CHAPTER 48 Epilepsy Surgery Overview
Neurological surgery has played an important role in the management of patients with epilepsy throughout the history of our specialty.1 The types of operative procedures performed and the indications for surgical intervention have evolved and changed in parallel with technical and scientific advances in multiple related disciplines. The chapters in this section are organized to provide a comprehensive review of these topics and are authored by leading investigators and neurosurgeons in their respective fields. In this introduction to the section on epilepsy surgery we provide a brief overview of the topics that will be covered and the rationale for their inclusion.
The history of epilepsy surgery has been strongly influenced by the dynamic balance between the perceived values of surgical procedures and medical treatments. The risk-benefit calculation for epilepsy surgery is affected by multiple factors, many of which are difficult to rigorously quantify and extrapolate across large patient populations and may not be directly related to the surgical treatment itself. The probability of a seizure-free outcome after surgery, for example, is dependent on the ability to accurately characterize a patient’s seizure disorder.2–6 Thus, technologic advances in nonsurgical disciplines that have an impact on the presurgical evaluation process (e.g., magnetoencephalography [MEG]) have the potential to indirectly alter the surgical risk-benefit assessment. On the medical management side, enormous resources have been committed over a period of many decades to research and develop new antiepileptic drugs (AEDs). In the past, the actual effectiveness of AEDs or the anticipated usefulness of new AEDs in the development pipeline provided a rationale for treating physicians to not explore surgical treatment options.
In the modern era, the epilepsy surgical decision-making calculus has changed significantly. Contemporary clinical reports, including a landmark prospective study of epilepsy surgery versus best medical management for intractable temporal lobe seizures, provide incontrovertible evidence of the safety and efficacy of epilepsy surgery.7–11 It is also now widely accepted that neuronal cell loss occurs with persistent seizures and that uncontrolled epilepsy can be associated with progressive, irreversible loss of brain functions.7,8,12 Hopes that new AEDs would prove to be markedly more effective than older generation drugs have largely been unrealized to date.13,14 The side effects of newer AEDs are better tolerated by some patients, but the complex underlying pathophysiology of refractory seizure disorders continues to resist a medical “magic bullet.” For these and other reasons, it is now widely accepted that patients with intractable seizures should be evaluated for possible epilepsy surgery after a circumscribed period of expert medical management. Persistent seizures should not be tolerated if a viable surgical option exists. The probability of a new drug succeeding in eliminating a patient’s seizure disorder when other drugs have failed is exceedingly low.7,14
Contemporary reviews of bench epilepsy research and experimental animal models are included in this section because of their direct relevance to epilepsy surgery. Much of this research is designed to gain new insights into the neurophysiologic and molecular mechanisms of epilepsy that can be used to develop more effective AEDs. However, information gained from this research also guides the design and implementation of new, nonablative functional neurosurgical applications. As an example, drugs that are demonstrated to disrupt pathologic epileptic circuitry in animal models but have unacceptable side effects when given systemically to humans at the desired concentration could be delivered in a brain site–specific manner by using stereotactically implanted catheters and drug pumps.15,16 Knowledge of the fine details of abnormal epileptic discharges and the effects of precisely timed electrical stimulation of the abnormal medial temporal lobe circuitry set the stage for ongoing clinical trials of patterned electrical stimulation through implanted electrodes as a new neurosurgical treatment.17–19 In these and other examples, the concept of bench-to-bedside translational research has had a direct impact on the treatment of epilepsy patients.
