1. Evidence-Based Clinical Practice*
Anita Duhl Glicken, M. Douglas. Jones Jr. and Mary Enzman-Hines
Spectacular therapeutic disasters have made it clear that informal let’s-try-it-and-see methods of testing new proposals are risky, now more than ever. Because there are no certainties in medicine and nursing, every clinical test of a new treatment is, by definition, a step into the unknown. Silverman described how painfully slow health care providers were to embrace a culture of skepticism. The use of experimentation and the scientific method has ultimately led to our present views of how to ask and answer clinical questions. 41 Mistakes have also occurred at the other extreme, as well, resulting in a failure to adopt therapies that are of proven benefit or an assumption that the risks associated with changing practice justify complacency about current treatments. It is wrong to assume that traditional clinical practices have been studied in appropriately selected populations of sufficient size to accurately predict their efficacy, benefit, safety, side effects, and cost.
Evidence-based practice (EBP) is a systematic way to improve patient and organization outcomes. EBP stresses that clinical decision making involves the consideration of evidence from multiple sources: systematic research, the clinician’s clinical experience, and the patients being served. 4 Furthermore, EBP presents an opportunity to enhance patient health and illness outcomes, increase staff satisfaction, and reduce health care expenses. Unfortunately, EBP is not easily integrated into existing clinical settings and changes in routine practice are even more difficult to implement. 18 Integrating EBP requires decisions about health care based on the best available, current, valid, and relevant evidence. 18 The current state of science has provided limited rigorous clinical trials to direct change within clinical practice.
QUALITY OF EVIDENCE
As new therapies are integrated into practice, health care providers must continue to increase existing knowledge of the health and health problems of newborns. Providers must learn to overcome impatience with asking specific questions about the quality of evidence regarding risks and benefits of new practices. Clinical questions arise through practice and careful reading of research literature. Evidence-based practice begins with questions that can best be answered by the careful design and conduct of clinical trials.
It is not the purpose of this chapter to provide a detailed review of the various research designs that permit reliable scientific inference. Rather, our purpose is to promote the propositions that (1) challenge clinical observations and wisdom by subjecting them to systematic study and (2) encourage careful assessment and critique of research that supports or challenges the use of new and established clinical practices.
Clinical observations, although valuable in shaping research questions, are limited by selective perception—a desire to see a strategy work or fail to work. At times, a single case or case study may prompt us to question whether we should consider changing current practice. In some situations, much can be learned from carefully maintained databases. However, such knowledge is gained only when we have formed databases with clear intentions and have collected the necessary data.
Sinclair and Bracken43 described four levels of clinical research used to evaluate safety and efficacy, based on their ability to provide an unbiased answer. In ascending order, these are (1) single case or case series reports without controls, (2) nonrandomized studies with historical controls, (3) nonrandomized studies with concurrent controls, and (4) randomized controlled trials (RCTs). For a variety of reasons, case-controlled and prospective studies with historic controls are sometimes the only feasible way to approach clinical questions. 21,25RCTs have been identified as the strongest design for evaluating the effects of therapy. RCTs test hypotheses by using randomly assigned treatment and control groups of adequate size to examine the efficacy and safety of a new therapy. In theory, random assignment of the treatment balances unknown or unmeasured factors that might otherwise bias the outcome of the trial. A meta-analysis combines and reports the results of several trials. Tyson47 has suggested criteria for identifying proven therapies in current literature (Box 1-1). Although conclusions drawn from systematic reviews of RCTs have been regarded as the strongest level of evidence, evidence from descriptive and qualitative studies should be factored into clinical decisions when either randomized trials are not available or additional information is sought related to personal experiences or perspectives on care. Evidence-based practice, using knowledge gained from qualitative studies, recognizes the expertise of individual clinicians and parents in evaluating health care provision. Price,36using a qualitative methodology, explored the experience of parents with a child in the neonatal intensive care unit (NICU) and revealed how non-technical aspects of care, such as comforting infants after painful procedures, were as important to parents as the “technical aspects.” Wigert51 used a phenomenological hermeneutic design to elicit the experiences of having an infant in the NICU. Parents experienced a tension between exclusion and participation in their infant’s care with an emphasis on exclusion. In a qualitative study, Charchuk and Simpson12 described a similar situation of parents experiencing a lack of disclosure of their infant’s condition and a lack of control. Raines37 used a qualitative design to describe nurses’ expertise in the NICU. Through analysis, Raines described how neonatal nurses, after learning technical skills, could focus on parental needs.
BOX 1-1
Reported to be beneficial in a well-performed meta-analysis of all trials
or
Beneficial in at least one multicenter trial or two single-center trials
Modified from Tyson JE: Use of unproven therapies in clinical practice and research: how can we better serve our patients and their families? Semin Perinatol 19:98, 1995.
PRESSURES TO INTERVENE
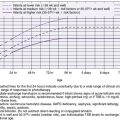
Although RCTs are cited as providing the best evidence for guiding clinical decisions, they take time, and it is difficult to delay introduction of promising therapies. The pressure to intervene and change practice before studies are conducted or completed has many sources. Ian Chalmers, 9 in considering the struggle to gather scientific evidence in a climate of firmly held beliefs, has illustrated some of the pressures facing the scientific investigator (Figure 1-1). Bryce and Enkin8 discussed myths about RCTs that lead to reasons to not conduct them. One myth is that randomization is unethical. This might be true in the rare instance that an intervention is dramatically effective and lifesaving. The more common situation is one in which there is relatively poor evidence for both the current and the alternative strategy. To compare an established strategy whose benefit is not scientifically supported (even though widely acclaimed) with one that is openly “experimental” is not unethical; in fact, both are “experimental.” It is continued use of an unstudied practice that might more readily be labeled “unethical.”
