CHAPTER 53 DRUG TREATMENT
Treatment of epilepsy begins as soon as the diagnosis is made. Typically, this occurs after the second unprovoked seizure, but ancillary data, such as neuroimaging and electroencephalographic (EEG) recording, may support the diagnosis after a single seizure (see Chapters 50 and 52). On the other hand, the diagnosis could be inappropriate after even several seizures, if each can be plausibly regarded as provoked or acutely symptomatic of another condition, as in the case of repeated episodes of alcohol withdrawal or hypoglycemia (described as “occasional seizures” in Chapter 52). Of note is that the seizure risk in some clinical situations is sufficiently high that theoretically epilepsy could be suspected even before a single seizure has occurred; however, one practical argument against this approach is the observation that none of the tested antiepileptic drugs reliably prevents the first seizure in this circumstance.
TREATMENT WITH ANTIEPILEPTIC DRUGS
Principles of use are outlined as follows:
Use of Specific Antiepileptic Drugs
Drugs for Partial and Tonic-Clonic Seizures
Oxcarbazepine
The therapeutic range is 10 to 35 mg/L (monohydroxy-derivative).
Preparations include Trileptal tablets, 150, 300, and 600 mg, and Trileptal syrup, 300 mg/5 mL.
Phenytoin
With regard to pharmacokinetics, the half-life (level-dependent) is 20 to 30 hours when the usual therapeutic range is used; protein binding is 90% (higher with renal failure or hypoalbuminemia).
The usual therapeutic range is 10 to 20 mg/L (arguably 5 to 25 mg/L).
Gabapentin
Teratogenic risk with gabapentin is unknown.
Pregabalin
The disadvantage is that relatively slow titration is needed, to avoid sedation.
Teratogenic risk with pregabalin is unknown.
The provisional therapeutic range is unknown.
Preparations include Lyrica capsules, 25, 50, 75, 100, 150, 200, 225, and 300 mg.
Tiagabine
Teratogenic risk with tiagabine is unknown.
With regard to pharmacokinetics, the half-life is 4 to 9 hours; protein binding is 96%.
The provisional therapeutic range is unknown.
Preparations include Gabitril, 2-, 4-, 12, and 16-mg tablets.
Vigabatrin
A disadvantage is that it may exacerbate generalized epilepsies.
Teratogenic risk with vigabatrin is unknown.
The provisional therapeutic range is unknown.
Preparations include Sabril, 500-mg tablets, and a powder sachet, 500 mg.
Phenobarbital
Advantages of phenobarbital include a long half-life (daily dosing) and its low cost.
The usual therapeutic range is 10 to 40 mg/L (arguably 5 to 30 mg/L).
Drugs for Generalized Seizures, Including Absence and Myoclonic, as Well as Tonic-Clonic
These also are effective against partial seizures.
Valproate
Valproate has teratogenic effects, including a 1% to 2% incidence of neural tube defects.
The usual therapeutic range is 50 to 120 mg/L.
Preparations include Depakene or generic valproic acid capsules, 250 mg; generic syrup, 250 mg/5 mL; Depakote delayed-release tablets, 125, 250, and 500 mg; Depakote Sprinkles slow-release capsules, 125 mg; Depakote-ER extended-release capsules, 250 and 500 mg; and Depacon intravenous infusion, 100 mg/5 mL.
Lamotrigine
Teratogenicity is likely at higher dosages, particularly cleft palate.
Topiramate
Teratogenic risk with topiramate is unknown.
Initiation should be at 25 mg/day, increasing by 25 mg/day per 1 to 2 weeks to a target of 200 mg/day or higher. In pediatric patients (aged ≥2), the dosage should start at 1 to 3 mg/kg/day, increasing by similar amount every 1 to 2 weeks to 5 to 9 mg/kg/day.
The therapeutic range is 5 to 20 mg/L provisionally.
Preparations include Topamax tablets, 25, 100, and 200 mg; Topamax Sprinkles capsules, 15 and 25 mg.
Levetiracetam
The teratogenic risk of levetiracetam is unknown.
Zonisamide
Disadvantages include the need for slow titration and sedation.
Teratogenic risk with zonisamide is unknown.
The therapeutic range is 20 to 40 mg/L provisionally.
The preparation is Zonegran, 100-mg capsules, and generic zonisamide 100-mg capsules.
Methsuximide
Teratogenicity with methsuximide is unknown.
The therapeutic range is 10 to 40 mg/L (N,N-desmethylmethsuximide).
Drugs with a Narrow Spectrum of Action or for Use in Specific Situations
Ethosuximide
Disadvantages include narrow spectrum, with absence seizures the only well-established target.
Teratogenicity with ethosuximide is not known.
Benzodiazepines
Clonazepam
This drug is used as adjunctive therapy for myoclonic and atonic seizures and less often for partial seizures. Its half-life is 20 to 40 hours, shortened by enzyme inducers; the initial dosage is 0.5 mg once or twice daily, increasing by 0.5 mg/day every 3 to 7 days to a target of 1.5 to 4 mg/day. Preparations include Klonopin or generic tablets, 0.5, 1, and 2 mg. An intravenous formulation is available in Europe.
