Elbow and Forearm
Neuroanatomy Overview: Paths of the Musculocutaneous, Radial, Median, and Ulnar Nerves throughout the Elbow, Forearm, Wrist, and Hand
The elbow and forearm complex consists of three bones and four joints (Figure 6-1). The humero-ulnar and humeroradial joints form the elbow. The motions of flexion and extension of the elbow provide a means to adjust the overall functional length of the upper limb. This mechanism is used for many important activities, such as feeding, reaching, throwing, and personal hygiene.
OSTEOLOGY
The anterior and posterior surfaces of the mid-to-distal humerus provide proximal attachments for the brachialis and the medial head of the triceps brachii (Figures 6-2 and 6-3). The distal end of the shaft of the humerus terminates medially as the trochlea and the medial epicondyle, and laterally as the capitulum and lateral epicondyle. The trochlea resembles a rounded, empty spool of thread. The medial and lateral borders of the trochlea flare slightly to form medial and lateral lips. The medial lip is prominent and extends farther distally than the adjacent lateral lip. Midway between the medial and lateral lips is the trochlear groove, which, when one looks from posterior to anterior, spirals slightly toward the medial direction (Figure 6-4). The coronoid fossa is located just proximal to the anterior aspect of the trochlea (see Figure 6-2).
The medial epicondyle of the humerus projects medially from the trochlea (see Figures 6-2 and 6-4). This prominent and easily palpable structure serves as the proximal attachment of the medial collateral ligament of the elbow as well as most forearm pronator and wrist flexor muscles.
Ulna
The ulna has a very thick proximal end with distinct processes (Figures 6-5 and 6-6). The olecranon process forms the large, blunt, proximal tip of the ulna, making up the “point” of the elbow (Figure 6-7). The roughened posterior surface of the olecranon process accepts the insertion of the triceps brachii. The coronoid process projects sharply from the anterior body of the proximal ulna.
The radial notch of the ulna is an articular depression just lateral to the inferior aspect of the trochlear notch (see Figures 6-5 and 6-7). Extending distally and slightly dorsally from the radial notch is the supinator crest, marking the attachments for part of the lateral collateral ligament complex and the supinator muscle. The tuberosity of the ulna is a roughened impression just distal to the coronoid process, formed by the attachment of the brachialis muscle (see Figure 6-5).
The ulnar head is located at the distal end of the ulna (Figure 6-8). Most of the rounded ulnar head is covered with articular cartilage. The pointed styloid process (from the Greek root stylos, pillar) projects distally from the posterior-medial region of the extreme distal ulna.
Radius
In the fully supinated position, the radius lies parallel and lateral to the ulna (see Figures 6-5 and 6-6). The proximal end of the radius is small and therefore constitutes a relatively small structural component of the elbow. Its distal end, however, is enlarged, forming a major part of the wrist joint.
The radial head is a disclike structure located at the extreme proximal end of the radius. Articular cartilage covers about 280 degrees of the rim of the radial head.44 The rim of the radial head contacts the radial notch of the ulna, forming the proximal radio-ulnar joint. Immediately inferior to the radial head is the constricted radial neck (see Figure 6-5).
The distal end of the radius articulates with carpal bones to form the radiocarpal joint at the wrist (see Figure 6-8). The ulnar notch of the distal radius accepts the ulnar head at the distal radio-ulnar joint. The prominent styloid process projects from the lateral surface of the distal radius, extending approximately 1 cm farther distal than the ulnar styloid process.
ARTHROLOGY
GENERAL FEATURES OF THE HUMERO-ULNAR AND HUMERORADIAL JOINTS
Early anatomists classified the elbow as a ginglymus or hinged joint owing to its predominant uniplanar motion of flexion and extension. The term modified hinge joint is actually more appropriate because the ulna experiences a slight amount of axial rotation (i.e., rotation around its own longitudinal axis) and side-to-side motion as it flexes and extends.48 Bioengineers must account for these relatively small “extra-sagittal” accessory motions in the design of elbow joint prostheses. Without attention to this detail, the prosthetic implants are more likely to loosen prematurely.13,29
Normal “Valgus Angle” of the Elbow: Elbow flexion and extension occur around a relatively stationary medial-lateral axis of rotation, passing through the vicinity of the lateral epicondyle (Figure 6-9, A).71 From medial to lateral, the axis courses slightly superiorly owing in part to the distal prolongation of the medial lip of the trochlea. This asymmetry in the trochlea causes the ulna to deviate laterally relative to the humerus. The natural frontal plane angle made by the extended elbow is referred to as normal cubitus valgus. (The term “carrying angle” is often used, reflecting the fact that the valgus angle tends to keep carried objects away from the side of the thigh during walking.) Paraskevas and co-workers reported an average cubitus valgus angle in healthy persons of about 13 degrees, with a standard deviation close to 6 degrees.58 On average, women had a greater valgus angulation than men by about 2 degrees. Two studies using a large sample of normal subjects have shown that, regardless of gender, valgus angle is greater on the dominant arm.58,85
Occasionally the extended elbow may show an excessive cubitus valgus that exceeds about 20 or 25 degrees (see Figure 6-9, B). In contrast, the forearm may less commonly show a cubitus varus (or “gunstock”) deformity, where the forearm is deviated toward the midline (see Figure 6-9, C). The terms valgus and varus are derived from the Latin turned outward (abducted) and turned inward (adducted), respectively.
A marked varus or valgus deformity may result from trauma, such as a severe fracture through the “growth plate” of the distal humerus in children. Excessive cubitus valgus may overstretch and damage the ulnar nerve as it crosses medial to the elbow.11
PERIARTICULAR CONNECTIVE TISSUE
The articular capsule of the elbow encloses the humero-ulnar joint, the humeroradial joint, and the proximal radio-ulnar joint (Figure 6-10). The articular capsule surrounding these joints is thin and reinforced anteriorly by oblique bands of fibrous tissue. A synovial membrane lines the internal surface of the capsule (Figure 6-11).
The articular capsule of the elbow is strengthened by collateral ligaments. These ligaments provide an important source of stability to the elbow joint. Motions that increase the tension in the ligaments are listed in Table 6-1. The medial collateral ligament consists of anterior, posterior, and transverse fiber bundles (Figure 6-12). The anterior fibers are the strongest and stiffest fibers of the medial collateral ligament.63 As such, these fibers provide the most significant resistance against a valgus (abduction) force to the elbow. The anterior fibers arise from the anterior part of the medial epicondyle and insert on the medial part of the coronoid process of the ulna.18 Because the anterior fibers span both sides of the axis of rotation, at least some fibers are taut throughout sagittal plane movement. The anterior fibers therefore provide articular stability throughout the entire range of motion.10
The posterior fibers of the medial collateral ligament are less defined than the anterior fibers and are essentially thickenings of the posterior-medial capsule. As depicted in Figure 6-12, the posterior fibers attach on the posterior part of the medial epicondyle and insert on the medial margin of the olecranon process. The posterior fibers resist a valgus force, as well as become taut in the extremes of elbow flexion.63 A third and poorly developed set of transverse fibers cross from the olecranon to the coronoid process of the ulna. Because these fibers originate and insert on the same bone, they do not provide significant articular stability.
In addition to the medial collateral ligaments, the proximal fibers of the wrist flexor and pronator group of muscles also resist excessive valgus-producing strain at the elbow, most notably by the flexor carpi ulnaris. For this reason, these muscles are referred to as dynamic medial stabilizers of the elbow.38
The medial collateral ligament is susceptible to injury when the fully extended elbow is violently forced into excessive valgus, often from a fall onto an outstretched arm and hand (Figure 6-13).12 The ligamentous injury may be associated with a fracture within the humeroradial joint or anywhere along the length of the radius—the forearm bone that accepts 80% of the compression force applied through the wrist. A severe valgus-producing force may also injure the ulnar nerve or proximal attachments of the pronator–wrist flexor muscles. The anterior capsule may also be injured if the joint is excessively hyperextended. The medial collateral ligament is also susceptible to injury from repetitive, valgus-producing forces to the elbow in non–weight-bearing activities, such as pitching a baseball and spiking a volleyball.65,83
The lateral collateral ligament complex of the elbow is more variable in form than the medial collateral ligament (Figure 6-14). The ligamentous complex originates on the lateral epicondyle and immediately splits into two fiber bundles. One fiber bundle, traditionally known as the radial collateral ligament, fans out to blend with the annular ligament. A second fiber bundle, called the lateral (ulnar) collateral ligament, attaches distally to the supinator crest of the ulna. These fibers become taut during full flexion.63 By attaching to the ulna, the lateral (ulnar) collateral ligament and the anterior fibers of the medial collateral ligament function as collateral “guy wires” to the elbow, providing medial-lateral stability to the ulna during sagittal plane motion.
The lateral collateral ligament complex and the posterior-lateral aspect of the capsule are primary stabilizers against a varus-producing force.56 Often after a single traumatic sporting event, rupture of this ligament system can cause not only increased varus (“adduction”) of the elbow, but also posterior-lateral rotary instability. This instability is expressed as excessive external rotation of the forearm with subsequent subluxation of both the humero-ulnar and humeroradial joints.19,54
The ligaments around the elbow are endowed with mechanoreceptors consisting of Golgi organs, Ruffini terminals, Pacinian corpuscles, and free nerve endings.59 These receptors may supply important information to the nervous system for augmenting proprioception and detecting safe limits of passive tension in the structures around the elbow.
As all joints do, the elbow joint has an intracapsular air pressure. This pressure, which is determined by the ratio of the volume of air to the volume of space, is lowest at about 80 degrees of flexion.24 This joint position is often considered the “position of comfort” for persons with joint inflammation and swelling. Maintaining a swollen elbow in a flexed position may improve comfort but may predispose the person to an elbow flexion contracture (from the Latin root contractura, to draw together).
KINEMATICS
Functional Considerations of Flexion and Extension: Elbow flexion performs several important physiologic functions, such as pulling, lifting, feeding, and grooming.77 The inability to actively bring the hand to the mouth for feeding, for example, significantly limits the level of functional independence. Persons with a spinal cord injury above the C5 nerve root may experience this profound functional impairment because of paralysis of elbow flexor muscles.
The maximal range of passive motion generally available to the elbow is from 5 degrees beyond neutral (0 degree) extension through 145 degrees of flexion (Figure 6-16). Research indicates, however, that several common activities of daily living use a more limited “functional arc” of motion, usually between 30 and 130 degrees of flexion.47 Unlike in lower extremity joints, such as the knee, the loss of the extremes of motion at the elbow usually results in only minimal functional impairment.
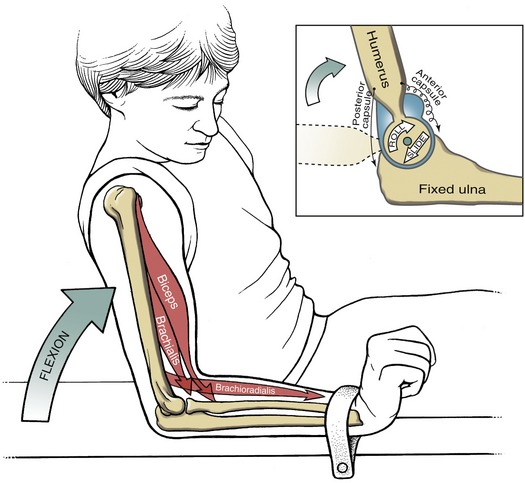
Arthrokinematics at the Humero-Ulnar Joint: The humero-ulnar joint is the articulation between the concave trochlear notch of the ulna and the convex trochlea of the humerus (Figure 6-17). Hyaline cartilage covers about 300 degrees of articular surface on the trochlea, compared with only 180 degrees on the trochlear notch. The natural congruency and shape of this joint limits motion primarily within the sagittal plane.
In order for the humero-ulnar joint to be fully extended, sufficient extensibility is required in the dermis anterior to the elbow, flexor muscles, anterior capsule, and anterior fibers of the medial collateral ligament (Figure 6-18, A). Full extension also requires that the prominent tip of the olecranon process become wedged into the olecranon fossa. Excessive ectopic (from the Greek root ecto, outside, + topos, place) bone formation around the olecranon fossa can therefore limit full extension. Normally, once in extension, the healthy humero-ulnar joint is stabilized primarily by articular congruency and also by the increased tension in the stretched connective tissues.
During flexion at the humero-ulnar joint, the concave surface of the trochlear notch rolls and slides on the convex trochlea (see Figure 6-18, B). Full elbow flexion requires elongation of the posterior capsule, extensor muscles, ulnar nerve,68,73 and certain portions of the collateral ligaments, especially the posterior fibers of the medial collateral ligament. Stretching of the ulnar nerve from prolonged or repetitive elbow flexion activities can lead to neuropathy. A common surgical treatment for this condition is to transfer the ulnar nerve anterior to the medial epicondyle, thereby reducing the tension in the nerve during flexion.43
Arthrokinematics at the Humeroradial Joint: The humeroradial joint is an articulation between the cuplike fovea of the radial head and the reciprocally shaped rounded capitulum. The arthrokinematics of flexion and extension consist of the fovea of the radius rolling and sliding across the convexity of the capitulum (Figure 6-19). During active flexion, the radial fovea is pulled firmly against the capitulum by contracting muscles.46
Compared with the humero-ulnar joint, the humeroradial joint provides minimal sagittal plane stability to the elbow. The humeroradial joint does, however, provide about 50% of the resistance against a valgus-producing force to the elbow.49
Structure and Function of the Interosseous Membrane
The radius and ulna are bound together by the interosseous membrane of the forearm (Figure 6-20). Although several accessory fibers have been described, the more prominent central bands are directed distal-medially from the radius, intersecting the shaft of the ulna at about 20 degrees.69 The central bands are nearly twice the thickness of other fibers and have an ultimate tensile strength similar to that of the patellar tendon of the knee.61 A few separate sparse and poorly defined bands flow perpendicular to the central bands of the interosseous membrane. One of these bands, the oblique cord, runs from the lateral side of the tuberosity of the ulna to just distal to the radial tuberosity. Another unnamed band is located at the extreme distal end of the interosseous membrane.
