Chapter 4 Elbow Ultrasound
![]() Additional videos for this topic are available online at www.expertconsult.com.
Additional videos for this topic are available online at www.expertconsult.com.
Elbow Anatomy
The elbow is a synovial joint composed of three elbow joint articulations: the trochlea and ulna, the capitellum and the radial head, and the proximal ulna and radius (Fig. 4-1). The elbow joint has prominent joint recesses located in the coronoid and radial fossae anteriorly and within the olecranon fossa posteriorly. Within each joint recess exists an intracapsular but extrasynovial fat pad, which becomes displaced with joint distention. The medial elbow joint is stabilized by the ulnar collateral ligament, of which the anterior band that extends anteriorly to the sublime tubercle of the ulna is the most important. Other components of the ulnar collateral ligament include posterior and oblique bands. Laterally, the elbow joint is stabilized by the radial collateral ligament complex, which is composed of the radial collateral ligament, the annular ligament, and a smaller accessory radial collateral ligament. An additional component, the lateral ulnar collateral ligament, extends from the lateral epicondyle to insert on the crista supinator of the proximal ulna.
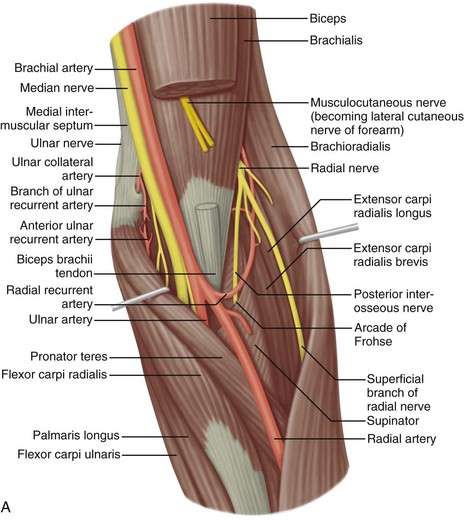
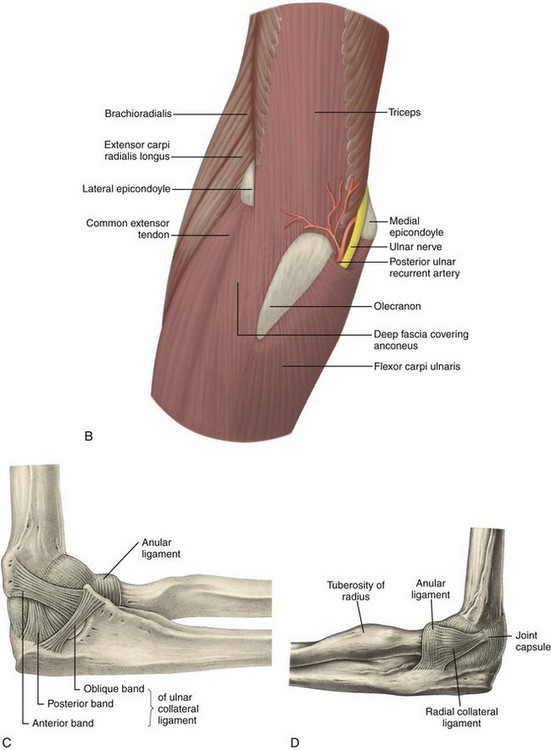
FIGURE 4-1 Elbow anatomy.
(From Standring S: Gray’s anatomy: the anatomical basis of clinical practice, ed 39, Edinburgh, 2005, Churchill Livingstone.)
Anterior to the elbow joint, the brachialis inserts on the ulna, and the biceps brachii tendon inserts on the radial tuberosity. With regard to the biceps brachii, a dual insertion exists where the short head is superficial and inserts more distal relative to the long head on the radial tuberosity.1 Posteriorly, the triceps brachii inserts on the olecranon process of the proximal ulna, over which is located the olecranon bursa. The lateral and long heads of the triceps brachii represent the most superficial layer of the distal triceps, whereas the deep aspect with a relatively shorter tendon is the medial head.2 The anconeus is located between the olecranon process and the lateral epicondyle of the humerus. Medially, the common flexor tendon, consisting of the flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis, originates on the medial epicondyle of the distal humerus. Laterally, the common extensor tendon, composed of the extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris, originates at the lateral epicondyle of the distal humerus. The extensor carpi radialis brevis is the most anteriorly located of the group; the extensor carpi radialis longus originates proximal to the lateral epicondyle on the lateral humeral metaphysis.
The space between the olecranon process of the ulna and the medial epicondyle is bridged by the cubital tunnel retinaculum (or Osborne fascia) and contains the ulnar nerve. Just distal to this, the ulnar nerve enters the true cubital tunnel, between the dual origins of the flexor carpi ulnaris and deep to the arcuate ligament.3 The median nerve is located medial to the brachial artery and courses distally between the ulnar and humeral heads of the pronator teres. The radial nerve is located at the posterior aspect of the humeral shaft and then courses distally and laterally beneath the brachioradialis, where a deep branch courses between the two heads of the supinator muscle and a superficial branch courses beneath the brachioradialis and into the forearm.
Ultrasound Examination Technique
Table 4-1 is an elbow ultrasound examination checklist. Examples of diagnostic elbow ultrasound reports are available online at www.expertconsult.com (see eBox 4-1 and 4-2).
| Location | Structures of Interest |
|---|---|
| Anterior |
eBox 4-1 Sample Diagnostic Elbow Ultrasound Report
Normal, Complete
Examination: Ultrasound of the Elbow
History: Elbow pain, evaluate for tendon abnormality
Findings: No evidence of joint effusion or synovial process. The biceps brachii and brachialis are normal. The common flexor and extensor tendons are also normal. No significant triceps brachii abnormality. The anterior band of the ulnar collateral ligament and radial collateral ligament complex are normal. The ulnar nerve, radial nerve, and median nerve at the elbow are unremarkable. No abnormality in the cubital tunnel region with dynamic imaging. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression: Unremarkable ultrasound examination of the elbow.
eBox 4-2 Sample Diagnostic Elbow Ultrasound Report
Abnormal, Complete
Examination: Ultrasound of the Elbow
History: Elbow pain, evaluate for tendon abnormality
Findings: There is a partial-thickness tear of the distal biceps brachii tendon involving the superficial short head tendon with approximately 2 cm of retraction but with intact long head. Dynamic evaluation shows continuity of the long head excluding full-thickness tear. No joint effusion. The triceps brachii, common extensor, and common flexor tendons are normal. The ulnar, radial, and median nerves are unremarkable, including dynamic evaluation of the ulnar nerve. Unremarkable ulnar and radial collateral ligaments. No bursal distention.
Impression: Partial-thickness tear of the distal biceps brachii tendon.
Anterior Evaluation
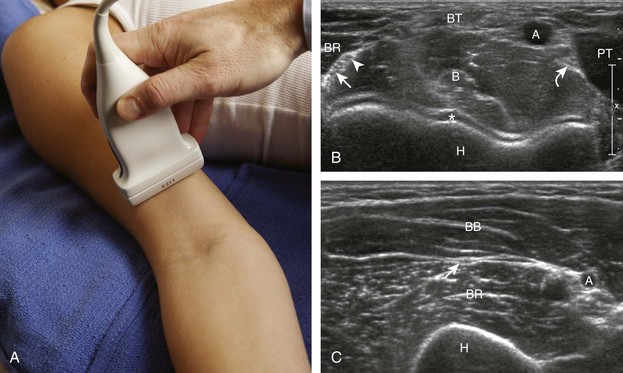
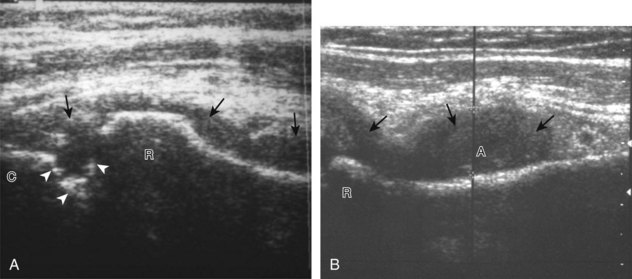
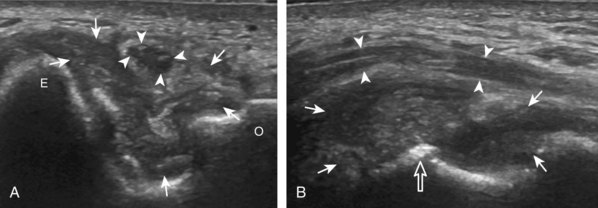
The primary structures evaluated from the anterior approach are the brachialis, the distal biceps brachii, the median nerve, and the anterior elbow joint recess. For sonographic evaluation, the elbow is comfortably extended, and the hand is supinated. Evaluation begins with the transducer short axis to the biceps brachii and brachialis just superior to the elbow joint. For orientation, it is helpful to begin at the medial aspect of the anterior elbow and locate the brachial artery, identified by its pulsation and flow on color Doppler imaging (Fig. 4-2). Deep to the brachial artery and in midline is the brachialis muscle, immediately adjacent to the distal humerus. The hypoechoic layer over the hyperechoic cortex is the hyaline articular cartilage. Normal muscle is predominantly hypoechoic with intervening hyperechoic fibroadipose septations. Just lateral to the brachial artery and superficial to the brachialis is the biceps brachii tendon. Immediately medial to the brachial artery is the median nerve, which has a speckled appearance from hypoechoic nerve fascicles and surrounding hyperechoic connective tissue. Medial to the median nerve is the humeral head of the pronator teres muscle. At the far lateral aspect of the anterior elbow is the brachioradialis muscle. In between the brachialis and brachioradialis is an oblique fascial layer, which contains the superficial and deep branches of the radial nerve. More proximal to the elbow joint, the musculocutaneous nerve can be identified between the biceps brachii and brachialis muscles (see Fig. 4-2C).
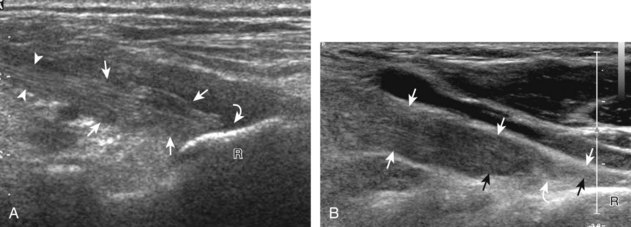
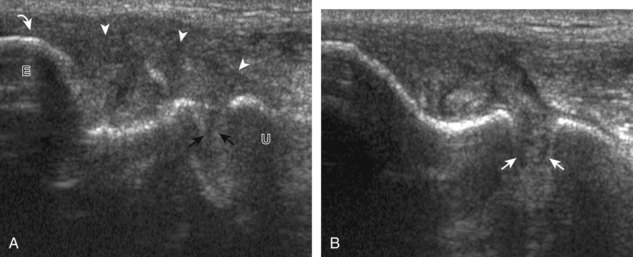
To evaluate the biceps brachii tendon, the transducer is centered over the biceps tendon and rotated 90 degrees (Fig. 4-3). At this location, the biceps tendon will be hyperechoic and fibrillar with a uniform thickness over the brachialis muscle (see Fig. 4-3B). As the biceps brachii tendon courses deep along the outer contour of the brachialis, the tendon will become hypoechoic from anisotropy (see Fig. 4-3C). Using the heel-toe maneuver, the sound beam is angled superiorly in order to image the tendon perpendicular to eliminate anisotropy (see Fig. 4-3D). Some ultrasound machines will have beam steering, which can assist in reducing anisotropy (see Figs. 4-3E and F). If the distal biceps is difficult to visualize, the elbow position may be changed with additional minimal flexion or extension. The biceps brachii is also evaluated in short axis (Fig. 4-4). The lacertus fibrosis or bicipital aponeurosis can be seen extending from the biceps brachii tendon to the pronator teres and flexor musculature, superficial to the brachial artery and median nerve, by placing the transducer over the anterior elbow angled from the biceps brachii tendon distal and medial (see Fig. 4-4C).