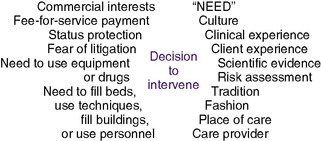 |
| FIGURE 1-1
(From Chalmers I: Scientific inquiry and authoritarianism in perinatal care and education, Birth 10:3, 1983.)
|
Pressure to intervene is, however, often overpowering. Believing that an infant is in trouble, interventions occur through a cascade of interventions, 32 one leading to the next and each carrying risk. One of the most frequently cited examples is the epidemic of blindness associated with use of oxygen in newborns. 40,41 Oxygen, used since the early 1900s for resuscitation and treatment of cyanotic episodes, was noted in the 1940s to “correct” periodic breathing in premature infants. After World War II and introduction of new gas-tight incubators, an epidemic of blindness occurred, resulting from retrolental fibroplasia (RLF). Silverman pointed out that although many causes were suspected, it was not until 1954 that a multicenter, controlled trial confirmed the association between high oxygen concentrations and RLF. 40 Frequently forgotten, however, is that in subsequent years, mortality was increased in infants cared for with an equally experimental regimen of strict restriction of oxygen administration and many survivors had spastic diplegia. In the 1960s, introduction of microtechniques for measuring arterial oxygen tension permitted better monitoring of oxygen therapy, with a reduction in mortality, spastic diplegia, and RLF, now called retinopathy of prematurity (ROP). ROP is currently limited to extremely low-birth-weight (ELBW) infants; 40 research continues to explore causes, preventive measures, and treatments (see Chapter 23).
The desire to see an intervention “work” encourages practitioners and investigators to seek early signs of benefit. Long-term effects are frequently overlooked. One reason is that they may not be foreseen. Consider the example of diethylstilbestrol (DES). DES administration to pregnant women was introduced in 1947 without clinical trials to prevent miscarriage, fetal death, and preterm delivery. 8,22 It was thought to be effective after uncontrolled studies despite controlled trials summarized in an overview (meta-analysis) by Goldstein et al23 (Table 1-1) that showed the opposite. Clearly, DES was not effective, but it continued to be used until the 1970s, when the Food and Drug Administration (FDA) finally disapproved its use. The unforeseen result was that female children born to mothers who were given DES had structural abnormalities of the genital tract, pregnancy complications, decreased fertility, and an increased risk for vaginal adenocarcinoma in young women. Male children had epididymal cysts. The Centers for Disease Control and Prevention (CDC) has even considered the possibility of effects in grandchildren of exposed women. 17 This is not the only example of physicians continuing to use therapies that have been shown in RCTs to be of no benefit. 11
| *An odds ratio is an estimate of the likelihood (or odds) of being affected by an exposure (e.g., a drug or treatment), compared with the odds of having that outcome without having been exposed. Women receiving DES did not have fewer stillbirths, premature births, or miscarriages than women who were untreated. |
||
| Data from Goldstein PA, Sacks HS, Chalmers TC: Hormone administration for the maintenance of pregnancy. In Chalmers I, Enkin M, Keirse M, editors: Effective care in pregnancy and childbirth, New York, 1989, Oxford University Press. | ||
| Typical Odds Ratio* | 95% Confidence Limits | |
|---|---|---|
| Miscarriage | 1.20 | 0.89–1.62 |
| Stillbirth | 0.95 | 0.50–1.83 |
| Neonatal death | 1.31 | 0.74–2.34 |
| All three | 1.38 | 0.99–1.92 |
| Prematurity | 1.47 | 1.08–2.00 |
The costs of long-term studies and follow-up surveillance are numerous. However, when effects are measurable later in life (e.g., psychological problems, ability to function in school), cost should not determine study design. Even when randomized trials are conclusive, unanswered questions remain: Will a technology or treatment have the same effect in all settings? Has an “appropriate” target population been selected? Are there long-term unforeseeable consequences?
