Chapter 27 Esophageal-Tracheal Double-Lumen Airways
The Combitube and EasyTube
I Combitube
A Use of the Endotracheal Tube for Intubation and Ventilation
Rapid establishment of a patent airway to facilitate adequate ventilation during cardiopulmonary resuscitation (CPR) is the primary task of the rescuer. Mouth-to-mouth ventilation carries the disadvantages of possible gastric insufflation and the danger of aspiration. Endotracheal intubation remains the gold standard in airway maintenance, but this skill is acquired only after intensive training and requires constant practice. The people performing resuscitation procedures often are untrained in intubation, which is sometimes difficult or impossible even for skilled personnel.1 It requires good exposure of the patient’s airway, a skilled endoscopist, and equipment or facilities for intubation. Because the main objectives of airway management are ventilation and oxygenation, the need arises for a simple and efficient alternative to endotracheal intubation.2
B Use of the Esophageal Obturator Airway as an Alternative Airway Adjunct
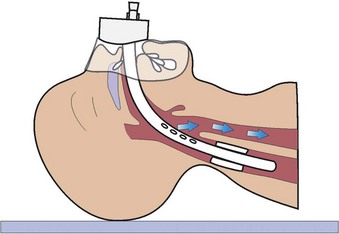
The esophageal obturator airway was constructed by Don Michael and colleagues as an alternative to using the endotracheal tube during emergency intubation.3 The esophageal obturator airway is a 34-cm-long tube with a balloon at its distal tip (Fig. 27-1). The balloon should lie below the level of the tracheal bifurcation after insertion. The distal end is blocked. Proximal to the balloon, there are 16 holes that are positioned in the region of the hypopharynx after positioning the airway. At the proximal end, a face mask is connected to the airway, sealing the mouth and nose during ventilation.
The esophageal obturator airway is inserted by first grasping the back of the patient’s tongue and the lower jaw with the thumb and index finger and then guiding the airway gently into the esophagus. The distal balloon is inflated to occlude the esophagus while the mask is pressed against the patient’s face. Air enters the proximal end and then enters the hypopharynx through perforations because the distal end is blocked. From there, air is forced over the opened glottis into the trachea because the mouth and nose are sealed by the mask and the esophagus by the balloon (see Fig. 27-1).
1 Testing and Trials of the Esophageal Obturator Airway
Subsequent physiologic testing and field trials of the esophageal obturator airway have been performed. Schofferman and colleagues evaluated the airway in 18 patients suffering from cardiac arrest,4 in whom resuscitation was performed by paramedics. Arterial blood gas analysis was obtained during ventilation with the esophageal obturator airway and subsequently with the endotracheal tube (ETT). There was little or no improvement in oxygenation after endotracheal intubation, implying that failure to oxygenate some patients did not result from the esophageal obturator airway.
Shea and associates compared two similar groups of patients during cardiopulmonary arrest with ventricular fibrillation5; 296 patients were intubated with an ETT or esophageal obturator airway. Survival rates and neurologic sequelae of survivors showed no statistically significant difference for the two groups. Hammargren and colleagues compared both devices after standardizing the method of oxygen delivery and ensuring true sampling of arterial blood.6 In 48 victims who had prehospital cardiac arrest, blood gases were sampled during ventilation with the esophageal obturator airway and subsequent ventilation with the ETT. There was no statistically significant difference between the two devices for the PaO2 and PaCO2 values. The investigators concluded that the esophageal obturator airway was an effective means of airway management, with the ventilation achieved equal to that of an ETT. Nevertheless, it soon became apparent from studies in the controlled environment of the operating room that considerable technical difficulties were associated with the esophageal obturator airway.7
2 Disadvantages of the Esophageal Obturator Airway
1. There are significant difficulties in obtaining a tight face mask seal and maintaining the seal during transportation. Effective use requires at least two hands to seal the mask. Obtaining an adequate mask fit is particularly difficult in edentulous or bearded patients.6,7
2. Inadvertent or unrecognized tracheal intubation may occur.8 The patient’s airway is completely obstructed, and attempts at repositioning are usually unsuccessful.
3. Esophageal or gastric ruptures have been reported.9–12 Ruptures of the esophagus or the stomach may be due to the length of the esophageal obturator airway. Because many cardiac arrest patients exhibit left atrial dilatation with subsequent lateral deviation of the lower half of the esophagus, the esophageal obturator airway may be forced in a left lateral direction in addition to the curved sagittal direction, which can lead to ruptures.
C Development of the Combitube Esophageal-Tracheal Double-Lumen Airway
The previously described disadvantages and the idea that both tracheal and esophageal intubation allow ventilation and oxygenation led to the development of the Combitube. It was devised by Michael Frass in cooperation with Reinhard Frenzer and Jonas Zahler in Mödling and Vienna, Austria.13–17
The Combitube design was intended to deal effectively with the problem of managing the airway with the greatest success possible. Studies in large populations demonstrate that the Combitube provides a much better chance of ventilation and oxygenation than other devices18–21 by isolating and protecting the airway from digestive regurgitation and aspiration.22 The Combitube can be used when airway management is difficult independent of the cause, such as anatomic factors, the patient’s position with respect to the operator, space and illumination restrictions, and presence of a full stomach. The Combitube does not need special equipment, energy, or complex techniques to be properly used. Because the Combitube is available in only two sizes (37 and 41 F), no time is lost in selecting the proper size among many alternatives.
D Technical Description
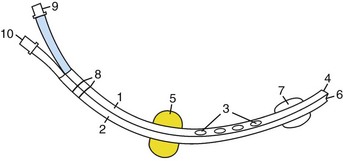
The Esophageal Tracheal Combitube (Combitube; Tyco Healthcare, Mansfield, MA) is a device for emergency intubation that combines the functions of an esophageal obturator airway and a conventional ETT (Fig. 27-2). The Combitube is a double-cuff and double-lumen tube (Fig. 27-3). The oropharyngeal balloon is located at the middle portion of the tube and the tracheoesophageal cuff is located at the distal end.23 The lumens are separated by a partition wall. Proximally, both lumens are opened and linked by short tubes with universal connectors. Distally, the pharyngeal lumen is blocked and has eight perforations at the level between the cuffs, and the tracheoesophageal lumen is open. This design allows ventilation when the Combitube is positioned in the esophagus through the perforations of the pharyngeal lumen and in the trachea through the opened distal end of the tracheoesophageal lumen. The pharyngeal balloon seals the oral and nasal cavities after inflation. Printed ring marks proximal to the oropharyngeal balloon indicate the limit of insertion.
The 37-F Small Adult (SA) Combitube may be used in patients 4 to 6.5 ft tall.18,24,25 The 41-F model is used in patients taller than 6 ft (with some overlap with the SA model). The 37-F SA Combitube usually is the preferred model because it works well in patients up to 6.5 ft tall.
E Insertion Techniques
1 Conventional Technique
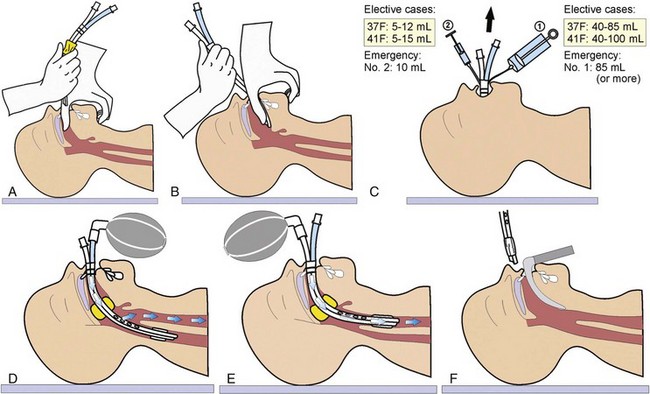
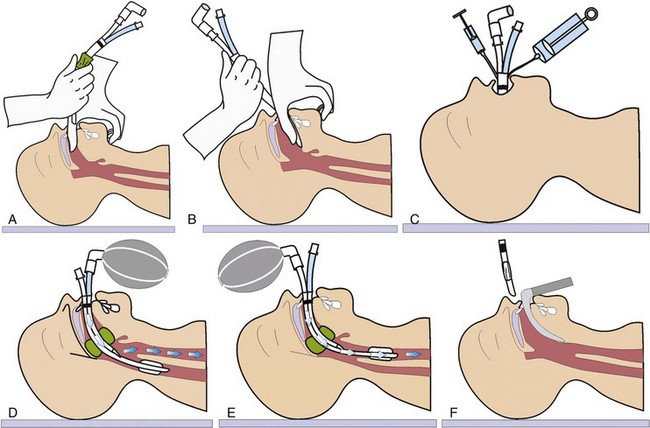
With the operator behind the patient’s head, the lower jaw and tongue are lifted by the thumb and index finger. The tongue is pressed forward by the thumb, and the tube is inserted in a curved downward movement until the printed ring marks lie between the teeth or the alveolar ridges in edentulous patients (Fig. 27-4A). The insertion should be performed along the tongue to avoid potential damage of the posterior pharyngeal mucosa. Sometimes, a rocking motion may alleviate problems encountered with insertion. Next, the oropharyngeal balloon is inflated with up to 85 mL of air for the 37-F SA Combitube (or up to 100 mL for the 41-F Combitube) through port no. 1 with the blue pilot balloon using the large syringe with the blue color code (see Fig. 27-4B). When the minimal-volume technique is used, enough air is added to inflate the balloon and obtain a seal (see “General Anesthesia”), or a cuff pressure gauge may be used to achieve a seal of 60 mm Hg. If sufficient sealing of the mouth and nose cannot be accomplished, the oropharyngeal balloon may be filled with an additional 50 mL of air, up to a total amount of 150 mL.26
During inflation, the tube may move slightly out of the patient’s mouth because of the self-positioning properties of the balloon. A useful sign indicating malposition due to insufficient insertion is that the inflated pharyngeal balloon can be seen when looking into the patient’s mouth (Fig. 27-5). If this occurs, the pharyngeal balloon should be deflated, and the tip’s position should be reevaluated. The Combitube may become kinked during placement, and reinsertion may be necessary. The anatomic relationships of the oropharyngeal balloon have been demonstrated radiologically.26 The balloon protrudes in an oral direction after overinflation so that it does not close the epiglottis. Figure 27-6 shows a cross-sectional magnetic resonance imaging (MRI) view of the Combitube in the esophageal position. It displays anterior movement of the larynx, a situation that can often be observed clinically. Knowledge of this may facilitate subsequent location of the larynx for endotracheal intubation.

Figure 27-5 Seeing the inflated oropharyngeal balloon in the patient’s mouth indicates malposition of the Combitube.

Figure 27-6 Cross-sectional MRI view of a patient intubated with Combitube in the esophageal position.
(Courtesy of B. Panning, MD, Department of Anesthesiology, and C. Ehrenheim, MD, Department of Nuclear Medicine and Special Biophysics, Hannover School of Medicine, Hannover, Germany.)
The distal balloon is then inflated with 10 mL of air through port no. 2 with the white pilot balloon and using the small syringe.27 With blind insertion, there is a high probability that the tube will be placed into the esophagus. Test ventilation is recommended through the longer, blue no. 1 tube leading to the esophageal lumen (see Fig. 27-4C). Air passes into the pharynx and then through the glottis into the trachea because the mouth, nose, and esophagus are blocked by the balloons. Auscultation of breath sounds in the absence of gastric insufflation confirms adequate ventilation when the Combitube is in the esophagus. Ventilation is then continued through this lumen. In this position, the Combitube allows closed suctioning and active decompression of the stomach.28 Closed suctioning provides the advantage of reduced cross contamination between the bronchial system and gastric juices.29 Gastric contents can be suctioned through the unused tracheoesophageal lumen with the help of a small suction catheter (10 or 12 F) included in the kit.
The most common cause of failed ventilation through the blue connector is a tracheal position of the distal tip (see Fig. 27-4D). Without changing the position of the Combitube, ventilation is changed to the shorter, transparent no. 2 tube leading to the tracheoesophageal lumen, and the position is again confirmed by auscultation. Ventilation is then carried out through the tracheoesophageal lumen directly into the trachea. The oropharyngeal balloon may be deflated in case of regurgitation to allow suctioning with a conventional catheter. Otherwise, the balloon should remain inflated to stabilize the Combitube.
If no breath sounds are heard over the lungs or a capnographic curve is absent while ventilating through the blue connector, the second most common cause is that the Combitube has been inserted too deeply, and the oropharyngeal balloon lies just opposite the laryngeal aperture and occludes the airway.30 In this situation, both balloons should be deflated and the Combitube pulled back about 2 to 3 cm out of the patient’s mouth and then fixed in this position.
The third most common cause of failed ventilation is a phenomenon (e.g., laryngospasm, bronchospasm, pulmonary edema) leading to high airway pressure. In this situation, cause should be identified and treated. Unlike other airway devices, the Combitube allows ventilation against high airway pressure, and administration of inhaled bronchodilators28,31 and proper treatment of the spastic phenomenon can be started immediately after full inflation of the balloon to ensure high-pressure ventilation.
An investigation by Wafai and coworkers was designed to test the reliability of the self-inflating bulb in identifying the location of the Combitube and facilitating its proper position in anesthetized patients.32 In group 1 (n = 26), the Combitube was introduced blindly. In group 2 (n = 20), the tube was placed in the trachea (8 patients) or once in the trachea and once in the esophagus randomly (12 patients) under direct vision rigid laryngoscopy by the anesthesiologist performing the intubation. In both groups, the efficacy of the self-inflating bulb in identifying the location of the Combitube was tested by a second blinded anesthesiologist. In group 1, blind insertion of the Combitube resulted in esophageal placement in all patients, and in each case, it was correctly identified. The second anesthesiologist reported no reinflation when the compressed self-inflating bulb was connected to the distal lumen. When the compressed self-inflating bulb was connected to the proximal lumen, instantaneous reinflation was observed in 23 patients, delayed reinflation (2 to 4 seconds) in 2, and no reinflation (>4 seconds) in 1. Instantaneous reinflation occurred in these three patients after repositioning the Combitube. In group 2, the second anesthesiologist correctly identified the location of the Combitube in all cases. The results confirm previous findings that blind introduction of the Combitube leads to esophageal placement and yields adequate ventilation. The self-inflating bulb can quickly identify the location of the Combitube and facilitate its positioning with the use of a simple algorithm. This can be important if the Combitube is used in a patient whose lungs cannot be ventilated by mask and whose trachea cannot be intubated.