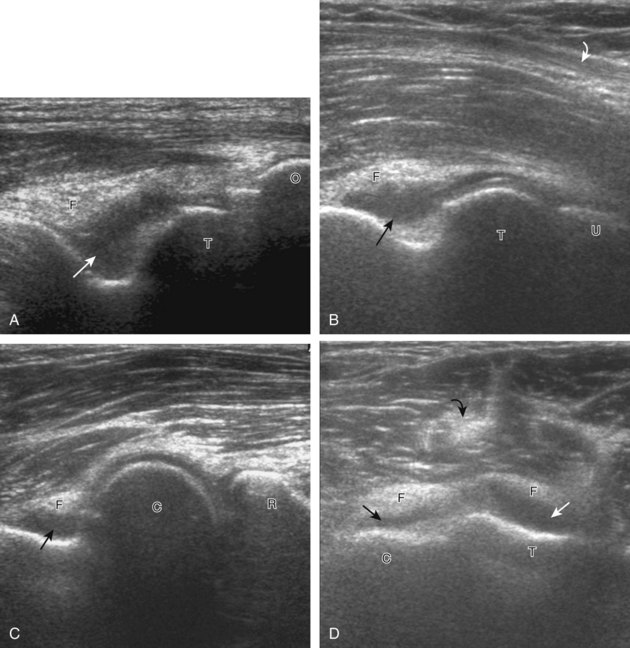
If the distal biceps brachii tendon insertion onto the radial tuberosity in long axis is not clearly seen, a more medial approach should be attempted (Fig. 4-5). With the transducer long axis to the biceps brachii tendon in the sagittal plane on the body, the transducer is moved slightly medial with the beam angled slightly lateral toward the center of the elbow. If the brachial vasculature is visualized, then the transducer needs to be angled laterally. This maneuver is continued, only a millimeter at a time, while adding the heel-toe manuever until the distal tendon is visualized. With the transducer over the medial elbow angled toward the lateral elbow, often the distal biceps brachii tendon can be seen through the medial brachial vasculature as an acoustic window.4 Distal tendon attachment can also be assessed during supination and pronation dynamically (Video 4-1)![]() .
.
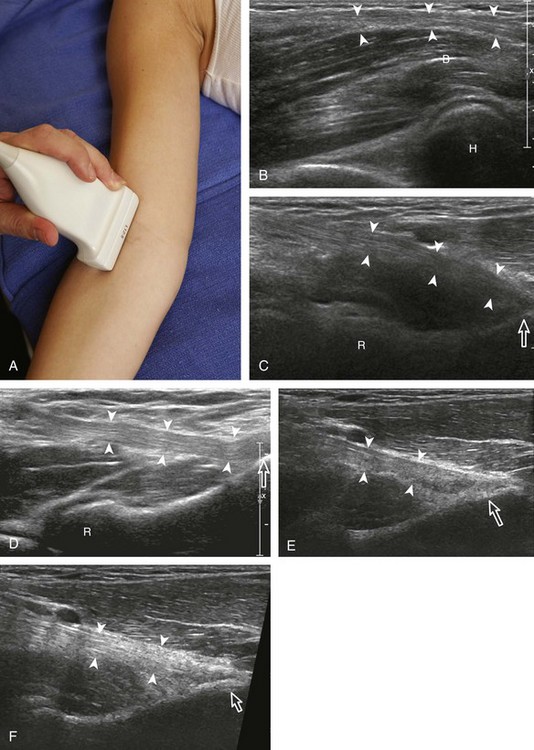
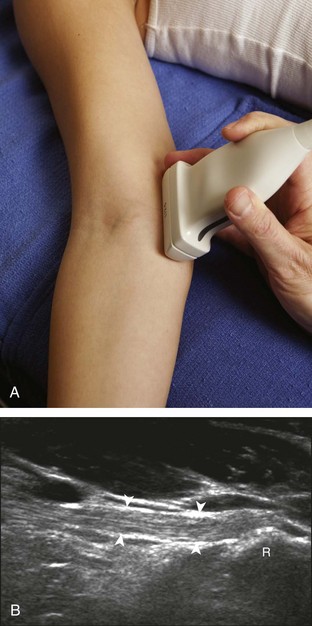
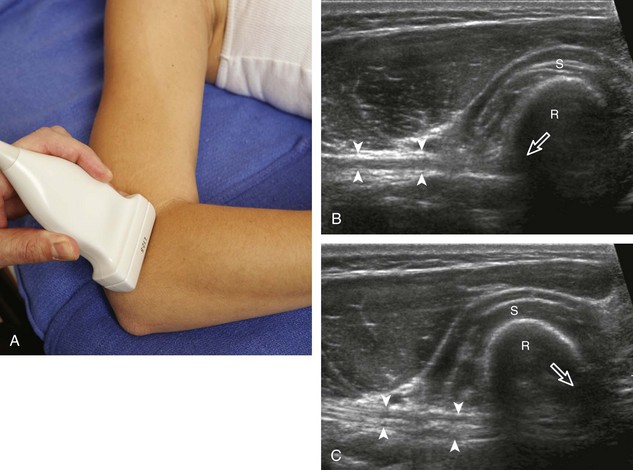
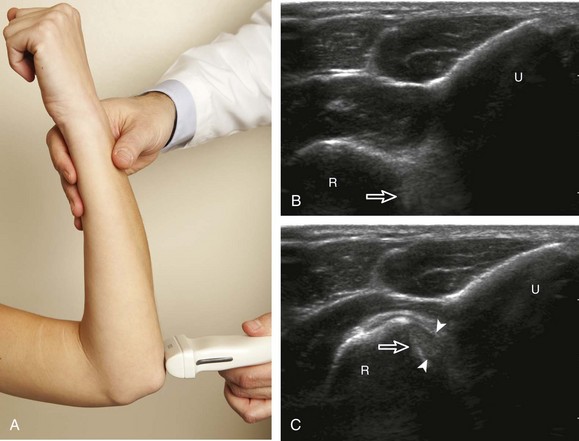
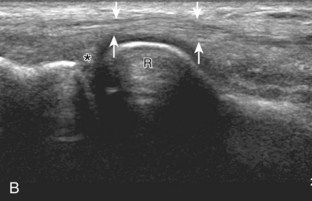
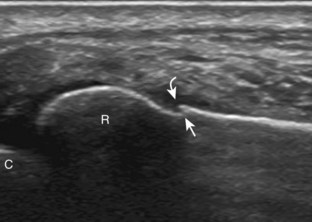
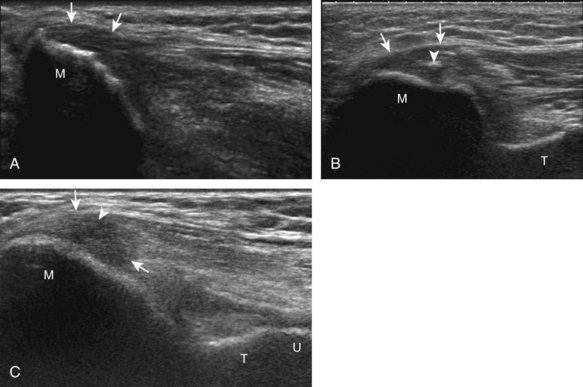
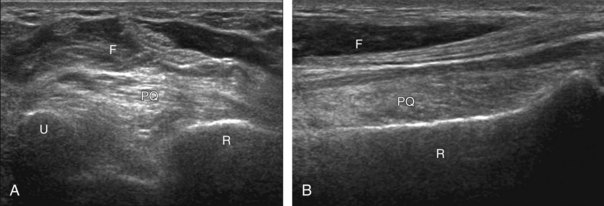
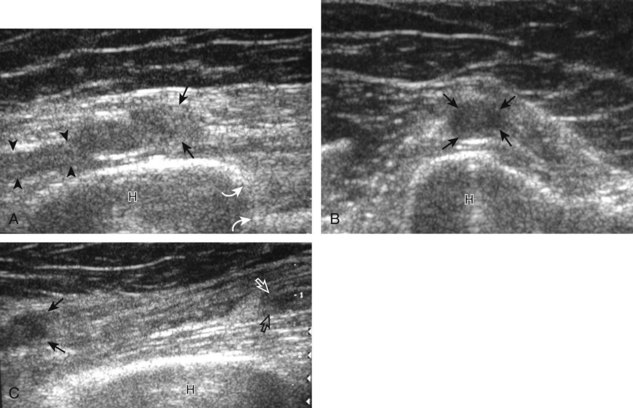
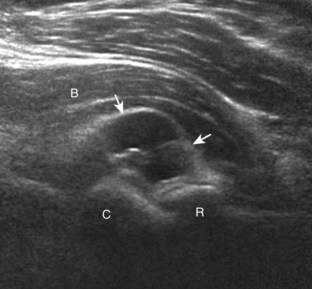
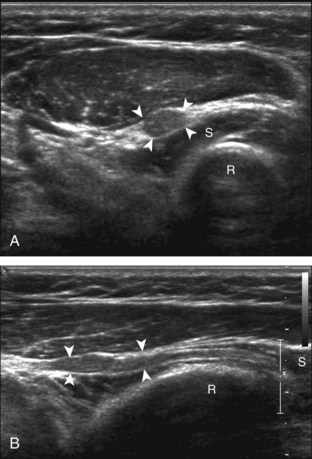
An additional method to evaluate the distal biceps brachii tendon to differentiate a nonretracted full-thickness tear from a partial-thickness tear is from a lateral approach with the elbow flexed.5 Examination with this technique begins with the transducer in short axis relative to the proximal radius (Fig. 4-6). The radial head is visualized as a curvilinear echogenic structure, and the transducer is moved toward the wrist over the radial neck, where the surrounding supinator muscle can be seen. At this level, the hand can be passively supinated and pronated to visualize movement of the biceps brachii tendon, which is perpendicular to the sound beam (Video 4-2)![]() . There is also one additional method to evaluate the most distal aspect of the biceps brachii tendon (Fig. 4-7), in which the transducer is placed transverse to the radius dorsally between the radius and ulna with the hand in pronation to visualize the radial tuberosity insertion.
. There is also one additional method to evaluate the most distal aspect of the biceps brachii tendon (Fig. 4-7), in which the transducer is placed transverse to the radius dorsally between the radius and ulna with the hand in pronation to visualize the radial tuberosity insertion.
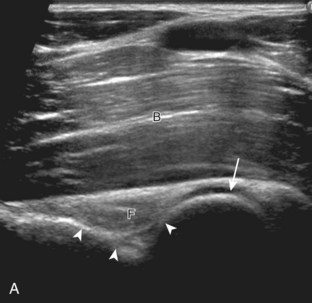
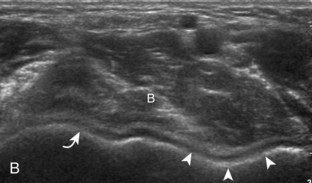
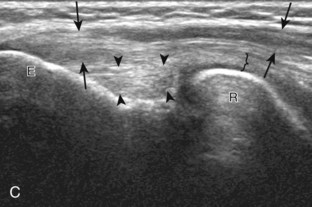
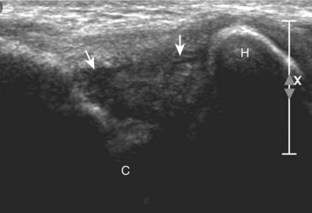
To complete the anterior evaluation of the elbow, the transducer is returned to the sagittal plane directly long axis to the brachialis to visualize the anterior recess of the elbow joint (Fig. 4-8A and B). Here, the coronoid fossa and smaller radial fossa are visible as concavities in the distal humerus. Within these fossae, a triangular hyperechoic intracapsular fat pad is normally seen. The hypoechoic hyaline cartilage of the trochlea and capitellum can also be identified. Returning to the original short axis view of the brachial artery, the normal median nerve is again identified in short axis and can be followed distally as it courses between the humeral and ulnar heads of the pronator teres, a potential site of nerve entrapment (see Fig. 4-8C and D). The ulnar head of the pronator teres is located between the median nerve and the ulnar artery.
