Chapter 75 Evaluation of the Cervical Spine after Trauma
Unrecognized injury to the cervical spine can produce catastrophic neurologic disability; clinicians are obligated to actively rule out cervical spine injury (CSI). The absence of injury is both difficult and imperative to define. Emergency departments in the United States and Canada are treating more than 13 million trauma victims annually who are at risk for CSI. The guidelines for cervical spine clearance are conflicting, and the management of patients is variable across medical institutions and different countries. Among neurologically intact patients, CSI is detected in 1%, the incidence in blunt trauma patients is 4.3%, and patients suffering a traumatic brain injury have a 5% to 10% chance of having CSI.1–4
Recent published studies examined radiation exposure as the cause of cancer. These studies extrapolate from data collected on radiation exposure and secondary malignancies in populations that experienced atomic bombing. Richards et al. compared the use of cervical radiographs combined with head CT to CT of the head and cervical spine. The calculated risk for lifetime cancer was 1:4500 and 1:2400, respectively. They concluded that as a screening procedure for a low-incidence finding, the risks might outweigh the benefits.5
Clinical Clearance of the Cervical Spine
The proper diagnosis of cervical spine trauma is considered extremely important and therefore results in the liberal use of cervical radiographs. These radiographs are easy to perform, but they expose the patient to ionizing radiation and account for substantial medical health expenses. Several small studies have suggested that patients with blunt trauma have a low probability of injury to the cervical spine if they meet all five of the following criteria: They do not have tenderness at the posterior midline of the cervical spine, they have no focal neurologic deficit, they have a normal level of alertness, they have no evidence of intoxication, and they do not have a clinically apparent, painful injury that might distract them from the pain of a CSI. These studies led to a large trial by the National Emergency X-Radiography Utilization Study Group (NEXUS) regarding criteria for clinical cervical spine clearance. A prospective observational multicenter study in 21 centers in the United States evaluated 34,069 patients with blunt trauma, of whom 4309 patients fulfilled all criteria for clinical clearance. The implementation of the criteria identified all but 8 of the 818 patients who had CSI picked by three-view radiographs. Only 2 of the 8 patients, missed by the clinical evaluation, had significant CSI. Following the outlined clinical algorithm, 12.6% of blunt trauma patients would have avoided the radiography screening.2
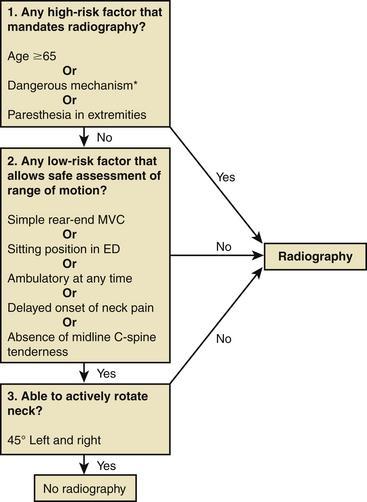
Stiell et al. proposed a different algorithm (Fig. 75-1) for cervical spine trauma. They studied 8924 patients after blunt head or neck trauma with stable vital signs and a Glasgow Coma Scale score of 15 points, of whom 151 (1.7%) had important C-spine injury. The algorithm consisted of three questions: whether the patient has high-risk factors, whether the patient has low-risk factors, and whether the patient has the ability to rotate the head. The sensitivity of this algorithm was 100% and the specificity was 42.5%, compared to three-view cervical radiograph or 2-week follow-up, reducing the radiography ordering rate to 58.2%.6
Stiell et al. compared the use of the NEXUS criteria to those of the Canadian Cervical-Spine Rule (CCR). The sensitivity and specificity for both tests were calculated after evaluation of 8283 Canadian patients suffering from head or neck trauma, 169 of whom (2%) had clinically significant spinal injury. The CCR was more sensitive than the NEXUS (99.4% vs. 90.7%, P < .001) and more specific (45.1% vs. 36.8%, P < .001) for injury, and its use would have resulted in lower radiography rates (55.9% vs. 66.6%, P < .001).4 The CCR algorithm is statistically superior but is also more complex to remember and implement, thus necessitating screening by well-trained trauma physicians. On the other hand, the NEXUS is less complex and can be utilized by physicians of various specializations.
