74
Environmental and Sports-Related Skin Diseases
Cutaneous Injury Due to Heat Exposure
Thermal Burns
• Traumatic injury to the skin caused by an external heat source.
• The burn depth determines the severity and classification of the injury, its potential for healing and need for surgical intervention (Table 74.1).
Table 74.1
Classification and treatment of thermal burns.
Based on the 2009 American Burn Association revised classification system for burns. http://www.ameriburn.org/Chapter14.pdf
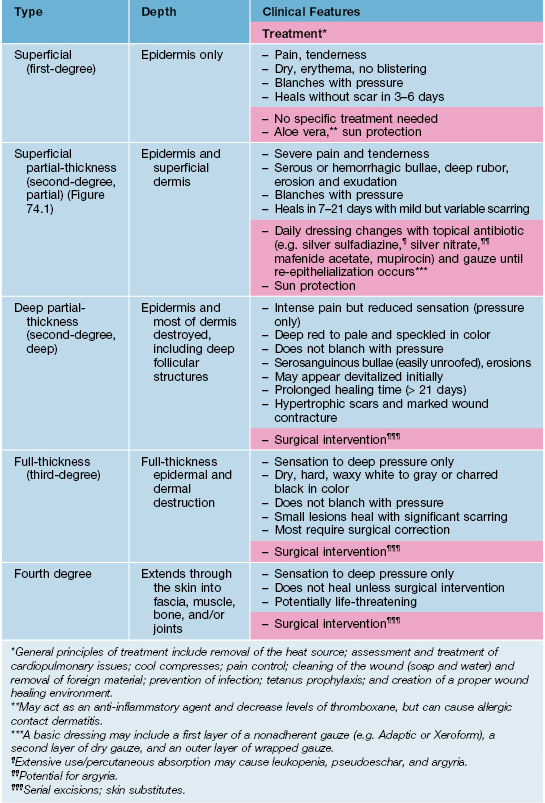
• In 2009, the American Burn Association replaced the traditional classification of burn wounds (i.e. first-, second-, third-degree) with a system that reflects the need for surgical intervention (see Table 74.1; Fig. 74.1).

Fig. 74.1 Thermal burn. This superficial partial-thickness burn is characterized by bullae that contain serous fluid. Courtesy, Kalman Watsky, MD.
• The most accurate method for estimating BSA involvement in adults and children is the Lund–Browder chart (http://www.tg.org.au/etg_demo/phone/etg-lund-and-browder.pdf); the ‘rule of nines’ method is perhaps more expeditious in adults, but it cannot be used for children (Fig. 74.2).
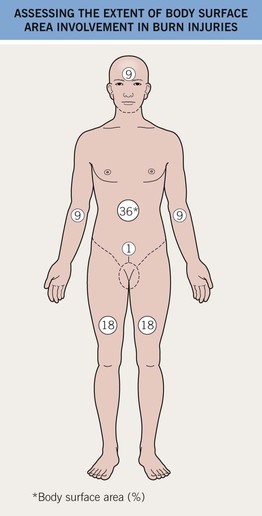
Fig. 74.2 Assessing the extent of body surface area involvement in burn injuries: Rule of nines. In adults, an estimate of burn extent is often based on this surface area distribution chart. Infants and children have a relatively increased head : trunk surface area ratio and this chart is ineffective for them. These estimates are also used for primary cutaneous disorders. The most accurate method of estimating the BSA involvement of burn injury in adults and children is with the Lund–Browder chart (http://www.tg.org.au/etg_demo/phone/etg-lund-and-browder.pdf).
• General principles of treatment are outlined in Table 74.1.
Erythema Ab Igne
• Multiple heat sources have been implicated (Table 74.2).
Table 74.2
Heat sources reported to cause erythema ab igne.
| • Heating pads | • Steam radiators |
| • Hot water bottles | • Heated car seats |
| • Electric stove/heater | • Heated reclining chairs |
| • Open fires | • Heating blanket |
| • Coal stoves | • Hot bricks |
| • Peat fires | • Infrared lamps |
| • Wood stoves | • Microwave popcorn |
| • Sauna belt | • Laptop computer* |
* Anterior thighs >> abdomen.
Courtesy, Mary Beth Cole, MD, and Michael Smith, MD.
• Early lesions: asymptomatic, initially transient, blanchable macular erythema in a broad, reticulated pattern that corresponds to the venous plexus; size and shape approximates that of the heat source (Fig. 74.3A).


