Emergency Medical Services
Overview and Ground Transport
Perspective
Development of Emergency Medical Services
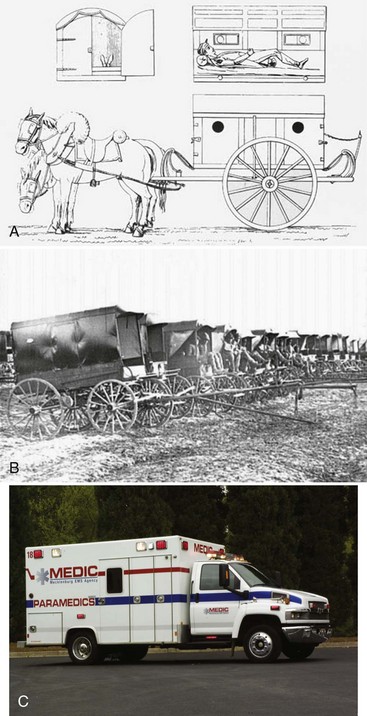
Before the advent of civilian ambulance services, the sick and injured were transported by any means available, including passerby motorists, wagons, farm machinery, delivery carts, buses, and taxicabs. Figure 190-1 depicts the early Larrey ambulance used during the Napoleonic Wars, the Rucker wagon used during the American Civil War, and a modern ambulance used today. In 1865, the Commercial Hospital in Cincinnati established the first hospital-based ambulance service. Four years later, the first city service began at New York’s Bellevue Hospital.1
In 1965, the President’s Commission on Highway Safety recommended a National Accident Response Program to decrease death and injury from highway accidents.2 Results from a second national survey by the National Academy of Sciences–National Research Council were used to draft a white paper entitled Accidental Death and Disability: The Neglected Disease of Modern Society.3 Published in 1966, this document described the hazardous conditions of emergency care provision at all levels and outlined the necessary building blocks for future maturation of emergency medical services (EMS). These national efforts were the impetus for congressional legislation that directed the U.S. Department of Transportation (DOT)–National Highway Traffic Safety Administration (NHTSA) to develop a program for improving emergency medical care.
During the mid-1960s, out-of-hospital cardiac care included field defibrillation programs in Belfast, Northern Ireland, and cardiac arrest research in several U.S. cities.4,5 In 1969, the first National Conference on EMS convened, resulting in the development of a curriculum, certification process, and national registry for the emergency medical technician–ambulance (EMT-A). By 1972, the U.S. Department of Labor recognized the EMT as an occupational specialty.6 Interested physicians and nurses later provided advanced educational courses and practical experiences for the EMTs, and thus began the paramedic providers.7,8
Additional programs prompted Congressional passage of the EMS Systems Act of 1973 (P.L. 93-154), which authorized funding that dramatically improved the development of comprehensive regional EMS delivery systems. Efforts to improve pediatric emergency care occurred in 1984 when Congress adopted the Emergency Medical Services for Children (EMS-C) initiative through the Health Services, Preventive Health Services, and Home Community Based Services Act of 1984 (P.L. 98-555).9 An Institute of Medicine (IOM) study, released in 1994, promoted the integration of EMS-C not just into existing EMS systems but into comprehensive systems of care provision, including injury prevention, primary and definitive care, and rehabilitation services.10
In 1996, the NHTSA published Emergency Medical Services Agenda for the Future, which broadly outlined the principles required for future EMS development.11 All components of an EMS system, both operational and clinical, were identified and discussed. This document has been used by many individuals and organizations as valuable reference material for planning, administration, and forecasting of the future of EMS delivery. More than 40 years since publishing the 1966 white paper, the IOM released a report on the status of emergency care entitled The Future of Emergency Care in United States Health System. The report focused on three separate yet related topics: (1) emergency care: at the breaking point, (2) emergency medical services at the crossroads, and (3) emergency care for children: growing pains.12–14
Emergency Medical Service Systems
Multiple EMS system designs exist, all predicated on the type of community served. Whereas this is a local decision, all states incorporate an administrative office that governs or oversees the provision of EMS activities. Typically the role is not to direct any individual service but to assist in planning, licensing services, and establishing or enforcing the scope and standards for practice. Other functions may include training, examining, certifying, and recertifying providers; record keeping; data collection; and auditing or investigating programs. A description of systems for the 200 most populous cities in the United States is periodically published in the Journal of Emergency Medical Services.15 For simplicity, the following categorization of systems is used: private and public agencies; basic life support (BLS) and advanced life support (ALS) services; and single-tiered, multitiered, and first responder systems.