2 Alternative Insertion Technique
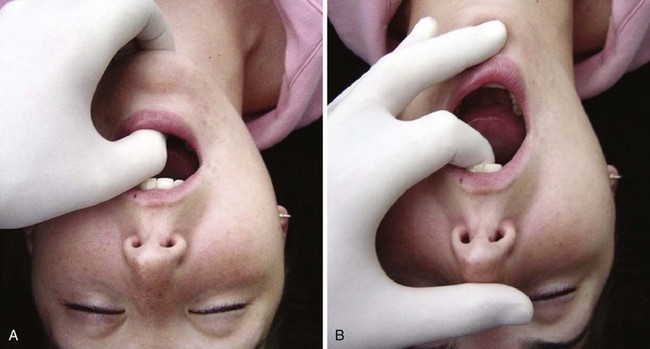
Another way of inserting the Combitube has been described by Urtubia and colleagues.33 This insertion technique (Fig. 27-7A and B) consists of grasping the upper teeth or the upper alveolar ridge with the index finger while pushing the chin with the middle finger. To avoid contact of the tip of the Combitube with the posterior oropharyngeal wall, Urtubia recommends keeping the Combitube bent as long as possible before blind insertion.33 Similarly, Urtubia and associates describe a modification of the Lipp maneuver for blind insertion of the Combitube.34
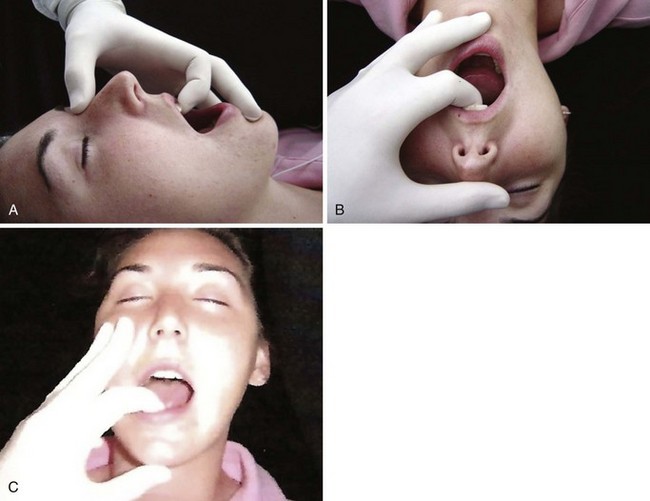
Figure 27-7 A and B, New insertion technique as described by Urtubia and coworkers.33 C, Alternative insertion technique.
(Courtesy of Carin Hagberg, MD, Houston, TX.)
For patients in sitting and prone positions or when the operator is facing the patient, a similar technique can be useful. The index finger grasps the lower teeth or alveolar ridge while the middle finger pushes the cheek (see Fig. 27-7C). The enlarged interincisor distance allows easier insertion of the Combitube, especially in partially edentulous patients and in patients with a limited oral opening (Fig. 27-8A and B). As with the original technique, it does not require any cervical movement, which makes it suitable for patients with cervical spine trauma.
The Combitube may be inserted blindly or with the aid of a laryngoscope. Use of a laryngoscope is recommended during the initial training period when endotracheal intubation using laryngoscopy fails (i.e., insert the Combitube with the laryngoscope still in place) and when blind insertion of the Combitube fails.28
F Indications, Advantages, and Complications
1 Out-of-Hospital Emergency Intubation
The Combitube is especially suitable for emergency intubation in and out of the hospital when endotracheal intubation is not immediately possible. It may be used in the following three situations. First, in patients with difficult anatomy (e.g., bull neck, lockjaw, small mouth opening), the Combitube can be inserted in those with an interincisor distance (i.e., oral aperture) as small as 15 mm.35 Second, the Combitube can be inserted in difficult spatial circumstances, such as limited access to a patient’s head when the patient lies on the floor in a small room, when the patient is lying with his head close to the wall in the general ward or in the intensive care unit (ICU) with many lines at the side impeding quick access to the head, or when a patient is trapped in a car after an accident. Third, the Combitube can be inserted despite challenging illumination, such as bright light, massive bleeding, or regurgitation that can inhibit direct laryngoscopy. The Combitube prevents aspiration, which may occur with repeated suction maneuvers or vomiting.22,24,36
2 Elective and Emergency Surgery
a General Anesthesia
Use of the Combitube is indicated in routine surgery in patients for whom conventional intubation is not mandatory, such as singers and actors who may be afraid of damage to the vocal cords by endotracheal intubation, or in patients with rheumatoid arthritis with atlantoaxial subluxation. The main advantages of the Combitube in elective and emergency surgery are higher insertion and ventilation rates, reliable protection of the airway against regurgitation and aspiration of gastric contents (e.g., patients with a full stomach, gynecologic laparoscopy), and ventilation and oxygenation against high airway pressures (e.g., obesity, laryngospasm, bronchospasm). As with emergency intubation, it is especially suitable in patients with difficult anatomic conditions. When endotracheal intubation cannot be performed immediately, the Combitube should be considered (Box 27-1). The main advantage in the case of failed intubation or ventilation is immediate esophageal insertion of the Combitube under direct vision without removing the laryngoscope.
Box 27-1 Suggested Indications for Use of the Combitube in Anesthesia and Emergencies
1. The patient’s head does not have to be placed in the traditional sniffing position, as recommended for conventional endotracheal intubation. The patient’s head should remain in a neutral position that allows free movement of the lower jaw. Depending on the situation, the chin may be pushed toward the patient’s chest. Some clinicians prefer to extend the head or to use a small cushion. In patients with a cervical spine injury, the Combitube allows airway management while avoiding mobilization of the neck.
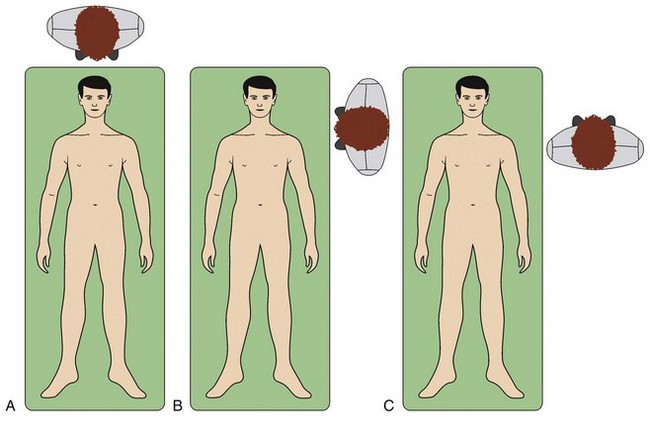
2. The position of the operator (Fig. 27-9) may be behind the patient, especially when a laryngoscope is used (see Fig. 27-9A); to the side of the patient’s head (see Fig. 27-9B); or face to face, when the operator stands beside the patient’s thorax and faces the patient (see Fig. 27-9C). In all three positions, it is necessary to insert the Combitube with a curved downward-caudal movement.
3. During elective surgery, it is always necessary to achieve an adequate depth of anesthesia, with or without additional relaxation. One half of the intubating dose of a neuromuscular blocking agent may be enough to ensure a smooth insertion.18 Gaitini and colleagues have used the Combitube in patients with controlled mechanical ventilation and in spontaneously breathing patients without relaxation.18 However, grasping and elevating the epiglottis with the fingers during insertion may reduce the need for relaxation.
4. Recommended induction agents are propofol or sevoflurane, with or without opioids.37 In a study of 50 female patients undergoing gynecologic laparoscopy, Urtubia and associates successfully inserted the Combitube in 100% of cases using inhalational induction with sevoflurane as the sole agent,38 without opioids or neuromuscular blockade. Use of a laryngoscope is recommended to avoid damage to the oral and pharyngeal mucosa. Nevertheless, with a well-performed blind insertion technique and an adequate level of anesthesia, the risk of damage is comparable to that with the laryngeal mask airway (LMA) or the ETT in terms of postoperative sore throat (16% to 25%).18,24,27 With the laryngoscope, the Combitube is then intentionally introduced into the esophagus. When endotracheal intubation fails, a Combitube can be placed under direct visualization with the laryngoscope still in the patient’s mouth.
5. Another method that may facilitate Combitube insertion and minimize insertion trauma is warming the Combitube in a bottle of warm saline or water, similar to the procedure performed with an ETT for nasal intubation. This technique also allows Combitube insertion without additional application of lubricant.
6. The minimal-volume technique should be applied in elective cases and in emergencies after stabilization of the patient. Studies have shown that adequate sealing of the oropharyngeal balloon can be achieved with 40 to 85 mL of air for the SA Combitube.18,24,27,38–41 Gaitini and colleagues reported that the mean inflation volume of the oropharyngeal balloon at which an air leak was first observed was 45.5 ± 12.3 mL for the 37-F Combitube and 48.1 ± 12.1 mL for the 41-F Combitube.40 The balloon should be initially filled with 40 mL of air only. If a tight seal can be achieved as evaluated by auscultation, comparable to inspiratory and expiratory tidal volumes and the flow-volume curve, the volume is not increased. If a leak is observed, additional increments of 10 mL of air each are added into the balloon until a tight seal is confirmed. The volumes of the oropharyngeal balloon also must be adjusted with the use of nitrous oxide and volatile anesthetics.
b Awake Intubation
In an experiment on himself, Panning showed that the Combitube can be inserted easily with local pharyngeal anesthesia.42 Keller and coworkers inserted the Combitube in four awake volunteers with topical anesthesia.43 Nevertheless, unless an urgent insertion is required, the Combitube should always be inserted when gag reflexes are suppressed because of the risk of mucosal damage or vomiting.
c Replacement of the Combitube
The Combitube may be left in place for up to 8 hours.44 Although emergency and routine surgical procedures may be successfully carried out during this period, the Combitube is not intended for long-term ventilation, because the pressure on the pharyngeal mucosa may be harmful. We recommend replacing the Combitube after a maximum duration of 8 hours. Replacement of the Combitube in the esophageal position by an ETT can be performed in several ways with no danger of aspiration:
1. While the distal cuff remains inflated, deflate the oropharyngeal balloon completely, with the Combitube remaining in the esophagus. Displace the Combitube to the left corner of the mouth, and insert an ETT by laryngoscopy or fiberoptic intubation.45 After successful placement of the ETT, insert a suction catheter through the tracheoesophageal lumen into the esophagus, and during continuous suctioning, deflate the distal cuff, and remove the Combitube. If ETT insertion is impossible, push the Combitube back into its original midline position, reinflate the oropharyngeal balloon, and continue ventilating through the longer no. 1 lumen (blue) of the Combitube until the next endotracheal intubation attempt or until a surgical airway is established.
2. Gaitini and associates described another method.46 The oropharyngeal balloon is partly deflated according to the minimal-volume technique so that the least amount of air allows adequate sealing of the oral and nasal cavities. During continued ventilation through the no. 1 lumen, a fiberoptic bronchoscope mounted with an ETT is introduced through the patient’s mouth. Without a time limit, the bronchoscope may be advanced into the trachea. The unique feature of this method is that ventilation is not interrupted during the entire replacement procedure. All the patients in this study had Mallampati class III or IV oral cavity anatomy.
3. The Combitube may be replaced by surgical means, such as cricothyrotomy or tracheostomy.47 These were the first surgical procedures performed with the Combitube. An advantage of this method is that the trachea is not occupied by an ETT, and ventilation can be continued while the surgical airway is established. A disadvantage is that the trachea is not protected against aspiration of blood generated during the surgical procedure.
4. If there is no danger of aspiration, the Combitube may be removed and replaced by conventional means (e.g., laryngoscopy, bronchoscopy). This approach may be advantageous because intubation around the Combitube can be difficult. In a cadaver study, the laryngeal view with and without the Combitube in place has been compared and the difficulty of intubation around the device evaluated.48 Nine participants in an airway workshop placed 37-F Combitubes in eight non-embalmed cadavers. The pharyngeal balloon was deflated and laryngoscopy attempted with the Combitube in place. Each operator assessed the percentage of glottic opening (POGO) score and tried to pass a tracheal tube around the device. Difficulty of tube passage was rated by the operator. The Combitube was then removed and laryngoscopy (and POGO scoring) repeated without the device. POGO scores with and without the Combitube averaged 61% (95% confidence interval [CI], 49% to 73%) and 92% (CI, 89% to 95%), respectively. Fourteen (19%) of 72 intubation attempts with the Combitube failed. Major difficulty was reported for 22 (31%) of 72 attempts, and minor difficulty for 34 (47%) of 72. The investigators concluded that a previously placed Combitube significantly worsened the laryngeal view at laryngoscopy and prevented intubation in 19% of cases in this cadaver study. They suggest that removal of the Combitube is warranted if any difficulty with laryngoscopy is anticipated or encountered.
5. Harrison and colleagues described the successful replacement of the Combitube with an ETT by retrograde intubation.49 The retrograde intubation was successfully performed without removing an in situ Combitube.
6. A Combitube in the tracheal position can be replaced by an ETT. After lubrication, a pediatric (8-F) tracheal tube exchanger (Cook Critical Care, Bloomington, IN) is introduced into the tracheoesophageal lumen through the shorter no. 2 lumen (transparent) into the trachea, the Combitube is removed, and an ETT is advanced using the tube exchanger as a guide.50,51 If not contraindicated, laryngoscopy should be performed, to facilitate advancement of the ETT through the glottis.
3 Advantages
The Combitube has a wide range of applications and advantages (Box 27-2). Those benefiting from its use include anesthesiologists and physicians in emergency departments,18,19,23 paramedics and emergency medical technicians,19,50,52–57 combat medics,58 parkmedics,59 and physicians in private practice (e.g., responding to anaphylactic reactions).28,31 Cardiac arrests usually do not occur under ideal circumstances, and CPR often is performed in awkward locations, poorly lighted areas, and with limited access to the patient’s head. Because the Combitube can be inserted without a laryngoscope, establishment of a patent airway is not hampered by adverse environmental factors or staff unskilled in endotracheal intubation.27 It is safe against aspiration, and high ventilatory pressures may be applied.
