CHAPTER 28 Elbow Dislocations
INTRODUCTION
The elbow is the second most commonly dislocated joint, after the shoulder, in adults. In the pediatric age group, it is the joint most commonly dislocated. Despite the prevalence of this injury, there are few analyses of series of this dislocation in the literature.7,16,19,25,29,36,46,52,68,76,96
MECHANISM OF INJURY
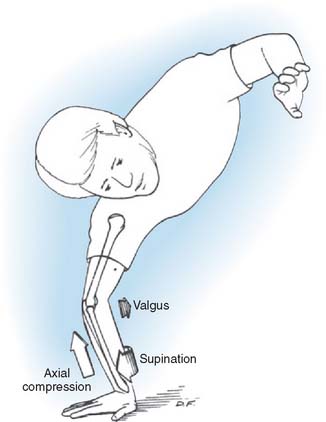
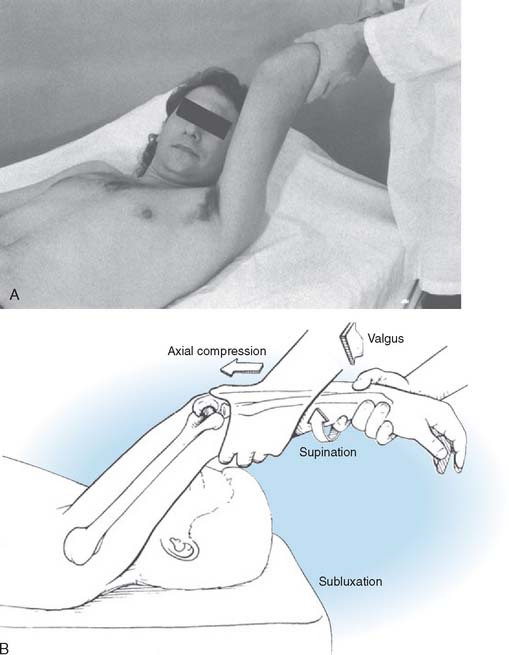
Although it used to be thought that dislocations occurred by hyperextension, it is now widely accepted that the mechanism of posterolateral rotatory posterior displacement of the elbow is responsible for most posterior dislocations resulting from falls on the outstretched hand. Motor vehicle accidents, direct trauma, and miscellaneous causes that account for the rest can have other mechanisms. The elbow experiences an axial compressive force during flexion as the body approaches the ground. As the body rotates internally on the elbow (forearm rotates externally on the trunk), a supination moment occurs at the elbow. A valgus moment results from the fact that the mechanical axis is lateral to the elbow (Fig. 28-1). This combination of valgus instability and supination with axial compression during flexion is precisely the mechanism that results in a posterolateral rotatory subluxation or dislocation of the elbow and can be reproduced clinically by the lateral pivot-shift test, which is described later.55 We have documented this exact mechanism in two patients whose dislocations were caught on video camera during wrestling matches.
Osborne and Cotterill64 first suggested a posterolateral rotational displacement as the mechanism of elbow dislocation. The radial collateral ligament and the lateral capsule are torn. They suggested a method of repair for recurrent dislocation based on this theory of mechanism, which involved imbrication of the lateral soft tissues. The method has been used with success.25
The forces acting on the joint, besides producing tensile forces that disrupt the ligamentous constraints, also produce substantial compressive and shear forces on the articular surfaces. Therefore, adjunctive fractures, such as those occurring in the radial head and neck or capitellum, are frequent.2,15 There is evidence from reports of dislocations treated by open means that chondral injuries to the capitellar and trochlear surfaces are probably much more common than was previously believed.11,23
In the child, late nucleation and closure of the physes alter the response to dislocation forces and certainly increase the difficulty of radiographic interpretation. This is covered separately in Chapter 16.
CLASSIFICATION
Acute elbow dislocations are classified as posterior, anterior, and divergent.
POSTERIOR DISLOCATIONS
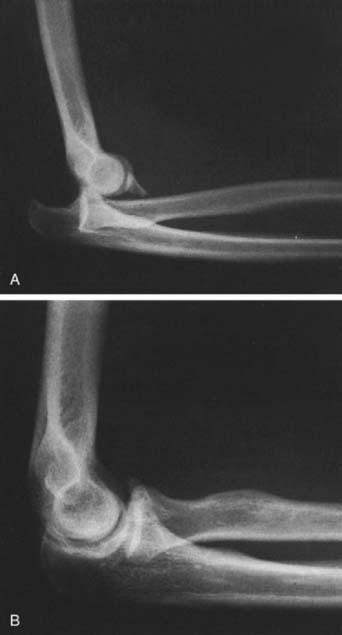
By far the most common dislocation occurs posteriorly (Fig. 28-2). Whether the forearm is medially or laterally displaced is irrelevant to the pathologic condition seen or the ultimate treatment.