Fig. 74.3 Erythema ab igne. A Early phase with pink reticulated patches predominating over reticulated hyperpigmentation. B Later phase with large area of reticulated hyperpigmentation and superimposed pink keratotic plaques centrally. A, Courtesy, Jeffrey Callen, MD; B, Courtesy, Peter Klein, MD.
• Later lesions: dusky reticulated hyperpigmentation; lesions are fixed and no longer blanchable (Fig. 74.3B).
• End stage: may become keratotic and bullae may appear.
• Rx: remove the heat source; if applicable, identify and treat the underlying source of pain.
Burns Associated with MRI and Fluoroscopy
MRI
Fluoroscopy
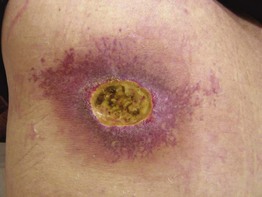
• This radiodermatitis may be acute, but with time continued changes can develop, e.g. hair loss, desquamation, permanent erythema, and ulceration (Fig. 74.4).
Cutaneous Injury Due to Cold Exposure
Frostbite
• Can occur when the skin temperature drops below about –2°C (28°F).
• There are four categories of severity based on depth of tissue injury; these are only recognizable upon rewarming (Fig. 74.5).

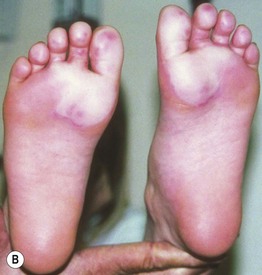
Fig. 74.5 Frostbite. A Erythema, edema, and hemorrhage are seen on the fingertips in a first-degree frostbite (frostnip); full recovery is expected, with only mild desquamation. B Bullae filled with clear fluid on the distal plantar surfaces in a second-degree frostbite; many such patients develop long-term sensory neuropathies. In third-degree frostbite there is full-thickness dermal loss with hemorrhagic bullae or waxy, dry, mummified skin. In fourth-degree frostbite there is full-thickness loss of the entire part, with skin, muscle, tendon, and bone damage; amputation may occur. A, Courtesy, Michael L. Smith, MD; B, Courtesy, Timothy Givens, MD.
• Symptomatically, early erythema, edema, and numbness are replaced by marked hyperemia and pain.
Pernio (Chilblains)
• An abnormal inflammatory response to cold, damp, nonfreezing conditions.
• Classically presents with single or multiple erythematous to blue-violet macules, papules, or nodules distributed symmetrically on distal toes (Fig. 74.6) and fingers, and less often on the remainder of the foot or hand, nose and ears.

