Pediatric orbit tumors and tumorlike lesions: nonosseous lesions of the extraocular orbit. Radiographics. 2007; 27(6):1777–1799.
Chung, E. M., Specht, C. S., Schroeder, J. W. From the archives of the AFIP: Pediatric orbit tumors and tumorlike lesions: neuroepithelial lesions of the ocular globe and optic nerve. Radiographics. 2007; 27(4):1159–1186.
11.11
Mass in maxillary antrum
(a) Mucous retention cyst – often arises from floor.
(b) Dentigerous cyst – expands up into floor of antrum; displaced tooth may be seen in antrum.
2. Trauma – herniation of orbital muscle through fracture.
4. Wegener’s granulomatosis – usually presents in 40–50-year-olds; mucosal thickening progresses to formation of soft-tissue mass with extensive bony destruction.
Dym, R. J., Masris, D., Shifteh, K. Imaging of the paranasal sinuses. Oral Maxillofac Surg Clin North Am. 2012; 24(2):175–189.
Kantarci, M., Karasen, R. M., Alper, F., et al. Remarkable anatomic variations in paranasal sinus region and their clinical importance. Eur J Radiol. 2004; 50(3):296–302.
Madani, G., Beale, T. J., Lund, V. J. Imaging of sinonasal tumors. Semin Ultrasound CT MR. 2009; 30(1):25–38.
11.12
Cystic lesions in the mandible/maxilla
Non-dental
2. Hyperparathyroidism – brown tumours.
3. Ameloblastoma – commonest in mandible (80%), usually near angle; slow-growing painless mass; well-defined unilocular or multilocular expansile mass. May extend through cortex.
4. Langerhans’ cell histiocytosis.
10. Bone cyst – may be post-traumatic; unilocular asymptomatic cyst; indistinct borders.
11.15
Nasopharyngeal mass
11.16
Prevertebral soft-tissue mass in an adult on lateral cervical X-ray
Friedman, E. R., John, S. D. Imaging of pediatric neck masses. Radiol Clin North Am. 2011; 49(4):617–632.
Ibrahim, M., Hammoud, K., Maheshwari, M., Pandya, A. Congenital cystic lesions of the head and neck. Neuroimaging Clin N Am. 2011; 21(3):621–639.
Kadom, N., Lee, E. Y. Neck masses in children: current imaging guidelines and imaging findings. Semin Roentgenol. 2012; 47(1):7–20.