ANTERIOR DISLOCATIONS
Anterior dislocations are extremely rare and are usually seen in younger individuals (Fig. 28-3).5,93 The forearm bones are displaced anterior to the distal humerus. The mechanism of injury is not well understood or proven, but there is a forward rebounding force that allows the olecranon to slide under the trochlea and the radial head to dislocate from the capitellum. In adults, the olecranon is usually fractured.
PATHOMECHANICS OF ELBOW INSTABILITY
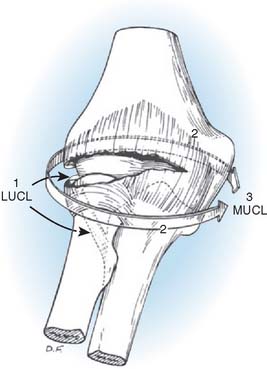
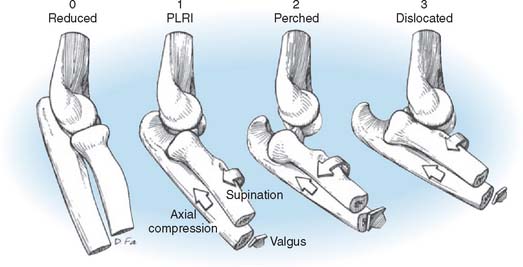
The pathoanatomy can be thought of as a circle of soft tissue disruption from lateral to medial in three stages (Figs. 28-4 and 28-5).
In stage 1, the ulnar part of the lateral collateral ligament is disrupted (the remainder of the lateral collateral ligament complex may be intact or disrupted). This results in posterolateral rotatory subluxation of the elbow, which reduces spontaneously.6,55,61
With further disruption anteriorly and posteriorly, the elbow is capable of an incomplete posterolateral dislocation (stage 2). The concave medial edge of the ulna rests on the trochlea in such a way that a lateral radiograph gives one the impression that the coronoid is perched on the trochlea.51
Stage 3 has two parts. In stage 3A, all the soft tissues are disrupted around to and including the posterior part of the medial collateral ligament, leaving the important anterior band intact. This permits posterior dislocation by the previously described posterolateral rotatory mechanism. The elbow pivots around on the intact anterior band of the medial collateral ligament. In stage 3B, the entire medial collateral complex is disrupted. Gross varus and valgus as well as rotatory instability is present following reduction, owing to the fact that all ligaments and capsules are disrupted. Surgical exploration has established that the anterior medial collateral ligament usually is disrupted by a complete dislocation of the elbow.7,9,11,13 These pathoanatomic stages correlate with clinical degrees of elbow instability.
Therefore, dislocation is the final of three sequential stages of elbow instability resulting from posterolateral ulnohumeral rotatory subluxation, with soft tissue disruption progressing from lateral to medial. In each stage, the pathoanatomy is correlated with the pattern and degree of instability. This has been confirmed in studies of cadaver elbows; 12 of 13 of the elbows could be dislocated posteriorly, with the anterior medial collateral ligament intact.21,56 In all 13 elbows, the coronoid could be perched on the trochlea after release of the lateral collateral ligament complex and the lateral half of the anterior capsule. Following reduction, the elbows were clinically stable to valgus stress.
This hypothesis explains the spectrum of instability, from posterolateral rotatory instability to perched dislocation to posterior dislocation without or with disruption of the anterior medial collateral ligament, which occurs with further posterior displacement. Such a posterolateral rotatory mechanism of dislocation is compatible with those suggested by Osborne and Cotterill,64 Roberts,76 and others.1,27,63 The injury patterns in the lateral collateral ligament have been documented.47 The overwhelming majority are by detachment of the lateral collateral ligament (LCL) complex from its origin on the lateral condyle. In most cases, the common extensor tendon is also disrupted.
ASSOCIATED INJURIES
Associated injuries with elbow dislocation are com-mon.28,32,62,77,80,95,97 Radial head and neck fractures occur in about 5% to 10% of cases secondary to compressive loading at the radiocapitellar joint. Avulsion of fragments from either the medial or the lateral epicondyles occurs in approximately 12% of cases, and fractures of the coronoid process occur in 10% of dislocations (see Fig. 28-2). It is essential to obtain stability following a fracture-dislocation because the treatment of persistent instability following fracture dislocations is unpredictable.65 One should be particularly careful to assess for fractures of the anteromedial facet of the coronoid (computed tomography [CT] scanning with three-dimensional surface rendering is best) because even an apparently minor fragment can be the only sign of a very serious injury with a grave prognosis due to posteromedial rotatory instability from a fracture subluxation.10,57,59,60
Displacement of the medial epicondyle in adolescents ranges from minimal to incarceration of the epicondyle within the joint (Fig. 28-6).36,69,79,88,90,98 The latter, if undetected, results in significant traumatic arthrosis (Fig. 28-7). Medial epicondylar fracture can predispose to late secondary dislocation.36 This may be explained by the loss of medial collateral ligament integrity.
