215 Emergency Medical Services and Disaster Medicine
• Emergency medical services (EMS) consist of a heterogeneous group of entities that vary according to urbanization, training procedures, skill level of practitioners, resources, and scope.
• Although EMS research is developing rapidly, controversy exists over the role of EMS interventions and protocols in commonly encountered conditions such as trauma and cardiovascular emergencies.
• Disaster medicine encompasses planning, resource allocation, and health care response to any event—natural or man-made—that overwhelms the resources of a particular locality.
• Weapons of mass destruction have the potential to cause severe physical damage and health concerns that require specific, targeted planning and coordination for emergency care personnel.
Introduction and History
An emergency medical services (EMS) system can be defined as “a coordinated arrangement of resources (including personnel, equipment, and facilities) organized to respond to medical emergencies, regardless of the cause.”1 Modern EMS systems in the United States have their origins largely in battlefield medicine.2–6 Indeed, it was a surgeon in the Napoleonic military campaign who pioneered the concept of rapid response to injured soldiers in the field of combat.3 Baron Larrey, the “father of modern prehospital care,” developed a systematic approach to combat trauma in which ambulances transported wounded soldiers from the battlefield to organized medical stations. In the American Civil War, ambulances were placed under structured medical direction. Successive advances in technology and EMS organization in later wars resulted in significantly decreased mortality rates for battle combatants who were transported to field hospitals.5
Although civilian “rescue societies” and ambulance services existed from the mid-1800s, the most significant nonmilitary advancement in EMS occurred in the 1950s with the establishment of life support training programs through the Chicago Fire Department. From this effort the basis for the now widely accepted emergency medical technician (EMT) and paramedic training programs were formed.2 By the 1960s, some regions had nascent ambulance systems with paramedics trained in advanced life support (ALS) techniques, although others developed a separate system of “heartmobiles” with physicians on board to provide care only for cardiac emergencies.7
The need for sophisticated, coordinated EMS systems was brought to the national spotlight in 1966 with publication of the National Academy of Sciences paper titled “Accidental Death and Disability: The Neglected Disease of Modern Society.” This paper noted that few people were trained in advanced resuscitation, no widely accepted standards had been established for training ambulance personnel, and communication systems and supplies were lacking. This report spurred a national, organized effort to increase awareness of traumatic disease and the need for development of a comprehensive EMS system.5 Congress responded with the National Highway Safety Act of 1966 and the EMS Systems Act of 1973, which authorized federal grants to state, local, and regional governments for the development of EMS systems within a specified “systems approach” framework.8 In 1981, however, guaranteed federal funding for EMS was replaced with state block grants and increased financial insecurity.4 Currently, nearly 1 million people are certified in some form as emergency response personnel, and nearly 20 million patients are treated in the EMS system annually, but heterogeneity in system design, scope, and certification requirements persists.9
EMS System Design
EMS systems are, arguably, some of the most complex organizational entities in modern society. They include representatives from municipalities of every size, law enforcement, fire and safety, health care, transportation services, and community groups. Federal governing bodies define the necessary components of EMS systems but do not directly oversee organization or management. Coordination between agencies is essential but often difficult to achieve.1 Ideally, EMS system design is centered around the particular needs of the community that it serves, with one standard characteristic: emergency medical personnel act as on-scene “physician surrogates” to provide appropriate life support techniques.7 Common models categorize different systems in terms of control by the public or private agencies, rural or urban communities, and single-tiered or multitiered systems.
Rural and Urban EMS Systems
The design of and challenges faced by EMS systems are often significantly different between rural and urban areas. In general, rural systems developed later than urban ones and are more likely to be staffed with unpaid volunteers.3 These volunteer-based organizations may be public or private and are generally nonprofit entities. Volunteers are usually citizens with outside employment who offer their services on an unpaid basis for emergency response, training, and community education. Funding is largely through taxes and municipal support, although private donations and fund-raising are often necessary. Volunteer EMS systems face many challenges that are representative of rural systems as a whole, namely, high cost to cover large geographic areas with few citizens, high response times, lower levels of training, and relatively low patient volumes.10,11 Urban EMS systems have their own distinct set of difficulties, among them high patient volumes, traffic congestion, and limited resources.
Evidence suggests that rural emergency morbidity and mortality is significantly greater than that for comparable urban patients. Reasons for this difference include longer response and scene times, lower patient volumes, and less overall training for first responders.12–15 Technologic advances such as “E911” (enhanced 911) show some promise in significantly reducing emergency responders’ transport time to the scene.16 Adapting specific on-scene protocols and increasing access to high-quality medical care (prehospital and in-hospital) in rural areas have also been suggested as possibilities to decrease the gap in rural-urban adverse outcomes.15
EMS System Organization, Training, and Transport Types
Dispatch and Medical Control
In the United States, 99% of the population has access to 911 for emergency calls.7 Most dispatch centers use E911, a system whereby the caller’s location is shown on the dispatch operator’s screen. Formal training for 911 dispatch personnel exists, and national guidelines that advocate for certification standards have been established.17 There is a trend toward consolidation of all emergency calls into one 911 center, where dispatchers take calls and then directly relay information to the appropriate EMS or public safety agency. Dispatch actions and instructions may be shaped by established guidelines that allow adaptation to the situation at hand or by more rigid protocols that detail a specific plan of action. Some agencies may rely on computerized algorithms to assist dispatch; a controlled trial of British nonurgent emergency calls found that using a computerized decision tool plus either nurse or paramedic input resulted in more than half the calls triaged as not needing an emergency ambulance. However, only 20% of these callers chose to cancel the ambulance, and this group had similar hospital admission rates as those triaged as needing emergency transport.18
EMS systems rely heavily on both online (direct) and off-line (indirect) medical control. Physician involvement in EMS medical control developed as physicians spent less time directly in the field and paramedics increased their training and ability to act as physician surrogates. Every EMS system is headed by a medical director, a physician with or without specialty training who has direct authority over operation of the system, performance of emergency personnel, and patient care. Standardized guidelines and requirements for EMS medical direction have been published by the American College of Emergency Physicians (ACEP).19,20
The evidence basis for improved patient outcomes with online medical control is mixed. It has been shown to significantly increase on-scene time, and orders given rarely deviate from existing protocols.21–23 However, there is some evidence that online medical direction may decrease the use of inappropriate resources while preserving outcomes in some patients.24 The greatest benefits of online direction may be in resolving difficult ethical or medicolegal situations on scene and in notifying receiving hospitals of incoming critical patients so that resources can be assembled and are ready before arrival of the patient.