Rethnam et al. retrospectively analyzed 114 alert trauma patients who had radiographs for cervical spine screening. If the CCR had been utilized, there would have been a 75.8% reduction in the number of patients who received radiographs, and neither of the two CSI patients would have been missed.7 Grossman et al. surveyed trauma centers in the United States and reported a wide variety of approaches to cervical spine clearance, with significant differences according to the trauma center level.1 Guidelines from the Eastern Association for the Surgery of Trauma (EAST) are based on the NEXUS algorithm.8,9 Because the best algorithm for cervical clearance is not agreed upon, it seems prudent that trauma centers should have a consensus algorithm implemented by all trauma caregivers.
Radiologic Clearance of the Cervical Spine
Radiographs
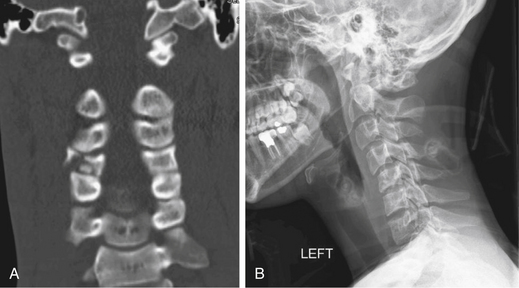
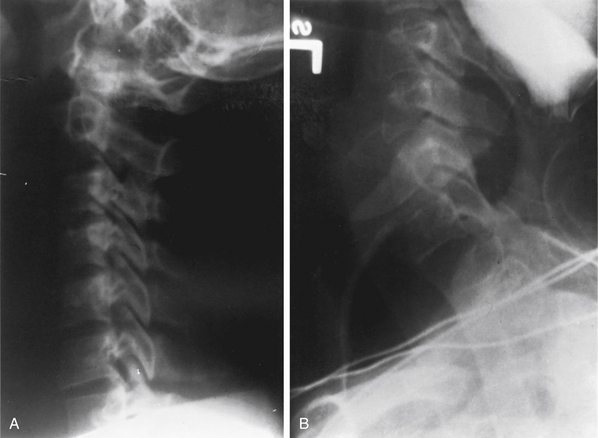
The American College of Surgeons Committee on Trauma published recommendations for the initial cervical spine radiographic evaluation in trauma victims. The committee included anteroposterior (Fig. 75-2A), lateral (Fig. 75-2B), and odontoid views of the cervical spine in this evaluation. Optimally, the lateral view images the rostral aspect of the first thoracic vertebra. Lateral films were reported to identify 85% of bony pathology; the addition of anteroposterior and odontoid views increases the sensitivity to 95%.10,11 However, newer studies utilizing CT and MRI scans in addition to radiographs report a 39% to 94% sensitivity with radiograph alone.12 Some authors conclude that CT is superior to radiography as a screening tool and should be utilized routinely in severe trauma, with or without radiography.13,14 Often, conventional lateral radiographs are insufficient, and a swimmer’s view may be necessary to image the cervicothoracic junction (Fig. 75-3).