Medial Evaluation
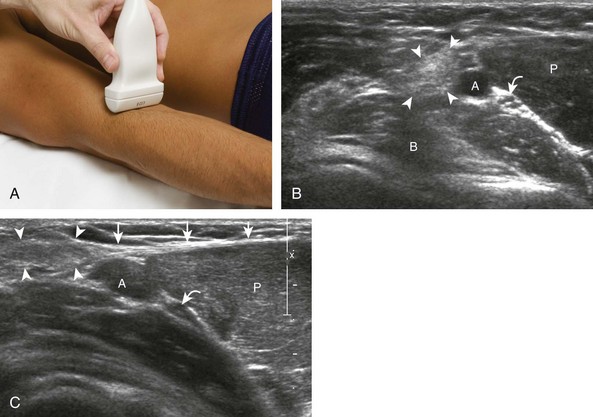
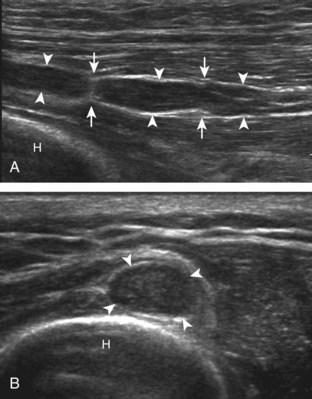
For medial evaluation, the elbow is slightly flexed to bring the anterior band of the ulnar collateral ligament into the coronal plane. Sonographic evaluation of the medial elbow structures begins by visually identifying or palpating the medial epicondyle of the humerus. The transducer is then placed in long axis to the forearm with the proximal aspect over the medial epicondyle (Fig. 4-9). The characteristic hyperechoic bony contours of the medial epicondyle should be seen. Distal to the medial epicondyle, the humerus has a flattened surface where the humerus articulates with the proximal ulna. In this imaging plane long axis to the forearm, as indicated by the characteristic bone contours, both the common flexor tendon and the anterior band of the ulnar collateral ligament can be identified (see Fig. 4-9B). The origin of the common flexor tendon should be seen at the superficial aspect of the medial epicondyle as hyperechoic and fibrillar, with transition to hypoechoic musculature more distally. In addition, the anterior band of the ulnar collateral ligament is seen attached to the medial epicondyle as hyperechoic and fibrillar, but somewhat more compact than that of tendon. If not perpendicular to the ligament, the anterior band of the ulnar collateral ligament will be hypoechoic from anisotropy, but still fairly uniform in thickness where it extends distally over the joint space to insert on the proximal ulna.6 The anterior band of the ulnar collateral ligament has a somewhat variable appearance at its proximal attachment to the humerus; it may appear as a uniform band, or it may fan out more proximally, interspersed with hyperechoic fatty tissue.7 The normal joint recess of the elbow extends proximally between the anterior band of the ulnar collateral ligament and adjacent humerus, but it should not extend medially from this point at the humeral attachment of the ligament or distal over the ulna. The long axis view is the key plane in the imaging of both the common flexor tendon and anterior band of the ulnar collateral ligament, although if a pathologic process is identified, further characterization is completed by imaging in short axis to these structures. In addition, the ulnar collateral ligament and medial joint space can be evaluated with dynamic valgus stress with the elbow in slight flexion to assess for ligamentous injury.8,9
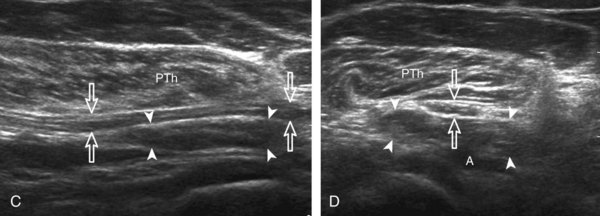
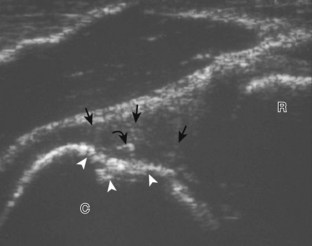
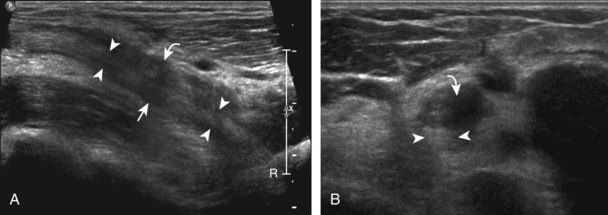
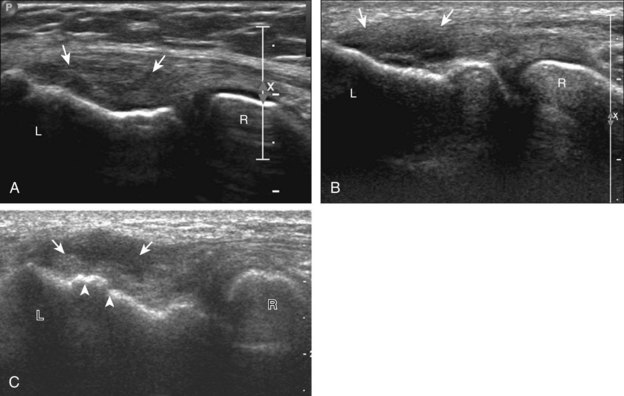
After evaluation of the common flexor tendon and anterior band of the ulnar collateral ligament is completed, attention is turned to the cubital tunnel region more posteriorly. To evaluate the cubital tunnel region, the elbow is turned outward so that the bony protuberances of the olecranon process and the medial epicondyle can be visualized and are palpable. Evaluation should begin with the elbow extended; if the elbow is flexed at this point, it is possible that the ulnar nerve may dislocate and be difficult to locate, and identification of an anconeus epitrochlearis becomes difficult as well (see discussion later). The ultrasound transducer is placed in the transverse plane between the olecranon process and the medial epicondyle, and the characteristic hyperechoic and shadowing bone contours of these structures are seen (Fig. 4-10A and B). The ulnar nerve is visible as speckled or honeycomb in appearance from hypoechoic nerve fascicles and hyperechoic connective tissue. However, the ulnar nerve posterior to the medial epicondyle often appears hypoechoic surrounded by hyperechoic fat and may be bilobed or bifid. Superficial to the ulnar nerve, the cubital tunnel retinaculum (or Osborne fascia) is located and, when present, appears as a thin structure between the olecranon and medial epicondyle. Distally, the ulnar nerve can be followed into the true cubital tunnel between the humeral and ulnar heads of the flexor carpi ulnaris and under the arcuate ligament (see Fig. 4-10C). With rotation of the transducer 90 degrees, the ulnar nerve can be evaluated in long axis (see Fig. 4-10D and E).
It is also important to evaluate the cubital tunnel region dynamically for pathology.10 With the transducer again placed in the transverse plane between the medial epicondyle and olecranon process and fixed over the medial epicondyle, the patient is asked to actively flex the elbow (Fig. 4-11). During this maneuver, the olecranon process moves out of the imaging plane and is replaced by the hypoechoic triceps brachii muscle. It is often helpful to first perform this maneuver passively so that if the bone contour of the medial epicondyle apex is no longer visualized, the movement can be stopped and the transducer repositioned until the epicondyle is found again and the motion continued. Normally during elbow flexion, the ulnar nerve moves toward the apex of the medial epicondyle but should not translate over the epicondyle anteriorly. Abnormal ulnar nerve translation over the medial epicondyle may be felt as a palpable snap through the transducer, and typically it returns back into normal position as the elbow is extended. It is important not to place too much pressure with the transducer during this dynamic evaluation because this may inhibit the abnormal ulnar nerve translation; intermittent reduction in transducer pressure during the maneuver avoids this pitfall. Ulnar nerve dislocation has been described in up to 20% of asymptomatic individuals, so it is important to correlate with abnormal ulnar nerve morphology and symptoms.11 It is also essential to differentiate isolated ulnar nerve dislocation from snapping triceps syndrome. In this situation, both the medial head of the triceps muscle and the ulnar nerve dislocate over the medial epicondyle of the humerus in elbow flexion.7
Lateral Evaluation
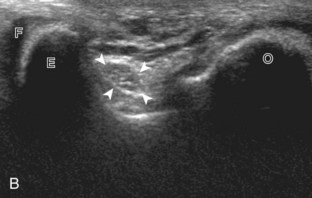
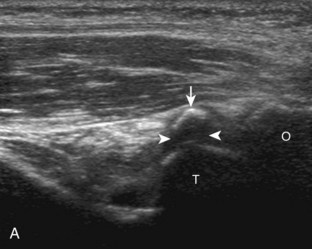
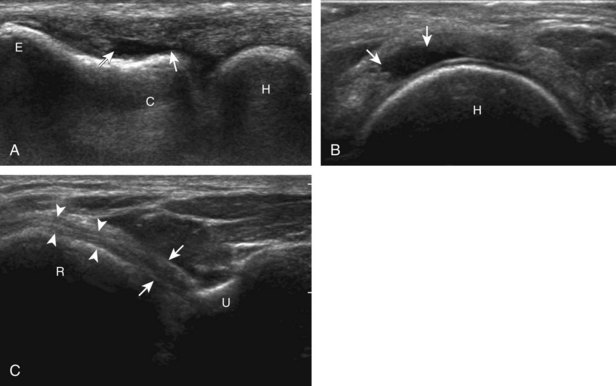
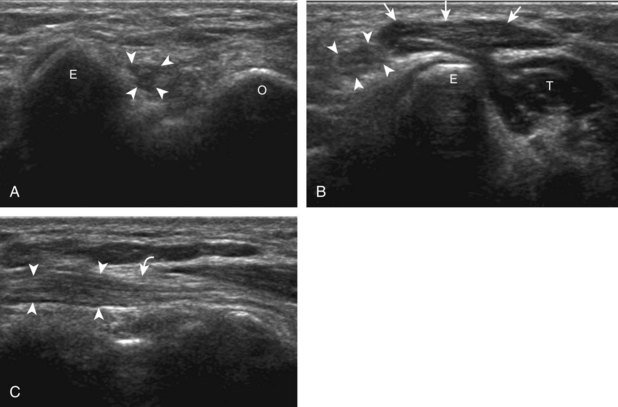
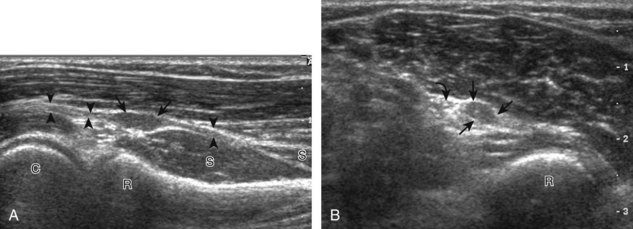
For evaluation of the lateral elbow structures, the arm is rotated inward and slightly flexed. Structures of interest laterally include the common extensor tendon, the radial collateral ligament complex, the radial head and annular recess, and the capitellum. Unlike the medial aspect of the elbow, the lateral epicondyle is not clearly visible to the eye and is more difficult to palpate. Therefore, bone landmarks as seen at sonography are used for orientation. To begin, the transducer is placed in long axis relative to the forearm over the lateral elbow (Fig. 4-12A), and the characteristic hyperechoic shadowing contour of the radial head is readily identified (see Fig. 4-12B). More proximal scanning in this plane reveals the radius articulation with the capitellum, and more proximally, the relatively flattened contour of the lateral epicondyle (see Fig. 4-12C). At this site, the hyperechoic and fibrillar common extensor tendon can be seen originating on the lateral epicondyle. Although the long axis view is optimum in identification of the common extensor tendon, any abnormality should also be characterized in short axis as well. Care should be taken to include evaluation of the most anterior aspect of the common extensor tendon, where tendon abnormalities most commonly occur. Deep to the common extensor tendon in the long axis plane over the lateral epicondyle is the radial collateral ligament (see Fig. 4-12C).12 It is often difficult to discern the separation between the proximal common extensor tendon and the adjacent radial collateral ligament; however, if one follows these structures distally, the deeper radial collateral ligament will attach to the annular ligament, seen immediately over the radial head, whereas the more superficial common extensor tendon will continue more superficial and become muscle. If the transducer is placed over the lateral elbow and angled posteriorly from the distal humerus to the ulna, the hyperechoic and fibrillar lateral ulnar collateral ligament can be seen (see Fig. 4-12D).12,13 At the level of the radial neck, the collapsed annular recess is difficult to discern unless it is abnormally distended (see Fig. 4-20B).