COMMON CLINICAL SITUATIONS AND SPECIFIC SYNDROMES
Approaches to common clinical situations and to specific syndromes are discussed as follows, presented when possible in order of the usual age at manifestation (see Chapter 52 for clinical and diagnostic considerations).
West’s Syndrome (Infantile Spasms)
Alternatives, typically used when ACTH fails or is not tolerated, include prednisone, valproate, clonazepam, lamotrigine, topiramate, felbamate, and tiagabine. Valproate can be initiated at 15 mg/kg/day in three doses and increased in 5- to 10-mg/kg/day weekly increments. Clonazepam is begun at 0.01 to 0.03 mg/kg/day in three doses, increasing by 0.25 to 0.50 mg every three days to a target of 0.1 to 0.2 mg/kg/day. The AED vigabatrin, an inhibitor of γ-amino butyric acid catabolism, is unavailable in the United States, but it can be dramatically effective, especially when the spasms are caused by tuberous sclerosis.
LESIONAL EPILEPSY
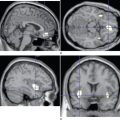
Although structural lesions account for fewer than half of all cases of epilepsy, this proportion is higher among patients with partial epilepsies and those with a later age at onset, especially after age 60. At younger ages, pathological specimens suggest that microscopic structural abnormalities, often disorders of cortical development, underlie many cases of at least medically intractable partial epilepsy, even in those with adolescent or adult onset. Other important pathological causes include neoplasm, especially benign brain tumors such as gangliogliomas, oligodendrogliomas, dysembryoplastic neuroepithelial tumors, and astrocytomas; infections, particularly parasitic infections such as cysticercosis, but also long-term sequelae of bacterial and viral meningoencephalitis; traumatic brain injury, especially penetrating but also closed-head injury if moderate or severe; stroke, both hemorrhagic and ischemic; and congenital or acquired vascular anomalies, such as arteriovenous malformations or cavernous angiomas.
SPECIAL ISSUES RELATED TO EPILEPSY IN WOMEN
Pathophysiology
The mechanisms by which AEDs cause teratogenicity are not well understood and may be different for different AEDs. One hypothesis is that oxidative injury to fetal cells results from reactive AED metabolites. Folate deficiency is also associated with several AEDs and can adversely affect fetal cell division.
SEIZURES AND EPILEPSY IN ELDERLY PERSONS
Diagnosis
Differential diagnosis of transient neurological dysfunction is similar to that discussed in Chapter 52, but in elderly patients, the likelihood of psychogenic nonepileptic seizures is lower than in younger patients, and the risk of such physiological causes as syncope or transient ischemic attack is higher. Prolonged electrocardiographic or video-EEG monitoring may be required for diagnosis. Among sleep disorders, rapid-eye-movement behavior disorder is a parasomnia that is much more common among elderly persons and is often associated with extrapyramidal movement disorders; polysomnography is required for diagnosis.
RESECTIVE SURGERY
Among patients with medically refractory, location-related epilepsy, a significant proportion are candidates for resection of the epileptic focus. In appropriately selected patients, seizure-free rates range from 60% to 80%. The best prognosis is for patients with structural lesions, especially those with mesial temporal sclerosis. The key to a successful outcome is localization of a resectable epileptogenic region, for which a variety of structural and functional tests are used. These commonly include scalp-recorded ictal and interictal EEG recordings, usually with synchronized videography to clarify the ictal semiology; high-quality structural magnetic resonance imaging; positron emission tomography; single photon emission computed tomography (especially if an ictal tracer injection can be accomplished); formal neuropsychological testing; intracarotid amobarbital testing to lateralize language and memory; and, in select cases, magnetoencephalography and functional magnetic resonance imaging. If data are not concordant with regard to the likely epileptogenic and functional regions, intracranial recording with depth and/or subdural electrodes is often needed to identify these areas more definitively.
COMPLEMENTARY AND ALTERNATIVE THERAPIES
Bromfield EB. Clinical use of anticonvulsants: a neurologist’s perspective. Harv Rev Psychiatry. 2003;11:257-268.
Bromfield EB. Epilepsy. In: Samuels MA, editor. Manual of Neurologic Therapeutics. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2004:65-75.
Duncan JS, Sander JW, Sisodiya SM, et al. Adult epilepsy. Lancet. 2006;367:1087-1100.
Spencer SS, Berg AT, Vickrey BG, et al. Predicting long-term seizure outcome after resective epilepsy surgery: the multicenter study. Neurology. 2005;65:912-918.
Wyllie E, Gupta A, Lachhwani DK, editors. The Treatment of Epilepsy: Principles and Practice, 3rd ed., Philadelphia: Lippincott Williams & Wilkins, 2005.