Off-line medical direction refers to written protocols that guide common patient interactions, as well as continuing education and quality assurance initiatives. EMS systems have specific protocols for commonly encountered situations that, ideally, should improve patient outcomes and reduce time at the scene. Protocols should be developed on the basis of patient history, mechanism of injury, physiologic characteristics, local hospital capability, and transport times. Medical directors should be active in developing and implementing protocols, as well as in training responders in their application and quality evaluation of patient records.25 Research indicates that use of well-developed standing protocols significantly reduces on-scene time and decreases inappropriate treatment in the field.26 Furthermore, diagnostic accuracy plus agreement with physician assessment of patients is generally high.27
EMS Responder Personnel
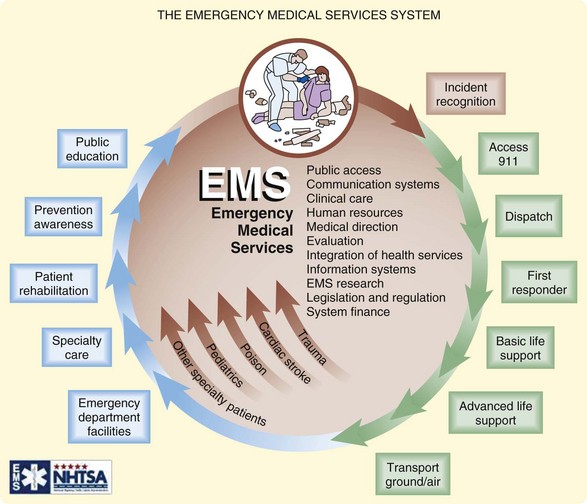
Before the National Academy of Sciences paper on trauma in the 1960s, few standardized training programs existed for EMS personnel. Subsequent creation of the Department of Transportation resulted in a formalized 70-hour curriculum for basic EMT certification. Passage of the EMS Systems Act of 1973 provided millions of dollars for EMS training, equipment, and research and identified basic elements that must be included in all EMS systems (Fig. 215.1).28 However, until recently, heterogeneity of regional systems persisted such that a 1996 survey identified more than 40 different types of EMS personnel certification across the country.29
Recognition of the wide regional variation in training standards and skill levels led to development of the National Highway Traffic Safety Administration National EMS Scope of Practice Model in 2005. This consensus document promotes national standardization in training and education to improve consistency within and among agencies, increase public understanding of EMS roles, and move toward a coordinated national EMS system.9 The model advocates four separate and sequential levels of certification—emergency medical responder, EMT, advanced EMT, and paramedic—and clearly defines minimum educational levels and skill sets for each. Most states have already implemented or are in the process of testing these national guidelines for local use.
There is some evidence basis for the current multilevel EMS personnel system. Early EMS research found a significant reduction in mortality from cardiac arrest with the use of paramedic responder crews versus EMT-Bs.30,31 Outcomes in trauma have also been shown to improve significantly when ALS-capable ambulances are on scene as compared with BLS personnel.32,33 However, other studies evaluating paramedic- and non–paramedic-containing crews found mixed results. In general, on-scene time is significantly longer for crews in which one or all of the responders are paramedics.34,35 Paramedic crews had higher skill levels and provided more on-scene interventions, but some authors suggest that their presence on every ambulance may not be warranted.36
EMS Vehicles, Equipment, and Types of Transport
Equipment available on emergency transport vehicles varies by both type of vehicle and the skill level of responder personnel on board. Joint guidelines developed by the ACEP and the American College of Surgeons detail the minimum necessary supplies for appropriate patient care.36 Items needed for basic-level interventions include ventilation and airway equipment, monitors and defibrillators, immobilization devices and bandages, mobile communication devices, obstetric and pediatric specialty equipment, and infection control and injury prevention measures. Ambulances with advanced life support capability (EMT-I or EMT-P) should contain all the aforementioned basic equipment plus vascular access material, advanced airway and ventilation tools, advanced cardiac life support and other protocol-driven medications, more sophisticated monitoring, and advanced diagnostic equipment (e.g., glucometer, pulse oximeter). In addition, all vehicles should have some measure of extrication equipment for use in patient rescue.
Air Medicine Transport
Although a full description of air ambulance systems is beyond the scope of this chapter, this method of transportation plays a crucial role in the transport and transfer of critically ill patients. Ground emergency transport remains the mainstay of prehospital transport and transfer; however, air medical services can have a significant impact on patient care in selected conditions.37,38 The benefits of air ambulance transport are largely attributed to increased speed and higher crew skill levels; however, safety, cost, and limited evidence to support improved outcomes are major concerns.