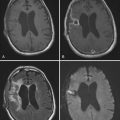
The vast majority of epilepsy surgery procedures are performed at major centers that have the resources to support a comprehensive multidisciplinary program.20 One of the main tasks of this group is to correctly identify patients who will probably benefit from epilepsy surgery. In most instances, neurologists, neuropsychologists, and neuroradiologists gather and perform the primary analysis of the data that are used to make this determination. The epilepsy surgeon, however, must have a thorough understanding of the strengths and limitations of these preoperative examinations. Preoperative evaluation topics are addressed in sections throughout many of the chapters in this section. Technical advances in areas such as functional brain imaging have had an impact on the preoperative evaluation process, with some caveats. One of the most difficult diagnostic challenges is to identify brain activation patterns that typify a patient’s seizure-onset patterns. This necessitates measuring brain activity during a seizure, and in most instances, because of technical constraints, it is not feasible to obtain functional magnetic resonance imaging (fMRI), MEG, or positron emission tomography (PET) data during these ictal events. Functional brain imaging data provide valuable information that influences clinical decision making; however, well-established electroencephalography (EEG)-based diagnostic methods that can be used in both the interictal and ictal states continue to play a preeminent role in the preoperative evaluation process.2,3,21,22
A wide range of surgical strategies are used for the treatment of medically refractory epilepsy. The indications, techniques, risks, and results of these procedures are included in this section. Although the specific techniques used vary somewhat across centers, all contemporary epilepsy procedures can be grouped into clearly identifiable categories. The most commonly performed resective procedure is temporal lobectomy. A variety of methods are used to plan the extent of resection, and different technical approaches can be used to access the mesial portions of the temporal lobe. Irrespective of the approach used, seizure control outcomes are excellent in properly selected patients with temporal lobe epilepsy.7,9,11 Approximately 60% to 80% of patients are seizure free on long-term follow-up, as opposed to less than 10% of refractory patients who continue to be managed with medical treatment alone.
Seizure disorders localized to brain regions outside the temporal lobe represent a more difficult surgical challenge. This heterogeneous group of disorders typically requires a more extensive presurgical evaluation than needed for temporal lobe cases. Even when seizure onsets appear to be accurately localized to noneloquent brain regions, extratemporal lobe resections are associated with only approximately 50% to 60% seizure-free outcome rates.23 In cases in which the seizure focus localizes to eloquent brain regions, such as primary motor or sensory cortex or language critical sites, resective surgery often cannot be performed safely. In this setting, multiple subpial transection (MST) surgery is a treatment option.24–26 As with extratemporal resective surgery, seizure-free outcome rates after MST are significantly lower than after temporal lobe procedures. The rationale for pursuing these treatment options, despite the high rate of persistent seizures after surgery, is that the alternative of continued medical management is associated with an even higher incidence of persistent seizures and progressive neurological decline.
As with all neurosurgical procedures, the potential benefits of surgery must be weighed against the potential risks. In the case of epilepsy surgery, the risk variable is particularly important and is specifically addressed in a chapter devoted to this topic. Most patients who undergo resective surgery have results on neurological examination that are grossly normal or are in a state of chronic compensation for a long-standing deficit. With the exception of SUDEP (sudden unexplained death in epilepsy), the condition being treated surgically is not usually life-threatening in the conventional sense. Although major neurological complications, such as stroke causing hemiplegia, are rare, when they do occur, the functional consequences for the patient can be devastating. In addition, because of the nature of the brain regions being removed and the preexisting chronic neurological injury caused by frequent seizures, some patients will experience significant procedure-related morbidity even when no complications occurred during surgery. Such morbidity includes loss of memory function and depression.15,27–31 Epilepsy surgeons and their patients must thoroughly understand the avoidable and unavoidable risks before electing a surgical treatment option.
In many patients with refractory epilepsy, the results of the presurgical evaluation will reveal that they are poor candidates for resection surgery. A typical scenario in this setting is one in which the patient is found to have multiple seizure foci that localize to widely distributed brain regions. In the past, there was no viable surgical treatment option for these patients. Now, many of them can be helped by implantation of a vagal nerve stimulator.32–34 This is a low-risk procedure that reduces the frequency of seizures in more than half of the patients implanted, but it rarely results in a seizure-free outcome. As described earlier, other nonablative surgical interventions are also under development, including chronic electrical brain stimulation and local drug infusion methods.