EVALUATION OF THERAPIES
The major cause of death in premature infants is respiratory failure from respiratory distress syndrome (RDS) (see Chapter 23). Previously called hyaline membrane disease (HMD), this syndrome of expiratory grunting, nasal flaring, chest wall retractions, and cyanosis unresponsive to high oxygen concentrations was a mystery until the 1950s. 41
The evaluation of various therapies for RDS contrasts the value of controlled and uncontrolled trials. Sinclair42 noted that uncontrolled studies were more likely to show benefit than controlled trials. In 19 uncontrolled studies, 17 popular therapies showed “benefit.” In 18 controlled studies, only 9 demonstrated benefit. An untrained reviewer of the research might base clinical practice on faulty conclusions of uncontrolled trials
Surfactant Therapy
In contrast to many proposed treatments, surfactant therapy in premature infants has been well studied in RCTs. 20a,25 Studies have evaluated the use of surfactant in treatment of RDS, including the optimal source and composition of surfactant and prophylactic versus rescue treatment. Morbidity (including pneumothorax, periventricular or intraventricular hemorrhage, bronchopulmonary dysplasia [BPD], and patent ductus arteriosus) and mortality rates in treatment and control groups have been compared. A recent summary of these RCTs shows increased survival rates, improved oxygenation and ventilation, and a decrease in the incidence of pneumothorax. 20a Effects on BPD are less consistent. Although RCTs involving thousands of newborns have clearly demonstrated the benefits of surfactant therapy, unanswered questions remain. Research is needed to define the optimal dose, optimal number of treatments, and most efficacious formulation. 20a
Corticosteroid Therapy
Misuse of corticosteroids in perinatal medicine illustrates the consequences of failure to practice evidence-based medicine. Many practitioners initially declined to use single doses of antenatal steroids to promote maturation of the immature fetal lung and prevent RDS despite strong supportive evidence, demonstrating a failure to use a proven therapy. At the same time, other practitioners administered repeated doses despite lack of evidence of additional benefit and questions about safety, representing unproven use of a proven therapy. Postnatal glucocorticoids, administered to the infant after birth, were widely used despite weak evidence of long-term benefit and suggestions of possible harm, illustrating use of an uncertain therapy. 27,28
ANTENATAL CORTICOSTEROID THERAPY: SINGLE COURSE
Antenatal administration of corticosteroids to pregnant women who threatened to deliver prematurely was first shown in 1972 to decrease neonatal mortality rate and the incidence of RDS and intraventricular hemorrhage (IVH) in premature infants. 29 In 1990, Crowley et al15 used meta-analysis to evaluate 12 RCTs of maternal corticosteroid administration involving more than 3000 women. The data showed that maternal corticosteroid treatment significantly reduced the risk for neonatal mortality, RDS, and IVH. After two decades of published clinical trials10,13,14,26 and the consensus development conference statement on “Effects of Corticosteroids for Fetal Maturation on Perinatal Outcomes,”33 antenatal corticosteroid treatment of women at risk for preterm delivery between 24 and 34 weeks of gestation has been shown to be effective and safe in enhancing fetal lung maturity and reducing neonatal mortality. Yet adoption by caretakers was inexplicably slow. 26
ANTENATAL CORTICOSTEROID THERAPY: REPEATED COURSES
Repeated courses of antenatal corticosteroids have been shown in humans and animals to improve lung function and the quantity of pulmonary surfactant. 16,24 They may also have adverse effects on lung structure, fetal somatic growth, and neonatal adrenocortical function, as well as poorly understood effects on blood pressure, carbohydrate homeostasis, and psychomotor development. 16,31 A 2000 NIH Consensus Development Conference found limited high-quality studies on the use of repeated courses of antenatal steroids. 34 The consensus statement discouraged routine use of repeated courses of antenatal corticosteroids. Results since 2000 are conflicting, with studies finding variously that repeated doses of antenatal corticosteroids are beneficial, 15 of no benefit, 17 or possibly harmful. 34 The paucity of school-age follow-up assessment of infants who received multiple courses has recently been re-emphasized. 2 The American College of Obstetricians and Gynecologists continues to advise that repeated courses of antenatal corticosteroids should be limited to patients enrolled in RCTs. 14
POSTNATAL STEROID THERAPY
Despite early calls for caution in the use of postnatal corticosteroids to decrease the risk for chronic lung disease and limit ventilator time, 29 they were used liberally in the 1990s. 45,46 A number of years passed before RCTs of postnatal corticosteroid administration included long-term follow-up. Taken together, these studies showed positive short-term effects on the lungs. They also showed increased blood pressure and blood glucose concentrations in the short term; increased incidence of septicemia and gastrointestinal perforation in the intermediate term; and with dexamethasone administered soon after birth, abnormal neurodevelopmental outcome, including cerebral palsy, in the long term. 19,26,42,46,49 An increased risk for septicemia should have been anticipated, because it was first identified in an RCT by Reese et al38 over 50 years earlier.
In 2002, the American Academy of Pediatrics (Committee on Fetus and Newborn) and the Canadian Paediatric Society (Fetus and Newborn Committee) advised against the use of systemic dexamethasone. They suggested that aside from “exceptional clinical circumstances,” use of corticosteroids should be limited to patients enrolled in RCTs that include assessment of long-term developmental outcomes. 1 A 2005 re-analysis of many of the same data by Doyle et al19 suggests that relative risks and benefits of postnatal corticosteroids vary with level of risk for BPD. When the risk for BPD or death is high, the risk for developmental impairment from postnatal corticosteroids might be outweighed by benefit. 20 Watterberg et al have suggested that hydrocortisone might have the benefits of dexamethasone on the lungs without adverse neurologic effects. 50 Much remains to be learned about postnatal use of corticosteroids to determine dose, timing, duration, type of steroid, benefits, and risks.
SYSTEMATIC REVIEW IN PERINATAL CARE AND THE BIRTH OF EVIDENCE-BASED MEDICINE
Evidence-based medicine (EBM) has been defined as the “conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients”35 Examples from the literature, such as those cited in the preceding sections, illustrate how the application of the principles of evidence-based medicine offers a strong argument countering those who assert that EBM is nothing more than “typical practice using good clinical judgment.” Proponents of EBM argue that the principal four steps of evidence-based practice—formulating a clinical question, retrieving relevant information, critically appraising the relevant information, and applying the evidence to patient care—provide a foundation for practice that leads to improved newborn outcomes and avoidance of repeating medical disasters. It is interesting to note that the roots of the EBM movement can be found in perinatal medicine.
Believing that the results of perinatal controlled trials had to be summarized in a manner useful to practitioners, Chalmers et al11 and other perinatal professionals from various countries developed a registry of RCTs. They reviewed a vast amount of literature from published trials, sought out unpublished trials, and encouraged those who had begun, but not completed, studies to make them known to the registry. Once gathered, the studies’ findings were summarized in “overviews.”