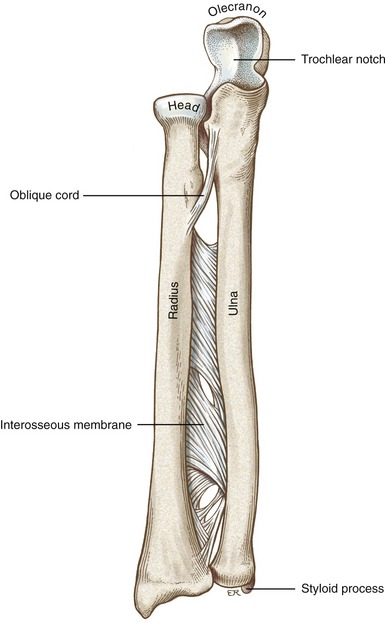
FIGURE 6-20. An anterior view of the right forearm, highlighting the components of the interosseous membrane.
The primary functions of the interosseous membrane are to bind the radius to the ulna, serve as a stable attachment site for several extrinsic muscles of the hand, and provide a mechanism for transmitting force proximally through the upper limb. As illustrated in Figure 6-21, about 80% of the compression force that crosses the wrist is directed through the radiocarpal joint. (This fact accounts, in part, for the relatively high likelihood of fracturing the radius from a fall on an outstretched hand.) The remaining 20% of the force crosses the medial side of the wrist, through the soft tissues located within the “ulnocarpal space.”57 Because of the fiber direction of the central bands of the interosseous membrane, part of the proximal directed force through the radius is transferred across the membrane to the ulna.60 This mechanism allows a significant portion of the compression force that naturally acts on the radius to cross the elbow via the humero-ulnar joint.46 In this way, both the humero-ulnar and humeroradial joints more equally “share” the compression forces that cross the elbow, thereby reducing each individual joint’s long-term wear and tear.
Most elbow flexors, and essentially all primary supinator and pronator muscles, have their distal attachment on the radius. As a consequence, contraction of these muscles pulls the radius proximally against the capitulum of the humerus, especially when the elbow is near full extension. Biomechanical analysis indicates that the resulting compression force at the humeroradial joint reaches three to four times body weight during maximal-effort activities.2 Based on the mechanism described in Figure 6-21, the interosseous membrane helps shunt some of the muscular-produced compression forces from the radius to the ulna. In this way the interosseous membrane helps protect the humeroradial joint from large myogenic compression forces. Tears within the interosseous membrane can cause a measurable proximal migration of the radius due to activation of the regional muscles, leading to increased loading and possible degeneration at the humeroradial joint.32,55 In cases where the head of the radius has been surgically removed because of trauma, the proximal migration is typically pronounced.26 Over time, this proximal “drift” of the radius can cause bony asymmetry in the wrist or distal radio-ulnar joint, causing significant pain and loss of function.16
The predominant fiber direction of the interosseous membrane is not aligned to resist distally applied forces on the radius. For example, holding a heavy suitcase with the elbow extended causes a distracting force almost entirely through the radius (Figure 6-22). The distal pull on the radius slackens, rather than tenses, most of the interosseous membrane, thereby placing larger demands on other tissues, such as the oblique cord and annular ligament, to accept the weight of the load. Contraction of the brachioradialis or other muscles normally involved with grasp can assist with holding the radius and load firmly against the capitulum of the humerus. A deep aching in the forearm in persons who carry heavy loads for extended periods may be from fatigue in these muscles. Supporting loads through the forearm at shoulder level, for example, like a waiter carrying a tray of food, directs the weight proximally through the radius, so that the interosseous membrane can assist with dispersing the load more evenly through the forearm.
Joints of the Forearm
GENERAL FEATURES OF THE PROXIMAL AND DISTAL RADIO-ULNAR JOINTS
The radius and ulna are bound together by the interosseous membrane and the proximal and distal radio-ulnar joints. This set of joints, situated at either end of the forearm, allows the forearm to rotate into pronation and supination. Forearm supination places the palm up, or supine, and pronation places the palm down, or prone. This forearm rotation occurs around an axis of rotation that extends from the radial head through the ulnar head—an axis that intersects and connects both radio-ulnar joints (Figure 6-23).31 Pronation and supination provide a mechanism that allows independent “rotation” of the hand without an obligatory rotation of the ulna or humerus.
In the anatomic position the forearm is fully supinated when the ulna and radius lie parallel to each other (see Figure 6-23, A). During pronation the distal segment of the forearm complex (i.e., the radius and hand) rotates and crosses over an essentially fixed ulna (see Figure 6-23, B). The ulna, through its firm attachment to the humerus at the humero-ulnar joint, remains nearly stationary during an isolated pronation and supination movement. A stable humero-ulnar joint provides an essential rigid link that the radius, wrist, and hand can pivot on. Movement of the humero-ulnar joint during pronation and supination has been described, but only as a very slight counter-rotation of the ulna relative to the radius.35 It certainly is possible for the ulna to rotate freely during pronation and supination, but only if the humerus is also freely rotating at the glenohumeral joint.
JOINT STRUCTURE AND PERIARTICULAR CONNECTIVE TISSUE
Proximal Radio-Ulnar Joint: The proximal radio-ulnar joint, the humero-ulnar joint, and the humeroradial joint all share one articular capsule. Within this capsule the radial head is held against the proximal ulna by a fibro-osseous ring. This ring is formed by the radial notch of the ulna and the annular ligament (Figure 6-24, A). About 75% of the ring is formed by the annular ligament and 25% by the radial notch of the ulna.
The annular (from the Latin annulus, ring) ligament is a thick circular band of connective tissue attaching to the ulna on either side of the radial notch (see Figure 6-24, B). The ligament fits snugly around the radial head, holding the proximal radius against the ulna. The internal circumference of the annular ligament is lined with cartilage to reduce the friction against the radial head during pronation and supination. The external surface of the ligament receives attachments from the elbow capsule, the radial collateral ligament, and the supinator muscle.8 The quadrate ligament is a thin, fibrous ligament that arises just below the radial notch of the ulna and attaches to the medial surface of the neck of the radius (see Figure 6-24, B). This function of the poorly defined ligament is not clear, although it may support the capsule of the proximal radio-ulnar joint throughout forearm rotation.70
Distal Radio-Ulnar Joint: The distal radio-ulnar joint consists of the convex head of the ulna resting on the shallow concavity formed by the ulnar notch on the radius and the proximal surface of an articular disc (Figure 6-26). This important joint firmly connects the distal ends of the radius and ulna. The shallow and often irregularly shaped ulnar notch of the radius affords only marginal osseous containment to the joint. The stability of the distal radio-ulnar joint is furnished through activation of muscles,28 plus an elaborate set of local connective tissues.
The articular disc at the distal radio-ulnar joint is also known as the triangular fibrocartilage, indicating its shape and predominant tissue type. As depicted in Figure 6-26, A, the lateral side of the disc attaches along the entire rim of the ulnar notch of the radius. The main body of the disc fans out horizontally into a triangular shape, with its apex attaching medially into the depression on the ulnar head and adjacent styloid process. The anterior and posterior edges of the disc are continuous with the palmar (anterior) and dorsal (posterior) radio-ulnar joint capsular ligaments (see Figure 6-26). The proximal surface of the disc, along with the attached capsular ligaments, holds the head of the ulna snugly against the ulnar notch of the radius during pronation and supination.51,81 Experimentally cutting the capsular ligaments in fresh cadaver specimens causes marked increases in multidirectional translations of the distal radius in all positions of supination and pronation.80
Introduction to the Triangular Fibrocartilage Complex: The articular disc is part of a larger set of connective tissue known as the triangular fibrocartilage complex—typically abbreviated TFCC.25,34,67 The TFCC occupies most of the “ulnocarpal space” between the head of the ulna and the ulnar side of the wrist. Several adjacent connective tissues are typically included with this complex, such as the capsular ligaments of the distal radio-ulnar joint and ulnar collateral ligament (see Figure 6-26, B). The TFCC is the primary stabilizer of the distal radio-ulnar joint.80
Other structures that provide stability to the distal radio-ulnar joint are the pronator quadratus, the tendon of the extensor carpi ulnaris, and the more distal fibers of the interosseous membrane.22,82 Tears or disruptions of the TFCC, especially the disc,39 may cause complete dislocation or generalized instability of the distal radio-ulnar joint, making pronation and supination motions, as well as motions of the wrist, painful and difficult to perform. (The triangular fibrocartilage complex is anatomically and functionally associated with other structures of the wrist, and hence is discussed further in Chapter 7.)
KINEMATICS
Functional Considerations of Pronation and Supination: Forearm supination occurs during many activities that involve rotating the palmar surface of the hand toward the face, such as feeding, washing, and shaving. Forearm pronation, in contrast, is used to place the palmar surface of the hand down on an object, such as grasping a coin or pushing up from a chair.
The neutral or zero reference position of forearm rotation is the “thumb-up” position, midway between complete pronation and supination. On average the forearm rotates through about 75 degrees of pronation and 85 degrees of supination (Figure 6-27, A). As shown in Figure 6-27, B, several activities of daily living require only about 100 degrees of forearm rotation—from about 50 degrees of pronation through 50 degrees of supination.47 As in the elbow joint, a 100-degree functional arc exists—an arc that does not include the terminal ranges of motion. Persons who lack the last 30 degrees of complete forearm rotation, for example, are still capable of performing many routine activities of daily living. To some extent, reduced pronation and supination can be compensated for by internally and externally rotating the shoulder, respectively.
Arthrokinematics at the Proximal and Distal Radio-Ulnar Joints: Pronation and supination require simultaneous movements at both the proximal and distal radio-ulnar joints. As will be explained, pronation and supination also require movement at the adjacent humeroradial joint. A restriction at any one of these joints would restrict the overall movement of forearm rotation. Restrictions in passive range of motion can occur from tightness in muscle and/or connective tissues. Table 6-2 lists a sample of these tissues.
Supination: Supination at the proximal radio-ulnar joint occurs as a rotation of the radial head within the fibro-osseous ring formed by the annular ligament and radial notch of the ulna (Figure 6-28, bottom box). The tight constraint of the radial head by the fibro-osseous ring prohibits standard roll-and-slide arthrokinematics.5
Supination at the distal radio-ulnar joint occurs as the concave ulnar notch of the radius rolls and slides in similar directions on the head of the ulna (see Figure 6-28, top box).5 During supination the proximal surface of the articular disc remains in contact with the ulnar head. At the end range of supination, the palmar capsular ligament is stretched to its maximal length, creating a stiffness that naturally stabilizes the joint.17,67,78 This stiffness provides increased stability at a position of reduced joint congruency. At the extremes of both supination and pronation, only about 10% of the surface of the ulnar notch of the radius is in direct contact with the ulnar head.20 This is in sharp contrast to the 60% contact area in the neutral (midposition) of pronation and supination.
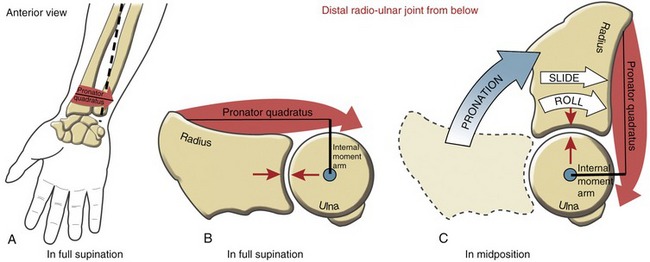
Pronation: The arthrokinematics of pronation at the proximal and distal radio-ulnar joints occur by mechanisms similar to those described for supination (Figure 6-29). As depicted in the top inset of Figure 6-29, full pronation elongates and thereby increases the tension in the dorsal capsular ligament at the distal radio-ulnar joint.17 Full pronation slackens the palmar capsular ligament to about 70% of its original length.67 In addition, full pronation exposes the articular surface of the ulnar head (see the asterisk in Figure 6-29, top inset), making it readily palpable.
Humeroradial Joint: a “Shared” Joint between the Elbow and the Forearm: During pronation and supination, the proximal end of the radius rotates at both the proximal radio-ulnar and humeroradial joints. Both joints have distinctive arthrokinematics during pronation and supination. The arthrokinematics at the proximal radio-ulnar joint were explained previously. The arthrokinematics at the humeroradial joint involve a spin of the fovea of the radial head against the rounded capitulum of the humerus. Figure 6-30 shows the arthrokinematics during active pronation under the power of the pronator teres muscle. Contraction of this muscle—as well as others inserting into the radius—can generate significant compression forces on the humeroradial joint, especially when the joint is near extension. This compression force is associated with a proximal migration of the radius, which is greater during active pronation than during supination.46 Because the interosseous membrane as a whole is relatively slackened in pronation,32,42 it is likely less able to resist the proximal pull on the radius imparted by pronator muscle contraction. The natural proximal migration of the radius and associated increased joint compression of the humeroradial joint during active pronation has been referred to as the “screw home” mechanism of the elbow.45
Based on location, the humeroradial joint is mechanically linked to the kinematics of both the elbow and forearm. Any motion performed at the elbow or forearm requires movement at this joint. A postmortem study of 32 cadavers (age at death ranging from 70 to 95 years) showed more frequent and severe degeneration across the humeroradial than the humero-ulnar joint.1 The increased wear on the lateral compartment of the elbow can be explained in part by the frequent and complex arthrokinematics (spin and roll-and-slide), combined with varying amounts of muscular-produced compression force. Pain or limited motion at the humeroradial joint can significantly disrupt the functional mobility of the entire distal upper extremity.