Intra-articular fracture, as in the capitellum, occurs occasionally, but osteochondral injuries are probably much more common than standard radiographs would lead one to suspect.18
Injuries at other sites are also common with elbow dislocations, occurring in approximately 12% of the cases.36,52,94 Fractures of the distal radius and the ulnar styloid, perilunar dislocations, and shoulder injuries of the same extremity are the most common of these injuries, with multiple injuries of other areas secondary to severe trauma accounting for the rest.
Neurovascular injuries occur with elbow dislocations just as with any other joint injury.69 Neurovascular compromise can also develop following the dislocation rather than during it.
ASSESSMENT AND TREATMENT OF ACUTE ELBOW INSTABILITY
ASSESSMENT OF STABILITY
On the basis of the aforementioned observations and interpretations, it can be recommended that posterior elbow dislocations be reduced in supination to clear the coronoid under the trochlea, thereby minimizing additional trauma to the medial soft tissues that have not yet been disrupted. Following reduction, instability isbest assessed with the patient under general anesthesia, but this is not always practical. It is indicated when there is any clinical or radiographic evidence for suspicion of persistent instability. The elbow is examined for valgus, varus, and posterolateral rotatory instability (Fig. 28-8). Forced pronation prevents instability by using the intact medial soft tissues as a hinge or fulcrum, just as the periosteum is used for this purpose during the reduction of a supracondylar fracture in a child. Both valgus and varus testing are performed with the elbow in full extension and several degrees of flexion up to about 30 degrees to unlock the olecranon from the olecranon fossa. Posterolateral rotatory instability is diagnosed by the lateral pivot-shift test of the elbow, which is described in the next section on recurrent instability and is described in detail in Chapters 47 and 48. A positive test is manifested by a clunk that is heard and felt when the ulna and the radius reduce on the humerus. With severe soft tissue disruption, the elbow can sometimes remain dislocated even when flexed past 90 degrees. The patient should be followed with sequential radiographs for any radiographic signs of instability. The drop sign is a key radiographic warning sign of elbow instability, and it indicates severe soft tissue disruption both laterally and medially and a propensity for persistent or recurrent instability.8
DELAYED TREATMENT
Delayed treatment for neglected dislocations41,85 is discussed in detail in Chapter 30. Open reduction may be indicated for a problem that has been neglected for more than 10 days when firm but gentle manipulation fails.35 Rarely, closed reduction is prevented by interposition of the annular ligament or a collateral ligament.24,66,83 A laterally placed Kocher incison is preferred, especially if there are concomitant intra-articular fractures or loose fragments at the radiocapitellar joint.12 Buttonholing of the radial head through the capsule may be recognized readily with this approach.24 Proximal radioulnar translocation, a rare entity, has been reported and is treated by open reduction.54
Long-standing chronic dislocations should be reduced open, and the joint should be freed of scar tissue and reconstructed as described in the sections on collateral ligament reconstruction. Open reduction is usually used to retrieve an incarcerated medial epicondyle from within the ulnotrochlear joint,69 a situation that usually occurs in the pediatric patient. If this is necessary, the ulnar nerve should be identified beneath the deep fascia posterior to the medial intermuscular septum for protection during the procedure. The medial collateral ligament attached to the epicondyle also may have been avulsed from the proximal area of the medial humeral condyle. It should be reapproximated and tacked into position with sutures as necessary to maintain its position and ensure better medial stability. If there has been obvious ulnar nerve injury or clinical neurapraxia, anterior translocation may be considered simultaneously before reattaching the medial epicondyle. In many instances, moderate displacement of the epicondyle may be present without significant neurovascular problems. Accurate anatomic reduction and fixation are, however, desirable.
POSTREDUCTION CARE AND REHABILITATION
Treatment recommendations following acute soft tissue injuries correspond to the stages outlined in the spectrum of instability. Initially, the elbow is placed in a padded dressing with a posterior plaster splint in full pronation at 90 degrees of flexion, after assessment for stability. Persistent or increasing pain or loss or diminution of the pulse requires wide release of the dressing anteriorly, inspection of the antecubital space, and a check of the neuromuscular status for signs of impending ischemia. Valgus stability following reduction is present in stages 1 to 3A when the forearm is fully pronated. These injuries are permitted unlimited flexion and extension. Protection may be added by the use of a hinged brace, which is applied with the forearm in full pronation. If the elbow feels stable in any position of forearm rotation, a brace is not necessary. Such stability is usually due to the dynamic stabilizing effects of the muscles crossing the elbow joint. In stage 3B, the elbow is unstable in extension, and a hinged brace (usually in pronation, but occasionally in neutral rotation) is applied with an extension block incorporated to prevent extension beyond the point of instability. This is gradually extended during the healing phase. A total of 3 to 6 weeks of protected motion is adequate. If by 6 to 8 weeks full motion has not been attained, special patient-adjusted static flexion and extension splints are used to quickly regain the remaining motion.