A systematic review (or meta-analysis) pools the results of independently conducted RCTs whose study methods are reasonably similar, both in the selection and characteristics of participants and in the treatments that are offered. The results produce unbiased estimates of the effect of an intervention on clinical outcomes and are distinguished from nonsystematic reviews in which author opinions often are reported along with the evidence. Tables 1-1 and 1-2 were developed after pooling the results of different studies.
| *In this table it can be seen that mortality was not different when the results of the two treatments were compared. |
||||
| †None of the relative risk estimates were statistically significant. |
||||
| Data from Soll RF, McQueen MC: Respiratory distress syndrome. In Sinclair JC, Bracken MB, editors: Effective care of the newborn infant, Oxford, England, 1992, Oxford University Press. | ||||
| Author | Prophylactic | Treatment | Relative Risk† | 95% Confidence Interval |
|---|---|---|---|---|
| Dunn | 09/62 | 08/60 | 1.09 | 0.45, 2.65 |
| Kendig | 29/235 | 49/244 | 0.62 | 0.62, 0.94 |
| Merritt | 29/102 | 23/101 | 1.25 | 0.78, 2.00 |
| Typical effect | 0.85 | 0.63, 1.14 | ||
From these systematic reviews, practitioners can learn the strengths or weakness of clinical trials and evaluate the claims of benefit for implementing a strategy. The result of the efforts of Chalmers et al was the 1989 publication of a remarkably useful book, Effective Care in Pregnancy and Childbirth.11 At the end of their book, they reported their own views of the reviewed treatments based on conclusions formed in the preceding articles. They found that although some strategies and forms of care were useful, others were questionable. Some interventions believed to be useful were not useful, of little benefit, or in fact, even harmful. In 1991, a companion publication, Effective Care of the Newborn Infant,43 compiled and reviewed neonatal RCTs.
Multiple networks have been developed to perform multicenter RCTs. This is particularly useful, providing an opportunity to see whether treatments have similar effects in different practice settings. It is also useful in that practitioners in individual settings may not always see enough cases to reach robust conclusions. Rare conditions and rare outcomes are better understood when trials are replicated or their findings are pooled. Systematic reviews provide the opportunity to understand these findings in the context of clinical practice. About the same time the Chalmers et al book was published, the Cochrane Collaboration was established, again largely through the efforts of Ian Chalmers(www.cochrane.org/index0.htm). The Cochrane Collaboration is a worldwide group with over 50 Collaborative Review Groups whose members prepare, maintain, and disseminate systematic reviews based primarily on the results of RCTs. These reviews are published electronically in the Cochrane Library, which contains the Cochrane Database of Systematic Reviews (CDSR: www.cochrane.org/reviews/index.htm), along with editorial comments on these reviews. Comments come from an international group of individuals and institutions dedicated to summarizing randomized controlled trials relevant to health care. In addition to the Collaborative Review Groups, there are now 12 Cochrane Centers in the world. These centers provide support for the review groups. The Neonatal Group is based at McMaster University in Hamilton, Ontario, Canada; and the Pregnancy and Childbirth Group is based at the University of Liverpool, Liverpool, England. Cochrane Neonatal Reviews are available at the National Institute of Child Health and Human Development (NICHD) Cochrane Neonatal Internet home page; approximately 250 overviews are listed .32
Additional sources of high-grade integrative literature are also available to the practicing clinician. Critical appraisal of published research takes considerable time, and several groups assemble high-grade literature using a uniform methodology that is typically described to readers as a supplementary article. Reading this article once can inform the practitioner if the method used to assemble a review or guideline is sufficiently rigorous. Also, a number of sites do not produce integrative literature but collect it from a number of sources. Some of these sites discuss the quality of the information presented. If we cannot appraise the method used to collect this information, we should always proceed with caution. Additional reliable sites include the following:
• The Database of Abstracts of Reviews of Effectiveness (DARE) (www.crd.york.ac.uk/crdweb/), a collection of international reviews including those from the Cochrane Collaboration. Reviewers at the National Health Service Center for Reviews and Dissemination at the University of York, England, provide quality oversight including detailed structured abstracts that describe the methodology, results, and conclusions of the reviews. The quality of the reviews is discussed along with implications for health care.
• National Guidelines Clearinghouse (www.guidelines.gov/browse/guideline_index.arpx), maintained by the U.S. Department of Health and Human Services, Agency for Health Care Research and Quality (AHRQ), in partnership with the American Medical Association (AMA) and the American Association of Health Plans (AAHP). This site provides a wide range of clinical practice guidelines from institutions and organizations. Structured abstracts facilitate critical appraisal, and abstracts on the same topic can be compared on a side-by-side table, allowing comparisons of relevance, generalizability, and rigor of research findings. Links also are provided to the full text of each guideline, when available.
Admittedly, there are problems with EBM. Conducting systematic reviews is time-consuming; thus not many are available. Often, the power of randomized controlled trials, especially in neonatology, is low. The evidence in published studies does not always apply to our specific patient. In addition, locating relevant evidence is time-consuming and may require access to online resources and a higher level of information-seeking skills than is available. Finally, although recognizing that medical expertise and scientific knowledge are crucial components of neonatal care, these rigorous, objective, scientific evaluations create the potential to overlook valuable experiential knowledge of the NICU provided by practitioners and parents.