Box 27-2 Advantages of the Combitube and EasyTube
• Noninvasive compared with cricothyrotomy
• Universal size (37-F Small Adult Combitube fits patients 4 to 6.5 ft)18,23,104
• Universal model (one type only)
• Easy to learn, even by untrained personnel58,68,110,129,130
• No preparations necessary; tube and syringes are ready to use
• Helpful under difficult conditions of space and illumination
• Simultaneous fixation after inflation of the oropharyngeal balloon
• Works in the tracheal or esophageal position
• Active decompression of the esophagus and stomach
• Minimized risk of aspiration22,36,38,57,101,106
• Controlled mechanical ventilation possible at high ventilation pressures (≤50 cm H2O)19,24,27,36,51,93,101
• Independent of power supply (e.g., batteries of laryngoscope)
• Well suited for obese patients76,140
• May be used in paralyzed patients who cannot be intubated or mask ventilated
• Only device for insertion in patients with trismus and limited mobility of cervical spine and those with combined pathologic conditions, such as trismus plus limited mobility of the spine and trismus plus tongue edema129
• Fast, safe, and easy to use with successful skill retention129,130
There is no need for additional fixation of the Combitube after inflation of the oropharyngeal balloon, because the anterior upper wall of the oropharyngeal balloon lies just behind the posterior end of the hard palate, thereby guaranteeing strong anchoring during ventilation and transportation. Providing a more secure airway is an attractive advantage of the Combitube compared with other devices used during transportation of emergency patients. Studies have shown that the Combitube is easy to learn and that the skills are retained over time.57
4 Disadvantages
A potential disadvantage of the Combitube is that suctioning tracheal secretions is impossible in the esophageal position. However, studies of use of the esophageal obturator airway in cardiac arrest patients have shown that the outcome of those cases is not statistically different compared with cases in which endotracheal intubation is used.5,6 The Combitube is designed to bridge the short gap between the prehospital setting and admission of the patient to the emergency department. If prolonged ventilation is required, glycopyrronium bromide may be administered to suppress tracheal secretions (e.g., during surgery). Krafft and colleagues have described a redesigned Combitube in which two proximal anterior holes are replaced by one large hole, allowing a bronchoscope to pass for inspection and suctioning of the trachea and as a means for replacing the Combitube using a guidewire.60
6 Complications
Ovassapian and coworkers observed livid discoloration of the tongue during ventilation with the Combitube in a few patients without further sequelae.45 Tongue engorgement was described after 4 hours of Combitube use.61 In an out-of-hospital study with paramedics as rescuers, two lacerations of the esophagus were found in autopsies of cardiac arrest patients ventilated with the Combitube.62 However, the investigators found that the distal cuff was overfilled with 20 to 40 mL of air (instead of 10 ± 1 mL). As outlined in the instructions, the Combitube should not be advanced with use of force. Klein and associates reported an esophageal rupture after insertion of a Combitube, stiff suctioning catheter, LMA, laryngoscope, and ETT.35 A traumatic procedure with one or more of these devices probably caused the complication.
Overinflation of the esophageal balloon was described in a case reporting airway obstruction secondary to tracheal compression. In this case, the esophageal balloon was inflated with 22.4 mL according to the computed tomography (CT) measurement.63 Richards reported a case of piriform sinus perforation during the insertion of the Combitube.64 This patient presented with cardiorespiratory arrest due to angioedema, probably caused by treatment with angiotensin-converting enzyme inhibitors. Another case of piriform sinus perforation during Combitube placement was reported by Moser.65
Oczenski and coworkers reported a very high number of complications for cases of elective surgery.66 The total complication rate found by Oczenski’s group66 was fourfold that found in the studies led by Gaitini,18 Hartmann,27 and Urtubia.24 This unexpectedly high rate of complications probably was caused by traumatic maneuvers during airway management, which is in accordance with an 8% rate of pharyngeal hematoma associated with the LMA. Vezina and colleagues retrospectively reviewed medical records of patients with cardiac or respiratory arrest.67 The study was performed in the Quebec City Health Region, where paramedics use the Combitube as a primary airway device for patients with cardiorespiratory arrest. A high incidence of complications was reported.
The study of Oczenski and coworkers demonstrates that all precautions should be considered when there are obvious handling problems.66 When facing difficulties during insertion, a laryngoscope should be used immediately to insert the Combitube intentionally into the esophagus under direct vision.
G Medical Literature
1 Combitube in Cardiac Arrest Patients
a IN-Hospital Studies
Application of the Combitube during CPR has been investigated.14–1621 The first study consisted of two parts.15 The first part considered the blood gas analyses of 19 patients after 15 minutes of ventilation with the Combitube. In the second part, the blood gas analyses of samples taken from 12 patients during ventilation with the Combitube were compared with those taken during subsequent ventilation with a conventional ETT. Blood gas analyses showed higher arterial oxygen pressures with the Combitube than with an ETT (124 ± 33 versus 103 ± 30 mm Hg; P = 0.001). Carbon dioxide pressure was not significantly different.
A second study reported the use of the Combitube during in-hospital CPR.14 In a randomized sequence, the Combitube or a conventional ETT was used in 43 patients. After stabilization of the patients, each tube was replaced with the other type of tube. Blood gas analyses revealed increased oxygen tensions during Combitube ventilation, and the intubation time was significantly shorter with the Combitube.
Another study evaluated the safety and effectiveness of the 41-F Combitube as used by ICU nurses under medical supervision compared with an ETT established by ICU physicians during CPR.68 The intubation time was shorter for the Combitube, and results of blood gas determinations for each device were comparable, although arterial oxygen tension was slightly higher during ventilation with the Combitube. The study suggests that the Combitube as used by ICU nurses is as effective as the ETT as used by ICU physicians during CPR.
b Out-of-Hospital Studies
Atherton and Johnson investigated the ability of paramedics in a nonurban emergency medical setting to use the 41-F Combitube.52 Fifty-two cases of prehospital Combitube insertion by paramedics were examined, and 11 paramedics were evaluated for skill retention. Combitube insertion was attempted in 52 cardiac arrest patients in a prehospital setting, and 69% of them were intubated successfully. Paramedics recognized esophageal versus tracheal placement in 100% of cases. The Combitube was inserted successfully in 64% of patients who could not be tracheally intubated by direct visualization. The Combitube was inserted successfully in 71% of cases when used as a first-line airway adjunct. Fifteen months later, a follow-up study of 9 of 11 randomly selected paramedics demonstrated inadequate skill retention (e.g., improper insertion angle resulting in resistance and inability to insert the tube, inappropriate inflation of the balloons, insertion too deep or not deep enough). After this reevaluation and retraining, the success rate rose to almost 100%.69 These results demonstrate that as with every device, there is a necessity for a reevaluation of skills after initial training. A study of emergency medicine residents suggests that they can learn and retain these airway skills.70
In a prehospital setting, three alternative airway devices and an oral airway were compared in a modified, randomized, crossover study by emergency medical assistants who were not trained in advanced life support (ALS) techniques.20 The pharyngeal-tracheal lumen (PTL) airway, the LMA, and the 41-F Combitube were compared objectively for success of insertion, ventilation, and arterial blood gas and spirometry measurements performed on arrival at the hospital. Subjective assessment was carried out by emergency medical assistants and receiving physicians. Operating room training was performed only with the LMA. Autopsy findings and survival to hospital discharge were analyzed. The study took place in four non-ALS communities over 4.5 years and involved 470 patients in cardiac or respiratory arrest, or both. Emergency medical assistants had automatic external defibrillator training but no endotracheal intubation skills. Successful insertion and ventilation was highest for the Combitube (86% versus 82% with PTL airway and 73% with LMA, P = 0.048). Differences in subjective evaluation were significant. The Combitube was associated with the fewest problems with ventilation, and it was preferred by most emergency medical assistants. Unlike LMA use, no aspirations were found in autopsies after use of the Combitube.
A retrospective study was designed to determine the choice of airway devices used for nontraumatic,21 out-of-hospital cardiac arrest patients and to evaluate the success and failure of insertion and airway control or ventilation by three airway adjuncts—the 41-F Combitube, the esophageal-gastric tube airway (EGTA), and the LMA—which were used in conjunction with the bag-valve-mask ventilation by emergency life-saving technicians in Japan. A survey of 1079 technicians was performed to identify the type of airway devices, the success rates of airway insertion, the effectiveness of airway control/ventilation, and associated complications in 12,020 cases of cardiac arrest. The choice of airway devices included bag-valve-mask ventilation for 7180 cases, EGTA for 545 cases, Combitube for 1594 cases, and LMA for 2701 cases. Successful insertion rates on the first attempt were 82.7% for EGTA, 82.4% for Combitube, and 72.5% for LMA (P = 0.0001). Rates of failed insertion were 8.2% for EGTA, 6.9% for Combitube, and 10.5% for LMA (P = 0.0001). Successful ventilation rates were 71.0% for EGTA, 78.9% for Combitube, and 71.5% for LMA (P = 0.0004). Six cases of aspiration were reported in the LMA group, whereas nine cases of soft tissue injuries, including one esophageal perforation, were reported in the 41-F Combitube group; 17.8% had vomited before or during airway placement. The Combitube appears to be the most appropriate choice among the airway devices examined.
The ability to train emergency medical technicians with defibrillation capabilities (EMT-Ds) to effectively use the 41-F Combitube for intubations in the prehospital environment was evaluated in a prospective field study lasting for 18 months.71 Indications for use of the Combitube included unconsciousness without a purposeful response, absence of the gag reflex, apnea or a respiratory rate of less than 6 breaths/min, age older than 16 years, and height of at least 5 ft. Twenty-two EMT-D provider agencies involving approximately 500 EMT-Ds were included as study participants. Combitube insertions were attempted in 195 patients in cardiorespiratory arrest in a prehospital setting. An overall successful intubation rate of 79% was observed, with identical success rates for medical and trauma patients. The device was placed in the esophagus in 91% of cases. Resistance during insertion was the major reason for unsuccessful Combitube intubations. The overall hospital admission rate was 19%. No complications were reported. The study confirmed that EMT-Ds could be trained to use the Combitube as a means of establishing an airway in patients in the prehospital setting.
Rural EMTs were educated in selected advanced skills, and the safety and effectiveness of practice were evaluated.55 After a minimum of 72 hours of training, EMTs employed three skills (i.e., Combitube insertion, glucometry, and automated external defibrillation) and seven medications (i.e., albuterol, nitroglycerin, naloxone, epinephrine, glucagon, activated charcoal, and aspirin). Congruence between prehospital assessment and emergency department diagnosis was assessed, along with correct use of airway skills (18 of 36 months). The Combitube functioned satisfactorily in 15 (79%) of 19 cases, and EMTs always correctly found the correct lumen to ventilate.
The purpose of another study was to assess the feasibility, safety, and effectiveness of the Combitube when used by EMT-Ds in cardiorespiratory arrest patients of all causes.72 The EMTs had automatic external defibrillator training but no prior advanced airway technique skills. The prehospital intervention was reviewed using the EMTs cardiac arrest report, the automatic external defibrillator tape recording of the event, and the assessment of the receiving emergency physician. Hospital records and autopsy reports of 831 adult, cardiac arrest patients were reviewed in search of complications. Placement was successful in 725 (95.4%) of the 760 patients in whom Combitube insertion was attempted, and ventilation was successful in 695 (91.4%) patients. An autopsy was performed in 133 patients, and no esophageal lesions or significant injuries to the airway structures were observed. Results suggest that EMT-Ds can use the Combitube for control of the airway and ventilation in cardiorespiratory arrest patients safely and effectively. In other field studies investigating the best time for postshock analysis after out-of-hospital defibrillation with automated external defibrillators, 86 (93.7%) of 96 patients were successfully intubated with the Combitube.53,73 Similar results were found in a study by Cady and Pirrallo, who found a success rate of 89.4% for 860 Combitube insertions performed by paramedics experienced in endotracheal intubation.74
Mort reviewed an emergency intubation database to determine what airway devices were used as a backup to rescue the primary rescue device failures.75 The bougie and the LMA have intrinsic failure rates. In each of the 18 patients, the Combitube was placed in the esophagus with no tracheal insertions identified. Carbon dioxide detection confirmed tracheal air exchange in each case. Minor adjustments were required to optimize the air exchange with the Combitube in nine cases and involved moving the Combitube distally (deeper) or proximally (shallower). Four of the 18 patients required a second attempt of Combitube placement when ventilation was obstructed despite repositioning (i.e., presumed epiglottic impingement by Combitube). After Combitube placement, effective ventilation and life-sustaining oxygen saturations (>92%) were established and maintained in each case until further steps were taken to secure the airway. Steps required to secure the airway (tracheal intubation) after successful placement of the Combitube varied. Eleven patients were tracheally intubated with the Combitube maintained in the esophageal position (i.e., direct laryngoscopy alone in four patients and direct laryngoscopy and bougie-assisted tracheal intubation in seven patients). Because of the poorly recognized periglottic anatomy with the Combitube in place, two patients had the Combitube exchanged to a Fastrach LMA as a successful intubation conduit. Five patients had unrecognizable periglottic anatomy due to excessive edema, significant secretions, and tissue trauma and therefore had a surgical airway created with the Combitube supporting ventilation and oxygenation (i.e., four cases in the emergency department and one general ward patient transported to the operating room for surgical airway procedure). The Combitube, commonly used in the emergency prehospital setting, appeared to be a useful secondary rescue device in the hospital setting when the bougie and LMA failed.
c Case Reports
Liao and Shalit reported a case of successful Combitube treatment of an acute respiratory arrest caused by an acute asthma exacerbation.59 A level II EMT (National Park Service Parkmedic) used this device.59 The female patient was successfully intubated and ventilated and was flown by helicopter for more than 2 hours. Despite repeated episodes of vomiting, no aspiration occurred in this patient. The Combitube was replaced by an ETT, and the patient was extubated 2 days later and discharged on day 3 after the initial event.
The Combitube was helpful in a bull-necked patient when movement of the neck and opening of the mouth were impossible and in the case of a rapidly enlarging cervical hematoma,76,77 which caused upper airway obstruction and required immediate intubation after endotracheal intubation had failed because the epiglottis could not be visualized with a laryngoscope.78
In Chile, a 65-year-old woman with chronic renal insufficiency and atrial fibrillation experienced sudden respiratory arrest during the dialysis procedure at an out-of-hospital dialysis center. Ventilation with a face mask was impossible. As the patient’s condition rapidly deteriorated, a nonskilled nurse reestablished her oxygenation by blind insertion of a Combitube.79
For a patient with acute respiratory failure,22 attempts at endotracheal intubation failed due to continued vomiting that rendered fiberoptic visualization of the vocal cords impossible. Blind insertion of the Combitube led to successful ventilation, and replacement by an endotracheal airway was performed without danger of aspiration.