Based on comprehensive research on elbow kinematics, King and associates31 have shown that that LCL-deficient elbow should be rehabilitated by performing flexion/extension with the forearm pronated. The addition of active muscle contraction further stabilizes the joint. This is readily achieved by overhead exercises in the supine position. Forearm rotation is performed actively and only in the flexed position.
ACUTE LIGAMENT REPAIR
The indication for surgery, acute ligament repair, or reconstruction is instability that does not permit early protected motion in a hinged brace or with a removable splint. This usually occurs only when there are associated fractures. In such cases, the ligaments may have been avulsed and can be repaired directly to the bone with heavy sutures. If they are torn and cannot be repaired, they can be reconstructed using the techniques described in the chapters on injuries to the medial and lateral collateral ligaments. In some cases, the tissue can be repaired but not strongly enough to stabilize the joint. The alternative to ligament repair is the application of a hinged external fixator,59,73,87 which is particularly appealing in patients with bilateral elbow dislocations, a rather rare condition.33
RESULTS
Melhoff and associates48 reviewed the long-term sequelae of simple elbow dislocations in 52 patients. Half of the patients were asymptomatic; one third had some loss of motion, mainly extension. This related to the duration of postreduction immobilization. Those immobilized for longer than 3 weeks were likely to develop contractures, whereas those immobilized for shorter periods were less likely.
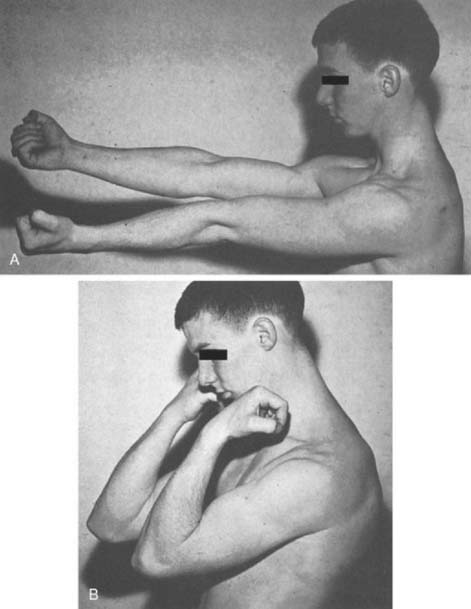
Uncomplicated dislocations generally have satisfactory results. Excellent results with full range of motion, normal strength, absent pain, and good stability may be expected in half of simple dislocations (Fig. 28-9). Good results with a loss of no more than 15 degrees of either flexion or extension, minimal discomfort, and normal stability are anticipated in an additional one third of cases. Fair or poor results generally are associated with complications (discussed later) and may be expected in 15% of dislocations. Fair or poor results generally are seen in the more severe original injuries.36
Recurrent instability has not been commonly reported, although symptoms have been noted in up to 35% of patients.31,42,48,86 It has been widely taught that the medial collateral ligament heals predictably following elbow dislocations and that instability is uncommon.11,50,78,98 However, these opinions have been formulated largely in the absence of objective assessments of elbow stability that have been tested and proven reliable. In addition, most reports precede the generalized awareness of posterolateral rotatory instability or how to diagnose it. Egandal and colleagues17 are to be commended for detailed follow-up analysis of 50 patients with posterolateral dislocations of the elbow treated by closed reduction and conservative treatment. A valgus radiographic stress x-ray study was performed on every patient, and in fact, this revealed that half (24 of 50) of the patients had clear radiographic evidence of valgus instability.
COMPLICATIONS
NEUROVASCULAR
Neurovascular problems have already been discussed in the section on treatment, but they deserve additional emphasis. Stretching and distortion of the anterior structures may result in spasm, intimal damage, thrombosis, or rupture of the brachial artery.14,20,32,36,39,43,44,53,71,81,84,89,92 Neurologic problems occur in approximately 20% of dislocations. The ulnar nerve is the most susceptible major nerve.36 Symptoms vary from transient paresthesias in the ulnar distribution to a rare permanent ulnar palsy. Median nerve symptoms are less common and also range from a transient to a complete palsy.