The literature on selected prehospital air transport focuses largely on trauma patients and presents mixed evidence for its use. Retrospective evaluations of trauma patients have shown a significant decrease in mortality with helicopter transport39,40; however, several studies have found no difference in patient outcomes for both trauma and nontrauma conditions36–38 and that air transport is overused and costly.40–44 Criteria for air transport can vary widely by EMS system, and overtriaging is common.45
The National Association of EMS Physicians has published guidelines regarding the use of various methods of air transport, as well as which patients are most likely to benefit from its use. In general, helicopters are best used for transport involving a shorter distance (less than 100 miles) but are subject to weather concerns. Fixed-wing aircraft are preferable for distances greater than 100 miles and are less dependent on inclement weather, but they must land at airports (thereby prolonging transport time). Severely injured trauma patients at some distance from a regional trauma center are most likely to benefit from air transport or transfer; critically ill nontrauma, cardiac, pediatric, and possibly obstetric patients may also have improved outcomes in selected situations.46
The safety of both patients and medical staff is a prominent issue in air medical transport. As the number of flights has increased in recent years, so has the number of aircraft accidents. Between 2002 and 2005, 55 crashes occurred and resulted in 54 fatalities; the incidence of aircraft accidents per number of flights increased as well.47 Patient safety in flight is also of concern; an estimated 5% of patients suffer a “critical event” (decompensation or deterioration) during transport.45 Factors such as weather, time of the day, terrain, communication difficulties, and medical crew training have been found to be associated with adverse events, but more study is needed to improve air transport safety.
Current Controversies in EMS
Cardiovascular Emergencies
Some of the earliest organized EMS research focused on cardiac arrest and early CPR and defibrillation. A 20-year review of EMS systems in 29 cities found that systems with a single emergency responder were associated with lower rates of survival of patients in cardiac arrest than were two-responder (EMT and paramedic) systems, largely because of early CPR in the latter.48 Time to defibrillation has consistently been found to improve outcomes after cardiac arrest.49,50 A 25-year retrospective review of cardiac arrest with EMS intervention found that survival rates remained unchanged; however, the authors suggested that improvements in EMS delivery, such as dispatcher-assisted bystander CPR and early defibrillation, balanced the adverse temporal trends that would otherwise have increased mortality rates.51 New life support guidelines emphasize the role of EMS dispatch in instructing hands-only CPR to bystanders and widespread use of AEDs, both of which are considered to be an important adjunct to trained EMS response.52,53
Prehospital Resuscitative Interventions
Advanced resuscitative techniques, such as endotracheal intubation and intravenous fluid administration, are frequently performed by skilled paramedics on critically ill patients. Common thinking has been that earlier intervention should improve outcomes; however, solid evidence supporting prehospital intubation is lacking. Although studies are most frequently observational, the literature available suggests that EMS intubation does not improve morbidity and mortality and may in some cases worsen patient outcomes.47,54 Similarly, a recent large multicenter study found that prehospital intravenous fluid administration was associated with increased mortality in nearly all subsets of trauma patients, particularly those with penetrating trauma, hypotension, and severe head injury.55 This evidence indicates that a “less is more” or “scoop and run” approach to EMS transport may be safer for patients.
Trauma
Much research on EMS response to trauma focuses on response times and the perceived benefit of “regionalization” of trauma care—that is, linking prehospital systems with participating hospitals, public health agencies, and other care providers within a certain region to achieve optimal system efficiency and outcomes.56 Regional systems generally have specific protocols governing EMS responder actions and transport to specialized trauma centers when appropriate. Even though patients transported directly to designated trauma centers in lieu of the closest facility have more critical injuries, mortality generally remains low, largely because of decreased prehospital time until direct transfer to the specialty hospital.57
Despite the advantages of regionalization, the effect of EMS transport to a trauma center may not always be significant. Some evidence suggests that critically ill patients transported to a trauma center by EMS arrive at the hospital significantly faster than did patients in private vehicles but have no significant improvement in mortality rates, complications, or length of stay.58
Response Time
EMS response time is often used as a benchmark of overall system performance, with accepted standards of 4 minutes for BLS and 8 minutes for ALS arrival.59 Specifically, national guidelines recommend medical intervention within 4 to 6 minutes of EMS activation for patients in cardiac or respiratory arrest, although such intervention may include dispatcher-assisted bystander CPR or AED use.60 Studies of set response time criteria have shown mixed results. Retrospective and post hoc analyses of urban EMS transport show a possible survival benefit for patients transported to hospitals in 4 minutes or less, although the advantage was not significant for those not in cardiac arrest.59,61 E911 systems—in which caller location is available instantly—can decrease response times because they help plan more direct routes to the scene and reduce the likelihood of ambulance crews becoming lost.16 Furthermore, response times should be targeted to specific regional needs and may be maximized by a strong community-wide first-responder presence, strategic placement of ambulances based on historical call data, mobile mapping or global positioning systems, and adequate fleet maintenance.5,61
Disaster Medicine
Introduction and History
Disaster medicine can be defined as “a sudden and extraordinary misfortune that overwhelms the immediate ability to manage or compensate.”2 Increasing attention has been focused on this nascent medical specialty in recent years with such high-profile disasters as the September 11, 2001, terrorist attacks and severe natural disasters such as hurricanes, earthquakes, and tsunamis. With each successive disaster and its medical and public health response, more is learned and planning can be refined for the next event.
Although the existence of apathy toward disaster planning (and resource allocation toward this end) is well documented,62,63 major and minor disasters occur with regular and increasing frequency. In the past hundred years, millions of lives have been lost internationally from natural disasters. In 2005, Hurricane Katrina–related flooding was responsible for more than 1500 fatalities along the U.S. Gulf Coast. Worldwide, flooding of the Yangtze River in China caused 3 million casualties in 1931, deaths from the Indian Ocean tsunami in 2004 approached 300,000, and the devastating 2010 Haiti earthquake killed more than 230,000 and displaced up to an additional 2 million. Over the years, earthquakes, landslides, volcano eruptions, and massive fires have resulted in staggering economic losses, population displacement, disease, and death. Research suggests that losses from natural disasters are probably only going to rise because of growing population density (particularly in high-risk areas) and increased hazards as a result of rapidly expanding technology (i.e., transportation of more dangerous materials, fire threats in high-rise buildings, vulnerable financial and economic infrastructure).62
Despite the clear threats from natural disasters, much of the focus of disaster medicine in recent years has been placed on intentional, man-made events—namely, terrorism and mass casualty incidents. Even before the devastating terrorist attacks on New York City in 2001, researchers predicted that the probability of exactly such an event was extremely high.64 Despite performing a mass casualty drill just 3 days before September 11, none of the existing protocols or triage systems proved adequate for the resulting event.65 Subsequent creation of the Department of Homeland Security (DHS) has provided federal agency support for and focus on expanded research into and development of all aspects of disaster planning for man-made incidents.
