Chapter 37 Drugs and Substance Abuse, Addiction, and Treatment
| Abbreviations | |
|---|---|
| AIDS | Acquired immunodeficiency syndrome |
| CNS | Central nervous system |
| DA | Dopamine |
| GABA | γ-Aminobutyric acid |
| GHB | γ-Hydroxybutyrate |
| 5-HT | Serotonin |
| IV | Intravenous |
| LSD | d-Lysergic acid diethylamide |
| MDMA | Methylenedioxymethamphetamine |
| NAcc | Nucleus accumbens |
| NE | Norepinephrine |
| NMDA | N-methyl-D-aspartate |
| NRT | Nicotine replacement therapy |
| PCP | Phencyclidine |
| THC | Tetrahydrocannabinol |
| VTA | Ventral tegmental area |
Therapeutic Overview
In a 2006 survey conducted by the U.S. Substance Abuse and Mental Health Services Administration, more than 20 million Americans aged 12 and older had used illicit drugs in the month before the survey, representing more than 8% of the population. The most commonly used illicit drug was marijuana, followed by prescription pain relievers, cocaine, stimulants, and the hallucinogens (Table 37-1). In addition, more than 50% of Americans used ethanol, with 23% reporting binge drinking (five or more drinks on one occasion) and nearly 7% reporting heavy drinking (binge drinking on at least five occasions) during the past month. Nearly 73 million Americans use some form of tobacco.
TABLE 37–1 Prevalence of Illicit Drug Use in the Unites States in 2006*
| Marijuana | 14.8 |
| Prescription pain relievers | 5.2 |
| Cocaine | 2.4 |
| Stimulants | 1.2 |
| Hallucinogens | 1.0 |
| Inhalants | 0.76 |
* Data from the U.S. Substance Abuse and Mental Health Services Administration; numbers represent millions of persons.
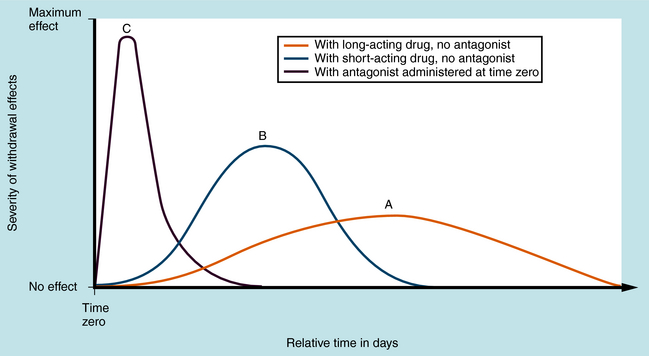
Dependence is characterized by physiological or behavioral changes after discontinuation of drug use, effects that are reversible on resumption of drug administration. Psychological dependence is characterized by intense craving and compulsive drug-seeking behavior. Abused substances often possess reinforcing effects accompanied by intense euphoria and feelings of well-being that foster their continued use. This is particularly true of stimulants such as cocaine and amphetamine. Physical dependence is associated with characteristic withdrawal signs upon cessation of drug administration. The withdrawal syndrome is similar for drugs within a pharmacological class but differs between classes. Its time course varies according to the rate of elimination of the drugs or their active metabolites. Withdrawal from long-acting drugs has a delayed onset, is relatively mild, and occurs over many days or weeks (Fig. 37-1, A), whereas withdrawal from more rapidly inactivated or eliminated drugs is more intense but of shorter duration (Fig. 37-1, B). Typically, physical dependence occurs when substances are used over extended times—usually days, weeks, or months. With repeated use, dependence becomes increasingly severe. Normally, occasional drug use does not result in clinically significant withdrawal. Spontaneous withdrawal occurs on cessation of drug taking. Precipitated withdrawal occurs when an antagonist is administered to displace the drug from its receptors, causing more rapid and severe effects (Fig. 37-1, C). An example is the administration of the opioid antagonist naltrexone to heroin-dependent individuals.