Combined median-ulnar nerve injuries usually are associated with severe injuries that frequently involve the brachial artery as well. Vascular injuries usually result in significant long-term disabilities35 (see Complications). Because dislocation often is also disruptive of collateral circulation, the forearm is at risk in this instance. Ischemic myositis, impaired vascularity, or later claudication may result (see Chapter 16).
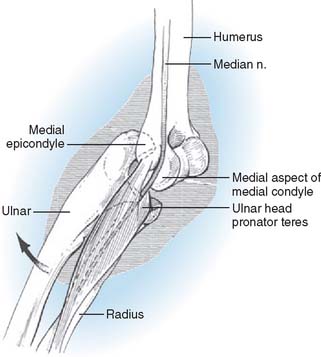
Median nerve symptoms are apt to be associated with arterial injury because of the close proximity of nerve and artery in their course between the brachialis and the pronator teres. Stretch injuries to the nerve occur at the time of dislocation.70 These injuries must be differentiated from secondary compressive injuries, which may occur with increased intracompartmental pressure in the flexor space or intra-articular entrapment. The latter may be suspected if median paresthesias occur shortly after reduction, if there is widening of the medial joint space, or if reduction has an “incomplete feel.”78 This complication is more common in children(Fig. 28-10). There have been several explanations of the mechanism of intra-articular entrapment of the median nerve. The nerve may be displaced posteriorly through a space created by avulsion of the medial epicondyle or the common flexor origin.82 Tension of the nerve across the margin of the epicondylar flare may “notch” the bone to produce a late radiographic sign known as Matev’s sign, after the investigator who described it.45 The nerve also has been seen to slip through the space between the medial condyle and the collateral ligament and then become entrapped between the trochlea and the semilunar notch on reduction.67
The ulnar nerve is the nerve most frequently injured in elbow dislocations, primarily because of valgus stretching.35,79 The induration, hypertrophy, and ossification present within the cubital tunnel may compress the nerve and diminish gliding, causing persistent symptoms. For this reason, anterior translocation may be considered if progressive resolution of paresthesias and paresis is not apparent.
OSTEOCHONDRAL INJURIES
Loose flecks of bone within the joint following reduction usually represent inclusion of an avulsed fragment of the medial epicondyle or a fragment of the articular surface.23 In the latter case, the fragment is usually significantly larger than the radiographic appearance suggests, owing to the radiolucent chondral layer. Such fragments should be removed or replaced as indicated by the findings. If the joint is explored, dèbridement, irrigation, and soft tissue replacement should be accomplished as soon as possible.12
HETEROTOPIC BONE FORMATION
Heterotopic bone formation occurs at three primary locations following dislocation. Ossification in the lateral and medial collateral ligaments occurs frequently and occasionally may be sufficient to cause marked functional impairment. Obviously it does, however, affect the suppleness of the ligaments. Ossification also occurs in the anterior capsule above the coronoid process (Fig. 28-11). Occasionally, marked heterotopic ossification occurs in the brachialis muscle, seriously impairing flexion and extension of the elbow.34,38,75,91 Excision isdelayed until the reactive bone mass is mature, usually at 1 year. Excision may be performed between 4 to 6 months after injury. Excision at that time usually allows substantial improvement in motion after excitation of the osteoblastic response has subsided.
1 Abe M., Ishizu T., Morikawa J. Posterolateral rotatory instability of the elbow after posttraumatic cubitus varus. J. Shoulder Elbow Surg. 1997;6:405.
2 Adler B., Shaftan G.W. Radial head fractures: is excision necessary? J. Trauma. 1964;4:115.
3 Altuntas A.O., Balakumar J., Howells R.J., Graham H.K. Posterior divergent dislocation of the elbow in children and adolescents: A report of three cases and review of the literature. J. Pediatr. Orthop. 2005;25:317.
4 Basanagoudar P., Pace A., Ross D. Paediatric transverse divergent dislocation of the elbow. Acta Orthop. Belg. 2006;72(3):359-361.
5 Blatz D.J. Anterior dislocation of the elbow. Findings in a case of Ehlers-Danlos syndrome. Orthop. Rev. 1981;10:129.
6 Cohen M., Hastings H. Rotatory instability of the elbow. J. Bone Joint Surg. 1997;79A:225.
7 Conn J., Wade P. Injuries of the elbow: a ten year review. J. Trauma. 1961;1:248.
8 Coonrad R.W., Roush T.F., Major N.M., Basamania C.J. The drop sign, a radiographic warning sign of elbow instability. J. Shoulder Elbow Surg. 2005;14:312.
9 DeLee J.C. Transverse divergent dislocation of the elbow in a child. J. Bone Joint Surg. 1981;63A:322.
10 Doornberg J.N., Ring D.C. Fracture of the anteromedial facet of the coronoid process. J. Bone Joint Surg. 2006;88:2216.