Definitions and Classifications
In general, disasters are classified by their relationship to the hospital setting, inciting event (natural or man-made), and the anticipated necessary response. Internal events occur solely within a particular hospital or medical center (e.g., power outage, building collapse), whereas external events involve some part of the larger community. This system is most useful in preparing the facility to either receive patients from outside or deal with internal problems; however, many disasters have both internal and external effects, and such a narrow classification scheme is not easily applicable to a variety of situations. In terms of anticipated response, most disasters are classified into one of three categories. Level I disasters are those in which local emergency response teams and organizations are adequate to manage the event alone. Level II incidents require a regional approach and mutual aid from surrounding areas. Level III events overwhelm local and regional efforts and require state or federal support.63
Disaster Planning
Although The Joint Commission (TJC) requires all health care facilities to conduct two disaster drills per year, disaster planning is rarely emphasized or sufficient. Many factors contribute to the inadequacy of most hospital or regional disaster plans, namely, the unexpected and sudden nature of most events (thus making prospective evaluation impossible), poor record keeping, faulty assumptions on which significant parts of the plan are based, and failure of communication and command structures.66 For disaster plans to be effective, they must be based on valid assumptions of what may occur in a variety of event settings. Furthermore, the planning process must include all systems and organizations that will be affected by the disaster and have a role in its aftermath, and all parties must have a working knowledge of the plan, the chain of command, and their role in it.62
Critical to the development of an appropriate plan is a hazards analysis of particular events to which a hospital or region is most susceptible. In this manner, organizations can plan effectively for the types of disasters that they are most likely to experience. A standard tool for evaluating hospitals’ disaster plans is available through the Agency for Healthcare Research and Quality.67 Frequent rehearsals of disaster plans are of utmost importance. A written plan is useless unless it is thoroughly understood and practiced by all parties involved.62 Rehearsals should be varied and include single-agency drills, tabletop exercises with participating community organizations, functional experiences with state and local emergency operations centers, and a full-scale interagency real-time drill. The latter should be as realistic as possible, with mock patients, evolving scenarios, and full community-wide participation. Equally important to any disaster plan is the “afteraction”—discussion of the drill or real-life event with a focus on identification and rectification of problems and appropriate refinement of the plan.68
A good disaster plan should cover both internal agency and external community needs and focus on all phases of the inciting event: prodrome/mitigation, impact, rescue, and recovery.2,63 Interhospital plans should involve all departments responsible for patient care and infrastructure and detail clear policies related to the chain of command and physical control centers, communication and public relations, record keeping, personnel needs, and equipment and resource supply. External planning should involve all local agencies responsible for protection and care of citizens. The Incident Command Structure (ICS) provides a means to delineate a clear chain of command and management structure during critical events. Developed after a series of devastating California wildfires in the 1970s, this model provides for an overall incident commander of any disaster event who oversees predesignated public relations, logistics, finance, supply, and organizational section chiefs. Each section has a variety of personnel with specific duties and areas of focus who report to the chiefs at regular intervals. The ICS is frequently revised and is designed to be flexible, predictable, and accountable, with improved documentation, common language, and cost efficiency.69
Disaster Response
Response to a catastrophic event requires rapid mobilization and efficient use of available resources. Clear and defined roles should be established for prehospital providers, health care facilities, and all levels of governmental agencies involved in public safety and welfare. The usual standard of medical care may not be possible or desirable in the acute postdisaster period, and alterations in practice will probably be necessary, within accepted boundaries.70
Prehospital Disaster Response and Triage
Though fully capable of responding to individual emergency calls, most local EMS systems are often not able to respond adequately to a widespread or overwhelming event.71 The concept of prehospital triage, used routinely by EMS, is of utmost importance in managing disasters. Unlike routine triage—where the aim is to identify those few critically ill patients who require immediate, aggressive resource utilization—disaster triage attempts to “do the most good for the most people” and often requires that seriously injured victims receive little to no immediate care. Disaster triage models attempt to rapidly identify individuals who will benefit most from immediate stabilization with the least amount of available resources.
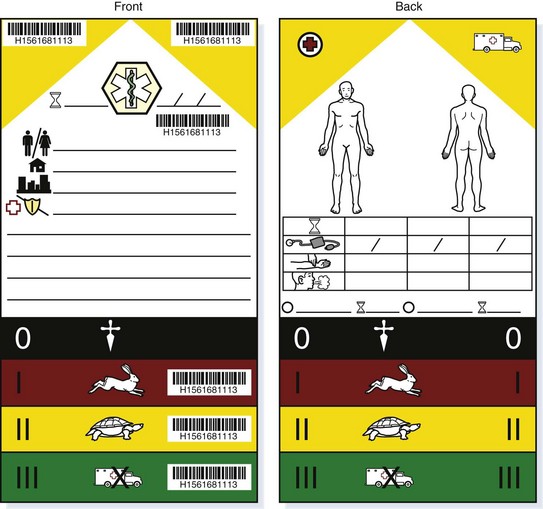
The simplest method of triage assigns each patient a color-coded tag with frequent opportunities for reassessment (Fig. 215.2). Green tags are given to patients who require minor, nonimmediate medical intervention. Yellow tags indicate potentially serious injuries, but ones that are relatively stable and can wait a short period. Red tags designate patients who have life-threatening, but potentially treatable injuries that require immediate medical care. Black tags signify dead or critically ill patients who will not survive without significant use of resources and time unavailable under disaster conditions. For example, an apneic victim of a large-scale blast injury with significant head and abdominal injuries may be tagged “black” because the immediate resuscitative and stabilization needs of the victim would require an inordinate use of personnel and equipment given the number of victims and likelihood of a meaningful outcome.