| Therapeutic Overview | |
|---|---|
| Cannabinoids | Hashish, marijuana |
| Depressants | Barbiturates, benzodiazepines, ethanol, GHB, methaqualone |
| Dissociative compounds | PCP, ketamine |
| Hallucinogens | LSD, mescaline, psilocybin |
| Opioids | Codeine, fentanyl, heroin, hydrocodone, hydromorphone, meperidine, morphine, opium, oxycodone |
| Stimulants | Amphetamine, cocaine, MDMA, methamphetamine, methylphenidate, nicotine |
| Anabolic steroids | Nandrolone, oxandrolone, oxymetholone, stanozolol, testosterone |
| Inhalants | Volatile solvents (toluene), gases (N2O), nitrites (amyl nitrite) |
Mechanisms of Action
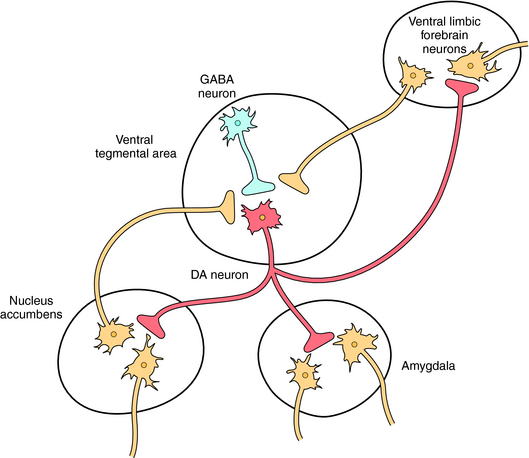
Several pharmacological classes of abused drugs including the cannabinoids, depressants, opioids, and the stimulants all share the ability to activate the mesolimbic dopamine (DA) “reward” pathway in the brain (see Fig. 27-8). These agents either directly activate these dopaminergic neurons or alter the activity of other neurotransmitters such as acetylcholine, γ-aminobutyric acid (GABA), glutamate, serotonin (5-HT), and norepinephrine (NE), which modulate the activity of these neurons. A diagram of ventral tegmental area (VTA)-nucleus accumbens (NAcc) dopamine neurons and pathways affecting the activity of these neurons is shown in Figure 37-2.
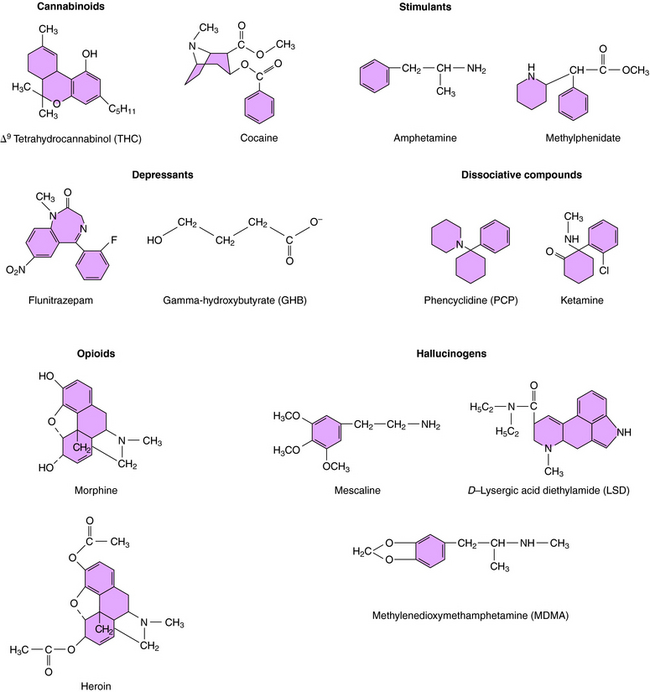
Marijuana (cannabis) is the dried leaf material, buds, and flowering tops from the common hemp plant Cannabis sativa. It has a variety of names including “pot,” “weed,” “grass,” and “maryjane.” Hashish is the dried resinous material exuded by mature plants. Cannabis is the most commonly abused illegal drug in the United States (see Table 37-1). Its major active chemical is Δ9-tetrahydrocannabinol (Δ9-THC; Fig. 37-3). Δ9-THC and related molecules are termed cannabinoids and exert their effects by binding to specific CB1 and CB2 cannabinoid G protein-coupled receptors (see Chapter 1). CB1 receptors are expressed in the brain and gastrointestinal tract and CB2 receptors in the periphery and immune system. The endogenous ligand for these receptors is anandamide, a long-chain arachidonic acid derivative.