Basic Life Support and Advanced Life Support Service
BLS systems may be associated with poor survival rates from out-of-hospital cardiac arrest, especially those not incorporating AED technology.16 Alternatively, there is debate on the effectiveness of ALS for medical and traumatic emergencies.17 Despite this evidence, few urban communities across the United States operate solely at the BLS level. Many rural and some suburban EMS services rely on volunteers who may not wish to become advanced-level providers. Because these services may have low call volumes, it becomes more difficult for personnel to maintain advanced skills and a proficient knowledge base. Also, such communities may not have access to medical supervision or hospital sponsorship for ALS care.18
The number of EMT-Ps in any jurisdiction has come under scrutiny, in that cities with more paramedics per capita tend to have lower survival rates.19 Although this may seem implausible, one explanation might be that the number of patient encounters per paramedic decreases and the sharpness of skills degrades when that community is saturated with paramedics.
Single-Tiered, Multitiered, and First Responder Systems
The design of an EMS system is targeted toward providing quality patient care in the briefest time after unexpected injury or illness. A desirable and cost-effective design might include BLS nontransport first responders with short response times (average 2-4 minutes), having the capability of providing early defibrillation and airway support, coupled with ensuing ALS care and transport services.20
Levels of Provider and Scope of Practice
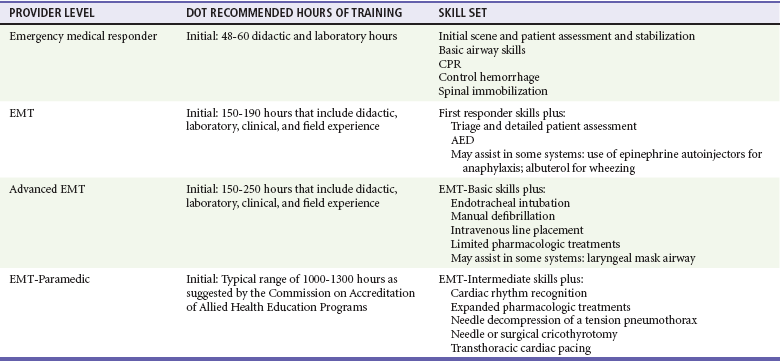
At the federal level, the NHTSA is responsible for development of the education standards and scope of practice for the different certification levels. The National EMS Education Agenda21 and the National EMS Scope of Practice Model22 now define the curriculum, education content, and core competencies for each level of provider. Individual state legislation is responsible for provider levels recognized, initial and continuing medical education requirements at each level, testing, and time intervals for course completion and recertification. The following sections outline the new suggested levels of provider and incorporated skills. Suggested hours of training are listed in Table 190-1.
Emergency Medical Responder
The four elements referred to as the chain of survival by the American Heart Association, which decrease mortality from out-of-hospital cardiac arrest, are early access to care, CPR, defibrillation, and advanced airway management and medications.23 Because early defibrillation may improve the odds of survival of out-of-hospital cardiac arrest, the use of an AED should be a mandatory procedure for the emergency medical responder.24
Emergency Medical Technician
In 1995, the NHTSA released the revised EMT curriculum to include 46 lessons, each with cognitive, effective, and psychomotor objectives.25 Many states expanded the course to include more skills, such as AED use, epinephrine autoinjections, albuterol administration by hand-held nebulizer or metered-dose inhaler, and use of adjunctive airway devices such as the extraglottic airway.
Emergency Medical Technician–Paramedic
The initial training course for the EMT-P includes didactic, clinical, and field education. All course content focuses on technical and professional competencies. Additional modules are included that allow programs to incorporate an expanded scope of practice.26 With the expansion of EMS technology and management career options, many paramedic educational programs have advanced from 1-year certificate curriculums to 2-year associate or 4-year baccalaureate degrees. The National EMS Education Standards document recommends that all paramedic education programs be accredited in the future by the Commission on Accreditation of Allied Health Education Programs.