2 Combitube in Trauma Patients
a Studies
Blostein and colleagues have prospectively studied use of the Combitube in trauma patients in whom orotracheal rapid-sequence intubation (RSI) failed.80 Flight nurses were trained in the use of the Combitube by mannequin simulation, videotape review, and didactic sessions. Combitube insertion was attempted after failure of two or more attempts at orotracheal RSI. Over a 12-month period, 12 patients had successful Combitube insertion, and 10 cases qualified for review. Injuries, number of failed orotracheal RSI attempts, definitive airway control, initial arterial blood gas results, and outcome were recorded. Combitube insertion was successful in all 10 patients in whom placement was attempted. Definitive airway control was achieved by conversion to orotracheal intubation in seven patients, emergency department cricothyroidotomy in one patient, and operative room tracheostomy in two patients. No patient died because of failure to control the airway. Seven patients requiring Combitube had mandible fractures, four had traumatic brain injuries, two had facial fractures, and one had hemopneumothorax. Data suggest that Combitube insertion is an effective method of airway control in trauma patients who fail orotracheal RSI. It may be particularly useful in the patient with maxillofacial trauma and offers a practical alternative to surgical cricothyroidotomy in difficult airway situations.
The ability of paramedic RSI to facilitate intubation of patients with severe head injuries in an urban out-of-hospital system was evaluated by Davis and colleagues.73 Adult patients with head injuries were prospectively enrolled over a 1-year period by using the following inclusion criteria: Glasgow Coma Scale score of 3 to 8, transport time greater than 10 minutes, and inability to intubate without RSI. Midazolam and succinylcholine were administered before laryngoscopy, and rocuronium was given after tube placement was confirmed by means of capnometry, syringe aspiration, and pulse oximetry. The Combitube was used as a salvage airway device. Outcome measures included intubation success rates, oxygen saturation values before and after intubation, arrival arterial blood gas values, and total out-of-hospital times for patients intubated en route versus on scene. Of 114 enrolled patients, 96 (84.2%) underwent successful endotracheal intubation, and 17 (14.9%) underwent Combitube intubation, with only 1 (0.9%) airway failure. There were no unrecognized esophageal intubations. On arrival at the trauma center, median oxygen saturation was 99%, mean arrival PaO2 was 307 mm Hg, and mean arrival PaCO2 was 35.8 mm Hg.73,81
Mercer and Gabbott considered the influence of neck position on ventilation with the Combitube, which was inserted in 40 patients undergoing general anesthesia.77 A rigid cervical collar was then used to immobilize the neck of each patient. In all 40 subjects, adequate ventilation of the lungs was possible in this position as assessed by chest movement and auscultation, measurement of expired tidal volume, and maintenance of satisfactory arterial oxygen saturation. In 18 (45%) of 40 patients, small traces of blood were present on the Combitube after removal. Reducing the volume of air injected into the proximal balloon of the Combitube appeared to reduce the incidence of airway trauma during insertion.
In another study, a rigid cervical collar was used to immobilize the neck in 15 American Society of Anesthesiologists (ASA) physical class I or II patients under general anesthesia.82 Insertion of the Combitube was then attempted. In 10 (66%) of 15 patients, blind insertion was impossible. In 5 (33%) of 15 successful blind insertions, the Combitube was in an esophageal position on each occasion. In 8 of 10 of the failures, reinsertion of the Combitube was attempted with the aid of a Macintosh laryngoscope. In 6 (75%) of 8 cases satisfactory placement was then possible, with the Combitube entering the esophagus on each occasion. Ventilation was satisfactory in all patients when insertion was successful. Blood staining of the Combitube was present in 7 (47%) of 15 patients. The investigators state that the Combitube cannot be recommended for use in patients whose necks are immobilized in rigid cervical collars. The alternative insertion technique may improve the rate of successful insertion in this group of patients, because it provides a larger oral aperture than the classic maneuver. However, in cases of suspected or evident cervical spine injury, manual in-line traction before intubation and application of a cervical collar is recommended.
In a 4-year, prospective study, Timmermann and colleagues followed the airway interventions performed by anesthesia-trained emergency physicians.83 The Combitube or LMA was used in 2% of cases of failed intubation, with a success rate of 85% and 89%, respectively.
b Case Reports
A 14-year-old boy had been hit by a motorcycle while riding his bicycle. He suffered severe oronasal bleeding associated with craniofacial injury.84 Computed tomography (CT) at admission indicated multiple craniofacial fractures (i.e., left frontal bone, maxilla, mandible, sphenoid bone, zygomatic bone, nasal bone, and ethmoid bone) with an epidural hematoma of the frontal lobe. His face was depressed about the nose. To keep the airway from oronasal bleeding, an emergency tracheostomy was performed after endotracheal intubation. Nasal and oral packing using Foley balloon catheters was performed but failed to control oronasal bleeding. Bradycardia appeared with ventricular fibrillation during the course because of marked hypovolemia. To get tighter packing, a Combitube was inserted. When the pharyngeal cuff of the Combitube was inflated, the blood pressure rose from 105/60 to 140/90 mm Hg, and the heart rate immediately decreased from 145 to 95 beats/min. Stable circulation was realized by this method during angiography. Embolization produced hemostasis. The Combitube was removed the next day. Surgery for facial fractures was conducted on the 16th hospital day, and the patient was discharged on the 70th hospital day. The Combitube was used in this case to effectively control severe oronasal bleeding before performing angiography. This method was easy to perform, and the investigators recommend the Combitube for oronasal bleeding before embolization.
In another case, an 18-year-old driver lost control of his car and crashed into a tree standing beside the street.85 On arrival of the ambulance, the patient required immediate intubation, but he was trapped in the car. When the car struck the tree, the windshield was broken. Intubation was performed with the Combitube through the broken windshield with one hand only, and ventilation was performed successfully. The patient was then extracted and was intubated by an endotracheal airway. The patient survived and passed high school examinations soon after the accident.
A similar situation occurred for a 24-year-old man who was trapped in his jeep after a motor vehicle collision.86 During his rescue, immediate intubation became mandatory. Because access to the patient’s head was limited, a Combitube was inserted while standing in front of him, and ventilation was easily accomplished. The patient was admitted to the hospital and weaned from the ventilator 3 days later. After 4 weeks, he was discharged from the hospital without any neurologic sequelae. The Combitube appeared to be a valid alternative to endotracheal intubation in cases of difficult access to the patient’s head.
Deroy and Ghoris described a case of elective anesthetic airway management in a patient with a cervical spine fracture.87 In several unusual cases, the Combitube has proved superior to conventional endotracheal intubation. The Combitube proved to be useful in the case of neck impalement with a large, wooden splinter entering at the left angle of the mandible, traversing the pharynx and soft palate, and entering the right maxillary cavity below the floor of the orbit.88
Mercer reported a patient with a difficult airway who was in a halo frame for cervical immobilization.89 The Combitube was successfully used after difficult bag-mask-valve ventilation and failed LMA ventilation.89 Bhagwat and coworkers described the successful use of the Combitube to control oral cavity bleeding.90 The patient had uncontrollable, torrential bleeding caused by the rupture of a right cheek and mandible arteriovenous malformation. The Combitube was used to ensure the airway and to control bleeding through the tamponade effect exercised by the pharyngeal balloon while performing external carotid artery ligation.
3 Anesthesiologic Studies
a General Anesthesia
Function and effectiveness of the Combitube were first tested in animal experiments and subsequently in humans.13,14 The effectiveness of ventilation with the Combitube was compared with ventilation with an ETT during routine surgery in a crossover study.17 Twenty-three patients were ventilated first with the Combitube and then with an ETT (group 1). In group 2, application of the tubes was performed in a reversed order in eight patients. After 20 minutes of ventilation with each airway, arterial blood samples were analyzed. In all cases, patients were ventilated with the Combitube without problems, comparable to ventilation with an ETT. Arterial oxygen pressure was higher during ventilation with the Combitube (142 ± 43 mm Hg with the Combitube versus 119 ± 40 mm Hg with the ETT in group 1, P =.001; 117 ± 16 mm Hg with the endotracheal airway versus 146 ± 13 mm Hg with the Combitube in group 2, P =.001), whereas the differences in arterial carbon dioxide tension and pH were not significant.
The reasons for increased oxygen tension during ventilation with the Combitube were investigated in another study.91 In 12 patients undergoing general anesthesia during routine surgery, a thin catheter was placed with its tip 10 cm below the vocal cords. Patients were then ventilated by mask, by the Combitube in the esophageal position, and by an ETT in a randomized sequence. Pressures were recorded in the trachea and at the airway openings. Blood gas analysis showed a higher arterial oxygen tension with the Combitube than with the ETT (151 ± 37 mm Hg versus 125 ± 32 mm Hg, P < 0.05) and a higher arterial carbon dioxide tension (36 ± 4 mm Hg versus 33 ± 4 mm Hg, P < 0.05). This slightly higher carbon dioxide tension with the Combitube may in part reflect integration of the hypopharynx into the physiologic dead space. Compared with mask ventilation, carbon dioxide tension was lower with the Combitube.
Although peak pressures at the airway openings may be high due to the resistance of the double-lumen airway, intratracheal pressures were comparable for the two tubes. The peak endotracheal pressure was 10 ± 4 mm Hg with a Combitube and 12 ± 6 mm Hg with an ETT (P was not significant [ns]). The endotracheal-plateau pressure was 8 ± 2 mm Hg with the Combitube and 8 ± 4 mm Hg with the ETT (P = ns).14 The Combitube may also be used for prolonged ventilation.39 In seven patients in the ICU, the Combitube was used over a period of 2 to 8 hours during mechanical ventilation. Results showed adequate ventilation compared with subsequent endotracheal ventilation. Lipp and associates had an average time for insertion of the Combitube of 12 to 23 seconds.92 In 3 of 50 patients, the Combitube had to be withdrawn 1 to 2 cm.
Urtubia and coworkers studied the proper use of the Combitube.24 Although the manufacturer recommends that the SA Combitube be used in patients between 122 and 152 cm tall, the aim of this study was to evaluate whether ventilation was effective and reliable in patients taller than 152 cm with the Combitube in the esophageal position. They investigated whether airway protection was adequate and whether direct intubation of the trachea with the Combitube inserted in the esophagus was possible. Urtubia and colleagues studied 25 anesthetized, paralyzed, adult patients who were 150 to 180 cm tall.24 Methylene blue was given orally to all patients before anesthesia induction. Under direct vision, an SA Combitube was inserted in the esophagus of all patients. The pharyngeal balloon inflation volume was titrated to air leak, and cuff pressures were measured. During surgery, a laryngoscope was inserted into the pharynx with the pharyngeal balloon deflated, and the laryngoscopic view was evaluated by using the Cormack-Lehane scale. The presence of methylene blue in the hypopharynx was investigated by direct laryngoscopy. Ventilation was effective and reliable in all 25 patients who were 150 to 180 cm tall (average, 169 ± 7 cm). A direct relationship between the pharyngeal balloon volume and patient height was established (P < 0.05) by using linear regression models, suggesting that the 37-F SA Combitube can be used in patients up to 6 feet (185 cm) tall and implying that the SA Combitube is the preferred size for most patients. The laryngoscopic view of the glottis was adequate to allow direct tracheal intubation. No trace of methylene blue was detected in the hypopharynx. The investigators concluded that the SA Combitube may be used in patients 122 to 185 cm tall. The trachea could be directly intubated with the Combitube in the esophageal position in patients with normal airways, and airway protection appeared to be adequate.
Gaitini and coworkers investigated the effectiveness of the Combitube in elective surgery during mechanical and spontaneous ventilation.18 Two hundred ASA physical status I or II patients with normal airways who were scheduled for elective surgery were randomly allocated to two groups: nonparalyzed, spontaneously breathing (n = 100) or paralyzed, mechanically ventilated (n = 100). After induction of general anesthesia and insertion of the Combitube, SpO2, EtCO2, isoflurane concentration, systolic and diastolic blood pressure, heart rate, and breath-by-breath spirometry data were obtained every 5 minutes. In 97% of patients, it was possible to maintain oxygenation, ventilation, respiratory mechanics, and hemodynamic stability during mechanical or spontaneous ventilation for the duration of surgery, which was between 15 and 155 minutes. The results of this study suggest that the Combitube is an effective and safe airway device for continued management of the airway in 97% of elective surgery cases.
Walz and colleagues tested the smaller SA Combitube in patients exceeding 5 feet tall.25 They studied 104 patients (66 men and 38 women between 3.93 [120 cm] and 6.5 ft [198 cm]) who received the SA Combitube during general anesthesia, most often during implantation of an automatic implantable cardioverter defibrillator. The duration of the procedures ranged from 45 to 360 minutes. In each case, the investigators were able to document with the use of pulse oximetry, capnometry, and ventilation parameters that the patients could be oxygenated and ventilated adequately. The oropharyngeal cuff volume of 85 mL, recommended by the manufacturer, was sufficient in 71 patients (68%). The remaining 33 patients required an additional insufflation volume of 25 to 50 mL in the oropharyngeal balloon to prevent air leakage. The group concluded that the SA Combitube could be used without restriction in patients exceeding 5 feet tall. Because of its smaller size, the SA Combitube is easier to use and seems to be less traumatic to soft tissues. Walz and colleagues preferred to use a laryngoscope during insertion of the SA Combitube, which resulted in less trauma and reduced the number of intubation failures.25
Evaluation of safety, efficacy, and maximum ventilatory pressures during routine surgery was investigated by Frass and coworkers.93 Five hundred patients receiving general anesthesia were enrolled in the study. Type of surgery, duration of surgery, ease of airway insertion, and potential complications were recorded, along with maximum ventilatory pressures and leaks. The Combitube worked well in all but two patients. Duration of surgery varied between 30 and 360 minutes. The Combitube was placed in the esophagus in 97% of patients. More than 95% of the blind Combitube insertions were successful on the first attempt, with an average intubation time of less than 15 seconds. Efficacy of oxygenation and ventilation with the Combitube was evaluated by pulse oximetry and EtCO2. An SpO2 greater than 95% was documented in all cases, and the EtCO2 was 35 to 45 mm Hg. Leak, expressed as a fraction of the inspired volume, did not increase more than 5%, up to a ventilation pressure of 50 cm H2O. Data suggest that the Combitube is safe, easy to insert, and useful during routine surgery. The device may be used when ETT placement is not immediately possible.