Reasons to use an evidence-based approach have been well documented. According to Asztalos, 2 there are basically two reasons to try to keep up with the literature: (1) to maintain clinical competence; and (2) to solve specific clinical problems. Phillips and Glasziou35 suggest that clinicians seek information “just in time” (as a clinician seeing patients) and “just in case” (to keep up with a clinical specialty). The former can be achieved by actively searching for information in filtered, summarized clinical point-of-care resources. FirstConsult, DynaMed, Clinical Medicine, and UpToDate fall into this category. The latter, “just in case” learning, also called surveillance of the literature, is best achieved by using technology tools to survey the current original literature. These tools include auto-alerts and RSS feeds in PubMed or online databases and journals. Learning about these ever-changing resources is a challenge. Many hospitals and clinics are beginning to include a clinical librarian or informationist as part of the health care team. 4.5.6. and 7.30,36,44,48At the end of this chapter is a list of additional evidence-based medicine resources. To use these resources effectively, individuals must become familiar with the principles and value of evidence-based patient care. EBM can be practiced successfully at the individual level; in addition, an individual clinician can act as a change agent and advocate for evidence-based institutional practice.
As stated by Silverman40:
Since ours is the only species on the planet that has achieved rates of newborn survival which exceed 90 percent, it seems to me we must demand the highest order of evidence possible before undertaking widespread actions that may affect the full lifetimes of individuals in the present, as well as in future generations. Here a strong case can be made for a slow and measured pace of medical innovation.
REFERENCES
1. American Academy of Pediatrics, Committee on Fetus and Newborn, Postnatal corticosteroids to treat or prevent chronic lung disease in preterm infants, Pediatrics 109 (2002) 330.
2. Asztalos, E., The need to go beyond: evaluating antenatal corticosteroid trials with long-term outcomes, J Obstet Gynaecol Can 29 (2007) 429.
3. Reference deleted in proofs.
4. Brackenbury, T.; Burroughs, E.; Hewitt, L., A qualitative examination of current guidelines for evidence-based practice in child language intervention, Lang Speech Hear Serv Sch 39 (2008) 78.
5. Brandes, S., Experience and outcomes of medical librarian rounding, Med Ref Serv Q 26 (2007) 85.
6. Brettle, A.; Hulme, C.; Ormandy, P., The costs and effectiveness of information skills training and mediated searching: qualitative results from the empiric project, Health Info Libr J 23 (2006) 239.
7. Brettle, A.; Hulme, C.; Ormandy, P., Effectiveness and information skills training and mediated searching: qualitative result from the empiric project, Health Info Libr J 24 (2007) 24.
8. Bryce, R.L.; Enkin, M.W., Six myths about controlled trials in perinatal medicine, Am J Obstet Gynecol 151 (1985) 707.
9. Chalmers, I., Scientific inquiry and authoritarianism in perinatal care and education, Birth 10 (1983) 151.
10. In: (Editor: Chalmers, I.) Oxford database of perinatal trials ( 1988)Oxford University Press, Oxford, England.
11. Chalmers, I.; Enkin, M.; Keirse, M., Effective care in pregnancy and childbirth. ( 1989)Oxford University Press, New York.
12. Charchuk, M.; Simpson, C., Hope, disclosure, and control in the neonatal intensive care unit, Health Commun 17 (2) ( 2005) 191.
13. Collaborative Santiago Surfactant Group, Collaborative trial of prenatal thyrotropin-releasing hormone and corticosteroids for prevention of respiratory distress syndrome, Am J Obstet Gynecol 178 (1 Pt 1) ( 1998) 33.
14. Committee on Obstetric Practice, Antenatal corticosteroid therapy for fetal maturation, Obstet Gynecol 111 (2008) 805.
15. Crowley, P.; Chambers, I.; Keirse, M.J., The effects of corticosteroid administration before preterm delivery: an overview of the evidence from controlled trials, Br J Obstet Gynaecol 97 (1990) 11.
16. Crowther, C.A.; Haslam, R.R.; Hiller, J.E.; et al., Neonatal respiratory distress syndrome after repeat exposure to antenatal corticosteroids: a randomized controlled trial, Lancet 367 (2006) 1913.
17. Crowther, C.A.; Harding, J.E., Repeat doses of prenatal corticosteroids for women at risk of preterm birth for preventing neonatal respiratory disease, Cochrane Database Syst Rev ( 3) ( 2007); CD003935’ DOI, 10.1002/14651858.CD003935.pub2.
18. Dawes, M.; Davies, P.; Gray, A., Evidence based practice: a primer for health care professionals. ( 2004)Churchill Livingstone, New York.
19. Doyle, L.; Halliday, H.L.; Ehrenkranz, R.A.; et al., Impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk for chronic lung disease, Pediatrics 115 (2005) 655.
20. Eichenwald, E.C.; Stark, A.R., Are postnatal steroids ever justified to treat severe bronchopulmonary dysplasia?Arch Dis Child Fetal Neonatal Ed 92 (2007) 334.
20a. Engle, W.A., and the Committee on Fetus and Newborn: Surfactant-replacement therapy for respiratory distress in the preterm and term neonate, Pediatrics 121 (2008) 419.
21. Finer, N.N.; Craft, A.; Vaucher, Y.E.; et al., Postnatal steroids: short-term gain, long-term pain?J Pediatr 137 (2000) 9.
22. Fletcher, R.H.; Fletcher, S.W.; Wagner, E.H., Clinical epidemiology. ed 2 ( 1988)Williams & Wilkins, Baltimore.
23. Goldstein, P.A.; Sacks, H.S.; Chalmers, T.C., Hormone administration for the maintenance of pregnancy, In: (Editors: Chalmers, I.; Enkin, M.; Keirse, M.) Effective care in pregnancy and childbirth ( 1989)Oxford University Press, New York.
24. Guinn, D.A.; Atkinson, M.W.; Sullivan, L.; et al., Single vs weekly courses of antenatal corticosteroids for women at risk of preterm delivery: a randomized controlled trial, JAMA 286 (2001) 1581.