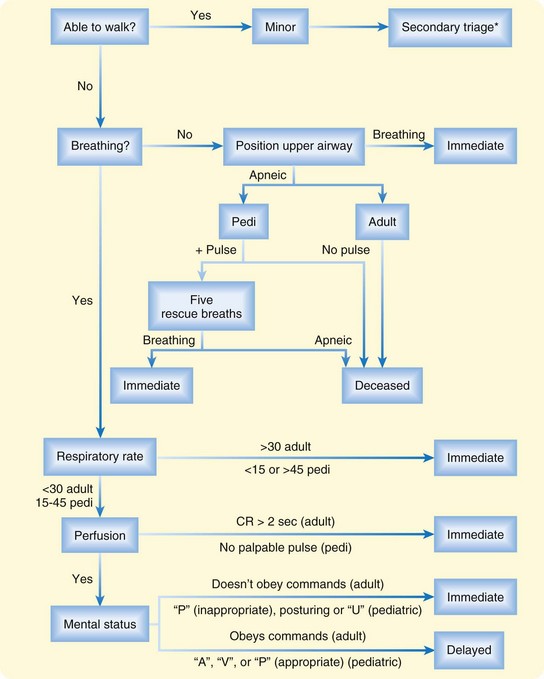
Tag systems are combined with triage models to provide specific algorithms for classification of patients. Widely used in the United States, the START (Simple Triage and Rapid Assessment) system triages mass casualty patients by several simple variables: breathing, ambulation, radial pulse, and ability to follow commands (Fig. 215.3). Patients are categorized as “green” if they are initially ambulatory with minor injuries. “Yellow” victims are those who may be unable to walk but are breathing with respiratory rates lower than 30 breaths/min, are well perfused (capillary refill longer than 2 seconds), and can follow simple commands. Patients with respiratory rates higher than 30 (with or without airway positioning), delayed capillary refill, or inability to follow simple commands are tagged as “red,” and the need for immediate lifesaving attention is assessed. Apneic patients are tagged as “black,” and no further interventions are performed. Refinement of this model has led to specific, but still simple modifications for pediatric patients.72
The SAVE (Secondary Assessment of Victim Endpoint) model was developed as an adjunct to the START system. After primary assessment with START, secondary triage is performed with SAVE to assess the following: prognosis if only minimal treatment is performed and prognosis with just the available resources on site or at the disaster medical aid center. Patients are sent to a treatment area only if treatment will reduce morbidity or mortality within the delayed time to definitive care without consuming a disproportionate amount of resources.73 The SAVE protocol provides specific guidelines based on age, injury location (head, extremity, spine, chest, and abdomen), and type of injury (burns, crush injuries, blunt or penetrating trauma) and suggests treatment priorities in order of likelihood of success (Box 215.1).
Box 215.1
Secondary Assessment of Victim Endpoint Protocol Treatment Priorities (in Descending Order)
Pressure dressings to stop bleeding
Treatment of shock after control of bleeding
From Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE—a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med 1996;11:117–24.
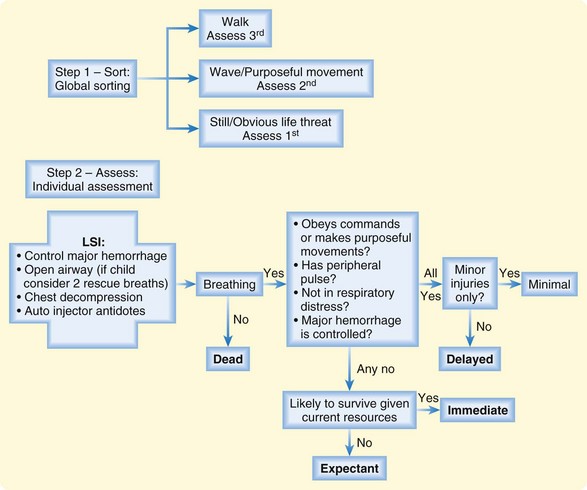
The START system has been shown to have high sensitivity, be quick to administer, and easily be taught to first responders.74,75 However, real-time use of the START system during the terrorist attacks in New York City in 2001 proved ineffective. Because of the dynamic nature of the event, the loss of communications, and the fact that rescue personnel were in personal danger, the START system was abandoned.65 International triage systems (Careflight, Triage Save, and Sort) are comparable with START in prediction of critical injury,76 but currently no national triage guideline exists. The SALT (sort, assess, lifesaving intervention, treatment/transport) model was developed by a multidisciplinary panel of disaster experts to provide such a national standard.74 This model includes anatomic and physiologic considerations, as well as assessment of available resources (Fig. 215.4).
Hospital and Agency Disaster Response
With proper triage and communication, the prehospital disaster response can successfully reduce the burden of any mass incident on receiving health care facilities.66,77 TJC requirements necessitate that hospitals prepare for both internal and external events; these plans should easily be integrated in the event of a combined internal and external disaster. Internal and external events may involve different roles for emergency department (ED) staff. In an internal disaster, the ED’s main focus is generally to treat individuals within the institution who may be injured, with actual management and control of the situation being left to other in-hospital departments according to the institution’s incident command protocol. The possibility of ED evacuation should be part of any hospital plan and be well thought out and rehearsed for maximum speed and safety. In an internal disaster, resources and outside aid should be sufficient for patient care and evacuation such that critically ill patients can be treated or evacuated (or both) with highest priority.