Future
To complement many of the educational issues addressed in the EMS Agenda for the Future document and at the request of the National Association of State EMS Officials (NASEMSO), the NHTSA along with the Health Resources and Services Administration under the Department of Health and Human Services published the Emergency Medical Services Education Agenda for the Future: A Systems Approach in 2000.27 This document sets forth the processes required to improve EMS education delivery similar to what is realized with other allied health care professions, provides a means of ensuring more instructor flexibility and EMS adaptation to community needs and resources, and moves toward standardization of all levels of certification across the United States. From this document, multiple activities have been completed and published, including the National EMS Core Content, a National EMS Scope of Practice Model of minimum competencies, and the 2009 National EMS Education Standards, which would ultimately replace the current National Standard Curricula for each level of provider. The NASEMSO has been collaborating with multiple EMS stakeholders and the federal partner organizations to assist states in implementing this agenda. The National Registry of Emergency Medical Technicians is in the process of revising their examination, with a new paramedic examination being finalized by January 2013. Future goals include the establishment of a national EMS certification program, consistent levels of provider that build off of each advancing level (emergency medical responder, emergency medical technician, advanced emergency medical technician, and paramedic), the requirement for educational programs to be nationally accredited, and the limitation of examinations only to those graduates who completed these accredited programs.
Material Resources
Before the mid-1960s, few if any regulations governed system design, operations, and equipment. As EMS development progressed, guidelines for emergency vehicle specifications were adopted by the DOT and equipment lists were proposed. Today, collaborative efforts from multiple professional medical colleges and organizations continue to publish documents that recommend design, equipment, and medications for ambulances.28
Medications
During the 1980s, many believed that prehospital drug administration was unjustified and simply delayed hospital transport.29,30 Moreover, although there was a profound paucity of outcomes-based research into the use of various medications and practices in the prehospital environment, this has been improved in recent years.31 There is significant evidence for early defibrillation and certain advanced cardiac life support medications, which are carried by most ALS services.24,32 The wide variety of alternative medications is less uniform. This includes respiratory and anaphylaxis medications, preparations for altered mental status, analgesics, and antiemetics. Medications are traditionally administered in the field by the parenteral route, but the intranasal route is becoming popular for certain preparations. The beneficial aspects are that absorption is rapid with an onset of action similar to that of parenteral administration. Medications that are commonly administered intranasally are naloxone for narcotic overdose, midazolam for pediatric seizure, and fentanyl for pain control.33,34
Ambulances
Three basic ambulance vehicle designs are recognized by the DOT: type I, type II, and type III. Both type I and type III ambulances incorporate a modular patient compartment mounted on a conventional truck and van chassis, respectively. The type II vehicle is a standard van. The larger medium-duty vehicle, mounted on a business-class chassis, has become popular in recent years. This configuration requires less periodic maintenance and offers extended service time. Each ambulance manufacturer promotes various interior cabinetry and all include sufficient lighting, outlets for 110-volt equipment, suction, oxygen systems, and external audible and visual warning devices. The six-pointed blue star, or Star of Life, surrounding the staff of Aesculapius is recognized worldwide as the standard symbol for EMS.35
Communications
Emergency Medical Dispatch
Dispatching encompasses multiple elements that assist patients in receiving expeditious medical care.36 There are several recognized programs with varying sensitivities and specificities that assist call-takers in identifying a patient’s acuity level on the basis of the caller’s information.37,38
Oversight
Local
An EMS medical director is a physician with specialized interest and knowledge of patient care activities unique to the out-of-hospital environment. Medical oversight must extend from the communications center through all components of field care. Typically, a contractual arrangement for services provides the physician with administrative authority to implement patient care protocols, to interact with all aspects of the system, and to remove a provider from practice if medical care or behavior is substandard. Published guidelines describing the activities and performance of an EMS medical director have been prepared by the American College of Emergency Physicians, National Association of EMS Physicians, NHTSA, and Health Resources and Services Administration.39–41
Indirect Medical Control
Once patient care protocols are developed and implemented, there must be mechanisms, such as retrospective patient care report review or direct field observation, for evaluation of individual and system performance and patient outcome. Deviations from specific protocols may reflect problems with individual EMTs, medical control personnel, or the protocol itself, each requiring education and re-evaluation. Deficiencies, both operational and clinical, should be identified for appropriate remediation to occur, which may be in the form of counseling, educational instruction, or revisions of system design or patient care protocols.42 Competency, knowledge retention, and skill performance are measurable parameters. Time standards (e.g., out-of-chute time [time from ambulance notification to deployment], response time, and scene time) are equally important measures.43–46
Direct Medical Control
Agencies and organizations involved in EMS development and oversight are listed in Table 190-2.