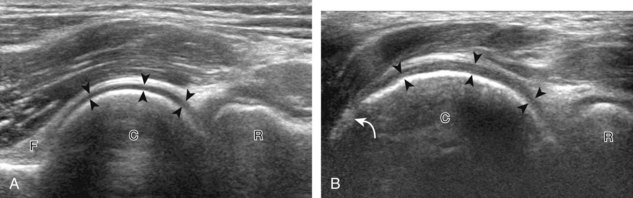
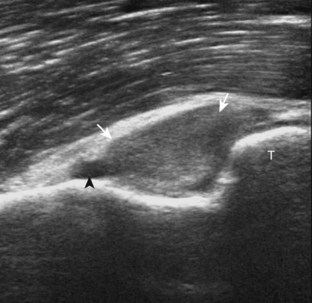
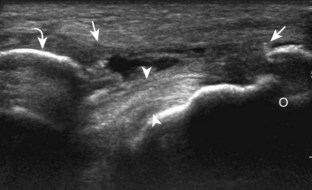
With elbow extension and the transducer anterolateral in the sagittal plane, the thin uniform hypoechoic layer of hyaline cartilage can be seen over the anterior aspect of the capitellum (Fig. 4-13A). At the radiocapitellar joint, a hyperechoic, triangular, meniscus-like synovial reflection or fold, also termed the posterolateral plica, extends from the radial collateral ligament and joint capsule into the joint.14,15 With movement of the transducer posteriorly over the capitellum, the irregular cortex represents a normal appearance void of cartilage and should not be misinterpreted as an osteochondral abnormality.14 With the elbow in flexion and the transducer posterior in the sagittal plane, the central and posterior aspect of the capitellum hyaline cartilage can also be visualized (Fig. 4-13B).
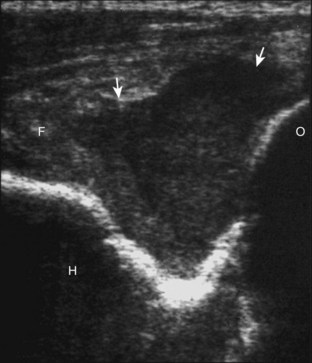
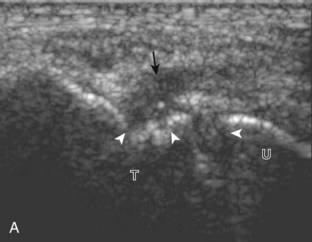
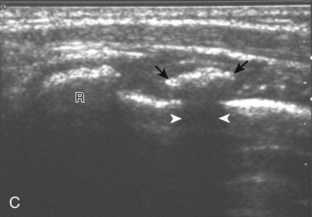
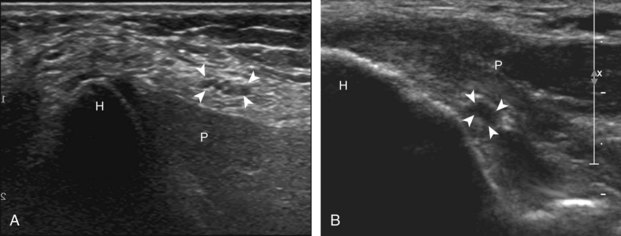
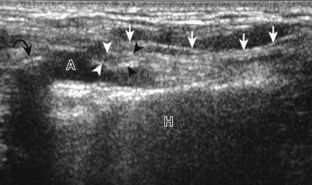
For evaluation of the radial nerve, one approach is to first find the oblique fascial plane between the brachioradialis and the brachialis anteriorly in the transverse plane, where the deep and superficial branches of the radial nerve are seen as round and hypoechoic (Fig. 4-14A; see Fig. 4-2B). These individual branches can be followed proximally in short axis where they join to form the radial nerve (see Fig. 4-14B and C). Evaluation can continue more proximal to follow the radial nerve as it traverses the intermuscular fascia and follows the posterior cortex of the humerus. The transducer is turned 90 degrees to evaluate the radial nerve and its branches in long axis as well. Following the radial nerve branches distally, the deep branch is seen entering into the supinator muscle as the posterior interosseous nerve (see Fig. 4-14D). The deep branch of the radial nerve often changes shape as it passes beneath the arcade of Frohse and should not be interpreted as nerve swelling.16 The superficial branch of the radial nerve may also be followed distally into the forearm.
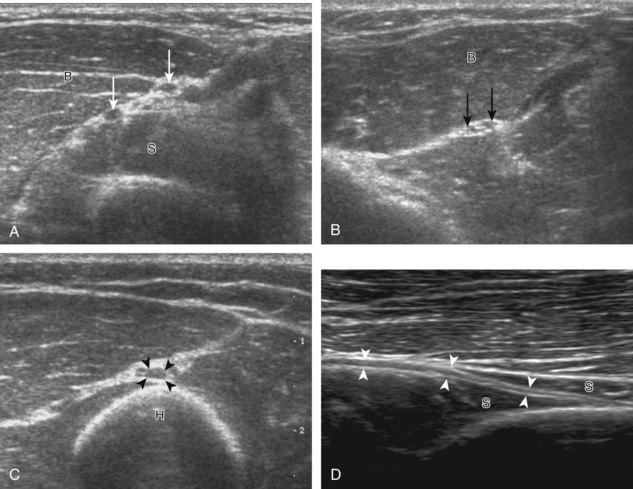
FIGURE 4-14 Radial nerve evaluation.
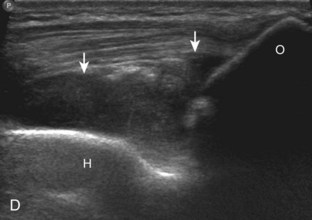
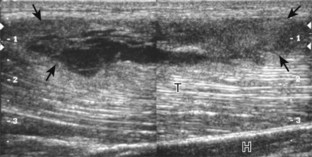
Transverse imaging over anterior elbow (see Fig. 4-2A) shows (A) the superficial and deep branches of the radial nerve (arrows) deep to the brachioradialis (B). Sequential proximal imaging (B and C) shows the radial nerve branches (arrows) joining to form radial nerve (arrowheads) adjacent to the posterior humerus (H). D, Sagittal imaging shows the deep branch of the radial nerve (arrowheads) in long axis between the two heads of the supinator muscle (S).
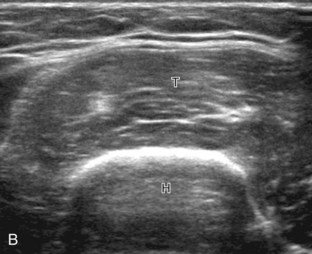
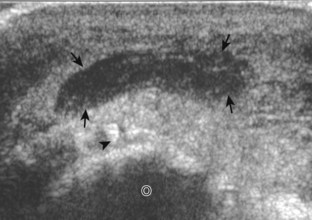
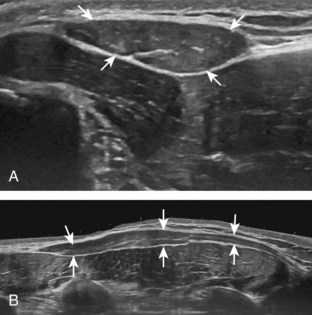
Posterior Evaluation
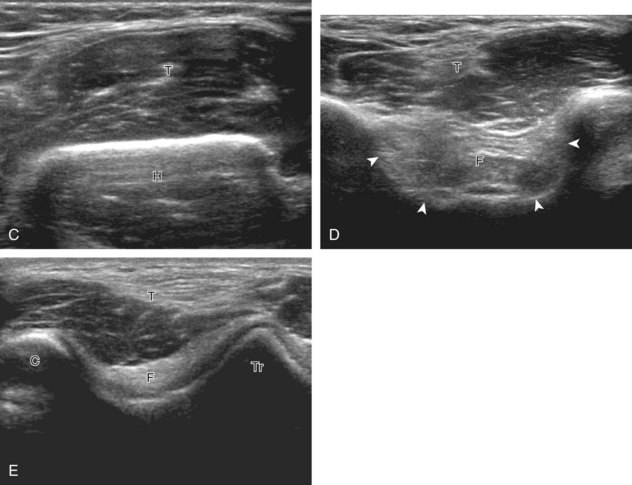
To evaluate the posterior structures of the elbow, the patient is asked to flex the elbow to 90 degrees. If the patient is supine, this can be accomplished by asking the patient to place his or her hand across the abdomen. Structures of interest include the posterior joint recess, the triceps brachii, and the soft tissues over the olecranon. By placing the transducer posteriorly in the sagittal plane over the proximal elbow, the characteristic hyperechoic shadowing bone contours of the humerus are identified (Fig. 4-15). As the humeral diaphysis approaches the elbow joint, there is a pronounced concavity, which represents the olecranon fossa. This is also demonstrated in the transverse plane relative to the humerus (Fig. 4-16). This fossa is normally filled with the hyperechoic posterior elbow fat pad and is the site of evaluation for joint fluid, intra-articular bodies, and other joint processes. The hypoechoic trochlear and capitellum hyaline cartilage can also be identified. Superficial to the olecranon recess, the hypoechoic triceps brachii muscle and more distal hyperechoic tendon can be seen inserting onto the olecranon process. Although not discernable in the normal situation, the superficial layer of the triceps brachii represents the confluence of the lateral and long heads, whereas the deeper layer with a very short tendon represents the medial head of the triceps brachii. With elbow extension, the soft tissues superficial to the olecranon process can be evaluated for olecranon bursal fluid. It is important to float the transducer with a thick layer of gel in evaluation for olecranon bursal fluid because minimal transducer pressure may displace small amounts of fluid away from view. Although the sagittal plane is most important in evaluation of the foregoing structures, imaging in the orthogonal transverse plane also shows the above anatomic structures and is important when characterizing pathology.