Computed Tomography
Many centers use CT as the first subsequent study following radiography. CT is fast, is readily available, and facilitates patient monitoring (Fig. 75-4). The sensitivity of CT for cervical spine fractures has been reported to be between 90% and 99%, with specificities of 72% to 89%, and studies examining the sensitivity of radiography usually consider CT scan to be the gold standard.14,15 Nunez et al. compared radiographic screening to CT screening in 88 severe trauma patients. CT depicted 32 fractures that were not identified by radiography, most at the C1-2 and C6-7 regions. One third of these were unstable or clinically important.13 Link et al. demonstrated that inclusion of the cervicocranial region in the head CT, in addition to a three-view cervical radiograph, revealed additional cervical fractures in 5% of severe head trauma patients.14 According to EAST recommendations, CT should be utilized, in addition to radiography, for all patients with insufficient imaging of a specific region or evidence of radiographic abnormality, neurologic deficit, or impaired consciousness.8,9 Patient evaluation with both radiography and CT raised the question of whether the radiographic studies were necessary. In patients with severe trauma, it is difficult to obtain high-quality radiographic studies. Furthermore, imaging the patient delays further studies that may be needed and delivers further radiation to the thyroid. Hashem et al. retrospectively examined the added value of radiography to CT, in patients with CSI admitted to a level 1 trauma center. While CT demonstrated 100% of the pathologies, the sensitivity of radiography was 61%.16 These data should be considered when the guidelines for cervical spine clearance are being updated.
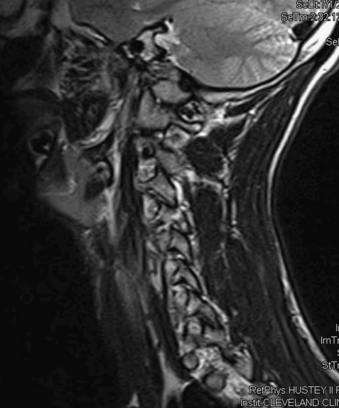
Magnetic Resonance Imaging
Radiographic and CT images are very sensitive to bony anatomy but are not efficient or sensitive in the detection soft tissue injury. Occurrence of cervical spine ligamentous injury, which is potentially unstable, is estimated to be 0.04% to 0.9%17; it is a rare condition but with possible severe consequences. MRI is considered by some to be the gold standard modality for evaluation of soft tissue injury. The images can identify prevertebral hematomas, lesions pressing on the cord such as herniated discs, ossification of the posterior longitudinal ligament, epidural hematoma, and spinal cord contusions or edema (Fig. 75-5). The data that are presented by MRI are a valuable diagnostic tool. Unlike CT, in which axial acquisition is reconstructed to three planes, MRI acquisition is accomplished in three planes, thus reducing the possibility of missing pathology that parallels the acquisition plane. MRI does not deliver radiation and hence reduces potential future risks for cancer. On the other hand, MRI is not always available in some trauma centers; it requires more time and personnel; it requires the use of special ventilator and monitoring techniques; and some immobilization and traction devices will not fit into the MRI or are not MRI compatible. Finally, hemodynamically or respiratory unstable patients should not undergo an MRI.12,18,19
The authors used limited MRI (sagittal T1- and T2-weighted images) as the routine subsequent imaging study in the comatose or obtunded trauma patient. This enabled full visualization of the cervical spine for alignment as well as for identification of soft tissue injury.20,21 Holmes et al.22 compared the sensitivity of CT to that of MRI. While MRI was extremely sensitive to spinal cord lesions and ligamentous injury, it missed 45% of vertebral fractures, was 78% sensitive to locked facets, and was 86% sensitive to vertebral dislocation or subluxation. CT was 97% sensitive to vertebral fractures and locked facets, 100% sensitive to vertebral dislocations, and 82% sensitive to subluxation. CT images did not recognize any of the spinal cord injuries but suggested them in a few patients according to the bony damage. Ligamentous injury was reported in 36 patients undergoing CT; 25% of them were inferred by the scan on the basis of bony displacement or angulation. Stassen et al.23 screened obtunded patients with CT, followed by MRI screening for the patients with negative CTs. They found that 13% of patients with negative CT had positive MRI for ligament injury. These patients were treated by immobilization in a collar and did not undergo surgery. In a review of the literature, MRI detects ligamentous injury in 22.7% of obtunded patients, 80.8% required treatment, and 5.6% required surgical or halo-vest immobilization.17
A meta-analysis study assessing the accuracy of MRI in trauma patients demonstrated 97.2% sensitivity and 98.5% specificity.18 The use of MRI, according to EAST guidelines, is warranted in cases of neurologic deficit only.8,9 Whether or not MRI should be a part of the routine screening process should be assessed according to level 1 evidence, which is currently unavailable.