Fig. 74.6 Pernio. Violaceous macules and patches, primarily on the toes but also on the plantar surface of the foot; note the associated scaling. Courtesy, Jean L. Bolognia, MD.
• In severe cases, blistering and ulceration may be seen.
• Lesions typically resolve in 1–3 weeks but can take much longer or become chronic in elderly patients with venous insufficiency.
• DDx: chilblain lupus; frostbite; lupus pernio (a variant of sarcoidosis involving mainly the nose and ears) (Table 74.3).
Table 74.3
Differential diagnosis and evaluation of skin lesions induced by nonfreezing cold exposure.
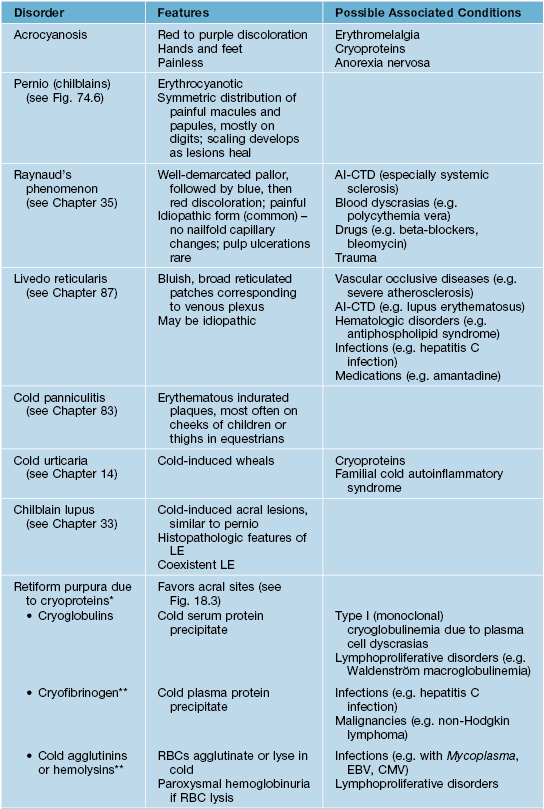
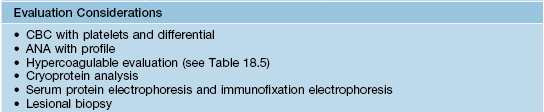
* Acrocyanosis, Raynaud’s phenomenon, livedo reticularis, and cold urticaria can also be observed in association with cryoproteins.
** Rarely cause cold-related occlusion syndromes.
AI-CTD, autoimmune connective tissue disease; CMV, cytomegalovirus; EBV, Epstein–Barr virus; RBC, red blood cell; CBC, complete blood count; ANA, anti-nuclear antibody.
Courtesy, Michael L. Smith, MD.
Cutaneous Injury Due to Chemical Exposure
Chemical Hair Discoloration
Chronic Arsenical Dermatoses
• Chronic arsenicism is characterized by mottled hyperpigmentation with areas of hypopigmentation (Fig. 74.7A); arsenical keratoses on the palms and soles (Fig. 74.7B–C); multiple non-melanoma skin cancers (particularly Bowen’s disease); peripheral neuropathy and internal malignancies (e.g. bladder, lung, liver).
Cutaneous Findings Resulting from Toxic and Heavy Metal Exposure
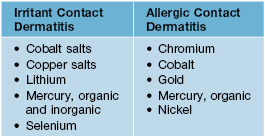
• Various toxic and heavy metals are known to cause irritant and/or allergic contact dermatitis, including the following (Table 74.5):
– Beryllium is a metal known to cause dermatitis and sarcoidosis-like granulomas of the skin and lung.
– Gold, as an elemental salt, can cause a variety of cutaneous eruptions (Table 74.6).
Table 74.6
Cutaneous eruptions associated with gold exposure (as an elemental salt).
| Most Common | Less Common |
| • Lichen planus, lichenoid drug eruption • Allergic contact dermatitis • Pityriasis rosea-like eruptions • Erosive stomatitis |
• Chrysiasis • Erythema nodosum • Erythema multiforme, toxic epidermal necrolysis • Exfoliative dermatitis |
Cutaneous Findings of Frictional and Traumatic Injury to the Skin
Corns and Calluses
• Keratotic lesions resulting from repeated trauma and the subsequent cycle of friction, pressure, and thickening (Fig. 74.8).

Fig. 74.8 Callus plus hard corns. Calluses are broad based and have increased skin markings while corns are round, more sharply defined papules with a central translucency and an interruption in dermatoglyphics. The skin overlying the second and third metatarsal heads is a common location for such lesions. Courtesy, Jean L. Bolognia, MD.
• Corns and calluses can often be mistaken for verrucae; gentle paring of the lesions with a blade and noticing the lesion’s effect on dermatoglyphics can help distinguish between these three entities (Table 74.7).
Table 74.7
Distinguishing features of verrucae, corns, and calluses.
| Lesion | Paring Revelations | Effect on Dermatoglyphics |
| Verruca | Thrombosed capillaries, multiple bleeding points | Interrupted |
| Corn | Central translucent, whitish-yellow core | Interrupted |
| Callus | Layers of yellowish keratin | Accentuated |
• Treatment involves both symptomatic relief and correction of the underlying biomechanical problem:
3. Soft cushions (e.g. silicone sheet, sheep skin) and donut-shaped corn pads.
– Biomechanical correction – properly-fitted footwear and use of appropriate orthotics.
Black Heel (Talon Noir)
• Black macules on the palms or soles due to hemoglobin within the thickened stratum corneum (Fig. 74.9).