Joint and Bursa Abnormalities
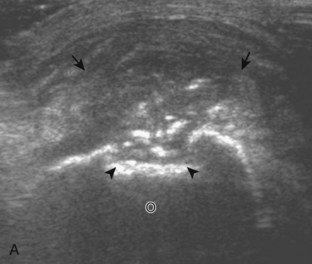
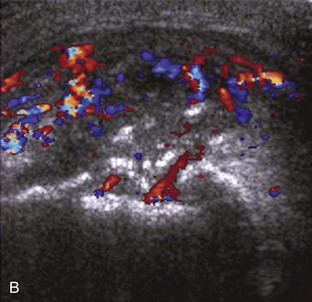
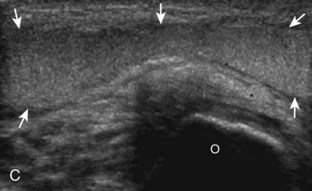
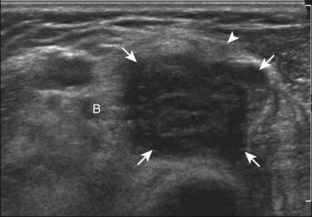
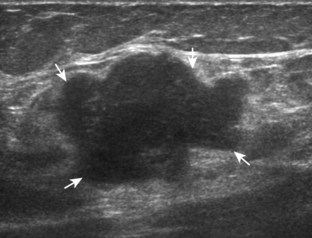
Although a joint effusion may distend the anterior and less commonly the annular joint recesses, the posterior olecranon recess in elbow flexion is the most sensitive location for identification of joint fluid (Fig. 4-17).17 Imaging in the sagittal plane over the posterior joint recess demonstrates superior and posterior displacement of the hyperechoic fat pad when the joint is distended, similar to findings at radiography. Fat pad displacement, both in the anterior and posterior joint fossae, may result from anechoic simple fluid, although complex fluid may vary from hypoechoic to hyperechoic (Fig. 4-18). Heterogeneous joint fluid may be caused by hemorrhage or infection (Fig. 4-19). Synovial hypertrophy, more commonly diffuse, may also distend the joint recesses and may appear hypoechoic (or, less commonly, isoechoic or hyperechoic) relative to the subcutaneous fat. The findings of joint recess compressibility, redistribution or motion of joint recess contents with transducer pressure, and lack of increased blood flow on color or power Doppler imaging suggest complex fluid rather than synovial hypertrophy when their gray-scale appearances are similar. Synovial hypertrophy may be the result of infection (Fig. 4-20), rheumatoid arthritis (Fig. 4-21), and other inflammatory arthritides (Fig. 4-22), or less likely an adjacent bone process, such as intra-articular osteoid osteoma (Fig. 4-23, online).18 Chronic synovial hypertrophy can result in significant distention of the joint recesses, potentially compressing the ulnar nerve (Fig. 4-24) and radial nerve (Fig. 4-25). In the setting of synovitis, cortical discontinuity and irregularity could represent bone erosions (see Figs. 4-20 and 4-21). Other synovial proliferative disorders, such as pigmented villonodular synovitis and synovial osteochondromatosis, are also possible, with calcified hyperechoic foci identified within the synovium in the latter condition. Rarely, a soft tissue mass, such as an intra-articular fibroma, may be found (Fig. 4-26, online). In addition to evaluation of the joint recesses for fluid or synovial hypertrophy, it is important to evaluate for intra-articular bodies, which if ossified will be hyperechoic, with possible shadowing. Common sites for intra-articular bodies include the olecranon, coronoid, and annular recesses (Fig. 4-27). Evaluation of the articular hyaline cartilage for an osteochondral abnormality, particularly over the capitellum, is important in this setting because the donor site for the intra-articular body may be identified (Fig. 4-28). In patients with trauma, joint effusion may be hemorrhagic, and the finding of step-off deformity of the radial head or neck indicates fracture (Fig. 4-29).
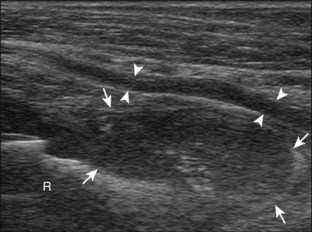
FIGURE 4-25 Radial nerve, deep branch compression: rheumatoid arthritis.
(Courtesy of V. Flores, MD, Fort Worth, Tex. From Jacobson JA, Fessell DP, Lobo Lda G, et al: Entrapment neuropathies I: upper limb (carpal tunnel excluded). Semin Musculoskel Radiol 14:473–486, 2010.)
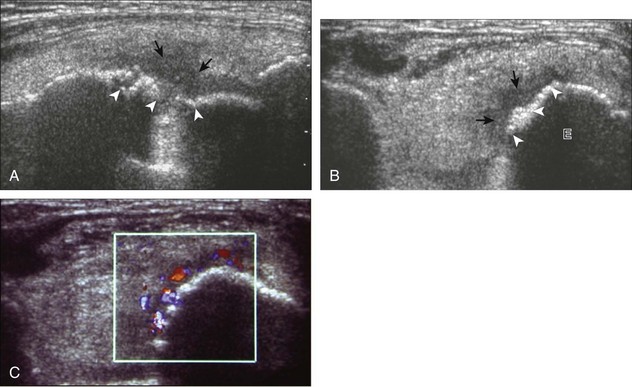
FIGURE 4-23 Intra-articular osteoid osteoma.
(From Ebrahim FS, Jacobson JA, Lin J, et al: Intraarticular osteoid osteoma: sonographic findings in three patients with radiographic, CT, and MR imaging correlation. AJR Am J Roentgenol 177:1391–1395, 2001.)
The olecranon bursa is located superficial to the olecranon process of the ulna and is a common site of pathology. Although the normal and collapsed olecranon bursa is difficult to identify, anechoic or hypoechoic distention makes this structure quite conspicuous. It is important to float the transducer on a layer of thick gel in evaluation for olecranon bursal fluid because minimal transducer pressure may displace bursal fluid from view (Video 4-3)![]() . If the bursal distention is hypoechoic, isoechoic, or hyperechoic, considerations include complex fluid, synovial hypertrophy, and other types of synovial proliferation. Similar to joint recess distention, the findings of joint recess compressibility, redistribution or motion of bursal contents with transducer pressure, and lack of increased blood flow on color or power Doppler imaging suggest complex fluid over synovial hypertrophy when their gray-scale appearances are similar (Video 4-4)
. If the bursal distention is hypoechoic, isoechoic, or hyperechoic, considerations include complex fluid, synovial hypertrophy, and other types of synovial proliferation. Similar to joint recess distention, the findings of joint recess compressibility, redistribution or motion of bursal contents with transducer pressure, and lack of increased blood flow on color or power Doppler imaging suggest complex fluid over synovial hypertrophy when their gray-scale appearances are similar (Video 4-4)![]() . Causes of bursal distention include trauma (Fig. 4-30), gout (Fig. 4-31), rheumatoid arthritis (Fig. 4-32), and infection (Fig. 4-33). The characteristic location and well-defined borders of the olecranon bursa distinguish this from a nonspecific fluid collection or abscess. If there is concern for infection, ultrasound-guided percutaneous aspiration may be considered (see Fig. 4-30A). The presence of cortical irregularity could indicate adjacent erosions related to inflammation. Another bursa in the elbow, the bicipitoradial bursa, is described later in the discussion of the biceps brachii tendon.
. Causes of bursal distention include trauma (Fig. 4-30), gout (Fig. 4-31), rheumatoid arthritis (Fig. 4-32), and infection (Fig. 4-33). The characteristic location and well-defined borders of the olecranon bursa distinguish this from a nonspecific fluid collection or abscess. If there is concern for infection, ultrasound-guided percutaneous aspiration may be considered (see Fig. 4-30A). The presence of cortical irregularity could indicate adjacent erosions related to inflammation. Another bursa in the elbow, the bicipitoradial bursa, is described later in the discussion of the biceps brachii tendon.
Tendon and Muscle Abnormalities
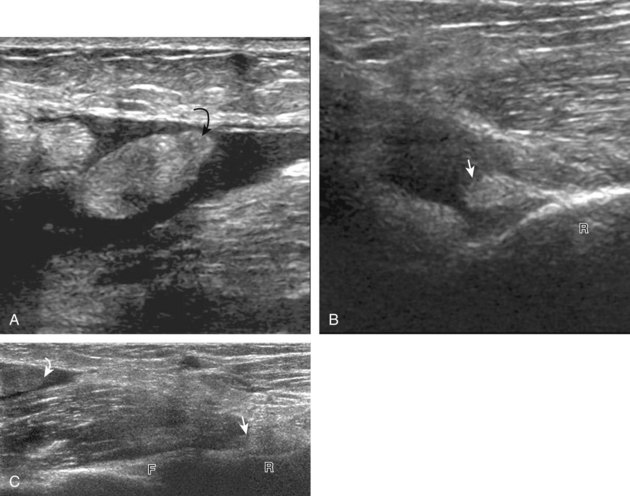
Biceps Brachii
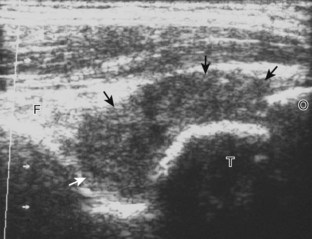
Distal biceps brachii tendon tears most commonly occur near the tendon’s insertion 1 to 2 cm proximal to the radial tuberosity.19 Usually secondary to forced extension against active elbow flexion, this injury increases in prevalence with increasing age, typically seen after the age of 40 years. With a full-thickness tear, many injuries are associated with significant retraction of the torn tendon stump, typically visualized several centimeters proximal to the radius directly superficial to the brachialis muscle and at the level of the elbow joint (Fig. 4-34). However, one must be aware that retraction may be minimal or absent when the bicipital aponeurosis (or lacertus fibrosus), which extends from the biceps medially, is intact (Fig. 4-35).19,20 Like other tendon tears, a full-thickness tear is characterized by anechoic or hypoechoic tendon fiber disruption. The presence of tendon retraction at the tendon tear is a useful finding to indicate a full-thickness tear.
The diagnosis of nonretracted full-thickness tear, partial-thickness tear, and tendinosis of the distal biceps brachii tendon becomes more problematic because of the oblique course of the distal tendon and resulting anisotropy.20 Tendinosis appears as hypoechoic swelling of the tendon (Fig. 4-36), whereas partial-thickness tears have superimposed hypoechoic or anechoic tendon fiber disruption and tendon thinning (Fig. 4-37). In contrast, the distal biceps brachii tendon should be uniform in thickness even when hypoechoic from anisotropy. Distal partial-thickness tear may only involve one of the two heads.1 Isolated tear of the superficial short head may be seen, where distal shadowing from the torn and retracted tendon stump may create difficulty in evaluation of the deeper long head (Fig. 4-38). To differentiate a partial-thickness tendon tear from a nonretracted full-thickness tear, lateral evaluation with dynamic imaging is helpful (see Fig. 4-6).5 In the setting of a full-thickness tear, the visualized proximal tendon segment will show little or no movement when the hand is moved from pronation to neutral (Video 4-5)![]() . In contrast, a partial-thickness tear will show movement or translation of the tendon equal to the amount of rotation of the radial tuberosity, indicating that fibers remain attached to the radial tuberosity (Video 4-6)
. In contrast, a partial-thickness tear will show movement or translation of the tendon equal to the amount of rotation of the radial tuberosity, indicating that fibers remain attached to the radial tuberosity (Video 4-6)![]() . Similar technique is used to evaluate for re-tear after tendon repair (Video 4-7)
. Similar technique is used to evaluate for re-tear after tendon repair (Video 4-7)![]() . Dynamic evaluation can be completed using the medial approach as well.4
. Dynamic evaluation can be completed using the medial approach as well.4
One must also be aware of another pathologic condition at the distal biceps tendon that can cause interpretation difficulties, namely, distention of the bicipitoradial bursa. This normal bursa surrounds the distal biceps brachii tendon as it approaches the radial tuberosity.21 When the bursa is distended, it may contain anechoic simple fluid, or it may appear as heterogeneous hypoechoic, isoechoic, and hyperechoic complex fluid and synovial hypertrophy with possible flow on color or power Doppler imaging (Fig. 4-39).22 When symptomatic, this condition has also been called cubital bursitis and may compress the superficial branch of the radial nerve (Fig. 4-40).21 This bursa may also be confused with a nonspecific heterogeneous mass at imaging. The key to an accurate diagnosis of bicipitoradial bursitis is identification of its horseshoe-shaped configuration as it surrounds the distal biceps brachii tendon (Video 4-8)![]() . Although any inflammatory or proliferative condition that involves a bursa may affect the bicipitoradial bursa, this condition is most commonly the result of repetitive trauma.21 One must also be aware that a tendon sheath is not present at the distal biceps brachii tendon, so the diagnosis of tenosynovitis is not possible at this location.