11 Dryer R., Buckwalter J., Sprague B. Treatment of chronic elbow instability. Clin. Orthop. Relat. Res. 1974;100:254.
12 Durig M., Muller W., Ruedi T.P., Gauer E.F. The operative treatment of elbow dislocation in the adult. J. Bone Joint Surg. 1979;61A:23.
13 Edward G.E., Rostrup O. Radial head prosthesis in the management of radial head fractures. Can. J. Surg. 1960;3:153.
14 Eliason E.L., Brown R.B. Posterior dislocation at the elbow with rupture of the radial and ulnar arteries. Ann. Surg. 1937;106:1111.
15 Eppright R.H., Wilkins K.E.. Fractures and dislocations of the elbow. Rockwood C.A., Green D.P., editors. Fractures, Vol I. Philadelphia: J. B. Lippincott Co., 1975.
16 Exarchou E.J. Lateral dislocation of the elbow. Acta Orthop. Scand. 1977;48:151.
17 Eygendaal D., Verdegaal S.H., Obermann W.R., van Vugt A.B., Poll R.G., Rozing P.M. Posterolateral dislocation of the elbow joint. Relationship to medial instability. J. Bone Joint Surg. 2000;82:555.
18 Faber K.J., King G.J.W. Posterior capitellum impression fracture: a case report associated with posterolateral rotatory instability of the elbow. J. Shoulder Elbow Surg. 1998;7:157.
19 Fazzi U.G., Rymaszewski L.A. Recurrent dislocation of the elbow in identical twins. J. Shoulder Elbow Surg. 1996;5:401.
20 Galbraith K.A., McCullough C.J. Acute nerve injury as a complication of closed fractures or dislocations of the elbow. Injury. 1979;11:159.
21 Garland D.E., O’Hollaren R.M. Fractures and dislocations about the elbow in the head-injured adult. Clin. Orthop. Relat. Res. 1982;168:38.
22 Graham T.J., Jacobson P.A., Bamberger H.B., Infante A.. Contemporary management of complex elbow disorders. Am. J. Orthop, 1998;Suppl.:33.
23 Grant I.R., Miller J.H. Osteochondral fracture of the trochlea associated with fracture-dislocation of the elbow. Injury. 1976;6:257.
24 Greiss M., Messias R. Irradiable postolateral elbow dislocation: a case report. Acta Orthop Scand. 1987;58:42.
25 Heusner L. Ein Fall von habitueller Luxation des Ellenbogen. In Festschrift zur Feier des funfzigjahrigen Jubilamus des Vereins der Aertze des Regierungsberzirks Dusseldorf. Weisbaden; 1894.
26 Hotchkiss R.N. Fractures and dislocations of the elbow. In: Rockwood C.A., Green D.P., Bucholz R.W., Heckman J.D., editors. Fractures in Adults. Philadelphia: Lippincott-Raven; 1996:980.
27 Johanson O. Capsular and ligamentous injuries of the elbow joint: A clinical and arthrographic study. Acta Chir. Scand. 1962;287(Suppl):1.
28 Johnston G.W. Followup of 100 cases of fracture of the head of the radius. Ulster Med. J. 1962;31:51.
29 Josefsson P.O., Johnell O., Wendeberg B. Ligamentous injuries in dislocations of the elbow joint. Clin. Orthop. Relat. Res. 1987;221:221.
30 Kazuki K., Miyamoto T., Ohzono K. A case of traumatic divergent fracture-dislocation of the elbow combined with Essex-Lopresti lesion in an adult. J. Shoulder Elbow Surg. 2005;14:224.
31 King T. Recurrent dislocation of the elbow. J. Bone Joint Surg. 1953;35B:50.
32 Kini M.G. Dislocation of the elbow and its complications. J. Bone Joint Surg. 1940;22:107.
33 Koslowsky T.C., Mader K., Siedek M., Pennig D. Treatment of bilateral elbow dislocation suing external fixation with motion capacity: A report of two cases. J. Orthop. Trauma. 2006;20:499.
34 Krishan M. Myositis ossificans traumatic of the elbow. Int. Surg. 1972;57:475.
35 Krishnamoorthy S., Bose K., Wong K.P. Treatment of old unreduced dislocation of the elbow. Injury. 1976;8:39.
36 Linscheid R.L., Wheeler D.K. Elbow dislocations. J. A. M. A. 1965;194:1171.
37 Lippe C.N., Williams D.P. Combined posterior and convergent elbow dislocations in an adult. A case report and review of the literature. J. Bone Joint Surg. 2005;87:1597.
38 Loomis L.K. Reduction and aftertreatment of posterior dislocation of the elbow. With special attention to the brachialis muscle and myositis ossificans. Am. J. Surg. 1944;63:56.