Table 190-2
Emergency Medical Services Resource and Contact Information
| RESOURCE | URL |
| Advocates for EMS | www.advocatesforems.org |
| American Ambulance Association | www.the-aaa.org |
| American College of Emergency Physicians | www.acep.org |
| Centers for Disease Control and Prevention | www.cdc.gov |
| Commission on Accreditation of Ambulance Services | www.caas.org |
| EMS Division, NHTSA | www.nhtsa.dot.gov/people/injury/ems |
| Maternal and Child Health Bureau, EMS-C | www.ems-c.org |
| National Association of EMS Educators | www.naemse.org |
| National Association of EMS Physicians | www.naemsp.org |
| National Association of EMTs | www.naemt.org |
| National Association of State EMS Officials | www.nasemso.org |
| National Registry of EMTs | www.nremt.org |
Out-of-Hospital Medical Care and Controversies in Management
Airway Support and Respiratory Emergencies
Interventions
Respiratory complaints account for a significant number of EMS responses. Basic measures to control and support a patient’s airway include manual maneuvers (e.g., chin lift or jaw thrust), oral and nasopharyngeal devices, and bag-mask ventilation. At a more advanced level, interventions may include use of extraglottic-type airway devices (e.g., Combitube, laryngeal mask airway, or laryngeal tracheal airway), which have been shown to enable faster placement and to provide improved minute ventilation. Studies have shown that basic-level EMTs were able to successfully place laryngeal mask airways in simulated arrest models and also demonstrated an improved minute ventilation with these devices compared with bag-valve mask ventilations.47,48 Similar studies have demonstrated that laryngeal mask airways are more successful than endotracheal intubation for paramedics because they provide a faster technique, require fewer attempts for successful insertion, and improve ventilation.49
Commonly used by air medical services, drug-assisted intubation (DAI) and rapid sequence intubation (RSI) procedures are well established in ground transport services, despite a lack of supporting evidence. Although many services routinely perform intubation, several studies have challenged the effectiveness of out-of-hospital intubation, particularly in view of an alarming incidence of esophageal intubation in some systems and poor outcomes with the use of RSI for head-injured patients.50–53 One prospective, randomized study of pediatric out-of-hospital airway management concluded that in the urban setting, bag-mask ventilation may be superior to intubation in certain groups of patients.54 Although controversy exists and the debate will continue, most would agree that to have a successful airway management program, the educational and quality management component must be meaningful and should be as comprehensive and compulsive as possible.55 For programs using DAI or RSI procedures, the experiential component should include operating room time and simulator sessions. Ideally, training would also occur in an emergency department setting where patients requiring emergent intubation would potentially have the full complement of confounding variables (e.g., combative status, full stomachs, blood and vomit in the airway). Such training may be difficult or impossible to achieve, particularly ongoing maintenance of skills sessions, especially in rural communities. Unless EMS systems perform a large number of intubations, with at least several intubations per provider per year, use of an extraglottic device for tracheal intubation should be strongly considered.56
Traditionally used in the hospital, continuous positive airway pressure (CPAP) is intensifying in the out-of-hospital setting. The effectiveness of out-of-hospital use of CPAP has been demonstrated; however, patient outcome studies have been limited.57,58 Out-of-hospital use would require strict protocols that outline such variables as indications and contraindications, clinical applications, mental status assessment, hemodynamic status, and mechanisms for transfer of the patient at the hospital.