Dynamic Studies
Although flexion-extension (FE) lateral radiographs are considered the standard for identifying ligamentous instability, their role should be considered carefully. The EAST recommendation utilizes FE imaging in three situations:8,9
1. An alert patient complaining of neck pain with normal radiograph if the patient can move the neck
2. Late examination (i.e., >14 days after the trauma) in an alert patient complaining of neck pain with normal radiograph but with limited motion of the neck (the patient is left in a collar until cleared)
3. An obtunded patient with normal radiograph and CT of the cervical spine (before removal of the collar)
Using FE to clear alert patients following acute trauma requires availability of a technician and a radiologist, delivers ionizing radiation to the patient, and is associated with a high incidence of suboptimal imaging because of body habitus or neck immobility.24–26 Goodnight et al. retrospectively compared the findings with CT and those with FE views. They found that FE did not provide added value in the face of a negative CT. They concluded that FE views were not efficient.27 The role of CT in the alert patient for cervical spine clearance is yet to be determined. It should be kept in mind that both CT and FE expose the patient to substantial radiation.
The dispute concerning the use of FE to clear the cervical spine in the obtunded patient is even more intense. Cooper and Ackland19 compared CT to FE use in obtunded patients. FE studies did not uncover additional injuries that had not already been identified by CT. Griffiths et al. examined the safety and efficacy of FE. They concluded that the examination is safe but did not identify new findings that were not identified by CT.28 Sliker et al. reviewed the literature concerning FE for clearance of the cervical spine. In 10 studies evaluating the role of FE, 1166 patients were included, 12 of them had CSI, of which 11 were diagnosed by FE, 60% of which required surgical treatment or halo-vest immobilization.17 The absence of level 1 evidence fosters confusion. The optimal method is yet to be determined.
Cervical Spine Clearance Algorithm
An algorithm for cervical spine clearance was published by EAST,8,9 but since imaging technology is advancing at a faster pace than the medical guidelines, this algorithm is not uniformly accepted. In addition, the availability of imaging studies and interpreters is not uniform across institutions. Therefore, a universal clearance algorithm is not accepted. The authors will present a proposed algorithm.
Alert Patient
Alert patients could be clinically screened by using either the NEXUS criteria or the CCR algorithm.2,6 For alert patients who do not qualify for clinical clearance, radiographic clearance should be employed. EAST guidelines are recommended, with the use of anteroposterior, lateral, and open-mouth views. If these are adequate and normal and the patient is neurologically intact and can move the head freely, no further studies are required. Inadequate studies can be supplemented with a swimmer’s view or CT scan through the areas of concern. For patients who complain of significant neck pain, FE views should be ordered. If the angle change between flexion and extension is above 30 degrees and no abnormal motion is detected, the cervical spine is cleared. Patients with restricted neck motion should be kept in a hard collar for 10 to 14 days until neck stiffness resolves, and then FE views should be ordered.8,9 Trauma victims who are expected to require cervical spine CT because of body habitus or mechanism of trauma might not require the use of three-view radiography.16 Once evidence of injury is found, further studies should be ordered to confirm or reject the findings and to define the characteristics and extent of injury. CT should be ordered to address bony pathology, and either FE studies or MRI should be ordered to define ligamentous injury. After unstable fractures are diagnosed, one should not proceed with FE studies, as they could potentially harm the cord; MRI should be utilized.8,9,29
Neurologic Deficit
Perhaps the least controversial clinical scenario is that of the patient with an obvious neurologic deficit. These patients should be evaluated for both bony pathology and soft tissue pathology. Because most will undergo CT and MRI, radiography might not be necessary.16 The optimal timing for both studies, according to EAST recommendations, is within 2 hours from arrival at the emergency department.8,9 These recommendations cannot always be followed, depending on personnel and equipment availability, and should be adjusted to provide the best medical treatment according to the resources.