25. Halliday, H.L., Surfactants: past, present and future, J Perinatol 28 (Suppl 1) ( 2008) S47.
26. Jobe, A.H., Glucocorticoids in perinatal medicine: misguided rockets?J Pediatr 137 (2000) 1.
27. Jobe, A.H.; Mitchel, B.R.; Gunkel, J.H., Beneficial effects of the combined use of prenatal corticosteroids and postnatal surfactant on preterm infants, Am J Obstet Gynecol 168 (1993) 508.
28. LeFlore, J.L.; Salhab, W.A.; Broyles, R.S.; et al., Association of antenatal and postnatal dexamethasone exposure with outcomes in extremely low birth weight neonates, Pediatrics 110 (2002) 275.
29. Liggins, G.C.; Howie, R.N., A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants, Pediatrics 50 (1972) 515.
30. Mann, M.; Sander, L.; Weightman, A., Signposting best evidence: a role for information professionals, Health Info Libr J 23 (Suppl 1) ( 2006) S61.
31. Mildenhall, L.J.F.; Battin, M.R.; Morton, S.M.B.; et al., Exposure to repeat doses of antenatal corticoids is associated with altered cardiovascular status after birth, Arch Dis Child 91 (2006) F56.
32. National Institute of Child Health and Human Development, Cochrane Neonatal Home Page:www.nichd.nih.gov/cochrane.
33. National Institutes of Health Consensus Development Conference Statement, Effects of corticosteroids for fetal maturation on perinatal outcomes, JAMA 273 (1995) 413.
34. National Institutes of Health, Antenatal corticosteroids revisited: repeat courses, NIH Consensus Statement 2000 17 (2000) 1.
35. Phillips, R.; Glasziou, P., Evidence based practice: the practicalities of keeping abreast of clinical evidence while in training, Postgrad Med J 84 (2008) 450.
36. Price, P.J., Parents’ perceptions of the meaning of quality nursing care, ANS Adv Nurs Sci 16 (1) ( 1993) 33.
37. Raines, D., Parents’ values: a missing link in the neonatal intensive care equation, Neonatal Netw 15 (3) ( 1996) 7.
38. Reese, A.B.; Blodi, F.C.; Locke, J.C.; et al., Results of use of corticotropin (ACTH) in treatment of retrolental fibroplasia, AMA Arch Ophthalmol 47 (1952) 551.
39. Reference deleted in proofs
40. Silverman, W.A., RLF: a modern parable. ( 1980)Grune & Stratton, New York.
41. Silverman, W.A., Human experimentation: a guided step into the unknown. ( 1985)Oxford University Press, New York.
42. Sinclair, J.C., Prevention and treatment of respiratory distress syndrome, Pediatr Clin North Am 13 (1966) 711.
43. Sinclair, J.C.; Bracken, M.B., Effective care of the newborn infant. ( 1992)Oxford University Press, New York.
44. Spak, J.M.; Glovver, J.G., The personal librarian program: an evaluation of a Cushing/Whitney Medical Library outreach initiative, Med Ref Serv Q 26 (2007) 15.
45. Stark, A.R.; Carlo, W.A.; Tyson, J.E.; et al., Adverse effects of early dexamethasone treatment on extremely low-birth-weight infants, N Engl J Med 344 (2001) 95.
46. Stoll, B.J.; Temprosa, M.; Tyson, J.E.; et al., Dexamethasone therapy increases infection in very low birth weight infants, Pediatrics 104 (1999) 63.
47. Tyson, J.E., Use of unproven therapies in clinical practice and research: how can we better serve our patients and their families?Semin Perinatol 19 (1995) 98.
48. Urquhart, C.; Turner, J.; Durbin, J.; et al., Changes in information behavior in clinical teams after introduction of a clinical librarian service, J Med Lib Assoc 95 (2007) 14.
49. Watterberg, K.L., Postnatal steroids for bronchopulmonary dysplasia: where are we now?J Pediatr 150 (2007) 327.
50. Watterberg, K.L.; Gerdes, J.S.; Cole, C.H.; et al., Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial, Pediatrics 114 (2004) 1649.
51. Wigert, H., Mothers’ experiences of having their newborn child in a neonatal intensive care unit, Scand J Caring Sci 20 (2006) 35.
EVIDENCE-BASED MEDICINE RESOURCES
Databases of Evidence and Search Engines
ACP Journal Club, www.acponline.org/journals/acpjc/jcmenu.htm; Evidence-based evaluative summaries of articles taken from 100 clinical journals, written by MDs and others, with comments from MDs.
Campbell Collaboration, www.campbellcollaboration.org/; An independent, international, non-profit organization that aims to help people make well-informed decisions about the effects of interventions in the social, behavioral, and educational arenas. The vision of the Campbell Collaboration is to bring about positive social change and to improve the quality of public and private services across the world by preparing, maintaining, and disseminating systematic reviews of existing social science evidence. The Campbell Collaboration’s substantive priorities include, though are not confined to, education, social welfare, and crime and justice.
Cochrane Library, www.thecochranelibrary.com; Premier evidence-based medicine resource composed of the following:.
Database Database of Systematic Reviews containing systematic reviews and meta-analyses conducted by Cochrane Study Groups
Database Database of Reviews of Effects including systematic reviews and meta-analyses from non-Cochrane sources, many with structured abstracts with comments on the reviews
Central Center Register of Controlled Trials: Indexes many trials not included in MEDLINE
HTA HTA and NHS EED Include evidence-based reviews of technology and economic issues
Clinical ClinicalTrials.gov, http://clinicaltrials.gov/ct/gui; Provides regularly updated information about federally and privately supported clinical research in human volunteers. Gives information about a trial’s purpose, who may participate, locations, and phone numbers for more details.