Another unique aspect of the subspecialty of epilepsy surgery is the opportunities that it affords to study normal human brain functions. Safe and effective epilepsy surgery is predicated on the ability of the surgical team to accurately localize seizure activity and map the normal functions of the human brain. For this reason, many epilepsy operations and all chronic extraoperative monitoring procedures are performed on awake subjects. This provides a unique opportunity not only to examine the pathophysiology of epilepsy but also to study normal human brain functions by using invasive research techniques that do not increase the risks associated with epilepsy surgery. The strategy of using epilepsy surgery patients to perform basic neuroscience research was pioneered by Wilder Penfield and colleagues at the Montreal Neurological Institute.35–39 Even with the development of powerful noninvasive brain research methods such as fMRI, answers to certain important neuroscience questions can still be answered only with direct, invasive methods. For this reason, multidisciplinary basic research teams throughout the world have incorporated this investigative approach into their overall human brain research strategy.40–43 The range of research activities being pursued, along with specific examples, are presented in the chapter devoted to this topic. Well-trained neurosurgeon-scientists are critical members of these teams, and future prospects for young neurosurgeons who wish to pursue this career path have never been brighter.
1 Feindel W, Leblanc R, de Almeida AN. Epilepsy surgery: historical highlights 1909-2009. Epilepsia. 2009;50:131-151.
2 Baumgartner C, Pataraia E. Revisiting the role of magnetoencephalography in epilepsy. Curr Opin Neurol. 2006;19:181-186.
3 Kilpatrick C, Cook M, Kaye A, et al. Non-invasive investigations successfully select patients for temporal lobe surgery. J Neurol Neurosurg Psychiatry. 1997;63:327-333.
4 Knake S, Triantafyllou C, Wald LL, et al. 3T phased array MRI improves the presurgical evaluation in focal epilepsies—a prospective study. Neurology. 2005;65:1026-1031.
5 Koepp MJ, Woermann FG. Imaging structure and function in refractory focal epilepsy. Lancet Neurol. 2005;4:42-53.
6 Theodore WH, Sato S, Kufta C, et al. Temporal lobectomy for uncontrolled seizures: the role of positron emission tomography. Ann Neurol. 1992;32:789-794.
7 Engel J, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy—Report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Epilepsia. 2003;44:741-751.
8 Langfitt JT, Wiebe S. Early surgical treatment for epilepsy. Curr Opin Neurol. 2008;21:179-183.
9 Spencer S, Huh L. Outcomes of epilepsy surgery in adults and children. Lancet Neurol. 2008;7:525-537.
10 Tellez-Zenteno JF, Dhar R, Hernandez-Ronquillo L, et al. Long-term outcomes in epilepsy surgery: antiepileptic drugs, mortality, cognitive and psychosocial aspects. Brain. 2007;130:334-345.
11 Wiebe S, Blume WT, Girvin JP, et al. A randomized, controlled trial of surgery for temporal lobe epilepsy. N Engl J Med. 2001;345:311-318.
12 Engel JJr. Etiology as a risk factor for medically refractory epilepsy: a case for early surgical intervention. Neurology. 1998;51:1243-1244.
13 Cramer JA, Ben Menachem E, French J. Review of treatment options for refractory epilepsy: new medications and vagal nerve stimulation. Epilepsy Res. 2001;47:17-25.
14 Mohanraj R, Brodie MJ. Diagnosing refractory epilepsy: response to sequential treatment schedules. Eur J Neurol. 2006;13:277-282.
15 Foong J, Flugel D. Psychiatric outcome of surgery for temporal lobe epilepsy and presurgical considerations. Epilepsy Res. 2007;75:84-96.
16 Heiss JD, Walbridge S, Morrison P, et al. Local distribution and toxicity of prolonged hippocampal infusion of muscimol. J Neurosurg. 2005;103:1035-1045.
17 Cohen-Gadol AA, Brffton JW, Wetjen NM, et al. Neurostimulation therapy for epilepsy: current modalities and future directions. Mayo Clin Proc. 2003;78:238-248.
18 Skarpaas TL, Morrell MJ. Intracranial stimulation therapy for epilepsy. Neurotherapeutics. 2009;6:238-243.
19 Sun FT, Morrell MJ, Wharen RE. Responsive cortical stimulation for the treatment of epilepsy. Neurotherapeutics. 2008;5:68-74.