Obtunded and Comatose Patients
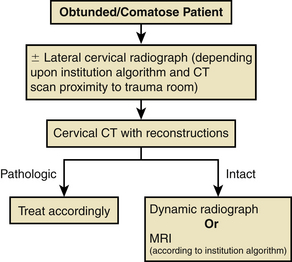
Obtunded and comatose patients should be treated as though they have a CSI until sufficient evidence is accrued to confirm or document absence of injury. According to EAST recommendations, trauma victims presenting with altered mental status for whom return of normal mental status is not anticipated for 2 days or more should undergo radiography and CT; if these are normal, an FE study should clear ligamentous injury.8,9 Multiple authors have challenged this approach. This subset of patients will undergo brain CT, and in many cases sufficient radiographic studies cannot be performed, as the patients are not cooperative and the tubing obscures the cervical spine. Hashem et al. questioned the added information provided by radiography over CT. They concluded that the sensitivity of CT was 100%; hence, radiographic studies are not necessary in these cases,16 Removing the radiograph from the algorithm reduces both the radiation dose and the time before the patient can be transferred to the CT scanner. Although CT for these patients is generally accepted, opinions regarding the next appropriate steps are highly variable.
Padayachee et al. examined the role of FE studies when added to CT in this subset population of patients. In this study, the FE did not identify any instability that was not recognized by CT.3 Spiteri et al. reported a series of 87 patients with unstable injuries, two of which were missed by CT. One was detected on FE, and the other was missed. They concluded that although FE studies are safe, they are not warranted because of their low rate of true-positive findings that are not identified by CT.30 Goodnight et al. reported a series of patients in which all positive FEs after negative CT were negative for ligamentous injury on MRI.27 These studies do not take into consideration the negative effect of transport to the fluoroscopy unit of these unstable patients, the cost, and the harmful effects of ionizing radiation to the patient and health-care providers.
The most sensitive imaging modality is MRI. MRI is more sensitive to soft tissue than to bony pathology. Holmes et al. studied a cohort of patients who had undergone both CT and MRI. They reported that the sensitivity to osseous fractures was 55%, while the sensitivity to cord injury and ligamentous injury was 100%.22 MRI in the setting of the polytrauma patient who is ventilated and sedated poses many concerns. These patients are difficult to transport to the MRI suite, special equipment is required to ventilate and monitor them, and they are escorted by professional staff for long periods of time and occupy the MRI scanner and personnel for long durations. In a study examining 173 trauma patients with risk factors for CSI and lack of significant findings in radiography, 36% had soft tissue injury detected by MRI. Of these patients, one was operated upon, and all were placed in either a hard cervical collar or a Minerva jacket.20 In a study of 121 obtunded or comatose trauma patients who had normal cervical spine radiographs and underwent MRI of the cervical spine as routine screening, 25.6% were found to have sustained significant soft tissue injury, 6.6% were operated upon, and all were treated with a rigid collar.21 Stassen et al. utilized a protocol containing both CT and MRI for obtunded trauma patients. They reported 25% of patients with negative CT but positive MRI for ligamentous injury. All were treated with a rigid collar.23
Sliker et al.17 reviewed the literature comparing FE studies to MRI for CSI screening. They detected a 0.9% true-positive rate for ligamentous injury using FE studies, of which 0.5% of patients underwent surgery. On the other hand, MRI detected 22.7% of patients with ligamentous injury, but 19.5% when only the obtunded patient population was assessed. Only 1.3% underwent surgery. It is obvious that MRI is very sensitive for the detection of ligamentous injury. The significance of these injuries, however, is uncertain. A meta-analysis examining MRI for cervical spine trauma clearance, encompassing five studies with a total enrollment of 464 patients, reported an incidence of 20.9% MRI abnormalities that were not evident on radiography, with or without CT. Fifteen patients in this cohort underwent surgery. All of these patients were studied with either radiograph or CT prior to the MRI. The authors concluded that while a negative MRI can confirm the absence of ligamentous injury, the false-positive rate has not yet been determined.18
It is reasonable to image obtunded patients with CT, with or without cervical radiography. Ligamentous integrity should be demonstrated before final clearance of the cervical spine. That can be done by either dynamic studies or MRI, depending on the institution’s resources and availabilities (Fig. 75-6).