CB1 receptors are found in high levels in the cerebellum (coordination of movement), cerebral cortex (cognitive functions), hippocampus (learning and memory), VTA and NAcc (rewarding effects), hypothalamus (satiety/feeding area), and basal ganglia (control of movement). The cannabinoids activate CB1 receptors in both the VTA and NAcc and increase the firing rate of VTA-NAcc neurons. Cannabinoids also increase corticotropin-releasing factor in the amygdala, a common action of many rewarding drugs.
CNS depressants such as barbiturates, non-barbiturate sedatives, and benzodiazepines enhance inhibitory GABA transmission by enhancing the action of endogenous GABA at GABAA receptors (see Chapter 31). Flunitrazepam is a particularly notoriously abused benzodiazepine known as “roofies” or “rophies.”
GABA interneurons in the VTA express GABAA receptors that normally function to tonically suppress the firing of DA neurons (see Fig. 37-2). GABAA receptors are also located on DA cell bodies in the VTA, but these receptors lack α1 subunits and thus are a different subunit composition than those expressed by the GABA neurons. Studies suggest that the depressants, by hyperpolarizing GABA interneurons in the VTA, produce a disinhibition of mesolimbic DA neurons, thereby increasing DA release.
GHB, which is produced endogenously at low levels during GABA metabolism, also belongs in this group (see Fig. 37-3) and is commonly called “liquid ecstasy,” “G,” “grievous bodily harm,” or “Georgia Home Boy.” Studies suggest that GHB interacts with specific binding sites on GABAB receptors, which are present on both GABA interneurons and DA neurons in the VTA, the former more sensitive to GHB than the latter. At low concentrations reflecting those used by the typical abuser, GHB is thought to activate only the receptors expressed by the GABA neurons, thereby inhibiting GABA activity, promoting DA release.
Alcohol is also a CNS depressant that activates the mesolimbic DA pathway. Although several mechanisms have been postulated to be involved in the actions of ethanol including effects of GABAA receptors (see Chapter 32), recent studies suggest that the ability of ethanol to promote DA release in the NAcc may involve its ability to release endocannabinoids and activate CB1 receptors. Further studies are warranted to discern the specific cellular mechanisms mediating the rewarding effects of alcohol.
Opiates are compounds isolated from the opium poppy that act at opioid receptors, whereas opioids are any synthetic or natural compounds that interact with opioid receptors; however, these terms are often used interchangeably. The two principal naturally occurring opiates are morphine and codeine. Heroin (“H” or “smack”), which is 3-,6-diacetylmorphine (Fig. 37-3), is the most commonly abused opioid and is approximately three times more potent than morphine, but the two have very similar effects. Heroin is metabolized to 6-acetylmorphine and morphine to exert its effects. Codeine, which is 3-methoxymorphine, is also demethylated to the more potent morphine by cytochrome P450 enzymes (see Chapter 2). The isoform involved is genetically polymorphic, and persons with mutated forms are unresponsive to codeine. Other synthetic opioids are widely available and abused, often as diverted prescription medications.
The reinforcing actions of the opioids are mediated by μ opioid receptors on GABA interneurons in the VTA, which inhibit GABAergic inhibitory activity (see Chapter 36).