Schreier and associates studied the 37-F SA Combitube in 20 children.94 The average age was 9.3 ± 2.4 years, height was 137.3 ± 10.5 cm, and weight was 35 ±10.8 kg. The Combitube worked well in all cases. This study shows that the 37-F SA Combitube can be used in “cannot intubate, cannot ventilate” (CICV) cases for children taller than 122 cm.
A 46-year-old, obese, white woman with a short neck was scheduled for excision of a thyroid goiter.95 One hour after extubation, a hematoma was identified in the right anterior neck. Immediate intubation was mandatory. Fiberoptic intubation failed, but a blind attempt at inserting an ETT resulted in an esophageal intubation. An interincisor distance of 13 mm prevented insertion of a no. 3 LMA. An SA Combitube was then inserted blindly. Oxygen saturation rapidly improved and was maintained at 97% with an FIO2 of 1.0. General anesthesia was completed, and after evacuation of the hematoma, ventilation improved as peak airway pressures declined. The Combitube was superior to the LMA in this case because of its slim design. The Combitube should be considered as an additional tool for managing patient airways in difficult circumstances.
Hagberg and colleagues reported successful use of the Combitube in a 50-year-old patient who had a severe contracture of the mouth and significant tracheal stenosis after prolonged intubation following a burn injury to the face.96 His airway evaluation revealed a Mallampati class IV airway, one-finger-breadth mouth opening, and full range of neck mobility. Because of the patient’s airway examination and concern about endotracheal intubation causing further subglottic tracheal stenosis, a Combitube was chosen for airway management. The otorhinolaryngology surgeons were present in the room when the patient’s neck was prepared and draped and equipment was set up for a tracheostomy, if necessary. A fiberoptic bronchoscope was prepared for use. The investigators found the Combitube to be a very advantageous airway device in establishing an airway in this case and thought it should be considered for elective use in patients with limited mouth opening. They also recommended more extensive use of the Combitube in the operating room so that physicians are familiar with the device when it is needed emergently.97,98
The ease of learning to use the Combitube has been assessed. Enlund and associates reported a case in which conventional endotracheal intubation failed.99 The patient was ventilated by a face mask in the sitting position while the Combitube was brought to the operating room. Although the surgeons were inexperienced in Combitube use, they read the manufacturer’s instructions in the operating room and successfully inserted the Combitube. The device worked well throughout the entire surgical procedure.
Because tracheal suctioning is impossible with the Combitube placed in the esophageal position, the Combitube was redesigned.60 The two anterior, proximal perforations of regular Combitubes were replaced by a larger, ellipsoid hole. Twenty patients with normal airways (Mallampati class I or II) were studied. During general anesthesia, patients were esophageally intubated with the Combitube. A flexible bronchoscope was inserted and guided through the modified hole and glottic opening down the trachea. For the replacement procedure, a J-tip guidewire was introduced through the bronchoscope. The bronchoscope and the Combitube were removed, and a standard ETT was advanced over a guide catheter. Bronchoscopic evaluation of the trachea and guided replacement of the Combitube by an ETT was successful in all 20 patients. The average time needed to perform airway exchange was 90 ± 20 seconds. Arterial oxygen saturation and EtCO2 levels remained normal in all patients. No case of laryngeal trauma was observed during intubation or the airway exchange procedure. The redesigned Combitube enables fiberoptic bronchoscopy, fine-tuning of its position in the esophagus, and guided airway exchange in patients with normal airways. Further studies are warranted to demonstrate the value of this redesigned Combitube in patients with abnormal airways. This version is not commercially available.
b Laparoscopic Surgery
Airway management during laparoscopy is complicated by intraperitoneal carbon dioxide inflation, Trendelenburg position, increased airway pressures, and increased risk of pulmonary aspiration. The Combitube was used in 25 cases of laparoscopic cholecystectomy. Gastric insufflation could not be observed on the video film at the beginning or end of surgery.100 Hartmann and coworkers investigated whether the SA Combitube was a suitable airway during gynecologic laparoscopy.27 One hundred patients were randomly allocated to receive the SA Combitube (n = 49) or ETT (n = 51). Esophageal placement of the Combitube was successful at the first attempt (16 ± 3 seconds). Peak airway pressures were 25 ± 5 cm H2O. An airtight seal was obtained using air volumes of 55 ± 13 mL (oropharyngeal balloon) and 10 ± 1 mL (esophageal cuff). Significant correlations were observed between the patient’s height and weight and the volumes necessary to produce a seal. Similar findings were recorded for the control group; tracheal intubation was difficult in three patients. The SA Combitube provided a patent airway during laparoscopy. Nontraumatic insertion was possible, and an airtight seal was provided at airway pressures of up to 30 cm H2O.
Exposure to sevoflurane and nitrous oxide (N2O) during ventilation using an SA Combitube was compared with waste gas exposure using a conventional ETT.101 Trace concentrations of sevoflurane and N2O were assessed using a direct-reading spectrometer during 40 gynecologic laparoscopic procedures performed under general anesthesia. Measurements were made at the patients’ mouths and in the anesthesiologists’ breathing zones. Mean (±SD) concentrations of sevoflurane and N2O measured at the patients’ mouths were comparable in the SA Combitube group (0.6 ± 0.2 ppm of sevoflurane; 9.7 ± 8.5 ppm of N2O) and ETT group (1.2 ± 0.8 ppm of sevoflurane; 17.2 ± 10.6 ppm of N2O). These values caused comparable contamination of the anesthesiologists’ breathing zones: 0.6 ± 0.2 ppm of sevoflurane and 4.3 ± 3.7 ppm of N2O for the SA Combitube group, compared with 0.5 ± 0.2 ppm of sevoflurane and 4.1 ± 1.8 ppm of N2O for the ETT group. Use of the SA Combitube during positive-pressure ventilation was not necessarily associated with increased waste gas exposure, especially when air conditioning and scavenging devices were available. The Combitube functioned satisfactorily in 22 patients scheduled for elective laparotomy.91
c Obstetric Anesthesia
Airway-related problems represent the most frequent cause of death among women who die of a complication of general anesthesia for cesarean delivery.102 The Combitube has been included in algorithms for managing an unexpected difficult airway during general anesthesia for cesarean delivery.102,103
Urtubia and colleagues reported two cases of emergency cesarean delivery under general anesthesia in which an SA Combitube was used for first-line management of the airway.104 Acute, severe fetal bradycardia in a 17-year-old, obese, pregnant girl did not allow time to perform spinal blockade. General anesthesia was induced, and the airway was maintained through a face mask while applying the Sellick maneuver. After delivery, an SA Combitube was blindly inserted into the esophagus while maintaining cricoid pressure. Ventilation and oxygenation were adequate. For a 27-year-old, deaf-mute, pregnant woman, emergent cesarean delivery was performed because of fetal distress under spinal anesthesia. Soon after surgery began, the patient demonstrated clear signs of pain, and general anesthesia was induced and ventilation performed through the SA Combitube inserted in the esophagus under laryngoscopic guidance. No postoperative pharyngeal symptoms and no respiratory complications were detected in both cases. The Combitube allowed adequate ventilation and airway protection for emergency cesarean delivery in these patients. The Combitube was quickly inserted blindly and with laryngoscopic guidance.
The Combitube was used as a rescue device in a CICV situation during induction of general anesthesia for a cesarean delivery. This case was followed by transient dysfunction of cranial nerves IX and XI, which was attributed to excessive pressure exerted on the pharyngeal mucosa.105 This problem can be avoided by using the minimal inflation technique.40
Wissler used the Combitube in obstetric anesthesia.106 He found that the Combitube was most easily and atraumatically inserted into the esophagus under direct vision using a laryngoscope. In his practice of obstetric anesthesia, the Combitube is his first choice for the anesthetized parturient who cannot be intubated or mask ventilated with cricoid pressure. He thinks it provides a better barrier against regurgitation and aspiration than the LMA.
In a pilot study performed by Hagberg and colleagues, the Combitube was determined to be comparable to the LMA regarding the incidence of gastroesophageal reflux (GER) and tracheal acid aspiration as detected by pH monitoring.36 Fifty-seven patients were randomly assigned to receive an LMA or a Combitube for their elective surgical procedures. All patients were paralyzed and received positive-pressure ventilation. Two monocrystalline antimony catheters were used for pH monitoring of the trachea, oropharynx, and esophagus. One episode of GER occurred with the Combitube in place on extubation, but there were no pH changes reflected in the oropharyngeal or tracheal regions. Three patients in the LMA group met the pH criterion for aspiration (pH < 4.0 lasting at least 15 seconds), compared with only one patient in the Combitube group, but no patient developed any clinical signs of aspiration. By providing reliable airway protection, the Combitube provides another alternative in managing a difficult airway.
d Combitube Compared with Alternative Airway Techniques
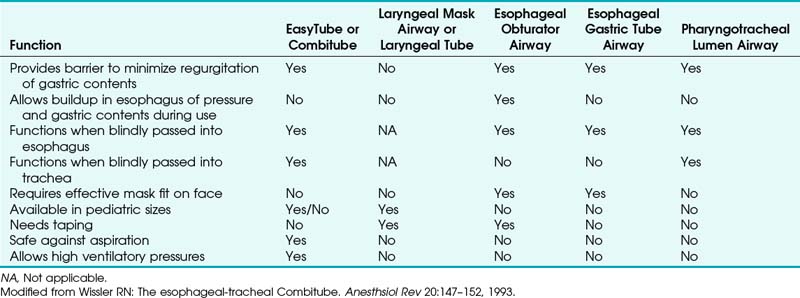
The design of the Combitube has several advantages over other devices, including an open distal tip that allows decompression and suctioning of the esophagus and stomach in the esophageal position and ventilation in the tracheal position (Table 27-1).106 Compared with other devices, the double-lumen design of the Combitube prevents lumen occlusion if the patient bites the tube, which avoids ventilation emergencies during the awakening period.
Compared with the LMA, the VBM Laryngeal Tube (LT; VBM Medizintechnik, Sulz, Germany), and other similar devices, the Combitube provides a decompression barrier (i.e., tracheoesophageal lumen) to minimize regurgitation of gastric contents and allows controlled mechanical ventilation with ventilation pressures higher than 20 cm H2O.91,107 Because the Combitube is safe against aspiration and avoids gastric insufflation during positive-pressure ventilation, use of the LMA is recommended only in elective cases without danger of aspiration. The LT is a device that simulates the design of the Combitube. Although the LT bears no lumen for active decompression, the VBM Laryngeal Tube Suction (LTS) does allow decompression of gastric contents. However, the device is very bulky and may be difficult to place in patients with a small interincisor distance. Another disadvantage is that analogous to the LMA, several sizes should be available to meet the needs of different sizes of patients.
In a training course for emergency care physicians, Winterhalter and associates compared emergency intubation with the Magill tube,108 LMA, and Combitube in mannequins. The Combitube was rated highest with regard to effectiveness and ease of placement. In another comparative study involving nonanesthesia house officers, ventilation by face mask and LMA in a model led to gastric insufflation, but there was none with the Combitube.109
H Recommendations for the Combitube
The Combitube has gained worldwide interest as an adjunct to standard airway equipment in many anesthesiology departments and ambulance services.110–113 The Combitube has been recommended in the ASA practice guidelines for management of the difficult airway; the difficult airway algorithm calls for using the Combitube when an anesthetized patient can be neither intubated nor mask ventilated. Since 1992, it has been included in the guidelines for cardiopulmonary resuscitation and emergency cardiac care of the American Heart Association (AHA) as the first alternative airway, replacing the esophageal obturator as an alternative to the ETT.114–117 The AHA has described the Combitube as a valuable tool for emergency intubation.116
In 2000, the Combitube was upgraded by the AHA to a class IIa device.117 Recommendations for use of the Combitube have been included in the guidelines of the European Resuscitation Council, the Difficult Airway Society guidelines for management of unanticipated difficult intubations, and in many national guidelines.118–121 The Combitube is included in the Street-Level Airway Management (SLAM) Emergency Airway Flowchart, a guideline created for advanced airway practitioners in anesthesiology, emergency medicine, and prehospital care.113
The Combitube is cited in many review articles as an alternative method for artificial ventilation, and it is recommended for patients with massive regurgitation or airway hemorrhage when visualization of the vocal cords may be impossible.28,31,50,51,111,122,123 Gaitini and coworkers described the Combitube as an easily inserted, double-lumen/double-balloon supraglottic airway device.18 The major indication for the Combitube is as a backup device for airway management. It is highly recommended for rescue ventilation in in-hospital and out-of-hospital environments and in situations of difficult ventilation and intubation, especially in patients with massive airway bleeding or limited access to the airway and those in whom neck movement is contraindicated.
Agró and colleagues emphasized that the Combitube is an easily inserted and highly efficacious device to be used as an alternative airway whenever conventional ventilation fails.28 The Combitube allows ventilation and oxygenation whether the device is located in the esophagus (common) or the trachea (rare). Their review of the literature found the Combitube described as a valuable and effective airway in the emergency and prehospital settings, in cardiopulmonary resuscitation, in elective surgery, and in critically ill patients in the ICU. Some studies demonstrated the superiority of the Combitube over other supraglottic ventilatory devices in resuscitation as assessed by success rates for insertion and ventilation. Unlike the LMA, the Combitube may help in patients with limited mouth opening. It may especially benefit patients with massive bleeding or regurgitation, and it minimizes the risk of aspiration.
II Easytube
A Development of the EasyTube Esophageal-Tracheal Double-Lumen Airway
The EasyTube (Rüsch EasyTube, Teleflex Medical, Research Triangle Park, NC) was developed to improve the standard of the Combitube. The outer appearance and handling are similar to those features of the Combitube.124
B Technical Description and Insertion Technique
The EasyTube has a pharyngeal lumen that provides a supraglottic ventilation outlet ending just below the oropharyngeal balloon, which allows passage of a bronchoscope for inspection of the trachea, suctioning of tracheal secretions, or replacement, if necessary (Fig. 27-10). Because of this design, the longer tracheoesophageal lumen has a smaller outer tube diameter together and a larger inner diameter, and it ends like an ETT, decreasing the chance of injury to the pharyngeal and tracheal mucosa.