20 Walczak TS. National Assoc Epilepsy Center guidelines for essential services, personnel, and facilities in specialized epilepsy centers in the United States. Epilepsia. 2001;42:804-814.
21 Chakraborty A, McEvoy AW. Presurgical functional mapping with functional MRI. Curr Opin Neurol. 2008;21:446-451.
22 Laufs H, Duncan JS. Electroencephalography/functional MRI in human epilepsy: what it currently can and cannot do. Curr Opin Neurol. 2007;20:417-423.
23 Zentner J, Hufnagel A, Ostertun B, et al. Surgical treatment of extratemporal epilepsy: clinical, radiologic, and histopathologic findings in 60 patients. Epilepsia. 1996;37:1072-1080.
24 Benifla M, Otsubo H, Ochi A, et al. Multiple subpial transections in pediatric epilepsy: indications and outcomes. Childs Nerv Syst. 2006;22:992-998.
25 Blount JP, Langburt W, Otsubo H, et al. Multiple subpial transections in the treatment of pediatric epilepsy. J Neurosurg. 2004;100:118-124.
26 Mulligan LP, Spencer DD, Spencer SS. Multiple subpial transections: the Yale experience. Epilepsia. 2001;42:226-229.
27 Baxendale S. The impact of epilepsy surgery on cognition and behavior. Epilepsy Behav. 2008;12:592-599.
28 Blumer D, Wakhlu S, Davies K, et al. Psychiatric outcome of temporal lobectomy for epilepsy: incidence and treatment of psychiatric complications. Epilepsia. 1998;39:478-486.
29 Kanner AM. Depression in epilepsy: a complex relation with unexpected consequences. Curr Opin Neurol. 2008;21:190-194.
30 Kemp S, Coughlan AK, Goulding PJ, et al. Measurement of remote memory pre- and post-temporal lobectomy: a longitudinal case study. Epilepsy Behav. 2007;10:195-202.
31 Wrench J, Wilson SJ, Bladin PF. Mood disturbance before and after seizure surgery: a comparison of temporal and extratemporal resections. Epilepsia. 2004;45:534-543.
32 Amar AP, Heck CN, Levy ML, et al. An institutional experience with cervical vagus nerve trunk stimulation for medically refractory epilepsy: rationale, technique, and outcome. Neurosurgery. 1998;43:1265-1276.
33 Mulligan LP, Spencer DD, Spencer SS. Vagus nerve stimulation for intractable epilepsy: a review. J Clin Neurophysiol. 1997;14:358-368.
34 Tecoma ES, Iragui VJ. Vagus nerve stimulation use and effect in epilepsy: what have we learned? Epilepsy Behav. 2006;8:127-136.
35 Feindel W. Neurosurgery at the Montreal Neurological Institute and McGill University Hospitals. Neurosurgery. 1996;39:830-839.
36 Penfield W, Boldrey E. Somatic motor and sensory representation in the cerebral cortex of man as studied by electrical stimulation. Brain. 1937;60:389-443.
37 Preul MC, Feindel W. Origins of Penfield, Wilder surgical technique—the role of the Cushing ritual and influences from the European experience. J Neurosurg. 1991;75:812-820.
38 Rasmussen TB. Surgical treatment of epilepsy. Can Med Assoc J. 1977;116:1369-1370.
39 Weber M. History of the surgical treatment of epilepsy: from origin to MNI. Epilepsies. 2007;19:91-95.
40 Engel AK, Moll CKE, Fried I, et al. Invasive recordings from the human brain: clinical insights and beyond. Nat Rev Neurosci. 2005;6:35-47.
41 Hamberger MJ, Seidel WT, Mckhann GM, et al. Brain stimulation reveals critical auditory naming cortex. Brain. 2005;128:2742-2749.
42 Kawasaki H, Kaufman O, Damasio H, et al. Single-neuron responses to emotional visual stimuli recorded in human ventral prefrontal cortex. Nat Neurosci. 2001;4:15-16.
43 Ojemann GA, Ojemann SG, Fried I. Lessons from the human brain: neuronal activity related to cognition. Neuroscientist. 1998;4:285-300.