The stimulant drugs are sympathomimetic amines that act on the CNS by enhancing NE and DA neurotransmission. Cocaine (“coke,” “snow,” “blow,” or “crack” for the free base; see Fig. 37-3) is the active ingredient of the South American coca bush. Amphetamines are structurally related to catecholamine neurotransmitters and ephedrine (see Chapter 11) and include amphetamine, N-methylamphetamine (methamphetamine, known as “speed,” “meth,” or “ice”), and others such as methylphenidate.
The reinforcing effects of stimulants arise from enhanced neurotransmission at dopaminergic synapses in the mesolimbic and mesocortical pathways (see Fig. 37-2). Cocaine binds to DA transporters and blocks the reuptake of DA, increasing its synaptic concentration. Amphetamines also act on DA transporters to enhance DA release and may increase its concentrations by inhibiting destruction by monoamine oxidase. Amphetamines may also directly activate postsynaptic receptors. Nicotine interacts directly with nicotinic receptors on DA neurons in the VTA to increase the firing of these neurons.
PCP (“angel dust”) and ketamine (“K” or “special K”) were originally developed as anesthetics (see Fig. 37-3). Ketamine is still used for changing burn dressings, for anesthesia in children (see Chapter 35), and for short-duration anesthesia in veterinary medicine. PCP is not used therapeutically because of the severity of emergence delirium in patients. Dextromethorphan (“DXM” or “robo”) is an over-the-counter cough suppressant and when taken in high doses, produces effects similar to those of PCP and ketamine.
PCP, ketamine, and high-dose dextromethorphan produce their effects through a use-dependent noncompetitive antagonism at excitatory glutamate N-methyl-D-aspartate (NMDA) receptors throughout the CNS (see Chapter 1).
Hallucinogens produce changes in mood, thought, and sensory perception such that colors, sounds, and smells are intensified. Because of the latter actions, these compounds are referred to as psychedelic or psychotomimetic agents. The hallucinogens have no recognized medical uses. Abused hallucinogens fall into two chemical classes, the substituted phenethylamines, of which mescaline is the prototype, and the indoleamines, of which D-lysergic acid diethylamide (LSD) is the prototype (see Figure 37-3). Others hallucinogens include psilocybin (from mushrooms) and dimethyltryptamine.
MDMA (“ecstasy” or “XTC”) is a substituted amphetamine (see Fig. 37-3) and has properties of both a hallucinogen and a stimulant. MDMA acts to increase the release of DA and 5-HT. Methylenedioxyamphetamine is a related compound.
Anabolic steroids are synthetic substances related to androgens, male sex hormones. These drugs promote growth of male sexual characteristics and have important clinical uses (see Chapter 41). However, steroid abuse is widespread in body-building and sports for enhancement of skeletal muscle growth. Abused steroids include testosterone itself as well as synthetic compounds, such as nandrolone, oxandrolone, oxymetholone, and stanozolol. The mechanism of action of these compounds is discussed in Chapter 41.
Pharmacokinetics
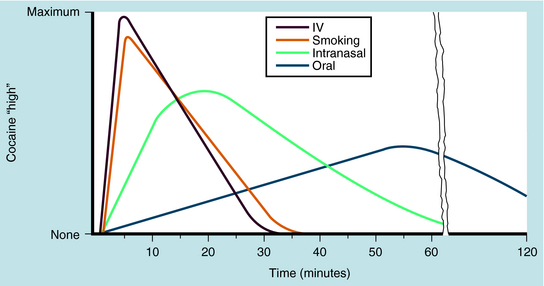
Abused substances represent many compounds whose pharmacokinetics depend on their structures and methods of use. A rapid effect is sought by opioid and stimulant abusers, and methods such as smoking or IV injection are preferred. Smoking allows the drug to pass rapidly from the lungs into the blood and brain. This is not true for slower-acting depressants such as alcohol or GHB or longer-lasting compounds such as LSD. The difference in degree of euphoria and the length of stimulant action for cocaine administered by different routes of administration is shown in Figure 37-4.