External disasters usually result in sudden and often overwhelming volumes of patients at one or more local health care facilities. Ideally, controlled prehospital triage should result in even and appropriate distribution of patients to local hospitals; however, research on a variety of disasters has shown that frequently, the majority of patients do not arrive at hospitals via ambulance.66 This fact can cause significant disruption of carefully planned dispersion of resources and lead to rapid saturation of the closest or most familiar facilities, as well as difficulty in patient tracking and timely hospital notification. Hospitals should be prepared for significant communication breakdown, restricted access, limited outside help, mass influx of victims with a variety of injuries, and personnel limitations. For example, hospitals in the flood zone of Hurricane Katrina suffered prolonged austere conditions because of protracted physical inaccessibility, primitive communications, and lack of timely outside aid. Other prolonged mass casualty events, such as the 2009 H1N1 influenza pandemic, affect both hospital functioning and the community at large and create chronic resource shortages both internally and externally.
Although FEMA search-and-rescue teams are ideally deployed within 6 hours after declaration of a disaster and can provide basic scene and patient stabilization, federal resources are often delayed for several days. Evidence suggests that local response to disasters has the most lifesaving potential because outside aid generally arrives too late for meaningful immediate medical care.78
Weapons of Mass Destruction and Hazardous Materials
Traditional disaster medicine developed mainly in response to natural events such as floods, earthquakes, tornadoes, and other disasters. However, increasing sophistication and spread of man-made disasters in recent years have brought these types of catastrophic incidents to the forefront of focus and research. Potential agents available to terrorists include chemical, biologic, nuclear, radiologic, and explosive devices (generally referred to as weapons of mass destruction [WMD]); although the overall likelihood of an attack is low, the consequences may be cataclysmic. One gram of botulin toxin has the potential to kill 1 million people,79 and the effects of nuclear and radioactive agents can reach across continents. The response to WMD events may differ significantly from the traditional disaster models described earlier, with shifting priority on decontamination, agent-specific triage, and special resources and personnel.
Preparing for biologic and chemical attacks is difficult and must be adaptive. Disease surveillance programs that link a community are essential for detection and prompt response because biologic agents may not be detected for days to weeks.80,81 Predisaster emphasis should be on hazard analysis, as well as training and stockpiling of antidotes for the most likely agents to be used. The Strategic National Stockpile is a national reserve of medical supplies, antidotes, and medications managed by the Centers for Disease Control and Prevention and strategically placed in states for rapid availability following a mass casualty event.
Traditionally, preparation for WMD has used the more common hazardous materials (HAZMAT) exposure training methods. These models may not, however, be appropriate.64,82 HAZMAT events assume an exposure away from health care facilities, where response teams with maximum personal protection and extensive decontamination equipment work to rescue and decontaminate small numbers of victims. Large-scale exposure to WMD may encompass public areas and health care facilities, thereby compromising response efforts and calling into question the traditional decontamination methods.83 For example, in the 1995 Japanese subway nerve gas attacks, several thousand people were potentially exposed, yet fewer than 100 were killed or seriously injured. However, thousands arrived at hospitals by private vehicle without on-scene decontamination, which quickly overwhelmed the facilities and potentially exposed scores of essential medical personnel.80
The Role of Emergency Physicians in Disaster Medicine
Published ACEP policy advocates a leadership role for emergency physicians in all aspects of disaster research, planning, and implementation.84 The traditional focus of disaster medicine—to do the most good for the greatest number of people—may seem to be at odds with the traditional emergency medical principles of aggressive resource utilization for selected critically ill patients. However, the emergency physician is generally the best-trained individual to coordinate medical control, supervise triage, connect with other municipal and public health agencies, and oversee direct patient care during a catastrophic event. Several formal disaster medicine fellowships exist for emergency medical physicians, and disaster training is included in the emergency medical residency curriculum. Advances in research and increased global attention to natural and man-made disasters create exciting potential for emergency physicians to lead the development of disaster medicine as a discipline.
1 Narad RA. Coordination of the EMS system: an organizational theory approach. Prehosp Emerg Care. 1998;2:145–152.
2 Dara SI, Ashton RW, Farmer JC, et al. Worldwide disaster medical response: an historical perspective. Crit Care Med. 2005;33(1 Suppl):S2–S6.
3 McSwain NE, Jr. Prehospital care from Napoleon to Mars: the surgeon’s role. J Am Coll Surg. 2005;200:487–504.
4 Mullins RJ. A historical perspective of trauma system development in the United States. J Trauma. 1999;47(3 Suppl):S8–S14.
5 Boyd DR. The conceptual development of EMS systems in the United States, part I. Emerg Med Serv. 1982;11:19–23.
6 Hoff WS, Schwab CW. Trauma system development in North America. Clin Orthop Relat Res. 2004;422:17–22.
7 Pozner CN, Zane R, Nelson SJ, et al. International EMS systems: the United States: past, present, and future. Resuscitation. 2004;60:239–244.
8 Boyd DR. The conceptual development of EMS systems in the United States, part II. Emerg Med Serv. 1982;11:26. 28–30, 32–33
9 National Highway Traffic Safety Administration. The National EMS Scope of Practice Model. Washington, DC: U.S. Department of Transportation/National Highway Traffic Safety Administration; 2005. DOT HS 809 898
10 Heady HR. A delicate balance: the economics of rural health care delivery. JAMA. 2002;287:110.
11 Freeman V, Slifkin R, Patterson D. Challenges for rural emergency medical services: medical oversight. Findings brief, May 2008. Available at www.shepscenter.unc.edu/research_programs/rural_program/ Accessed January 28, 2011
12 Grossman DC, Kim A, Macdonald SC, et al. Urban-rural differences in prehospital care of major trauma. J Trauma. 1997;42:723–729.
13 Nathens AB, Brunet FP, Maier RV. Development of trauma systems and effect on outcomes after injury. Lancet. 2004;363:1794–1801.
14 Esposito TJ, Maier RV, Rivara FP, et al. The impact of variation in trauma care times: urban versus rural. Prehosp Disaster Med. 1995;10:161–166.