Current Controlled Trials, www.controlled-trials.com/; Allows users to search, register, and share information about randomized controlled trials.
Google Coop Netting the Evidence, http://decenturl.com/google/nettingtheevidence; Andrew Booth, a pioneer in evidence-based information practice at the University of Sheffield, created one of the first lists of evidence-based health care resources on the Internet. He has taken this one step further with a Google Coop site that limits your Google search to over 100 authoritative, evidence-based websites. Type a condition and diagnostic method or treatment into the search box to quickly find resources with an evidence-based approach.
HSTAT HSTAT, http://hstat.nlm.nih.gov/; A free, web-based resource of full-text documents that provide health information and support health care decision making. HSTAT’s audience includes health care providers, health service researchers, policy makers, payers, consumers, and the information professionals who serve these groups.
NHS Centre for Reviews and Dissemination, www.york.ac.uk/inst/crd/; Resource for systematic reviews of health economics and technology assessment. Also maintains the DARE, Health Technology Assessment, and NHS Economic Evaluation databases included in Cochrane.
National Institutes of Child Health and Human Development (NICHD) Cochrane Neonatal, www.nichd.nih.gov/cochrane/; Resource for systematic reviews of child health topics.
SUMSearch SUMSearch, http://sumsearch.uthscsa.edu/; Identifies sources of evidence-based information using this metasearch engine.
TRIP TRIP Database, www.tripdatabase.com/; Locates high-quality, evidence-based medical literature using this metasearch engine. Some resources in the results list may require subscription.
WHO WHO Clinical Trial Search Portal, www.who.int/trialsearch/; Enables researchers, health practitioners, consumers, journal editors, and reporters to search more easily and quickly for information on clinical trials.
Databases of Guidelines
CMA Infobase, Clinical Practice Guidelines, www.cma.ca/; Click on Clinical Resources tab; requires membership. Excellent access to guidelines and other point-of-care resources.
Guidelines International Network (G-I-N), www.g-i-n.net/; Guidelines organized by health topic. Links to worldwide sources of guidelines.
National Guideline Clearinghouse, www.guideline.gov/; Use “Detailed Search” link on left for more specific searches. A U.S. resource for evidence-based clinical practice guidelines. A display tool allows side-by-side comparison of guidelines.
NHS National Institute for Clinical Excellence (NICE), www.nice.org.uk/; Evidence-based guidance on technology use, clinical care, and interventional procedures.
Scottish Intercollegiate Guidelines Network (SIGN), www.sign.ac.uk/; Use link on left to view guidelines by topic. Distribution point for Scottish national clinical guidelines.
U.S. Preventive Services Task Force (USPSTF), www.ahrq.gov/clinic/uspstfix.htm; A collection of materials related to the work of an independent panel of experts in primary care and prevention that systematically reviews the evidence of effectiveness and develops recommendations for clinical preventive services.
Evidence-Based Medicine Resources
Canadian Centres for Health Evidence, www.cche.net/; Based in Alberta, this centre provides resources and support for evidence-based practice.
Centre for Evidence-Based Medicine, (Oxford), www.cebm.net/; Major website for learning about, practicing, and teaching EBM. The Toolbox provides valuable resources for learning and practice.
Centre for Evidence-Based Medicine, (Toronto), www.cebm.utoronto.ca/; In addition to learning resources, this site provides focused syllabi for specialties and a glossary.
Cochrane Cochrane Collaboration, www.cochrane.org/; This international non-profit and independent organization is dedicated to making up-to-date, accurate information about the effects of health care readily available worldwide through systematic review of medical research.
Core Library for Evidence-Based Practice, www.shef.ac.uk/scharr/ir/netting/; This resource provides a directory of a wide variety of evidence-based learning and practice materials.
Evidence Based Medicine Tool Kit, www.med.ualberta.ca/ebm/; A collection of tools for identifying, assessing, and applying relevant evidence for better health care decision making.
PedsCCM Evidence-Based Medicine Resources, http://pedsccm.org/EBJournal_Club_intro.php; An online collection of resources and training tools for the pediatric professional.
Student’s Guide to the Medical Literature, http://140.226.6.124/SG/; A guide suitable for anyone new to evidence-based medicine, written by a former UCD-AMC medical student for other students.
Understanding Evidence-based Healthcare: A Foundation for Action, http://apps1.jhsph.edu/cochrane/CUEwebcourse.htm; A web course created by the U.S. Cochrane Center that is designed to help the user understand the fundamentals of evidence-based health care concepts and skills. The 6-module course can be done in 15-minute segments and takes a minimum of 5 to 6 hours. Course registration is free and open to all. The hosts request that participants commit to completing the evaluations.
Users’ Guides to the Medical Literature, first edition:http://pubs.ama-assn.org/misc/usersguides.dtl; secondedition:www.JAMAevidence.com; Excellent self-paced learning modules based on the JAMA Users’ Guide series, featuring interactive activities designed to reinforce learning.
History of Evidence-Based Medicine
Chronology of the Cochrane Collaboration, www.cochrane.org/cochrane/cchronol.htm; A source of information about the development of the Cochrane Collaboration and its significance to evidence-based health care.
Controlled Trials from History at the James Lind Library, www.jameslindlibrary.org/; Excellent source of historical examples of RCTs; perfect for presentations on evidence-based health care.