Summary
Occult CSI can have devastating sequelae if undetected. Physicians treating traumatized patients must maintain a high level of suspicion when attempting to clear the cervical spine. It cannot be overstated that the completeness of imaging studies is mandatory. The odontoid process and the rostral aspect of T1 must be included in each evaluation. Patients with equivocal neurologic examinations must undergo some form of soft tissue evaluation. The literature comparing one method of screening to another should be evaluated carefully, as new imaging technologies will most likely supercede older technologies; and since no true gold standard exists, one must understand that a sensitivity and specificity that approximate 100% are ideal. We must, however, accept a lesser sensitivity and specificity, since many imaging findings are of minimal, if any, significance. Oversensitive examinations may result in unnecessary workups and treatments.
Hoffman J.R., Mower W.R., Wolfson A.B., et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
Holmes J.F., Mirvis S.E., Panacek E.A., et al. Variability in computed tomography and magnetic resonance imaging in patients with cervical spine injuries. J Trauma. 2002;53(3):524-529. discussion 530
Marion D. Determination of cervical spine stability in trauma patients (update of the 1997 EAST Cervical Spine Clearance document). Chicago: Eastern Association for the Surgery of Trauma; 2000.
Muchow R.D., Resnick D.K., Abdel M.P., et al. Magnetic resonance imaging (MRI) in the clearance of the cervical spine in blunt trauma: a meta-analysis. J Trauma. 2008;64(1):179-189.
Stiell I.G., Wells G.A., Vandemheen K.L., et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841-1848.
1. Grossman M.D., Reilly P.M., Gillett T., et al. National survey of the incidence of cervical spine injury and approach to cervical spine clearance in U.S. trauma centers. J Trauma. 1999;47(4):684-690.
2. Hoffman J.R., Mower W.R., Wolfson A.B., et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
3. Padayachee L., Cooper D.J., Irons S., et al. Cervical spine clearance in unconscious traumatic brain injury patients: dynamic flexion-extension fluoroscopy versus computed tomography with three-dimensional reconstruction. J Trauma. 2006;60(2):341-345.
4. Stiell I.G., Clement C.M., McKnight R.D., et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26):2510-2518.
5. Richards P.J., Summerfield R., George J., et al. Major trauma and cervical clearance radiation doses and cancer induction. Injury. 2008;39(3):347-356.
6. Stiell I.G., Wells G.A., Vandemheen K.L., et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841-1848.
7. Rethnam U., Yesupalan R., Gandham G. Does applying the Canadian Cervical Spine rule reduce cervical spine radiography rates in alert patients with blunt trauma to the neck? A retrospective analysis. BMC Med Imaging. 2008;8:12.
8. Marion D. Determination of cervical spine stability in trauma patients (update of the 1997 EAST Cervical Spine Clearance document). Chicago: Eastern Association for the Surgery of Trauma; 2000.
9. Marion D. Practice management guidelines for identifying cervical spine injuries following trauma. Chicago: Eastern Association for the Surgery of Trauma; 1998.
10. Ross S.E., Schwab C.W., David E.T., et al. Clearing the cervical spine: initial radiologic evaluation. J Trauma. 1987;27(9):1055-1060.
11. American College of Surgeons. Spine and spinal cord trauma. In ATLS: course for physicians, student manual, ed 7. Chicago: American College of Surgeons, 1997.