15 National Cooperative Highway Research Program. Rural emergency medical services. Available at http://safety.transportation.org/htmlguides/rural Accessed January 30, 2011
16 Careless J. The importance of rural E9-1-1. Emerg Med Serv. 2005;34(4):56.
17 National Association of EMS Physicians. Position paper. Emergency medical dispatch. Prehosp Emerg Care. 2008;12:217.
18 Dale J, Higgins J, Williams S, et al. Computer assisted assessment and advice for “non-serious” 999 ambulance service callers: the potential impact on ambulance dispatch. Emerg Med J. 2003;20:178–183.
19 American College of Emergency Physicians, National Association of EMS Physicians, National Association of State EMS Officials. Position statement. Role of the State EMS Medical Director. Available at www.acep.org/content.aspx?id=29676 Accessed January 28, 2011
20 American College of Emergency Physicians. Policy statement. Medical direction of EMS. Available at www.acep.org/content.aspx?id=29570 Accessed January 28, 2011
21 Erder MH, Davidson SJ, Cheney RA. On-line medical command in theory and practice. Ann Emerg Med. 1989;18:261–268.
22 Wuerz RC, Swope GE, Holliman CJ, et al. On-line medical direction: a prospective study. Prehosp Disaster Med. 1995;10:174–177.
23 Holliman CH, Wuerz RC, Vazques-de Miguel G, et al. Comparison of interventions of prehospital care by standing orders versus interventions ordered by direct (on-line) medical command. Prehosp Disaster Med. 1994;9:202–209.
24 Verma A, Gladstone VA, Fang J, et al. Effect of online medical control on prehospital code stroke triage. CJEM. 2010;12:103–110.
25 Blackwell TH. Prehospital care. Emerg Med Clin North Am. 1993;11:1–14.
26 Rottman SJ, Schriger DL, Charlop G, et al. On-line medical control versus protocol-based prehospital care. Ann Emerg Med. 1997;30:62–68.
27 Wuerz RC, Meador SA. Evaluation of a prehospital chest pain protocol. Ann Emerg Med. 1995;26:595–597.
28 Delbridge TR, Bailey B, Chew Jr, JL., et al. EMS Agenda for the Future: where we are … where we want to be. EMS Agenda for the Future Steering Committee. Ann Emerg Med. 1998;31:251–263.
29 United States Department of Transportation, National Highway Traffic Safety Administration. EMS Education Agenda for the Future: a systems approach. Prehosp Emerg Care. 2000;4:365–366.
30 Eisenberg M, Bergner L, Hallstrom A. Paramedic programs and out-of-hospital cardiac arrest: I. Factors associated with successful resuscitation. Am J Public Health. 1979;69:30–38.
31 Eisenberg M, Bergner L, Hallstrom A. Paramedic programs and out-of-hospital cardiac arrest: II. Impact on community mortality. Am J Public Health. 1979;69:39–42.
32 Messick WJ, Rutledge R, Meyer AA. The association of advanced life support training and decreased per capita trauma death rates: an analysis of 12,417 trauma deaths. J Trauma. 1992;33:850–855.
33 Jacobs LM, Sinclair A, Beiser A, et al. Prehospital advanced life support: benefits in trauma. J Trauma. 1984;24:8–13.
34 Weston CF, McCabe MJ. Audit of an emergency ambulance service: impact of a paramedic system. J R Coll Physicians Lond. 1992;26:86–89.
35 Kelly AM, Currell A. Do ambulance crews with one advanced paramedic skills officer have longer scene times than crews with two? Emerg Med J. 2002;19:152–154.
36 American College of Emergency Physicians and American College of Surgeons. Equipment for ambulances. Available at www.acep.org/content.aspx?id=29436 Accessed January 28, 2011
37 Moylan JA. Impact of helicopters on trauma care and clinical results. Ann Surg. 1988;208:673–678.
38 Schneider C, Gomez M, Lee R. Evaluation of ground ambulance, rotor-wing, and fixed-wing aircraft services. Crit Care Clin. 1992;8:533–564.
39 Thomas SH, Harrison TH, Buras WR, et al. Helicopter transport and blunt trauma mortality: a multicenter trial. J Trauma. 2002;52:13–45.
40 Wills VL, Eno L, Walker C, et al. Use of an ambulance-based helicopter retrieval service. Aust N Z J Surg. 2000;70:506–510.
41 Skogvoll E, Bjelland E, Thorarinson B. Helicopter emergency medical service in out-of-hospital cardiac arrest—a 10-year population-based study. Acta Anaesthesiol Scand. 2000;44:972–979.
42 DeWing MD, Curry T, Stephenson E, et al. Cost-effective use of helicopters for the transportation of patients with burn injuries. J Burn Care Rehabil. 2000;21:535–540.
43 Di Bartolomeo S, Sanson G, Nardi G, et al. Effects of 2 patterns of prehospital care on the outcome of patients with severe head injury. Arch Surg. 2001;136:1293–1300.
44 Slater H, O’Mara MS, Goldfarb IW. Helicopter transportation of burn patients. Burns. 2002;28:70–72.
45 Isakov A. Urgent air-medical transport: right patient, place and time. CMAJ. 2009;181:569–570.
46 Thomson DP, Thomas SH, 2002-2003 Air Medical Services Committee of the National Association of EMS Physicians. Guidelines for air medical dispatch. Prehosp Emerg Care. 2003;7:265–271.
47 Eisenberg MS, Horwood BT, Cummins RO, et al. Cardiac arrest and resuscitation: a tale of 29 cities. Ann Emerg Med. 1990;19:179–186.
48 Bunch TJ, Hammill SC, White RD. Outcomes after ventricular fibrillation out-of-hospital cardiac arrest: expanding the chain of survival. Mayo Clin Proc. 2005;80:774–782.
49 White RD, Bunch TJ, Hankins DG. Evolution of a community-wide early defibrillation programme experience over 13 years using police/fire personnel and paramedics as responders. Resuscitation. 2005;65:279–283.