Pronation and Supination with the Radius and Hand Held Fixed: Up to this point in this chapter, the kinematics of pronation and supination have been described as a rotation of the radius and hand relative to a stationary, or fixed, humerus and ulna (see Figures 6-28 and 6-29). The forearm rotation occurs when the upper limb is in a non–weight-bearing position. Pronation and supination are next described when the upper limb is in a weight-bearing position. In this case the humerus and ulna rotate relative to a stationary, or fixed, radius and hand.
Consider a person bearing weight through an upper extremity with elbow and wrist extended (Figure 6-31, A). The person’s right glenohumeral joint is held partially internally rotated. The ulna and radius are positioned parallel in full supination. (The “rod” placed through the epicondyles of the humerus helps with the orientation of this position.) With the radius and hand held firmly fixed with the ground, pronation of the forearm occurs by an external rotation of the humerus and ulna (see Figure 6-31, B). Because of the naturally tight structural fit of the humero-ulnar joint, rotation of the humerus is transferred, nearly degree for degree, to the rotating ulna. Moving back to the fully supinated position involves internal rotation of the humerus and ulna relative to the fixed radius and hand. It is important to note that these pronation and supination kinematics are essentially an expression of active external and internal rotation of the glenohumeral joint, respectively.
Figure 6-31, B depicts an interesting muscle “force-couple” used to pronate the forearm from the weight-bearing position. The infraspinatus rotates the humerus relative to a fixed scapula, whereas the pronator quadratus rotates the ulna relative to a fixed radius. Both muscles, acting at either end of the upper extremity, produce forces that contribute to a pronation torque at the forearm. From a therapeutic perspective, an understanding of the muscular mechanics of pronation and supination from this weight-bearing perspective provides additional exercise strategies for strengthening or stretching muscles of the forearm and shoulder.
The far right side of Figure 6-31, B illustrates the arthrokinematics at the radio-ulnar joints during pronation while the radius and hand are stationary. At the proximal radio-ulnar joint the annular ligament and radial notch of the ulna rotate around the fixed radial head (see Figure 6-31, B, top inset). Although not depicted, the capitulum of the humerus is spinning relative to the fovea of the fixed radius. At the distal radio-ulnar joint the head of the ulna rotates around the fixed ulnar notch of the radius (see Figure 6-31, bottom inset). Table 6-3 summarizes and compares the arthrokinematics at the radio-ulnar joints for both weight-bearing and non–weight-bearing conditions of the upper limb.
TABLE 6-3.
Arthrokinematics of Pronation and Supination
| Weight-Bearing (Radius and Hand Fixed) | Non–Weight-Bearing (Radius and Hand Free to Rotate) | |
| Proximal radio-ulnar joint | Annular ligament and radial notch of the ulna rotate around a fixed radial head. | Radial head rotates within a ring formed by the annular ligament and the radial notch of the ulna. |
| Distal radio-ulnar joint | Convex ulnar head rolls and slides in opposite directions on the concave ulnar notch of the radius. | Concavity of the ulnar notch of the radius rolls and slides in similar directions on the convex ulna head. |
MUSCLE AND JOINT INTERACTION
The musculocutaneous nerve, formed from the C5-C7 spinal nerve roots, innervates the biceps brachii, coracobrachialis, and brachialis muscles (Figure 6-32, A). As its name implies, the musculocutaneous nerve innervates muscle then continues distally as a sensory nerve to the skin, supplying the lateral forearm.
The radial nerve, formed from the C5-T1 spinal nerve roots, is a direct continuation of the posterior cord of the brachial plexus (see Figure 6-32, B). This large nerve courses within the radial groove of the humerus to innervate the triceps and the anconeus. The radial nerve then emerges laterally at the distal humerus to innervate muscles that attach on or near the lateral epicondyle. Proximal to the elbow, the radial nerve innervates the brachioradialis, a small lateral part of the brachialis, and the extensor carpi radialis longus. Distal to the elbow, the radial nerve consists of superficial and deep branches. The superficial branch is purely sensory, supplying the posterior-lateral aspects of the distal forearm, including the dorsal “web space” of the hand. The deep branch contains the remaining motor fibers of the radial nerve. This motor branch supplies the extensor carpi radialis brevis and the supinator muscle. After piercing through an intramuscular tunnel in the supinator muscle, the final section of the radial nerve courses toward the posterior side of the forearm. This terminal branch, often referred to as the posterior interosseous nerve, supplies the extensor carpi ulnaris and several muscles of the forearm, which function in extension of the digits.
The median nerve, formed from the C6-T1 spinal nerve roots, courses toward the elbow to innervate most muscles attaching on or near the medial epicondyle of the humerus. These muscles include the wrist flexors and forearm pronators (pronator teres, flexor carpi radialis, and palmaris longus) and the deeper flexor digitorum superficialis (see Figure 6-32, C). A deep branch of the median nerve, often referred to as the anterior interosseous nerve, innervates the deep muscles of the forearm: the lateral half of the flexor digitorum profundus, the flexor pollicis longus, and the pronator quadratus. The terminal part of the median nerve continues distally to cross the wrist through the carpal tunnel, under the cover of the transverse carpal ligament. The nerve then innervates several of the intrinsic muscles of the thumb and the lateral fingers. The median nerve provides a rich source of sensation to the lateral palm, palmar surface of the thumb, and lateral two and one-half fingers (see Figure 6-32, C, inset on median nerve sensory distribution).
The ulnar nerve, formed from the spinal nerve roots C8-T1, is formed by a direct branch of the medial cord of the brachial plexus (see Figure 6-32, D). After passing posterior to the medial epicondyle, the ulnar nerve innervates the flexor carpi ulnaris and the medial half of the flexor digitorum profundus. The nerve then crosses the wrist external to the carpal tunnel and supplies motor innervation to many of the intrinsic muscles of the hand. The ulnar nerve supplies sensation to the skin on the ulnar side of the hand, including the medial side of the ring finger and entire small finger.
Innervation of Muscles and Joints of the Elbow and Forearm
INNERVATION OF MUSCLE
Table 6-4 summarizes the peripheral nerve and primary spinal nerve root innervation to the muscles of the elbow and forearm. This table was derived primarily from Appendix II, Part A, which lists the primary nerve roots that innervate the muscles of the upper extremity. Appendix II, Parts B to D include additional reference items to help guide the clinical assessment of the functional status of the C5-T1 spinal nerve roots and several major peripheral nerves of the upper limb.
SENSORY INNERVATION OF JOINTS
Humero-Ulnar and Humeroradial Joints: The humero-ulnar and humeroradial joints and the surrounding connective tissues receive their sensory innervation from the C6-C8 spinal nerve roots.33 Fibers from these afferent nerve roots are carried primarily by the musculocutaneous and radial nerves and by the ulnar and median nerves.70
Proximal and Distal Radio-Ulnar Joints: The proximal radio-ulnar joint and surrounding elbow capsule receive sensory innervation from fibers within the median nerve that enter the C6-C7 spinal nerve roots.70 The distal radio-ulnar joint receives most of its sensory innervation from fibers of the ulnar nerve that enter the C8 nerve root.33
Function of the Elbow Muscles
Muscles acting primarily on the wrist also cross the elbow joint. For this reason, many of the wrist muscles have a potential to flex or extend the elbow.3 This potential is relatively minimal and is not discussed further. The proximal and distal attachments and nerve supply of the muscles of the elbow and forearm are listed in Appendix II, Part E.
ELBOW FLEXORS
The biceps brachii, brachialis, brachioradialis, and pronator teres are primary elbow flexors. Each of these muscles produces a force that passes anterior to the medial-lateral axis of rotation at the elbow. Structural and related biomechanical variables of these muscles are included in Table 6-5.
TABLE 6-5.
Structural and Related Biomechanical Variables of the Primary Elbow Flexor Muscles*
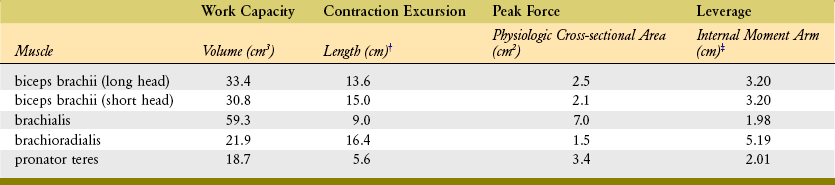
*Structural properties are indicated by italics. The related biomechanical variables are indicated in bold.
†Muscle belly length measured at 70 degrees of flexion.
‡Internal moment arm measured with elbow flexed to 100 degrees and forearm fully supinated.
Data from An KN, Hui FC, Morrey BF, et al: Muscles across the elbow joint: a biomechanical analysis, J Biomech 14:659, 1981.
Individual Muscle Action of the Elbow Flexors: The biceps brachii attaches proximally on the scapula and distally on the radial tuberosity on the radius (Figure 6-33). Secondary distal attachments include the deep fascia of the forearm through an aponeurotic sheet known as the fibrous lacertus.
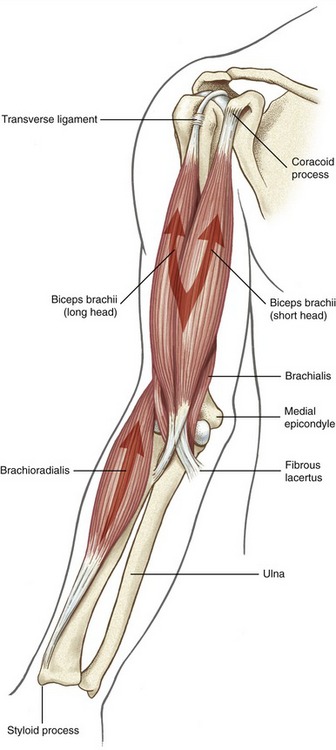
FIGURE 6-33. Anterior view of the right biceps brachii and brachioradialis muscles. The brachialis is deep to the biceps.
The biceps produces its maximal electromyographic (EMG) signal when performing both flexion and supination simultaneously,6 such as when bringing a spoon to the mouth. The biceps exhibits relatively low levels of EMG activity when flexion is performed with the forearm deliberately held in pronation. This lack of muscle activation can be verified by self-palpation.
The brachialis lies deep to the biceps, originating on the anterior humerus and attaching distally on the extreme proximal ulna (Figure 6-34). This muscle’s sole function is to flex the elbow. As shown in Table 6-5, the brachialis has an average physiologic cross-section of 7 cm2, the largest of any muscle crossing the elbow. For comparison, the long head of the biceps has a cross-sectional area of only 2.5 cm2. Based on its large physiologic cross-section, the brachialis is expected to generate the greatest force of any muscle crossing the elbow.
The brachioradialis is the longest of all elbow muscles, attaching proximally on the lateral supracondylar ridge of the humerus and distally near the styloid process of the radius (see Figure 6-33). Maximal shortening of the brachioradialis causes full elbow flexion and rotation of the forearm to the near neutral position. EMG studies suggest that the brachioradialis is a primary elbow flexor, especially during rapid movements against a high resistance.6,15,21
The brachioradialis muscle can be readily palpated on the anterior-lateral aspect of the forearm. Resisted elbow flexion, from a position of about 90 degrees of flexion and neutral forearm rotation, causes the muscle to stand out or “bowstring” sharply across the elbow (Figure 6-35). The bowstringing of this muscle increases its flexion moment arm to a length that exceeds that of the other flexors (see Table 6-5).
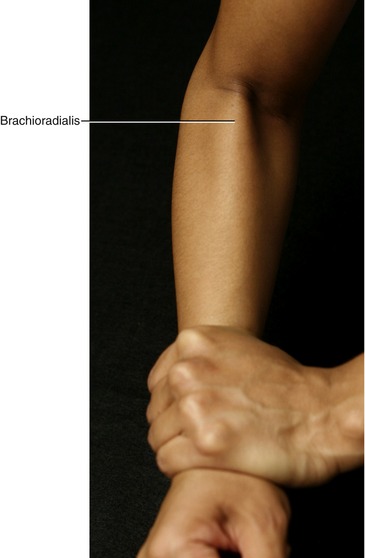
FIGURE 6-35. The right brachioradialis muscle is shown “bowstringing” over the elbow during a maximal-effort isometric activation.
The anatomy of the pronator teres is described under the section on pronator muscles (see Figure 6-48). As a point of comparison, the pronator teres has a similar flexor moment arm as the brachialis, but only about 50% of its physiologic cross-sectional area (see Table 6-5).
Torque Generated by the Elbow Flexor Muscles: Figure 6-36 shows the line of force of three primary elbow flexors. The strength of the flexion torque varies considerably based on age,23 gender, weightlifting experience,76 speed of muscle contraction, and position of the joints across the upper extremity.84 According to a study reported by Gallagher and colleagues,23 the dominant side produced significantly higher levels of flexion torque, work, and power. No significant differences, however, were found for elbow extension and forearm pronation and supination.
Maximal-effort flexion torques of 725 kg-cm for men and 336 kg-cm for women have been reported for healthy middle-aged persons (Table 6-6).4 These data show that flexion torques are about 70% greater than extensor torques. In the knee, however, which is functionally analogous to the elbow in the lower extremity, the strength differential favors the extensor muscles, by an approximately similar magnitude. This difference likely reflects the greater relative functional demands typically placed on the flexors of the elbow as compared with the flexors of the knee.
TABLE 6-6.