Cardiovascular Emergencies
Early research demonstrated the effectiveness of early defibrillation for termination of ventricular fibrillation and improvement of survival rates from sudden cardiac death.59 Advances in technology have improved such that defibrillators, traditionally used by paramedics, are now used by a variety of public safety responders and bystanders. Public access defibrillation programs are continuing to be implemented throughout the country, with devices being placed in high-volume, populous, and secluded areas such as airports and airplanes, casinos, churches, office buildings, and other locations identified as high risk for resuscitation.60 The acquisition and transmission of out-of-hospital 12-lead electrocardiograms is becoming more prevalent as well. Although it is expensive to implement, several studies have revealed minimal delays in scene time while the electrocardiogram is obtained and a shorter time to intervention (thrombolytic administration or catheterization laboratory admission) by use of this technology.61,62
A factor now recognized to improve survival from cardiac arrest is uninterrupted or minimally interrupted chest compressions. Each interruption of compressions (e.g., while intubating, checking for pulses, analyzing rhythms) decreases coronary perfusion pressure, which in turn decreases cellular respiration.63 This same tenant may be used for prearrival telephone CPR instructions in that more bystanders may be willing to perform continuous chest compressions if artificial ventilations were discarded.
Although the statistics for cardiac arrest survival across the United States are dismal, those who do survive may suffer some degree of hypoxic encephalopathy. Recent evidence suggests that with cooling of patients who achieve a spontaneous return of circulation after cardiac arrest, especially with ventricular fibrillation as the initial rhythm, higher survival rates and level of neurologic functioning are achieved.64,65 The explanation may be due to several mechanisms, including a decrease in neuronal cell oxygen consumption, cell membrane protection, slowing of degradative reactions resulting from reperfusion, and limiting of acidosis.66 International guidelines now call for the institution of hypothermia for patients who are resuscitated from cardiac arrest, and many out-of-hospital systems have implemented protocols that may include administration of chilled saline, sedation, or neuromuscular blockers in coordination with receiving hospital emergency departments.
Medications
Traditional cardiac medications recommended by advanced cardiac life support are used by most ALS systems. Recent investigations involving amiodarone as an out-of-hospital agent to terminate refractory ventricular fibrillation have resulted in higher survival rates to hospital arrival; however, improvement in survival to discharge is still not significant.67 Whether amiodarone should replace lidocaine for out-of-hospital ventricular fibrillation requires further investigation, although many systems have already made this expensive change. The use of out-of-hospital fibrinolytic agents for acute ST elevation myocardial infarction has not gained wide acceptance and may be a useful intervention only for systems having prolonged transport times or if hospitals may not have catheterization or intervention facilities available. Future recommendation for out-of-hospital use of these agents remains speculative.
Traumatic Emergencies
Interventions for specific medical emergencies, such as cardiac arrest (i.e., defibrillation, intubation, intravenous line, and medication administration), may be effectively performed while on the scene or before hospital transport. Alternatively, it is widely accepted that most interventions for traumatic injuries should be performed en route to the hospital, and all efforts should be extended to reduce on-scene time. Only two interventions should be considered for critical injuries, control of the airway to reverse hypoxemia and to prevent aspiration and stopping of uncontrolled hemorrhage. Although it is a routine part of prehospital trauma care, tracheal intubation is not known to be beneficial for severely injured patients.68 There are many potential drawbacks to prehospital intubation for major trauma. To be successful, paramedics should rapidly place the endotracheal tube correctly, assess and confirm the placement, and secure the tube to prevent displacement. In addition, providing the correct minute and tidal volumes is equally important. Inadvertent hyperventilatory rates may impair cardiac output and cause further tissue damage. Patients sustaining blunt head injury pose special problems that should be expeditiously addressed and resolved. Intubation is but one means of providing ventilatory assistance and airway protection, but misadventure, complications, and improper postintubation care may negate these potential benefits. Attempting to intubate head-injured patients may result in dental or soft tissue damage in those patients with clenched teeth, and intracranial pressure may be exacerbated from an intact gag reflex or from subsequent regurgitation. Studies on the use of RSI in head-injured patients reveal that patients experience significant hypoxia and bradycardia during the procedure, and outcome is actually worse.46 Thus the role of RSI in prehospital airway management in trauma patients is in question, just as it is for medical patients. The use of extraglottic airway devices may be a promising addition to prehospital airway management in trauma patients. Routine use of prehospital intubation is not recommended unless the system can ensure that its providers meet the standards previously outlined. Emergent hemorrhage control is also essential in reducing mortality in severe trauma. For internal bleeding, limiting of total prehospital time and transfer to definitive surgical care are paramount. Recent evidence on the battlefield has demonstrated the effectiveness of tourniquet application to extremity wounds. These devices may have application in the civilian setting, are quick and easy to apply, and do not result in the complications once thought to exist.69
The issue of intravenous fluid administration has gained controversy over the years. High-volume intravenous fluid for hemodynamic instability resulting from traumatic injury has traditionally been the accepted standard in most out-of-hospital care systems. Previous data, however, support a paradigm shift to restrictive or hypotensive resuscitation for penetrating truncal injuries. Restoration of hemodynamic stability with fluid resuscitation before definitive surgical hemostasis may lead to increased morbidity.70 The use of prehospital intubation and high-volume crystalloid infusion bears unfortunate similarity to the widespread, unsupported adoption of the pneumatic antishock garment in the 70s and 80s. Despite lack of evidence of benefit and significant evidence of harm or potential harm, these practices are notoriously difficult to discontinue once adopted.