The EasyTube may be positioned blindly or with the help of a laryngoscope. Laryngoscopic insertion is similar to that used for a standard tracheal tube. After placing the patient’s head in a sniffing position and performing direct laryngoscopy, the trachea is intubated with the EasyTube. A black mark at the distal end of the tube indicates correct depth of insertion just below the vocal cords. Ventilation is performed through the transparent no. 2 lumen. In a CICV situation, the EasyTube can be inserted in the esophagus using a laryngoscope. Ventilation is then performed using the colored no. 1 lumen. The EasyTube also may be inserted blindly, as health care providers usually perform it, especially in the prehospital setting. While the patient’s head is kept in a neutral position, the tube is inserted in a straightforward movement, parallel to the frontal axis of the patient, until the proximal black ring mark is positioned at the level of the upper incisor teeth. In the esophageal position, the no. 2 lumen may be used to drain gastric contents or allow insertion of a gastric tube. The pharyngeal and the distal cuffs are inflated with 80 and 10 mL of air, respectively, using the two prefilled syringes in the package (Fig. 27-11).
C Indications, Advantages, and Complications
Indications for use of the EasyTube are the same as for the Combitube (see Box 27-1). It is designed for emergency intubation and for use in patients undergoing general anesthesia. It has been especially useful in various CICV situations. The 28-F pediatric size may be advantageous, because advanced airway management in children can be challenging, and the potential for morbidity is increased by failed attempts.125 Nagler and Bachur posit that supraglottic rescue devices, including the LMA, esophageal–tracheal double-lumen tube, and laryngeal tube, offer suitable ventilation strategies after failed intubation and in arrest scenarios.125 They encourage pediatric providers to develop familiarity with emerging rescue ventilation devices and with advances in the practice of RSI and laryngoscopy.
3 Advantages
The EasyTube provides several advantages over the Combitube:
1. The pharyngeal lumen of the EasyTube ends just below the oropharyngeal balloon. The tracheoesophageal lumen is thinner than that of the Combitube, which carries the two lumens down to the end. The thinner distal lumen of the EasyTube decreases the chance of injury to the pharyngeal and tracheal mucosa.
2. The oropharyngeal balloon is latex free.
3. The EasyTube is available in two sizes. The 28-F version is designed for pediatric patients 90 to 130 cm tall. The 41-F EasyTube is designed for patients taller than 130 cm, which includes most patients.
4. A fiberoptic scope can be passed through the pharyngeal lumen, because it is open at the distal end. This feature allows inspection of the trachea and offers one way to replace the EasyTube using a guidewire.
5. A larger suction catheter can be passed through both lumens (e.g., 16-F suction catheter in the 41-F EasyTube).
6. The eight small holes or ventilation apertures of the terminal oropharyngeal lumen of the Combitube may be responsible for a greater resistance, leading to larger differences in peak airway pressure measurements.126 The EasyTube has only one supraglottic ventilation aperture.
The slim design allows insertion of the EasyTube in patients with an interincisor distance as small as 12 mm. As in the Combitube, the oropharyngeal cuff of the EasyTube prevents aspiration of blood or secretions from the oral or nasal cavity, and the distal cuff seals the esophagus preventing aspiration of esophageal or gastric secretions. This has been confirmed in a cadaver study.107 Bercker and colleagues designed a study to compare the seal of seven supraglottic airway devices in a cadaver model of elevated esophageal pressure.107 The Classic laryngeal mask airway (LMA-Classic), ProSeal laryngeal mask airway (PLMA), Fastrach intubating laryngeal mask airway (ILMA-Fastrach), Laryngeal Tube Suction (LTS), Laryngeal Tube Suction II (LTS II), Combitube, and EasyTube were inserted in unfixed human cadavers with an exposed esophagus that had been connected to a water column 130 cm high. Slow and fast increases of esophageal pressure were performed, and the water pressure at which leakage appeared was registered. The Combitube, EasyTube, and ILMA-Fastrach withstood water pressure up to more than 120 cm H2O. The PLMA, LTS, and LTS II were able to block the esophagus until 72 to 82 cm H2O. The LMA-Classic showed leakage at 48 cm H2O, but only minor leakage was found in the trachea. Devices with an additional esophageal drainage tube drained fluid sufficiently without pulmonary aspiration. The investigators thought that the use of devices with an additional esophageal drainage lumen might be superior for use in patients with an increased risk of aspiration.107 The Combitube, EasyTube, and ILMA-Fastrach showed the best capacity to withstand an increase of esophageal pressure.
Based on a review of the literature and his own experience as a paramedic and anesthesiologist, Bollig suggests that the Combitube and the EasyTube should be recommended in the Scandinavian guidelines for prehospital airway management.127 He argues that the Combitube has been recommended as an alternative airway device in the ALS guidelines of the European Resuscitation Council and in the ASA guidelines for CICV situations.114,116 A review of the literature revealed the following advantages of the Combitube and EasyTube:
1. Insertion time is shorter for these devices than for endotracheal intubation.
2. The double-lumen airways offer better protection against aspiration than a laryngeal mask.
3. Insertion is possible despite a smaller mouth opening and in patients with massive bleeding or regurgitation.
4. Blind insertion is possible in patients who are trapped in a sitting position (e.g., car crash).
5. Epinephrine and lidocaine can be applied through the Combitube.
6. Mechanical ventilation in intensive care is possible for several hours using the Combitube.
D Medical Literature
1 Mannequin Studies
Based on the results from a mannequin study, the use of an impedance threshold valve for ventilation during CPR is possible in combination with the Combitube, EasyTube, or other supraglottic airway device.128 Robak and coworkers reported the superiority of Combitube and EasyTube for controlling the airway in a mannequin under simulated pathologic airway conditions.129 Fifty medical students assessed the success rate and insertion time for seven supraglottic airway devices: LMA Unique, LMA Fastrach single use, LMA Supreme, King LTS disposable (LTS-D), i-gel, Combitube, and EasyTube. All airways were inserted without problems, but only the Combitube and EasyTube were successfully inserted in simulated trismus, limited mobility of the cervical spine, and in cases of combined pathologic conditions such as trismus plus limited mobility of the spine and trismus plus tongue edema.
In another mannequin model, Ruetzler and colleagues studied the performance and skill retention of intubation by paramedics using seven airway devices: ETT, LMA Unique, PLMA, LTS-D, i-gel, Combitube, and EasyTube.130 After 3 months, 100% successful skill retention was reported for five of six supraglottic airway devices (i.e., LMA Unique, LTS-D, i-gel, Combitube, and EasyTube), and a rate of 58% was reported for endotracheal intubation.
2 In-Hospital Studies
Bollig and colleagues determined the difference in the rate of and time to successful airway placement and ventilation using tracheal intubation compared with use of the esophageal-tracheal Combitube or EasyTube. Twenty-six paramedics, who were trained in tracheal intubation, received additional training in the use of the Combitube and the EasyTube.131 Each participant performed all three methods twice in a random order on a manikin. Time to successful ventilation (presented as the mean and standard deviation) and the success rate were recorded. Mean time to successful ventilation was significantly longer for tracheal intubation (45.2 ± 15.8 seconds) than for the Combitube (36.0 ± 8.6 seconds, P = 0.002) and the EasyTube (38.0 ± 15.3 seconds, P = 0.023), with no difference between the latter two methods (P = 1.000). The combined success rate for the Combitube and EasyTube (103 of 104 attempts) was significantly higher than for tracheal intubation (45 of 52 attempts) (odds ratio [OR] = 16.0; 95% confidence interval [CI], 1.9 to 134; P = 0.002). For the paramedics tested on manikins, the placement success rate was higher and less time was required for the Combitube and EasyTube than for tracheal intubation, with no differences identified between the Combitube and EasyTube.
In a study by Thierbach and Werner, 30 adult patients (ASA physical status I or II, Mallampati class I and II, and weight between 50 and 80 kg) undergoing minor surgery were randomly allocated to the esophageal EasyTube insertion group using a blind or laryngoscopically guided technique.132 Data were collected for number of attempts, time taken to provide an effective airway, blood staining, and postoperative airway morbidity. The time to obtain an effective airway was measured from removal of the face mask to confirmation of normal ventilation and evaluated by bilateral chest movement and a normal capnography curve. There were no failures on inserting the device with either technique. First attempt and second attempt insertion rates were 86% and 14% for the blind insertion technique and 93% and 7% for the laryngoscopically guided technique, respectively. Time to achieve an effective airway was 31 ± 4 seconds for the blind technique and 33 ± 6 seconds for the laryngoscopically guided technique. After removal of the device, blood stains were observed in eight patients, with four patients in each group. The rate of sore throat in the postanesthesia care unit was 20% for both groups, and no patient required treatment. Data suggest that insertion of the EasyTube has the same success rate with or without using a laryngoscope. A study determined that pressures exerted on the oropharyngeal mucosa were lower than with laryngeal masks.133
Lorenz and associates studied the effectiveness, safety, and ease of placement of the EasyTube compared with an ETT in 200 patients randomized to one of these two groups.134 Even though the number of insertions was equal in both groups, the insertion time was shorter with the EasyTube. (15.5 ± 3.6 seconds for the EasyTube versus 19.3 ± 4.6 seconds for the ETT, P = 0.0001). Ease of insertion was greater in the EasyTube group, and there was no difference in the incidence of sore throat, dysphagia, and hoarseness.
Gaitini and colleagues evaluated the ease of use of the EasyTube compared with the Combitube in 80 patients randomized to one of these two groups.135 All patients were intubated blindly in the esophagus. Less time was required to achieve an effective airway using the EasyTube (19.4 ± 5.3 seconds) compared with the esophageal-tracheal Combitube (30.6 ± 4.1 seconds, P < 0.001). EasyTube insertion was rated significantly easier than Combitube insertion (P = 0.008) by anesthesiologists participating in the study. EasyTube insertion was rated easy in 36 cases and moderately difficult in 4 cases. Combitube insertion was rated easy in 26 cases and moderately difficult in 14 cases. No insertion in either group was rated difficult or impossible.
3 Out-of-Hospital Studies
In a prehospital setting, Chenaitia and coworkers evaluated the effectiveness and safety of use of the EasyTube in cases of difficult airway management by emergency physicians with minimal training with the device.136 They performed a prospective, multicenter, observational study of patients requiring airway management conducted in a prehospital emergency setting in France by three mobile ICUs from October 2007 to October 2008. Data were available for 239 patients who needed airway management and were classified in two groups: the easy airway management group (225 patients [94%]) and the difficult airway management group (14 patients [6%]). All patients had a successful airway management. The EasyTube was used in eight men and six women; the mean age was 64 years. It was used for ventilation for a maximum of 150 minutes, and the mean time was 65 minutes. It was positioned successfully at first attempt, except for two patients; one needed an adjustment because of an air leak, and in the other patient, the EasyTube was replaced due to complete obstruction during bronchial suction. The investigators concluded that emergency physicians could use the EasyTube safely and effectively with minimal training in cases of difficult airway management. Because of its very high success rate for ventilation, the possibility of blind intubation, the low failure rate after a short training period, they thought it should be introduced in new guidelines for managing difficult airways in prehospital emergency settings.133
4 Study of the EasyTube in Emergencies
A preliminary study was undertaken by Thierbach and colleagues to assess early experiences with the EasyTube in prehospital and in-hospital emergency airway management procedures.137 All airway management procedures with the EasyTube were recorded for a period of 18 months. The EasyTube was successfully used in 15 patients with unanticipated airway difficulties during anesthesia induction or prehospital airway management. In all patients, the EasyTube was positioned successfully at the first attempt, with a median time of 31 seconds until start of ventilation. Effective supraglottic ventilation and oxygenation were achieved within 25 to 40 seconds. In three patients, the EasyTube needed one additional repositioning maneuver. On removal of the EasyTube, no blood was observed on the surface of the device, and no injuries were observed in the patients’ mouth, pharynx, or esophagus. The investigators concluded that the device successfully established sufficient ventilation and oxygenation.137
5 Study Results and Applications
Studies demonstrate that the Combitube and EasyTube are effective alternatives to traditional intubation techniques. Both devices have been shown to be as effective as an endotracheal tube in emergency situations. The wide range of applications and ease of insertion make them valuable pieces of equipment in wards, operating rooms, and prehospital conditions, and the Combitube may be reused.138 Operators involved in airway management should be familiar with the techniques described for these rescue devices to successfully manage an emergency and to avoid using the Combitube or EasyTube for the first time during a crisis.
Data suggest that the Combitube can be inserted successfully during microgravity (e.g., parabolic flights).135,139 These results may aid in developing protocols for managing airway emergencies during space missions.
Studies show that double-lumen airways such as the Combitube and EasyTube are superior to other supraglottic devices in emergency situations.20,21,75 Further study of these devices is recommended because they require less training than endotracheal intubation and are easier to insert than an endotracheal airway.66
III Case Examples of Airway Management with Combitube, Easytube, and Other Devices
A 54-year-old, morbidly obese woman was admitted to the ICU because of respiratory failure.140 Her neck was short and rigid, with thick, subcutaneous fat pads. Anatomic landmarks such as thyroid and cricoid cartilages were impossible to identify. Her tongue was very large, and the Mallampati score was class IV. Tracheal intubation by flexible fiberoptic bronchoscope (FOB) was performed under local anesthesia. Four days later, extubation was uneventful, and continuous positive airway pressure (CPAP) was initiated with the patient in the sitting position. Oxygen saturation ranged from 95% to 97%, but the patient was uncooperative and did not tolerate the CPAP mask. After removing the CPAP mask, supplemental oxygen (8 L/min) was given by an open face mask. Oxygen saturation decreased to 85%, she became rapidly cyanotic and dyspneic, and a severe bronchospasm was identified by direct thorax auscultation. Immediate tracheal intubation using the FOB was attempted under topical anesthesia, but respiratory parameters rapidly deteriorated. During intubation, the patient developed severe laryngeal spasm, which made passage of the FOB through the vocal cords impossible. Oxygen saturation dropped to 60%, and the patient became unconscious and bradycardic. Three-handed mask ventilation was established with 100% supplemental oxygen and an oropharyngeal and two nasopharyngeal cannulas. Oxygen saturation increased to 80%. An expert anesthesiologist made one attempt at laryngoscopy, but only the tip of the epiglottis could be seen under direct vision. Laryngoscopy was immediately stopped because oxygen saturation dropped to 60% and the patient did not tolerate apnea. Cricothyrotomy was considered but excluded because it was impossible to identify the anatomic landmarks of the cricothyroid membrane. In view of the CICV situation, a 41-F Combitube was considered. Insertion was easy, and after checking the esophageal position by auscultation, ventilation was obtained using the device’s pharyngeal tube. Inflation pressure appeared to be high, but oxygen saturation returned quickly to 95%. A 50-mg dose of atracurium was administered intravenously, and the patient was connected to a mechanical ventilator. Peak pressure was 45 cm H2O. Residual bronchospasm was treated with 750 mg of aminophylline. The patient was transferred to the operating room for a tracheotomy while she was ventilated through the Combitube. The next day, the patient was fully awake and responsive, and she had no symptoms of neurologic damage. She was weaned from the ventilator 10 days after the tracheostomy and discharged from the ICU on day 22 after admission without neurologic sequelae.140
A 40-year-old man was scheduled for revision of scars caused by facial burns due to a gas explosion. The initial injury occurred 14 months before this procedure, and the patient had received a tracheostomy during his stay in the ICU. Preoperative evaluation revealed a reduced glottic opening and tracheal stenosis. Because of the existing airway pathology and the impossibility of using tapes, the EasyTube was elected for airway management. The EasyTube was inserted under direct vision with a laryngoscope into the esophagus and successfully used throughout the 130-minute surgical procedure.141
Paramedics failed to intubate a 51-year-old patient who was found unresponsive, but they successfully placed a Combitube. On arrival in the emergency department, it was decided to exchange the Combitube for an ETT. Three attempts to exchange the Combitube with an ETT using direct laryngoscopy failed. After deflation of the proximal cuff of the Combitube, an 8-mm ETT was advanced over a gum elastic bougie into the trachea under visualization of the oropharynx using a Direct Coupled Interface video intubating system.142
All references can be found online at expertconsult.com.