Average Maximal Isometric Internal Torques across the Elbow and Forearm
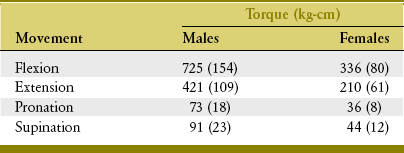
Data from Askew LJ, An KN, Morrey BF, Chao EY: Isometric elbow strength in normal individuals, Clin Orthop Relat Res 222:261, 1987.
Elbow flexor torques produced with the forearm supinated are about 20% to 25% greater than those produced with the forearm fully pronated.62 This difference is due primarily to the increased flexor moment arm of the biceps50 and the brachioradialis when the forearm is in or approaches supination.
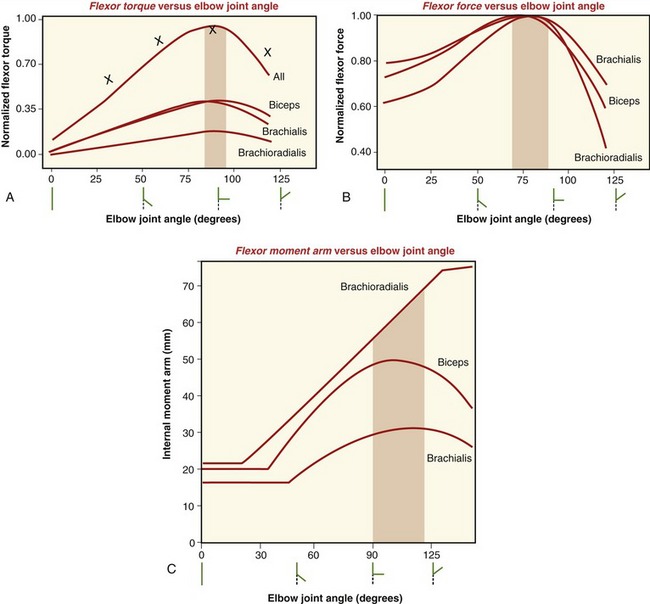
Biomechanical and physiologic data can be used to predict the maximal flexion torque produced by the three primary elbow flexor muscles across a full range of motion (Figure 6-37, A). The predicted maximal torque for all muscles occurs at about 90 degrees of flexion, which agrees in general with actual torque measurements in healthy persons.62,76 The two primary factors responsible for the overall shape of the maximal torque-angle curve of the elbow flexors are (1) the muscle’s maximal flexion force potential and (2) the internal moment arm length. The data plotted in Figure 6-37, B predict that the maximal force of all muscles occurs at a muscle length that corresponds to about 80 degrees of flexion. The data plotted in Figure 6-37, C predict that the average maximal moment arm of all three muscles occurs at about 100 degrees of flexion. At about this joint angle, the insertion of the biceps tendon to the radius is near 90 degrees (see Figure 6-36). This mechanical condition maximizes the internal moment arm of a muscle and thereby maximizes the conversion of a muscle force to a joint torque. It is interesting that the data presented in Figure 6-37, B and C predict peak torques across generally similar joint angles. The natural ability to produce maximal elbow flexion torque at about 90 degrees of flexion functionally corresponds to the angle at which the greatest external torque (due to gravity) typically acts against the forearm, at least while standing or in an upright sitting position.
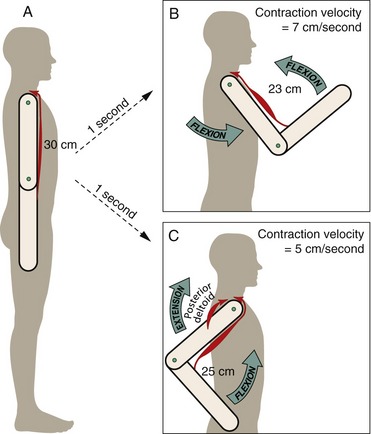
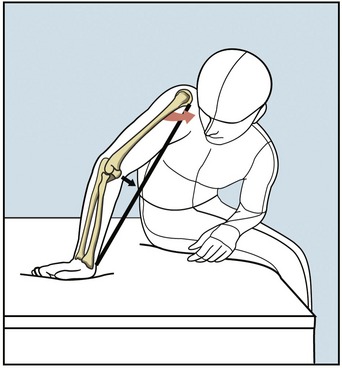
Polyarticular Biceps Brachii: a Physiologic Advantage of Combining Elbow Flexion with Shoulder Extension: The biceps is a polyarticular muscle that produces force across multiple joints. As subsequently described, combining active elbow flexion with shoulder extension is a natural and effective way for producing biceps-generated elbow flexor torque. The following hypothetic example proposes a physiologic mechanism that favors this natural movement combination.
For the sake of discussion, assume that at rest in the anatomic position the biceps is about 30 cm long (Figure 6-38, A). The biceps then shortens to about 23 cm after an active motion that combines 90 degrees of elbow flexion with 45 degrees of shoulder flexion (see Figure 6-38, B). If the motion took 1 second to perform, the muscle experiences an average contraction velocity of 7 cm/sec. In contrast, consider a more natural and effective activation pattern involving both the biceps and posterior deltoid to produce elbow flexion with shoulder extension (see Figure 6-38, C). During an activity such as pulling a heavy load up toward the side, for example, the activated biceps produces elbow flexion while at the same time it is elongated across the extending shoulder. By extending the shoulder, the contracting posterior deltoid, in effect, reduces the net shortening of the biceps. Based on the example in Figure 6-38, C, combining elbow flexion with shoulder extension reduces the average contraction velocity of the biceps to 5 cm/sec. This is 2 cm/sec slower than combining elbow flexion with shoulder flexion. As described in Chapter 3, the maximal force output of a muscle is greater when its contraction velocity is closer to zero, or isometric.
The simple model described here illustrates one of many examples in which a one-joint muscle, such as the posterior deltoid, can enhance the force potential of another polyarticular muscle. In the example, the posterior deltoid serves as a powerful shoulder extensor for a vigorous pulling motion. In addition, the posterior deltoid assists in controlling the optimal contraction velocity and operational length of the biceps throughout the elbow flexion motion. The posterior deltoid, especially during high-power activities, is a very important synergist to the elbow flexors. Consider the consequences of performing the lift described in Figure 6-38, C with total paralysis of the posterior deltoid.
ELBOW EXTENSORS
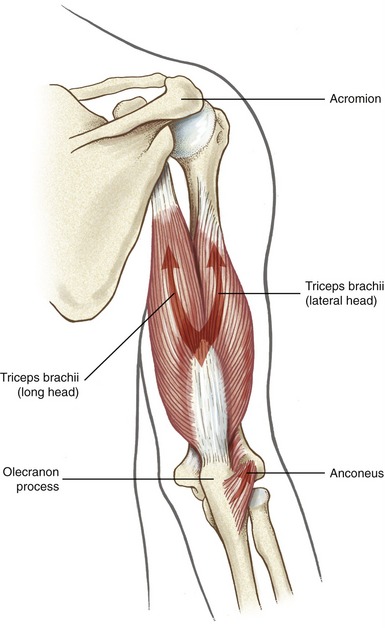
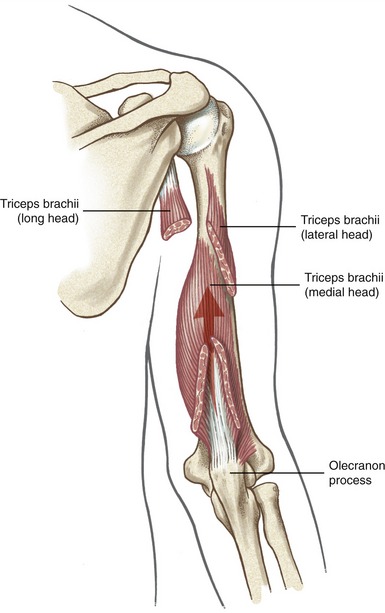
Muscular Components: The primary elbow extensors are the triceps brachii and the anconeus (Figures 6-39 and 6-40). The triceps converge to a common tendon attaching to the olecranon process of the ulna.
The triceps brachii has three heads: long, lateral, and medial. The long head has its proximal attachment on the infraglenoid tubercle of the scapula, thereby allowing the muscle to extend and adduct the shoulder. The long head has an extensive volume, exceeding all other muscles of the elbow (Table 6-7).
TABLE 6-7.
Structural and Related Biomechanical Variables of the Primary Elbow Extensor Muscles*
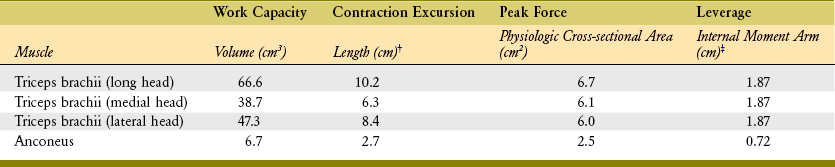
*Structural properties are indicated by italics. The related biomechanical variables are indicated in bold.
†Muscle belly length measured at 70 degrees of flexion.
‡Internal moment arm measured with elbow flexed to 100 degrees.
Data from An KN, Hui FC, Morrey BF, Chao EY: Muscles across the elbow joint: a biomechanical analysis, J Biomech 14:659, 1981.
The lateral and medial heads of the triceps muscle have their proximal attachments on the humerus, on either side and along the radial groove. The medial head has an extensive proximal attachment on the posterior side of the humerus, occupying a location relatively similar to that of the brachialis on the bone’s anterior side. Some of the more distal fibers of the medial head attach directly into the posterior capsule of the elbow. These fibers may be analogous to the articularis genu muscle at the knee, with a similar function in drawing the capsule taut during extension.70 Indeed, these muscle fibers are often referred to as the articularis cubiti.
The anconeus is a small triangular muscle spanning the posterior side of the elbow. The muscle is located between the lateral epicondyle of the humerus and a strip along the posterior aspect of the proximal ulna (see Figure 6-39). Compared with the triceps muscle, the anconeus has a relatively small cross-sectional area and a small moment arm for extension (see Table 6-7). Although the anconeus is not capable of producing large elbow extension torque, it still provides important longitudinal and medial-lateral stability across the humero-ulnar joint. This stability is beneficial during extension activities, but also during active pronation and supination. The anconeus has a similar topographic orientation at the elbow as the oblique fibers of the vastus medialis have at the knee. This orientation is best appreciated by visually internally rotating the upper limb by 180 degrees, such that the olecranon faces anteriorly—a position more structurally and functionally analogous to the lower limb.
Electromyographic Analysis of Elbow Extension: Maximal-effort elbow extension generates near maximum levels of EMG activity from all components of the elbow extensor group. During submaximal efforts of elbow extension, however, different parts of muscles are recruited only at certain levels of effort.74 The anconeus is usually the first muscle to initiate and maintain low levels of elbow extension force.36 As extensor effort gradually increases, the medial head of the triceps is usually next in line to join the anconeus.74 The medial head remains active for most elbow extension movements.21 The medial head has therefore been termed the “workhorse” of the extensors, functioning as the extensor counterpart to the brachialis.74
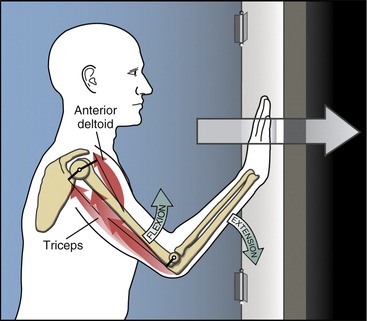
Torque Generation by the Elbow Extensors: The elbow extensor muscles provide static stability to the elbow, similar to the way the quadriceps muscles are often used to stabilize the knee. Consider the common posture of bearing weight through the upper limb with elbows held partially flexed. The extensors stabilize the flexed elbow through isometric contraction or very-low–velocity eccentric activation. In contrast, these same muscles are required to generate much larger and dynamic extensor torques through high-velocity concentric or eccentric activations. Consider activities such as throwing a ball, pushing up from a low chair, or rapidly pushing open a door. As with many explosive pushing activities, elbow extension is typically combined with some degree of shoulder flexion (Figure 6-41). The shoulder flexion function of the anterior deltoid is an important synergistic component of the forward push. The anterior deltoid produces a shoulder flexion torque that drives the limb forward and neutralizes the shoulder extension tendency of the long head of the triceps. From a physiologic perspective, combining shoulder flexion with elbow extension minimizes the rate and amount of shortening required by the long head of the triceps to completely extend the elbow.
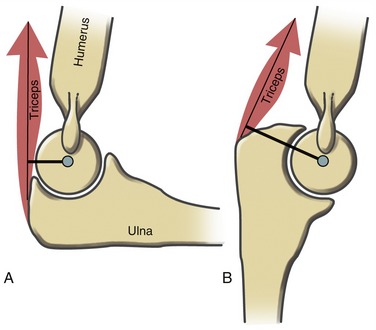
The elbow extensor muscles produce maximal-level torque when the elbow is flexed to about 90 degrees.14,62 This is approximately the same angle at which the elbow flexor muscles, as a group, produce maximum-flexion torque. The 90-degree flexed elbow therefore is the most actively isometric stable position of the joint. Of interest, although both muscle groups produce peak, maximal-effort torques at roughly similar joint angles, the largest internal moment arms for the two groups occur at very different joint angles: about 90 degrees of flexion for the elbow flexors, and near full extension for the triceps and anconeus.3 Full extension places the thick olecranon process between the joint’s axis of rotation and the line of force of the tendon of the triceps (Figure 6-42). The fact that peak elbow extensor torque occurs near 90 degrees of flexion instead of near extension suggests that muscle length, not leverage, is very influential in determining where in the range of motion that peak elbow extension torque naturally occurs.