Interfacility and Specialized Transports
Interfacility transfer of patients that is medically indicated must fall under a set of requirements referred to as the Emergency Medical Treatment and Active Labor Act.71 Although the EMS system providing the transport plays a key role, these guidelines primarily involve particular information and obligations that must be satisfied by the transferring and receiving facilities before transfer. An unstable patient should not be transferred to another facility at the request of a managed care organization unless the transferring hospital is incapable of providing standard care and the receiving hospital does have the capability to manage the condition and foreseeable complications. Box 190-1 lists various requirements that should be completed before a patient is transferred to another facility.
As with any EMS activity, all interfacility transports should be reviewed for appropriateness of transfer and medical care provided. In 1993, the Practice Management Committee of the American College of Emergency Physicians updated the 1990 policy statement on interfacility transfers.72
References
1. Haller, JS. The beginnings of urban ambulance service in the United States and England. J Emerg Med. 1990;8:743.
2. President’s Commission on Highway Safety. Health, Medical Care, and Transportation of the Injured. Washington, DC: U.S. Government Printing Office; 1965.
3. Division of Medical Sciences, National Academy of Sciences–National Research Council. Accidental Death and Disability: The Neglected Disease of Modern Society. Washington, DC: National Academy of Sciences; 1966.
4. Pantridge, JF, Geddes, JS. A mobile intensive care unit in the management of myocardial infarction. Lancet. 1967;2:271.
5. Cobb, LA, Alvarez, H, Kopass, MK. A rapid response system for out-of-hospital cardiac emergencies. Med Clin North Am. 1976;60:283.
6. U.S. Department of Transportation–National Highway Traffic Safety Administration. Basic Training Program for Emergency Medical Technician–Ambulance. Washington, DC: U.S. Department of Transportation; 1971.
7. Lewis, RP, et al. Effectiveness of advanced paramedics in a mobile coronary care system. JAMA. 1979;241:1902.
8. Nagel, EL, et al. Telemetry–medical command in coronary and other mobile emergency care systems. JAMA. 1970;214:332.
9. Law of the 98th Congress, Health Services, Preventive Health Services, and Home Community Based Services Act of 1984, Public Law 98-555. 1984.
10. Institute of Medicine, National Academy of Sciences. Emergency Medical Services for Children. Washington, DC: National Academy of Sciences; 1993.
11. U.S. Department of Transportation–National Highway Traffic Safety Administration. Emergency Medical Services Agenda for the Future. Washington, DC: U.S. Department of Transportation; 1996.
12. Institute of Medicine, Committee of the Future of Emergency Care in the U.S. Health System. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academy Press; 2006.
13. Institute of Medicine, Committee of the Future of Emergency Care in the U.S. Health System. Emergency Medical Services at the Crossroads. Washington, DC: National Academy Press; 2006.
14. Institute of Medicine, Committee of the Future of Emergency Care in the U.S. Health System. Emergency Care for Children: Growing Pains. Washington, DC: National Academy Press; 2006.
15. Williams, DM, Ragone, M. 2009 JEMS 200-city survey. Zeroing in on what matters. JEMS. 2010;35:38.
16. Nichol, G, et al. Effectiveness of emergency medical services for victims of out-of-hospital cardiac arrest: A metaanalysis. Ann Emerg Med. 1996;27:700.