1 Benumof JL. Management of the difficult adult airway. Anesthesiology. 1991;75:1087–1110.
18 Gaitini LA, Vaida SJ, Mostafa S, et al. The Combitube in elective surgery: A report of 200 cases. Anesthesiology. 2001;94:79–82.
20 Rumball CJ, MacDonald D. The PTL, Combitube, laryngeal mask, and oral airway: A randomized prehospital comparative study of ventilatory device effectiveness and cost-effectiveness in 470 cases of cardiorespiratory arrest. Prehosp Emerg Care. 1997;1:1–10.
24 Urtubia RM, Aguila CM, Cumsille MA. Combitube: A study for proper use. Anesth Analg. 2000;90:958–962.
27 Hartmann T, Krenn CG, Zoeggeler A, et al. The oesophageal-tracheal Combitube Small Adult. An alternative support during gynaecological laparoscopy. Anaesthesia. 2000;55:670–675.
32 Wafai Y, Salem MR, Baraka A, et al. Effectiveness of the self-inflating bulb for verification of proper placement of the Esophageal Tracheal Combitube. Anesth Analg. 1995;80:122–126.
72 Lefrancois DP, Dufour DG. Use of the esophageal tracheal Combitube by basic emergency medical technicians. Resuscitation. 2002;52:77–83.
73 Davis DP, Valentine C, Ochs M, et al. The Combitube as a salvage airway device for paramedic rapid sequence intubation. Ann Emerg Med. 2003;42:697–704.
130 Ruetzler K, Roessler B, Potura L, et al. Performance and skill retention of intubation by paramedics using seven different airway devices—A manikin study. Resuscitation. 2011;82:593–597.
139 Rabitsch W, Moser D, Inzunza MR, et al. Airway management with endotracheal tube versus Combitube during parabolic flights. Anesthesiology. 2006;105:696–702.
1 Benumof JL. Management of the difficult adult airway. Anesthesiology. 1991;75:1087–1110.
2 Tiah L, Wong E, Chen MF, et al. Should there be a change in the teaching of airway management in the medical school curriculum. Resuscitation. 2005;64:87–91.
3 Don Michael TA, Lambert EH, Mehran A. Mouth-to-lung airway for cardiac resuscitation. Lancet. 1968;2:1329.
4 Schofferman J, Oill P, Lewis AJ. The esophageal obturator airway: A clinical evaluation. Chest. 1976;69:67–71.
5 Shea SR, MacDonald JR, Gruzinski G. Prehospital endotracheal tube airway or esophageal gastric tube airway: A critical comparison. Ann Emerg Med. 1985;14:102–112.
6 Hammargren Y, Clinton JE, Ruiz E. A standard comparison of esophageal obturator airway and endotracheal tube ventilation in cardiac arrest. Ann Emerg Med. 1985;14:953.
7 Bryson TK, Benumof JL, Ward CF. The esophageal obturator airway: A clinical comparison of ventilation with a mask and oropharyngeal airway. Chest. 1978;74:537–539.
8 Gertler JP, Cameron DE, Shea K, et al. The esophageal obturator airway: Obturator or obtundator? J Trauma. 1985;25:424–426.
9 Crippen D, Olvey S, Graffis R. Gastric rupture: An esophageal obturator airway complication. Ann Emerg Med. 1981;10:370–373.
10 Johnson KR, Genovesi MG, Lassar KH. Esophageal obturator airway: Use and complications. JACEP. 1976;5:36–39.
11 Pilcher DB, DeMeules JE. Esophageal perforation following use of esophageal airway. Chest. 1976;69:377–380.
12 Scholl DG, Tsai SH. Esophageal perforation following the use of the esophageal obturator airway. Radiology. 1977;122:315–316.
13 Frass M, Frenzer R, Zahler J, et al. First experimental studies with a new device for emergency intubation (esophageal tracheal Combitube). Anasthesiol Intensivmed Notfallmed Schmerzther. 1987;24:390–392.
14 Frass M, Frenzer R, Rauscha F, et al. Evaluation of esophageal tracheal Combitube in cardiopulmonary resuscitation. Crit Care Med. 1987;15:609–611.
15 Frass M, Frenzer R, Rauscha F, et al. Ventilation with the esophageal tracheal Combitube in cardiopulmonary resuscitation: Promptness and effectiveness. Chest. 1988;93:781–784.
16 Frass M, Frenzer R, Zahler J. Respiratory tube or airway. U.S. patent no.. 1987;4:688. 568
17 Frass M, Frenzer R, Zdrahal F, et al. The esophageal tracheal Combitube: Preliminary results with a new airway for CPR. Ann Emerg Med. 1987;16:768–772.
18 Gaitini LA, Vaida SJ, Mostafa S, et al. The Combitube in elective surgery: A report of 200 cases. Anesthesiology. 2001;94:79–82.
19 Rabitsch W, Krafft P, Lackner FX, et al. Evaluation of the oesophageal-tracheal double-lumen tube (Combitube) during general anaesthesia. Wien Klin Wochenschr. 2004;116:90–93.
20 Rumball CJ, MacDonald D. The PTL, Combitube, laryngeal mask, and oral airway: A randomized prehospital comparative study of ventilatory device effectiveness and cost-effectiveness in 470 cases of cardiorespiratory arrest. Prehosp Emerg Care. 1997;1:1–10.
21 Tanigawa K, Shigematsu A. Choice of airway devices for 12,020 cases of nontraumatic cardiac arrest in Japan. Prehosp Emerg Care. 1998;2:96–100.
22 Hofbauer R, Röggla M, Staudinger T, et al. Emergency intubation with the Combitube in a patient with persistent vomiting. Anasthesiol Intensivmed Notfallmed Schmerzther. 1994;29:306–308.
23 Urtubia R, Aguila C. Combitube: A new proposal for a confusing nomenclature [letter]. Anesth Analg. 1999;89:803.
24 Urtubia RM, Aguila CM, Cumsille MA. Combitube: A study for proper use. Anesth Analg. 2000;90:958–962.
25 Walz R, Davis S, Panning B. The Combitube: A useful emergency airway device for anesthesiologists? Anesth Analg. 1999;88:233.
26 Frass M, Johnson JC, Atherton GL, et al. Esophageal tracheal Combitube (ETC) for emergency intubation: Anatomical evaluation of ETC placement by radiography. Resuscitation. 1989;18:95–102.
27 Hartmann T, Krenn CG, Zoeggeler A, et al. The oesophageal-tracheal Combitube Small Adult. An alternative support during gynaecological laparoscopy. Anaesthesia. 2000;55:670–675.
28 Agró F, Frass M, Benumof JL, Krafft P. Current status of the Combitube: A review of the literature. J Clin Anesth. 2002;14:307–314.
29 Rabitsch W, Koestler WJ, Fiebiger W, et al. Closed suctioning system reduces cross-contamination between bronchial system and gastric juices. Anesth Analg. 2004;99:886–892.
30 Green K, Beger T. Proper use of the Combitube. Anesthesiology. 1994;81:513–514.
31 Agró F, Frass M, Benumof J, et al. The esophageal tracheal Combitube as a non-invasive alternative to endotracheal intubation. A review. Minerva Anestesiol. 2001;67:863–874.
32 Wafai Y, Salem MR, Baraka A, et al. Effectiveness of the self-inflating bulb for verification of proper placement of the Esophageal Tracheal Combitube. Anesth Analg. 1995;80:122–126.
33 Urtubia RM, Frass M, Agro F. New insertion technique of the Esophageal-Tracheal Combitube. Acta Anaesthesiol Scand. 2002;46:340–341.
34 Urtubia RM, Frass M, Staudinger T, et al. Modification of the Lipp maneuver for blind insertion of the Esophageal-Tracheal Combitube. Can J Anaesth. 2005;52:216–217.
35 Klein H, Williamson M, Sue-Ling HM, et al. Esophageal rupture associated with the use of the Combitube. Anesth Analg. 1997;85:937–939.
36 Hagberg C, Vartazarian TN, Chelkly JE, et al. The incidence of gastroesophageal reflux and tracheal aspiration detected with pH electrodes is similar with the Laryngeal Mask Airway and Esophageal-Tracheal Combitube—A pilot study. Can J Anaesth. 2004;51:243–249.
37 Smith I, Ding Y, White PF. Comparison of induction, maintenance, and recovery characteristics of sevoflurane-N2O and propofol-sevoflurane-N2O with propofol-isoflurane-N2O anesthesia. Anesth Analg. 1992;74:253–259.
38 Urtubia R, Medina J, Marshall J, et al. Insertion of Esophageal-Tracheal Combitube using inhalational anesthetic induction with sevoflurane. Difficult Airway. 2002;3:51–57.
39 Frass M, Frenzer R, Mayer G, et al. Mechanical ventilation with the esophageal tracheal Combitube (ETC) in the intensive care unit. Arch Emerg Med. 1987;4:219–225.
40 Gaitini L, Somri M, Yanovski B, et al. Minimal inflation volume for Combitube oro-pharyngeal balloon. Arad Med J. 2010;13:27–32.
41 Piotrowski D, Gaszynski W, Wacowska-Szewczyk M, et al. Intubation with the oesophageal tracheal Combitube for elective laparotomy. Anaesthesiol Intens Ther. 1995;27:25–30.
42 Panning B. Self-intubation with a Combitube , 1998. Available at http://www.youtube.com/watch?v=4kAtsfH-LbE (accessed March 2012)
43 Keller C, Brimacombe J, Boehler M, et al. The influence of cuff volume and anatomic location on pharyngeal, esophageal, and tracheal mucosal pressures with the esophageal tracheal Combitube. Anesthesiology. 2002;96:1074–1077.
44 Frass M, Frenzer R, Ilias W, et al. The esophageal tracheal Combitube (ETC): Animal experiment results with a new emergency tube [in German]. Anasthesiol Intensivmed Notfallmed Schmerzther. 1987;22:142–144.
45 Ovassapian A, Liu S, Krejcie T. Fiberoptic tracheal intubation with Combitube in place [abstract]. Presented at the 67th Congress of International Anesthesia Research Society, San Diego, CA, March 19-23, 1993. Anesth Analg. 1993;76:S315.
46 Gaitini LA, Vaida SJ, Somri M, et al. Fiberoptic-guided airway exchange of the Esophageal-Tracheal Combitube in spontaneously breathing vs. mechanically ventilated patients. Anesth Analg. 1999;88:193–196.
47 Wiltschke C, Kment G, Swoboda H, et al. Ventilation with the Combitube during tracheotomy. Laryngoscope. 1994;104:763–765.
48 Kinkle W, Pisaturo J, Butler K, et al. Tracheal Intubation around the Combitube: A prospective study on a cadaveric model. Acad Emerg Med. 2007;14(Suppl 1):275.
49 Harrison WL, Bertrand ML, Andeweg SK, et al. Retrograde intubation around an in situ Combitube: A difficult airway management strategy. Anesthesiology. 2005;102:1061–1062.
50 Rich JM, Mason AM, Bey TA, et al. The critical airway, rescue ventilation, and the Combitube: Part I. AANA J. 2004;72:17–27.
51 Rich JM, Mason AM, Bey TA, et al. The critical airway, rescue ventilation, and the Combitube: Part II. AANA J. 2004;72:115–124.
52 Atherton GL, Johnson JC. Ability of paramedics to use the Combitube in prehospital cardiac arrest. Ann Emerg Med. 1993;22:1263–1268.
53 Blouin D, Topping C, Moore S, et al. Out-of-hospital defibrillation with automated external defibrillators: Postshock analysis should be delayed. Ann Emerg Med. 2001;38:256–261.
54 Dunham CM, Barraco RD, Clark DE, et al. EAST Practice Management Guidelines Work Group. Guidelines for emergency tracheal intubation immediately after traumatic injury. J Trauma. 2003;55:162–179.
55 Haynes BE, Pritting J. A rural emergency medical technician with selected advanced skills. Prehosp Emerg Care. 1999;3:343–346.
56 Johnson JC, Atherton GL. The esophageal tracheal Combitube: An alternate route to airway management. J Emerg Med Serv. 1991;5:23–34.
57 Krafft P, Frass M. The difficult airway [in German]. Wien Klin Wochenschr. 2000;112:260–270.
58 Rich M, Thierbach A, Frass M. The Combitube, self-inflating bulb, and colorimetric carbon dioxide detector to advance airway management. In the first echelon of the battlefield. Mil Med. 2006;171:389–395.
59 Liao D, Shalit M. Successful intubation with the Combitube in acute asthmatic respiratory distress by a Parkmedic. J Emerg Med. 1996;14:561–563.
60 Krafft P, Röggla M, Fridrich P, et al. Bronchoscopy via a re-designed Combitube in the esophageal position. A clinical evaluation. Anesthesiology. 1997;86:1041–1045.
61 McGlinch BP, Martin DP, Volcheck GW, et al. Tongue engorgement with prolonged use of the esophageal-tracheal Combitube. Ann Emerg Med. 2004;44:320–322.