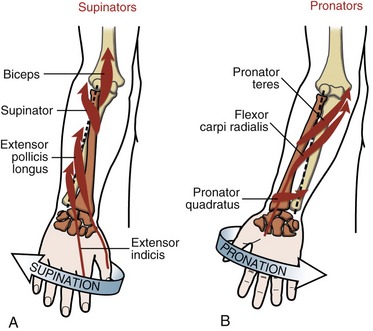
Function of the Supinator and Pronator Muscles
The lines of force of most pronator and supinator muscles of the forearm are shown in Figure 6-44. In order to be even considered as a pronator or a supinator, a given muscle must possess two fundamental features. First, the muscle must attach on both sides of the axis of rotation—that is, a proximal attachment on the humerus or the ulna and a distal attachment on the radius or the hand. Muscles such as the brachialis or extensor pollicis brevis therefore cannot pronate or supinate the forearm, regardless of any other biomechanical variable. Second, the muscle must produce a force that acts with an internal moment arm around the axis of rotation for pronation and supination. The muscle’s moment arm is greatest if its line of force is perpendicular to the axis of rotation. Although no pronator or supinator muscle (at least when considered in the anatomic position) has such an ideal line of force, the pronator quadratus comes very close (see Figure 6-44, B).
Pronation and supination of the forearm are functionally associated with internal and external rotation at the shoulder. Shoulder internal rotation often occurs with pronation, whereas shoulder external rotation often occurs with supination. Combining these shoulder and forearm rotations allows the hand to rotate nearly 360 degrees in space, rather than only 170 to 180 degrees by pronation and supination alone. A functional association in strength has also been demonstrated, at least between shoulder external rotation and forearm supination. Supination torques are 9% greater when performed with the shoulder externally rotated as compared with internally rotated.66 The mechanism for this difference is not clear but may involve the biceps muscle—the primary supinator of the forearm. External rotation may elongate the long head of the biceps slightly as its tendon crosses the humeral head, thereby augmenting the muscle’s force-generating ability.
SUPINATOR MUSCLES
The primary supinator muscles are the supinator and biceps brachii.9 Secondary muscles with a limited potential to supinate are the radial wrist extensors, which attach near the lateral epicondyle of the humerus, the extensor pollicis longus, and the extensor indicis (see Figure 6-44, A). The brachioradialis is considered a secondary supinator and a secondary pronator, especially during short-arc, high-power motions.6,15,21 Regardless of the position of the forearm, contraction of the brachioradialis rotates the forearm to the neutral, thumb-up position.9 From a fully pronated position, therefore, the muscle supinates; from a fully supinated position, the muscle pronates. Of interest, contraction of the brachioradialis biases the forearm toward a position that maximizes its moment arm as an elbow flexor.
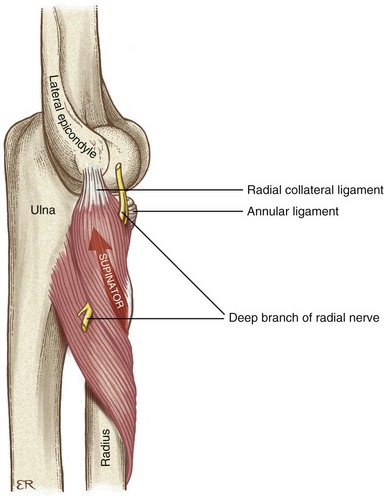
Supinator versus Biceps Brachii: The supinator muscle has an extensive proximal muscle attachment (Figure 6-45). A superficial set of fibers arises from the lateral epicondyle of the humerus and the radial collateral and annular ligaments. A deeper set of fibers arises from the ulna near and along the supinator crest. Both sets of muscle fibers attach distally along the proximal one third of the radius. From a pronated position, the supinator is twisted and elongated around the radius and therefore is in excellent position to supinate the forearm. The supinator has only minimal attachments to the humerus and passes too close to the medial-lateral axis of rotation at the elbow to produce significant flexion or extension torque.
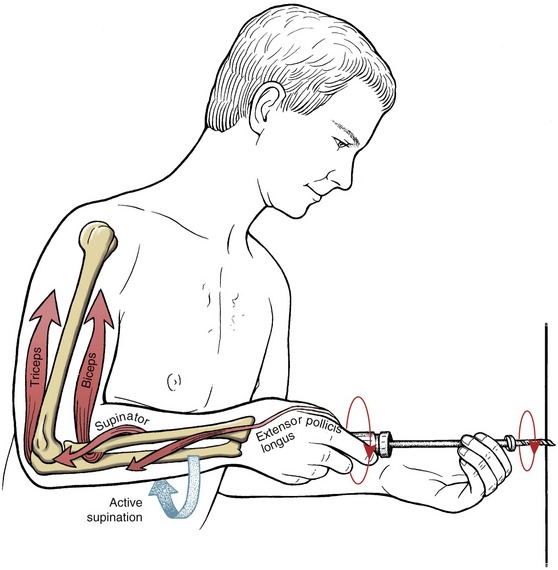
The supinator muscle is a relentless forearm supinator, similar to the brachialis during elbow flexion. The supinator muscle generates significant EMG activity during forearm supination, regardless of the elbow angle or the speed or power of the action.75 The biceps muscle, also a primary supinator, is normally recruited during higher power supination activities, especially those associated with elbow flexion.
The biceps brachii is a powerful supinator muscle of the forearm. The biceps has about three times the physiologic cross-sectional area as the supinator muscle.37 The dominant role of the biceps as a supinator can be verified by palpating the biceps during a series of rapid and forceful pronation-to-supination motions, especially with the elbow flexed to 90 degrees. As the forearm is pronated, the biceps tendon wraps around the proximal radius. From a fully pronated position, active contraction of the biceps “spins” the radius sharply into supination.
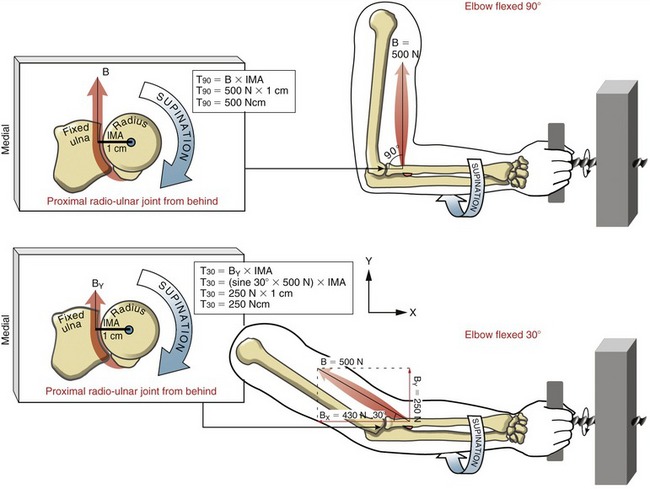
The effectiveness of the biceps as a supinator is greatest when the elbow is flexed to about 90 degrees.9 For this reason, the elbow is naturally held flexed to about 90 degrees during many high-powered supination tasks. At a 90-degree elbow angle, the tendon of the biceps approaches a 90-degree angle-of-insertion into the radius. This biomechanical situation allows the entire magnitude of a maximal-effort biceps force to intersect nearly perpendicular to the axis of rotation of the forearm. When the elbow is flexed to only 30 degrees, for example, the tendon of the biceps loses its right-angle intersection with the axis of rotation. As depicted by the calculations shown in Figure 6-46, this change in angle reduces the mechanical supinator torque potential of the biceps by 50%. Clinically, this difference is important during evaluation of the torque output from a strength-testing apparatus or when providing advice about ergonomics.
When high-power supination torque is required to vigorously turn a screw, for example, the biceps is recruited by the nervous system to assist other muscles, such as the smaller supinator muscle and extensor pollicis longus. For reasons described previously, this task typically requires that the elbow be held flexed to about 90 degrees (Figure 6-47). Maintaining this elbow posture during the task requires that the triceps muscle co-contract synchronously with the biceps muscle. The triceps muscle supplies an essential force during this activity because it prevents the biceps from actually flexing the elbow and shoulder during every supination effort. Unopposed biceps action causes the screwdriver to be pulled away from the screw on every effort—hardly effective. By attaching to the ulna versus the radius, the triceps is able to neutralize the elbow flexion tendency of the biceps without interfering with the supination task. This muscular cooperation is an excellent example of how two muscles can function as synergists for one activity while at the same time remaining as direct antagonists.
PRONATOR MUSCLES
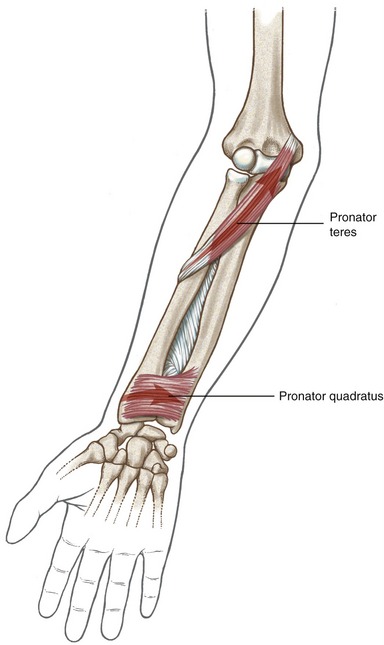
The primary muscles for pronation are the pronator teres and the pronator quadratus (Figure 6-48). The flexor carpi radialis and the palmaris longus are secondary pronators, both attaching to the medial epicondyle of the humerus (see Figure 6-44, B).
Pronator Teres versus Pronator Quadratus: The pronator teres has two heads: humeral and ulnar. The median nerve passes between these two heads and therefore is a site for possible nerve compression.64 The pronator teres functions as a primary forearm pronator, as well as an elbow flexor. The pronator teres produces its greatest EMG activity during higher-power pronation actions,7 such as attempting to unscrew an overtightened screw with the right hand or pitching a baseball. The triceps is an important synergist to the pronator teres, often required to neutralize the ability of the pronator teres to flex the elbow.
The pronator quadratus is located at the extreme distal end of the anterior forearm, deep to all the wrist flexors and extrinsic finger flexors. This flat, quadrilateral muscle attaches between the anterior surfaces of the distal one quarter of the ulna and the radius. Overall, from proximal to distal, the pronator quadratus has a slight obliquity in fiber direction, similar to, but not quite as angled as, the pronator teres. The pronator quadratus is the most active and consistently used pronator muscle, involved during all pronation movements, regardless of the power demands or the amount of associated elbow flexion.7
The pronator quadratus is well designed biomechanically as an effective torque producer and a stabilizer of the distal radio-ulnar joint.25,72 The pronator quadratus has a line of force oriented almost perpendicular to the forearm’s axis of rotation (Figure 6-49, A). This design maximizes the potential of the muscle to produce a torque. In addition to effectively producing a pronation torque, the muscle simultaneously compresses the ulnar notch of the radius directly against the ulnar head (see Figure 6-49, B). This compression force stabilizes the distal radio-ulnar joint throughout the range of pronation (see Figure 6-49, C). This active force augments the passive force produced by the triangular fibrocartilage complex. The force of the pronator quadratus also guides the joint through its natural arthrokinematics.
SYNOPSIS
About half of the muscles studied in this chapter control multiple regions of the arm or forearm. For this reason, movements that appear quite simple and limited to just one region—such as the forearm, for example—are typically more complex and involve a larger than expected set of participating muscles. Reconsider the forceful biceps-driven supination action required to tighten a screw (previously highlighted in Figure 6-47). During this task, triceps activation is also required to neutralize the strong (and unwanted) elbow flexion component of the biceps. The co-contraction of the long head of the biceps and triceps muscles must also kinetically balance and stabilize the glenohumeral joint. In addition, axial-scapular muscles, such as the trapezius, rhomboids, and serratus anterior, are needed to stabilize the scapula against the strong pull of the biceps and triceps muscles. Without this stabilization—be it from selective nerve injury, loss of motor control, pain, or simple disuse—the muscles of the elbow and forearm are less effective at performing their tasks.
REFERENCES
1. Ahrens, PM, Redfern, DR, Forester, AJ. Patterns of articular wear in the cadaveric elbow joint. J Shoulder Elbow Surg. 2001;10:52–56.
2. Amis, AA, Dowson, D, Wright, V. Elbow joint force predictions for some strenuous isometric actions. J Biomech. 1980;13:765–775.
3. An, KN, Hui, FC, Morrey, BF, et al. Muscles across the elbow joint: a biomechanical analysis. J Biomech. 1981;14:659–669.
4. Askew, LJ, An, KN, Morrey, BF, Chao, EY. Isometric elbow strength in normal individuals. Clin Orthop Relat Res. 1987;222:261–266.
5. Baeyens, JP, Van, GF, Goossens, M, et al. In vivo 3D arthrokinematics of the proximal and distal radioulnar joints during active pronation and supination. Clin Biomech (Bristol, Avon). 2006;21(Suppl 1):S9–S12.
6. Basmajian, JV, Latif, A. Integrated actions and functions of the chief flexors of the elbow: A detailed electromyographic analysis. J Bone Joint Surg Am. 1957;39:1106–1118.
7. Basmajian, JV, Travill, A. Electromyography of the pronator muscles of the forearm. Anat Rec. 1961;139:45–49.
8. Bozkurt, M, Acar, HI, Apaydin, N, et al. The annular ligament: an anatomical study. Am J Sports Med. 2005;33:114–118.
9. Bremer, AK, Sennwald, GR, Favre, P, Jacob, HA. Moment arms of forearm rotators. Clin Biomech (Bristol, Avon). 2006;21:683–691.