Fig. 74.9 Black heel (talon noir) and palm. This black color is due to hemoglobin within the thickened stratum corneum of plantar skin. Courtesy, Julie V. Schaffer, MD.
• Secondary to impact trauma and resolves with paring or spontaneously with time.
Chondrodermatitis Nodularis Helicis (CNH)
• Presents with a skin-colored to erythematous, dome-shaped papule or nodule with a central crust or keratin-filled crater; often exquisitely tender (Fig. 74.10).

Fig. 74.10 Chondrodermatitis nodularis helicis (CNH). Tender, erythematous papulonodule with central scale-crust on the mid antihelix of an older woman. This represented the site most susceptible to pressure-induced ischemia. Courtesy, Kalman Watsky, MD.
• Rx: mostly anecdotal and not standardized (e.g. intralesional CS, topical antibiotics, specially designed CNH pillows for sleeping, cryosurgery, electrodesiccation and curettage, CO2 laser ablation); full-thickness excision is the most definitive and favored treatment for particularly bothersome lesions.
Acanthoma Fissuratum
• Results from ill-fitting eyeglass frames that create a frictional injury to the postauricular sulcus or the upper lateral nose (Fig. 74.11).
Weathering Nodules of the Ears
• Multiple, bilateral, firm (feels like cartilage), asymptomatic, whitish, 2- to 3-mm papules located along the inner rim of the helices in older males >> females (Fig. 74.12).

Fig. 74.12 Weathering nodules. Multiple asymptomatic, small, whitish papules along the helix of an older man with photodamage. Courtesy, Jean L. Bolognia, MD.
• Associated consistently with a history of significant sun exposure and actinic damage.
• DDx: CNH, gouty tophi, calcinosis cutis, elastotic nodules, granuloma annulare.
Sports-Related Dermatoses
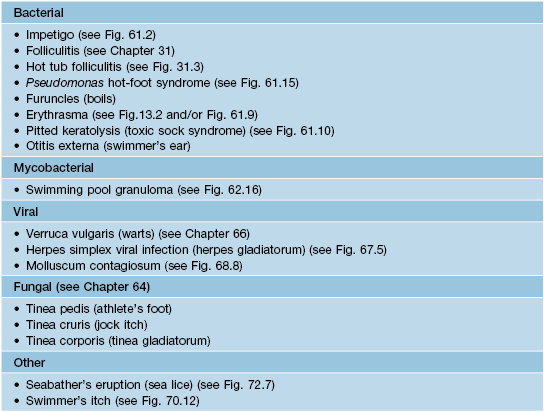
• Participation in sports is often associated with a number of cutaneous injuries, dermatoses, or infections, related to acute and chronic mechanical trauma (Tables 74.8 and 74.9; Fig. 74.13 and 74.14).
Table 74.8
Selected frictional and mechanical dermatoses in athletes.
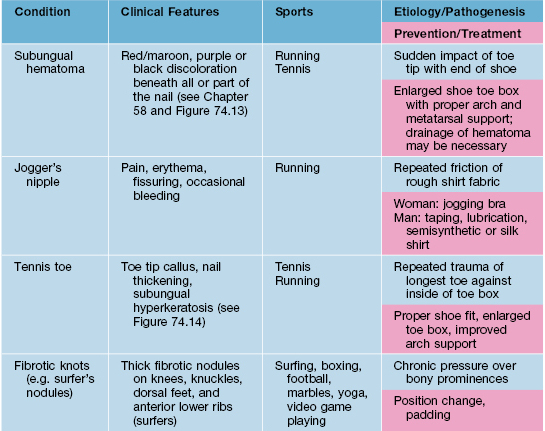
Courtesy, Michael L. Smith, MD.

Fig. 74.13 Subungual hematoma. A common sports-related (e.g. tennis, running, basketball) injury due to the sudden impact of the toe tip with the end of the shoe. Note the subungual dark purplish discoloration, which may be misdiagnosed as melanoma. Clues to the diagnosis of subungual hematoma include: a normal-appearing proximal nail plate upon gentle retraction of the cuticle (arrow); characteristic dermoscopic features (e.g. red-brown to purplish-black round globules); and determination that the discoloration grows out distally. Courtesy, Jean L. Bolognia, MD.
For further information see Ch. 88. From Dermatology, Third Edition.