12. Bagley L.J. Imaging of spinal trauma. Radiol Clin North Am. 2006;44(1):1-12. vii
13. Nunez D.B.Jr., Zuluaga A., Fuentes-Bernardo D.A., et al. Cervical spine trauma: how much more do we learn by routinely using helical CT? Radiographics. 1996;16(6):1307-1318. discussion 1318–1321
14. Link T.M., Schuierer G., Hufendiek A., et al. Substantial head trauma: value of routine CT examination of the cervicocranium. Radiology. 1995;196(3):741-745.
15. Daffner R.H. Cervical radiography for trauma patients: a time-effective technique? AJR Am J Roentgenol. 2000;175(5):1309-1311.
16. Hashem R., Evans C.C., Farrokhyar F., et al. Plain radiography does not add any clinically significant advantage to multidetector row computed tomography in diagnosing cervical spine injuries in blunt trauma patients. J Trauma. 2009;66(2):423-428.
17. Sliker C.W., Mirvis S.E., Shanmuganathan K. Assessing cervical spine stability in obtunded blunt trauma patients: review of medical literature. Radiology. 2005;234(3):733-739.
18. Muchow R.D., Resnick D.K., Abdel M.P., et al. Magnetic resonance imaging (MRI) in the clearance of the cervical spine in blunt trauma: a meta-analysis. J Trauma. 2008;64(1):179-189.
19. Cooper D.J., Ackland H.M. Clearing the cervical spine in unconscious head injured patients: the evidence. Crit Care Resusc. 2005;7(3):181-184.
20. Benzel E.C., Hart B.L., Ball P.A., et al. Magnetic resonance imaging for the evaluation of patients with occult cervical spine injury. J Neurosurg. 1996;85(5):824-829.
21. D’Alise M.D., Benzel E.C., Hart B.L. Magnetic resonance imaging evaluation of the cervical spine in the comatose or obtunded trauma patient. J Neurosurg. 1999;91(Suppl 1):54-59.
22. Holmes J.F., Mirvis S.E., Panacek E.A., et al. Variability in computed tomography and magnetic resonance imaging in patients with cervical spine injuries. J Trauma. 2002;53(3):524-529. discussion 530
23. Stassen N.A., Williams V.A., Gestring M.L., et al. Magnetic resonance imaging in combination with helical computed tomography provides a safe and efficient method of cervical spine clearance in the obtunded trauma patient. J Trauma. 2006;60(1):171-177.
24. Barba C.A., Taggert J., Morgan A.S., et al. A new cervical spine clearance protocol using computed tomography. J Trauma. 2001;51(4):652-656. discussion 656–657
25. Insko E.K., Gracias V.H., Gupta R., et al. Utility of flexion and extension radiographs of the cervical spine in the acute evaluation of blunt trauma. J Trauma. 2002;53(3):426-429.
26. Anglen J., Metzler M., Bunn P., et al. Flexion and extension views are not cost-effective in a cervical spine clearance protocol for obtunded trauma patients. J Trauma. 2002;52(1):54-59.
27. Goodnight T.J., Helmer S.D., Dort J.M., et al. A comparison of flexion and extension radiographs with computed tomography of the cervical spine in blunt trauma. Am Surg. 2008;74(9):855-857.
28. Griffiths H.J., Wagner J., Anglen J., et al. The use of forced flexion/extension views in the obtunded trauma patient. Skeletal Radiol. 2002;31(10):587-591.
29. Ghanta M.K., Smith L.M., Polin R.S., et al. An analysis of Eastern Association for the Surgery of Trauma practice guidelines for cervical spine evaluation in a series of patients with multiple imaging techniques. Am Surg. 2002;68(6):563-567. discussion 567–568
30. Spiteri V., Kotnis R., Singh P., et al. Cervical dynamic screening in spinal clearance: now redundant. J Trauma. 2006;61(5):1171-1177. discussion 1177