39 Louis D., Ricciardi J., Spengler D. Arterial injury: a complication of posterior elbow dislocation. J. Bone Joint Surg. 1979;56A:1631.
40 MacSween W.A. Transposition of radius and ulna associated with dislocation of the elbow in a child. Injury. 1979;10:314.
41 Mahaisavariya B., Laupattarakasem W. Neglected dislocation of the elbow. Clin. Orthop. Relat. Res. 2005;431:21.
42 Mantle J.A. Recurrent posterior dislocation of the elbow. J. Bone Joint Surg. 1966;48B:590.
43 Marcheix B., Chaufour X., Avel J., Hollington L., Mansat P., Barret A., Bossavy J. Transection of the brachial artery after closed posterior elbow dislocation. J. Vasc. Surg. 2005;42:1230.
44 Martin D.J., Fazzi U.G., Leach W.J. Brachial artery transection associated with closed and open dislocation of the elbow. Eur. J. Emerg. Med. 2005;12:30.
45 Matev I. A radiological sign of entrapment of the median nerve in the elbow joint after posterior dislocation: a report of two cases. J. Bone Joint Surg. 1976;58B:353.
46 Maylahn D.J., Fahey J.J. Fractures of the elbow in children: review of three hundred consecutive cases. J. A. M. A. 1958;166:220.
47 McKee M.D., Schemitsch E.H., Sala M.J., O’Driscoll S.W. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J. Shoulder Elbow Surg. 2003;12:391.
48 Melhoff T.L., Noble P.C., Bennett J.B., Tullos H.S. Simple dislocation of the elbow in the adult. J. Bone Joint Surg. 1988;70A:244.
49 Morrey B.F. Complex instability of the elbow. J. Bone Joint Surg. 1997;79A:460.
50 Morrey B.F., An K.N. Articular ligamentous contributions to the stability of the elbow joint. Am. J. Sports Med. 1983;11:315.
51 Morrey B.F.. Fractures and dislocations of the elbow. Gustillo R., editor. Preparation, Fractures and Dislocations, Vol. I. Year Book Publishers, Chicago, 1993;387-499.
52 Neviaser J.S., Wickstrom J. Dislocation of the elbow: a retrospective study of 115 patients. South. Med. J. 1977;70:172.
53 Noonan K.J., Blair W.F. Chronic median-nerve entrapment after posterior fracture-dislocation of the elbow. J. Bone Joint Surg. 1995;77A:1572.
54 Nybonde O.E.T., Karlsson G. Luxation of the elbow complicated by proximal radioulnar translocation. Acta Radiol. 1990;31:146.
55 O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J. Bone Joint Surg. 1991;73A:440.
56 O’Driscoll S.W. Classification and evaluation of recurrent instability of the elbow. Clin. Orthop. Relat. Res. 2000;370:34.
57 O’Driscoll S.W. Coronoid fractures. In: Norris T.R., editor. Orthopaedic knowledge update: Shoulder and elbow 2. 2nd ed. Rosemont American Academy of Orthopaedic Surgeons; 2002:379.
58 O’Driscoll S.W. Instability. Hand Clin. 1994;10:405.
59 O’Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: Pearls and pitfalls. Instr. Course Lect. 2003;52:113.
60 O’Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: pearls and pitfalls. Instruct. Course Lect. 2005;1:465.
61 O’Driscoll S.W., Morrey B.F., Korinek S., An K.N. Elbow subluxation and dislocation: A spectrum of instability. Clin. Orthop. Relat. Res. 1992;280:186.
62 O’Hara J.P., Morrey B.F., Johnson E.W., Johnson K.A. Dislocations and fractured dislocations of the elbow. Fracture Conference. Minn. Med. 1975;58:697.
63 Olsen B.S., Sojbjerg J.O., Nielsen K.K., Vaesel M.T., Dalstra M., Sneppen O. Posterolateral elbow joint instability. The basic kinematics. J. Shoulder Elbow Surg. 1998;7:19.
64 Osborne G., Cotterill P. Recurrent dislocation of the elbow. J. Bone Joint Surg. 1966;48B:340.
65 Papandrea R.F., Morrey B.F., O’Driscoll S.W. Reconstruction for persistent instability of the elbow after coronoid fracture-dislocation. J. Shoulder Elbow Surg. 1997;16:68.
66 Pawlowski R.F., Palumbo F.C., Callahan J.J. Irreducible posterolateral elbow dislocation: report of a rare case. J. Trauma. 1970;10:260.
67 Pritchard D.J., Linscheid R.L., Svein H.J. Intraarticular median nerve entrapment with dislocation of the elbow. Clin. Orthop. Relat. Res. 1973;90:100.
