Erythroderma

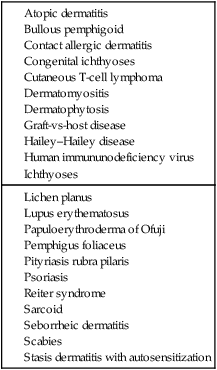
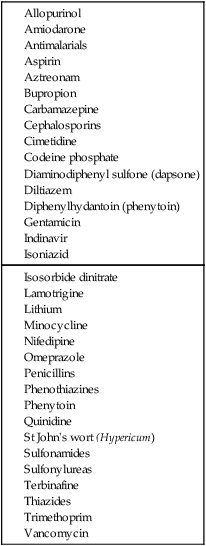
Erythroderma (exfoliative dermatitis) is defined as inflammation of at least 90% of the body surface, characterized by generalized erythema and a variable degree of scaling or desquamation. Erythroderma is commonly the result of generalization of a pre-existing chronic dermatosis or a systemic disease (see Table 75.1). These include genodermatoses and congenital disorders such as severe ichthyoses and ichthyosiform erythrodermas; severe cases of dermatoses such as psoriasis, atopic or seborrheic or contact allergic dermatitis; cutaneous T-cell lymphoma; allergic reactions to drugs (see Table 75.2); and internal malignancies (especially lymphoma and other lymphoreticular malignancies). Some cases develop without any apparent trigger and erythroderma remains ‘idiopathic’ in up to 25% of the cases.
Specific investigations
Second-line therapies
Third-line therapies













 Bed rest in hospital
Bed rest in hospital Emollients
Emollients Topical corticosteroids
Topical corticosteroids Psoralen and UVA (PUVA)
Psoralen and UVA (PUVA) Systemic corticosteroids
Systemic corticosteroids PUVA with retinoid
PUVA with retinoid Cyclosporine
Cyclosporine Cytotoxic drugs/antimetabolites
Cytotoxic drugs/antimetabolites Systemic retinoids
Systemic retinoids Extracorporeal photochemotherapy
Extracorporeal photochemotherapy UVA1 phototherapy
UVA1 phototherapy Topical calcipotriol
Topical calcipotriol Topical tacrolimus
Topical tacrolimus Erythromycin
Erythromycin Photopheresis and interferon
Photopheresis and interferon Infliximab
Infliximab Etanercept
Etanercept Alemtuzumab
Alemtuzumab Daclizumab
Daclizumab Bexarotene
Bexarotene