. Although any inflammatory or proliferative condition that involves a bursa may affect the bicipitoradial bursa, this condition is most commonly the result of repetitive trauma.21 One must also be aware that a tendon sheath is not present at the distal biceps brachii tendon, so the diagnosis of tenosynovitis is not possible at this location.
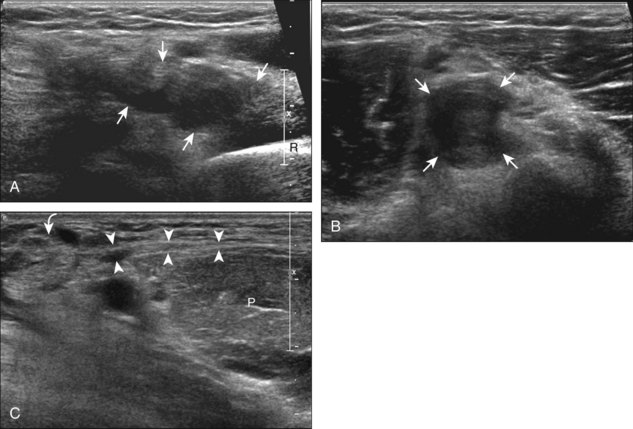
Triceps Brachii
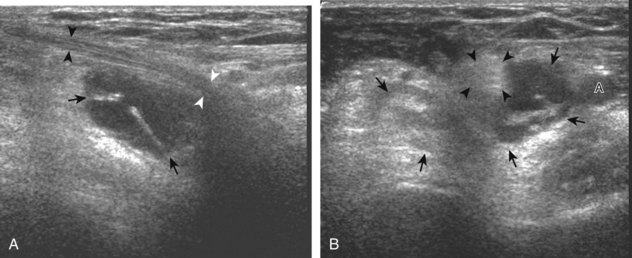
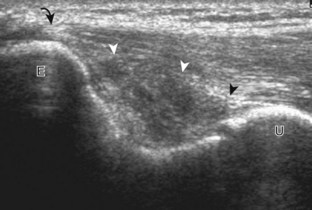
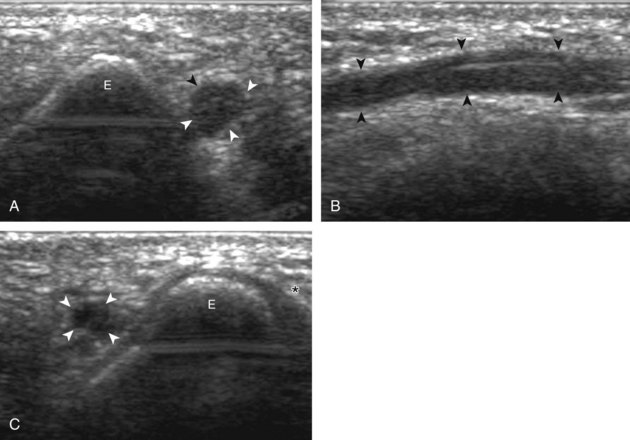
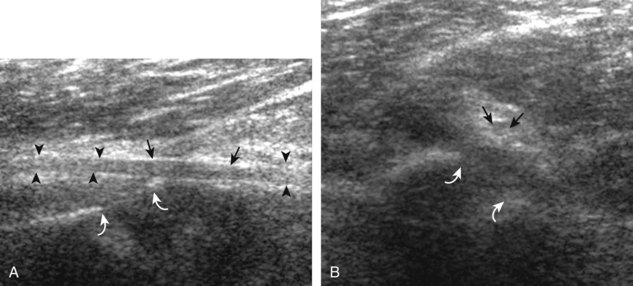
Injuries to the triceps brachii may take the form of direct impact injury or distal avulsion. As with any muscle, a direct impact can cause muscle tear and hemorrhage, most typically at the muscle belly with a heterogeneous but predominantly hypoechoic appearance (Fig. 4-41). Distally, triceps tendon tears and avulsions at the olecranon process are possible. A full-thickness tear appears as complete anechoic or hypoechoic tendon disruption with retraction. Tendinosis appears as hypoechoic swelling of intact fibers, whereas a partial-thickness tendon tear appears as incomplete hypoechoic or anechoic tendon fibers disruption. Partial-thickness tears most commonly involve the superficial layer of the tendon, which is the combined lateral and long head attachments, typically associated with a fractured and displaced enthesophyte (Figs. 4-42 and 4-43) (Video 4-9)![]() .23 It is important to identify the intact deeper medial head, which is predominantly muscle with a very short tendon attachment, to exclude full-thickness tear. Another abnormality of the triceps muscle, called snapping triceps syndrome, is described later, under the discussion of the ulnar nerve and cubital tunnel. Lastly, although a well-defined enthesophyte commonly involves the distal triceps brachii tendon from degeneration, the presence of an ill-defined enthesophyte with adjacent abnormal tendon and hyperemia could indicate an inflammatory enthesopathy, as seen with seronegative spondyloarthropathies such as psoriatic arthritis (Fig. 4-44).
.23 It is important to identify the intact deeper medial head, which is predominantly muscle with a very short tendon attachment, to exclude full-thickness tear. Another abnormality of the triceps muscle, called snapping triceps syndrome, is described later, under the discussion of the ulnar nerve and cubital tunnel. Lastly, although a well-defined enthesophyte commonly involves the distal triceps brachii tendon from degeneration, the presence of an ill-defined enthesophyte with adjacent abnormal tendon and hyperemia could indicate an inflammatory enthesopathy, as seen with seronegative spondyloarthropathies such as psoriatic arthritis (Fig. 4-44).
Common Flexor and Extensor Tendons
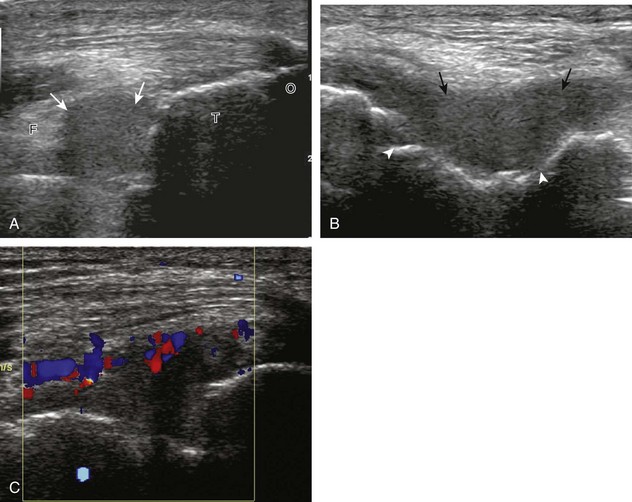
Abnormalities of the common flexor tendon origin at the medial epicondyle (Fig. 4-45) and the common extensor tendon origin at the lateral epicondyle (Figs. 4-46 and 4-47) are commonly referred to as epicondylitis, or golfer’s and tennis elbow, respectively.24 The term epicondylitis is a misnomer in that the tendon is primarily involved and not the epicondyle, and the abnormality consists of degeneration, tendinosis, and possible tendon tear rather than true active inflammation.25 This process is most often from trauma or overuse conditions, and with regard to lateral epicondylitis, the extensor carpi radialis brevis component of the common extensor tendon (seen most anterior) is most commonly affected.26 At sonography, tendinosis appears as hypoechoic swelling of the involved tendon (>4.2 mm if common extensor tendon), with possible hyperechoic calcification and adjacent bone irregularity.25,27,28 Hyperemia on color or power Doppler imaging is variable. A superimposed partial-thickness tear appears as anechoic clefts and incomplete fiber discontinuity.25,29 Ultrasound-guided tendon fenestration has been used to treat this condition with success (see Chapter 9).30,31 Uncommonly, a full-thickness tear of the common extensor tendon can be seen with complete discontinuity and retraction (Fig. 4-48). Given the close proximity of the radial collateral ligament to the common extensor tendon, it is important to distinguish which structure is involved and in fact both may be abnormal.12,32 The size of an intrasubstance common extensor tendon tear and the presence of a radial collateral ligament tear indicate poor outcome.29
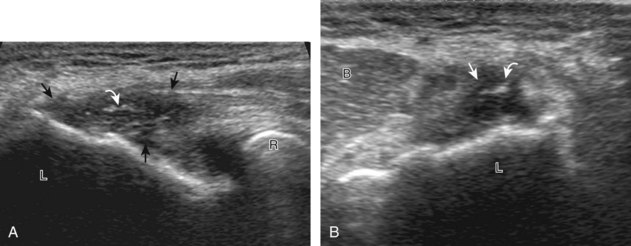
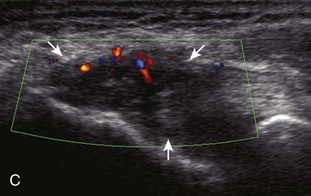
FIGURE 4-47 Lateral epicondylitis.
(From Jacobson JA, Miller BS, Morag Y: Golf and racquet sports injuries. Semin Musculoskelet Radiol 9:346–359, 2005.)
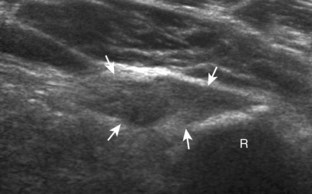
Ligament Abnormalities
The medial elbow joint is stabilized by the ulnar collateral ligament, which consists of a strong anterior band, a posterior band, and a weaker oblique band. Evaluation primarily focuses on the anterior band, normally hyperechoic with compact fibers that extend from the undersurface of the medial epicondyle to the sublime tubercle of the proximal ulna, although its appearance may be hypoechoic from anisotropy.6,7 A partial tear or sprain of the ulnar collateral ligament appears as hypoechoic swelling and heterogeneity of the ligament, but without complete ligament fiber disruption (Fig. 4-49). A remote injury may result in an intact but lax ligament (Fig. 4-50). A full-thickness tear appears as complete fiber discontinuity, with variable anechoic, hypoechoic, and isoechoic fluid and hemorrhage (Fig. 4-51).33 Distinguishing between a partial-thickness and full-thickness tear may be difficult, especially if the tear is subacute and hemorrhage is present. To assist with the differentiation, dynamic imaging is employed (Videos 4-10 and 4-11)![]() . Under sonographic observation, the minimally flexed elbow (about 30 degrees) is placed into valgus stress with the hand supinated. This can be accomplished if the patient is lying down by manually applying valgus pressure with the arm extending off of the bed, or with the assistance of another person if the patient is seated.8 In addition to visible separation of the torn ligament ends, abnormal widening of the joint immediately beneath the ligament (>0.5 mm difference between rest and stress) indicates full-thickness involvement.9 It is important to compare this with the asymptomatic contralateral side because asymmetry supports the pathologic findings, although some asymmetry may be normal in asymptomatic baseball pitchers.9
. Under sonographic observation, the minimally flexed elbow (about 30 degrees) is placed into valgus stress with the hand supinated. This can be accomplished if the patient is lying down by manually applying valgus pressure with the arm extending off of the bed, or with the assistance of another person if the patient is seated.8 In addition to visible separation of the torn ligament ends, abnormal widening of the joint immediately beneath the ligament (>0.5 mm difference between rest and stress) indicates full-thickness involvement.9 It is important to compare this with the asymptomatic contralateral side because asymmetry supports the pathologic findings, although some asymmetry may be normal in asymptomatic baseball pitchers.9
At the lateral aspect of the elbow, the radial collateral ligament, the annular ligament, and the lateral ulnar collateral ligament can be identified.12,13 As in the ulnar collateral ligament, partial tears appear as partial hypoechoic tendon disruption, whereas full-thickness tears appear as complete ligament fiber discontinuity (Fig. 4-52). Joint instability may also be demonstrated with varus stress in the setting of a full-thickness tear (Video 4-12)![]() . The proximal aspect of the radial collateral ligament is in close proximity to the common extensor tendon, and both may be abnormal (see Fig. 4-48). It is important to evaluate the lateral elbow during hand supination and pronation for abnormal radial head movement (Fig. 4-53) (Video 4-13)
. The proximal aspect of the radial collateral ligament is in close proximity to the common extensor tendon, and both may be abnormal (see Fig. 4-48). It is important to evaluate the lateral elbow during hand supination and pronation for abnormal radial head movement (Fig. 4-53) (Video 4-13)![]() or abnormal snapping of the annular ligament (Video 4-14)
or abnormal snapping of the annular ligament (Video 4-14)![]() .