Teaching Evidence-Based Medicine
Centre for Evidence-Based Medicine, (Oxford), www.cebm.net/?o=1021; Major website for learning about, practicing, and teaching EBM. The Toolbox provides valuable resources for learning and practice.
Evidence Based Medicine Teaching Materials, www.ebmny.org/teach.html; Resource list that includes courses, teaching tools, presentation materials, and a link to a systematic review of the effectiveness of teaching critical appraisal skills.
Fresno Test of Evidence Based Medicine, http://grinch.uchsc.edu/education/ebhc/fresno-test.pdf; This validated test measures competence in searching for and evaluating medical literature.
Richardson, W.S., Teaching evidence-based practice on foot, ACP J Club 143 (2) ( 2005) A10; This article describes methods for teaching evidence-based medicine during rounds.
Syllabi For Practicing EBM, www.cebm.utoronto.ca/syllabi/; These syllabi, taken from the book Evidence-Based Medicine: How to practice and teach EBM include scenarios and teaching materials for 14 different fields, including general practice, geriatrics, physiotherapy, nursing, child health, complementary medicine, gastroenterology, and purchasing.
Tips Tips for learners [and teachers] of evidence-based medicine, CMAJ ( 2004-2005); www.cmaj.ca/cgi/collection/evidence_based_medicine_series/; This series is devoted to helping clinicians understand and apply the basic principles of EBM. The series also targets teachers of EBM principles and offers tips for teaching key concepts. Be sure to advance to page 2 to see all of the articles in the series. Teachers should click on the “Online Appendix” links for teaching advice.
Websites
Centers Centers for Health Evidence
www.cche.net/usersguides/main.asp www.cche.net/usersguides/main.asp.
Directory Directory of EBM sites and resources
www.herts.ac.uk/lis/subjects/health/ebm.htm www.herts.ac.uk/lis/subjects/health/ebm.htm.
EBM EBM Toolbox
www.cebm.net/toolbox.asp www.cebm.net/toolbox.asp.
Evidence Evidence-Based Medicine: What It Is and What It Isn’t
www.cods.edu/cebd-i/articles/article01.htm www.cods.edu/cebd-i/articles/article01.htm.
Health Health Information Research Unit (HIRU)
hiru.mcmaster.ca/ http://hiru.mcmaster.ca/.
Health Health Care Information Resources: Evidence-Based Health Care Practitioners Links
www-hsl.mcmaster.ca/resources/ebpractice.htm www-hsl.mcmaster.ca/resources/ebpractice.htm.
Users Users Guide to the Medical Literature
www.shef.ac.uk/scharr/ir/userg.html www.shef.ac.uk/scharr/ir/userg.html.
Texts
Craig, J.; Snyth, R., The evidence-based practice manual for nurses. ( 2007)Churchill Livingstone, New York.
Dawes, M.; Davies, P.; Gray, A., Evidence based practice: a primer for health care professionals. ( 2004)Churchill Livingstone, New York.
Dicenso, A.; Guyat, G.; Ciliska, D., Evidence based nursing: a guide to clinical practice. ( 2005)Mosby, St Louis.
Friedland, D.J.; Go, A.S.; Davoren, J.B.; et al., Evidence-based medicine: a framework for clinical practice. ( 1998)Appleton-Lange, Stamford, Conn.
Greenhalgh, T., How to read a paper: the basics of evidence-based medicine. ed 2 ( 2001)BMJ Publishing Group, London.
Malloch, K.; Porter-Grady, T., Introduction to evidence-based practice in nursing and health care. ( 2006)Jones & Bartlett Publishers, Boston.
Melnyk, B.; Fineout-Overholt, E., Evidence based practice in nursing and healthcare. ( 2005)Lippincott Williams & Wilkins, Philadelphia.
Riegelman, R.K., Studying a study and testing a test: how to read the medical evidence. ed 4 ( 2000)Little, Brown, Boston.
Sackett, D.L.; Richardson, W.S.; Rosenberg, W.; et al., Evidence-based medicine: how to practice and teach EBM. ( 2000)Churchill Livingstone, Edinburgh.
Articles
Ambalavanan, N.; Whyte, R.K., The mismatch between evidence and practice: common therapies in search of evidence [Review], Clin Perinatol 30 (2003) 305.
Gonzalez de Dios, J., Bibliometric analysis of systematic reviews in the Neonatal Cochrane Collaboration: its role in evidence-based decision making in neonatology [Spanish], An Pediatr (Barc) 60 (2004) 417.
Kramer, M.S., Randomized trials and public health interventions: time to end the scientific double standard [Review], Clin Perinatol 30 (2003) 351.
The Learning and Information Services, University of Hertfordshire, maintains an updated and selective, but substantial list of references on the theory and methodology of evidence-based medicine/healthcare. Retrospective references are available as well from 1993 to 2002. Retrieved fromwww.herts.ac.uk/lis/subjects/health/ebm.htm#refs.
Shulman, S.T., Neonatology, then and now, Pediatr Ann 32 (2003) 562.
Sinclair, J.C., Evidence-based therapy in neonatology: distilling the evidence and applying it in practice [Review], Acta Paediatr 93 (2004) 1146.
Sinclair, J.C.; Haughton, D.E.; Bracken, M.B.; et al., Cochrane neonatal systematic reviews: a survey of the evidence for neonatal therapies, Clin Perinatol 30 (2003) 285.
Strand, M.; Phelan, K.J.; Donovan, E.F., Promoting the uptake and use of evidence: an overview of the problem [Review], Clin Perinatol 30 (2003) 389.