10. Callaway, GH, Field, LD, Deng, XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223–1231.
11. Chang, CW, Wang, YC, Chu, CH. Increased carrying angle is a risk factor for nontraumatic ulnar neuropathy at the elbow. Clin Orthop Relat Res. 2008;466:2190–2195.
12. Cohen, MS, Bruno, RJ. The collateral ligaments of the elbow: Anatomy and clinical correlation. Clin Orthop Relat Res. 2001;383:123–130.
13. Cooney, WP. Reconstructive procedures of the elbow: Joint replacement arthroplasty. In Morrey BF, ed.: The elbow and its disorders, ed 3, Philadelphia: Saunders, 2000.
14. Currier, DP. Maximal isometric tension of the elbow extensors at varied positions. I. Assessment by cable tensiometer. Phys Ther. 1972;52:1043–1049.
15. de Sousa, OM, de Moraes, JL, Vieira, FL. Electromyographic study of the brachioradialis muscle. Anat Rec. 1961;139:125–131.
16. DeFrate, LE, Li, G, Zayontz, SJ, Herndon, JH. A minimally invasive method for the determination of force in the interosseous ligament. Clin Biomech (Bristol, Avon). 2001;16:895–900.
17. DiTano, O, Trumble, TE, Tencer, AF. Biomechanical function of the distal radioulnar and ulnocarpal wrist ligaments. J Hand Surg [Am]. 2003;28:622–627.
18. Dugas, JR, Ostrander, RV, Cain, EL, et al. Anatomy of the anterior bundle of the ulnar collateral ligament. J Shoulder Elbow Surg. 2007;16:657–660.
19. Dunning, CE, Zarzour, ZD, Patterson, SD, et al. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 2001;83:1823–1828.
20. Ekenstam, F, Hagert, CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plastic Reconstruct Surg. 1985;19:17–25.
21. Funk, DA, An, KN, Morrey, BF, Daube, JR. Electromyographic analysis of muscles across the elbow joint. J Orthop Res. 1987;5:529–538.
22. Gabl, M, Zimmermann, R, Angermann, P, et al. The interosseous membrane and its influence on the distal radioulnar joint. An anatomical investigation of the distal tract. J Hand Surg [Br]. 1998;23:179–182.
23. Gallagher, MA, Cuomo, F, Polonsky, L, et al. Effects of age, testing speed, and arm dominance on isokinetic strength of the elbow. J Shoulder Elbow Surg. 1997;6:340–346.
24. Gallay, SH, Richards, RR, O’Driscoll, SW. Intraarticular capacity and compliance of stiff and normal elbows. Arthroscopy. 1993;9:9–13.
25. Garcia-Elias, M. Soft-tissue anatomy and relationships about the distal ulna. Hand Clin. 1998;14:165–176.
26. Geel, CW, Palmer, AK. Radial head fractures and their effect on the distal radioulnar joint. A rationale for treatment. Clin Orthop Relat Res. 1992;275:79–84.
27. Gefen, JY, Gelmann, AS, Herbison, GJ, et al. Use of shoulder flexors to achieve isometric elbow extension in C6 tetraplegic patients during weight shift. Spinal Cord. 1997;35:308–313.
28. Gordon, KD, Kedgley, AE, Ferreira, LM, et al. Effect of simulated muscle activity on distal radioulnar joint loading in vitro. J Orthop Res. 2006;24:1395–1404.
29. Hargreaves, D, Emery, R. Total elbow replacement in the treatment of rheumatoid disease. Clin Orthop Relat Res. 1999;366:61–71.
30. Hoffmann, G, Laffont, I, Hanneton, S, Roby-Brami, A. How to extend the elbow with a weak or paralyzed triceps: Control of arm kinematics for aiming in C6-C7 quadriplegic patients. Neuroscience. 2006;139:749–765.
31. Hollister, AM, Gellman, H, Waters, RL. The relationship of the interosseous membrane to the axis of rotation of the forearm. Clin Orthop Relat Res. 1994;298:272–276.
32. Hotchkiss, RN, An, KN, Sowa, DT, et al. An anatomic and mechanical study of the interosseous membrane of the forearm: pathomechanics of proximal migration of the radius. J Hand Surg [Am]. 1989;14:256–261.
33. Inman, VT, Saunders, JB. Referred pain from skeletal structures. J Nerv Ment Dis. 1944;99:660–667.
34. Ishii, S, Palmer, AK, Werner, FW, et al. An anatomic study of the ligamentous structure of the triangular fibrocartilage complex. J Hand Surg [Am]. 1998;23:977–985.
35. Kleinman, WB, Graham, TJ. The distal radioulnar joint capsule: Clinical anatomy and role in posttraumatic limitation of forearm rotation. J Hand Surg [Am]. 1998;23:588–599.
36. Le Bozec, S, Maton, B, Cnockaert, JC. The synergy of elbow extensor muscles during static work in man. Eur J Appli Physiol Occup Physiol. 1980;43:57–68.
37. Lehmkuhl, LD, Smith, LK. Brunnstrom’s clinical kinesiology, ed 4. Philadelphia: FA Davis; 1983.
38. Lin, F, Kohli, N, Perlmutter, S, et al. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16:795–802.
39. Lindau, T, Adlercreutz, C, Aspenberg, P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg [Am]. 2000;25:464–468.
40. MacConaill, MA, Basmajian, JV. Muscles and movements: a basis for human kinesiology. New York: Robert E. Krieger; 1977.
41. Mandelbaum, BR, Silvers, HJ, Watanabe, DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003–1010.
42. Manson, TT, Pfaeffle, HJ, Herdon, JH, et al. Forearm rotation alters interosseous ligament strain distribution. J Hand Surg [Am]. 2000;25:1058–1063.
43. Matei, CI, Logigian, EL, Shefner, JM. Evaluation of patients with recurrent symptoms after ulnar nerve transposition. Muscle Nerve. 2004;30:493–496.
44. Miyasaka, KC. Anatomy of the elbow. Orthop Clin North Am. 1999;30:1–13.
45. Morrey, BF. Radial head fracture. In Morrey BF, ed.: The elbow and its disorders, ed 3, Philadelphia: Saunders, 2000.
46. Morrey, BF, An, KN, Stormont, TJ. Force transmission through the radial head. J Bone Joint Surg [Am]. 1988;70:250–256.
47. Morrey, BF, Askew, LJ, Chao, EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg [Am]. 1981;63:872–877.
48. Morrey, BF, Chao, EY. Passive motion of the elbow joint. J Bone Joint Surg [Am]. 1976;58:501–508.
49. Morrey, BF, Tanaka, S, An, KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;Apr:187–195.
50. Murray, WM, Delp, SL, Buchanan, TS. Variation of muscle moment arms with elbow and forearm position. J Biomech. 1995;28:513–525.
51. Nakamura, T, Yabe, Y, Horiuchi, Y. Dynamic changes in the shape of the triangular fibrocartilage complex during rotation demonstrated with high resolution magnetic resonance imaging. J Hand Surg [Br]. 1999;24:338–341.
52. Neumann, DA. Use of diaphragm to assist rolling for the patient with quadriplegia. Phys Ther. 1979;59:39.
53. Neumann, DA, Soderberg, GL, Cook, TM. Electromyographic analysis of hip abductor musculature in healthy right-handed persons. Phys Ther. 1989;69:431–440.
54. O’Driscoll, SW, Jupiter, JB, King, GJ, et al. The unstable elbow. Instr Course Lect. 2001;50:89–102.
55. Ofuchi, S, Takahashi, K, Yamagata, M, et al. Pressure distribution in the humeroradial joint and force transmission to the capitulum during rotation of the forearm: Effects of the Sauve-Kapandji procedure and incision of the interosseous membrane. J Orthop Sci. 2001;6:33–38.
56. Olsen, BS, Søjbjerg, JO, Dalstra, M, Sneppen, O. Kinematics of the lateral ligamentous constraints of the elbow joint. J Shoulder Elbow Surg. 1996;5:333–341.
57. Palmer, AK, Werner, FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;187:26–35.
58. Paraskevas, G, Papadopoulos, A, Papaziogas, B, et al. Study of the carrying angle of the human elbow joint in full extension: A morphometric analysis. Surg Radiol Anat. 2004;26:19–23.
59. Petrie, S, Collins, JG, Solomonow, M, et al. Mechanoreceptors in the human elbow ligaments. J Hand Surg [Am]. 1998;23:512–518.
60. Pfaeffle, HJ, Fischer, KJ, Manson, TT, et al. Role of the forearm interosseous ligament: Is it more than just longitudinal load transfer? J Hand Surg [Am]. 2000;25:683–688.
61. Pfaeffle, HJ, Tomaino, MM, Grewal, R, et al. Tensile properties of the interosseous membrane of the human forearm. J Orthop Res. 1996;14:842–845.
62. Provins, K.A., Salter, N. Maximum torque exerted about the elbow joint. J Appl Physiol. 1955;7:393–398.
63. Regan, WD, Korinek, SL, Morrey, BF, et al. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. 1991;271:170–179.
64. Rehak, DC. Pronator syndrome. Clin Sports Med. 2001;20:531–540.
65. Sabick, MB, Torry, MR, Lawton, RL, Hawkins, RJ. Valgus torque in youth baseball pitchers: A biomechanical study. J Shoulder Elbow Surg. 2004;13:349–355.
66. Savva, N, McAllen, CJ, Giddins, GE. The relationship between the strength of supination of the forearm and rotation of the shoulder. J Bone Joint Surg Br. 2003;85:406–407.
67. Schuind, F, An, KN, Berglund, L, et al. The distal radioulnar ligaments: a biomechanical study. J Hand Surg [Am]. 1991;16:1106–1114.
68. Schuind, FA, Goldschmidt, D, Bastin, C, Burny, F. A biomechanical study of the ulnar nerve at the elbow. J Hand Surg [Br]. 1995;20:623–627.
69. Skahen, JR, 3rd., Palmer, AK, Werner, FW, Fortino, MD. The interosseous membrane of the forearm: anatomy and function. J Hand Surg [Am]. 1997;22:981–985.
70. Standring, S. Gray’s anatomy: the anatomical basis of clinical practice, ed 40. St Louis: Elsevier; 2009.
71. Stokdijk, M, Meskers, CG, Veeger, HE, et al. Determination of the optimal elbow axis for evaluation of placement of prostheses. Clin Biomech. 1999;14:177–184.
72. Stuart, PR. Pronator quadratus revisited. J Hand Surg [Br]. 1996;21:714–722.
73. Topp, KS, Boyd, BS. Structure and biomechanics of peripheral nerves: Nerve responses to physical stresses and implications for physical therapist practice. Phys Ther. 2006;86:92–109.
74. Travill, A. Electromyographic study of the extensor apparatus. Anat Rec. 1962;144:373–376.
75. Travill, A., Basmajian, JV. Electromyography of the supinators of the forearm. Anat Rec. 1961;139:557–560.
76. Tsunoda, N, O’Hagan, F, Sale, DG, MacDougall, JD. Elbow flexion strength curves in untrained men and women and male bodybuilders. Eur J Appl Physiol Occup Physiol. 1993;66:235–239.
77. van Andel, CJ, Wolterbeek, N, Doorenbosch, CA, et al. Complete 3D kinematics of upper extremity functional tasks. Gait Posture. 2008;27:120–127.
78. Van der Heijden, EP, Hillen, B. A two-dimensional kinematic analysis of the distal radioulnar joint. J Hand Surg [Br]. 1996;21:824–829.
79. Vardakas, DG, Varitimidis, SE, Goebel, F, et al. Evaluating and treating the stiff elbow. Hand Clin. 2002;18:77–85.
80. Ward, LD, Ambrose, CG, Masson, MV, Levaro, F. The role of the distal radioulnar ligaments, interosseous membrane, and joint capsule in distal radioulnar joint stability. J Hand Surg [Am]. 2000;25:341–351.
81. Watanabe, H, Berger, RA, An, KN, et al. Stability of the distal radioulnar joint contributed by the joint capsule. J Hand Surg [Am]. 2004;29:1114–1120.
82. Watanabe, H, Berger, RA, Berglund, LJ, et al. Contribution of the interosseous membrane to distal radioulnar joint constraint. J Hand Surg [Am]. 2005;30:1164–1171.
83. Williams, RJ, III., Urquhart, ER, Altchek, DW. Medial collateral ligament tears in the throwing athlete. Instr Course Lect. 2004;53:579–586.
84. Winters, JM, Kleweno, DG. Effect of initial upper-limb alignment on muscle contributions to isometric strength curves. J Biomech. 1993;26:143–153.
85. Yilmaz, E, Karakurt, L, Belhan, O, et al. Variation of carrying angle with age, sex, and special reference to side. Orthopedics. 2005;28:1360–1363.
STUDY QUESTIONS
1. List both muscular and nonmuscular tissues that are able to resist a distal pull (distraction) of the radius.
2. Describe how the different fibers of the medial collateral ligament of the elbow provide useful tension throughout the entire range of flexion and extension.
3. Describe the arthrokinematics at the humeroradial joint during a combined motion of elbow flexion and supination of the forearm.
4. Based on moment arm alone, which tissue shown in Figure 6-18, A could generate the greatest resistive torque opposing an elbow extension movement?
5. How many nerves innervate muscles that flex the elbow?
6. Based on data provided in Table 6-7, which head of the triceps produces the greatest elbow extension torque?
7. Why was the extensor pollicis brevis muscle not included in this chapter as a secondary supinator muscle of the forearm?
8. What is the kinesiologic role of the anterior deltoid during a “pushing” motion that combines elbow extension and shoulder flexion?
9. What muscle is the most direct antagonist to the brachialis muscle?
10. A patient has a 10-degree elbow flexion contracture that is assumed to originate because of muscular tightness. At the patient’s end range of extension, you apply an extension torque and note that the forearm passively “drifts” into supination. What clue does this observation provide as to which muscle or muscles are most tight (stiff)?