.
Peripheral Nerve Abnormalities
Ulnar Nerve
The elbow has several sites where the ulnar nerve is prone to injury or entrapment.34 Between the medial epicondyle and the olecranon process, as the ulnar nerve passes beneath the cubital tunnel retinaculum or Osborne fascia, the ulnar nerve may be affected by acute trauma, chronic repetitive injury with elbow flexion, and ulnar nerve subluxation and dislocation. More distally, the ulnar nerve may be compressed where it enters the true cubital tunnel, formed by the humeral and ulnar origins of the flexor carpi ulnaris bridged by the arcuate ligament.3 The ultrasound diagnosis of ulnar nerve entrapment at this site or cubital tunnel syndrome relies on the visualization of hypoechoic swelling of the ulnar nerve just proximal to the cubital tunnel, usually with a transition to normal size within the cubital tunnel. A cross-sectional area of the ulnar nerve greater than 9 mm2 at the site of maximal enlargement is considered abnormal (Fig. 4-54).35
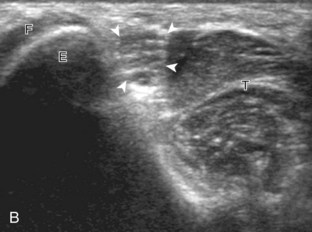
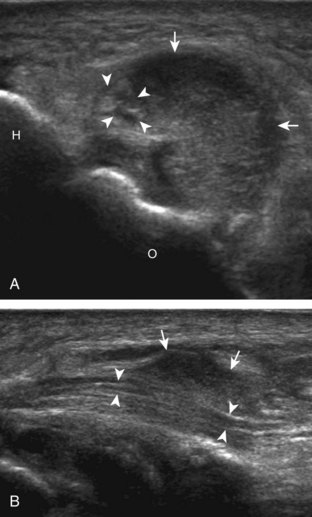
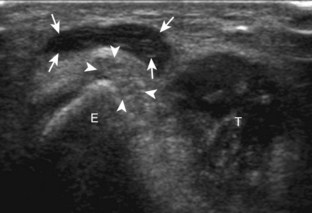
Although nerve entrapment may be idiopathic or from overuse, other causes of ulnar neuritis must be considered when an abnormally swollen ulnar nerve is visualized. One such cause is transient dislocation of the ulnar nerve, which may occur with absence of a cubital tunnel retinaculum.36 In this condition, the ulnar nerve dislocates medially and anteriorly over the medial epicondyle with elbow flexion, which causes direct nerve irritation and makes it prone to direct injury (Fig. 4-55) (Video 4-15)![]() .37 With elbow extension, the ulnar nerve relocates to normal position within the cubital tunnel. Up to 20% of individuals with ulnar nerve dislocation may be asymptomatic, so it is important to correlate with the presence of abnormal ulnar nerve swelling and symptoms that suggest neuritis. Another similar pathologic process associated with ulnar nerve dislocation is snapping triceps syndrome (Fig. 4-56) (Videos 4-16 and 4-17)
.37 With elbow extension, the ulnar nerve relocates to normal position within the cubital tunnel. Up to 20% of individuals with ulnar nerve dislocation may be asymptomatic, so it is important to correlate with the presence of abnormal ulnar nerve swelling and symptoms that suggest neuritis. Another similar pathologic process associated with ulnar nerve dislocation is snapping triceps syndrome (Fig. 4-56) (Videos 4-16 and 4-17)![]() .10 Described in weight lifters, this condition is characterized by abnormal dislocation of the ulnar nerve and subluxation of the medial head of the triceps muscle with elbow flexion and reduction in elbow extension, which may result in the palpation of two snaps rather than one with isolated ulnar nerve dislocation. One treatment for ulnar neuritis and dislocation is surgical transposition of the ulnar nerve, which may then be subcutaneous over the pronator teres (Fig. 4-57A) or submuscular in location (see Fig. 4-57B).
.10 Described in weight lifters, this condition is characterized by abnormal dislocation of the ulnar nerve and subluxation of the medial head of the triceps muscle with elbow flexion and reduction in elbow extension, which may result in the palpation of two snaps rather than one with isolated ulnar nerve dislocation. One treatment for ulnar neuritis and dislocation is surgical transposition of the ulnar nerve, which may then be subcutaneous over the pronator teres (Fig. 4-57A) or submuscular in location (see Fig. 4-57B).
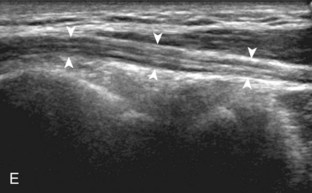
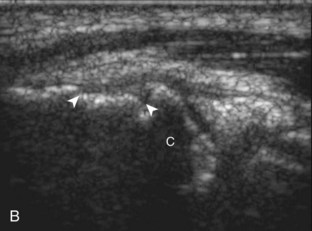
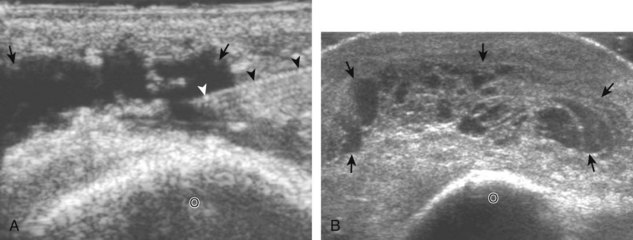
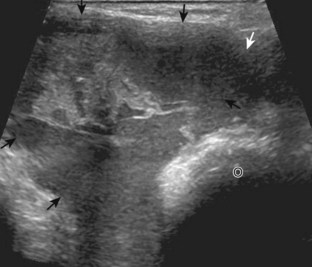
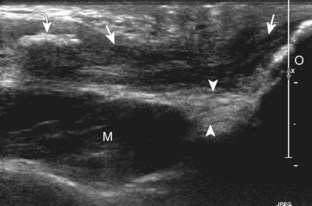
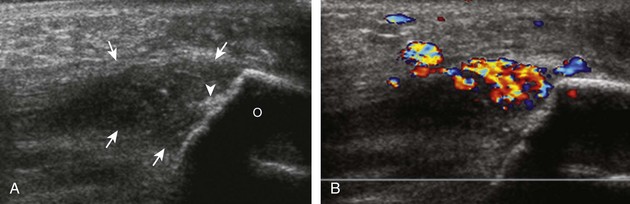
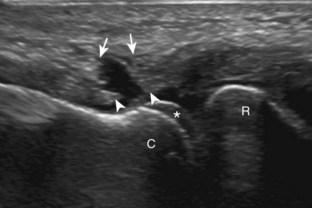
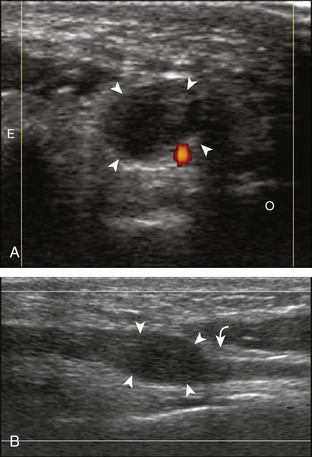
Another potential cause of ulnar nerve compression is an anconeus epitrochlearis muscle, which is a normal variant that occurs in up to 23% of the population (Fig. 4-58).38 The anconeus epitrochlearis muscle has a variable size but characteristically is hypoechoic with hyperechoic fibroadipose tissue similar to other muscles and extends from the triceps brachii toward the medial epicondyle in place of Osborne fascia. The diagnosis of anconeus epitrochlearis is easiest when the elbow is in extension, where no muscle tissue should be present between the olecranon and medial epicondyle, which is in contrast to elbow flexion, where the triceps brachii is normally located adjacent to the medial epicondyle. Dynamic imaging with elbow flexion may also show crowding deep to Osborne fascia from an anconeus epitrochlearis as well as abnormal snapping (Fig. 4-59) (Video 4-18)![]() . Lastly, the ulnar nerve may also be compressed by adjacent elbow joint abnormalities, such as synovial hypertrophy (see Fig. 4-24), intra-articular bodies, and intra-articular hemorrhage after trauma (Fig. 4-60).
. Lastly, the ulnar nerve may also be compressed by adjacent elbow joint abnormalities, such as synovial hypertrophy (see Fig. 4-24), intra-articular bodies, and intra-articular hemorrhage after trauma (Fig. 4-60).
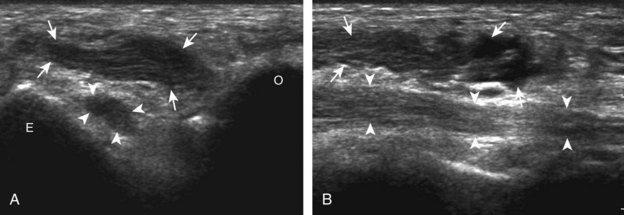
FIGURE 4-58 Anconeus epitrochlearis muscle.
(From Jacobson JA, Fessell DP, Lobo Lda G, et al: Entrapment neuropathies I: upper limb (carpal tunnel excluded). Semin Musculoskelet Radiol 14:473–486, 2010.)
Median Nerve
The median nerve courses along the anteromedial aspect of the elbow and may be entrapped at several locations, although less commonly than nerve entrapment at the wrist as part of carpal tunnel syndrome.34 One site of potential entrapment is at the level of the distal humerus, where the ligament of Struthers may extend from a normal variant bone excrescence of the anterior humerus (called the supracondylar process) to the medial epicondyle with compression of the median nerve (Fig. 4-61).39 In the antecubital region, the median nerve may be entrapped between the humeral and ulnar heads of the pronator teres and may cause pronator teres syndrome. More distally, a branch of the median nerve, the anterior interosseous nerve, may also be a site of compression from fibrous bands or an anomalous muscle. It is important to include evaluation of the distal musculature innervated by the nerve in question because increased echogenicity from atrophy may be a clue to the nerve entrapment (Fig. 4-62).40
Radial Nerve
Pathologic processes of the radial nerve include nerve injury associated with the spiral groove of the humerus, termed spiral groove syndrome, characterized by wrist drop and sensory findings but with spared triceps brachii function.3,34 One cause of radial nerve injury at this site is fracture of the humeral shaft, where the injured radial nerve can range from a swollen nerve segment (Fig. 4-63) to complete nerve transection and retraction (Fig. 4-64).41 In this latter condition, the transected nerve ends appear hypoechoic and swollen. Direct transducer pressure over the nerve end can elicit referred symptoms. The radial nerve may also be injured and swollen at the level of the spiral groove from external compression (termed Saturday night palsy). A swollen radial nerve may also show constriction by the intermuscular septum and fibrous bands (Fig. 4-65).
Another site of radial nerve entrapment involves the deep branch of the radial nerve as it courses distally and posteriorly between the two heads of the supinator (called supinator syndrome or radial tunnel syndrome).42 Just proximal to this location, abnormal hypoechoic swelling of the involved nerve can be seen at the entry site of the arcade of Frohse (Fig. 4-66). Causes of such compression may be due to a fibrous band or prior trauma, or less commonly abnormal recurrent blood vessels (termed the leash of Henry).34 Because the deep branch of the radial nerve normally flattens as it enters the supinator, it is important to assess for changes in nerve area in short axis to the nerve so as not to mistake the normal change in shape of the nerve entering the supinator as fusiform thickening in long axis.16 A mass, cyst (Fig. 4-67), bicipitoradial bursa (see Fig. 4-40), or adjacent elbow joint process (see Fig. 4-25) may cause secondary nerve compression.