CNS depressants are taken orally, with rapid-acting barbiturates, such as secobarbital and pentobarbital, more widely abused than those with a slower onset, such as phenobarbital and benzodiazepines. GHB is rapidly absorbed and readily penetrates the CNS, producing effects within 15 to 30 minutes and lasting 2 to 3 hours. Oral flunitrazepam shows effects after 30 minutes and lasts up to 8 hours. The pharmacokinetics of the benzodiazepines are discussed in Chapter 31.
Heroin and morphine have poor oral bioavailability because of first-pass metabolism in the liver, although this is not true for codeine (see Chapter 36). Heroin is usually snorted, smoked (“chasing the dragon”), or injected and provides a rapid feeling of euphoria in 7 to 8 seconds when taken IV or 10 to 15 minutes when snorted or smoked. Its effects last approximately 4 to 6 hours, depending on dose. This very rapid euphoria contributes to its powerful addictive actions.
Pure cocaine is used as an H2O-soluble salt or as a free base. Cocaine salt is a bitter-tasting, white, crystalline material that is generally snorted or injected IV. Crack (free base cocaine), sold as small hard pieces or “rocks,” is volatilized and inhaled. It is rapidly absorbed and provides an almost instantaneous action. When administered IV, cocaine takes a few seconds to take effect, whereas snorted cocaine takes 5 to 10 minutes but lasts longer. Oral cocaine is slowly absorbed (Fig. 37-4) and produces a less intense effect. The effect of IV or inhaled cocaine generally lasts only 30 minutes, and redosing is common in an attempt to maintain intoxication. Cocaine is rapidly metabolized by blood and liver esterases, with urinary metabolites present for up to a week after use. Some N-demethylation occurs in the liver, with metabolites excreted in urine. Measurement of urinary cocaine metabolites is an important basis for establishing recent usage.
Relationship of Mechanisms of Action to Clinical Response
Cannabinoids are effective antiemetics and appetite stimulants and have some analgesic actions. Dronabinol is a synthetic, orally active cannabinoid approved for the treatment of cachexia (see Chapter 33) in patients with cancer or acquired immunodeficiency syndrome (AIDS) and to treat emesis caused by cancer chemotherapy in patients who do not respond to conventional antiemetics. Many also argue for use of smoked marijuana in treating chronic pain, improving appetite in AIDS patients, and suppressing spasticity in multiple sclerosis and spinal injury.
The effects of the benzodiazepines are discussed in Chapter 31 and those of ethanol in Chapter 32. GHB induces anterograde amnesia and with increased doses causes drowsiness and sleep, leading to general anesthesia, coma, respiratory and cardiac depression, seizures, and death.
The effects of the opioids are discussed in Chapter 36. The biological mechanisms underlying physical dependence on opioids are poorly understood. The most consistent indication of dependence is the increased sensitivity to precipitated withdrawal by administration of an opioid antagonist. This may begin with the first opioid dose, because under laboratory conditions, high doses of an antagonist can precipitate a withdrawal syndrome within a few hours after a single dose of morphine.
Pharmacovigilance: Side Effects, Clinical Problems, and Toxicity
Problems associated with drug abuse are summarized in the Clinical Problems Box.
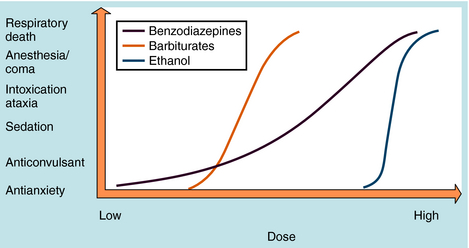
Dose-response curves for abused CNS depressant drugs are essentially the same as those for ethanol, except that they usually have shallower slopes. If one considers that a blood ethanol concentration of 0.1% represents one quarter to one third of the lethal concentration (see Chapter 32), the therapeutic index for alcohol would be among the poorest of any legal drug. In contrast, gram quantities of benzodiazepines may not be lethal, resulting in much larger therapeutic indices. Like ethanol, barbiturates, non-barbiturate sedatives, and GHB have dose-response curves with slopes much steeper than slopes of dose-response curves for benzodiazepines (Fig. 37-5).