17. Bickell, WH, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105.
18. Custalow, CB, Armacost, M, Honigman, B. Unique curriculum for emergency medicine residents as medical directors for rural out-of-hospital agencies. Acad Emerg Med. 2000;7:6743.
19. Davis, R, Many lives are lost across USA because emergency services fail. USA Today 2005. www.usatoday.com/news/nation/ems-day1-cover.htm.
20. Nichol, G, et al. Cost-effectiveness analysis of potential improvements to emergency medical services for victims of out-of-hospital cardiac arrest. Ann Emerg Med. 1996;27:711.
21. National EMS Education Agenda. www.nasemso.org/EMSEducationImplementationPlanning/documents/FinalEducationAgenda.pdf.
22. National EMS Scope of Practice Model. www.nasemso.org/EMSEducationImplementationPlanning/documents/EMS_Feb07_PMS314SOP.pdf.
23. Cummins, RO, et al. Improving survival from sudden cardiac arrest: The “chain of survival.”. Circulation. 1991;83:1832.
24. Berdowski, J, et al. Survival and health care costs until hospital discharge of patients treated with onsite, dispatched or without automated external defibrillator. Resuscitation. 2010;81:962.
25. U.S. Department of Transportation–National Highway Traffic Safety Administration. Emergency Medical Technician–Basic: National Standard Curriculum. Washington, DC: U.S. Department of Transportation; 1994.
26. U.S. Department of Transportation–National Highway Traffic Safety Administration. Emergency Medical Technician–Paramedic: National Standard Curriculum. Washington, DC: U.S. Department of Transportation; 1998.
27. U.S. Department of Transportation–National Highway Traffic Safety Administration. Emergency Medical Services Education Agenda for the Future: A Systems Approach. Washington, DC: U.S. Department of Transportation; 2000.
28. American College of Surgeons Committee on Trauma, American College of Emergency Physicians, National Association of EMS Physicians, Pediatric Equipment Guidelines Committee–Emergency Medical Services for Children (EMSC) Partnership for Children Stakeholder Group, American Academy of Pediatrics Position Paper. Equipment for Ambulances. Prehosp Emerg Care. 2009;13:364.
29. Smith, JP, Bodai, BI. The urban paramedic’s scope of practice. JAMA. 1989;253:544.
30. Shuster, M, Chong, J. Pharmacologic intervention in prehospital care: A critical appraisal. Ann Emerg Med. 1989;18:192.
31. Millin, MG, et al. Evolution of the literature identifying physicians’ roles in leadership, clinical development, and practice of the subspecialty of emergency medical services. Prehosp Disaster Med. 2011;26:49.
32. Neumar, CW, et al. Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S729–S767.
33. Barton, ED, et al. Intranasal administration of naloxone by paramedics. Prehosp Emerg Care. 2002;6:54.
34. Lahat, E, et al. Comparison of intranasal midazolam and intravenous diazepam for treating febrile seizures in children: Prospective randomized study. BMJ. 2000;321:83.
35. Department of Transportation–National Highway Traffic Safety Administration. “Star of Life” Emergency Medical Care Symbol. Washington, DC: U.S. Department of Transportation; 1979.
36. National Association of Emergency Medical Services Physicians Position Paper. Emergency medical dispatching. Prehosp Disaster Med. 1989;4:163.
37. Feldman, MJ, et al. Comparison of the medical priority dispatch system to an out-of-hospital patient acuity score. Acad Emerg Med. 2006;13:954.
38. Hinchey, P, et al. Low acuity EMS dispatch criteria can reliably identify patients without high-acuity illness or injury. Prehosp Emerg Care. 2007;11:42.
39. Alonso-Serra, H, Blanton, D, O’Connor, RE. Position paper, National Association of EMS Physicians: Physician medical direction in EMS. Prehosp Emerg Care. 1998;2:153.
40. Polsky, S, et al. Guidelines for medical direction of prehospital EMS. Ann Emerg Med. 1993;22:742.
41. U.S. Department of Transportation–National Highway Traffic Safety Administration, National Association of EMS Physicians, American College of Emergency Physicians, Health Resources and Services Administration–Maternal and Child Health Bureau. Guide for Preparing Medical Directors. Washington, DC: U.S. Department of Transportation; 2001.