11. How would a radial nerve lesion in the axilla affect the task depicted in Figure 6-47?
12. What position of the upper extremity maximally elongates the biceps brachii muscle?
13. Why would a surgeon be concerned about the integrity of the interosseous membrane prior to a radial head resection?
14. A patient has a median nerve injury at the level of the middle of the humerus. Would you expect any weakness in active flexion of the elbow? Over time, what deformity or “tightness pattern” is most likely to develop at the forearm?
15. Assume you want to maximally stretch (elongate) the brachialis muscle by passively extending the elbow. Would the effectiveness of the stretch be enhanced by combining full passive pronation or supination of the forearm to the elbow extension?
 Answers to the study questions can be found on the Evolve website.
Answers to the study questions can be found on the Evolve website.

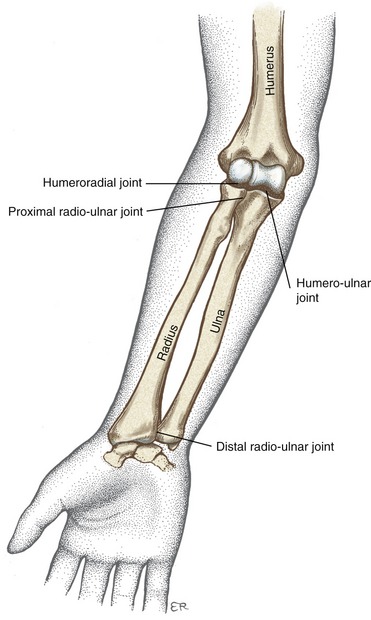
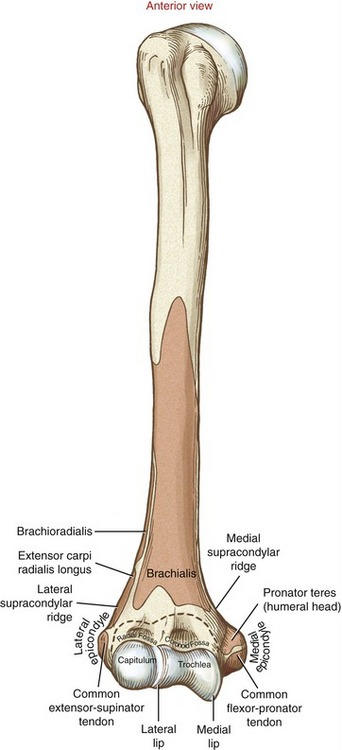
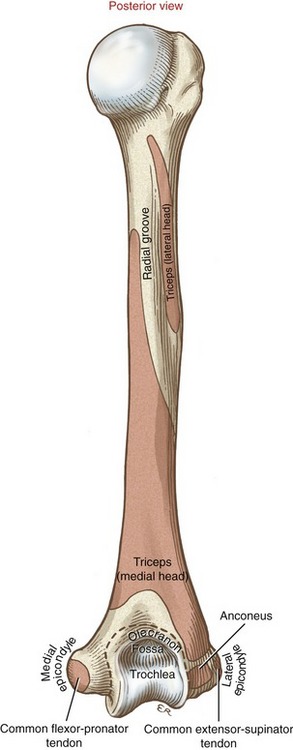
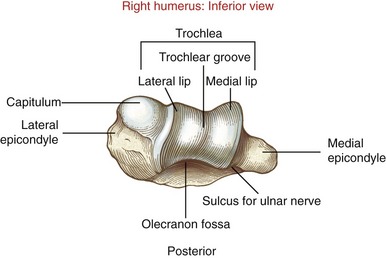
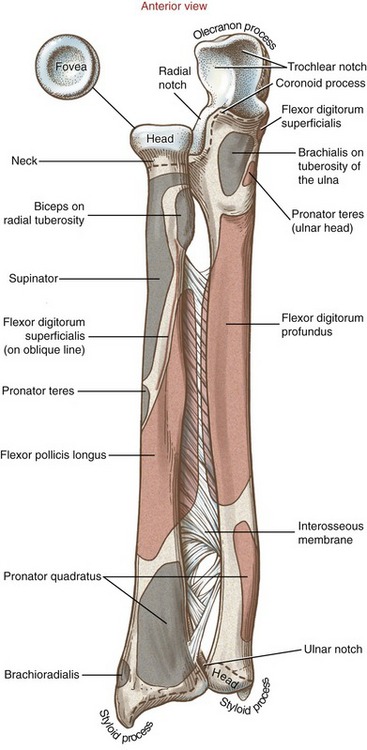
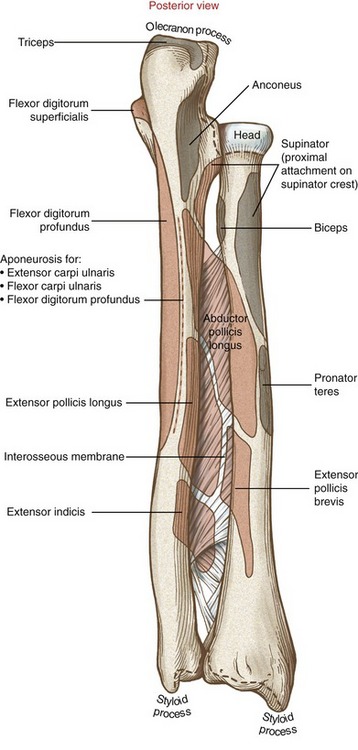
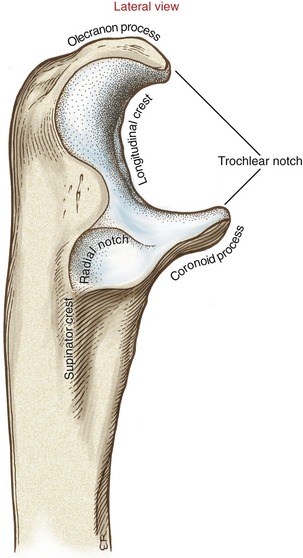
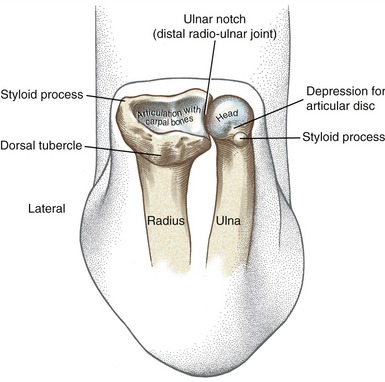
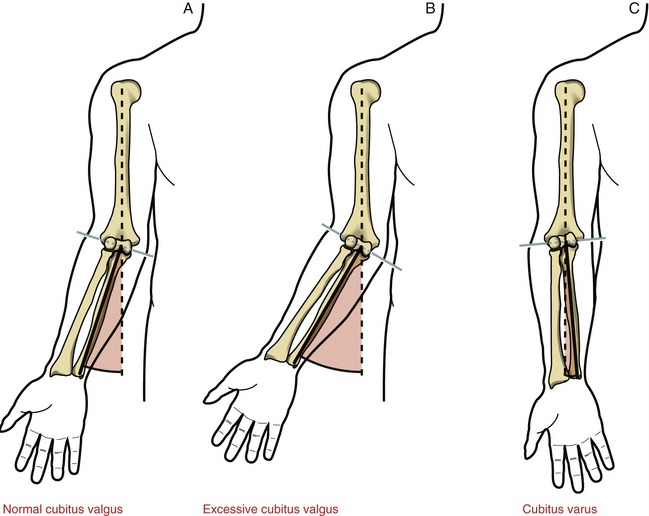
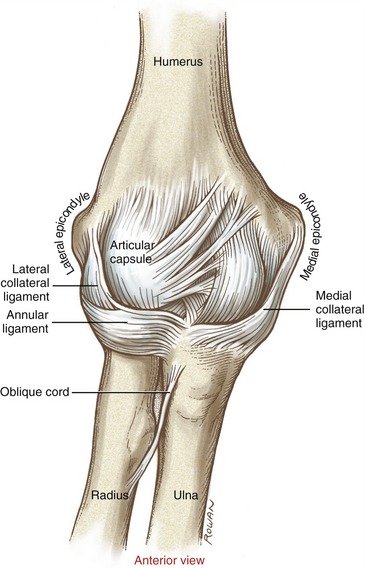
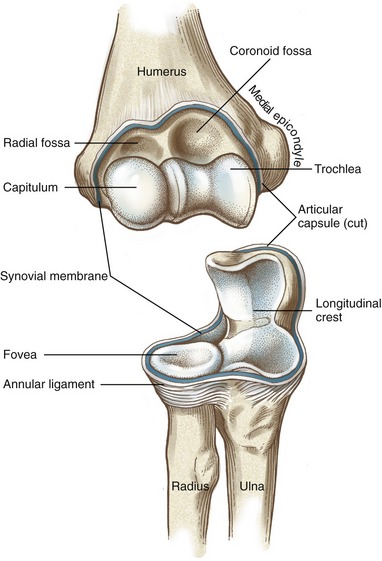