62 Vezina D, Lessard MR, Bussieres J, et al. Complications associated with the use of the Esophageal-Tracheal Combitube. Can J Anaesth. 1998;45:76–80.
63 Portereiko JV, Perez MM, Hojman H, et al. Acute upper airway obstruction by an overinflated Combitube esophageal obturator balloon. J Trauma. 2006;60:426–427.
64 Richards CF. Piriform sinus perforation during Esophageal-Tracheal Combitube placement. J Emerg Med. 1998;16:37–39.
65 Moser MS. Piriform sinus perforation during esophageal-tracheal Combitube placement. J Emerg Med. 1999;17:129.
66 Oczenski W, Krenn H, Dahaba AA, et al. Hemodynamic and catecholamine stress responses to insertion of the Combitube, laryngeal mask airway or tracheal intubation. Anesth Analg. 1999;88:1389–1394.
67 Vezina MC, Trepanier CA, Nicole PC, et al. Complications associated with the Esophageal-Tracheal Combitube in the pre-hospital setting. Can J Anaesth. 2007;54:124–128.
68 Staudinger T, Brugger S, Watschinger B, et al. Emergency intubation with the Combitube: Comparison with the endotracheal airway. Ann Emerg Med. 1993;22:1573.
69 Johnson JC: Personal communication, 1995.
70 Ander DS, Hanson A, Pitts S. Assessing resident skills in the use of rescue airway devices. Ann Emerg Med. 2004;44:314–319.
71 Ochs M, Vilke GM, Chan TC, et al. Successful prehospital airway management by EMT-Ds using the Combitube. Prehosp Emerg Care. 2000;4:333–337.
72 Lefrancois DP, Dufour DG. Use of the esophageal tracheal Combitube by basic emergency medical technicians. Resuscitation. 2002;52:77–83.
73 Davis DP, Valentine C, Ochs M, et al. The Combitube as a salvage airway device for paramedic rapid sequence intubation. Ann Emerg Med. 2003;42:697–704.
74 Cady CE, Pirrallo RG. The effect of Combitube use on paramedic experience in endotracheal intubation. Am J Emerg Med. 2005;23:868–871.
75 Mort TC. Laryngeal mask airway and bougie intubation failures: The Combitube as a secondary rescue device for in-hospital emergency airway management. Anesth Analg. 2006;103:1264–1266.
76 Banyai M, Falger S, Röggla M, et al. Emergency intubation with the Combitube in a grossly obese patient with bull neck. Resuscitation. 1993;26:271–276.
77 Mercer M, Gabbott D. The influence of neck position on ventilation using the Combitube airway. Anaesthesia. 1998;53:146–150.
78 Bigenzahn W, Pesau B, Frass M. Emergency ventilation using the Combitube in cases of difficult intubation. Eur Arch Otorhinolaryngol. 1991;248:129–131.
79 Urtubia R, Lorca E, De la Fuente D. Successful rescue of out-of-hospital airway emergency using the esophageal-tracheal Combitube by nonskilled personnel [in Spanish]. Rev Med Chil. 2001;129:119–120.
80 Blostein PA, Koestner AJ, Hoak S. Failed rapid sequence intubation in trauma patients: Esophageal tracheal Combitube is a useful adjunct. J Trauma. 1998;44:534–537.
81 Ochs M, Davis D, Hoyt D, et al. Paramedic-performed rapid sequence intubation of patients with severe head injuries. Ann Emerg Med. 2002;40:159–167.
82 Mercer MH, Gabbott DA. Insertion of the Combitube airway with the cervical spine immobilised in a rigid cervical collar. Anaesthesia. 1998;53:971–974.
83 Timmermann A, Eich C, Russo SG, et al. Prehospital airway management: A prospective evaluation of anaesthesia trained emergency physicians. Resuscitation. 2006;70:179–185.
84 Morimoto F, Yoshioka T, Ikeuchi H, et al. Use of Esophageal Tracheal Combitube to control severe oronasal bleeding associated with craniofacial injury: Case report. J Trauma. 2001;51:168–169.
85 Knacke P: Personal communication, 2003.
86 Lorenz V, Frass M. Securing the airway with the help of the Combitube in a patient trapped in a car. Difficult Airway. 2001;2:64–67.
87 Deroy R, Ghoris M. The Combitube elective anesthetic airway management in a patient with cervical spine fracture. Anesth Analg. 1998;87:1441–1442.
88 Eichinger S, Schreiber W, Heinz T, et al. Airway management in a case of neck impalement: Use of the oesophageal tracheal Combitube airway. Br J Anaesth. 1992;68:534–535.
89 Mercer M. Respiratory failure after tracheal extubation in a patient with halo frame cervical spine immobilization-rescue therapy using the Combitube airway. Br J Anaesth. 2001;86:886–891.
90 Bhagwat AG, Saxena KN, Dua K, et al. A novel use of esophageal tracheal airway: The control of torrential oral bleeding. Minerva Anestesiol. 2008;74:675–677.
91 Frass M, Rodler S, Frenzer R, et al. Esophageal tracheal Combitube, endotracheal airway and mask: Comparison of ventilatory pressure curves. J Trauma. 1989;29:1476–1479.
92 Lipp M, Thierbach A, Daublander M, et al. Clinical evaluation of the Combitube. Presented at the 18th Annual Meeting of the European Academy of Anaesthesiology, August 29 to September 1. 1996. Copenhagen, Denmark, p 43
93 Frass M, Lackner FX, Frenzer R, et al. Analysis of 500 uses of the Combitube: Safety, efficacy, and maximum ventilatory pressures during routine surgery. Difficult Airway. 2001;2:84–90.
94 Schreier H, Papousek A, Aram L, et al. Use of the esophageal-tracheal Combitube in children. Proceedings of the Vienna International Anesthesiology and Intensive Care Congress, Vienna, October 2 to 5, 1996. Acta Anaesthesiol Scand. 1996;40:246.
95 Klein U, Rich JM, Seifert A, et al. Use of the Combitube as a rescue airway during a case of “can’t ventilate–can’t intubate (CVCI)” in the operating room when a laryngeal mask failed. Difficult Airway; 2002;3.
96 Hagberg C, Johnson S, Pillai D. Effective use of the esophageal tracheal Combitube following severe burn injury. J Clin Anesth. 2003;15:463–466.
97 Frass M. Development, patent procedure, and 15 years experience: Combitube-from bench to bedside. Curr Opin Clin Exp Res. 2000;2:31–38.
98 Urtubia RM, Aguila M. New thoughts on the difficult airway. Curr Opin Clin Exp Res. 2000;2:61–67.
99 Enlund M, Miregard M, Wennmalm K. The Combitube for failed intubation—Instructions for use. Acta Anaesthesiol Scand. 2001;45:127–128.
100 Vaida S. The effectiveness of the Esophageal-Tracheal Combitube in mechanically ventilated patients undergoing laparoscopic cholecystectomy. Anasthesiol Intensivmed Notfallmed Schmerzther. 1999;34:S121.
101 Hoerauf KH, Hartmann T, Acimovic S, et al. Waste gas exposure to sevoflurane and nitrous oxide during anaesthesia using the oesophageal-tracheal Combitube Small Adult. Br J Anaesth. 2001;86:124–126.
102 Munnur U, Suresh MS. Airway problems in pregnancy. Crit Care Clin. 2004;20:617–642.
103 Vaida S, Pott L, Budde A, Gaitini L. Suggested algorithm for management of the unexpected difficult airway in obstetric anesthesia. J Clin Anesth. 2009;21:385–386.
104 Urtubia RM, Medina JN, Alzamora R, et al. Combitube for emergency cesarean section under general anesthesia. Case reports. Difficult Airway. 2001;2:78–83.
105 Zamora JE, Saha TK. Combitube rescue for Cesarean delivery followed by ninth and twelfth cranial nerve dysfunction. Can J Anaesth. 2008;55:779–784.
106 Wissler RN. The esophageal-tracheal Combitube. Anesthsiol Rev. 1993;20:147–152.
107 Bercker S, Schmidbauer W, Volk T, et al. A comparison of seal in seven supraglottic airway devices using a cadaver model of elevated esophageal pressure. Anesth Analg. 2008;106:445–448.
108 Winterhalter M, Brummerloh C, Luttje K, et al. Emergency intubation with Magill tube, LMA and Combitube in a training-course for emergency care physicians. Anasthesiol Intensivmed Notfallmed Schmerzther. 2002;37:532–536.
109 Dörges V, Ocker H, Wenzel V, et al. Emergency airway management by non-anaesthesia house officers—A comparison of three strategies. Emerg Med J. 2001;18:90–94.
110 Clinton JE, Ruiz E. Emergency airway management procedures. In: Roberts JR, Hedges JR. Clinical procedures in emergency medicine. ed 2. Philadelphia: WB Saunders; 1991:7–8.
111 Cozine K, Stone G. The take-back patient in ear, nose, and throat surgery. In: Benumof JL, ed. Anesthesiology clinics of North America, vol 11. Philadelphia: WB Saunders; 1993.
112 Niemann JT. Cardiopulmonary resuscitation: Current concepts. N Engl J Med. 1992;327:1075–1080.
113 Rich JM, Mason AM, Ramsay MA. AANA journal course: Update for nurse anesthetists. The SLAM emergency airway flowchart: A new guide for advanced airway practitioners. AANA J. 2004;72:431–439.
114 American Society of Anesthesiologists’ Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway. Anesthesiology. 1993;78:597–602.
115 Practice Guidelines for Management of the Difficult Airway. An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277.
116 American Heart Association. Combination esophageal-tracheal tube. Guidelines for cardiopulmonary resuscitation and emergency cardiac care: Recommendations of the 1992 National Conference of the American Heart Association. JAMA. 1992;268:2203.
117 American Heart Association (AHA). Emergency cardiac care (ECC) guidelines, part 6: Advanced cardiovascular life support, section 3: Adjuncts for oxygenation, ventilation, and airway control. Airway adjuncts. Circulation. 2000;102:I-95–I-104.
118 Baskett PJF, Bossaert L, Carli P, et al. Guidelines for the advanced management of the airway and ventilation during resuscitation. A statement by the Airway and Ventilation Management Working Group of the European Resuscitation Council. Resuscitation. 1996;31:201–230.
119 Nolan J. European Resuscitation Council: Resuscitation. European Resuscitation Council guidelines for resuscitation 2005, section 1: Introduction. 2005;67(Suppl 1):S3–S6.
120 Henderson JJ, Popat MT, Latto IP, et al. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59:675–694.
121 Italian Society of Anesthesia, Resuscitation, and Intensive Therapy (SIAARTI). The difficult intubation and the problem of monitoring the adult airway [in Italian]. Minerva Anestesiol. 1998;64:361–371.
122 Gaitini LA, Vaida SJ, Agro F. The Esophageal-Tracheal Combitube. Anesthesiol Clin North Am. 2002;20:893–906.
123 Urtubia RM. Combitubo para el manejo electivo de la vía aérea. Rev Chil Anest. 2002;31:221–232.
124 Thierbach AR, Piepho T, Maybauer MO. A new device for emergency airway management: The EasyTube. Resuscitation. 2004;60:347.
125 Nagler J, Bachur RG. Advanced airway management [review]. Curr Opin Pediatr. 2009;21:299–305.
126 Gaitini L, Vaida S, Somri M, et al. The esophageal-tracheal Combitube and ventilatory pressures. J Clin Anesth. 2005;17:26–29.
127 Bollig G. Combitube and EasyTube should be included in the Scandinavian guidelines for pre-hospital airway management. Acta Anaesthesiol Scand. 2009;53:139–140.
128 Genzwuerker HV, Gernoth C, Hinkelbein J, et al. Influence of an impedance threshold valve on ventilation with supraglottic airway devices during cardiopulmonary resuscitation in a manikin. Resuscitation. 2010;81:1010–1013.
129 Robak O, Leonardelli M, Zedtwitz-Liebenstein K, et al: Speed of insertion of seven supraglottic airway devices by medical students: Superiority of Combitube and EasyTube under simulated pathological airway conditions. Canadian J Emerg Med. (In print)
130 Ruetzler K, Roessler B, Potura L, et al. Performance and skill retention of intubation by paramedics using seven different airway devices—A manikin study. Resuscitation. 2011;82:593–597.
131 Bollig G, Løvhaug SW, Sagen Ø, et al. Airway management by paramedics using endotracheal intubation with a laryngoscope versus the oesophageal tracheal Combitube and EasyTube on manikins: A randomised experimental trial. Resuscitation. 2006;71:107–111.
132 Thierbach AR, Werner C. Infraglottic airway devices and techniques. Best Pract Res Clin Anaethesiol. 2005;19:595–609.
133 Ulrich-Pur H, Hrska F, Krafft P, et al. Comparison of mucosal pressures induced by cuffs of different airway devices. Anesthesiology. 2006;104:933–938.
134 Lorenz V, Rich JM, Schebesta K, et al. Comparison of the EasyTube and endotracheal tube during general anesthesia in fasted adult patients. J Clin Anesth. 2009;21:341–347.
135 Gaitini L, Yanovsky B, Somri M, et al. Prospective randomized comparison between EasyTube and Esophageal Tracheal Combitube during general anesthesia with mechanical ventilation. J Clin Anesth. 2011;23:475–481.
136 Chenaitia H, Soulleihet V, Massa H, et al. The EasyTube for airway management in prehospital emergency medicine. Resuscitation. 2010;81:1516–1520.
137 Thierbach AR, Piepho T, Maybauer M. The EasyTube for airway management in emergencies. Prehosp Emerg Care. 2005;9:445–448.
138 Lipp M, Jaehnichen G, Golecki N, et al. Microbiological, microstructure, and material science examinations of reprocessed Combitubes after multiple reuse. Anesth Analg. 2000;91:693–697.
139 Rabitsch W, Moser D, Inzunza MR, et al. Airway management with endotracheal tube versus Combitube during parabolic flights. Anesthesiology. 2006;105:696–702.
140 Della Puppa A, Pittoni G, Frass M. Tracheal esophageal Combitube: A useful airway for morbidly obese patients who cannot intubate or ventilate. Acta Anaesthesiol Scand. 2002;46:911–913.
141 Urtubia RM, Leyton R. Successful use of the EasyTube for facial surgery in a patient with glottic and subglottic stenosis. J Clin Anesth. 2009;19:77–78.
142 Lam NC, Hagberg CA, Bassili LM. Use of the video laryngoscopy for Combitube exchange in a difficult airway. J Clin Anesth. 2009;21:294–296.