CHAPTER 56 Epidemiology of Disc, Joint, and Root Pain in Whiplash
INTRODUCTION
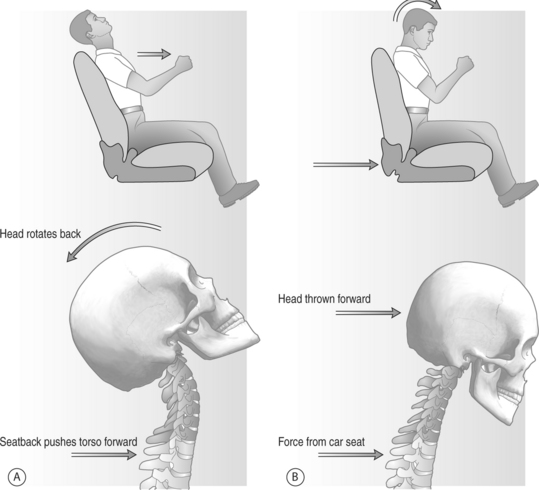
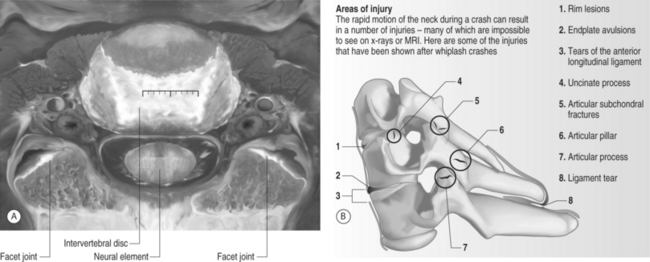
Neck pain resulting from a whiplash mechanism of injury is controversial and has attracted particular attention. A whiplash injury is typically defined as an injury to the cervical spine resulting from hyperextension and flexion of the head during a motor vehicle accident (Fig. 56.1). Sources of pain in whiplash patients are usually multifactorial. The primary affected anatomical structures of the cervical spine are perivertebral soft tissues, neuro-elements, intervertebral disc, and zygapophyseal joint (Fig. 56.2). Most whiplash-related neck pain is usually self-limiting, and can be adequately treated with conservative measures such as rest, nonsteroidal antiinflammatory agents, pain medications, muscle relaxants, and physical therapy. Patients failing to improve with this regimen may require further radiographic and interventional diagnostic work-ups.
Although epidemiology in whiplash has been relatively well studied, few studies have adequately provided detailed analyses of the anatomical structures involved in chronic neck pain in whiplash patients. Increased knowledge about the size and extent of this problem is essential as it may facilitate predictions of the need for medical services.1
EPIDEMIOLOGY OF WHIPLASH
Motor vehicle accidents with a whiplash mechanism of injury are one of the most common causes of neck injuries, with an incidence of perhaps 1 million per year in the United States.2 The social and economic costs are tremendous. Twenty-five to 30 billion dollars are spent annually on treatment for neck discomfort without neurologic signs in whiplash patients in the United States alone.3 The costs of whiplash injury are expected to rise with increasing incidence.
Whiplash injuries usually result in neck pain arising from injury to soft tissue, the disc, or zygapophyseal joint, and the etiology of this pain has been documented in animal and human studies. Headaches, reported in 82% of patients acutely, are usually of the muscle contraction type, and are often associated with greater occipital neuralgia related to C2 cervical nerve root injury, and less often to temporomandibular joint syndrome.4,5 Other frequent complaints include dizziness, paresthesia, postconcussion syndrome, and low back pain.6 Fifteen percent of whiplash patients suffer severe pain for 1–3 years, and 26–44% of patients will develop long-term problems.7 Chronic whiplash has long been a source of controversy, in large part because most patients do not have a readily identifiable injury in either the acute or chronic stage. Chronic unremitting pain occurs in 5% of patients.8
Incidence and prevalence
The incidence and severity of whiplash injury is increasing with the wider use of transport and the development of higher-velocity vehicles.9 Many epidemiologic studies have been reported from a number of countries utilizing automobile insurance company data. Considerable caution is necessary when comparing national statistics. Such statistics are dependent on complex social and legal variables, and cannot be used as an overall measure of incidence.10 The occurrence, severity, and duration of whiplash-related symptoms have been reported differently among different countries. Regional differences within the same country may also impact study results. Wide differences between countries in cultural attitude, insurance systems, or financial compensation may significantly impact statistical analyses. In an analysis of 300 cases showing lower whiplash incidence in Singapore relative to Australia,11 the author suggested that cultural differences in how whiplash was viewed in these two countries (e.g. as an illness, versus as an illness behavior) were a significant variable. A 1987 Quebec study showed increasing whiplash incidence.6 The overall incidence was 70 per 100 000 persons, but the rate in a Saskatchewan study was 700 per 100 000 persons. In this case, differences may be caused by regional variations in the insurance compensation system: a no-fault insurance system in Quebec versus a tort system in Saskatchewan.
Legislation changes in Australia (the claimant now has to report the accident to the police and bear the first $317 of medical expense), afforded a substantial effect upon whiplash incidence. One year following the new law, whiplash reported incidences were 50–70% fewer than previous years, even though there presumably may have been more vehicles on the road. A recent study also supported the idea that financial compensation by insurance systems has a profound effect on the frequency and duration of whiplash claims, and that claimants recover faster if compensation for pain and suffering is not available. Cassidy et al.14 studied a population-based cohort of persons who filed insurance claims for traffic injuries in Saskatchewan, where the insurance system was changed from the tort compensation system to a no-fault system. After the introduction of no-fault, there was a 28% reduction in incidence, and the median time to the closure of claims was reduced by more than 200 days.
Prognosis
Whiplash is associated with high costs and a prognosis that is variable and difficult to predict. A prospective study of 93 patients with cervical whiplash revealed that only 15% had persistent minor discomfort, but 43% of patients still had symptoms sufficiently severe to interfere with their ability to work 2 years after the injury.15
Many studies addressing prognostic factors have been published, but there have been various results. Hildingsson and Toolan15 found that acute symptoms, physical findings, forces and directions of impact, head rests, radiographs, and sex did not show prognostic value. However, Evans2 suggested that some risk factors, including older age, interscapular or upper back pain, occipital headache, paresthesia at presentation, reduced range of cervical spine movement, objective neurologic deficits, preexisting degenerative osteoarthritic changes, and an upper-middle occupational category correlated with less favorable recovery. These data showed long-term disability in over 6% of patients, and patients with those risk factors did not return to work after 1 year. There was, however, only minimal association between poor prognosis and collision speed or severity and the extent of vehicle damage.
In a recent study, risk factors for prolonged recovery time after whiplash injury were introduced.16