After an overdose with depressant drugs, patients are unresponsive, pupils are sluggish and miotic, respiration is shallow and slow, and deep tendon reflexes are absent or attenuated. There are no known antagonists for barbiturates, non-barbiturate sedatives, or GHB, whereas the competitive benzodiazepine antagonist flumazenil can completely reverse benzodiazepine intoxication (see Chapter 31). Although benzodiazepines are rarely lethal when taken alone, they enhance the effects of other depressants taken concurrently, including alcohol.
The withdrawal symptoms after abrupt discontinuation of depressants and a comparison with those associated with opioid withdrawal are summarized in Table 37-2.
| Opioid Withdrawal | Depressant Withdrawal* |
|---|---|
| Anxiety and dysphoria | Anxiety and dysphoria |
| Craving and drug-seeking behavior | Craving and drug-seeking behavior |
| Sleep disturbance | Sleep disturbance |
| Nausea and vomiting | Nausea and vomiting |
| Lacrimation | Tremors |
| Rhinorrhea | Hyper-reflexia |
| Yawning | Hyperpyrexia |
| Piloerection and gooseflesh | Confusion and delirium |
| Sweating | Convulsions |
| Diarrhea | Life-threatening convulsions |
| Mydriasis | |
| Abdominal cramping | |
| Hyperpyrexia | |
| Tachycardia and hypertension |
Opioids are widely abused and represent serious consequences for the users, their families, and the community. The administration of heroin IV causes a surge of intense euphoria, a “rush” accompanied by a warming of the skin, dry mouth, and heavy feelings in arms and legs. The rush subsides after a few minutes, and the user feels relaxed, carefree, and somewhat dreamy but able to carry on many normal activities. Users who are not physically dependent recover readily. Unlike a person intoxicated with alcohol or other CNS depressants, opioid abusers are difficult to detect by observable behaviors.
Overdose leads to unconsciousness, respiratory depression, and extreme miosis, although the latter is not always apparent because asphyxia can result in pupillary dilation. Deaths are due to respiratory failure. The IV injection of an opioid antagonist, such as naloxone or nalmefene, can reverse all effects immediately and produce rapid recovery (see Chapter 36). However, it is important not to administer too large a dose, because severe withdrawal could be precipitated in a physically dependent patient. The duration of action of naloxone is shorter than that of opioid agonists, and patients should be observed to ensure severe intoxication does not re-emerge. Nalmefene has a longer duration of action.
Mixed opioid agonist-antagonists and partial agonists such as pentazocine, butorphanol, nalbuphine, and buprenorphine (see Chapter 36) are less abused than full agonists, although each has a slightly different profile. Except for buprenorphine, they show little cross-dependence with heroin and can exacerbate withdrawal; thus they offer little attraction for addicts.
Another typical abuse pattern begins with self-medication. Some individuals such as long-distance truck drivers or students use stimulants to achieve sustained attention, while often homemakers use these drugs to make tasks (housework) appear easier and complete them faster. These patterns lead to increased doses and frequency of use, producing tolerance and further dose increases. Alcohol or depressant drugs are frequently used to counteract the resultant anxiety and insomnia, establishing a cycle of “uppers and downers.”
Personality changes often occur in stimulant abusers and include delusions, preoccupation with self, hostility, and paranoia. A toxic psychosis can develop. Often difficult to distinguish from paranoid schizophrenia, severe amphetamine and cocaine psychoses require psychiatric management. Antipsychotic medication can be useful (see Chapter 29).