68 Protzmann R.R. Dislocation of the elbow joint. J. Bone Joint Surg. 1978;60:539.
69 Purser D.W. Dislocation of the elbow and inclusion of the medial epicondyle in the adult. J. Bone Joint Surg. 1954;36B:247.
70 Rana N.A., Kenwright J., Taylor R.G., Rushworth G. Complete lesion of the median nerve associated with dislocation of the elbow joint. Acta Orthop. Scand. 1974;45:365.
71 Rasool M.N. Dislocations of the elbow in children. J. Bone Joint Surg. 2004;86B:1050.
72 Regan W., Morrey B.F. Fractures of the coronoid process of the ulna. J. Bone Joint Surg. 1989;71A:1348.
73 Ring D., Jupiter J.B. Compass hinge fixator for acute and chronic instability of the elbow. Oper. Orthop. Traumatol. 2005;17:143.
74 Ring D., Jupiter J.B. Fracture-dislocation of the elbow. J. Bone Joint Surg. 1997;80:566.
75 Roberts J.B., Pankratz D.G. The surgical treatment of heterotopic ossification at the elbow following long-term coma. J. Bone Joint Surg. 1979;61A:760.
76 Roberts P.H. Dislocation of the elbow. Br. J. Surg. 1969;56:806.
77 Scharplatz D., Allgower M. Fracture dislocations of the elbow. Injury. 1975;7:143.
78 Schwab G.H., Bennett J.B., Woods G.W., Tullos H.S. Biomechanics of elbow instability: The role of the medial collateral ligament. Clin. Orthop. Relat. Res. 1980;146:42.
79 Scharma R.K., Covelle N.A. An unusual ulnar nerve injury associated with dislocation of the elbow. Injury. 1976;8:145.
80 Smith D.N., Lee J.R. The radiological diagnosis of posttraumatic effusion of the elbow joint and its clinical significance: the “displaced fat pad” sign. Injury. 1978;10:115.
81 Spear H.C., Janes J.M. Rupture of the brachial artery accompanying dislocation of the elbow or supracondylar fracture. J. Bone Joint Surg. 1951;33A:889.
82 Strange F.G., St. Clair. Entrapment of the median nerve after dislocation of the elbow. J. Bone Joint Surg. 1982;64B:224.
83 Strong M.L. Irreducible posterolateral dislocation of the elbow without fracture. Report of two cases. Contemp. Orthop. 1985;11:69.
84 Sturm J.T., Rothenberger D.A., Strate R.G. Brachial artery disruption following closed elbow dislocation. Trauma. 1978;18:364.
85 Subasi M. Neglected dislocation of the elbow. Clin. Orthop. Relat. Res. 2005;439:292. author reply 292
86 Symeonides P.P., Paschaloglou C., Stavrou Z., Pangalides T. Recurrent dislocation of the elbow. J. Bone Joint Surg. 1975;57A:1084.
87 Tan V., Daluiski A., Capo J., Hotchkiss R. Hinged elbow external fixators: indications and uses. J. Am. Acad. Orthop. Surg. 2005;13:503.
88 Tayob A.A., Shively R.A. Bilateral elbow dislocations with intraarticular displacement of the medial epicondyles. J. Trauma. 1980;20:332.
89 Trias A., Comeau Y. Recurrent dislocation of the elbow in children. Clin. Orthop. Relat. Res. 1974;100:74.
90 Thomas T.T. A contribution to the mechanism of fractures and dislocations in the elbow region. Ann. Surg. 1929;89:108.
91 Thompson H., Garcia A. Myositis ossificans: aftermath of elbow injuries. Clin. Orthop. Relat. Res. 1967;50:129.
92 Van Rossum J., Buruma O.J.J., Kamphuisen H.A.C., Onolee G.J. Tennis elbow-a radial tunnel syndrome? J. Bone Joint Surg. 1978;60B:197.
93 Venkatram N., Wurm V., Houshian S. Anterior dislocation of the ulnar-humeral joint in a so-called “pulled elbow.”. Emerg. Med. J.. 2006;23:e37.
94 Walker R.H., Tanner J.B. Fracture of the proximal shaft of the radius associated with posterior dislocation of the elbow. Clin. Orthop. Relat. Res. 1982;168:35.
95 Wheeler D.K., Linscheid R.L. Fracture dislocations of the elbow. Clin. Orthop. Relat. Res. 1967;50:95.
96 Wiley J.J., Pegington J., Horwich J.P. Traumatic dislocation of the radius at the elbow. J. Bone Joint Surg. 1974;56B:501.
97 Wilson P.D. Fractures and dislocations in the region of the elbow. Surg. Gynecol. Obstet. 1933;56:335.
98 Woods W., Tullos H. Elbow instability and medial epicondyle fractures. Am. J. Sports Med. 1977;5:23.