Peripheral Nerve Sheath Tumors
Other possible peripheral nerve conditions that are not specific to the peripheral nerves around the elbow include peripheral nerve sheath tumors. Benign forms include schwannoma and neurofibroma and appear as a defined hypoechoic mass with low-level internal echoes.43 Plexiform neurofibromas involve peripheral nerves more extensively (Fig. 4-68) (Video 4-19)![]() . Peripheral nerve sheath tumors may be associated with increased through-transmission and can simulate a complex cyst; however, the presence of increased flow on color or power Doppler imaging indicates a solid mass. The presence of peripheral nerve continuity with the mass indicates a peripheral nerve sheath tumor. Malignant counterparts may also contain anechoic cystic or necrotic areas.
. Peripheral nerve sheath tumors may be associated with increased through-transmission and can simulate a complex cyst; however, the presence of increased flow on color or power Doppler imaging indicates a solid mass. The presence of peripheral nerve continuity with the mass indicates a peripheral nerve sheath tumor. Malignant counterparts may also contain anechoic cystic or necrotic areas.
Epitrochlear Lymph Node
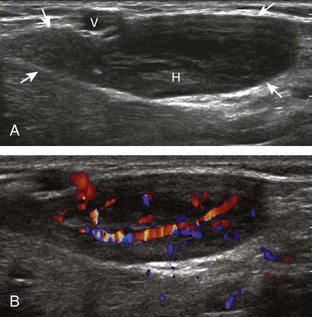
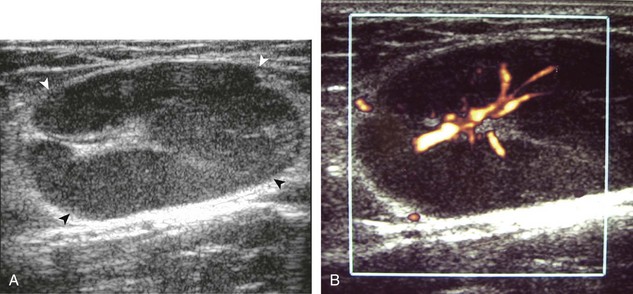
Most solid masses around the elbow that are not related to the joint are not specific for a single diagnosis. However, one must be aware of an enlarged epitrochlear lymph node, which, if correctly identified, can suggest a specific diagnosis. An epitrochlear lymph node is located at the medial aspect of the elbow just proximal to the medial epicondyle of the distal humerus between muscle and the subcutaneous tissues. A normal lymph node is oval, with an echogenic central hilum and a hypoechoic rim. The echogenic center results from interfaces between the fatty tissue and sinusoids, rather than from the fat itself, because pure fat is hypoechoic or anechoic at ultrasound. When a lymph node is enlarged but maintains an oval shape, normal echogenic hilum, and hilar vascular pattern, then hyperplasia from inflammation is suggested. One such example is cat-scratch disease (Fig. 4-69), in which the scratch of an animal such as a cat around the hand characteristically produces epitrochlear lymph node enlargement. Inflammation adjacent to the enlarged epitrochlear lymph node can create a heterogeneous appearance to the soft tissues, which can make identification of the involved lymph node difficult. If an enlarged lymph node is round with absence of the echogenic hilum, thickening of the hypoechoic cortex, and a peripheral or mixed pattern of vascularity on color and power Doppler imaging, then malignancy is suspected, although biopsy is required to provide a diagnosis. Other examples of epitrochlear lymph node enlargement include lymphoma (Fig. 4-70), metastasis, and sarcoidosis (Fig. 4-71).
1 Tagliafico A, Michaud J, Capaccio E, et al. Ultrasound demonstration of distal biceps tendon bifurcation: normal and abnormal findings. Eur Radiol. 2010;20:202–208.
2 Madsen M, Marx RG, Millett PJ, et al. Surgical anatomy of the triceps brachii tendon: anatomical study and clinical correlation. Am J Sports Med. 2006;34:1839–1843.
3 Martinoli C, Bianchi S, Pugliese F, et al. Sonography of entrapment neuropathies in the upper limb (wrist excluded). J Clin Ultrasound. 2004;32:438–450.
4 Smith J, Finnoff JT, O’Driscoll SW, et al. Sonographic evaluation of the distal biceps tendon using a medial approach: the pronator window. J Ultrasound Med. 2010;29:861–865.
5 Kalume Brigido M, De Maeseneer M, Jacobson JA, et al. Improved visualization of the radial insertion of the biceps tendon at ultrasound with a lateral approach. Eur Radiol. 2009;19:1817–1821.
6 Ward SI, Teefey SA, Paletta GA, Jr., et al. Sonography of the medial collateral ligament of the elbow: a study of cadavers and healthy adult male volunteers. AJR Am J Roentgenol. 2003;180:389–394.
7 Jacobson JA, Propeck T, Jamadar DA, et al. US of the anterior bundle of the ulnar collateral ligament: findings in five cadaver elbows with MR arthrographic and anatomic comparison—initial observations. Radiology. 2003;227:561–566.
8 De Smet AA, Winter TC, Best TM, et al. Dynamic sonography with valgus stress to assess elbow ulnar collateral ligament injury in baseball pitchers. Skeletal Radiol. 2002;31:671–676.
9 Nazarian LN, McShane JM, Ciccotti MG, et al. Dynamic US of the anterior band of the ulnar collateral ligament of the elbow in asymptomatic major league baseball pitchers. Radiology. 2003;227:149–154.
10 Jacobson JA, Jebson PJ, Jeffers AW, et al. Ulnar nerve dislocation and snapping triceps syndrome: diagnosis with dynamic sonography—report of three cases. Radiology. 2001;220:601–605.
11 Okamoto M, Abe M, Shirai H, et al. Morphology and dynamics of the ulnar nerve in the cubital tunnel: observation by ultrasonography. J Hand Surg [Br]. 2000;25:85–89.
12 Teixeira PA, Omoumi P, Trudell DJ, et al. Ultrasound assessment of the lateral collateral ligamentous complex of the elbow: imaging aspects in cadavers and normal volunteers. Eur Radiol. 2011;21:1492–1498.
13 Stewart B, Harish S, Oomen G, et al. Sonography of the lateral ulnar collateral ligament of the elbow: study of cadavers and healthy volunteers. AJR Am J Roentgenol. 2009;193:1615–1619.
14 Cotten A, Jacobson J, Brossmann J, et al. MR arthrography of the elbow: normal anatomy and diagnostic pitfalls. J Comput Assist Tomogr. 1997;21:516–522.
15 Husarik DB, Saupe N, Pfirrmann CW, et al. Ligaments and plicae of the elbow: normal MR imaging variability in 60 asymptomatic subjects. Radiology. 2010;257:185–194.
16 Dong Q, Jamadar DA, Robertson BL, et al. Posterior interosseous nerve of the elbow: normal appearances simulating entrapment. J Ultrasound Med. 2010;29:691–696.
17 De Maeseneer M, Jacobson JA, Jaovisidha S, et al. Elbow effusions: distribution of joint fluid with flexion and extension and imaging implications. Invest Radiol. 1998;33:117–125.
18 Ebrahim FS, Jacobson JA, Lin J, et al. Intraarticular osteoid osteoma: sonographic findings in three patients with radiographic, CT, and MR imaging correlation. AJR Am J Roentgenol. 2001;177:1391–1395.
19 Chew ML, Giuffre BM. Disorders of the distal biceps brachii tendon. Radiographics. 2005;25:1227–1237.
20 Miller TT, Adler RS. Sonography of tears of the distal biceps tendon. AJR Am J Roentgenol. 2000;175:1081–1086.
21 Skaf AY, Boutin RD, Dantas RW, et al. Bicipitoradial bursitis: MR imaging findings in eight patients and anatomic data from contrast material opacification of bursae followed by routine radiography and MR imaging in cadavers. Radiology. 1999;212:111–116.
22 Sofka CM, Adler RS. Sonography of cubital bursitis. AJR Am J Roentgenol. 2004;183:51–53.
23 Downey R, Jacobson JA, Fessell DP, et al. Sonography of partial-thickness tears of the distal triceps brachii tendon. J Ultrasound Med. 2011;30:1351–1356.
24 Jacobson JA, Miller BS, Morag Y. Golf and racquet sports injuries. Semin Musculoskelet Radiol. 2005;9:346–359.
25 Levin D, Nazarian LN, Miller TT, et al. Lateral epicondylitis of the elbow: US findings. Radiology. 2005;237:230–234.
26 Walz DM, Newman JS, Konin GP, et al. Epicondylitis: pathogenesis, imaging, and treatment. Radiographics. 2010;30:167–184.
27 Lee MH, Cha JG, Jin W, et al. Utility of sonographic measurement of the common tensor tendon in patients with lateral epicondylitis. AJR Am J Roentgenol. 2011;196:1363–1367.
28 Miller TT, Shapiro MA, Schultz E, et al. Comparison of sonography and MRI for diagnosing epicondylitis. J Clin Ultrasound. 2002;30:193–202.
29 Clarke AW, Ahmad M, Curtis M, et al. Lateral elbow tendinopathy: correlation of ultrasound findings with pain and functional disability. Am J Sports Med. 2010;38:1209–1214.
30 McShane JM, Nazarian LN, Harwood MI. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow. J Ultrasound Med. 2006;25:1281–1289.
31 McShane JM, Shah VN, Nazarian LN. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: is a corticosteroid necessary? J Ultrasound Med. 2008;27:1137–1144.
32 Connell D, Burke F, Coombes P, et al. Sonographic examination of lateral epicondylitis. AJR Am J Roentgenol. 2001;176:777–782.
33 Miller TT, Adler RS, Friedman L. Sonography of injury of the ulnar collateral ligament of the elbow—initial experience. Skeletal Radiol. 2004;33:386–391.
34 Jacobson JA, Fessell DP, Lobo Lda G, et al. Entrapment neuropathies I: upper limb (carpal tunnel excluded). Semin Musculoskelet Radiol. 2010;14:473–486.
35 Thoirs K, Williams MA, Phillips M. Ultrasonographic measurements of the ulnar nerve at the elbow: role of confounders. J Ultrasound Med. 2008;27:737–743.
36 O’Driscoll SW, Horii E, Carmichael SW, et al. The cubital tunnel and ulnar neuropathy. J Bone Joint Surg Br. 1991;73:613–617.
37 Okamoto M, Abe M, Shirai H, et al. Diagnostic ultrasonography of the ulnar nerve in cubital tunnel syndrome. J Hand Surg [Br]. 2000;25:499–502.
38 Husarik DB, Saupe N, Pfirrmann CW, et al. Elbow nerves: MR findings in 60 asymptomatic subjects—normal anatomy, variants, and pitfalls. Radiology. 2009;252:148–156.
39 Camerlinck M, Vanhoenacker FM, Kiekens G. Ultrasound demonstration of Struthers’ ligament. J Clin Ultrasound. 2010;38:499–502.
40 Hide IG, Grainger AJ, Naisby GP, et al. Sonographic findings in the anterior interosseous nerve syndrome. J Clin Ultrasound. 1999;27:459–464.
41 Bodner G, Buchberger W, Schocke M, et al. Radial nerve palsy associated with humeral shaft fracture: evaluation with US—initial experience. Radiology. 2001;219:811–816.
42 Chien AJ, Jamadar DA, Jacobson JA, et al. Sonography and MR imaging of posterior interosseous nerve syndrome with surgical correlation. AJR Am J Roentgenol. 2003;181:219–221.
43 Reynolds DL, Jr., Jacobson JA, Inampudi P, et al. Sonographic characteristics of peripheral nerve sheath tumors. AJR Am J Roentgenol. 2004;182:741–744.