50 Rea TD, Eisenberg MS, Becker LJ, et al. Temporal trends in sudden cardiac arrest: a 25-year emergency medical services perspective. Circulation. 2003;107:2780–2785.
51 Field JM, Hazinski MF, Savre MR, et al. Part 1: executive summary: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S640–S656.
52 Hazinski MF, Idris AH, Kerber RE, et al. Lay rescuer automated external defibrillator (“public access defibrillation”) programs: lessons learned from an international multicenter trial: advisory statement from the American Heart Association Emergency Cardiovascular Committee; the Council on Cardiopulmonary, Perioperative, and Critical Care; and the Council on Clinical Cardiology. Circulation. 2005;111:3336–3340.
53 von Elm E, Schoettker P, Henzi I, et al. Pre-hospital tracheal intubation in patients with traumatic brain injury: systematic review of current evidence. Br J Anaesth. 2009;103:371–386.
54 Strote J, Roth R, Cone DC, et al. Prehospital endotracheal intubation: the controversy continues. Am J Emerg Med. 2009;27:1143–1147.
55 Haut ER, Kalish BT, Cotton BA, et al. Prehospital intravenous fluid administration is associated with higher mortality in trauma patients: a National Trauma Data Bank analysis. Ann Surg. 2011;253:371–377.
56 Liberman M, Mulder DS, Jurkovich GJ, et al. The association between trauma system and trauma center components and outcome in a mature regionalized trauma system. Surgery. 2005;137:647–658.
57 Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46:565–579.
58 Cornwell 3rd, EE., Belzberg H, Hennigan K, et al. Emergency medical services (EMS) vs non-EMS transport of critically injured patients: a prospective evaluation. Arch Surg. 2000;135:315–319.
59 Pons PT, Haukoos JS, Bludworth W, et al. Paramedic response time: does it affect patient survival? Acad Emerg Med. 2005;12:594–600.
60 National Association of EMS Physicians. Position paper. Considerations in establishing emergency medical services response time goals. Prehosp Emerg Care. 2003;7:397–399.
61 Blackwell TH, Kaufman JS. Response time effectiveness: comparison of response time and survival in an urban emergency medical services system. Acad Emerg Med. 2002;9:288–295.
62 Auf der Heide E. Disaster response: principles of preparation and coordination. St. Louis: Mosby; 1989.
63 Goolsby CA, Mothershead JL. Disaster planning. Available at www.emedicine.com Updated January 15, 2010. Accessed January 31, 2011
64 Waeckerle JF. Domestic preparedness for events involving weapons of mass destruction. JAMA. 2000;283:252–254.
65 Asaeda G. The day that the START triage system came to a STOP: observations from the World Trade Center disaster. Acad Emerg Med. 2002;9:255–256.
66 Auf der Heide E. The importance of evidence-based disaster planning. Ann Emerg Med. 2006;47:34–49.
67 Cosgrove SE, Jenckes MW, Wilson LM, et al. Tool for evaluating core elements of hospital disaster drills. Prepared by Johns Hopkins Evidence-based Practice Center under Contract No. 290-02-0018. December 2007.
68 Vaughan W. Mass-casualty exercise design for EMS agencies. Emerg Med Serv. 2004;33(8):59–63.
69 . Hospital Emergency Incident Command System. 3rd ed. 1998. Available at http://www.heics.com/HEICS98a.pdf Accessed January 30, 2011
70 Prepared by Health Systems Research Inc. under Contract No. 290-04-0010. AHRQ Publication No. 05-0043. Altered standards of care in mass casualty events. Rockville, Md: Agency for Healthcare Research and Quality; April 2005.
71 Branas CC, Sing RF, Perron AD. A case series analysis of mass casualty incidents. Prehosp Emerg Care. 2000;4:299–304.
72 Romig L. The JumpSTART Algorithm. Available at http://www.jumpstarttriage.com/TheJumpSTARTAlgorithm.html Accessed January 31, 2011
73 Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE—a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med. 1996;11:117–124.
74 Lerner EB, Schwartz RB, Coule PL, et al. Mass casualty triage: an evaluation of the data and development of a proposed national guideline. Disast Med Public Health Prep. 2008;2(Suppl 1):S25–S34.
75 Risavi BL, Salen PN, Heller MB, et al. A two-hour intervention using START improves prehospital triage of mass casualty incidents. Prehosp Emerg Care. 2001;5:197–199.
76 Garner A, Lee A, Harrison K, et al. Comparative analysis of multiple-casualty incident triage algorithms. Ann Emerg Med. 2001;38:541–548.
77 McDonald CC, Koenigsberg MD, Ward S. Medical control of mass gatherings: can paramedics perform without physicians on-site? Prehosp Disaster Med. 1993;8:327–331.
78 Schultz CH, Koenig KL, Noji EK. A medical disaster response to reduce immediate mortality after an earthquake. N Engl J Med. 1996;334:438–444.
79 Arnon SS, Schechter R, Inglesby TV, et al. Botulinum toxin as a biological weapon: medical and public health management. JAMA. 2001;285:1059–1070.
80 World Health Organization. Public health response to biological and chemical weapons: WHO guidance, 2nd ed. Geneva: WHO; 2004.
81 Flowers LK, Mothershead JL, Blackwell TH. Bioterrorism preparedness. II: the community and emergency medical services systems. Emerg Med Clin North Am. 2002;20:457–476.
82 Macintyre AG, Christopher GW, Eitzen E, Jr., et al. Weapons of mass destruction events with contaminated casualties: effective planning for health care facilities. JAMA. 2000;283:242–249.
83 Okumura T, Takasu N, Ishimatsu S, et al. Report on 640 victims of the Tokyo subway sarin attack. Ann Emerg Med. 1996;28:129–135.
84 American College of Emergency Physicians. Disaster medical services policy statement. Available at http://www.acep.org/content.aspx?id=29176&terms=disaster%20medical%20services Accessed January 31, 2011