42. Persse, DE, Key, CB, Baldwin, JB. The effect of a quality improvement feedback loop on paramedic-initiated nontransport of elderly patients. Prehosp Emerg Care. 2002;6:31.
43. Blackwell, TH, Kaufman, JS. Response time effectiveness: Comparison of response time and survival in an urban emergency medical services system. Acad Emerg Med. 2002;9:288.
44. Pons, PT, et al. Paramedic response time: Does it affect patient survival? Acad Emerg Med. 2005;12:594.
45. Blackwell, TH, et al. Lack of association between prehospital response times and patient outcomes. Prehosp Emerg Care. 2009;13:444.
46. Newgard, CD, et al. Emergency medical services intervals and survival in trauma: Assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010;55:235.
47. Kurola, J, et al. Airway management in cardiac arrest—comparison of the laryngeal tube, tracheal intubation and bag-valve mask ventilation in emergency medical training. Resuscitation. 2004;61:149.
48. Guyette, FX, et al. Feasibility of laryngeal mask airway use by prehospital personnel in simulated pediatric respiratory arrest. Prehosp Emerg Care. 2007;11:245.
49. Hoyle, JD, et al. Comparative study of airway management techniques with restricted access to patient airway. Prehosp Emerg Care. 2007;11:330.
50. Mizelle, HL, et al. Preventable morbidity and mortality from prehospital paralytic assisted intubation: Can we expect outcomes comparable to hospital-based practice? Prehosp Emerg Care. 2002;6:472.
51. Davis, DP, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444.
52. Katz, SH, Falk, JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:62.
53. Davis, DP. Prehospital intubation of brain-injured patients. Curr Opin Crit Care. 2008;14:142.
54. Gausche, M, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. JAMA. 2000;283:783.
55. National Association of EMS Physicians Position Paper. Drug-assisted intubation in the prehospital setting. Prehosp Emerg Care. 2006;10:260.
56. Burton, JH, et al. Endotracheal intubation in a rural EMS state: Procedure utilization and impact of skills maintenance guidelines. Prehosp Emerg Care. 2003;7:352.
57. Kallio, T, Kuisma, M, Alaspää, A, Rosenberg, PH. The use of prehospital CPAP treatment in presumed acute severe pulmonary edema. Prehosp Emerg Care. 2003;7:209.
58. Kosowsky, J, et al. Prehospital use of CPAP for presumed pulmonary edema: A preliminary case series. Prehosp Emerg Care. 2006;5:190.
59. Eisenberg, MS, et al. Cardiac arrest and resuscitation: A tale of 29 cities. Ann Emerg Med. 1990;19:179.
60. Folke, F, et al. Location of cardiac arrest in a city center: Strategic placement of automated external defibrillators in public locations. Circulation. 2009;120:510.
61. Patel, RJ, Vilke, GM, Chan, TC. The prehospital electrocardiogram. J Emerg Med. 2001;21:35.
62. Ferguson, JD, et al. The prehospital 12-lead electrocardiogram: Impact on management of the out-of-hospital acute coronary syndrome patient. Am J Emerg Med. 2003;21:136.
63. Bobrow, BJ, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299:1158–1165.
64. Peberdy, MA, et al. Part 9: Post Cardiac Arrest Care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S768–S786.
65. Bernard, SA, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557.
66. The Hypothermia After Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549.
67. Kudenchuk, PJ, et al. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med. 1999;341:871.
68. Davis, DP, et al. The relationship between out-of-hospital airway management and outcome among trauma patients with Glasgow Coma Scale Scores of 8 or less. Prehosp Emerg Care. 2011;15:184.
69. Kragh, JF, Jr., et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249:1.
70. Haul, ER, et al. Prehospital intravenous fluid administration is associated with higher mortality in trauma patients: A National Trauma Data Bank analysis. Ann Surg. 2011;253:371.
71. Testa, PA, Gang, M. Triage, EMTALA, consultations, and prehospital medical control. Emerg Med Clin North Am. 2009;27:627.
72. American College of Emergency Physicians. Appropriate interhospital patient transfer. Ann Emerg Med. 1993;22:766.