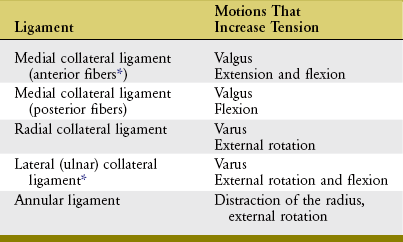
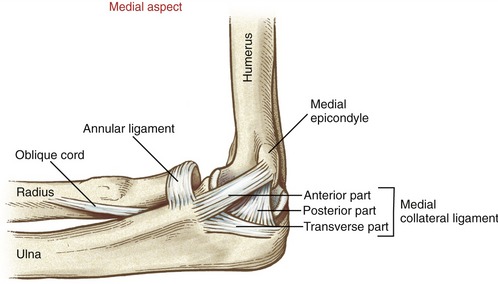

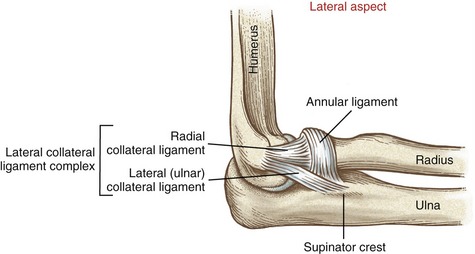
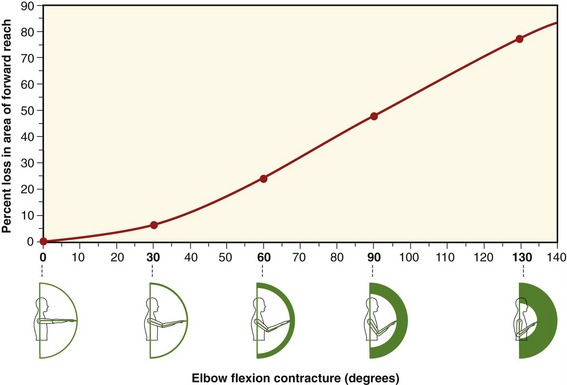
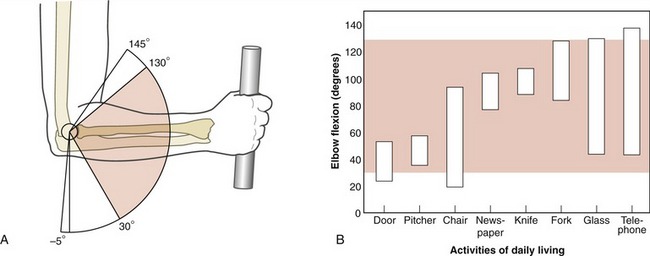
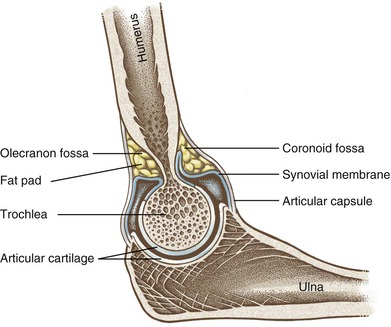
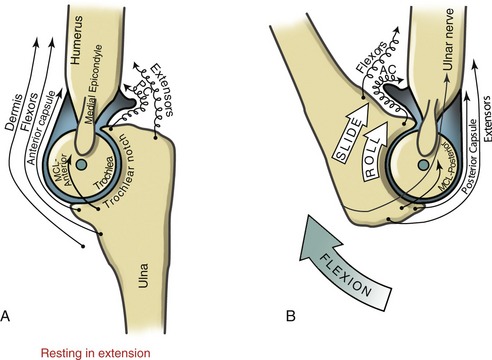
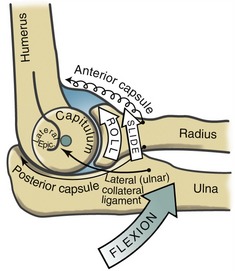
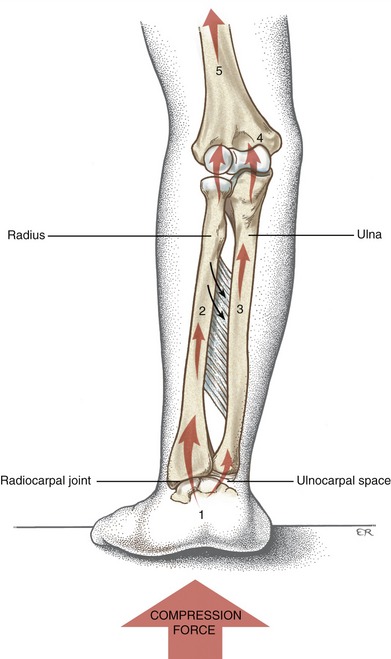
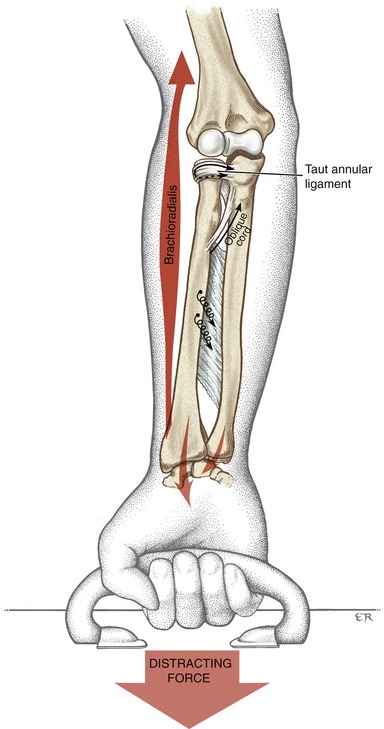
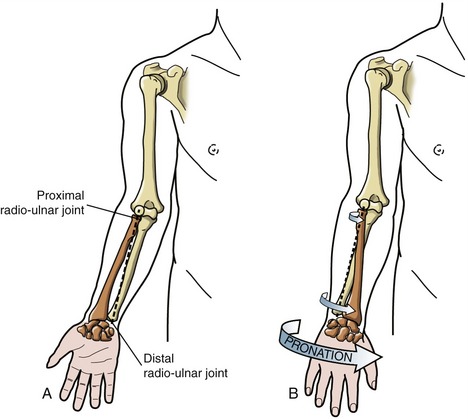
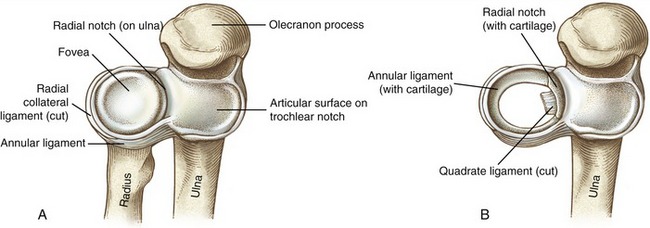

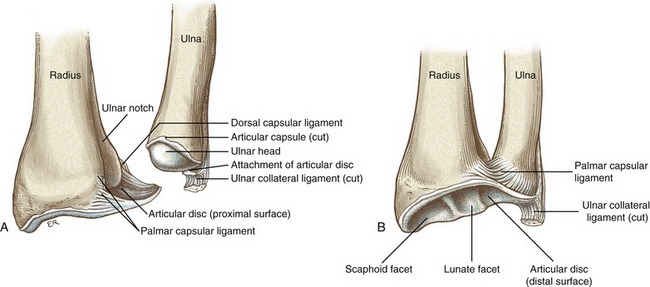
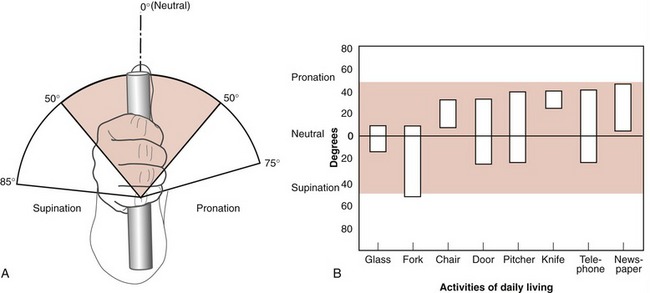
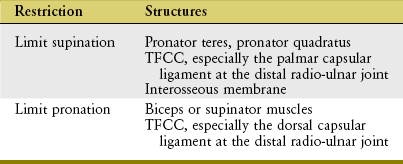
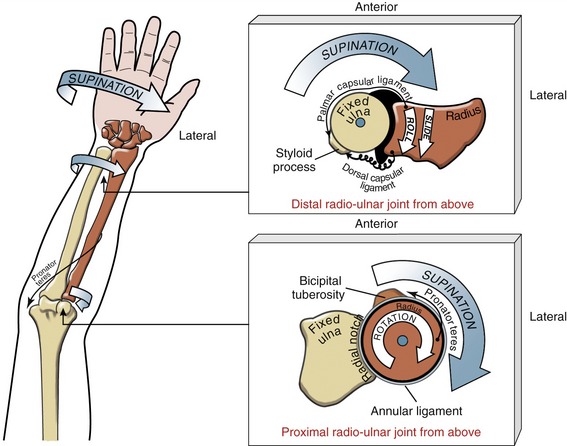
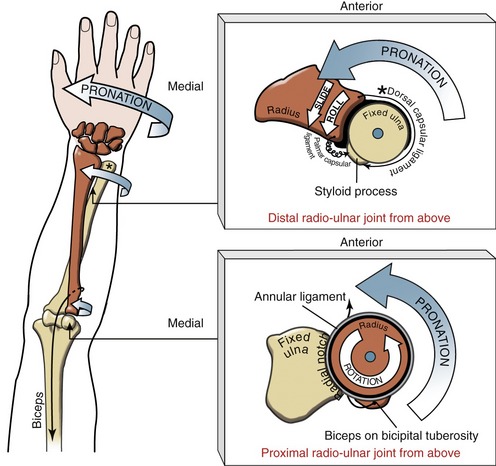
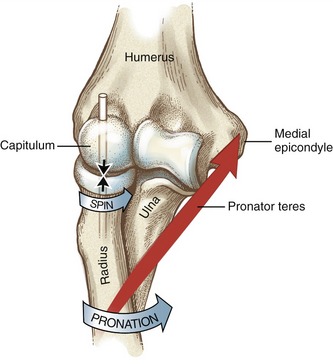
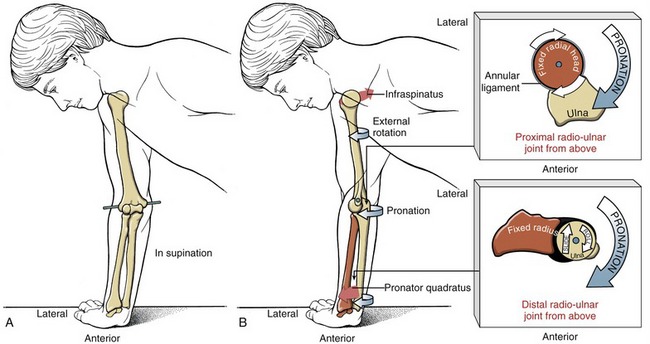
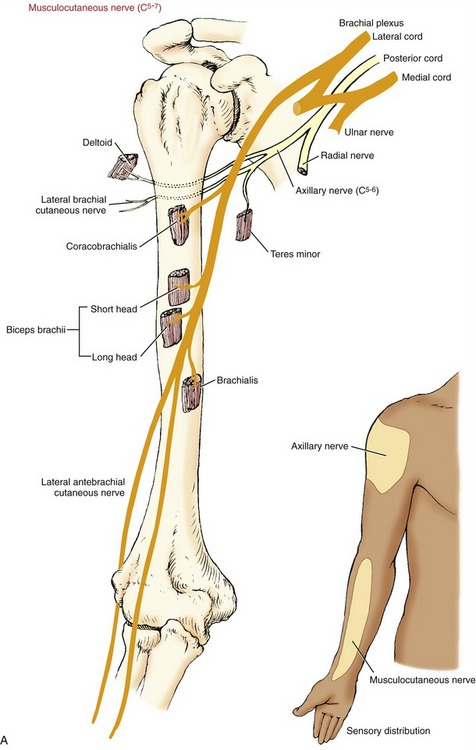
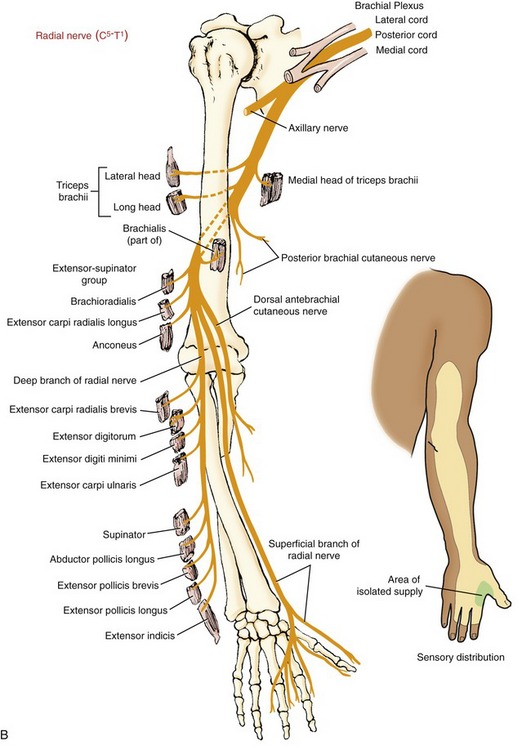
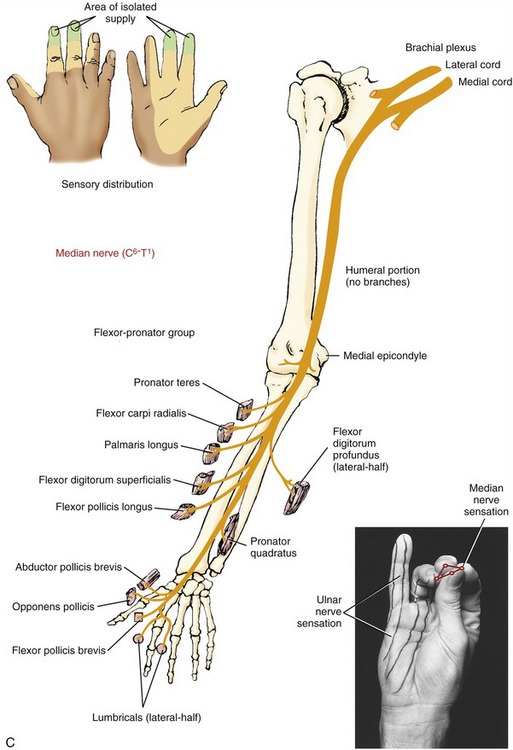
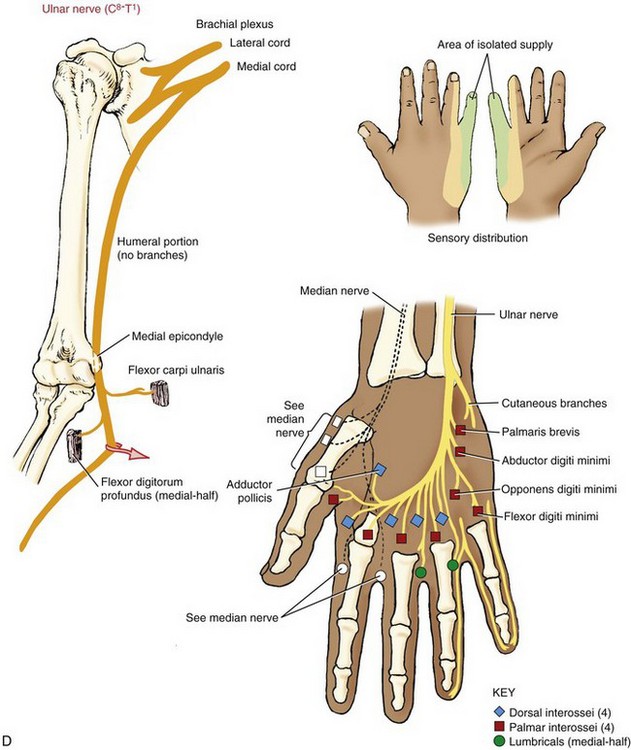
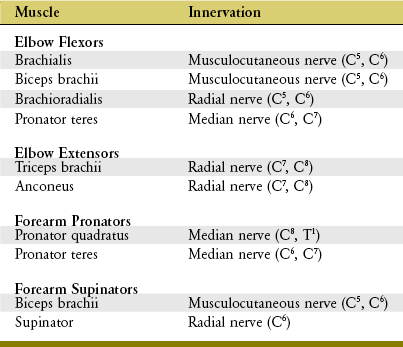
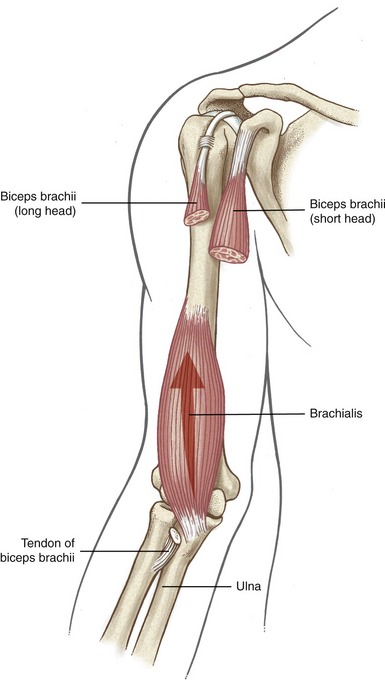
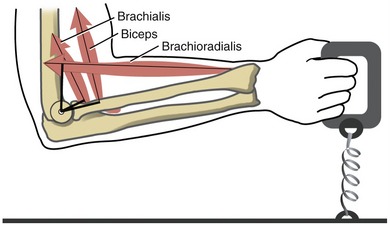
 age male = 41 yr,
age male = 41 yr,  age female = 45.1 yr. The elbow is maintained in 90 degrees of flexion with neutral forearm rotation. Data are shown for dominant limb only.
age female = 45.1 yr. The elbow is maintained in 90 degrees of flexion with neutral forearm rotation. Data are shown for dominant limb only.