Although acute overdose is not a common problem with hallucinogens, there are other hazards. The most significant is the risk of injury stemming from impaired judgment. In addition, even occasional use of hallucinogens may precipitate a psychiatric illness in predisposed subjects that is exacerbated by repeated use. A poorly understood aspect is the “flashback,” in which previous users re-experience aspects of intoxication while drug-free. Flashbacks also may occur in those who have used marijuana or PCP. They may be no more than déjà vu experiences, or they may be episodes that reflect an emerging psychopathological condition. LSD does not produce withdrawal symptoms or the intense craving caused by other drugs of abuse. However, strong tolerance occurs, with cross-tolerance to other hallucinogens, and increasingly higher doses may be used, leading to unpredictable consequences.
In addition to hallucinogens, other psychoactive drugs can also dramatically alter consciousness and perception. Some are used as adulterants or substitutes in “street drugs” and are frequently misrepresented as LSD or other drugs. The most notable class is antimuscarinics, which may be diverted from medical sources. Atropine and scopolamine are present in many plants and mushrooms, and certain groups of Native Americans and Central Americans practice their ritual use to produce profound alterations in consciousness. Antimuscarinic intoxication can be accompanied by signs of poisoning, and in severe cases, appropriate treatment with the cholinesterase inhibitor physostigmine should be instituted (see Chapter 10).
Steroids are abused largely by body-builders and athletes to improve performance. However, they are also used by others to improve muscle size and reduce body fat and by adolescents who partake in high-risk behaviors. Athletes and body-builders often “stack” steroids, taking different combinations of two or more compounds in cycles of weeks or months in the belief that this improves effects. Because amounts taken are far in excess of natural hormone levels, they result in negative feedback and prevent production of natural hormones. This often results in testicular atrophy, reduced sperm production, and gynecomastia. Steroids in high doses also increase irritability and aggression and produce depression on withdrawal. Many users report that steroids make them feel good and are addictive. A complete description of the side effects of these agents is presented in Chapter 41.
Dietary supplements including dehydroepiandrostenedione and androstenedione (see Chapter 7) are also abused and are converted to anabolic steroids in the body. The use of steroids and steroid supplements is banned by the governing bodies of most sports.
Pharmacotherapies for Substance Abuse
Similarly, there are no medications to treat dependence on CNS depressants, marijuana, hallucinogens, dissociative compounds, inhalants, or anabolic steroids. However, progress in the pharmacotherapy for opioid and nicotine addiction is increasing. The treatment of alcohol dependence is discussed in Chapter 32.
Detoxification of patients receiving opioids for pain relief is accomplished by tapering the dose of a prescribed opioid or by substituting a longer-acting drug. Only rarely does such iatrogenic dependence lead to illicit opioid use, and development of dependence should not be a consideration in providing adequate relief of terminal pain.
Although medications play an important role in treatment of opioid abuse, they are adjuncts to psychosocial and educational interventions. Simple detoxification alone is not usually sufficient to prevent relapse. Most abusers undergo detoxification numerous times, either medically or as a result of interrupted drug supply or incarceration. Non-drug detoxification can be used, or alternatively, abusers can be stabilized on a long-acting oral medication such as methadone. The daily dose is gradually decreased over 30 days (inpatient) or 180 days (outpatient). Withdrawal signs are mild, although the patient will be uncomfortable for most of the withdrawal period. Another approach is to terminate opioids abruptly with an antagonist and treat the symptoms of withdrawal, many of which reflect stress and sympathetic nervous system activation. Medications such as the α2-receptor antagonist clonidine have been used successfully for this purpose (see Chapter 11), particularly in mildly dependent subjects. Antianxiety agents may also be useful.
Benowitz NL. Neurobiology of nicotine addiction: Implications for smoking cessation treatment. Am J Med. 2008;121:S3-S10.
Howell LL, Kimmel HL. Monoamine transporters and psychostimulant addiction. Biochem Pharmacol. 2008;75:196-217.
Volkow et al. 2007 Volkow ND, Fowler JS, Wang GJ, Swanson JM, Telang F. Dopamine in drug abuse and addiction: Results of imaging studies and treatment implications. Arch Neurol. 2007;64:1575-1579.
For further information, see the National Institute for Drug Abuse at http://www.nida.nih.gov.